Documente Academic
Documente Profesional
Documente Cultură
The Influence of Mechanical Bowel Preparation
Încărcat de
Faisol KabirDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
The Influence of Mechanical Bowel Preparation
Încărcat de
Faisol KabirDrepturi de autor:
Formate disponibile
The American Journal of Surgery (2015) 210, 106-110
Clinical Science
The influence of mechanical bowel preparation
on long-term survival in patients surgically
treated for colorectal cancer
Hans Pieter vant Sant, M.D.a,*, Arnoud Kamman, M.D.a,
Wim C. J. Hop, Ph.D.b, Martijn van der Heijden, M.D.a,
Johan F. Lange, M.D., Ph.D.c, Caroline M. E. Contant, M.D., Ph.D.d
a
Department of Surgery, Ikazia Hospital, Montessoriweg 1, 3083 AN Rotterdam, The Netherlands;
Department of Biostatistics, cDepartment of Surgery, Erasmus University Medical Center, Rotterdam,
The Netherlands; dDepartment of Surgery, Maasstad Hospital, Rotterdam, The Netherlands
KEYWORDS:
Survival;
Colorectal cancer;
Surgery
Abstract
BACKGROUND: In this study, we evaluated long-term survival in patients treated with and without
mechanical bowel preparation (MBP) before colorectal surgery for cancer.
METHODS: Long-term outcome of patients of 2 main participating hospitals in a prior multicenter
randomized trial comparing clinical outcome of MBP versus no MBP was reviewed. Primary endpoint
was cancer-related mortality and secondary endpoint was all-cause mortality.
RESULTS: A total of 382 patients underwent potentially curative surgery for colorectal cancer. One
hundred seventy-seven (46%) patients were treated with MBP and 205 (54%) were not before surgery.
Median follow-up was 7.6 years (mean 6.6, range .01 to 12.73). There was no significant difference in
both cancer-related mortality and all-cause mortality in patients treated with MBP and without MBP (P
5 .76 and P 5 .36, respectively). Multivariate analysis, taking account of age, sex, AJCC cancer stage,
and ASA classification, also showed no survival difference.
CONCLUSIONS: Our results indicate that MBP does not seem to influence long-term survival in patients surgically treated for colorectal cancer.
2015 Elsevier Inc. All rights reserved.
There were no relevant financial relationships or any sources of support
in the form of grants, equipment, or drugs.
The authors declare no conflicts of interest.
Trial registration number for the randomized clinical trial this article
derived from was NCT00288496.
* Corresponding author. Tel.: 131-633332710; fax: 131-102975130.
E-mail address: hpieter44@hotmail.com
Manuscript received January 29, 2014; revised manuscript October 4,
2014
0002-9610/$ - see front matter 2015 Elsevier Inc. All rights reserved.
http://dx.doi.org/10.1016/j.amjsurg.2014.10.022
Traditionally, mechanical bowel preparation (MBP) was
believed to clean the colon and rectum from residual fecal
contents and lower the bacterial load to prevent anastomotic failure and reduce postoperative infectious complications.1 To date, however, there is significant evidence that
questions the beneficial effects of MBP. Recent systematic
reviews and meta-analyses of randomized controlled trials
have shown no evidence that MBP is associated with
reduced rates of anastomotic leakage or septic complications after elective colorectal surgery.24 Most studies
H.P. vant Sant et al.
MBP and survival for colorectal cancer
only evaluated the effects of MBP on short-term outcomes
and studies on the effects of long-term outcomes are scarce,
especially cancer related. At present, there is strong
evidence that postoperative complications influence the
long-term outcome and survival in patients with colorectal
cancer. Patients confronted with anastomotic leakage have
poorer long-term cancer-specific survival rates.57 In this
study, we tested the hypothesis that MBP has no positive influence on cancer-specific long-term survival (.6 years) after colorectal cancer surgery as MBP is not associated with
reduced anastomotic leakage rates in literature.
Methods
This study is a subgroup analysis of a prior large
multicenter randomized clinical trial published by Contant
et al.8 They enrolled 1,354 patients from 1998 to 2004 and
randomized between MBP and no MBP before elective
colorectal surgery and compared the incidence of anastomotic leakage and septic complications. Patients randomized for MBP received 2 to 4 l of polyethylene glycol
bowel lavage solution (***Klean Prep) in combination
with ***bisacodyl (11 hospitals) or sodium phosphate solution (2 hospitals). Exclusion criteria were an acute laparotomy, laparoscopic colorectal surgery, contraindications for
the use of MBP, an a priori diverting ileostomy, and age
less than 18 years old.
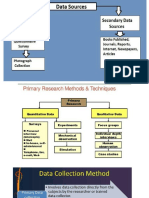
In the present subgroup analysis, 382 patients of 2 main
participating hospitals in the previously mentioned randomized trial were selected by the criteria of having
undergone potentially curative elective colorectal surgery
for cancer (Fig. 1). Clinical data were obtained through the
previous study by Contant et al8 with permission and linked
to death records to create a novel dataset. Death records up
to December 31, 2010 were obtained. The diagnosis of
colorectal cancer was confirmed by pathology reports. Cancer stage was determined through pathology reports, radiology reports, and clinical audit records. Our primary
Figure 1
107
endpoint was cancer-related mortality and secondary
endpoint was all-cause mortality.
Statistical analysis
KaplanMeier curves for overall and colon cancerspecific survival and log-rank tests were used to compare
the MBP arms. In the calculation of cancer-specific
survival, the survivals*** of patients who had died because
of other causes were considered censored*** survival
times. As the large majority of deaths were because of
cancer and there were only a few patients who had died
from an unknown cause, the latter patients were considered
to have died from cancer. Cox-regression analysis was used
to assess the independent effect of various putative
prognostic factors (age, sex, cancer stage, and ASA
classification) besides MBP. Analysis was by intention-totreat. Two-sided P value of less than .05 was considered
statistically significant.
Results
Data were collected from 382 patients retrospectively.
Patient selection is shown in Fig. 1. One hundred seventyseven (46%) patients were treated with MBP before surgery
and 205 (54%) were not. Baseline characteristics of patients are shown in Table 1 and were well balanced between
treatment groups. Overall median follow-up was 7.6 (mean
6.6, range .01 to 12.73) years. Median follow-up for MBP1
was 7.8 (mean 6.8, range .01 to 12.6) and for MBP2 was
7.4 (mean 6.4, range .01 to 12.7). One hundred ninetythree patients deceased during follow-up. Cancer-related
deaths occurred in 128 patients. Noncancer-related deaths
occurred in 48 patients. In 17 patients, the cause of death
could not be discovered. There was no significant difference in both overall mortality and cancer-related mortality
in patients treated with MBP and without MBP before elective colorectal surgery for cancer (log-rank test, P 5 .36
Organization chart for patient selection.9
108
The American Journal of Surgery, Vol 210, No 1, July 2015
Table 1 Baseline characteristics of 382 patients undergoing
elective surgical treatment for colorectal cancer
Sex
Male
Female
Age (years)
%60
6170
.70
Cancer stage*
I
II
III
IV
ASA classification
I
II
III/IV
Adjuvant chemotherapy
Radiation therapy
MBP2
(n 5 205)
MBP1
(n 5 177)
98 (48%)
107 (52%)
91 (51%)
86 (49%)
50 (24%)
70 (34%)
85 (42%)
42 (24%)
56 (32%)
79 (44%)
34
98
55
18
(16%)
(48%)
(27%)
(9%)
35
77
51
14
(20%)
(43%)
(29%)
(8%)
57
113
35
47
12
(28%)
(55%)
(17%)
(23%)
(6%)
39
116
22
32
18
(22%)
(66%)
(12%)
(18%)
(10%)
ASA 5 American Society of Anesthesiologists; MBP 5 mechanical
bowel preparation.
*Colon and rectum cancer stage according to the American Joint
Committee on Cancer.
and P 5 .76, respectively; Fig. 2). Thirty-day mortality for
the groups with and without MBP was 4.0% (7/177) and
2.4% (5/205), respectively (P 5 .58).
Cancer-specific survival at 5- and 10 years in the MBP1
arm was 67% (64% standard error) and 59% (64%),
respectively. In the MBP2 arm, these figures were 68%
(63%) and 60% (64%), respectively (Fig. 2).
Overall survival at 5- and 10 years in the MBP1 arm
was 64% (64%) and 54% (64%), respectively. In the
MBP2 arm, these figures were 62% (63%) and 47%
(64%), respectively (Fig. 2).
Also within the separate cancer stages, there were no
significant differences in overall and cancer-specific survival between the MBP arms (all P . .31). Cox-regression
analysis, allowing for age, sex, cancer stage, and ASA classification, also showed no significant differences between
the 2 MBP arms (Table 2). Further extension of the Cox
models with interaction terms to investigate whether the
baseline characteristics influenced the difference between
the 2 MBP arms showed no significant effect of any of
the characteristics. Also, the treatment center did not affect
the survival outcomes.
Postoperative complication rates between patients
treated with and without MBP are shown in Table 3.
Comments
Sufficient evidence has shown that anastomotic leakage
is associated with a higher prevalence of local recurrence
and diminished long-term survival after elective colorectal
cancer surgery.57 Recent meta-analysis and systematic reviews show no difference in anastomotic leakage rates
comparing MBP versus no MBP. Only Slim et al9 published
a meta-analysis in 2004 and found significantly more anastomotic leakage after MBP (5.6% vs 3.2%, P 5 .032).
However, a more recent meta-analysis also by Slim et al
invalidate this outcome having added 2 large randomized
Figure 2 KaplanMeier survival curves for OS and CaS for patients treated with and without MBP before elective colorectal surgery for
cancer. CaS 5 cancer-specific survival; OS 5 overall survival.
H.P. vant Sant et al.
MBP and survival for colorectal cancer
109
Table 2 Multivariate analyses of various factors in relation to cancer-related and all-cause mortality after elective colorectal resection
for cancer
Cancer-related mortality
MBP
No
Yes
Sex
Female
Male
Age
%60
6170
.70
Cancer stage
I
II
III
IV
ASA classification
I
II
III/IV
All-cause mortality
Hazard ratio
95% CI
P value
Hazard ratio
95% CI
P value
1.00
.94
.671.32
.73
1.00
.81
.611.09
.16
1.00
1.14
.811.61
.46
1.00
1.23
.911.65
.17
1.00
1.10
2.77
.641.91
1.594.84
.73
,.001
1.00
1.28
2.56
.802.05
1.604.11
.30
,.001
1.00
2.67
6.91
41.01
1.205.91
3.1215.28
17.6095.58
.02
,.001
,.001
1.00
1.57
2.97
17.86
.952.61
1.765.00
9.7732.66
.08
,.001
,.001
1.00
1.11
2.36
.671.85
1.284.35
.68
.006
1.00
1.38
3.05
.892.14
1.815.13
.15
,.001
ASA 5 American Society of Anesthesiologists; CI 5 confidence interval; MBP 5 mechanical bowel preparation.
Contant et al8 showed that MBP was associated with fewer
intra-abdominal abscesses after anastomotic leakage
compared with no MBP in elective colorectal surgery.
However, both studies show no difference in anastomotic
leakage rates. In summary, this leaves us with controversial
effects of MBP on anastomotic leakage and postoperative
infection rates. As a result the influence of applying or
withholding MBP on survival in patients surgically treated
for colorectal cancer remains unpredictable and unclear.
When looking at literature regarding MBP and longterm survival, Nicholson et al retrospectively collected data
of 1,730 patients who underwent potentially curative
colorectal cancer surgery.15 One thousand four hundred
sixty patients were treated with MBP and 270 patients
were not. Median follow-up was 3.5 (range .1 to 6.7) years.
They found a 28% survival benefit in favor of patients
treated with MBP (HR*** .72, .57 to .91) (P 5 .005).
controlled trials to their data and find no difference in anastomotic leakage rate between MBP and no MBP.2,8,10 Other
effects of MBP on postoperative complications have been
thoroughly investigated presenting controversial results.
Bucher et al11,12 suggest that MBP is associated with structural alteration and inflammatory changes in the large
bowel wall and that MBP is associated with higher postoperative morbidity rates in elective left-sided colorectal surgery. This is supported by Bretagnol et al, who noted that
MBP was associated with a significantly higher rate of infectious extra-abdominal complications.7 Mean hospital
stay was significantly longer for patients treated with
MBP in both studies.11,13 In contrast, authors of the French
Greccar III trial demonstrated that rectal cancer surgery
without MBP was associated with higher risk of overall
and infectious morbidity rates and suggest continuing to
perform MBP before elective rectal resection for cancer.14
Table 3
Complication rate after elective surgery for patients with colorectal cancer with and without preoperative MBP
Complication
MBP1 (n 5 177)
MBP2 (n 5 205)
No. of patients with complications*
Anastomotic leakage
Wound infection
Urinary tract infection
Pneumonia
Intra-abdominal abscess
Fascia dehiscence
59
7
18
12
14
6
2
82
8
25
18
16
9
6
MBP 5 mechanical bowel preparation.
*Patients can have more than one complication at a time.
(33%)
(4%)
(10%)
(7%)
(8%)
(3%)
(1%)
(40%)
(4%)
(12%)
(3%)
(8%)
(4%)
(3%)
110
The American Journal of Surgery, Vol 210, No 1, July 2015
However, this survival advantage was no longer significant
after adjustment for presentation for surgery (HR .85, .67 to
1.10) (P 5 .220). This can be clearly explained because of
the fact that patients undergoing emergency surgery are
usually not treated with MBP and that the emergency
setting is associated with poorer outcome.16,17 The authors
of this study conclude that neither postoperative complications nor long-term survival are improved by MBP in regards to colonic cancer. However, this retrospective
cohort study has several limitations. Their main conclusion
was based on all-cause mortality and not on cancer-related
mortality. In addition, patients were not randomized between MBP and no MBP and the decision for applying
MBP was solely made ad hoc by the medical staff before
surgery, creating a potential source of bias.
The results of the underlying study show that MBP has
no influence on all-cause and cancer-related long-term
survival in patients surgically treated for colorectal cancer
with a median follow-up of 6.7 years. Adverse events
relating to colorectal cancer survival would be expected
within this time frame. These findings were expected as we
found no difference in anastomotic leakage and other
postoperative morbidity rates between the MBP1 and
MBP2 groups in this study. One of the limitations of this
study is the selection procedure. We selected patients from
only 2 of the 13 hospitals who participated in a previous
randomized trial comparing the anastomotic leakage rate in
patients treated with and without MBP.8 By selecting patients only surgically treated for cancer, we created an
imbalance between MBP1 and MBP2 (177 vs 205,
respectively) and a possible selection bias cannot be
excluded. An additional limitation is that in 17 patients
the cause of death could not be recollected. For these 17 patients, cancer-related mortality was both calculated when
deaths were presumed cancer related and when left out.
There were no differences between both calculations.
Data are only shown when deaths were presumed cancer
related as this is most probable. As survival depends on
many factors, our study is underpowered. A large randomized trial would be preferable with long-term survival as
primary endpoint in a cancer-related patient group.
In conclusion, our results from a subgroup of a randomized trial suggest confirmation of our hypothesis that MBP
has no influence on long-term survival in patients surgically
treated for colorectal cancer. However, more research is
required to draw firm conclusions.
References
1. Fa-Si-Oen PR, Verwaest C, Buitenweg J, et al. Effect of mechanical
bowel preparation with polyethyleneglycol on bacterial contamination
and wound infection in patients undergoing elective open colon surgery. Clin Microbiol Infect 2005;11:15860.
2. Slim K, Vicaut E, Launay-Savary MV, et al. Updated systematic review and meta-analysis of randomized clinical trials on the role of mechanical bowel preparation before colorectal surgery. Ann Surg 2009;
249:2039.
3. Guenaga KK, Matos D, Wille-Jrgensen P. Mechanical bowel preparation for elective colorectal surgery. Cochrane Database Syst Rev 2009;
21:CD001544.
4. Pineda CE, Shelton AA, Hernandez-Boussard T, et al. Mechanical
bowel preparation in intestinal surgery: a meta-analysis and review
of the literature. J Gastrointest Surg 2008;12:203744.
5. Walker KG, Bell SW, Rickard MJ, et al. Anastomotic leakage is predictive of diminished survival after potentially curative resection for
colorectal cancer. Ann Surg 2004;240:2559.
6. McArdle CS, McMillan DC, Hole DJ. Impact of anastomotic leakage
on long-term survival of patients undergoing curative resection for
colorectal cancer. Br J Surg 2005;92:11504.
7. Kube R, Mroczkowski P, Granowski D, et al. Anastomotic leakage after colon cancer surgery: a predictor of significant morbidity and hospital mortality, and diminished tumour-free survival. Eur J Surg Oncol
2010;36:1204.
8. Contant CM, Hop WC, vant Sant HP, et al. Mechanical bowel preparation for elective colorectal surgery: a multicentre randomised trial.
Lancet 2007;370:21127.
9. Slim K, Vicaut E, Panis Y, et al. Meta-analysis of randomized clinical
trials of colorectal surgery with or without mechanical bowel preparation. Br J Surg 2004;91:112530.
10. Jung B, Pahlman L, Nystrom PO, et al. Multicentre randomized clinical trial of mechanical bowel preparation in elective colonic resection.
Br J Surg 2007;94:68995.
11. Bucher P, Gervaz P, Soravia C, et al. Randomized clinical trial of mechanical bowel preparation versus no preparation before elective leftsided colorectal surgery. Br J Surg 2005;92:40914.
12. Bucher P, Gervaz P, Egger JF, et al. Morphologic alterations associated
with mechanical bowel preparation before elective colorectal surgery:
a randomized trial. Dis Colon Rectum 2005;49:10912.
13. Bretagnol F, Alves A, Ricci A, et al. Rectal cancer surgery without mechanical bowel preparation. Br J Surg 2007;94:126671.
14. Bretagnol F, Panis Y, Rullier E, et al. Rectal cancer surgery
with or without bowel preparation. The French Greccar III
multicenter single-blinded randomized trial. Ann Surg 2010;
252:8638.
15. Nicholson GA, Finlay IG, Diament RH, et al. Mechanical bowel preparation does not influence outcomes following colonic cancer resection. Br J Surg 2011;98:86671.
16. Cuffy M, Abir F, Audisio RA, et al. Colorectal cancer presenting as
surgical emergencies. Surg Oncol 2004;13:14957.
17. Porta M, Fernandez E, Belloc J, et al. Emergency admission for cancer: a matter of survival? Br J Cancer 1998;77:47784.
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Rabies: Elimination of in BangladeshDocument41 paginiRabies: Elimination of in BangladeshFaisol KabirÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Overview of New Death Certificate PDFDocument59 paginiOverview of New Death Certificate PDFFaisol KabirÎncă nu există evaluări
- Emergency Department SOP V4.1Document17 paginiEmergency Department SOP V4.1Faisol KabirÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Emergency Department SOP V4.1Document17 paginiEmergency Department SOP V4.1Faisol KabirÎncă nu există evaluări
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- All About Rabies!: Level 3Document27 paginiAll About Rabies!: Level 3Faisol KabirÎncă nu există evaluări
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Patient's Follow Up Profile SU1Document2 paginiPatient's Follow Up Profile SU1Faisol KabirÎncă nu există evaluări
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Charter of Duties of Upazila Parishad Officers PDFDocument28 paginiCharter of Duties of Upazila Parishad Officers PDFFaisol KabirÎncă nu există evaluări
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Epidemic Situation of Tuberculosis in Bangladesh PDFDocument2 paginiEpidemic Situation of Tuberculosis in Bangladesh PDFFaisol KabirÎncă nu există evaluări
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Landscape Photography With Your Smartphone: PhotzyDocument30 paginiLandscape Photography With Your Smartphone: PhotzyFaisol KabirÎncă nu există evaluări
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Prescribed Leave Rules, 1959 (Bangla)Document3 paginiThe Prescribed Leave Rules, 1959 (Bangla)Faisol KabirÎncă nu există evaluări
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Epidemic Situation of Tuberculosis in Bangladesh PDFDocument2 paginiEpidemic Situation of Tuberculosis in Bangladesh PDFFaisol KabirÎncă nu există evaluări
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Malaria Treatment Guidelines-2 ND Edition 2011Document210 paginiMalaria Treatment Guidelines-2 ND Edition 2011Kevins KhaembaÎncă nu există evaluări
- WHO Dengue Guidelines 2013Document160 paginiWHO Dengue Guidelines 2013Jason MirasolÎncă nu există evaluări
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- BSMMU MS UROLOGY CurriculumDocument16 paginiBSMMU MS UROLOGY CurriculumFaisol KabirÎncă nu există evaluări
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Kdigo-Gn-Guideline GN PDFDocument143 paginiKdigo-Gn-Guideline GN PDFFerry JuniansyahÎncă nu există evaluări
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Snake Bite As A Public Health Problem Bangladesh PDocument7 paginiSnake Bite As A Public Health Problem Bangladesh PFaisol KabirÎncă nu există evaluări
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- CXR Reading in TB Suspects - JATADocument32 paginiCXR Reading in TB Suspects - JATAFaisol KabirÎncă nu există evaluări
- Treatment GuidelinesDocument223 paginiTreatment Guidelines14568586794683% (6)
- National Guidelines and Operational Manual For Tuberculosis Control PDFDocument90 paginiNational Guidelines and Operational Manual For Tuberculosis Control PDFFaisol KabirÎncă nu există evaluări
- Treatment of Liver AbscessDocument1 paginăTreatment of Liver AbscessFaisol KabirÎncă nu există evaluări
- KDIGO AKI Guideline DownloadDocument141 paginiKDIGO AKI Guideline DownloadSandi AuliaÎncă nu există evaluări
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- SAM Guideline PDFDocument95 paginiSAM Guideline PDFFaisol KabirÎncă nu există evaluări
- National Asthma - Bronchiolitis - COPD GuidelinesDocument84 paginiNational Asthma - Bronchiolitis - COPD GuidelinesFaisol Kabir86% (7)
- Data CollctionDocument3 paginiData CollctionFaisol KabirÎncă nu există evaluări
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- National Nipah Virus Guideline BangladeshDocument77 paginiNational Nipah Virus Guideline BangladeshFaisol KabirÎncă nu există evaluări
- Pathology BinderDocument406 paginiPathology BinderFaisol KabirÎncă nu există evaluări
- Anatomy BinderDocument816 paginiAnatomy BinderFaisol Kabir100% (1)
- Networking - How To Transfer Files Between Ubuntu and Windows - Ask UbuntuDocument3 paginiNetworking - How To Transfer Files Between Ubuntu and Windows - Ask UbuntuFaisol KabirÎncă nu există evaluări
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (120)
- Surgical Nursing Brunner 2016Document74 paginiSurgical Nursing Brunner 2016Faisol Kabir100% (1)
- Komposisi z350Document9 paginiKomposisi z350muchlis fauziÎncă nu există evaluări
- Inhibidores de La ECADocument16 paginiInhibidores de La ECAFarmaFMÎncă nu există evaluări
- BibliopocDocument4 paginiBibliopocKarlo ReyesÎncă nu există evaluări
- 18Th June 2019 Plab 1 Mock Test Plab ResourcesDocument30 pagini18Th June 2019 Plab 1 Mock Test Plab Resourceskhashayar HajjafariÎncă nu există evaluări
- NCP Ineffective Airway Clearance Related To Lung Impairment PNEUMOTHORAXDocument5 paginiNCP Ineffective Airway Clearance Related To Lung Impairment PNEUMOTHORAXMa. Elaine Carla Tating0% (2)
- Training Workshop On Attitudinal ChangeDocument5 paginiTraining Workshop On Attitudinal ChangeSam ONiÎncă nu există evaluări
- Homeopathy and PaediatricsDocument15 paginiHomeopathy and PaediatricsCristinaÎncă nu există evaluări
- FurosemideDocument5 paginiFurosemideRaja Mashood ElahiÎncă nu există evaluări
- Msds Nano PolishDocument5 paginiMsds Nano PolishGan LordÎncă nu există evaluări
- Chapter 11 Occlusal Adjustment PDFDocument8 paginiChapter 11 Occlusal Adjustment PDFDavid ColonÎncă nu există evaluări
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- List Alat OK Mayor Dan Minor 30 07 2022 20.12Document72 paginiList Alat OK Mayor Dan Minor 30 07 2022 20.12dehaaÎncă nu există evaluări
- Test 6 Question BankDocument43 paginiTest 6 Question Bankcannon butlerÎncă nu există evaluări
- Masseter HypertrophyDocument6 paginiMasseter Hypertrophysanchaita kohliÎncă nu există evaluări
- Assessment of 226Document35 paginiAssessment of 226ajay dalaiÎncă nu există evaluări
- Template HalodocDocument104 paginiTemplate HalodocSonia WulandariÎncă nu există evaluări
- Congenital HypothyroidismDocument36 paginiCongenital HypothyroidismRandi DwiyantoÎncă nu există evaluări
- Cervical Cancer - PreventionDocument10 paginiCervical Cancer - PreventionRae Monteroso LabradorÎncă nu există evaluări
- Neuromuscular Blocking DrugsDocument3 paginiNeuromuscular Blocking DrugsYogi drÎncă nu există evaluări
- Peran Perawat Dalam Penanggulangan Bencana: Vol 6, No 1 Mei, Pp. 63-70 P-ISSN 2549-4880, E-ISSN 2614-1310 WebsiteDocument8 paginiPeran Perawat Dalam Penanggulangan Bencana: Vol 6, No 1 Mei, Pp. 63-70 P-ISSN 2549-4880, E-ISSN 2614-1310 WebsiteEbato SanaeÎncă nu există evaluări
- 70000769rev.2ecube7 EngDocument599 pagini70000769rev.2ecube7 Engrizkiatul brawijayaÎncă nu există evaluări
- Tracheostomy CareDocument7 paginiTracheostomy CareJoanna MayÎncă nu există evaluări
- QUESTIONNAIREDocument3 paginiQUESTIONNAIREKatherine Aplacador100% (4)
- Prenatal RhogamDocument3 paginiPrenatal Rhogamgshastri7Încă nu există evaluări
- Case Report Acute Otitis MediaDocument28 paginiCase Report Acute Otitis Mediamayo djitro100% (2)
- + +Sandra+Carter +TMJ+No+More+PDF+ (Ebook) PDFDocument49 pagini+ +Sandra+Carter +TMJ+No+More+PDF+ (Ebook) PDFMassimiliano Marchionne0% (1)
- Charkoli ProjectDocument2 paginiCharkoli ProjectckbbbsrÎncă nu există evaluări
- Grade 3 Cot Filipino Pandiwa q4Document9 paginiGrade 3 Cot Filipino Pandiwa q4Maricar FaralaÎncă nu există evaluări
- Family Therapy For Autism Spectrum Disorders (Cto)Document21 paginiFamily Therapy For Autism Spectrum Disorders (Cto)Julie Rose AlboresÎncă nu există evaluări
- Atlas of Gastrointestinal Endoscopy and Related PathologyDocument2 paginiAtlas of Gastrointestinal Endoscopy and Related PathologyMaria PatituÎncă nu există evaluări
- Wellness Check PrintableDocument2 paginiWellness Check PrintablethubtendrolmaÎncă nu există evaluări
- The Obesity Code: Unlocking the Secrets of Weight LossDe la EverandThe Obesity Code: Unlocking the Secrets of Weight LossEvaluare: 4 din 5 stele4/5 (5)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDe la EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsÎncă nu există evaluări
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe la EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeEvaluare: 2 din 5 stele2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe la EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityEvaluare: 4 din 5 stele4/5 (24)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDe la EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDe la EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisEvaluare: 4.5 din 5 stele4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedEvaluare: 5 din 5 stele5/5 (80)