Documente Academic
Documente Profesional
Documente Cultură
Prognostic Value of Echocardiography in Peripartum.6
Încărcat de
Nefrida Namira MaarufDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Prognostic Value of Echocardiography in Peripartum.6
Încărcat de
Nefrida Namira MaarufDrepturi de autor:
Formate disponibile
Prognostic Value of Echocardiography in Peripartum
Cardiomyopathy
Jeff B. Chapa, MD, Heather B. Heiberger, MD, Lynn Weinert, RDCM, Jeanne DeCara, MD,
Roberto M. Lang, MD, and Judith U. Hibbard, MD
OBJECTIVE: To estimate whether echocardiography findings at the time of diagnosis of peripartum cardiomyopathy are predictive of persistent cardiac dysfunction.
METHODS: Chart review of patients with peripartum cardiomyopathy between 1988 and 2001 was performed. Data
from echocardiography, including fractional shortening
and left ventricular end diastolic dimension, were recorded
both at the time of diagnosis and at follow-up. Left ventricular dysfunction was defined by echocardiography as fractional shortening less than 30% and left ventricular end
diastolic dimension of 4.8 cm or more.
RESULTS: Of 32 patients meeting our definition for peripartum cardiomyopathy and for whom follow-up data were
available, 13 (41%) had recovery of ventricular function,
while 19 (59%) continued to have persistent left ventricular
dysfunction. Those who did not recover cardiac function
had a higher left ventricular end diastolic dimension and a
lower fractional shortening at diagnosis than those who
recovered. A fractional shortening value less than 20% and
a left ventricular end diastolic dimension 6 cm or greater at
the time of diagnosis was associated with a more than
3-fold higher risk for persistent left ventricular dysfunction.
CONCLUSION: Along with being an important diagnostic
tool in peripartum cardiomyopathy, echocardiography
may provide significant prognostic information with regards to recovery of cardiac function. (Obstet Gynecol
2005;105:1303 8. 2005 by The American College of
Obstetricians and Gynecologists.)
LEVEL OF EVIDENCE: III
Despite its original description in the medical literature
during the nineteenth century by Ritchie and Virchow,
peripartum cardiomyopathy remains a diagnosis associated
with great uncertainty.1 The incidence is estimated to be 1
in 3,000 4,000 deliveries in the United States, with 1,000
1,350 new cases reported annually,2,3 although tertiary
centers such as ours often report much higher incidences.4,5
Although a precise etiology for peripartum cardiomyopathy is unknown, there is much current interest in infectious,
From the Departments of Obstetrics and Gynecology and Internal Medicine,
University of Chicago, Pritzker School of Medicine, Chicago, Illinois.
VOL. 105, NO. 6, JUNE 2005
2005 by The American College of Obstetricians and Gynecologists.
Published by Lippincott Williams & Wilkins.
autoimmune, and genetic factors that may play a role in the
inciting event.6 Epidemiologic risk factors, well known to
the obstetrician, include age greater than 30 years, black
race, multiple gestation, obesity, preeclampsia, and chronic
hypertension.7 Peripartum cardiomyopathy historically
has had a 2550% mortality rate, a rate that may still persist
at some centers, with nearly one-half of all related deaths
occurring within the first 3 months after delivery.8 Despite
advances in medical therapy and the development of cardiac transplantation, the condition remains a significant
cause of maternal mortality, accounting for 6% of all maternal deaths among liveborn gestations in the United States.9
Recently, we described specific echocardiographic criteria to define the disorder,10 providing a more objective
definition than the traditional subjective parameters for
peripartum cardiomyopathy,11 because echocardiography is now the standard noninvasive tool for measuring
cardiac function, quantifying left ventricular performance and providing a definitive diagnosis of left ventricular dysfunction. Similar to idiopathic dilated cardiomyopathy, OConnell et al12 suggested that survivors of
peripartum cardiomyopathy have better echocardiographic ventricular function at the time of diagnosis
compared with those who succumb. Witlin et al,13 in a
series of only 9 patients, suggested that fractional shortening and end diastolic dimension at the time of diagnosis were prognostic. Although most patients with persistent cardiac dysfunction after the index pregnancy are
advised to avoid subsequent pregnancies, those parturients who experience prompt resolution of their symptoms and normalization of cardiac function may be more
problematic to counsel.
After recently reviewing and analyzing existing data,
the National Heart, Lung, and Blood Institute of the
National Institutes of Health concluded that uncertainty
regarding many aspects of peripartum cardiomyopathy
warrants further investigation and reporting of data.14
We have undertaken the current work to review our
own experience with peripartum cardiomyopathy and to
determine whether echocardiographic parameters at the
0029-7844/05/$30.00
doi:10.1097/01.AOG.0000161382.30233.ba
1303
time of diagnosis are predictive of outcome in our cohort
of patients. Furthermore, we wished to evaluate outcomes in those women undertaking a subsequent pregnancy after a diagnosis of peripartum cardiomyopathy.
MATERIALS AND METHODS
We performed an analysis of all patients with the diagnosis of peripartum cardiomyopathy who were cared for
at the University of Chicago from May 1988 to March
2001. Institutional review board approval was obtained
before beginning this investigation. Using International
Classification of Diseases, 9th Revision, discharge summary codes from cardiology outpatient clinics, echocardiographic laboratory records, and a computerized obstetric research database, we identified women with the
potential diagnosis of peripartum cardiomyopathy. The
inpatient and outpatient medical records of these patients, including echocardiographic data, were reviewed
to confirm the diagnosis. In each case, other potential
causes of heart failure in late gestation, including severe
preeclampsia, fluid overload, and amniotic fluid embolism, were determined not to be present. We used our
echocardiographic-based precise definition for peripartum cardiomyopathy, which requires a fractional shortening calculation of less than 30% and left ventricular
end diastolic dimension 4.8 cm or greater at the time of
diagnosis.10 Fractional shortening is defined as left ventricular end diastolic dimension minus left ventricular end
systolic dimension divided by left ventricular end diastolic dimension (LVEDD LVESD/LVEDD). Patients who did not meet these criteria were excluded
from our analysis.
Epidemiologic data, including age, race, and parity,
were recorded, as well as information on timing of
presentation in relation to gestation, presenting signs and
symptoms, risk factors, and subsequent pregnancy outcome. Patients were monitored with echocardiography
after delivery. Those who demonstrated either a return
of fractional shortening to more than 30% or left ventricular end diastolic dimension to less than 4.8 cm at the
time of follow-up were classified as recovered. Patients
who did not meet either of these criteria at follow-up
were classified as having persistent dysfunction. If available, data from long-term assessment of patients with left
ventricular dysfunction were collected, with particular
emphasis on outcomes such as need for transplantation
or patient death. For those who undertook a subsequent
pregnancy, the same criteria for follow-up were used.
Statistical analysis included comparison between patients with recovery of left ventricular function and those
with residual dysfunction using t tests for continuous
variables and Fisher exact test for categorical variables.
1304
Chapa et al
Echocardiography in Peripartum Cardiomyopathy
For left ventricular end diastolic dimension and fractional shortening results, the distribution of values for
both the recovered and persistent dysfunction subgroups
were assessed with the Lilliefors test for normality. Values for skewness and kurtosis were determined, and
there was little evidence found against a normal distribution for these results among either of the subgroups.
Relative risk (RR) and 95% confidence intervals for
recovery of left ventricular function were calculated, as
were P values for significance. We selected the values of
left ventricular end diastolic dimension greater than 6.0
cm and fractional shortening less than 20% at the time of
initial diagnosis as risk factors for persistent dysfunction
based on data from a previous study.13
RESULTS
During the study period, 40,200 live births occurred at
the University of Chicago. Of the 56 patients identified
as potentially suffering peripartum cardiomyopathy, 35
met our criteria for diagnosis and were included in this
investigation, corresponding to an incidence of 1 case per
1,149 live births. Three patients with peripartum cardiomyopathy were lost to follow-up. Twenty-one patients
who did not meet the criteria for this study were excluded. Preexisting disease, such as idiopathic dilated
cardiomyopathy or concurrent cardiovascular risk factors, including hypertension and alcoholism, were the
primary reasons for patient exclusion, as well as 6 cases
with insufficient data.
Eighty percent of study patients were African American, while the remainder were white, corresponding to
the overall obstetric population at our institution. The
mean age at the time of diagnosis of peripartum cardiomyopathy was 27 6 years, with a range of 16 38
years. Parity in the index pregnancy ranged from 1 to 6,
with a median value of 2. The diagnosis of peripartum
cardiomyopathy was made in the antepartum period in 7
gravidas and in the postpartum period in 28 women.
Included in our analysis are 2 patients who presented 2
and 3 months before delivery and one who presented at
7 months postpartum. Four women had multifetal gestations (3 twin, 1 triplet). Five gravidas had preeclampsia
and an additional five had been treated with tocolytics
for preterm labor with oral terbutaline for 6 56 days
(mean 24.5 days). The most common presenting symptoms and signs were dyspnea (90%), tachycardia (62%),
or peripheral edema (59%). One patient had a concomitant diagnosis of cerebral vascular accident. Only 2
women underwent endomyocardial biopsy, but neither
procedure was contributory to the diagnosis because one
revealed no abnormality and the other sample was insufficient for diagnostic purposes.
OBSTETRICS & GYNECOLOGY
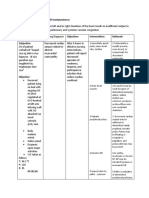
Table 1. Predisposing Factors and Echocardiographic Parameters at Diagnosis and Follow-up
Race
African-American
White
Parity
1
1
Age
30
30
Tocolytic use
Preeclampsia
Multiple gestation
At diagnosis
Fractional
shortening (%)
Left ventricular
end diastolic
diameter (cm)
At follow-up*
Fractional
shortening (%)
Left ventricular
end diastolic
dysfunction
(cm)
Recovered
(n 13)
Persistent
Dysfunction
(n 19)
11
2
14
5
.67
8
5
8
11
.47
7
6
2
1
2
7
12
2
4
2
.56
1.00
.62
1.00
22.48 4.82
13.96 6.24
.001
5.90 0.45
6.70 0.83
.003
32.9 2.6
18.8 6.0
5.64 0.82
6.33 0.79
Data presented as n or mean standard deviation.
* Median follow-up time 3 months.
At diagnosis, the mean fractional shortening of the
entire study group was 17.3 7.0%, with a mean left
ventricular end diastolic dimension of 6.4 0.8 cm. Of
the remaining 32 patients, 13 (41%) had recovered left
ventricular function at a median follow-up period of 3
months, while 19 (59%) had persistent ventricular dysfunction at a median of 46 months follow-up. Mean
fractional shortening and left ventricular end diastolic
dimension values, at the time of diagnosis and at followup, are presented for both of these groups in Table 1.
Fractional shortening and left ventricular end diastolic
dimension are significantly different between the group
that recovered left ventricular function and the group
with persistent ventricular dysfunction. An initial fractional shortening below a threshold value of 20% at the
time of diagnosis was associated with a 3-fold increased
risk of persistent left ventricular dysfunction at follow-up
(Table 2). Further, a left ventricular end diastolic dimension of 6.0 cm or greater at the time of the initial
diagnosis was associated with more than a 3.5 times
increased risk for persistent ventricular dysfunction compared with those who recovered (Table 2). With regard
to demographic characteristics and risk factors, there
were no significant differences between women whose
VOL. 105, NO. 6, JUNE 2005
Table 2. Risk for Persistent Left Ventricular Dysfunction
Based on Echocardiographic Parameters at Time
of Initial Diagnosis
Fractional shortening
20%
Left ventricular end
diastolic dimension
6.0 cm
Relative
Risk
95%
Confidence
Interval
3.06
1.317.16
.004
3.55
1.0212.33
.01
cardiac function improved and returned to normal and
those who remained with significant impairment (Table
1). Outcomes following the index pregnancy are presented in Figure 1. Two patients underwent cardiac
transplantation (6.5%), and 3 died from heart failure
(9.6%), including one of the transplant recipients.
Regarding outcomes with subsequent pregnancy after
the index pregnancy, 6 of 35 patients had 8 documented
subsequent gestations (Figure 2). Four of the patients
with recovered left ventricular function had one additional pregnancy each, while the 2 patients with persistent left ventricular dysfunction had 1 and 3 subsequent
pregnancies, respectively. All 4 patients with recovered
left ventricular function became symptomatic and demonstrated echocardiographic evidence of recurrent left
ventricular dysfunction in the third trimester. Three of
these gravidas with recurrence of peripartum cardiomyopathy then had persistent left ventricular dysfunction
after the subsequent pregnancy, while one again demonstrated full cardiac recovery. The 2 patients with persistent left ventricular dysfunction after the index pregnancy had no recurrence of symptoms in their
subsequent gestations, but continued to have stable left
ventricular dysfunction, both during and after the pregnancies (Figure 2).
DISCUSSION
Peripartum cardiomyopathy remains a significant cause
of maternal morbidity and mortality in the United States.
The increased incidence of peripartum cardiomyopathy at
our center is likely due in part to our role as a tertiary care
referral center for a large perinatal network, which serves
an urban, primarily African-American population.
Echocardiography is an important tool in properly
diagnosing peripartum cardiomyopathy and assessing
the degree of cardiac dysfunction. In this work we have
confirmed that the specific parameters of fractional shortening and left ventricular end diastolic dimension at the
time of diagnosis are predictive of the degree of recovery
Chapa et al
Echocardiography in Peripartum Cardiomyopathy
1305
Fig. 1. Left ventricular function
and outcome following index
pregnancy.
Chapa. Echocardiography in Peripartum
Cardiomyopathy. Obstet Gynecol 2005.
of cardiac function at follow-up. Those women with a
fractional shortening less than 20% or left ventricular
end diastolic diameter of 6.0 cm or greater on initial
echocardiogram incurred more than a 3 times increased
risk of not fully recovering their left ventricular function,
and in fact, 3 patients in this group suffered mortality. No
demographic risk factors differed between those women
who recovered and those who continued with ventricular impairment. The prognostic value of fractional shortening and left ventricular end diastolic dimension may
be beneficial in guiding treatment for and counseling
these patients.
Fig. 2. Outcomes in subsequent pregnancy based on left
ventricular function after index
gestation.
Chapa. Echocardiography in Peripartum
Cardiomyopathy. Obstet Gynecol 2005.
1306
Chapa et al
Echocardiography in Peripartum Cardiomyopathy
OBSTETRICS & GYNECOLOGY
Our findings are in accord with the observations of
OConnell et al12 who initially suggested that echocardiographic parameters, such as markedly reduced ejection fraction and increased left ventricular cavity size at
the time of diagnosis, are associated with increased maternal mortality. More recently, Witlin et al13 studied a
cohort of 9 peripartum cardiomyopathy patients and
noted that left ventricular end diastolic dimension of 6.0
cm or greater and fractional shortening of 21% or less
were risk factors for persistent left ventricular dysfunction. The results of this study confirm these findings in a
significantly larger cohort of peripartum cardiomyopathy patients. The morbidity in our patients, measured in
terms of persistent left ventricular dysfunction, is similar
to previous reports, but the mortality rate was lower than
that documented by other investigators.8,15,16 Advances
in cardiac critical care, the increasing availability of cardiac transplantation, and the exclusion of other cardiac
disease with echocardiography are likely causes of the
improvement in overall mortality figures.
Women with a history of peripartum cardiomyopathy
remain at high risk for recurrence of cardiac dysfunction
in subsequent pregnancies, despite seemingly full recovery. Our data, although limited by the small number of
patients embarking on a new conception, suggest that
recovery of left ventricular function after the index gestation, as documented by echocardiography, is not predictive of recurrence or outcome in subsequent pregnancies in our population. We were surprised that all 4 of the
completely recovered women had recurrent left ventricular dysfunction during pregnancy. Sutton et al17 and
DeSouza et al18 describe much better success with subsequent pregnancy in their recovered peripartum cardiomyopathy patients compared with our cohort, although
each report includes only 4 and 7 patients, respectively.
In contrast, Elkayam et al,19 in the largest series to date,
have documented significant deleterious effects of subsequent pregnancies in women with a history of peripartum cardiomyopathy who have echocardiographic evidence of residual dysfunction.
Perhaps additional factors are better indicative of the
hearts ability to compensate for the increased hemodynamic demands of a subsequent pregnancy. Lampert et
al20 demonstrated that patients diagnosed with peripartum cardiomyopathy and completely recovered left ventricular function actually had evidence of decreased left
ventricular contractile reserve, as demonstrated by a
dobutamine challenge test, suggesting that these women
may indeed be at risk for recurrence of disease in future
pregnancies. Because peripartum cardiomyopathy is associated with multiparity, it may be that each subsequent
pregnancy in susceptible individuals further compromises contractile reserve and is more likely to lead to
VOL. 105, NO. 6, JUNE 2005
persistent cardiac dysfunction. Still, a number of other
factors, as yet undefined, including genetic and autoimmune, may underlie and contribute to outcomes in these
women. Surprisingly, in our experience the gestations
that occurred in women with residual cardiac dysfunction after the index pregnancy were uncomplicated and
not marked by a significant worsening of symptoms or
cardiac function. These cases, however, are only 2 in
number, and both patients were receiving ongoing care
and maintained on appropriate medications. Thus, we
caution strongly against the extrapolation of this limited
data to other similar cases.
Improved outcomes in index cases of peripartum cardiomyopathy and in subsequent pregnancies are primarily due to advances in cardiac care, both medical and
surgical. Pharmacologic therapy for heart failure has
evolved tremendously and is now based on sound therapeutic principles that include afterload reduction and
increasing myocardial contractility. The former can be
attained effectively during gestation with careful use of a
potent vasodilator, such as hydralazine, whereas the
latter aim may be achieved with digoxin and other
pressor agents. Angiotensin-converting enzyme inhibitors are also an excellent choice in the postpartum setting
for afterload reduction, but these drugs can lead to
embryopathy when used during pregnancy. Fluid restriction and judicious use of diuretics may also alleviate
some of the symptoms associated with congestive heart
failure in the gravida. Finally, improvements in cardiac
critical care and the emergence of cardiac transplantation
have provided hope to patients who previously would
not have survived.
We have chosen to include 3 patients in our cohort
whose timing of disease is outside the previously suggested time period for diagnosis.11 These women met all
the stringent echocardiographic criteria, as well as all
subjective criteria, with the exception of timing. We
believe the time element is no longer relevant, and in
view of current diagnostic tools, medications, and cardiac intensive care, a diagnosis of peripartum cardiomyopathy antenatally does not automatically imply immediate delivery, particularly if the fetus is quite premature.
Thus, a gravida diagnosed with peripartum cardiomyopathy in the second or third trimester, more than 1
month before delivery, may indeed carry the gestation
much closer to term, allowing for improved fetal maturity. Similarly, the patient diagnosed with cardiomyopathy 7 months after delivery may have had echocardiographic evidence of cardiac dysfunction long before her
presentation. Thus, we believe that timing relative to
gestation may be a somewhat arbitrary consideration,
and inclusion of gravidas who otherwise meet all diagnostic criteria is warranted.
Chapa et al
Echocardiography in Peripartum Cardiomyopathy
1307
We acknowledge that because of the small sample
sizes in this study, which is due to the rarity of this
disease, some of our observations may have limited
statistical power. Additionally, the cases occurred over a
13-year time period, during which significant advances
in cardiac care have been made. Thus, the prognosis and
outcome for patients who presented in the more recent
past would be expected to be improved over those
patients presenting earlier. However, further subanalysis
of the data, according to year of diagnosis during the
study period, was not able to be performed because of
the small sample sizes. These limitations emphasize the
need for larger, prospective multicenter studies.
Echocardiography appears to be extremely valuable
in diagnosing peripartum cardiomyopathy, formulating
prognosis for recovery, and following the course of the
disease. Specific echocardiographic parameters, including fractional shortening and left ventricular end diastolic dimension at the time of diagnosis, may be predictive of long-term cardiac dysfunction. Subsequent
pregnancy in women who have been diagnosed with
peripartum cardiomyopathy should be approached with
extreme caution. Because our understanding of the underlying etiology and natural history of peripartum cardiomyopathy is currently incomplete, management of
these patients can prove to be difficult. We believe an
international registry of cases would greatly aid progress
in unraveling the complexities of this disease.
REFERENCES
1. Veille JC. Peripartum cardiomyopathies: a review. Am J
Obstet Gynecol 1984;148:80518.
2. Ventura SJ, Peters KD, Martin JA, Maurer JD. Births and
deaths: United States, 1996. Monthly vital statistics report;
Vol. 46, no. 1, suppl 2. Hyattsville (MD): National Center
for Health Statistics; 1997.
3. Guyer B, Strobino DM, Ventura SJ, Singh GK. Annual
summary of vital statistics1994. Pediatrics 1995;96:
1029 39.
4. Desai D, Moodley J, Naidoo D. Peripartum cardiomyopathy: experiences at King Edward VIII Hospital, Durban,
South Africa and a review of the literature. Trop Doct
1995;25:118 23.
5. Fett JD, Carraway RD, Dowell DL, King ME, Pierre R.
Peripartum cardiomyopathy in the Hospital Albert
Schweitzer District of Haiti. Am J Obstet Gynecol 2002;
186:100510.
6. Brown CS, Bertolet BD. Peripartum cardiomyopathy: a
comprehensive review. Am J Obstet Gynecol 1998;178:
409 14.
7. Heider AL, Kuller JA, Strauss RA, Wells SR. Peripartum
cardiomyopathy: a review of the literature. Obstet
Gynecol Surv 1999;54:526 31.
1308
Chapa et al
Echocardiography in Peripartum Cardiomyopathy
8. Demakis JG, Rahimtoola SH, Sutton GC, Meadows WR,
Szanto PB, Tobin JR, et al. Natural course of peripartum
cardiomyopathy. Circulation 1971;44:1053 61.
9. Koonin LM, MacKay AP, Berg CJ, Atrash HK, Smith JC.
Pregnancy-related mortality surveillanceUnited States,
19871990. MMWR CDC Surveill Summ 1997;46:1736.
10. Hibbard JU, Lindheimer M, Lang RM. A modified definition for peripartum cardiomyopathy and prognosis based
on echocardiography. Obstet Gynecol 1999;94:31116.
11. Demakis JG, Rahimtoola SH. Peripartum cardiomyopathy. Circulation 1971;44:964 8.
12. OConnell JB, Costanzo-Nordin MR, Subramanian R,
Robinson JA, Wallis DE, Scanlon PJ, et al. Peripartum
cardiomyopathy: clinical, hemodynamic, histologic and
prognostic characteristics. J Am Coll Cardiol 1986;8:52 6.
13. Witlin AG, Mabie WC, Sibai BM. Peripartum cardiomyopathy: a longitudinal echocardiographic study. Am J
Obstet Gynecol 1997;177:1129 32.
14. Pearson GD, Veille JC, Rahimtoola S, Hsia J, Oakley C,
Hosenpud JD, et al. Peripartum cardiomyopathy:
National Heart, Lung, and Blood Institute and Office of
Rare Diseases (National Institutes of Health) workshop
recommendations and review. JAMA 2000;283:1183 8.
15. Witlin AG, Mabie WC, Sibai BM. Peripartum cardiomyopathy: an ominous diagnosis. Am J Obstet Gynecol 1997;
176:182 8.
16. Costanzo-Nordin MR, OConnell JB. Peripartum cardiomyopathy in the 1980s: etiologic and prognostic consideration and review of the literature. Prog Cardiol 1989;2:
22539.
17. Sutton MS, Cole P, Plappert M, Saltzman D, Goldhaber S.
Effects of subsequent pregnancy on left ventricular function in
peripartum cardiomyopathy. Am Heart J 1991;121:17768.
18. de Souza JL Jr, de Carvalho Frimm C, Nastari L, Mady C.
Left ventricular function after a new pregnancy in patients
with peripartum cardiomyopathy. J Card Fail 2001;7:30 5.
19. Elkayam U, Tummala PP, Rao K, Akhter MW, Karaalp
IS, Wani OR, et al. Maternal and fetal outcomes of subsequent pregnancies in women with peripartum cardiomyopathy. N Engl J Med 2001;344:156771.
20. Lampert M, Weinert L, Hibbard J, Korcarz C, Lindheimer
M, Lang RM. Contractile reserve in patients with peripartum cardiomyopathy and recovered left ventricular function. Am J Obstet Gynecol 1997;176:189 95.
Address reprint requests to: Jeff B. Chapa, MD, Department of
Obstetrics and Gynecology, Section of MaternalFetal Medicine, University Hospitals of Cleveland, MacDonald Womens Hospital, 11100 Euclid Avenue, Cleveland, OH 44106;
e-mail: jeff.chapa@uhhs.com.
Received September 14, 2004. Received in revised form February 1,
2005. Accepted February 10, 2005.
OBSTETRICS & GYNECOLOGY
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Cleveland Clinic Cardiology Board ReviewDocument114 paginiThe Cleveland Clinic Cardiology Board ReviewSohil Elfar100% (1)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Internal MedicineDocument167 paginiInternal MedicineJason Steel86% (7)
- New York Heart Association (NYHA) Functional Classification in A Patient With Heart DiseaseDocument2 paginiNew York Heart Association (NYHA) Functional Classification in A Patient With Heart Diseasemanikchopra111Încă nu există evaluări
- Aortic Coarctation Cardiology Clinics 2020Document15 paginiAortic Coarctation Cardiology Clinics 2020Angela OrozcoÎncă nu există evaluări
- MSF Clinical Guidelines PDFDocument356 paginiMSF Clinical Guidelines PDFKirthinath BallalÎncă nu există evaluări
- Step by Step EchocardiographyDocument141 paginiStep by Step EchocardiographyMonica Surdu83% (6)
- Tata Laksana Perawatan Gigi Pada Pasien Kelainan Jantung Yang Ditanamkan Icd Dan Mengonsumsi WarfarinDocument17 paginiTata Laksana Perawatan Gigi Pada Pasien Kelainan Jantung Yang Ditanamkan Icd Dan Mengonsumsi WarfarinEka ApriantiÎncă nu există evaluări
- SemaglitidDocument5 paginiSemaglitidNguyên PhươngÎncă nu există evaluări
- CHF NCPDocument8 paginiCHF NCPZy Hallasgo100% (1)
- Presentation Chapter 27 Pulmonary Embolism and ARDS CaseDocument91 paginiPresentation Chapter 27 Pulmonary Embolism and ARDS Caseavoyiad100% (1)
- Innovation in Health Care Delivery: Jonathan Wilt AVP, Center For Innovation Ochsner Health SystemDocument47 paginiInnovation in Health Care Delivery: Jonathan Wilt AVP, Center For Innovation Ochsner Health SystemMedika UtamaÎncă nu există evaluări
- Drug StudyDocument4 paginiDrug StudyTeanu Jose Gabrillo TamayoÎncă nu există evaluări
- HerzinsuffizienzDocument10 paginiHerzinsuffizienzMagdalena PokusaÎncă nu există evaluări
- 2018 Krok2Document10 pagini2018 Krok2mohamed esamÎncă nu există evaluări
- Aegon Life Ci Care Rider: A Non Linked Critical Illness RiderDocument13 paginiAegon Life Ci Care Rider: A Non Linked Critical Illness Riderfaizahamed111Încă nu există evaluări
- HSE705 Cardiopulmonary Weekly Schedule 2015 1Document4 paginiHSE705 Cardiopulmonary Weekly Schedule 2015 1Ayden ShawÎncă nu există evaluări
- Elective II FinalsDocument15 paginiElective II FinalsAljon Dofeliz LlamasÎncă nu există evaluări
- Cardiovascular SystemDocument8 paginiCardiovascular SystemDawnmurph Dharlene Wag-eÎncă nu există evaluări
- Criterios Beers 2019Document8 paginiCriterios Beers 2019Viki BernalÎncă nu există evaluări
- Drugs To Watch: A Clarivate ReportDocument25 paginiDrugs To Watch: A Clarivate ReportjeetÎncă nu există evaluări
- Endokarditis, Miokarditis Perikarditis: Blok KardiovaskularDocument31 paginiEndokarditis, Miokarditis Perikarditis: Blok KardiovaskularTiara RamliÎncă nu există evaluări
- Acute Exacerbation of COPD Nursing Application of Evidence-Based GuidelinesDocument17 paginiAcute Exacerbation of COPD Nursing Application of Evidence-Based GuidelinesCandice ChengÎncă nu există evaluări
- Hipertensión Pulmonar (2022)Document114 paginiHipertensión Pulmonar (2022)Mauricio CabreraÎncă nu există evaluări
- 2003 World Health Organization (WHO) /international Society of Hypertension (ISH) Statement On Management of HypertensionDocument10 pagini2003 World Health Organization (WHO) /international Society of Hypertension (ISH) Statement On Management of HypertensionGhina NisrinaÎncă nu există evaluări
- Common Terminology Criteria For Adverse Events Following Chemotherapy or Biological Antineoplastic Therapy in Dogs and Cats. VCOG. 2011Document30 paginiCommon Terminology Criteria For Adverse Events Following Chemotherapy or Biological Antineoplastic Therapy in Dogs and Cats. VCOG. 2011Mario GonzálezÎncă nu există evaluări
- El Tratamiento de La Insuficiencia Mitral Secundaria en Pacientes Con Insuficiencia Cardíaca PDFDocument16 paginiEl Tratamiento de La Insuficiencia Mitral Secundaria en Pacientes Con Insuficiencia Cardíaca PDFmarlenjyÎncă nu există evaluări
- Epilat RetardDocument2 paginiEpilat RetardmahgadÎncă nu există evaluări
- الاختصارات الطبية PDFDocument37 paginiالاختصارات الطبية PDFdede jdjÎncă nu există evaluări
- Cardiomyopathy: Dr. Ibrahim AbuasbehDocument39 paginiCardiomyopathy: Dr. Ibrahim Abuasbehأبوأحمد الحكيمÎncă nu există evaluări
- P1 MS 3 Nur 200Document16 paginiP1 MS 3 Nur 200Xandra Joie Ondoy TabotaboÎncă nu există evaluări