Documente Academic
Documente Profesional
Documente Cultură
AIA Guidelines Patient Care Construction Air Change
Încărcat de
Minh van LeDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
AIA Guidelines Patient Care Construction Air Change
Încărcat de
Minh van LeDrepturi de autor:
Formate disponibile
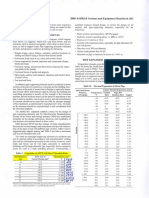
Table 3 Ventilation Requirements for Areas Affecting Patient Care in Hospitals and Outpatient Facilities
Pressure Minimum Air Minimum All Air Air
Relationship Changes of Total Air Exhausted Recirculated Relative Design
to Adjacent Outside Air Changes per Directly to Within Room Humidity,n Temperature,o
Function Space Areasa per Hourb Hourc Outsidem Unitsd % F
Surgery and Critical Care
Operating room (recirculating air system) Positive 5 25 No 45 to 55 62 to 80
Operating/surgical cystoscopic roomse, p, q Positive 5 25 No 45 to 55 68 to 73r
Delivery roomp Positive 5 25 No 45 to 55 68 to 73
Recovery roomp * 2 6 No 45 to 55 75 2
Critical and intensive care * 2 6 No 30 to 60 70 to 75
Newborn intensive care * 2 6 No 30 to 60 72 to 78
Treatment rooms * 6 30 to 60 75
Nursery suite Positive 5 12 No 30 to 60 75 to 80
Trauma roomf, s Positive 5 12 No 45 to 55 62 to 80
Anesthesia gas storage Negative 8 Yes
GI Endoscopy Negative 2 6 No 30 to 60 68 to 73
Bronchoscopyq Negative 2 12 Yes No 30 to 60 68 to 73
Emergency waiting rooms Negative 2 12 Yes 30 to 60 74 2
Triage Negative 2 12 Yes 70 to 75
Radiology waiting rooms Negative 2 12 Yest, u 70 to 75
Nursing
Patient room * 2 6v 30 (W), 50 (S) 75 2
Toilet roomg Negative Optional 10 Yes No
Newborn nursery suite * 2 6 No 30 to 60 72 to 78
Protective environment roomi, q, w Positive 2 12 No 75
Airborne infection isolation roomh,q, x Negative 2 12 Yesu No 75
Isolation alcove or anteroomw, x Pos./Neg. 2 10 Yes No
Labor/delivery/recovery/postpartum (LDRP) * 2 6v 30 (W), 50 (S) 75 2
Public corridor Negative 2 2
Patient corridor * 2 4
Ancillary
Radiologyy
X-ray (diagnostic and treatment) * 2 6 40 (W), 50 (S) 78 to 80
X-ray (surgery/critical care and Positive 3 15 No 30 to 60 70 to 75
catheterization)
Darkroom Negative 2 10 Yes j No
Laboratory, generaly Negative 2 6 Yes No 30 to 60 74 2
Laboratory, bacteriology Negative 2 6 Yes No 30 to 60 74 2
Laboratory , biochemistryy Positive 2 6 No 30 to 60 74 2
Laboratory, cytology Negative 2 6 Yes No 30 to 60 74 2
Laboratory, glasswashing Negative Optional 10 Yes
Laboratory, histology Negative 2 6 Yes No 30 to 60 74 2
Microbiologyy Negative 6 Yes No 30 to 60 74 2
Laboratory, nuclear medicine Negative 2 6 Yes No 30 to 60 74 2
Laboratory, pathology Negative 2 6 Yes No 30 to 60 74 2
Laboratory, serology Positive 2 6 Yes No 30 to 60 74 2
Laboratory, sterilizing Negative Optional 10 Yes No 30 to 60 74 2
Laboratory, media transfer Positive 2 4 No 30 to 60 74 2
Autopsy roomq Negative 2 12 Yes No
Nonrefrigerated body-holding roomk Negative Optional 10 Yes No 70
Pharmacy Positive 2 4 30 to 60 74 2
Administration
Admitting and Waiting Rooms Negative 2 6 Yes 30 to 60 74 2
Diagnostic and Treatment
Bronchoscopy, sputum collection, and Negative 2 12 Yes 30 to 60 74 2
pentamidine administration
Examination room * 2 6 30 to 60 74 2
Medication room Positive 2 4 30 to 60 74 2
Treatment room * 2 6 30 (W), 50 (S) 75 2
Physical therapy and hydrotherapy Negative 2 6 30 to 60 72 to 78/up to 80
Soiled workroom or soiled holding Negative 2 10 Yes No 30 to 60 72 to 78
Clean workroom or clean holding Positive 2 4
Sterilizing and Supply
ETO-sterilizer room Negative 10 Yes No 30 to 60 72 to 78
Sterilizer equipment room Negative 10 Yes No 30 to 60 74 2
Central medical and surgical supply
Soiled or decontamination room Negative 2 6 Yes No 30 to 60 72 to 78
Clean workroom Positive 2 4 No 30 to 60 72 to 78
Sterile storage Positive 2 4 Under 50 74 2
Table 3 Ventilation Requirements for Areas Affecting Patient Care in Hospitals and Outpatient Facilities (Continued)
Pressure Minimum Air Minimum All Air Air
Relationship Changes of Total Air Exhausted Recirculated Relative Design
to Adjacent Outside Air Changes per Directly to Within Room Humidity,n Temperature,o
Function Space Areasa per Hourb Hourc Outsidem Unitsd % F
Service
Food preparation centerl * 2 10 Yes No
Warewashing Negative Optional 10 Yes No
Dietary day storage * Optional 2 No
Laundry, general Negative 2 10 Yes No
Soiled linen sorting and storage Negative Optional 10 Yes No
Clean linen storage Positive 2 (Optional) 2
Linen and trash chute room Negative Optional 10 Yes No
Bedpan room Negative Optional 10 Yes No
Bathroom Negative Optional 10 Yes No 72 to 78
Janitors closet Negative Optional 10 Yes No
(W) = winter (S) = summer * = Continuous directional control not required
a Where continuous directional control is not required, variations should be minimized; in no o For indicated temperature ranges, systems should be capable of maintaining the
case should a lack of directional control allow spread of infection from one area to another. rooms at any point within the range during normal operation. A single figure indi-
Boundaries between functional areas (wards or departments) should have directional con- cates a heating or cooling capacity to at least meet the indicated temperature. This
trol. Lewis (1988) describes ways to maintain directional control by applying air-tracking is usually applicable when patients may be undressed and require a warmer envi-
controls. Ventilation system design should provide air movement, generally from clean to ronment. Use of lower temperature is acceptable when patients comfort and med-
less clean areas. If any VAV or load-shedding system is used for energy conservation, it ical conditions require those conditions.
must not compromise pressure-balancing relationships or minimum air changes required p NIOSH Criteria Documents 75-137 and 96-107 on waste anesthetic gases and
by the table. See note z for additional information. nitrous oxide indicate a need for both local exhaust (scavenging) systems and gen-
b Ventilation rates in this table cover ventilation for comfort, as well as for asepsis and odor eral ventilation of areas in which these gases are used.
control in areas of acute-care hospitals that directly affect patient care. Ventilation rates in q Differential pressure between space and corridors should be a minimum of 0.01 in.
accordance with ASHRAE Standard 62, Ventilation for Acceptable Indoor Air Quality, of water. If monitoring device alarms are installed, allowances should be made to
should be used for areas for which specific ventilation rates are not given. Where a higher prevent nuisance alarms.
outside air requirement is called for in Standard 62 than here, use the higher value. r Because some surgeons or surgical procedures may require room temperatures out-
c Total air changes indicated should be either supplied or, where required, exhausted. Num- side the indicated range, operating room design conditions should be developed in
ber of air changes can be reduced when the room is unoccupied, if the pressure relationship consort with all users, surgeons, anesthesiologists, and nursing staff.
is maintained and the number of air changes indicated is reestablished any time the space s The first-aid and/or emergency room used for initial treatment of accident victims
is used. Air changes shown are minimum values. Higher values should be used when can be ventilated as for the treatment room. Treatment rooms used for cryosurgery
required to maintain room temperature and humidity conditions based on the cooling load with nitrous oxide should have provisions for exhausting waste gases.
of the space (lights, equipment, people, exterior walls and windows, etc.). t In a recirculating ventilation system, HEPA filters can be used instead of exhausting
d Recirculating HEPA filter units used for infection control (without heating or cooling coils) the air to the outside; return air should pass through the HEPA filters before being
are acceptable. Gravity-type heating or cooling units such as radiators or convectors should introduced to any other spaces.
not be used in operating rooms and other special-care areas. u If exhausting air from an airborne-infection isolation room to the outside is not prac-
e For operating rooms, 100% outside air should be used only when codes require it and only tical, the air may be returned through HEPA filters to the air-handling system exclu-
if heat recovery devices are used. sively serving the isolation room.
f Trauma room here is a first-aid room and/or emergency room used for general initial v Total air changes per room for patient rooms, and labor/delivery/recovery/postpar-
treatment of accident victims. The operating room in the trauma center that is routinely tum rooms may be reduced to four when using supplemental heating and/or cooling
used for emergency surgery should be treated as an operating room. systems (radiant heating and cooling, baseboard heating, etc.).
g See section on Patient Rooms for discussion of central toilet exhaust system design. wProtective-environment airflow design specifications protect the patient from com-
h Airborne infectious isolation rooms here are those that might be used for infectious mon environmental airborne infectious microbes (e.g., Aspergillus spores). They
patients in the average community hospital. The rooms are negatively pressurized. Some should provide directed airflow from the cleanest patient area to less clean areas.
may have a separate anteroom. See the section on Infectious Isolation Unit for more infor- HEPA filters at 99.9% efficiency to 0.3 m should be used in the supply airstream,
mation. to protect patient rooms from environmental microbes in ventilation system compo-
i Protective-environment rooms are those used for immunosuppressed patients, positively nents. Recirculation HEPA filters can be used to increase equivalent room air
pressurized to protect the patient. Anterooms are generally required and should be nega- exchanges. Constant-volume airflow is required for consistent ventilation. If design
tively pressurized with respect to the patient room. criteria indicate that airborne-infection isolation is necessary for protective-environ-
j All air need not be exhausted if darkroom equipment has scavenging exhaust duct attached ment patients, an anteroom should be provided. Rooms with reversible airflow pro-
and meets ventilation standards of NIOSH, OSHA, and local employee exposure limits. visions (to allow switching between protective-environment and airborne-infection
k A nonrefrigerated body-holding room is only applicable to facilities that do not perform isolation) are not acceptable (AIA 2001).
autopsies onsite and use the space for short periods while waiting for the body to be trans- x Infectious disease isolation (AII) room here is one used to isolate the airborne
ferred. spread of infectious diseases, such as measles, varicella, or tuberculosis. Design
l Food preparation centers should have an excess of air supply for positive pressurization should include provision for normal patient care during periods not requiring isola-
when hoods are not in operation. The number of air changes may be reduced or varied for tion. Supplemental recirculating devices may be used in the patient room to increase
odor control when the space is not in use. Minimum total air changes per hour should be the equivalent room air exchanges; however, they do not provide outside air require-
that required to provide proper makeup air to kitchen exhaust systems. (See Chapter 31, ments. Air may be recirculated within individual isolation rooms if HEPA filters are
Kitchen Ventilation.) Also, exfiltration or infiltration to or from exit corridors must not used. Rooms with reversible airflow provisions (to allow switching between protec-
compromise exit corridor restrictions of NFPA Standard 90A, pressure requirements of tive-environment and AII) are not acceptable (AIA 2001).
NFPA Standard 96, or the maximum defined in the table. The number of air changes may y When required, provide appropriate hoods and exhaust devices for noxious gases or
be reduced or varied as required for odor control when the space is not in use. See AIA vapors [AIA (2001), see Section 7.31.D14 and 7.31.D15, and NFPA Standard 99).
(2001), Section 7.31.D1.p. z Simple visual methods such as smoke trail, ball-in-tube, or flutterstrip can be used
mAreas with contamination and/or odor problems should be exhausted to the outside and not to verify airflow direction. These devices require a minimum differential air pres-
recirculated to other areas. Individual circumstances may require special consideration for sure to indicate airflow direction. Per AIA (2001) guidelines, recirculating devices
air exhaust to the outside (e.g., intensive care units where patients with pulmonary infec- with HEPA filters may be used in existing facilities as interim, supplemental envi-
tion are treated, rooms for burn patients). To satisfy exhaust needs, replacement air from ronmental controls to meet requirements for airborne infectious agents control.
the outside is necessary. Minimum outside air quantities should remain constant while the Design limitations must be recognized. Either portable or fixed systems should pre-
system is in operation. vent stagnation and short-circuiting of airflow. Supply and exhaust locations should
n Relative humidity ranges listed are minimum and maximum limits where control is spe- direct clean air to work areas across the infectious source, and then to the exhaust,
cifically needed. These limits are not intended to be independent of space temperature. For so that health care workers are not positioned between the infectious source and the
example, relative humidity is expected to be at the higher end of the range when the tem- exhaust. Systems design should also allow easy access for scheduled preventative
perature is also at the higher end, and vice versa. maintenance and cleaning.
S-ar putea să vă placă și
- Table 07 2 2006Document6 paginiTable 07 2 2006Alven T BactadÎncă nu există evaluări
- CDC - Guidelines For Environmental Infection Control in Health-Care Facilities (CDC, 2003)Document9 paginiCDC - Guidelines For Environmental Infection Control in Health-Care Facilities (CDC, 2003)Kesehatan LingkunganÎncă nu există evaluări
- Pages From ASHRAE HVAC Design Manual For Hospitals and Clinics, 2nd Ed. PDFDocument4 paginiPages From ASHRAE HVAC Design Manual For Hospitals and Clinics, 2nd Ed. PDFAhmed Rabie Abd ElazeemÎncă nu există evaluări
- Hospital AC Design DataDocument2 paginiHospital AC Design DataSaleem BashaÎncă nu există evaluări
- Table 7.1 Design Parameters: ANSI/ASHRAE/ASHE Standard 170 - 2008Document6 paginiTable 7.1 Design Parameters: ANSI/ASHRAE/ASHE Standard 170 - 2008mkkÎncă nu există evaluări
- Performance Measure Target Key Performance Indicators: Recovery Room Central Sterile Supplies Cath LabDocument4 paginiPerformance Measure Target Key Performance Indicators: Recovery Room Central Sterile Supplies Cath LabNatasha BhasinÎncă nu există evaluări
- 10) S1-22-IsM - Session 10 - 12th and 13th Aug 2023Document103 pagini10) S1-22-IsM - Session 10 - 12th and 13th Aug 20232022da04123Încă nu există evaluări
- Enriquez Physio Ex3-Act5Document10 paginiEnriquez Physio Ex3-Act5Vergel Jigs EnriquezÎncă nu există evaluări
- Daoud2022 Pharmaceutics 1568782 SupplementaryDocument13 paginiDaoud2022 Pharmaceutics 1568782 SupplementaryFrederic DaoudÎncă nu există evaluări
- T TestDocument5 paginiT TestGanesh TiwariÎncă nu există evaluări
- T TestDocument5 paginiT TestGanesh TiwariÎncă nu există evaluări
- Inconclusive:Duetolowviralloadinsample, The SampleneedtoberepeatedDocument1 paginăInconclusive:Duetolowviralloadinsample, The SampleneedtoberepeatedPro GemurÎncă nu există evaluări
- Results of Treatment For Low-Grade Gliomas: Select Randomized TrialsDocument46 paginiResults of Treatment For Low-Grade Gliomas: Select Randomized Trialsana claraÎncă nu există evaluări
- لقطة شاشة ٢٠٢١-٠٤-١٨ في ٨.٤١.٢٠ صDocument32 paginiلقطة شاشة ٢٠٢١-٠٤-١٨ في ٨.٤١.٢٠ صWed LodÎncă nu există evaluări
- New PaperDocument20 paginiNew Papermohammed hassonaÎncă nu există evaluări
- LF G3920SA 0010 Clinical ReportDocument16 paginiLF G3920SA 0010 Clinical ReportRoxana HermosoÎncă nu există evaluări
- VIDHI GAJJAR B, InggrisDocument1 paginăVIDHI GAJJAR B, InggrisJigar GajjarÎncă nu există evaluări
- Penarikan Contoh 3Document2 paginiPenarikan Contoh 3DiasÎncă nu există evaluări
- Diagnostic TestingDocument55 paginiDiagnostic TestingMoldovan Nicolae-AndreiÎncă nu există evaluări
- Diagnostic Test - Ris 07 071107Document30 paginiDiagnostic Test - Ris 07 071107No NameÎncă nu există evaluări
- Targeted Therapies in Renal Cell CarcinomaDocument24 paginiTargeted Therapies in Renal Cell CarcinomabiomathenÎncă nu există evaluări
- PhysioEx Exercise 3 Activity 5Document7 paginiPhysioEx Exercise 3 Activity 5edvin merida proÎncă nu există evaluări
- Lembar Jawaban Ebm EliskaDocument30 paginiLembar Jawaban Ebm EliskaNovi YantiÎncă nu există evaluări
- Lembar Jawaban Skillab Evidence Based Medicine (Ebm) Nama: Rafika Triasa NIM: 040427223270003Document11 paginiLembar Jawaban Skillab Evidence Based Medicine (Ebm) Nama: Rafika Triasa NIM: 040427223270003Yahya Darmais FaridÎncă nu există evaluări
- Ajay NalgunwarDocument1 paginăAjay NalgunwarAnkit NalgundwarÎncă nu există evaluări
- Lembar Jawaban Skillab Evidence Based Edicine (Ebm) : Parameter Rerata SD RERATA+2sd Nilai AbnormalitasDocument26 paginiLembar Jawaban Skillab Evidence Based Edicine (Ebm) : Parameter Rerata SD RERATA+2sd Nilai Abnormalitassisil muntheÎncă nu există evaluări
- Improving Skills in Correcting Astigmastism (Dr. Putri Hartini, Sp. M.)Document33 paginiImproving Skills in Correcting Astigmastism (Dr. Putri Hartini, Sp. M.)Nisaa DwityarahmaÎncă nu există evaluări
- Contoh Skill Lab EBM-1Document23 paginiContoh Skill Lab EBM-1seakunbacaÎncă nu există evaluări
- Effect of Nateglinide On The Incidence of DiabetesDocument31 paginiEffect of Nateglinide On The Incidence of Diabetesfred opinionÎncă nu există evaluări
- Lecture 6 - Statistical Tests: Confidence Intervals Student Test ANOVA Test Fisher Test For Variances Nonparametric TestsDocument21 paginiLecture 6 - Statistical Tests: Confidence Intervals Student Test ANOVA Test Fisher Test For Variances Nonparametric TestsKennethBermudezÎncă nu există evaluări
- CAYBOT - PhysioEx Exercise 3 Activity 5Document8 paginiCAYBOT - PhysioEx Exercise 3 Activity 5Faustine CaybotÎncă nu există evaluări
- Bjs 11 H 048Document7 paginiBjs 11 H 048guiinacioÎncă nu există evaluări
- Case Processing SummaryDocument8 paginiCase Processing SummaryFirman Al KhatiriÎncă nu există evaluări
- Case Processing SummaryDocument8 paginiCase Processing SummaryFirman Al KhatiriÎncă nu există evaluări
- Evaluation Biosynex Tests AntigeniqueDocument4 paginiEvaluation Biosynex Tests AntigeniqueKrystian TomczeskiÎncă nu există evaluări
- ANSWER SHEET (Module 5) .: Z-Test: Two Sample For MeansDocument4 paginiANSWER SHEET (Module 5) .: Z-Test: Two Sample For MeansJan JanÎncă nu există evaluări
- 4333445492022-10-25T16 28 16.773Document6 pagini4333445492022-10-25T16 28 16.773Nina JordanÎncă nu există evaluări
- Autput Penelitian: StatisticsDocument3 paginiAutput Penelitian: StatisticsririÎncă nu există evaluări
- Dwi Putri Tania (04011181621024)Document34 paginiDwi Putri Tania (04011181621024)Raudhah SimahateÎncă nu există evaluări
- Pex 03 05Document10 paginiPex 03 05Jose Maria RojasÎncă nu există evaluări
- Chi Square ContingencyDocument8 paginiChi Square Contingencypandit shendeÎncă nu există evaluări
- Clear PlateletsDocument17 paginiClear PlateletsJorge Peregrino BragaÎncă nu există evaluări
- London Cancer Lung Radiotherapy Guidelines 2013 v1 0Document24 paginiLondon Cancer Lung Radiotherapy Guidelines 2013 v1 0Cosmin SaftaÎncă nu există evaluări
- Afisare Rezultat Final SpitalDocument1 paginăAfisare Rezultat Final SpitalUrsu EmiliaÎncă nu există evaluări
- Equ42-A-08 Caprisa Ref Range-Crit Val 27sep19Document4 paginiEqu42-A-08 Caprisa Ref Range-Crit Val 27sep19Rafat ElshemiÎncă nu există evaluări
- Specimens Were Collected From 454 Suspected COVID-19 Including Pre-Operative Patients at Siriraj HospitalDocument2 paginiSpecimens Were Collected From 454 Suspected COVID-19 Including Pre-Operative Patients at Siriraj HospitalKristian Sudana HartantoÎncă nu există evaluări
- SKRENINGDocument40 paginiSKRENINGPuti NoviandiniÎncă nu există evaluări
- Nejmc 2313517Document2 paginiNejmc 2313517carb0ne14rÎncă nu există evaluări
- Sgot/Sgpt Hemoglobin Trigliserid Totalkolestro L HDL LDL N Valid Missing Mean Std. DeviationDocument24 paginiSgot/Sgpt Hemoglobin Trigliserid Totalkolestro L HDL LDL N Valid Missing Mean Std. DeviationClarisya Resky VaniaÎncă nu există evaluări
- Practice Task F-TestDocument10 paginiPractice Task F-TestRiza Mae AlceÎncă nu există evaluări
- The Chi-Square ( ) Test: A Test of SignificanceDocument40 paginiThe Chi-Square ( ) Test: A Test of Significance22presentationÎncă nu există evaluări
- JR Orto FianDocument22 paginiJR Orto FianalifianÎncă nu există evaluări
- Table 1 Sociodemographic Details of The Study PopulationDocument9 paginiTable 1 Sociodemographic Details of The Study Populationvigneswari.lilacÎncă nu există evaluări
- Covid PresentationDocument43 paginiCovid PresentationSr. Section Engineer Coaching Depot-ValsadÎncă nu există evaluări
- Npar Tests: One-S Am Ple Kol Mogorov-S Mirnov Te STDocument6 paginiNpar Tests: One-S Am Ple Kol Mogorov-S Mirnov Te STcarissa rima putriÎncă nu există evaluări
- Barbosa 2016Document2 paginiBarbosa 2016Ottofianus Hewick KalangiÎncă nu există evaluări
- Barbosa 2016Document2 paginiBarbosa 2016Ottofianus Hewick KalangiÎncă nu există evaluări
- SD Rerata 2 SD Nilai AbnormalitasDocument10 paginiSD Rerata 2 SD Nilai AbnormalitasjasndkaaÎncă nu există evaluări
- CT Scan in Woman Oncology GynecologyDocument109 paginiCT Scan in Woman Oncology GynecologyAstien SuzmanÎncă nu există evaluări
- Appendix 4-WAREHOUSE - Hut Khoi WarehouseDocument6 paginiAppendix 4-WAREHOUSE - Hut Khoi WarehouseMinh van LeÎncă nu există evaluări
- Threaded Rod SelectionDocument1 paginăThreaded Rod SelectionMinh van LeÎncă nu există evaluări
- A-InD-01b Overtime Approval FormDocument3 paginiA-InD-01b Overtime Approval FormMinh van LeÎncă nu există evaluări
- GramarDocument5 paginiGramarHồ ThôngÎncă nu există evaluări
- Gas or Electric Space Heater MK II Underfloor Models SH2212B or SC2212B or SI2212BDocument22 paginiGas or Electric Space Heater MK II Underfloor Models SH2212B or SC2212B or SI2212BFelix Leone EnacheÎncă nu există evaluări
- Envi-Met Introduction 2019Document61 paginiEnvi-Met Introduction 2019Thắm PhạmÎncă nu există evaluări
- University of DhakaDocument15 paginiUniversity of DhakaMd. Sakib HossainÎncă nu există evaluări
- Axial & Centifugal Jet Fans SpecificationDocument9 paginiAxial & Centifugal Jet Fans SpecificationRamakrishnan100% (1)
- ETFE and Smoke Control WhitepaperDocument3 paginiETFE and Smoke Control Whitepapernawin10Încă nu există evaluări
- A Guide To Trickle VentilatorsDocument4 paginiA Guide To Trickle VentilatorsOctavian BumbescuÎncă nu există evaluări
- Air Conditioning System Selection&DesignDocument17 paginiAir Conditioning System Selection&DesignMuhammedShareefÎncă nu există evaluări
- NIBS Guidelines For CommissioningDocument337 paginiNIBS Guidelines For CommissioningWaseem SiddiqueÎncă nu există evaluări
- Office BuildingDocument10 paginiOffice BuildingZamfira Octavian100% (1)
- SRP-Series-KMI-Manual - Com Exemplo de CalcDocument22 paginiSRP-Series-KMI-Manual - Com Exemplo de CalcErich BuenoÎncă nu există evaluări
- Cooling Load CalculationDocument90 paginiCooling Load CalculationmiraqueelaliÎncă nu există evaluări
- Refrigirated CargoDocument58 paginiRefrigirated CargoPawan KumarÎncă nu există evaluări
- CA-270 Service ManualDocument499 paginiCA-270 Service ManualLambertGuevarraÎncă nu există evaluări
- Libro Fire Engineering Positive Pressure Attack For Ventilation & FirefightingDocument322 paginiLibro Fire Engineering Positive Pressure Attack For Ventilation & FirefightingYorman J. Mari Peraza100% (1)
- FPB 22.14 Rev.01 - Access To Heavy Duty Gas Turbine Enclosures With The Unit in OperationDocument27 paginiFPB 22.14 Rev.01 - Access To Heavy Duty Gas Turbine Enclosures With The Unit in Operationwaqar ahmadÎncă nu există evaluări
- Guideline 36 2021Document287 paginiGuideline 36 2021Shaliya KarunathilakaÎncă nu există evaluări
- HVAC Design GuideDocument12 paginiHVAC Design GuideAshok100% (2)
- GREEN Trade Marks Search Result Class 11Document65 paginiGREEN Trade Marks Search Result Class 11rajender RightsandMarksÎncă nu există evaluări
- 000 Technical Standards - Luxury & Premium - V1 - Dec-21Document173 pagini000 Technical Standards - Luxury & Premium - V1 - Dec-21HoangDung LeÎncă nu există evaluări
- How Our Homes Impact Our Health Using A COVID 19 Informed Approach To Examine Urban Apartment HousingDocument18 paginiHow Our Homes Impact Our Health Using A COVID 19 Informed Approach To Examine Urban Apartment HousingAna Paula ContenteÎncă nu există evaluări
- Heating For Pig ProductionpdfDocument4 paginiHeating For Pig ProductionpdfGabriel RaicaÎncă nu există evaluări
- Airflow: Weatherization Assistance Program Indiana Field GuideDocument46 paginiAirflow: Weatherization Assistance Program Indiana Field GuideAngel Daniel GarciajoyaÎncă nu există evaluări
- VentilationDocument14 paginiVentilationAndy ParkinsonÎncă nu există evaluări
- IGBC Green Homes Ver 2 Precertification Preliminary Review - Shivram CHS LTD, MumbaiDocument29 paginiIGBC Green Homes Ver 2 Precertification Preliminary Review - Shivram CHS LTD, MumbaiaalekhchandanÎncă nu există evaluări
- The New California Academy of Sciences: Na05 - XMMNNDocument19 paginiThe New California Academy of Sciences: Na05 - XMMNNJulian de GraciaÎncă nu există evaluări
- ASHRAE Guidelines and StandardsDocument12 paginiASHRAE Guidelines and StandardsKhalid0% (1)
- MATEST-S P A - UnipersonaleDocument603 paginiMATEST-S P A - UnipersonaleConstantin Ungureanu100% (1)
- Subway DrainageDocument6 paginiSubway DrainageAbhijit RoutÎncă nu există evaluări
- Thermaline 4700: Selection & Specification DataDocument4 paginiThermaline 4700: Selection & Specification Datagowtham_venkat_4Încă nu există evaluări
- AshraeDocument98 paginiAshraeotezgiden44% (9)