Documente Academic
Documente Profesional
Documente Cultură
2015 - XIV - 3 - The Assessment of Periodontal Lesions Using CBCT
Încărcat de
Simion IulianTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
2015 - XIV - 3 - The Assessment of Periodontal Lesions Using CBCT
Încărcat de
Simion IulianDrepturi de autor:
Formate disponibile
See
discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/286441998
THE ASSESSEMENT OF PERIODONTAL LESIONS
USING CBCT
Article January 2015
CITATIONS
READS
24
6 authors, including:
Ana Gabriela Benghiac
Danisia Haba
Universitatea de Medicina si Farmacie Grigor
Universitatea de Medicina si Farmacie Grigor
16 PUBLICATIONS 9 CITATIONS
55 PUBLICATIONS 116 CITATIONS
SEE PROFILE
SEE PROFILE
All content following this page was uploaded by Ana Gabriela Benghiac on 10 December 2015.
The user has requested enhancement of the downloaded file. All in-text references underlined in blue are added to the original document
and are linked to publications on ResearchGate, letting you access and read them immediately.
Revista Romn de Anatomie funcional i clinic, macro- i microscopic i de Antropologie
Vol. XIV Nr. 3 2015
CLINICAL ANATOMY
THE ASSESSEMENT OF PERIODONTAL
LESIONS USING CBCT
Alexandra Dumitrescu1, Ana Gabriela Benghiac1, I. Salamastrakis1, M.S.C. Haba2,
I.V. Simion2, Danisia Haba3
Gr.T. Popa University of Medicine and Pharmacy, Iai
1. PhD Student
2. Student
3. Oral and Maxillofacial Department
THE ASSESSEMENT OF PERIODONTAL LESIONS USING CBCT (Abstract): This article
aims at highlighting the role of CBCT in the assessment of the periodontal disease, a chronic
condition which is more common in current practice lately, and with multiple implications in the
oral cavity. We analyzed the presence of periodontal lesions using CBCT, in three planes, at a
total of three patients. The patients presented at the radiology center to take craniofacial CBCTs.
CBCT increases the certainty of diagnosis and treatment of periodontal diseases compared to
conventional methods, classical or digital dental radiography. So, as long as we can get appropriate diagnosis, the therapeutic plan will be handled better, implicitly entailing an excellent prognosis of treatment. Key words: CBCT, PERIODONTAL DISEASE, ALVEOLAR RESORPTION
INTRODUCTION
Periodontal disease is a chronic inflammatory disease caused by the invasion of anaerobic
bacteria and spirochaetes in the periodontal
space, including the gingival tissue, the periodontal ligament, the alveolar bone and can lead
to tooth loss and impaired oral functions. Periodontal disease diagnosis is mostly based on
signs and clinical symptoms, however when it
comes to bone resorption, radiography remains
the most conclusive investigation (1,2). Panoramic radiographs are often used to diagnose
alveolar resorption in periodontal disease, achieving a 2D image of several 3D structures and
presenting a number of disadvantages, among
which: underestimation of bone loss, difficult
identification of certain anatomical points and
overlap of adjacent anatomical structures, projection geometry, thus creating an image with
a non-high degree of accuracy; therefore, in
order to eliminate these shortcomings, CBCT
shall be used (1,3). Three-dimensional imaging
created by CBCT allows a better diagnosis,
treatment planning and monitoring, as well as
a better analysis of results, compared to conventional two-dimensional images. Due to this
new revolutionary imaging technology, we can
now create and interact with virtual models of
tooth and jaw structures of patients, fact which
allows us to offer an improved treatment compared to the previous options (4).
Cone Beam Computed Tomography (CBCT)
is one of the latest technologies in the field of
imaging which allows the three-dimensional
view of scanned areas. Using an X-ray cone
beam, the CBCT scanner needs a single rotation around the patient to take hundreds of
pictures of the area of interest, which are then
reconstructed using an imaging software in order to obtain a 3D virtual model of the patient.
The entire procedure is very short (5,6,7,8).
Several studies proved that CBCT presents
some advantages compared to other radiological investigation methods, and compared to CT,
the CBCT image shows a superior quality, reproducibility and validity and a much lower
exposure to radiation. These studies have concluded that CBCT is useful in the maxillofacial
483
Alexandra Dumitrescu et al.
Fig. 1. CBCT. Panoramic reconstruction plays severe periodontal lesions. Surrounding bone is sclerotic
and teeth appear as floating in air, the contour is deleted, irregular and lamina dura is missing.
Fig. 2. CBCT.Paraxial reconstruction- deep alveolar bone loss on the mandibular molar;
the molar appears as floating in air.
Fig. 3. CBCT. 3D Reconstruction osteodistruction of the alveolar bone,
teeth are like floating in the air.
area, especially for the evaluation of bone tissue; instead, images are not the desired ones
when it comes to injuries of the soft tissue (9).
In terms of irradiation dose, studies have found
that the radiation dose for CBCT is much lower
compared to a conventional CT, but increased
when compared to a panoramic x-ray (1,9).
CBCT gives the possibility of choosing the field
of view, depending on the area of interest, and
thus the area exposed to radiation is a single
one, the others areas being safe, and finally this
function is considered to be very important for
484
the patient because radiation dose will be low
(7,9).
CBCT can be used in the field of periodontology in: diagnosis of craters, furcation and
bone defects, in the assessment of the periodontal bone level and in the assessment of
continuity of lamina dura (1,6,10,11). Former
studies have shown that CT may render a clear
and precise image in case of periodontal bone
height and bone defects, but this can sometimes be unjustified by the high degree of irradiation (9).
The Assessement of Periodontal Lesions Using CBCT
Fig. 4. CBCT. Panoramic reconstruction- alveolar bone loss on the maxillar and mandibular area;
deep vertical bone resorption around 1.1, widening desmodontal space; deep horizontal resorption at
1.4,1.5; intraosseous lesions at 2.4,2.5; vertical bone resorption on surface of the first mandibular
molar; approximal septal defect in the third cadran on 3.6
Fig. 5. CBCT. Sagital reconstruction- Deep vertical bone resorption around 1.1,
widening desmodontal space marked with vestibular cortical thinning and discontinuity.
Fig. 6. CBCT. Paraxial reconstruction- deep horizontal resorption at 1.4,1.5
METHODOLOGY
The CBCT were obtained from the database
of the MedImagis private dental radiology clinic from Iasi, from three patients who made the
CBCT for investigations in the maxillofacial
area. The CBCT were achieved with Planmeca
3D MID and the evaluation of the periodontal
lesions was made with the softwear Romexis
3.6.0. Image density and contrast were adjusted digitaly for easy viewing. The CBCT
obtained were analized twice. The analises was
performed in a quiet environment with adecvate
485
Alexandra Dumitrescu et al.
Fig. 7. CBCT. Paraxial reconstruction-intraosseous lesions with two walls at 2.4,2.5
Fig. 8. CBCT. Paraxial reconstruction- performed using CBCT show a vertical bone resorption
on surface of the first mandibular molar
Fig. 9. CBCT. 3D reconstruction - alveolar bone loss in 1 and 4 cadran
lighting and was evaluated in three spatial
planes: coronal, sagittal axial and 3D reconstruction.
Case 1: A.V, 60 years old, male patient
who admit using CBCT scan using the following acquisition protocol; the exposure date was
3.06.2014, the image size is 458x458x458mm,
kV 90, mA 12, the voxel size 400 and the exposure time 13.817 s.
Case 2: A. I, 36 years old, male patient
who admit CBCT scan using the following protocol acquisitions: the exposure date was
11.10.2014, the image size is 505x505x434mm,
486
90 kV, 10 mA, voxel size 400, and the exposure
time 13.904s, DAP(mGyxcm)- 2490.
Case 3: I. M, 39 years old, female patient,
who admit CBCT scan using the following acquisition protocol: the exposure date was
4.10.2014, the image size is 452x452x447mm,
90 kV, 12 mA, voxel size 400, with an exposure
time 13.907s and DAP(mGyxcm)- 2964.
CONCLUSION
To conclude, CBCT is successfully used in
the investigation of periodontal disease, bringing multiple benefits, and it should also be used
The Assessement of Periodontal Lesions Using CBCT
Fig. 10. CBCT. Panoramic reconstruction-Chronic inflammation of the mucous reveals at right maxillary sinus in the lower 1/3 of dental origin without sinus ostium obstruction. Intrasinusal chronic
inflammatory lesion is possible due to chronic periodontal lesion 1.8. which has a much larger desmodontal spatial-looking pockets wich is thinning the cortical, and with discontinuity of sinus recession;
alveolar bone resorption on the 1.8, 1.6, 1.5 and 1.7 is absent; alveolar bone resorption on the second
cadran and furcation on 2.6,2.7; in the fourth cadran alveolar bone loss on vestibular and lingual face
on the teeth 4.6, 4.7,4.8 with discret desmodontal widening; moderate retraction of periodontal edge
predominantly in the right vestibular 3.7 and 3.8 molar roots.
Fig. 11. CBCT. Paraxial reconstruction- Chronic periodontal lesion at the level
of 1.6 with vestibulo-palatal bone resorption and furcation.
Fig. 12. CBCT. Paraxial reconstruction- presents a significant retraction mainly
palatal of the dental ridge without widening desmodontal space, on 1.5.
487
Alexandra Dumitrescu et al.
Fig. 13. CBCT. Paraxial reconstruction- Vestibular and palatal bone resorption
mainly with furcation on the tooth 2.6.
Fig. 14. CBCT. 3D Reconstruction- Vestibular and palatal bone resorption mainly
with furcation on the tooth 2.6, 2.7. Moderate retraction of periodontal edge predominantly
in the right vestibular 3.7 and 3.8 molar roots.
whenever the standard 2D x-ray may not provide the necessary information for dentist to
establish the diagnosis and the optimal treatment plan. CBCT diagnosis can give accurate
information on bone status and bone defects,
and injuries of furcation and craters appear to
be better represented. Yet, since the radiation
dose is higher than other radiological investigations, the choice of CBCT as a radiological
investigation must be justified and must have
an increased benefit for the patient, compared
to risks (6,12,13). Information about the CBCT
is still new to many medical specialties and due
to its importance and usefulness, it has to be
developed with the help of courses and research.
ACKNOWLEDGEMENTS
This paper received financial support by the
project Programme of excellence in doctoral
and postdoctoral multidisciplinary research in
chronic diseases, Grant No. POSDRU/
159/1.5/S/133377, project co-financed by Sectorial Operational Programme of Human Resources Development, financed from the European Social Fund.
REFERENCES
1. Buket A, Kivan K. Use of come beam computed tomography in periodontology. World J Radiol 2014;
6(5): 139-147
2. Jurgina S, Alvydas G, Astra V, Egle I, Victoras S. Relationship of clinical and microbiological variables in patients with type 1 diabetes mellitus and periodontitis. Med SciMonit, 2014; 20: 1871-1877
3. Mol A. Imaging methods in periodontology. Periodontology 2000, vol. 34, pp. 3448, 2004
4. Ion B.T.G. Modularea raspunsului imun cu vaccin stafilococic in boala parodontala, 2005
5. http://www.planmeca.com/en/imaging/3D-imaging/quality-imaging-with-low-dose
6. Yousef AA. Diagnostic Applications of one beam CT of periodontal diseases. IJD 2014
7. http://www.eadmfr.info
8. http://en.wikipedia.org/wiki/Cone_beam_computed_tomography
9. Shawn A, Wenjian Z, Tom Z, Paula N.ONeill. Cone beam computed tomography in dentistry: what
dental educators and learners should know. J Dent Educ 2012
488
The Assessement of Periodontal Lesions Using CBCT
10. Noujeim M, Prihoda T.J, Langlais R, and Nummikoski P. Evaluation of high-resolution cone beam
computed tomography in the detection of simulated interradicular bone lesion. DMFR vol. 38, no. 3,
pp. 156162, 2009
11. Leung C.C, Palomo L, Griffith R, and Hans M.G. Accuracy and reliability of cone-beam computed
tomography for measuring alveolar bone height and detecting bony dehiscences and fenestrations.
AJO-DO vol. 137, supplement 4, pp. S109S119, 2010
12. Vandenberghe B, Jacobs R, and Yang J. Detection of periodontal bone loss using digital intraoral and
cone beamcomputed tomography images: an in vitro assessment of bony and/or infrabony defects.
DMFR, vol. 37, no. 5, pp. 252260, 2008
13. Sedentex project. Radiation protection: Cone Beam CT for dental and maxillofacial radiology 20082011
Corresponding author
Fochi (Dumitrescu) Maria Alexandra
e-mail: fo_ale@yahoo.com
489
View publication stats
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- William S. Breitbart - Meaning-Centered Psychotherapy in The Cancer Setting - Finding Meaning and Hope in The Face of Suffering (2017, Oxford University Press)Document425 paginiWilliam S. Breitbart - Meaning-Centered Psychotherapy in The Cancer Setting - Finding Meaning and Hope in The Face of Suffering (2017, Oxford University Press)Nicole Marie-Madeleine Alberto100% (2)
- CT & MRI Pathology: A Pocket AtlasDocument570 paginiCT & MRI Pathology: A Pocket AtlasIvraym Barsoum100% (7)
- Role of Digital Image Processing in Telemedicine PDFDocument3 paginiRole of Digital Image Processing in Telemedicine PDFSimion IulianÎncă nu există evaluări
- GTR nc190 PDFDocument653 paginiGTR nc190 PDFSimion IulianÎncă nu există evaluări
- Scrapie Sheep: - A Disease ofDocument6 paginiScrapie Sheep: - A Disease ofSimion IulianÎncă nu există evaluări
- Owls Strigiformes - Annotated - and - Illustrated - Checklist PDFDocument371 paginiOwls Strigiformes - Annotated - and - Illustrated - Checklist PDFSimion IulianÎncă nu există evaluări
- CT and MRI Findings in Neoplasms of The Oral Cavity and OropharynxDocument2 paginiCT and MRI Findings in Neoplasms of The Oral Cavity and OropharynxSimion IulianÎncă nu există evaluări
- Anaesthesia For Vet Technicians-355finalDocument417 paginiAnaesthesia For Vet Technicians-355finalSimion IulianÎncă nu există evaluări
- Schult, Schlitt Use of Interdental...Document9 paginiSchult, Schlitt Use of Interdental...Simion IulianÎncă nu există evaluări
- Hem BiochDocument44 paginiHem BiochJonathan JohnsonÎncă nu există evaluări
- IADMFRv43n1 PDFDocument15 paginiIADMFRv43n1 PDFSimion IulianÎncă nu există evaluări
- Neuroimaging Clinics - Imaging of Head TraumaDocument184 paginiNeuroimaging Clinics - Imaging of Head TraumaSimion Iulian100% (1)
- Role of Digital Image in TelemedicineDocument8 paginiRole of Digital Image in TelemedicineSimion IulianÎncă nu există evaluări
- Organize System HealthcareDocument167 paginiOrganize System HealthcarePranav JainÎncă nu există evaluări
- CBCT - Tomografia Volumetrica DentaraDocument59 paginiCBCT - Tomografia Volumetrica DentaraSimion IulianÎncă nu există evaluări
- Ghid TromboembolismDocument40 paginiGhid TromboembolismSimion IulianÎncă nu există evaluări
- Blaylock Forced0415 130Document13 paginiBlaylock Forced0415 130RAMO STEF SZEKERESÎncă nu există evaluări
- (Lecture 4) Vice, Drug Education and ControlDocument25 pagini(Lecture 4) Vice, Drug Education and ControlJohnpatrick DejesusÎncă nu există evaluări
- Edwards Hemodynamic Monitoring For COVID Critically Ill PatientsDocument3 paginiEdwards Hemodynamic Monitoring For COVID Critically Ill PatientsblanquishemÎncă nu există evaluări
- SedativesDocument4 paginiSedativesalghashm001Încă nu există evaluări
- Tabel Severitas BPJS Tindakan JantungDocument9 paginiTabel Severitas BPJS Tindakan JantungTeduh ParamadinaÎncă nu există evaluări
- PARM LBP CPG 2nd Edition 2017 PDFDocument293 paginiPARM LBP CPG 2nd Edition 2017 PDFGumDropÎncă nu există evaluări
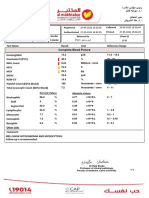
- Complete Blood Picture: 60 Year Female 23321506381Document3 paginiComplete Blood Picture: 60 Year Female 23321506381SilavioÎncă nu există evaluări
- PreparateDocument2 paginiPreparateVasile LozinschiiÎncă nu există evaluări
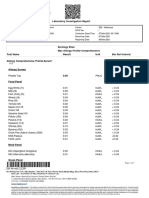
- Laboratory Investigation ReportDocument7 paginiLaboratory Investigation ReportAmarjeetÎncă nu există evaluări
- Medicinal PlantsDocument5 paginiMedicinal PlantszÎncă nu există evaluări
- General Examination For CVSDocument29 paginiGeneral Examination For CVSstudymedic100% (1)
- Management of Acute Glomerulonephritis in Children: Children's Services Medical GuidelinesDocument7 paginiManagement of Acute Glomerulonephritis in Children: Children's Services Medical GuidelinesdaypranitaÎncă nu există evaluări
- Pediatric AnesthesiaDocument70 paginiPediatric AnesthesiaEliyan KhanimovÎncă nu există evaluări
- Can Mung Beans Cause GoutDocument1 paginăCan Mung Beans Cause GoutAINA NAJWA BINTI ABDULLAH MoeÎncă nu există evaluări
- European University of Lefke: Eczacılık Fakültesi / Faculty of PharmacyDocument3 paginiEuropean University of Lefke: Eczacılık Fakültesi / Faculty of PharmacyMariem Ben HediaÎncă nu există evaluări
- Healing Sciatica Using The Feldenkrais MethodDocument1 paginăHealing Sciatica Using The Feldenkrais MethodLiviu CasuneanuÎncă nu există evaluări
- New Techniques in Chelonian Shell RepairDocument8 paginiNew Techniques in Chelonian Shell RepairChecko LatteÎncă nu există evaluări
- Practice Worksheet Class XiiDocument7 paginiPractice Worksheet Class XiiManjusha NayakÎncă nu există evaluări
- JednjakDocument15 paginiJednjakbojana1994Încă nu există evaluări
- Introduction To Cerebral Palsy 2022Document53 paginiIntroduction To Cerebral Palsy 2022Namakau MuliloÎncă nu există evaluări
- Differential Diagnostic by P'nutDocument141 paginiDifferential Diagnostic by P'nutRotate E100% (1)
- Brody Hall - Exercício Terapêutico Na Busca Da Função, 3 Ed, 2011 (Inglês)Document802 paginiBrody Hall - Exercício Terapêutico Na Busca Da Função, 3 Ed, 2011 (Inglês)SerenelaÎncă nu există evaluări
- Qualities of A Good Doctor 1209062789925412 9Document64 paginiQualities of A Good Doctor 1209062789925412 9Yus Ani100% (1)
- Ethnomedicine and Drug Discovery PDFDocument2 paginiEthnomedicine and Drug Discovery PDFJohn0% (1)
- 307-Article Text-578-1-10-20210309 PDFDocument13 pagini307-Article Text-578-1-10-20210309 PDFPUTRI LISTIANIÎncă nu există evaluări
- Muir's Textbook of Pathology 15e KulitDocument35 paginiMuir's Textbook of Pathology 15e Kulitputri theresiaÎncă nu există evaluări
- 01-2020 - Tactical Emergency Casualty Care (TECC)Document5 pagini01-2020 - Tactical Emergency Casualty Care (TECC)pibulinÎncă nu există evaluări
- Group 5 - Case Study Presentation PDFDocument7 paginiGroup 5 - Case Study Presentation PDFAkash HalsanaÎncă nu există evaluări
- Paper 1Document11 paginiPaper 1api-499574410Încă nu există evaluări