Documente Academic
Documente Profesional
Documente Cultură
Bone-Marrow Relapse in Paediatric Acute Lympho-Blastic Leukaemia
Încărcat de
hawinnurdianaTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Bone-Marrow Relapse in Paediatric Acute Lympho-Blastic Leukaemia
Încărcat de
hawinnurdianaDrepturi de autor:
Formate disponibile
Review
Bone-marrow relapse in paediatric acute lymphoblastic
leukaemia
L Charles Bailey*, Beverly J Lange*, Susan R Rheingold, Nancy J Bunin
Marrow relapse is the major obstacle to cure for 1015% of young patients with acute lymphoblastic leukaemia (ALL).
Recent investigations into the biology of minimal residual disease indicate that many early relapses derive from residual
cells present at rst diagnosis, but some late relapses might represent new mutations in leukaemic cells not eliminated
by conventional therapy. Treatment of marrow relapse involves higher doses and more intensive schedules of the drugs
used for initial therapy with or without haemopoietic stem cell transplantation. In most reports, transplantation is better
than continuation chemotherapy in early marrow relapse, but its role in later relapse is less clear. Current therapy cures
10% of patients with early marrow relapses and 50% of those with late relapses, but outcomes have changed little in the
past two decades. Understanding the molecular biology of ALL underlies development of improved risk stratication and
new therapies. Although better drugs are needed, introduction of new agents into clinical trials in paediatric disease has
been dicult. Innovative trial designs and use of valid surrogate endpoints may expedite this process.
Introduction
50 years of large randomised clinical trials of combination
chemotherapy and CNS prophylaxis have improved the
cure rate for acute lymphoblastic leukaemia (ALL) in
childhood from less than 5% in 1950 to 85% in 2000.1
Progress in this disease has come principally from prevention of relapses (gure 1) through more eective use of
established drugs and combination regimens in riskadapted treatment strategies, rather than introduction of
new drugs. Today few recurrences occur solely in the CNS
or other extramedullary sites,27 and most are curable,
especially those that happen well after initial treatment.811
Marrow relapse is the major impediment to cure (gure 2);
assuming a recurrence rate of 1015%, roughly
1000 patients each year relapse in Europe and North
America.12 Treatment of marrow relapse has not been as
successful as primary treatment despite intensied chemotherapy and use of haemopoietic stem cell transplantation,
and better therapeutic options are needed.
We describe recent advances in the understanding of
marrow relapse and past, present, and future approaches
to treatment. Molecular techniques provide insight into
the pathogenesis of relapse and support a targeted
approach to drug discovery that has produced new classes
of drugs with promising preclinical activity in lymphoid
malignancies.13 The logistics of introducing them into
paediatric clinical trials and proving their ecacy in
marrow relapse are daunting. Innovative trial designs and
use of surrogate endpoints could facilitate this process.1416
By use of the 3-[4,5-dimethyl-thiazole-2,5-diphenyl] tetrazolium bromide (MTT) cytotoxicity assay, both casecontrol
and matched-set comparisons of initial and relapse
samples showed that relapse samples are more resistant to
glucocorticoids, L-asparaginase, thiopurines, and anthracyclines in vitrothese drugs are central components of
initial treatment. However, the samples retain sensitivity
to etoposide and cyclophosphamide, which are sparingly
used in rst-line protocols.18 This nding suggests that
patients might benet after relapse from dierent drugs or
dosing strategies but does not distinguish between
acquired and inherent drug resistance in leukaemic
blasts.
Early studies of matched initial and relapse specimens
also found shifts in morphology and in chromosome
number in a third and changes in lineage-related surface
antigens in a half of patients;19 conversion to a new lineage
with a distinct karyotype was rare and usually indicated a
new, treatment-related leukaemia.19 Developments in
multichannel ow cytometry allow phenotypic detection of
fewer than one leukaemic blast among 1000 normal cells,
making it possible to quantify minimal residual disease
(table 1).20 Comparison of matched initial and relapse
specimens from patients with B-precursor ALL showed
A
Lancet Oncol 2008; 9: 87383
*These authors contributed
equally
Division of Oncology, Childrens
Hospital of Philadelphia, and
University of Pennsylvania
School of Medicine,
Philadelphia, PA, USA
(L C Bailey MD, Prof B J Lange MD,
S R Rheingold MD,
Prof N J Bunin MD)
Correspondence to:
Dr L Charles Bailey, Division of
Oncology, Childrens Hospital of
Philadelphia, 1 Childrens Center,
Philadelphia, PA 19104, USA
baileyc@email.chop.edu
Origins of relapse
Much of our knowledge about the pathogenesis of relapse
comes from casecontrol and matched-set studies of leukaemic cells at initial diagnosis, at relapse, and during
clinical remission. Casecontrol studies access large numbers of banked specimens, but relapse and control specimens commonly come from dierent individuals with
dierent types of ALL. Matched sets of samples from one
individual control for these variables, but are dicult to
assemble.17
www.thelancet.com/oncology Vol 9 September 2008
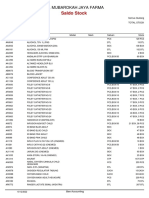
Figure 1: Marrow inltration by lymphoblasts
Lymphoblast morphology at initial diagnosis (A) and relapse (B) in a child with acute lymphoblastic leukaemia.
Stain=Wright-Giemsa.
873
Review
5 year event-free survival
Extramedullary relapse
Other
Marrow relapse
Outcome (% of all patients)
100
75
50
25
0
BFM
198195
CCG
198395
DFCI
198195
Tokyo CCSG
198195
UKMRC
198097
Figure 2: Trends in outcomes for primary treatment of paediatric acute lymphoblastic leukaemia
Results from large cooperative group trials show that marrow relapse remains the largest barrier to cure despite
improvements in overall outcome. Non-relapse outcomes not reported by US Childrens Cancer Group (CCG) or
Tokyo Childrens Cancer Study Group (Tokyo CCSG)marrow relapse estimated as event-free survival minus CNS
extramedullary relapse in CCG and minus all extramedullary relapse in Tokyo CCSG. BFM=Berlin-Frankfurt-Mnster
group. DFCI=Dana-Farber Cancer Institute. UKMRC=UK Medical Research Council (Childhood Leukaemia Working
Party). Each column represents outcomes for a specic trial or set of closely related trials.
Sensitivity
Limitation
Morphology
15%
Sensitivity; distinction between normal and
leukaemic blasts
Multiparameter ow cytometry
00101%
Marker selection; antigen shifts in leukaemic clone
RT-PCR
000010001%
Requires patient-specic probes at diagnosis;
genotypic shifts; false positives
Table 1: Development of methods for measurement of minimal residual disease
phenotypic shifts in 69%.21 Minimal residual disease
detected at the end of induction is phenotypically more
similar to the initial specimen than to the relapse
specimen.
The combination of assessment for minimal residual
disease and molecular genetic analysis provides evidence
that helps determine the cellular origins of relapse.
Southern blotting of genomic DNA shows that each case
of ALL has unique rearrangements of immunoglobulin or
T-cell receptor genes.22 PCR amplication, cloning, and
sequencing of these rearrangements generates probes to
investigate the genotypic composition of initial, minimalresidual-disease, and relapse specimens.23 About half of
initial samples have two or more immunoglobulin and
T-cell-receptor genotypes derived from a common clone.24
Matched pairs commonly have immunoglobulin and
T-cell-receptor genotypic shifts thought to reect normal
recombination events during lymphoid dierentiation.
Retrospective comparison of gene sequences from
specimens at diagnosis, remission, and relapse reveal that
the relapsing clone is present in the initial specimen, often
beneath the level of detection without a specic molecular
probe.2426 After induction, this clone persists in greater
copy numbers than others, probably indicating its
874
resistance to induction therapy.24,27 Although the relapsing
clone typically becomes undetectable after postinduction
therapy, it eventually reappears as minimal residual disease
and subsequently recurrence. Hence, early relapse
probably results from selection of a relatively resistant
clone present at initial diagnosis rather than generation of
a new clone by mutation (gure 3).
By contrast, late relapses may represent de novo
development of a second leukaemia from a common
premalignant clone. Studies of cord blood have established
that the ETV6RUNX1 (TELAML1) translocation occurs
in utero, but is not sucient to cause leukaemia. A second
mutation, most often a deletion of the normal ETV6 allele,
is required for leukaemogenesis.28 Each patients unique
translocation breakpoint sequence is a marker for the
preleukaemic clone that develops into acute lymphoblastic
leukaemia. Comparisons of matched initial and relapse
specimens document identical ETV6RUNX1 breakpoint
sequences and typical shifts in immunoglobulin and T-cellreceptor rearrangements, but dierent mutations in the
unrearranged ETV6 allele.28 Therefore, two separate
episodes of leukaemia must have arisen from metachronous
independent mutations in a common ETV6RUNX1
preleukaemic cell. Perhaps this explains why the second
leukaemia is commonly cured by therapy similar to that
used to treat initial disease (gure 3).28 Because the
mutations that characterise the preleukaemic clone are not
identied in most patients with ALL lacking the ETV6
RUNX1 translocation, distinguishing between evolution of
the initial leukaemic clone and new mutation in a distinct
population of preleukaemic cells is not yet possible.
Exploratory studies with whole-genome expression
proling of matched initial and relapse samples reveal
dierential expression of genes involved in cell
proliferation, cell-cycle regulation, transcription, DNA
repair, and apoptosis.17,29,30 Early relapse and late relapse
manifest distinct patterns of dierential expression.17,30
Casecontrol comparisons of independent samples
conrm changes to genes involved in proliferation, but
identication of the same genes in two studies is
uncommon.17,29 Genomic analysis of minimal residual
disease shows that changed expression of genes involved
in proliferation correlates with relapse; however, both
underexpression and overexpression of genes has been
described in relapse specimens.17,31 Most available cytotoxic
drugs target dividing cells, but some current models
implicate non-proliferating cells in resistance to conventional therapy.31
An unexpected nding of whole-genome studies is that
proles of blasts from relapsed acute lymphoblastic
leukaemia do not underexpress or overexpress genes
recognised in pharmacological and pharmacogenetic
analyses as classic mediators of drug metabolism and
resistance.17,32 Whole genome studies have great potential,
but consistent patterns have not yet emerged; improved
reproducibility and reconciliation across independent
datasets are needed.
www.thelancet.com/oncology Vol 9 September 2008
Review
Risk stratication of relapsed ALL
Site of relapse and duration of rst remission are crucial
predictors of second remission, event-free survival, and
overall survival after relapse.9,3336 Marrow relapses occurring
less than 1824 months into rst remission correlate with
poor survival, while relapses after 36 months of rst
remission have a much higher chance of cure (table 2).8,9,3744
Dierences in pathogenesis of early and late relapse might
partly explain the prognostic signicance of rst remission
duration in patients who relapse.
Historically, isolated marrow relapse has had the worst
prognosis; isolated CNS, testicular, or other extramedullary
relapse carried a signicantly better prognosis, and
combined marrow and extramedullary relapse, an
intermediate prognosis.8,33,41,43,44 Greater cure rates for
combined relapse compared with isolated marrow relapse
might reect dierences in disease biology, but might also
result from therapeutic craniospinal irradiation.41,43
A recent report challenged the current criteria for isolated
extramedullary relapse by nding PCR-detectable marrow
disease in most cases morphologically classied as isolated
extramedullary relapse.45 The risk of clinical relapse was
proportional to the amount of submicroscopic disease,
making marrow relapse a quantitative rather than a
qualitative phenomenon.
The Childrens Oncology Group and Berlin-FrankfurtMnster group have developed formal criteria for risk
stratication for relapsed ALL with the main intent of
identifying children for whom haemopoietic stem cell
transplantation might be better than continuation
chemotherapy once a second remission is attained
(table 3).33,35 The two systems are quite similar, but do have
some signicant dierences. For example, the BerlinFrankfurt-Mnster group distinguishes between marrow
relapses of less than 18 months from rst remission and
those at more than 18 months from remission but less
than 6 months o therapy, whereas the Childrens
Oncology Group does not further subdivide high-risk
relapses with rst remission at less than 36 months. The
Berlin-Frankfurt-Mnster group also classies T-cell
relapses as higher risk than their B-lineage counterparts
while the Childrens Oncology Group does not separate
T-cell from B-cell lineages at relapse, although T-cell
immunophenotype was found to be unfavourable in
Childrens Cancer Group and Pediatric Oncology Group
retrospective reviews of relapse.9,46 Other adverse risk
factors not captured in either system are initial high-risk
therapy,47,48 MLL rearrangement in infants or BCRABL
translocation,33,35 and, in many studies, male sex.41,44,47,48
Minimal residual disease at the end of reinduction also
correlates with outcome after second remission.49,50 Other
prognostic factors at initial diagnosis, such as age and
leucocyte count, do not consistently predict outcome at
relapse. Ongoing trials are changing the populations for
whom haemopoietic stem cell transplantation is the
treatment of choice, leading current practice to develop
beyond these classication guidelines.
www.thelancet.com/oncology Vol 9 September 2008
Mutation
Initiating
Transforming
Transforming
Treatment resistance
Normal lymphoid
progenitor cell
Pre-leukaemic
clones
Resistance emerges:
MRD persists
Acute leukaemia
Therapy
Selection
No resisitance:
leukaemia cured
Acute leukaemia
Mutation
Early relapse
Therapy
Late relapse
Second
mutation
Figure 3: Potential mechanisms of clinical relapse
Top: early recurrence may arise due to selection of resistant leukaemic cells during rst-line therapy. Bottom: late
relapse may represent a second, independent transforming event in an underlying preleukaemic clone.
Treatment of marrow relapse
Reinduction therapy after marrow relapse
Typical treatment of rst relapse involves a combination
of vincristine, a glucocorticoid (prednisone, prednisolone,
or dexamethasone), and asparaginase, plus an anthracycline, methotrexate, or cytarabine in varying doses and
schedules. Only a few randomised trials have investigated
reinduction therapy.5153 Most inuential is a Pediatric
Oncology Group study that showed signicantly higher
reinduction rates with weekly rather than biweekly
pegaspargase (97% vs 82%), leading to near universal
adoption of the weekly schedule.51 The Pediatric Oncology
Group compared vindesine to vincristine as the reinduction vinca alkaloid. Outcomes were similar, but
vindesine was more toxic and was abandoned in the USA53
though not in Berlin-Frankfurt-Mnster group trials.43
Over a series of trials, the Berlin-Frankfurt-Mnster group
randomised dose and duration of infusional methotrexate
in reinduction and thereafter. The group found no
dierence in reinduction rate or long-term outcome
between intermediate-dose (1 g/m over 36 h) and highdose (5 g/m over 24 h) infusions, and have adopted the
former for future trials.41,43
Institutional protocols from Philadelphia and Seattle use
idarubicin (30 mg/m total dose) as part of a four-drug
reinduction with apparent success11,54 and a trial by the
Italian Paediatric Haematology Oncology Association
(AIEOP) showed ecacy in combination with high-dose
cytarabine.55 However, the Childrens Cancer Group
randomised two doses of idarubicin (30 mg/m or
375 mg/m total dose) to daunorubicin (135 mg/m total
dose) but could not prove superiority of idarubicin,52
ndings consistent with the predictions of the MTT assay.18
The UK uses epirubicin, but most other groups now use
doxorubicin or daunorubicin.38,44,51
At St Jude Childrens Research Hospital (Memphis,
TN, USA), randomised dosing of etoposide once or twice
daily on a three-drug reinduction backbone showed no
dierences in area under the doseconcentration curve;
higher area under the curve was associated with
875
Review
remission.56 Etoposide and ifosfamide have shown
activity in marrow relapse.57 Childrens Cancer Group
study 1941 introduced etoposide and ifosfamide in
induction but reported no improvement in rates of
second remission or cure.58 Other drugs active in solid
tumours have minimum activity in relapsed ALL.
Combinations of idarubicin, udarabine, and cytarabine
have shown ecacy in studies of recurrent leukaemia in
adults59 and mixed paediatric and adult populations, but
measurement of the contributions of the two newer
drugs in mixed studies is dicult.
Across multiple studies, second remission is achieved in
more than 70% of early relapses and up to 96% of late
relapses (table 2).11,36,38,39,41,44,51,52,54,55 In the absence of
randomised trials and consistent risk-stratied reporting
of patient outcomes, whether any reinduction combination
Study period N
Early
in use today is signicantly superior to the others is
unclear.
Postremission therapy
Continuation chemotherapy
All patients who reach a second remission receive
additional chemotherapy, even if haemopoietic stem cell
transplantation is planned. To maintain control of
disease, higher dose intensity is used, and higher
regimen-related toxicity is tolerated than in rst-line
treatment. Most reports describe single-arm studies with
combinations of vincristine, glucocorticoids, methotrexate, cytarabine, etoposide, cyclophosphamide or
ifosfamide, and thiopurines, with or without maintenance
therapy for up to 2 years.36,39,41,43,44,52,54,55 CNS prophylaxis
includes high-dose methotrexate or cytarabine, intrathecal
Complete remission
Event-free survival
Overall survival
Early
Late
Earliest
Earliest
Early
Late
Early
References
Late
Great Ormond Street Hospital*
19722001
350
72%
76%
96%
6%
32%
71%
Nordic Paediatric Haematology-Oncology group
198194
216
72%
8%
19%
50%
37
8
Paediatric Oncology Group
198386
297
100%
83%
9%
12%
38
Childrens Cancer Group
198389
642
66%
5%
10%
33%
11%
43%
St Jude Childrens Research Hospital
198494
106
40%
66%
81%
13%
43%
39
Kyushu-Yamaguchi Childrens Cancer Study Group
198496
117
72%
16%
24%
35%
40
Berlin-Frankfurt-Mnster study group
198790
183
48%
73%
96%
18%
44%
20%
52%
41
United Kingdom Medical Research Council Working Party on
Childhood Leukaemia
198990
489
47%
1%
14%
33%
42
Berlin-Frankfurt-Mnster study group
199095
269
42%
91%
..
21%
48%
29%
26%
43
United Kingdom Medical Research Council Working Party on
Childhood Leukaemia
199095
121
35%
5%
35%
51%
44
Earliest relapses are less than 1824 months from rst remission, early relapses include these, as well as late relapses under 6 months from therapy discontinuation, and late relapses occurred after this time.
*Includes all relapses. Includes combined relapses. Excludes T-cell ALL relapses, and includes all combined relapses, intermediate-risk marrow relapses, and high-risk extramedullary relapses.
Table 2: Studies of outcomes after marrow relapse according to duration of rst remission
Marrow
Combined
Extramedullary
Very early
Early
Late
Very early
Early
Late
Early
Late
First remission duration
<18 months
18 months and
<6 months o
treatment
6 months o
treatment
<18 months
18 months and
<6 months o
treatment
6 months o
treatment
On treatment or
<6 months o
treatment
6 months o
treatment
B-precursor risk
High
High
Intermediate
High
Intermediate
Intermediate
Intermediate
Standard
B-precursor therapy
Allogeneic
HSCT
Allogeneic HSCT
MFD HSCT
Allogeneic
HSCT
MFD HSCT,
radiotherapy
Chemotherapy,
radiotherapy
Chemotherapy,
radiotherapy
Chemotherapy,
radiotherapy
T-cell risk
High
High
High
High
High
High
Intermediate
Standard
T-cell therapy
Allogeneic
HSCT
Allogeneic HSCT
Allogeneic
HSCT
Allogeneic
HSCT
Allogeneic HSCT,
radiotherapy
Allgeneic HSCT,
radiotherapy
Chemotherapy,
radiotherapy
Chemotherapy,
radiotherapy
First remission duration
<36 months
36 months
<36 months
36 months
<18 months
18 months
T-cell and B-cell precursor risk
High
Intermediate
High
Intermediate
Intermediate
Low
T-cell and B-cell precursor
therapy
Allogeneic HSCT
MFD HSCT
Allogeneic HSCT,
radiotherapy
MFD HSCT,
radiotherapy
MFD HSCT,
radiotherapy
Chemotherapy,
radiotherapy
Berlin-Frankfurt-Mnster
Childrens Oncology Group*
Allogeneic haemopoietic stem cell transplantation (HSCT) is transplantation of cells from any of matched familial donors (MFD), unrelated donors, or cord blood. *The Childrens Oncology Group had no very
early group. Time since diagnosis used in current studies as proxy for duration of rst remission.
Table 3: Risk stratication and treatment strategy for relapsed acute lymphoblastic leukaemia
876
www.thelancet.com/oncology Vol 9 September 2008
Review
chemotherapy, and in more recent Berlin-FrankfurtMnster group trials, 12001800 cGy cranial irradiation.43
The Paediatric Oncology Group study 8303 reported that
the addition of four-drug reinduction pulses did not
improve upon weekly rotation of cytarabine and
teniposide with vincristine and cyclophosphamide.38
Berlin-Frankfurt-Mnster group relapse trials randomised
patients with rst remission greater than 18 months to
high-dose or long-duration infusions of intermediatedose methotrexate with blocks of multidrug chemotherapy,41,43 with equivalent outcomes. Aside from these
randomised trials, published data do not show one
chemotherapy combination to be better than others.
In children with early marrow relapse who achieve remission, leukaemia-free survival is only 1020% with
chemotherapy alone. Outcomes are better for late relapse,
with several studies predicting leukaemia-free survival of
greater than 50%.36,39,44,54 However, some of these reports
overestimate leukaemia-free survival for isolated marrow
relapse by including patients with combined or isolated
extramedullary relapse or excluding patients with T-cell
ALL.
Haemopoietic stem cell transplantation
High-dose myeloablative chemotherapy followed by
haemopoietic stem cell transplantation is an alternative to
chemotherapy alone. However, the process requires
identication of a source of cells and a qualied transplant
centre with experienced physicians,60 successful reinduction of remission, and maintenance until transplantation, and adequate organ function; a host of social,
economic, and medical factors confound comparisons of
transplantation and chemotherapy (table 4).
Only 2530% of potential candidates for haemopoietic
stem cell transplantation have an HLA matched familial
donor. Unrelated donor registries and cord blood
banks have increased the donor pool, and advances in
immunogenetics have improved donor matching. Finding
an unrelated donor takes months, and with each passing
month, potential recipients relapse or die.58,61 Graft versus
leukaemia eect might reduce relapse risk after unrelated
donor transfer, but most studies report increased
transplant-related mortality, resulting in similar outcomes
for matched familial donor and unrelated donor
transplantation (table 5).35,6164 Transplantation of haemopoietic stem cells from unrelated cord blood is an
alternative approach in which HLA disparity is better
tolerated than in transplantation of cells from unrelated
donors, and time to procurement is shorter. Survival after
transplantation of cells from unrelated cord blood seems
similar to that obtained with transplantation of cells from
both unrelated donors and matched familial donors.65
Retrospective comparison in children with acute
leukaemias shows similar acute and chronic graft-versushost disease, transplant-related mortality, and relapse, but
increased transplant-related mortality for patients receiving
low cell doses and mismatched unrelated cord blood.35,6264
www.thelancet.com/oncology Vol 9 September 2008
Selection of patients
Treatment outcome
Biological and
physiological
factors
Relapse risk category
Achievement of second remission
Related donor availability
Unrelated donor availability
Burden of residual leukaemia
Therapy-associated toxicity
Donor age
Degree of HLA matching
Infection
GVHD
Initial treating
institution
Reinduction protocol
Referral policy
Experience with relapsed acute
lymphoblastic leukaemia
Transplanting
institution
Acceptance policy
Conditioning protocol
GVHD prophylaxis and treatment
Experience with HSCT
Socioeconomic
factors
Family resources at relapse
Opinions and beliefs regarding treatment
Limitation or refusal to cover costs of HSCT
Delays in securing approval for HSCT
Family resources after treatment
Health care resources available to patient
HLA=human leucocyte antigen. GVHD=graft vs host disease.
Table 4: Potential confounding factors aecting design and interpretation of trials of haemopoietic stem
cell transplantation (HSCT)
Published research on transplantation of haemopoetic
stem cells includes a mixture of conditioning regimens.
Cytoreduction that includes whole-body irradiation
achieves results superior to chemotherapy alone.6669
Delaying transplantation until only minimal residual
disease remains is benecial.14,70 Suppressing reemergence of the recipients stem cells after
transplantation by withdrawing immunosuppression,
or, in some cases, by infusion of donor lymphocytes,
might also confer some benet if given at a time of
minimal residual disease after transplantation,71 though
this technique has not generally been useful in treatment
of overt ALL.72
Comparison of haemopoietic stem cell transplantation and
chemotherapy
Comparison of the disparate treatments used in transplantation of haemopoietic stem cells, with its intrinsic
selection biases, with various chemotherapeutic regimens
is challenging. Studies present results many years after
trial closure, and variously report outcomes as relative risks
or actuarial event-free survival, leukaemia-free survival,
and survival with post-hoc risk-stratication. Some
cooperative groups have done prospective trials that either
tracked outcomes of chemotherapy and transplantation or
that formally assigned high-risk patients with donors
to allogeneic transplantation and those without donors to
chemotherapy or autologous transplantation.38,41,43,44,58 These
groups have also contributed to retrospective casecontrol
and matched-pair comparisons that often include patients
from the prospective trials.35,37,4648,73,74 Common ndings are
that autologous transplantation and chemotherapy have
the same outcomes and that trials that assign patients
based on donor availability uniformly experience problems
in compliance with treatment assignments.41,44,58 Table 6
shows leukaemia-free survival in large studies that reported
outcomes of chemotherapy and haemopoietic stem cell
877
Review
Population
Donor
Leukaemia-free survival
Follow-up
Comments
References
NMDP
Unrelated
363
36%
5 years
Adverse factors: rst remission <6 months, age
>15 years
62
Berlin-Frankfurt-Mnster group
Matched pairs
Unrelated
81
pairs
Intermediate risk: 39%,
high risk: 44%
5 years
Transplant related mortality 30%
35
Nordic Paediatric Haematology-
Oncology group
Unrelated
Matched sibling
28
39
54%
39%
5 years
No dierence at 5 years or for time of rst
remission before or after 2 years
61
Northwestern University
ALL second
remission
Unrelated
Unrelated cord
12
16
60%
61%
No dierence, most cord blood was HLA
mismatched
63
Childrens Oncology Group and
International Bone Marrow
Transplant Registry
AML and ALL:
High Risk
First Remission
and Second or
Later Remission
Unrelated cord
Matched
1 antigen mismatch
2 antigen mismatches
Marrow
Matched
Mismatched
64
30
201
267
60%
3645%*
33%
116
166
38%
37%
NMDP=United States National Marrow Donor Program. *Lowest in those with low cell count, highest in those with high cell count.
Table 5: Retrospective studies comparing unrelated donor or cord-blood transplant to matched familial donor or chemotherapy for acute lymphoblastic leukaemia in second or higher remission
transplantation in marrow relapse with some accounting
for duration of rst remission.35,38,41,46,47,58,69,7477
The Pediatric Oncology Group study 8303 (POG-8303) of
early marrow relapse showed that leukaemia-free survival
was 7% compared with 26% in tracked patients selected
for chemotherapy or haemopoietic stem cell transplantation,
respectively, but the dierence was not signicant.38
An International Bone Marrow Transplant Registry
(IBMTR) and Pediatric Oncology Group casecontrol
comparison of patients in rst marrow relapse, including
patients from POG-8303, found leukaemia-free survival in
patients receiving stem cells from matched familial donors
was signicantly higher than in those on chemotherapy
alone despite higher transplant-related mortality and
regardless of rst remission duration.46 In more recent
IBMTRPOG datasets, leukaemia-free survival was
signicantly higher only in early marrow relapse and only
with conditioning including total body irradiation (TBI).69
In the Berlin-Frankfurt-Mnster groups protokoll zur
Behandlung von Kindern mit Rezidiv einer akuten
lymphoblastischen Leukmie (ALL-REZ)-87 trial in
patients with high-risk or intermediate-risk marrow
relapse, leukaemia-free survival from the time of second
remission was signicantly higher in the group receiving
haemopoietic stem cells than in the chemotherapy group
(p=0026). In this trial 26% of patients with very early
relapse, but only 13% of those with early relapse had stem
cell transplantation.41 Results of autologous transplantation
and chemotherapy were the same. Matched-pair comparisons across Berlin-Frankfurt-Mnster group ALL-REZ
trials showed that unrelated donor transplantation achieved
signicantly better leukaemia-free survival than chemotherapy in high-risk relapse but not in intermediate-risk
relapse.35 In the Berlin-Frankfurt-Mnster group ALL-REZ90 trial, outcomes for chemotherapy and transplantation
of haemopoietic stem cells in patients with intermediaterisk marrow relapse are reported as not dierent without
other details;43 the authors conclude that they could not
878
assess the role of transplantation due to its rather
uncontrolled use.
The UK Medical Research Council ALL-R1 study assigned
haemopoietic stem cell transplantation to those with
matched donors, but only 9% of patients participated in
the biological randomisation. 5-year event-free survival
was 7% in the early-relapse group.44 Transplantation had
no signicant benecial eect for leukaemia-free survival
in any subset. Both increased transplant-related mortality
and relapse contributed to poor outcome with transplantation of haemopoietic stem cells. By contrast, the
Great Ormond Street institutional experience with Medical
Research Council protocols showed a signicant
transplantation benet in children in the Berlin-FrankfurtMnster groups high-risk stratum (p=0002), but not in
their intermediate risk group.37 The UK Medical Research
Council ALL-R2 trial could not document a signicant
benet from haemopoietic stem cell transplantation in any
risk stratum in four institutions including Great Ormond
Street; there were no survivors of early relapse treated with
chemotherapy and only two in the transplantation group,
resulting in a low level of enthusiasm for transplantation.36
In the Childrens Cancer Groups study 1941 for early
marrow relapse, nearly half the patients never arrived at
the point of planned haemopoietic stem cell transplantation
or chemotherapy randomisation because of induction
failure, early death, or second relapse.58 Leukaemia free
survival was 42% in the transplantation group and 30% in
the chemotherapy group, but the intention-to-treat analysis
showed apparent equivalence of the two approaches.
However, a third of patients randomised to chemotherapy
underwent alternative donor HSCT. On the basis of per
protocol analysis, the Childrens Oncology Group now
recommends transplantation of allogeneic haemopoietic
stem cells from best possible donor in all patients with
early relapse. For later relapse, a current Childrens
Oncology Group study is randomising between dierent
vincristine doses during chemotherapy, and recommends
www.thelancet.com/oncology Vol 9 September 2008
Review
Design
N
HSCT
Chemotherapy
Very early
Early
HSCT
HSCT
Chemotherapy
26%
Late
Chemotherapy
7%*
HSCT
References
Chemotherapy
POG-8303
Matched pair
42
192
38
IBMTR/POG
Matched pair
255
255
30%
14%
41%
7%
IBMTR/POG
Matched pair
188
40%
23%
53%
32%
46
61%
59%*
BFM REZ 87
Randomised
25
145
59%
30%
69
41
BFM REZ
Matched pair
81
81
44%
0%
49%
39%*
35
CCG-1941
Randomised
ITT/PP
29%/42%
27%/30%
58
NOPHO
Casecontrol
75
150
32%
11%
42%
29%
47
AIEOP/GITMO
Casecontrol
57
230
33%
16%
55%
40%*
74
Leiden
Casecontrol
75
150
44%
24%
75
MSKCC
Casecontrol
38
37
48%
9%
81%
37%
76
Westmead
Casecontrol
20
34
54%
10%
57%
0%*
77
Leukaemia-free survival adjusted for time to transplant; results are actuarial calculations except for two calculated from text and tables.38,69 Earliest relapses are less than
1824 months from rst remission, early relapses include these, as well as late relapses under 6 months from therapy discontinuation, and late relapses occurred after this
time. HSCT=haemopoietic stem cell transplantation. POG=Paediatric Oncology Group. IBMTR=International Bone Marrow Transplant Registry. BFM=Berlin-FrankfurtMnster group. CCG=Childrens Cancer Group. ITT=intention to treat. PP=per protocol. NOPHO=Nordic Paediatric Hematology-Oncology group. AIEOP=Associazione Italiana
Ematologia ed Oncologia Pediatrica. GITMO=Gruppo Italiano Trapianti Midollo Osseo. MSKCC=Memorial Sloan-Kettering Cancer Center. *p>005. p005. p 0005.
Table 6: Studies of leukaemia-free survival at 3 years or longer after allogeneic bone-marrow transplantation or chemotherapy for acute lymphoblastic
leukaemia in second remission
matched familial donor haemopoietic stem-cell transplantation as denitive therapy where possible.
Sequential population-based retrospective studies in
Scandinavian children treated for ALL relapse show that
transplantation of haemopoietic stem cells led to increased
long-term survival compared with chemotherapy irrespective of timing of rst remission.47,48 Over the course of
rst, second, and subsequent relapses, treatment-related
mortality was higher with chemotherapy than with
transplantation. Although these results suggest that transplantation should be used in every marrow relapse, because
of non-lethal morbidities6668 selection of patients who will
not relapse after chemotherapy alone is important.48
In the other studies, outcomes are better with transplantation of haemopoietic stem cells in patients with rst
remission lasting less than 18 months, but the advantage is
less in patients with later relapse (table 6).7477 In no
comparison is outcome after transplantation worse than
after chemotherapy alone.
Further relapse is the greatest barrier to cure after rst
relapse. Best possible allogeneic transplant oers a better
chance of cure than chemotherapy for patients who have
not had haemopoietic stem cell transplantation in the
recent past.36,48 Although some studies report occasional
long-term third remissions in patients at intermediate
and standard risk after second relapse,37,43 cure is unlikely
unless the patients have favourable features at initial
diagnosis and rst relapse.36,48
Despite the limitations of studies in marrow relapse, the
results provide reasonable support for broad principles to
guide current treatment and future clinical trials in rst
relapse. Fundamentally, both current chemotherapy and
transplantation of haemopoietic stem cells are toxic,
www.thelancet.com/oncology Vol 9 September 2008
and neither is highly eective in curing most patients with
marrow relapse.
Improving therapy for marrow relapse
Better targeted chemotherapy is central to improving
outcomes for patients with marrow relapse irrespective of
treatment.33,37 Assessment of new therapies begins with
patients in relapse. Many patients in second marrow relapse
respond, albeit transiently, to the same drugs used
previously, as well as to newer, costlier analogues of these
drugs and investigational drugs. Because of the success of
established drugs, investigational drugs are not widely used
for treatment of ALL until patients have become refractory
to multiple therapies. Phase I trials therefore include
disproportionate numbers of patients in second or higher
relapse. Drug resistance in this heavily pretreated
population might contribute to poor response rates that
underestimate the potential of these drugs in earlier relapse
and perpetuate beliefs that investigational drugs are futile.
In the absence of evidence for therapeutic benet, the use
of new drugs in early treatment regimens is hard to justify.
Pui and Jeha13 recently reviewed new drugs for leukaemia
in clinical trials, and Lee and co-workers78 have comprehensively catalogued new agents tested in paediatric
oncology trials between 1990 and 2004. The National
Institutes of Health Physician Data Query (PDQ) database79
also describes many of them. Table 7 lists the small
molecule inhibitors, antimetabolites, and monoclonal
antibodies in active development in paediatric leukaemia.
Some target specic mutant molecules and others are
broadly active, encompassing many subsets of ALL. The
small molecule inhibitor imatinib developed to inhibit
mutant BCRABL tyrosine kinase has already shown
879
Review
Mechanism of action
Disease subset
Rituximab
Antibody against CD20
B-lineage ALL
Epratuzumab, BL22
Antibody against CD22
B-lineage ALL
Alemtuzumab
Antibody against CD52
B-lineage and T-lineage ALL
Combotox
Antibody against CD19 and CD22
B-lineage ALL
Daclizumab
Antibody against interleukin-2 receptor (CD25) T-lineage ALL
Monoclonal antibodies
Small molecule inhibitors
Imatinib
Inhibition of BCRABL, cKIT, PDGFR
Ph+ ALL
Dasatinib
Inhibition of BCRABL, SRC
Ph+ ALL
Bortezomib
28S protease and inhibition of NF-B
B-lineage and T-lineage ALL
Sirolimus, temsirolimus
Inhibition of mTOR
B-lineage and T-lineage ALL
CEP-701
Inhibition of FLT3
Infant MLL
MK0572, Ly450139
Inhibition of NOTCH1 secretase
T-lineage ALL
SAHA, valproic acid
Histone deacetylase inhibition
B-lineage and T-lineage ALL
Nucleoside analogues
Clofarabine
Deoxyadenosine analogue
B-lineage and T-lineage ALL
Nelarabine
Deoxyguanosine analogue
T-lineage ALL
Forodesine
PNP inhibitor
T-lineage ALL
Intrathecal liposomal
cytarabine
DNA polymerase inhibition
CNS ALL
Decitabine
DNA demethylation
B-lineage and T-lineage ALL
FLT3=FMS-like tyrosine kinase. cKIT=c-kit stem cell factor (CD117). MLL=mixed lineage leukaemia. mTOR: mammalian
target of rapamycin. NFB=nuclear factor B. PDGFR=platelet-derived growth factor receptor. Ph+=Philadelphia
chromosome. PNP=purine nucleoside phosphorylase. SAHA=suberoylanilide hydroxamic acid. SRC=Src protein
tyrosine kinase.
Table 7: New drugs in development for trials in paediatric acute lymphoblastic leukaemia (ALL)
ecacy in frontline therapy of paediatric Philadelphia
chromosome-positive disease,80 and trials of the newer
inhibitor dasatinib are planned. The nucleoside analogues
clofarabine81 and nelarabine82 have proven activity in
B-precursor and T-lineage ALL, respectively. These drugs
have progressed from phase I to phase II or III randomised
trials by the Childrens Oncology Group and are approved
in the USA for treatment of paediatric ALL. Clofarabine is
also being incorporated in HSCT cytoreduction regimens.
Rituximab has proven activity in adult ALL, but has not
been investigated in paediatric disease.
FMS-related tyrosine kinase 3 (FLT3) is uniformly
overexpressed in MLL-rearranged infant acute lymphoblastic leukaemia. Preclinical models show synergy of the
FLT3 inhibitor lestaurtinib with cytotoxic chemotherapy.
In the next Childrens Oncology Group trial for infant
acute lymphoblastic leukaemia, lestaurtinib follows each
course of postremission intensication therapy. Whether
lestaurtinib will be as successful in treating overexpression
of FLT3 as in treating mutant constitutive expression
resulting from FLT3 internal tandem duplication in acute
myeloid leukaemia is unknown.
On the basis of activity in lymphoid disease in adult
phase I and II trials and demonstration of overexpressed
nuclear factor B in paediatric leukaemia, the proteasome
inhibitor bortezomib has completed phase I assessment,83
and is advancing in phase II combined with a standardised
880
Childrens Oncology Group three-block reinduction and
consolidation regimen. Ecacy will be assessed by
comparison to previous patients receiving the same
therapy without any new agent and those receiving this
therapy with epratuzumab, by use of the early endpoints of
second remission and minimal residual disease. After
consolidation therapy, transplantation of allogeneic
haemopoietic stem cells is recommended for all patients
with early marrow relapse.
There are still only a few drugs with sucient activity in
recurrent acute lymphoblastic leukaemia to warrant their
incorporation in phase II and III studies. To expedite
development of drugs with high probability of activity in
paediatric tumours, the US National Cancer Institute,
Childrens Oncology Group, and European cooperative
groups participate in the Pediatric Preclinical Testing
Program. The programmes core consists of a large
inventory of paediatric tumour cell lines, preclinical human
xenograft models, and samples from patients. Genomic
studies are used to identify targets and in-vitro and in-vivo
testing predicts activity against these targets. The
programme has conrmed good single agent activity of
vincristine and cyclophosphamide, sirolimus, dasatinib,
and bortezomib in murine models of ALL but has not
published on the discovery of agents that are not already
known to be active in lymphoid disease. Whether these
models are better predictors for activity in human beings
than the MTT assay that consistently shows good correlation
with clinical outcomes is unknown.18 Even with highthroughput technology, drug discovery is a slow process.
Although randomised trials of dierent continuation
chemotherapy with or without incorporating new agents
have been dicult to organise, there are several trials of
haemopoietic stem cell transplantation. Pilot studies
suggest that high doses of haemopoietic cells decrease
relapse after transplantation, and randomised trials
are underway to study this approach. The Blood and
Marrow Transplant Clinical Trials Network is leading a
multicentre trial randomising to haemopoietic stem cell
transplantation by use of cells from one or two cord blood
donors. The Childrens Oncology Group is comparing
standard marrow collection to collection after stimulation
with granulocyte colony stimulating factor in paediatric
marrow donors. Sirolimus, an inhibitor of the mammalian
target of rapamycin (mTOR), is in phase I studies for
refractory leukaemia in children and adults. A Childrens
Oncology Group trial exploits sirolimus dual immunosuppressive and antileukaemic activity by randomising
sirolimus and standard prophylaxis for graft versus host
disease at a time of minimal residual disease after
transplantation of haemopoietic stem cells. Although these
studies may improve outcomes after transplantation, the
heterogeneity of transplantation and absence of standard
continuation chemotherapy for patients not having
transplantation will confound assessment on the basis of
event-free survival, leukaemia-free survival, and overall
survival.
www.thelancet.com/oncology Vol 9 September 2008
Review
To accelerate the process of bringing new drugs to
patients, Skolnik and colleagues16 have proposed a new
phase I design that enrols up to six patients concurrently at
a dose level, on the basis of the number of evaluable
patients at that level and the number who have experienced
or remain at risk for dose-limiting toxicity. Simulations of
this rolling-six design predict about a 12% reduction in the
length of phase I studies when compared with the current
standard practice of pausing after every third patient for
reassessment. In most of medicine, phase II trials are
randomised comparisons of an established therapy with
and without a new treatment, but the usual phase II study
in oncology is a single arm study of ecacy of the maximum tolerated dose of a drug across a range of neoplasms,
with results compared with a historical control. Randomised
phase II comparisons will yield more informative results;
randomised comparisons of two new agents and a standard
regimen can show whether one is better than the other.
Because use of haemopoietic stem cell transplantation
confounds assessment of outcomes with a new agent,
surrogate markers of clinical benet are necessary. Time
and extent of minimal residual disease reduction are presently the most tested and useful markers in acute lymphoblastic leukaemia.14 Patients with isolated extramedullary
relapse and PCR-detectable marrow disease might oer an
ideal opportunity for investigation of the eects of single
biological agents on minimal residual disease, but these
studies would probably face the problems that have beset
treatments incoporating a specic therapeutic window.84
Conclusion
By contrast with the orderly succession of large randomised
trials and continuous progress in ALL at initial diagnosis,
most studies in marrow relapse are single-arm studies or
retrospective reviews that have not provided substantial
improvements. Polarisation around the issue of haemopoietic stem cell transplantation has thwarted potential
collaborations that might enrol enough patients for randomised trials. Such trials in relapse are dicult because
of the heterogeneity of the population. Nonetheless, randomised trials are needed to produce credible results that
change practice. Even if randomised comparisons of
chemotherapy with stem cell transplantation are not
possible, there are many investigations that are possible,
such as trials to dene a standard chemotherapy backbone
as the foundation for subsequent transplantation or continuation chemotherapy. Randomised phase II trials in
relapse also provide a platform for assessing how a new
drug does when added to a standard therapy or how two
new treatments compare with one another. Similarly,
randomised trials in patients having haemopoietic stem
cell transplantation could help to address some of the
heterogeneity in selection of patients and conditioning
regimens, which are matters of strong local preference.
Because the clone destined for relapse is often present at
diagnosis and is inherently more resistant to induction
chemotherapy,2427 prevention of marrow relapse remains
www.thelancet.com/oncology Vol 9 September 2008
Search strategy and selection criteria
References published in English since 1990 were identied by
searches of Pubmed and references cited in relevant
publications, particularly recent reviews. Search terms included
acute lymphoblastic leukemia, acute lymphocytic leukemia,
precursor cell lymphoblastic leukemia-lymphoma, relapse,
refractory, stem cell, marrow transplantation, phase I,
phase II, infant, child, preschool, child, and adolescent.
Case reports were excluded. To limit references to the allotted
number of citations, we prioritised recent publications, reviews,
cooperative group trials, trials with larger study populations,
and those with greatest potential to guide future developments.
the best strategy for improving survival in ALL. Augmenting
early postremission therapy in slow responders proved that
changing therapy early prevents relapse.85 Minimal residual
disease early in therapy identies the patients most likely
to have both a rst relapse and subsequent relapses. In the
future, there will ideally be a unied relapse risk stratication that includes assessment of minimal residual disease
in apparent isolated extramedullary relapse and time to
elimination of minimal residual disease after reinduction
and before haemopoietic stem cell transplantation.14,45
Dierential expression of genes will eventually play a part in
risk stratication both at diagnosis and at relapse. Assessment of minimal residual disease, reproducible molecular
signatures predicting response, and in-vivo testing for drug
sensitivity might permit early treatment modication. Better
understanding of molecular pathogenesis oers opportunities to develop dierent, possibly less toxic and possibly
more specic, drugs. Such agents are likely to provide the
best opportunities to improve long-term survival both before
and after relapse. In order to assess candidates rapidly
and rigorously, trials will need willingness to compromise among both oncologists and the public, and commitment to scientic inquiry and international collaboration.
Conicts of interest
The authors declared no conicts of interest.
Acknowledgments
The authors thank John Choi for providing photomicrographs of bone
marrow aspirates, and Anna Meadows and William G Woods for critical
review of the paper.
References
1
Pui CH, Evans WE. Treatment of acute lymphoblastic leukemia.
N Engl J Med 2006; 354: 16678.
2
Schrappe M, Reiter A, Zimmermann M, et al. Long-term results of
four consecutive trials in childhood ALL performed by the ALL-BFM
study group from 1981 to 1995. Leukemia 2000; 14: 220522.
3
Gaynon PS, Trigg ME, Heerema NA, et al. Childrens Cancer Group
trials in childhood acute lymphoblastic leukemia: 19831995.
Leukemia 2000; 14: 222333.
4
Silverman LB, Declerck L, Gelber RD, et al. Results of Dana-Farber
Cancer Institute Consortium protocols for children with newly
diagnosed acute lymphoblastic leukemia (1981-1995). Leukemia 2000;
14: 224756.
5
Vilmer E, Suciu S, Ferster A, et al. Long-term results of three
randomized trials (58831, 58832, 58881) in childhood acute
lymphoblastic leukemia: a CLCG-EORTC report. Leukemia 2000;
14: 225766.
881
Review
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
882
Tsuchida M, Ikuta K, Hanada R, et al. Long-term follow-up of
childhood acute lymphoblastic leukemia in Tokyo Childrens Cancer
Study Group 19811995. Leukemia 2000; 14: 2295306.
Eden OB, Harrison G, Richards S, et al. Long-term follow-up of the
United Kingdom Medical Research Council protocols for childhood
acute lymphoblastic leukaemia, 19801997. Leukemia 2000;
14: 230720.
Schroeder H, Garwicz S, Kristinsson J, Siimes MA, Wesenberg F,
Gustafsson G. Outcome after rst relapse in children with acute
lymphoblastic leukemia: a population-based study of 315 patients
from the Nordic Society of Pediatric Hematology and Oncology
(NOPHO). Med Pediatr Oncol 1995; 25: 37278.
Gaynon PS, Qu RP, Chappell RJ, et al. Survival after relapse in
childhood acute lymphoblastic leukemia: impact of site and time to
rst relapsethe Childrens Cancer Group Experience. Cancer 1998;
82: 138795.
Rizzari C, Valsecchi MG, Arico M, et al. Outcome of very late relapse
in children with acute lymphoblastic leukemia. Haematologica 2004;
89: 42734.
Thomson B, Park JR, Felgenhauer J, et al. Toxicity and ecacy of
intensive chemotherapy for children with acute lymphoblastic
leukemia (ALL) after rst bone marrow or extramedullary relapse.
Pediatr Blood Cancer 2004; 43: 57179.
Wrong Diagnosis. Statistics by country for acute lymphocytic
leukemia. http://wrongdiagnosis.com/a/acute_lymphocytic_
leukemia/stats-country.htm (accessed Aug 6, 2008).
Pui CH, Jeha S. New therapeutic strategies for the treatment of acute
lymphoblastic leukaemia. Nat Rev Drug Discov 2007; 6: 14965.
Appelbaum FR, Rosenblum D, Arceci RJ, et al. End points to
establish the ecacy of new agents in the treatment of acute
leukemia. Blood 2007; 109: 181016.
Ratain MJ, Humphrey RW, Gordon GB, et al. Recommended changes
to oncology clinical trial design: Revolution or evolution? Eur J Cancer
2008; 44: 811.
Skolnik JM, Barrett JS, Jayaraman B, Patel D, Adamson PC.
Shortening the timeline of pediatric phase I trials: the rolling six
design. J Clin Oncol 2008; 26: 19095.
Bhojwani D, Kang H, Moskowitz NP, et al. Biologic pathways
associated with relapse in childhood acute lymphoblastic leukemia:
a Childrens Oncology Group study. Blood 2006; 108: 71117.
Klumper E, Pieters R, Veerman AJ, et al. In vitro cellular drug
resistance in children with relapsed/refractory acute lymphoblastic
leukemia. Blood 1995; 86: 386168.
Abshire TC, Buchanan GR, Jackson JF, et al. Morphologic,
immunologic and cytogenetic studies in children with acute
lymphoblastic leukemia at diagnosis and relapse: a Pediatric
Oncology Group study. Leukemia 1992; 6: 35762.
Campana D, Coustan-Smith E. Advances in the immunological
monitoring of childhood acute lymphoblastic leukaemia.
Best Pract Res Clin Haematol 2002; 15: 119.
Borowitz MJ, Pullen DJ, Winick N, Martin PL, Bowman WP,
Camitta B. Comparison of diagnostic and relapse ow cytometry
phenotypes in childhood acute lymphoblastic leukemia: implications
for residual disease detection: a report from the childrens oncology
group. Cytometry B Clin Cytom 2005; 68: 1824.
Felix CA, Poplack DG. Characterization of acute lymphoblastic
leukemia of childhood by immunoglobulin and T-cell receptor gene
patterns. Leukemia 1991; 5: 101525.
van der Velden VH, Hochhaus A, Cazzaniga G, Szczepanski T,
Gabert J, van Dongen JJ. Detection of minimal residual disease in
hematologic malignancies by real-time quantitative PCR: principles,
approaches, and laboratory aspects. Leukemia 2003; 17: 101334.
Choi S, Henderson MJ, Kwan E, et al. Relapse in children with acute
lymphoblastic leukemia involving selection of a preexisting drugresistant subclone. Blood 2007; 110: 63239.
Germano G, del Giudice L, Palatron S, et al. Clonality prole in
relapsed precursor-B-ALL children by GeneScan and sequencing
analyses: consequences on minimal residual disease monitoring.
Leukemia 2003; 17: 157382.
Szczepanski T, van der Velden VH, Ra T, et al. Comparative analysis
of T-cell receptor gene rearrangements at diagnosis and relapse of
T-cell acute lymphoblastic leukemia (T-ALL) shows high stability of
clonal markers for monitoring of minimal residual disease and
reveals the occurrence of second T-ALL. Leukemia 2003; 17: 214956.
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
de Haas V, Verhagen OJ, von dem Borne AE, Kroes W,
van den Berg H, van der Schoot CE. Quantication of minimal
residual disease in children with oligoclonal B-precursor acute
lymphoblastic leukemia indicates that the clones that grow out during
relapse already have the slowest rate of reduction during induction
therapy. Leukemia 2001; 15: 13440.
Zuna J, Ford AM, Peham M, et al. TEL deletion analysis supports a
novel view of relapse in childhood acute lymphoblastic leukemia.
Clin Cancer Res 2004; 10: 535560.
Beesley AH, Cummings AJ, Freitas JR, et al. The gene expression
signature of relapse in paediatric acute lymphoblastic leukaemia:
implications for mechanisms of therapy failure. Br J Haematol 2005;
131: 44756.
Kirschner-Schwabe R, Lottaz C, Todling J, et al. Expression of late cell
cycle genes and an increased proliferative capacity characterize very
early relapse of childhood acute lymphoblastic leukemia.
Clin Cancer Res 2006; 12: 455361.
Flotho C, Coustan-Smith E, Pei D, et al. A set of genes that regulate
cell proliferation predicts treatment outcome in childhood acute
lymphoblastic leukemia. Blood 2007; 110: 127177.
Staal FJ, van der Burg M, Wessels LF, et al. DNA microarrays for
comparison of gene expression proles between diagnosis and
relapse in precursor-B acute lymphoblastic leukemia: choice of
technique and purication inuence the identication of potential
diagnostic markers. Leukemia 2003; 17: 132432.
Gaynon PS. Childhood acute lymphoblastic leukaemia and relapse.
Br J Haematol 2005; 131: 57987.
Uderzo C, Dini G, Locatelli F, Miniero R, Tamaro P. Treatment of
childhood acute lymphoblastic leukemia after the rst relapse:
curative strategies. Haematologica 2000; 85 (11 suppl): 4753.
Borgmann A, von Stackelberg A, Hartmann R, et al.
Unrelated donor stem cell transplantation compared with
chemotherapy for children with acute lymphoblastic leukemia in a
second remission: a matched-pair analysis. Blood 2003;
101: 383539.
Roy A, Cargill A, Love S, et al. Outcome after rst relapse in
childhood acute lymphoblastic leukaemialessons from the United
Kingdom R2 trial. Br J Haematol 2005; 130: 6775.
Chessells JM, Veys P, Kempski H, et al. Long-term follow-up of
relapsed childhood acute lymphoblastic leukaemia. Br J Haematol
2003; 123: 396405.
Buchanan GR, Rivera GK, Pollock BH, et al. Alternating drug pairs
with or without periodic reinduction in children with acute
lymphoblastic leukemia in second bone marrow remission:
a Pediatric Oncology Group Study. Cancer 2000; 88: 116674.
Rivera GK, Zhou Y, Hancock ML, et al. Bone marrow recurrence after
initial intensive treatment for childhood acute lymphoblastic
leukemia. Cancer 2005; 103: 36876.
Matsuzaki A, Nagatoshi Y, Inada H, et al. Prognostic factors for
relapsed childhood acute lymphoblastic leukemia: impact of allogeneic
stem cell transplantationa report from the Kyushu-Yamaguchi
Childrens Cancer Study Group. Pediatr Blood Cancer 2005; 45: 11120.
Einsiedel HG, von Stackelberg A, Hartmann R, et al. Long-term
outcome in children with relapsed ALL by risk-stratied salvage
therapy: results of trial acute lymphoblastic leukemia-relapse study
of the Berlin-Frankfurt-Munster Group 87. J Clin Oncol 2005;
23: 794250.
Wheeler K, Richards S, Bailey C, Chessells J. Comparison of bone
marrow transplant and chemotherapy for relapsed childhood acute
lymphoblastic leukaemia: the MRC UKALL X experience.
Br J Haematol 1998; 101: 94103.
von Stackelberg A, Hartmann R, Buhrer C, et al. High-dose as
compared with intermediate-dose methotrexate in children with a rst
relapse of acute lymphoblastic leukemia. Blood 2008; 111: 257380.
Lawson SE, Harrison G, Richards S, et al. The UK experience in
treating relapsed childhood acute lymphoblastic leukaemia: a report
on the medical research council UKALLR1 study. Br J Haematol 2000;
108: 53143.
Hagedorn N, Acquaviva C, Fronkova E, et al. Submicroscopic bone
marrow involvement in isolated extramedullary relapses in childhood
acute lymphoblastic leukemia: a more precise denition of isolated
and its possible clinical implications, a collaborative study of the
Resistant Disease Committee of the International BFM study group.
Blood 2007; 110: 402229.
www.thelancet.com/oncology Vol 9 September 2008
Review
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
61
62
63
64
65
Barrett A, Horowitz M, Pollock B, et al. Bone marrow transplants
from HLA-identical siblings as compared with chemotherapy for
children with acute lymphoblastic leukemia in a second remission.
N Engl J Med 1994; 331: 125358.
Schroeder H, Gustafsson G, Saarinen-Pihkala U, et al. Allogeneic
bone marrow transplantation in second remission of childhood acute
lymphoblastic leukemia: a population-based case control study from
the Nordic countries. Bone Marrow Transplant 1999; 23: 55560.
Saarinen-Pihkala UM, Heilmann C, Winiarski J, et al. Pathways
through relapses and deaths of children with acute lymphoblastic
leukemia: role of allogeneic stem-cell transplantation in Nordic data.
J Clin Oncol 2006; 24: 575062.
Eckert C, Biondi A, Seeger K, et al. Prognostic value of minimal
residual disease in relapsed childhood acute lymphoblastic
leukaemia. Lancet 2001; 358: 123941.
Coustan-Smith E, Gajjar A, Hijiya N, et al. Clinical signicance of
minimal residual disease in childhood acute lymphoblastic leukemia
after rst relapse. Leukemia 2004; 18: 499504.
Abshire TC, Pollock BH, Billett AL, Bradley P, Buchanan GR. Weekly
polyethylene glycol conjugated L-asparaginase compared with
biweekly dosing produces superior induction remission rates in
childhood relapsed acute lymphoblastic leukemia: a Pediatric
Oncology Group Study. Blood 2000; 96: 170915.
Feig SA, Ames MM, Sather HN, et al. Comparison of idarubicin to
daunomycin in a randomized multidrug treatment of childhood acute
lymphoblastic leukemia at rst bone marrow relapse: a report from
the Childrens Cancer Group. Med Pediatr Oncol 1996; 27: 50514.
Vats T, Buchanan G, Mehta P, et al. A study of toxicity and comparative
therapeutic ecacy of vindesine-prednisone vs. vincristine-prednisone
in children with acute lymphoblastic leukemia in relapse: aPediatric
Oncology Group study. Invest New Drugs 1992; 10: 23134.
Leahey AM, Bunin NJ, Belasco JB, Meek R, Scher C, Lange BJ. Novel
multiagent chemotherapy for bone marrow relapse of pediatric acute
lymphoblastic leukemia. Med Pediatr Oncol 2000; 34: 31318.
Testi AM, Del Giudice I, Arcese W, et al. A single high dose of
idarubicin combined with high-dose ARA-C for treatment of rst
relapse in childhood high-risk acute lymphoblastic leukaemia:
a study of the AIEOP group. Br J Haematol 2002; 118: 74147.
Edick MJ, Gajjar A, Mahmoud HH, et al. Pharmacokinetics and
pharmacodynamics of oral etoposide in children with relapsed or
refractory acute lymphoblastic leukemia. J Clin Oncol 2003; 21: 134046.
Bernstein ML, Whitehead VM, Devine S, et al. Ifosfamide with
mesna uroprotection and etoposide in recurrent, refractory acute
leukemia in childhood: a Pediatric Oncology Group Study. Cancer
1993; 72: 179094.
Gaynon P, Harris R, Altman A, et al. Bone marrow transplantation
versus prolonged intensive chemotherapy for children with acute
lymphoblastic leukemia and an initial bone marrow relapse within
12 months of the completion of primary therapy: Childrens Oncology
Group Study CCG-1941. J Clin Oncol 2006; 24: 315056.
Garcia-Manero G, Thomas DA. Salvage therapy for refractory or
relapsed acute lymphocytic leukemia. Hematol Oncol Clin North Am
2001; 15: 163205.
Loberiza FR Jr, Zhang MJ, Lee SJ, et al. Association of transplant
center and physician factors on mortality after hematopoietic stem
cell transplantation in the United States. Blood 2005; 105: 297987.
Saarinen-Pihkala U, Gustafsson F, Ringeden O, et al. No disadvantage
in outcome of using matched unrelated donors as compared with
matched sibling donors for bone marrow transplantation in children
with acute lymphoblastic leukemia in second remission. J Clin Oncol
2001; 19: 340614.
Bunin N, Carston M, Wall D, et al. Unrelated marrow transplantation
for children with acute lymphoblastic leukemia in second remission.
Blood 2002; 99: 315157.
Jacobsohn D, Hewlett B, Ranalli M, et al. Outcomes of unrelated cord
blood transplants and allogeneic-related hematopoietic stem cell
transplants in children with high-risk acute lymphocytic leukemia.
Bone Marrow Transplant 2004; 34: 90107.
Eapen M, Rubinstein P, Zhang MJ, et al. Outcomes of transplantation
of unrelated donor umbilical cord blood and bone marrow in children
with acute leukaemia: a comparison study. Lancet 2007; 369: 194754.
Gluckman E, Rocha V. Cord blood transplantation for children with
acute leukaemia: a Eurocord registry analysis. Blood Cells Mol Dis
2004; 33: 27173.
www.thelancet.com/oncology Vol 9 September 2008
66
67
68
69
70
71
72
73
74
75
76
77
78
79
80
81
82
83
84
85
Dai QY, Souillet G, Bertrand Y, et al. Antileukemic and long-term
eects of two regimens with or without TBI in allogeneic bone
marrow transplantation for childhood acute lymphoblastic leukemia.
Bone Marrow Transplant 2004; 34: 66773.
Davies SM, Ramsay NK, Klein JP, et al. Comparison of preparative
regimens in transplants for children with acute lymphoblastic
leukemia. J Clin Oncol 2000; 18: 34047.
Bunin N, Aplenc R, Kamani N, Shaw K, Cnaan A, Simms S.
Randomized trial of busulfan vs total body irradiation containing
conditioning regimens for children with acute lymphoblastic
leukemia: a Pediatric Blood and Marrow Transplant Consortium
study. Bone Marrow Transplant 2003; 32: 54348.
Eapen M, Raetz E, Zhang MJ, et al. Outcomes after HLA-matched
sibling transplantation or chemotherapy in children with B-precursor
acute lymphoblastic leukemia in a second remission: a collaborative
study of the Childrens Oncology Group and the Center for
International Blood and Marrow Transplant Research. Blood 2006;
107: 496167.
Bunin N, Johnston D, Roberts W, et al. Residual leukaemia after bone
marrow transplant in children with acute lymphoblastic leukaemia
after rst haematological relapse or with poor initial presenting
features. Br J Haematol 2003; 120: 71115.
Bader P, Kreyenberg H, Hoelle W, et al. Increasing mixed chimerism
is an important prognostic factor for unfavorable outcome in children
with acute lymphoblastic leukemia after allogeneic stem-cell
transplantation: possible role for pre-emptive immunotherapy?
J Clin Oncol 2004; 22: 1696706.
Blair A, Goulden NJ, Libri NA, Oakhill A, Pamphilon DH.
Immunotherapeutic strategies in acute lymphoblastic leukaemia
relapsing after stem cell transplantation. Blood Rev 2005; 19: 289300.
Eapen M, Giralt SA, Horowitz MM, et al. Second transplant for acute
and chronic leukemia relapsing after rst HLA-identical sibling
transplant. Bone Marrow Transplant 2004; 34: 72127.
Uderzo C, Valsecchi G, Bacigalupo A, et al. Treatment of childhood
acute lymphoblastic leukemia in second remission with allogeneic
bone marrow transplantation and chemotherapy: ten year experience
of the Italian Bone Marrow Transplantation Group and the Italian
Pediatric Hematology Oncology Association. J Clin Oncol 1995;
13: 35258.
Hoogerbrugge P, Gerritsen E, Does-van den Berg A, et al.
Case-control analysis of allogeneic bone marrow transplantation
versus maintenance chemotherapy for relapsed ALL in children.
Bone Marrow Transplant 1995; 15: 25559.
Boulad F, Steinherz P, Reyes B, et al. Allogeneic bone marrow
transplant versus chemotherapy for the treatment of childhood acute
lymphoblastic leukemia in second remission: a single-institution
study. J Clin Oncol 1999; 17: 197207.
Bleakley M, Shaw P, Nielsen J. Allogeneic bone marrow
transplantation for childhood relapsed acute lymphoblastic leukemia:
comparison of outcome in patients with and without a matched
family donor. Bone Marrow Transplant 2002; 30: 17.
Lee DP, Skolnik JM, Adamson PC. Pediatric phase I trials in oncology:
an analysis of study conduct eciency. J Clin Oncol 2005; 23: 843141.
National Cancer Institute. PDQNCIs comprehensive cancer
database. http://www.nci.nih.gov/cancerinfo/pdq/cancerdatabase
(accessed May 5, 2008).
Jones LK, Saha V. Philadelphia positive acute lymphoblastic
leukaemia of childhood. Br J Haematol 2005; 130: 489500.
Jeha S, Gaynon PS, Razzouk BI, et al. Phase II study of clofarabine in
pediatric patients with refractory or relapsed acute lymphoblastic
leukemia. J Clin Oncol 2006; 24: 191723.
Berg SL, Blaney SM, Devidas M, et al. Phase II study of nelarabine
(compound 506U78) in children and young adults with refractory
T-cell malignancies: a report from the Childrens Oncology Group.
J Clin Oncol 2005; 23: 337682.
Horton TM, Pati D, Plon SE, et al. A phase 1 study of the proteasome
inhibitor bortezomib in pediatric patients with refractory leukemia: a
Childrens Oncology Group study. Clin Cancer Res 2007; 13: 151622.
Smith MA, Anderson B. Phase II window studies: 10 years of
experience and counting. J Pediatr Hematol Oncol 2001; 23: 33437.
Nachman JB, Sather HN, Sensel MG, et al. Augmented postinduction therapy for children with high-risk acute lymphoblastic
leukemia and a slow response to initial therapy. N Engl J Med 1998;
338: 166371.
883
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Tabel Konversi FiO2Document2 paginiTabel Konversi FiO2arie_yuliantoÎncă nu există evaluări
- PELOD2Document13 paginiPELOD2hawinnurdianaÎncă nu există evaluări
- 26 Best Marma Images - Ayurveda, Acupressure, ReflexologyDocument1 pagină26 Best Marma Images - Ayurveda, Acupressure, Reflexologyion vasile100% (1)
- Clinical Pharmacy Pocket Companion 2nd EditionDocument567 paginiClinical Pharmacy Pocket Companion 2nd EditionA.M DiabÎncă nu există evaluări
- Unrelated Donor Stem Cell Transplantation Compared With Chemotherapy For Children With Acute Lymphoblastic Leukemia in A Second Remission A Matched-Pair AnalysisDocument5 paginiUnrelated Donor Stem Cell Transplantation Compared With Chemotherapy For Children With Acute Lymphoblastic Leukemia in A Second Remission A Matched-Pair AnalysishawinnurdianaÎncă nu există evaluări
- Global HIV/AIDS Response - Epidemic Update and Health Sector Progress Towards Universal Access - Progress Report 2011Document233 paginiGlobal HIV/AIDS Response - Epidemic Update and Health Sector Progress Towards Universal Access - Progress Report 2011UNICEF100% (1)
- Uropaty Obstruktif 2Document9 paginiUropaty Obstruktif 2hawinnurdianaÎncă nu există evaluări
- Leukemia and Nervous System PDFDocument25 paginiLeukemia and Nervous System PDFhawinnurdianaÎncă nu există evaluări
- Acute and Long-Term Neurological Complications in Children With Acute Lymphoblastic LeukemiaDocument4 paginiAcute and Long-Term Neurological Complications in Children With Acute Lymphoblastic LeukemiahawinnurdianaÎncă nu există evaluări
- Epidemiology Pneumonia PDFDocument8 paginiEpidemiology Pneumonia PDFhawinnurdianaÎncă nu există evaluări
- Outcome of Children and Adolescents With A Second or Third Relapse of Acute Lymphoblastic Leukemia (ALL) A Population-Based Analysis of The Austrian ALL-BFM (Berlin-Frankfurt-Münster) Study GroupDocument5 paginiOutcome of Children and Adolescents With A Second or Third Relapse of Acute Lymphoblastic Leukemia (ALL) A Population-Based Analysis of The Austrian ALL-BFM (Berlin-Frankfurt-Münster) Study GrouphawinnurdianaÎncă nu există evaluări
- Factors Influencing Survival After Relapse From Acute Lymphoblas-Tic Leukemia A Children's Oncology Group StudyDocument9 paginiFactors Influencing Survival After Relapse From Acute Lymphoblas-Tic Leukemia A Children's Oncology Group StudyhawinnurdianaÎncă nu există evaluări
- Outcome After First Relapse in Children With Acute Lym-Phoblastic Leukemia A Report Based On The Dutch Child-Hood Oncology Group (DCOG) Relapse All 98 ProtocolDocument7 paginiOutcome After First Relapse in Children With Acute Lym-Phoblastic Leukemia A Report Based On The Dutch Child-Hood Oncology Group (DCOG) Relapse All 98 ProtocolhawinnurdianaÎncă nu există evaluări
- Sexually Transmitted Diseases - CDCDocument116 paginiSexually Transmitted Diseases - CDCAnthony GómezÎncă nu există evaluări
- Adverse Effects of Treatment in Childhood Acute Lymphoblastic Leukemia General Overview and Implications For Long-Term Cardiac Health.Document21 paginiAdverse Effects of Treatment in Childhood Acute Lymphoblastic Leukemia General Overview and Implications For Long-Term Cardiac Health.hawinnurdianaÎncă nu există evaluări
- Acute and Long-Term Neurological Complications in Children With Acute Lymphoblastic LeukemiaDocument4 paginiAcute and Long-Term Neurological Complications in Children With Acute Lymphoblastic LeukemiahawinnurdianaÎncă nu există evaluări
- PCPDocument6 paginiPCPhawinnurdianaÎncă nu există evaluări
- Acute Lymphoblastic LeukemiaDocument30 paginiAcute Lymphoblastic LeukemiaHarancang Kahayana0% (1)
- Cervical LymphadenopathyDocument12 paginiCervical LymphadenopathyhawinnurdianaÎncă nu există evaluări
- HD Vs Crrt-cd003773Document53 paginiHD Vs Crrt-cd003773hawinnurdianaÎncă nu există evaluări
- Leukemia and Nervous System PDFDocument25 paginiLeukemia and Nervous System PDFhawinnurdianaÎncă nu există evaluări
- Leukemia and Nervous System PDFDocument25 paginiLeukemia and Nervous System PDFhawinnurdianaÎncă nu există evaluări
- CRRTDocument12 paginiCRRThawinnurdianaÎncă nu există evaluări
- What Is Acute Lymphocytic Leukemia?Document21 paginiWhat Is Acute Lymphocytic Leukemia?hawinnurdianaÎncă nu există evaluări
- Leukemia and Nervous System PDFDocument25 paginiLeukemia and Nervous System PDFhawinnurdianaÎncă nu există evaluări
- Diagnosis EntamoebaDocument2 paginiDiagnosis EntamoebaElsya ApriliaÎncă nu există evaluări
- Review of 100 Cases of Intestinal Amoebiasis in SwatDocument4 paginiReview of 100 Cases of Intestinal Amoebiasis in SwathawinnurdianaÎncă nu există evaluări
- The Liver in Pediatric Gastrointestinal Disease.4Document12 paginiThe Liver in Pediatric Gastrointestinal Disease.4hawinnurdianaÎncă nu există evaluări
- Encefalopatia HepaticaDocument11 paginiEncefalopatia HepaticahawinnurdianaÎncă nu există evaluări
- Ventilator Associated PneumonoaDocument3 paginiVentilator Associated PneumonoahawinnurdianaÎncă nu există evaluări
- Ventilator Associated Pneumonia and GuidelinesDocument28 paginiVentilator Associated Pneumonia and GuidelineshawinnurdianaÎncă nu există evaluări
- Co AmoxyclavDocument2 paginiCo AmoxyclavHaneulÎncă nu există evaluări
- Opioid Pharmacology: Pain Management and OpioidsDocument7 paginiOpioid Pharmacology: Pain Management and Opioidsslatcheshotmail.comÎncă nu există evaluări
- Guaifenesin and Dextromethorphan 01Document7 paginiGuaifenesin and Dextromethorphan 01not perfectÎncă nu există evaluări
- BHPDocument1 paginăBHPMuhammad YanieÎncă nu există evaluări
- Annex A - Ped 028 Fitness ProgramDocument2 paginiAnnex A - Ped 028 Fitness ProgramMiguel BautistaÎncă nu există evaluări
- The Efficacy of Platelet-Rich Plasma in The Field of Hair Restoration and Facial Aesthetics A Systematic Review and MetaanalysisDocument19 paginiThe Efficacy of Platelet-Rich Plasma in The Field of Hair Restoration and Facial Aesthetics A Systematic Review and MetaanalysisMariska Regina RannuÎncă nu există evaluări
- 97 Manufacturer of Medicine and DrugsDocument16 pagini97 Manufacturer of Medicine and DrugsHaroon Ur'Rashid100% (1)
- Molecules: Controlled Drug Delivery Systems: Current Status and Future DirectionsDocument45 paginiMolecules: Controlled Drug Delivery Systems: Current Status and Future DirectionsshivaniÎncă nu există evaluări
- Prostate Disease Management GuideDocument2 paginiProstate Disease Management GuidePrabha Amandari SutyandiÎncă nu există evaluări
- DECAL LNH Refrac JCO 2001Document7 paginiDECAL LNH Refrac JCO 2001sunrasta23Încă nu există evaluări
- Sample Pharmacist Manager ResumeDocument7 paginiSample Pharmacist Manager Resumemarko2606Încă nu există evaluări
- Question 1Document25 paginiQuestion 1Anonymous 1T0qSzPt1PÎncă nu există evaluări
- Daftar Harga Mpi All Product Agt 18 PDFDocument133 paginiDaftar Harga Mpi All Product Agt 18 PDFAulia mulidaÎncă nu există evaluări
- Introduction To Pharmacognosy and Scope of PharmacognosyDocument8 paginiIntroduction To Pharmacognosy and Scope of PharmacognosyabdullahÎncă nu există evaluări
- Clinical PharmacokineticsDocument26 paginiClinical PharmacokineticsNiki Rizqi rachmawatiÎncă nu există evaluări
- Droguri de StradaDocument13 paginiDroguri de StradaIon VirtosuÎncă nu există evaluări
- Jurna NuromolDocument6 paginiJurna NuromolFriedrick VecchioÎncă nu există evaluări
- Salbuterol Generic NameDocument4 paginiSalbuterol Generic NamejunieÎncă nu există evaluări
- UPDATE STOCK ALL Gudang 10.12.22Document20 paginiUPDATE STOCK ALL Gudang 10.12.22Reza AryfÎncă nu există evaluări
- Towards Fast AI-Infused Human-Centered ContouringDocument77 paginiTowards Fast AI-Infused Human-Centered ContouringParakhModyÎncă nu există evaluări
- FDA Drug ShortagesDocument8 paginiFDA Drug ShortagesWDIV NewsOpsÎncă nu există evaluări
- Anesthesia For Healthy Rabbits - Veterinary Anesthesia Update - VINDocument8 paginiAnesthesia For Healthy Rabbits - Veterinary Anesthesia Update - VINCristian FloreaÎncă nu există evaluări
- Article WJPR 1467266667Document10 paginiArticle WJPR 1467266667Atthapu ThirupathaiahÎncă nu există evaluări
- Lesson Plan 5 Medicine LabelDocument35 paginiLesson Plan 5 Medicine Labelnta tiekaÎncă nu există evaluări
- Basic Pharmacology: NTA Level 4 Semester 2Document23 paginiBasic Pharmacology: NTA Level 4 Semester 2MabusiÎncă nu există evaluări
- ATC DDD 2011guidelinesDocument286 paginiATC DDD 2011guidelinesEnrique Jorge Herrera VasquezÎncă nu există evaluări
- Original Article: BackgroundDocument4 paginiOriginal Article: BackgroundYuni IHÎncă nu există evaluări
- Manufacturing ProspectsDocument4 paginiManufacturing Prospectspushpanjali singhÎncă nu există evaluări