Documente Academic
Documente Profesional
Documente Cultură
Respiratory Self-Study Questions With Answers
Încărcat de
Abhineeth BhatDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Respiratory Self-Study Questions With Answers
Încărcat de
Abhineeth BhatDrepturi de autor:
Formate disponibile
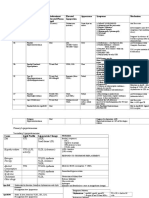
Self-Study Questions for the Respiratory Pathophysiology Unit
1. What determines FRC (functional residual capacity)?
page 14 of syllabus, section V. at the bottom of the page
2. Name at least three factors that can reduce airway resistance.
page 22, top of page under D.
3. List at least two factors that can shift the oxygen hemoglobin desaturation curve to the
LEFT.
page 40, figure 2
4. Calculate the alveolar-arterial oxygen gradient for a patient with the following set of arterial
blood gases: pH 7.08; PaCO2 80; PaO2 40; HCO3- 24.
page 37
5. What is your interpretation of the following arterial blood gas: pH 7.08; PaCO2 80; PaO2 40;
HCO3- 24?
page 45, top sections
6. Which of the following types of pulmonary vessels (arterial, venous &/or lymphatic) is/are
found in the connective tissue adjacent to airways?
arterial (bronchial and pulmonary) and lymphatics
7. Name at least two major differences between the histology of bronchi and bronchioles.
bronchi have plates of hyaline cartilage and submucosal glands; bronchioles don't
8. List at least three differences between the pathology of centrilobular and panlobular
emphysema.
centrilobular emphysema involves the center of the lobules to a greater extent, as
opposed to being distributed uniformly throughout the lobules
centrilobular emphysema is more severe in the upper lobes; panlobular emphysema is
more severe in the lower lobes
centrilobular emphysema usually has significant accompanying anthracosis; panlobular
emphysema, if caused by alpha1-antitrypsin deficiency alone, does not
Self-Study Questions for the Respiratory Pathophysiology Unit
Page 2
9. Name at least two similarities and two differences between the microscopic pathology of
chronic bronchitis and asthma.
similarities: airways with smooth muscle hyperplasia, inflammation and edema,
increased mucus production
differences: inflammation in asthma typically has a prominent infiltrate of eosinophils,
whereas chronic bronchitis usually has just "generic" acute and chronic inflammatory
cells; asthma has sub-basement membrane fibrosis, which is not present in chronic
bronchitis
10. What features would make you consider a diagnosis of cystic fibrosis rather than immotile
cilia syndrome in a 9 year-old child?
thick mucus; high sweat chloride; multiorgan involvement, especially pancreas; sputum
cultures growing resistant Pseudomonas
11. Why does infant respiratory distress syndrome potentially lead to pulmonary hypertension?
hypoxia pulmonary vasoconstriction vessel remodeling pulmonary hypertension
right heart strain and failure
12. List one diagnosis associated with each of the five classes of pulmonary hypertension.
pages 116-118
13. Name at least two risk factors for pulmonary thromboembolism.
page 126
14. Define paradoxical thromboembolism.
a deep venous thrombus gains access to the systemic circulation via an opening
between the right and left sides of the heart (e.g., ASD, VSD, patent foramen ovale)
15. Name an anticoagulant drug which does NOT depend on renal function for elimination.
argatroban
16. How do you monitor warfarin (Coumadin) for effectiveness?
INR
17. What laboratory tests on pleural fluid would indicate the fluid is a transudate? Why is it
important to distinguish a transudate from an exudate?
low protein and LDH; transudates are managed by treating the underlying condition
Self-Study Questions for the Respiratory Pathophysiology Unit
Page 3
18. If the majority of cells found in pleural fluid are lymphocytes, what disease(s) would you be
considering?
tuberculosis and malignancy
19. Describe the main differences between simple and complicated coal workers'
pneumoconiosis.
simple CWP is characterized by scattered small coal macules or nodules without
significant fibrosis; complicated CWP is characterized by large accumulations of carbon
pigment with significant fibrosis, leading to complications such as pulmonary
hypertension
20. The function of which pulmonary cell type is severely impaired in individuals with silicosis?
macrophage
21. List two important functions of
the cell type indicated by the arrows
in this photomicrograph of injured
lung.
type II pneumocytes produce surfactant
and are the regenerative cell type capable
of differentiating into both type I and II
pneumocytes after lung injury
22. What are some clinical clues that a patient is likely to have bacterial pneumonia rather than
just a bad cold?
top of page 215
23. Why does the absence of a spleen increase the risk for the development of Streptococcus
pneumoniae pneumonia?
The spleen puts opsonins on encapsulated bacteria making it easier for macrophages to
recognize and engulf them; with no spleen, no opsonins
Self-Study Questions for the Respiratory Pathophysiology Unit
Page 4
24. For the three major fungal pulmonary infectious diseases that can affect immunocompetent
individuals (blastomycosis, coccidioidomycosis and histoplasmosis), describe the areas in the
U.S. where these diseases are endemic, as well as the characteristic microscopic morphology
of the pathogenic organisms.
blastomycosis southeastern and central U.S.; large, broad-based budding yeasts at
body temperature
coccidioidomycosis western and southwestern U.S.; spherules with endospores at
body temperature
histoplasmosis Ohio and Mississippi river valleys; tiny, intracellular yeast at body
temperature
all 3 are dimorphic fungi, so are present as much more hardy forms (conidia) in the soil
25. Name at least three conditions which increase the risk for progression from latent
tuberculosis infection (LTBI) to active tuberculosis (TB disease).
top of page 230
26. If a patient is not doing well on a 4-drug treatment regimen for tuberculosis, what would be
the problem in adding a 5th drug to help?
page 232
27. Why do we start therapy for tuberculosis with 3-4 drugs?
page 232
28. What pathology MOST supports a diagnosis of idiopathic pulmonary fibrosis?
fibroblastic foci; heterogeneous pathology worse at the lung bases and under the pleura
29. Which of the idiopathic interstitial lung diseases have a strong association with smoking?
desquamative interstital pneumonitis (DIP), pulmonary Langerhans cell histiocytosis
idiopathic pulmonary fibrosis also has an association with smoking, but not as strong as
the two above
30. If a 30 year-old African American woman presents to your office with exertional dyspnea and
a dry cough, has a moderate restrictive defect on pulmonary function testing and has a chest Xray showing bilateral hilar lymphadenopathy, you would be able to guess the diagnosis. So why
would you need a biopsy?
rule out infection or malignancy before starting therapy for sarcoidosis
Self-Study Questions for the Respiratory Pathophysiology Unit
Page 5
31. List at least three non-infectious causes of granulomatous inflammation in the lung.
sarcoidosis, berylliosis, hypersensitivity pneumonitis
32. What factors would lead you to believe that a patient with suspected idiopathic pulmonary
fibrosis would NOT need an open lung biopsy?
classic high resolution CT findings in the appropriate clinical setting
33. What is the most common mechanism causing hypoxemia?
V/Q mismatch
34. When evaluating a patient, what factors might lead you to start mechanical (or assisted)
ventilation?
page 321, middle of page
35. For which cell type of lung cancer would you most likely expect hemoptysis (coughing up
blood)?
squamous cell carcinoma more locally destructive malignancy that usually erodes into
the central airways; remember that it can also cavitate
another important concept (which may not have been emphasized) is that there is one
paraneoplastic syndrome more commonly seen with squamous cell carcinoma than with
small cell carcinoma; this is ectopic secretion of PTHrP, which can produce
hypercalcemia
36. Compare and contrast the development of squamous cell carcinoma and adenocarcinoma
of the lung from normal epithelium to premalignant lesions to an invasive malignancy.
squamous cell carcinoma: pseudostratified ciliated columnar epithelium undergoes
squamous metaplasia as a result of chronic injury due to irritants (e.g., in cigarette
smoke)
then with exposure to numerous chemical carcinogens (initiators and promoters) in
cigarette smoke, squamous metaplasia may develop into progressively more severe
squamous dysplasia
with subsequent genetic abnormalities, the severely dysplastic squamous epithelial cells
can develop the ability to invade and progress to invasive squamous cell carcinoma
adenocarcinoma: with carcinogenic exposures, normal distal airway and alveolar
epithelium (which is glandular) can develop into atypical adenomatous hyperplasia (an
incidental finding)
with further genetic abnormalities, this can progress into adenocarcinoma in situ and
then ultimately into invasive adenocarcinoma
Self-Study Questions for the Respiratory Pathophysiology Unit
Page 6
37. How does a pathologist distinguish between a typical carcinoid tumor and small cell lung
carcinoma?
macroscopically, a typical carcinoid is usually well-defined, as opposed to the infiltrating
growth pattern of small cell carcinoma (often adjacent to airways as was discussed
yesterday)
microscopically, similarities between the two include the fact that they both have the
characteristic "salt and pepper" chromatin pattern of neuroendocrine cells, and both are
highly vascular
however, after that, their histologic appearance diverges; a typical carcinoid is
composed of a monotonous population of neuroendocrine cells with regular round
nuclei and more cytoplasm than is typical of small cell carcinoma; in addition, cytologic
atypia and mitotic figures are absent
small cell carcinoma is comprised of neuroendocrine cells with very scanty cytoplasm,
that frequently mold to one another; there is evidence of a high proliferative rate (e.g.,
mitotic figures, tumor cell necrosis), as well as cellular fragility (smeared DNA producing
the fairly reproducible crush artifact)
38. Who should be screened for lung cancer based on the National Lung Screening Trial?
smokers age 55-77, still within 15 years of quitting, 30 pack year smoking history
39. What is the clinical relevance of the long latency period for lung cancer (from the first
malignant cell to clinical manifestations)?
diagnosis is late
40. Define what is meant by a paraneoplastic syndrome and provide at least three examples.
signs/symptoms occurring in a minority of patients with malignancies that cannot be
attributed to tumor growth and spread or endogenous hormone synthesis
examples include tumor cell production of procoagulants or ectopic hormones (e.g.,
small cell carcinoma producing ACTH or ADH; squamous cell carcinoma producing
PTHrP)
other examples include cross-reacting immune responses between tumor cell antigens
and normal tissue components (e.g., Lambert-Eaton myasthenic syndrome, cerebellar
degeneration)
41. How can you differentiate non-REM from REM sleep?
pages 334-335
Self-Study Questions for the Respiratory Pathophysiology Unit
Page 7
42. Name at least one Dont of good sleep hygiene which you yourself are guilty of.
this is personal but check page 336 at the bottom
43. List at least three of the parameters monitored during a polysomnogram (sleep study).
page 338
44. List at least three causes of excessive daytime sleepiness.
obstructive sleep apnea, narcolepsy, inadequate sleep, poor sleep hygiene
45. What are the three changes in pulmonary mechanics that occur as people age?
page 352 I. A.
S-ar putea să vă placă și
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Jefferson - Aoa USMLE Step 1Document12 paginiJefferson - Aoa USMLE Step 1Mc Ase100% (1)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Usmle Hy Step1Document20 paginiUsmle Hy Step1Sindu SaiÎncă nu există evaluări
- Power Tube Biasing Operation Manual 15-01-08Document2 paginiPower Tube Biasing Operation Manual 15-01-08MitchÎncă nu există evaluări
- MATH8-Relations and Functions Worksheet AnswersDocument15 paginiMATH8-Relations and Functions Worksheet AnswersRhealyn Joy Narciso100% (2)
- Versant ModifiedDocument57 paginiVersant ModifiedAryan Kharadkar100% (3)
- STEP1 ResourcesDocument2 paginiSTEP1 ResourcesAbhineeth BhatÎncă nu există evaluări
- Policy For CCC Delayed Start StudentsDocument2 paginiPolicy For CCC Delayed Start StudentsAbhineeth BhatÎncă nu există evaluări
- Urinary Concentration and DilutionDocument10 paginiUrinary Concentration and DilutionAbhineeth BhatÎncă nu există evaluări
- Unit 2 Histo Study GuideDocument2 paginiUnit 2 Histo Study GuideAbhineeth BhatÎncă nu există evaluări
- Notion of Narrative Based On Whats Dominant in End of Life StoriesDocument1 paginăNotion of Narrative Based On Whats Dominant in End of Life StoriesAbhineeth BhatÎncă nu există evaluări
- GuideDocument16 paginiGuideAbhineeth BhatÎncă nu există evaluări
- Step 1 PlanDocument6 paginiStep 1 PlanUma MounaÎncă nu există evaluări
- Guide To BoardsDocument3 paginiGuide To BoardsAbhineeth BhatÎncă nu există evaluări
- Gi HyDocument2 paginiGi HyAbhineeth BhatÎncă nu există evaluări
- VocabDocument4 paginiVocabAbhineeth BhatÎncă nu există evaluări
- First SpeakerDocument2 paginiFirst SpeakerAbhineeth BhatÎncă nu există evaluări
- PathologyDocument54 paginiPathologyAli Abbas100% (8)
- DM2Document12 paginiDM2Abhineeth BhatÎncă nu există evaluări
- 2017 Fas1 Errata MarchDocument4 pagini2017 Fas1 Errata MarchФеденко ЭдуардÎncă nu există evaluări
- Guide PDDocument2 paginiGuide PDAbhineeth BhatÎncă nu există evaluări
- Wilhelm Endocrine PharmacologyDocument7 paginiWilhelm Endocrine PharmacologyAbhineeth BhatÎncă nu există evaluări
- Approved: HFHS Nov-June Only HFH Has No PrerequisitesDocument1 paginăApproved: HFHS Nov-June Only HFH Has No PrerequisitesAbhineeth BhatÎncă nu există evaluări
- Question PhilosophyDocument3 paginiQuestion PhilosophyAbhineeth BhatÎncă nu există evaluări
- LabDocument4 paginiLabAbhineeth BhatÎncă nu există evaluări
- Pharm - Endocrine - Anti-DiabeticsDocument1 paginăPharm - Endocrine - Anti-DiabeticsAbhineeth BhatÎncă nu există evaluări
- Lecture 2Document1 paginăLecture 2Abhineeth BhatÎncă nu există evaluări
- Lipoprotein Patterns and Associated ConditionsDocument4 paginiLipoprotein Patterns and Associated ConditionsAbhineeth BhatÎncă nu există evaluări
- GuideDocument1 paginăGuideAbhineeth BhatÎncă nu există evaluări
- GuideDocument1 paginăGuideAbhineeth BhatÎncă nu există evaluări
- Normal Parathyroid GlandsDocument30 paginiNormal Parathyroid GlandsAbhineeth BhatÎncă nu există evaluări
- PancreasDocument8 paginiPancreasAbhineeth BhatÎncă nu există evaluări
- Lipoprotein Patterns and Associated ConditionsDocument4 paginiLipoprotein Patterns and Associated ConditionsAbhineeth BhatÎncă nu există evaluări
- Aging and MenopauseDocument3 paginiAging and MenopauseAbhineeth BhatÎncă nu există evaluări
- Coloi Eeml Disease: Original ArticlesDocument67 paginiColoi Eeml Disease: Original ArticlesLuisAngelPonceTorresÎncă nu există evaluări
- D6528-07 ASTM Standard Consolidated Undrained Direct Simple Shear Testing of Cohesive SoilsDocument9 paginiD6528-07 ASTM Standard Consolidated Undrained Direct Simple Shear Testing of Cohesive SoilsDayana HernandezÎncă nu există evaluări
- Contact GRRSB Team for InquiriesDocument2 paginiContact GRRSB Team for Inquiriesmsis81Încă nu există evaluări
- Beckman DxI 800 Prolactin Assay Superiority for Monomeric ProlactinDocument5 paginiBeckman DxI 800 Prolactin Assay Superiority for Monomeric Prolactindoxy20Încă nu există evaluări
- Thank You For Taking The Week 3: Assignment 3. Week 3: Assignment 3Document3 paginiThank You For Taking The Week 3: Assignment 3. Week 3: Assignment 3DhivyaÎncă nu există evaluări
- Qualtrics Ebook Employee Lifecycle Feedback Apj - q8uL5iqE4wt2ReEuvbnIwfG4f5XuMyLtWvNFYuM5Document18 paginiQualtrics Ebook Employee Lifecycle Feedback Apj - q8uL5iqE4wt2ReEuvbnIwfG4f5XuMyLtWvNFYuM5RajÎncă nu există evaluări
- Edexcel A-Level Biology Experimental Design Marks Scheme (1) (Full Permission)Document16 paginiEdexcel A-Level Biology Experimental Design Marks Scheme (1) (Full Permission)FardeenKhanÎncă nu există evaluări
- LogiquidsDocument2 paginiLogiquidsAloma FonsecaÎncă nu există evaluări
- Abiotic and Biotic Factors DFDocument2 paginiAbiotic and Biotic Factors DFgiselleÎncă nu există evaluări
- Kerala Electricity Regulatory Commission Schedule of TariffDocument36 paginiKerala Electricity Regulatory Commission Schedule of TariffvjtheeeÎncă nu există evaluări
- The Baptismal Liturgy in The Easter Vigil According To The Sacramentary of Fulda (10th Century)Document7 paginiThe Baptismal Liturgy in The Easter Vigil According To The Sacramentary of Fulda (10th Century)Henry DonascoÎncă nu există evaluări
- CBSE Worksheet-01 Class - VI Science (The Living Organisms and Their Surroundings)Document3 paginiCBSE Worksheet-01 Class - VI Science (The Living Organisms and Their Surroundings)Ushma PunatarÎncă nu există evaluări
- LOGARITHMS, Exponentials & Logarithms From A-Level Maths TutorDocument1 paginăLOGARITHMS, Exponentials & Logarithms From A-Level Maths TutorHorizon 99Încă nu există evaluări
- Weber Grills - FinalDocument12 paginiWeber Grills - FinalDIVYANSHU SHEKHARÎncă nu există evaluări
- Termites and Microbial Biological Control StrategiesDocument30 paginiTermites and Microbial Biological Control StrategiesMuhammad QasimÎncă nu există evaluări
- Progressing Cavity Pump Overhaul GuideDocument5 paginiProgressing Cavity Pump Overhaul Guidesdsds-54Încă nu există evaluări
- Ca2Document8 paginiCa2ChandraÎncă nu există evaluări
- 2021 - Tet Purchase Behavior Report - INFOCUSDocument15 pagini2021 - Tet Purchase Behavior Report - INFOCUSGame AccountÎncă nu există evaluări
- OE Spec MTU16V4000DS2250 3B FC 50Hz 1 18Document6 paginiOE Spec MTU16V4000DS2250 3B FC 50Hz 1 18Rizki Heru HermawanÎncă nu există evaluări
- SDE1 V1 G2 H18 L P2 M8 - SpecificationsDocument1 paginăSDE1 V1 G2 H18 L P2 M8 - SpecificationsCleverson SoaresÎncă nu există evaluări
- Mahle KFWA MAIN Data SheetDocument4 paginiMahle KFWA MAIN Data SheetRudnikÎncă nu există evaluări
- Wirkungen FlechtenstoffeDocument21 paginiWirkungen FlechtenstoffeLogge UliÎncă nu există evaluări
- Tipologie Break in OutDocument17 paginiTipologie Break in OutGiorgio FantauzziÎncă nu există evaluări
- Datasheet Optris XI 410Document2 paginiDatasheet Optris XI 410davidaldamaÎncă nu există evaluări
- Workload Assessment in Railway ControlDocument8 paginiWorkload Assessment in Railway ControlbbeeÎncă nu există evaluări
- Cricothyroidotomy and Needle CricothyrotomyDocument10 paginiCricothyroidotomy and Needle CricothyrotomykityamuwesiÎncă nu există evaluări