Documente Academic
Documente Profesional
Documente Cultură
Nervous System
Încărcat de
Mini VijayDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Nervous System
Încărcat de
Mini VijayDrepturi de autor:
Formate disponibile
Case study
Linda Hutchison, a 49-year-old Caucasian high school teacher, has had multiple sclerosis (MS) for
over 20 years. She has been very tired lately, has had trouble maintaining urinary continence, is
experiencing weakness, and describes a pins and needles feeling in her legs. Also, muscle
spasms at night are affecting her ability to sleep. She is concerned about an exacerbation of her MS
and arrives at her scheduled appointment to discuss ways to prevent this from happening.
Biographical Data:
LH, 49-year-old Caucasian woman. Alert and oriented. Asks and answers
questions appropriately. Had been working as an office manager at the local high school, but recently
began teaching (her first love) language classes (French and German); she is also responsible for
teaching two physical education (PE) classes a week.
Reason for Seeking Health Care:
I have been so tired and weak lately, and have been having trouble with urinary continence and a
pins and needles feeling in my legs. Leg spasms at night are keeping me awake. I am anxious that I
will have an exacerbation of my MS.
History of Present Health Concern:
The current symptoms began after she recently changed jobs. I get so tired by the end of the week.
If I rest all weekend, I am OK by Monday morning. Ms. Hutchison has had MS for 20 years, but
has managed to function at a near-normal level for most of that time. I had one severe exacerbation
during my divorce, but I went into remission after about 6 months.
Ms. Hutchison denies numbness, seizures, or dizziness. She has not noticed a change in sensations of
taste or smell, hearing, or vision. Client denies difficulty speaking or swallowing. She denies loss
of bowel control. Client denies recent or remote memory loss.
Personal Health History:
Client denies head injury, meningitis, encephalitis, spinal cord injury, stroke or any treatments.
Family History:
Ms. Hutchison reports that her mother has hypertension and migraine headaches. Her father and 2
sisters are in excellent health. Maternal grandmother has hypertension and obesity. Maternal
grandfather died as a result of an automobile accident at age 35. Paternal grandmother has
rheumatoid arthritis. Paternal grandfather has coronary artery disease, hypertension, and diabetes
type 2. Ms. Hutchinson denies a family history of cerebrovascular disease, epilepsy, brain cancer, or
Huntingtons chorea.
Lifestyle and Health Practices:
Takes oxybutynin (Ditropan) as prescribed for MS. Takes multivitamin daily. Denies use of tobacco
or recreational drugs. Reports drinking 23 glasses of wine every 23 months. Reports wearing a
seatbelt at all times. Denies participation in any activities requiring protective headgear. 24-hour
diet recall: Breakfastcereal with 2% milk and 1 cup of coffee; lunchplain ham and cheese
sandwich, 1 small bag plain potato chips, and an apple, with unsweetened iced tea; dinnerpetite
filet mignon, loaded baked potato, salad, water. Denies exposure to lead, insecticides, pollutants, or
other chemicals. Denies frequent heavy lifting or repetitive motions. Reports that she is able to
perform ADLs independently. Denies any change in self-esteem or body image.
Physical Exam Findings:
Alert, thin, middle-aged woman with mildly elevated blood pressure and pulse rate (136/92 and 98).
According to her chart, Ms. Hutchisons blood pressure is normally 100/70.
CN I: Able to correctly identify scents bilaterally.
CN II: Vision 20/20 right eye, left eye, and both eyes. Visual fields intact. Red reflex present
bilaterally. No other internal structures visualized by examiner.
CN III, IV, VI: Extraocular movements intact. No ptosis noted bilaterally. Pupils 5 mm, constricting
to 3 mm bilaterally. Pupils reactive to light and accommodation.
CN V: Temporal and masseter muscles contract bilaterally. Able to identify light touch to forehead,
cheek, and chin. Corneal light reflex symmetric.
CN VII: Able to smile, frown, wrinkle forehead, show teeth, puff out cheeks, purse lips, raise
eyebrows, and close eyes against resistance.
CN VIII: Able to hear whispers from 3 feet bilaterally. Weber test with equal lateralization. Rinne test
AC > BC.
CN IX, X: Uvula and soft palate rise symmetrically with phonation. Gag reflex present. Swallows
without difficulty.
CN XI: Equal shoulder shrug with resistance bilaterally. Turns head in both directions with
resistance.
CN XII: Tongue midline without tremor. Strength of tongue intact.
Motor function:
Muscles are fully developed and symmetric in size.
All muscle are equally strong against resistance. Full range of motion of all extremities.
No involuntary movements noted.
Gait is steady with opposite arm swings. Maintains balance with tandem walking.
Romberg sign is negative.
Rapid alternating movements, finger-to-nose movements and heel-to-shin movement smooth and
intact.
Sensory:
Identifies light, sharp, and dull sensation to extremities and trunk.
Vibratory sensation, sensitivity to position, and stereognosis are intact.
Reflexes:
brachioradialis, bicep, triceps, patellar and achilles reflexes 2+ bilaterally with no ankle clonus.
Abdominal reflex present. Plantar reflex with toe flexion.
No signs of meningeal irritation or inflammation.
S-ar putea să vă placă și
- Health History and Physical Examination ReportDocument4 paginiHealth History and Physical Examination ReportKat SunicoÎncă nu există evaluări
- FNP 3 - JiaDocument16 paginiFNP 3 - Jiaapi-551073862100% (1)
- Geri SOAPsampleDocument8 paginiGeri SOAPsampleJacquelineÎncă nu există evaluări
- Acute PancreatitisDocument7 paginiAcute PancreatitisPatrick DycocoÎncă nu există evaluări
- Chronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicDe la EverandChronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicEvaluare: 5 din 5 stele5/5 (1)
- Final Assessment Soap NoteDocument13 paginiFinal Assessment Soap Noteapi-494643478100% (3)
- Carbuncle, Incision, Drainage, DebridementDocument11 paginiCarbuncle, Incision, Drainage, DebridementAlvin Germo PasuquinÎncă nu există evaluări
- Comprehensive H and P ExampleDocument5 paginiComprehensive H and P ExampleMallory ZaborÎncă nu există evaluări
- Family Case SampleDocument25 paginiFamily Case SampleGrInDoVe9097Încă nu există evaluări
- Objectives PsychDocument6 paginiObjectives PsychHerbie SoÎncă nu există evaluări
- Our Lady of Fatima UniversityDocument5 paginiOur Lady of Fatima UniversityEmmanuel De LeonÎncă nu există evaluări
- Genome PaperDocument7 paginiGenome Paperapi-444163791100% (1)
- Colorful Vintage Library Furniture Animated Illustration Book Report Education PresentationDocument51 paginiColorful Vintage Library Furniture Animated Illustration Book Report Education PresentationCarl Philip PerezÎncă nu există evaluări
- Carpe Diem Ruiz Protcol Grand Rounds 4Document9 paginiCarpe Diem Ruiz Protcol Grand Rounds 4John Christopher RuizÎncă nu există evaluări
- Y3 T2 PAM CWU 2 - Acute BronchiolitisDocument7 paginiY3 T2 PAM CWU 2 - Acute Bronchiolitisanon_67984147Încă nu există evaluări
- Headache: a family doctor’s guide to treating a common ailmentDe la EverandHeadache: a family doctor’s guide to treating a common ailmentÎncă nu există evaluări
- Gut: the new and revised Sunday Times bestsellerDe la EverandGut: the new and revised Sunday Times bestsellerEvaluare: 4 din 5 stele4/5 (393)
- NSG6435 Soap3Document6 paginiNSG6435 Soap3Hephzibah BeulahÎncă nu există evaluări
- Ward Paper LegitDocument13 paginiWard Paper LegitLuigi FranciscoÎncă nu există evaluări
- Chief ComplaintDocument7 paginiChief ComplaintyohannesÎncă nu există evaluări
- Carpe Diem Ruiz Protcol Grand Rounds 4Document10 paginiCarpe Diem Ruiz Protcol Grand Rounds 4John Christopher RuizÎncă nu există evaluări
- Nsg6435 Soap Note 2Document7 paginiNsg6435 Soap Note 2Hephzibah Beulah100% (1)
- Congestive Heart FailureDocument118 paginiCongestive Heart Failureunagracia100% (6)
- Head To Toe Write UpDocument3 paginiHead To Toe Write Upapi-554096544Încă nu există evaluări
- HPI ExampleDocument4 paginiHPI ExampleSteveÎncă nu există evaluări
- Case IhDocument43 paginiCase IhChie Hyun-AeÎncă nu există evaluări
- Datuin - PediaDocument13 paginiDatuin - PediaMika SaldañaÎncă nu există evaluări
- Hypertension Case IMDocument5 paginiHypertension Case IMPerlyn Mac Basiloy - AloÎncă nu există evaluări
- History 1Document11 paginiHistory 1KaleabÎncă nu există evaluări
- IM Gastro FinalDocument10 paginiIM Gastro FinalIzzyMaxinoÎncă nu există evaluări
- 3rd Year Precept Pedia Case 4 HydroceleDocument4 pagini3rd Year Precept Pedia Case 4 Hydrocelekristel_nicole18yaho100% (1)
- In the Shadow of Illness: Parents and Siblings of the Chronically Ill ChildDe la EverandIn the Shadow of Illness: Parents and Siblings of the Chronically Ill ChildÎncă nu există evaluări
- Sample Write UpDocument2 paginiSample Write UpNar Patrick Padilla100% (1)
- Junsay, Twinkle Mae D. Section A - Group 10 History #1Document15 paginiJunsay, Twinkle Mae D. Section A - Group 10 History #1Twinkle Mae JunsayÎncă nu există evaluări
- Ibn Sina College For Health Sciences Home Visit Plan For Elderly Studantns: Areej Al-Hawareen & Adel MahareeqDocument10 paginiIbn Sina College For Health Sciences Home Visit Plan For Elderly Studantns: Areej Al-Hawareen & Adel Mahareeqمالك مناصرةÎncă nu există evaluări
- Patient ChartDocument1 paginăPatient ChartEden Torres MirandaÎncă nu există evaluări
- Case Study - TonsillitisDocument7 paginiCase Study - TonsillitisFianne Villanueva67% (6)
- Soap Note - 6Document4 paginiSoap Note - 6api-546259691100% (1)
- Faculty of Medicine and Health Sciences Score Sheet For CASE Write-UpDocument30 paginiFaculty of Medicine and Health Sciences Score Sheet For CASE Write-UpJared Khoo Er HauÎncă nu există evaluări
- GERD (Gastroesophageal Reflux Disease)Document112 paginiGERD (Gastroesophageal Reflux Disease)Mharj Alfelor Cecilio100% (7)
- Nursing Case Study TAHBSODocument17 paginiNursing Case Study TAHBSOandymojer85% (13)
- University of Northern PhilippinesDocument6 paginiUniversity of Northern PhilippinesEliazar Alumbro Peniton Jr.Încă nu există evaluări
- FocusedDocument4 paginiFocusedlizdp21Încă nu există evaluări
- Case Study ESRDDocument30 paginiCase Study ESRDreginebenedicte100% (1)
- Case Study Activity 1-4Document7 paginiCase Study Activity 1-4kuma phÎncă nu există evaluări
- IM Clinics History 2Document4 paginiIM Clinics History 2LucyellowOttemoesoeÎncă nu există evaluări
- Pyomyositis (Ca1)Document66 paginiPyomyositis (Ca1)Emman Ramos60% (5)
- Patient Health HistoryDocument8 paginiPatient Health HistoryRafi LabÎncă nu există evaluări
- Pediatric No 1 Soap Notes 1Document5 paginiPediatric No 1 Soap Notes 1darrolddeleon1992Încă nu există evaluări
- Pedia Ward WorkDocument14 paginiPedia Ward WorkGrace Antonette PatiÎncă nu există evaluări
- Sample Case ProtocolDocument6 paginiSample Case ProtocoljheyfteeÎncă nu există evaluări
- Good Health in the 21st Century: a family doctor's unconventional guideDe la EverandGood Health in the 21st Century: a family doctor's unconventional guideÎncă nu există evaluări
- Psych Anamnesis SampleDocument3 paginiPsych Anamnesis Samplemefav777852043% (7)
- Flourishing After Adversity: A 3-Step Action Plan to Transform Pain into Purpose and Embrace Joy AgainDe la EverandFlourishing After Adversity: A 3-Step Action Plan to Transform Pain into Purpose and Embrace Joy AgainÎncă nu există evaluări
- Low Back PainDocument9 paginiLow Back PainDoc AchondoÎncă nu există evaluări
- Soap Note 2 Dominguez 2015Document5 paginiSoap Note 2 Dominguez 2015api-320062911Încă nu există evaluări
- Case History The Chief Complaint (CC)Document18 paginiCase History The Chief Complaint (CC)21912664Încă nu există evaluări
- NCP of Client With Cancer Servix With Multiple Bone MetastasisDocument17 paginiNCP of Client With Cancer Servix With Multiple Bone MetastasisHarismaPratamaÎncă nu există evaluări
- Adult Med Surgical Assessment ToolDocument6 paginiAdult Med Surgical Assessment ToolWesley WashingtonÎncă nu există evaluări
- Covid-19 Detector Using The Power of Python and Arduino, This Detector Measures and Records User TemperatureDocument5 paginiCovid-19 Detector Using The Power of Python and Arduino, This Detector Measures and Records User TemperatureAshu SÎncă nu există evaluări
- English Composition II 1Document11 paginiEnglish Composition II 1api-548473407Încă nu există evaluări
- Upper GI BleedingDocument70 paginiUpper GI BleedingMia MusÎncă nu există evaluări
- Covid-19 Expose (Unmask)Document2 paginiCovid-19 Expose (Unmask)Eduardo CasesÎncă nu există evaluări
- Primary and Secondary AmenorrhoeaDocument72 paginiPrimary and Secondary Amenorrhoead clarkeÎncă nu există evaluări
- Salmon Dna: Introducing Scientific Breaktrough From JapanDocument6 paginiSalmon Dna: Introducing Scientific Breaktrough From JapanLeonardo100% (1)
- Essay On WaterDocument111 paginiEssay On WaterBlue StoneÎncă nu există evaluări
- Contact Lens Complications and ManagementDocument10 paginiContact Lens Complications and Managementstrawberry8832850% (2)
- Final Coaching NP4 Set 1Document13 paginiFinal Coaching NP4 Set 1STEFFI GABRIELLE GOLEZÎncă nu există evaluări
- Master The Perfec Tnight of SleepDocument10 paginiMaster The Perfec Tnight of SleepPaulo André Prada de CamargoÎncă nu există evaluări
- Journal Reading Survey OphtalmologyDocument17 paginiJournal Reading Survey OphtalmologynadyajondriÎncă nu există evaluări
- Liver Pathology EMQDocument1 paginăLiver Pathology EMQhazirmm100% (2)
- USMLE Step 1 First Aid 2021-101-230Document130 paginiUSMLE Step 1 First Aid 2021-101-230mariana yllanesÎncă nu există evaluări
- Autism Spectre DisorderDocument13 paginiAutism Spectre DisorderJesus Hurtado100% (2)
- Diabetes Mellitus ResearchDocument6 paginiDiabetes Mellitus ResearchJohnÎncă nu există evaluări
- Chap 79Document5 paginiChap 79Ma.Nicole SubongÎncă nu există evaluări
- Home Quarantine Compliance 2022 1Document1 paginăHome Quarantine Compliance 2022 1Puting KahoyÎncă nu există evaluări
- Worku Antomy and Physiology of Reproductive OrganDocument206 paginiWorku Antomy and Physiology of Reproductive OrganMignot AnileyÎncă nu există evaluări
- Neurology & Pupils (No 467)Document231 paginiNeurology & Pupils (No 467)Mohamed GaberÎncă nu există evaluări
- SAM 350P User ManualDocument40 paginiSAM 350P User ManualkristiaÎncă nu există evaluări
- Analytical Case Study of Bmiof Mildly Symptomatic Covid-19 Patients With Reference To MizajDocument7 paginiAnalytical Case Study of Bmiof Mildly Symptomatic Covid-19 Patients With Reference To MizajyusufÎncă nu există evaluări
- Normal Periodontium 1Document49 paginiNormal Periodontium 1mdio midoÎncă nu există evaluări
- Cerebral PalsyDocument21 paginiCerebral PalsyEMily AbastaÎncă nu există evaluări
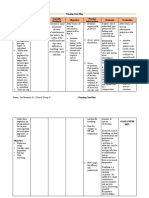
- Nursing Care PlanDocument13 paginiNursing Care PlanJan DamesÎncă nu există evaluări
- Heart Disease and Cancer: CirculationDocument4 paginiHeart Disease and Cancer: CirculationDewi AyuÎncă nu există evaluări
- Bazaar DrugsDocument104 paginiBazaar DrugsKartik Vashishta100% (1)
- Zybio Company Profile 20211109CDocument46 paginiZybio Company Profile 20211109CĐức Hòa100% (1)
- Pharmaceutical Market Europe - June 2020Document50 paginiPharmaceutical Market Europe - June 2020Areg GhazaryanÎncă nu există evaluări
- Setting The Standard: Managing Food Allergies in SchoolDocument50 paginiSetting The Standard: Managing Food Allergies in SchooldadowildcatsÎncă nu există evaluări
- Edible TallowDocument3 paginiEdible TallowteddydeÎncă nu există evaluări