Documente Academic
Documente Profesional
Documente Cultură
Case Report Anug
Încărcat de
Azi Pertiwi HussainDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Case Report Anug
Încărcat de
Azi Pertiwi HussainDrepturi de autor:
Formate disponibile
Dr Ashish singh et al . / IJRID Volume 5 Issue 5 Sep.-Oct.
2015
Available online at www.ordoneardentistrylibrary.org ISSN 2249-488X
Case report
INTERNATIONAL JOURNAL OF RESEARCH IN DENTISTRY
Case report on ANUG
Dr Ashish singh*, Dr Aditya sinha , Dr Jithendra k d , Dr Satendra sharma, Dr Mohit garg
K.D Dental College & Hospital Mathura UP
Received: 11 Aug. 2015; Revised: 9 Sep. 2015; Accepted: 5 Oct. 2015; Available online: 5 Nov. 2015
ABSTRACT
Acute Necrotizing Ulcerative Gingivitis (ANUG) is a distinct and specific disease. This disease entity has been
described as far back as the days of Hippocrates and is known by many synonyms. With the advent of antibiotics
and with improved nutritional status, the incidence has decreased and even become extinct in developed countries
In developing countries, however, the condition is still a commonly diagnosed clinical lesion because of the
persistently poor nutritional status. This case report showing the patients diagnosed as special form of distraction of
gingiva within 5days & treatment of this condition which called as ANUG
Keywords- Acute Necrotizing Ulcerative Gingivitis (ANUG), ANUP
INTRODUCTION
Acute Necrotizing Ulcerative Gingivitis (ANUG), now classified as Necrotizing Periodontal Disease according
to the 1999 American Academy of Periodontics classification system, is a distinct and specific disease
characterized by rapidly progressive ulceration typically starting at the tip of the interdental papilla, spreading
along the gingival margins, and going on to acute destruction of the periodontal tissue1,2.
This disease entity has been described as far back as the days of Hippocrates and is known by many synonyms
such as trench mouth, Vincents disease, and Vincents gingivostomatitis
In developing countries ANUG remains a commonly diagnosed clinical lesion3,4. This is of the existing poor
nutritional status, stress living conditions, poor oral hygiene, and a state of debilitation often resulting from
endemic contagious diseases In developing nations where the standard of living is gradually on the decline, this
disfiguring oral lesion becomes very important clinically as more and more children are exposed to the risk
factors which lead to the development of ANUG4-6
Etiology and Pathophysiology
Plaut & Vincent introduced the concept that NUG is caused by a specific bacteria namely, fusiform bacillus &
spirochetal orgnaisms . More recently , Loesche & colleagues described
29 Dr Ashish singh et al / IJRID Volume 5 Issue 5 Sep.-Oct. 2015
Dr Ashish singh et al . / IJRID Volume 5 Issue 5 Sep.-Oct. 2015
a constant & variable flora associated with ANUG ,Constant flora is composed of Fusospirochetal organisms &
also Bacteroides intermedius.
There are some systemic predisposing factors like Nutritional deficiency, debilitating disease & Psychosomatic
factors also with some local predisposing factors like pre-existing gingivitis ,injury to gingiva & smoking
STRESS SMOKING
Increased Corticosteroid Pre-existing gingivitis
Immunosuppression Increased bacterial growth
Nutritional deficiency ANUG
debilitating diseases
STAGES - INVOLVEMENT OF LESION
1- Necrosis of the tip of interdental papilla
2- Necrosis of the entire papilla
3- Necrosis extending to gingival margin
4- Necrosis extending to the attached gingiva
5- Necrosis extending into buccal or labial mucosa
6- Necrosis exposing alveolar bone
7- Necrosis perforating skin of cheek
ZONES- classified by Listgarten & Collegues
Zone 1- Bacterial zone - superficial zone
Zone 2- Neutrophil-rich zone
Zone 3- Nectrotic zone
Zone 4- Zone of spirochetal infiltration
30 Dr Ashish singh et al / IJRID Volume 5 Issue 5 Sep.-Oct. 2015
Dr Ashish singh et al . / IJRID Volume 5 Issue 5 Sep.-Oct. 2015
Treatment -
1- Non-ambulatory patient- with the symptoms of generalized systemic complications
2- Ambulatory patient - with no serious systemic complications 7
Case report
Two patients of Age 25 yr old reported to the periodontology OPD of K.D Dental college & hospital with chief
complaint of Severe pain & bleeding gums with burning sensation of gingiva since 5 days.
On extraoral examination there was no gross facial asymmetry detected, lips was competent, submandibular
lymph nodes are tender on palpation and local rise in temperature was detected.
Patient gave the history of elevated temperature for 1 week. On intraoral examination poor oral hygiene was
noticed with plaque and calculus deposition. There was no marginal gingiva and interdenta papilla because
there was necrosis of the interdental papillae occur.
There was traumatic bite in anterior teeth. Intraoral periapical radiograph revealed no bone loss in lower
anterior teeth. But in both case there is necrosis extending upto the attached gingiva this show the Stage 4
condition without no bone involvement thus this condition purely a ANUG not ANUP
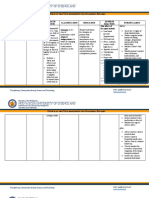
pre-operative images
Patient first Patient second
a) Stage 4- Lesion involving in lower anterior teeth in both case but no bone involvement was seen.
31 Dr Ashish singh et al / IJRID Volume 5 Issue 5 Sep.-Oct. 2015
Dr Ashish singh et al . / IJRID Volume 5 Issue 5 Sep.-Oct. 2015
OPG showing no bone loss
In the first visit after thorough examination only conservative treatment like removal of local factors and
maintenance of oral hygiene was planned. Trauma relieved in anterior teeth by selective grinding Supragingival
scaling was attempted a thoroughly as the condition allowed. Patients was advised to take adequate rest, proper
diet and maintain proper oral hygiene. they was prescribed amoxicillin 500 mg thrice in a day for 5 days and
local application of gel containing metronidazole three-four times day. they were also instructed to rinse with
3% H2O2 & sterile warm water (1:1) four times a day and also with 0.12% chlorhexidine rinses to maintain
oral hygeine as they were unable to clean her teeth with brush. Patients recalled on second day and again
supragingival scaling was done After 3 days the patients was re-evaluated and scaling and curettage was
performed. After 7 days patients was almost symptom free so thorough scaling & root planing was done. 3%
H2O2 rinses were now discontinued but 0.12% chlorohexidine rinses continued. Patient was re-evaluated after
one month & a good response was found in the form of healing of necrotic areas and reduction in the size of
gingival craters. Patient was kept on maintenance with instructions of oral hygiene and proper nutrition.
After phase I-
Patient - First
b) Image after phase I
32 Dr Ashish singh et al / IJRID Volume 5 Issue 5 Sep.-Oct. 2015
Dr Ashish singh et al . / IJRID Volume 5 Issue 5 Sep.-Oct. 2015
Patient - Second
c) Images after phase I
post-operative image after 1wk
Discussion
An eminent Bio statistician was contacted Necrotizing ulcerative gingivtis is an inflammatory destructive disease of the
gingiva ,which presents characteristic signs and symptoms. This disease entity was present as early as 400BC in Greek
soldiers, but it was first described by Plaut in 1894 and
Vincent in 18968,9. It is caused mainly by Fusiform bacilli and Spirochetes. In the present case report we have discussed
the pre-treatment and post treatment clinical picture of ANUG and its management. The predisposing factor in our case
report is stress & pre-existing gingivitis with smoking .These both patients are unemployed , & live in stressful condition ,
with history of pre-existing gingivits
Stress is believed to predispose to ANUG by causing an elevation in adrenocortical secretion. It also causes the release
of substance P, a peptide hormone which suppresses both specific and non specific immunity10,11. It also affects patients
moods resulting in changes in oral hygiene and nutrition.
Schluger who described ANUG as a disease of filth believes that a low standard of oral hygiene is the most single factor
contributing to ANUG. However, he does not state the presence of the disease is always a result of lack of oral hygiene
on the part of the patient but that plaque and debris accumulation occurs due to discomfort withoral hygiene practices.
Mentioned frequently in the literature is smoking as a predisposing factor to ANUG. Pindborg and Goldhabeg found 98%
of their patients were smokers.
33 Dr Ashish singh et al / IJRID Volume 5 Issue 5 Sep.-Oct. 2015
Dr Ashish singh et al . / IJRID Volume 5 Issue 5 Sep.-Oct. 2015
Kardachi and Clarke cite reports that local and systemic catecholamines are released in response to nicotine and
hypothesized the effect of cathecolamine super-imposed on psychological and physiological stress
Conclusion
Modalities of treating ANUG over the years is almost as varied as its synonyms though they all center on
reducing the bacteria flora. The use of antibiotics in the management of ANUG has
been strongly advocated. Metrondazole has also been found to be as effective as penicillin in causing remission
of the clinical symptoms, and this was parallel with reduction in the proportionof bacteria species associated
with the disease12.
However, the highly preventable ANUG entails implementing measures aimed at eradicating malnutrition,
improving oral hygiene status, and minimizing damage to oral mucosa as well as avoiding contamination of the
oral environment by a heavy load of Bacteroidacease, particularly
F. necrophorum.
References
1. Emslie RD. Cancrum oris. Dental Practitioner and Dental Record 1963: 13:481-495.
2. Enwonwu CO. Nutritional disease in the tropics. In: Prabhu SR et al., (eds) Oral diseases in the tropics.
Oxford University Press, 1992: 309-324.
3. Chandra RK. 1990 McCollum Award lecture. Nutrition and immunity: lessons from the past and new insights
into the future. Am J Clin Nutr. 1991 May;53(5):1087-101.
4. Enwonwu CO. Epidemiological and biochemical studies of necrotizing ulcerative gingivitis and noma
(cancrum oris) in Nigerian children. Arch Oral Biol. 1972 Sep;17(9):1357-71. No abstract available.
5. Tempest MN. Cancrum oris. Br J Surg. 1966 Nov;53(11):949-69. No abstract available.
6. Pindborg JJ, Bhat M, Roed-Peterson B. Oral changes in South Indian children with severe protein
deficiency. J Periodontol. 1967 May-Jun;38(3):218-21
7. Essentials of clinical periodontology & periodontics Shantipriya reddy
8. Goldberg HJ. Acute necrotizing ulcerative gingivitis. J Oral Ther Pharmacol. 1966 May;2(6):451-9.
9. Shields WD. Acute necrotizing ulcerative gingivitis. A study of some of the contributing factors and their
validity in an Army population. J Periodontol. 1977 Jun;48(6):346-9.
10.Kowolik MJ, Nisbet T. Smoking and acute ulcerative gingivitis. A study of 100 patients. Br Dent 11.Fitch
HB, Bethart H, Alling CC, et. al. Acute necrotising ulcerative gingivitis. J Periodontol. 1963;
34:422-425
12. Horning GM. Necotizing gingivostomatitis: NUG to noma. Compend Contin Educ Dent. 1996
Oct;17(10):951-4, 956, 957-8 passim; quiz 964. Review.
34 Dr Ashish singh et al / IJRID Volume 5 Issue 5 Sep.-Oct. 2015
S-ar putea să vă placă și
- 10-Week Physical Activity Program For A Hypertensive Obese AdultDocument19 pagini10-Week Physical Activity Program For A Hypertensive Obese AdultPhysiotherapist AliÎncă nu există evaluări
- Lecture Hemophilia and Thrombocytopenic PurpuraDocument55 paginiLecture Hemophilia and Thrombocytopenic PurpuraaymenÎncă nu există evaluări
- Plab 1 Mock 5th March 2017Document35 paginiPlab 1 Mock 5th March 2017RabeeyaÎncă nu există evaluări
- Uwise ReviewDocument14 paginiUwise ReviewAnonymous T1G9BQQÎncă nu există evaluări
- Presentation On Care of Critically Ill PatientDocument9 paginiPresentation On Care of Critically Ill Patientanamika sharmaÎncă nu există evaluări
- Marshall 2015Document13 paginiMarshall 2015MalikinNadalÎncă nu există evaluări
- Berglundh Et Al-2018-Journal of Clinical PeriodontologyDocument6 paginiBerglundh Et Al-2018-Journal of Clinical PeriodontologyCristian CulcitchiÎncă nu există evaluări
- Aspiration PneumoniaDocument27 paginiAspiration PneumoniaReya Awali SuasoÎncă nu există evaluări
- Understanding Periodontal Diseases: Assessment and Diagnostic Procedures in PracticeDe la EverandUnderstanding Periodontal Diseases: Assessment and Diagnostic Procedures in PracticeÎncă nu există evaluări
- Berglundh Et Al (2018) - Peri Implant Diseases and Conditions - Consensus Report of Workgroup 4 - 1Document9 paginiBerglundh Et Al (2018) - Peri Implant Diseases and Conditions - Consensus Report of Workgroup 4 - 1FelipeOyarceSalazarÎncă nu există evaluări
- Diagnostico PeriodontalDocument16 paginiDiagnostico PeriodontalLizeth GalvizÎncă nu există evaluări
- Indices of Periodontal DiseaseDocument33 paginiIndices of Periodontal DiseaseRichard Sullivan100% (12)
- Symptomatic BenignDocument5 paginiSymptomatic BenignTri Pamungkas IrawanÎncă nu există evaluări
- Prepubertal Periodontitis: A Rare Case Report: March 2015Document5 paginiPrepubertal Periodontitis: A Rare Case Report: March 2015Alya DayÎncă nu există evaluări
- Physiotherapy For Improving Mouth Opening & Tongue Protrution in Patients With Oral Submucous Fibrosis (OSMF) - Case SeriesDocument9 paginiPhysiotherapy For Improving Mouth Opening & Tongue Protrution in Patients With Oral Submucous Fibrosis (OSMF) - Case SeriesViral ParekhÎncă nu există evaluări
- Eksperimental 2021Document8 paginiEksperimental 2021Putri NurhadizahÎncă nu există evaluări
- Podj 4Document6 paginiPodj 4cutchaimahÎncă nu există evaluări
- Management of Necrotizing Ulcerative Gingivitis in A Pregnant Patient - A Rare Case ReportDocument6 paginiManagement of Necrotizing Ulcerative Gingivitis in A Pregnant Patient - A Rare Case ReportAZWAN RAHMADHAN PUTRAÎncă nu există evaluări
- Jurnal Gingivitis Vivian 190631174Document5 paginiJurnal Gingivitis Vivian 190631174VivianÎncă nu există evaluări
- Posición Ante Los Antibióticos 2016Document40 paginiPosición Ante Los Antibióticos 2016Sydney LópezÎncă nu există evaluări
- Journal of Periodontology - 2018 - Lang - Periodontal HealthDocument8 paginiJournal of Periodontology - 2018 - Lang - Periodontal HealthMonica MartínezÎncă nu există evaluări
- CR 4Document4 paginiCR 4Fitrah AndiÎncă nu există evaluări
- Treatment Planning 3Document6 paginiTreatment Planning 3api-454004347Încă nu există evaluări
- Periodontal Health: Niklaus P. Lang P. Mark BartoldDocument8 paginiPeriodontal Health: Niklaus P. Lang P. Mark BartoldChristine LomuntadÎncă nu există evaluări
- NIH Public Access: Author ManuscriptDocument19 paginiNIH Public Access: Author ManuscriptJean PradoÎncă nu există evaluări
- Feline Chronic Gingivostomatitis With Calicivirus InfectionDocument6 paginiFeline Chronic Gingivostomatitis With Calicivirus Infectionadinda larasÎncă nu există evaluări
- Sequelae of A Treated Stevens Johnson SyndromeA Case ReportDocument3 paginiSequelae of A Treated Stevens Johnson SyndromeA Case ReportInternational Journal of Innovative Science and Research TechnologyÎncă nu există evaluări
- 1752 1947 3 98Document4 pagini1752 1947 3 98Rini RiantiÎncă nu există evaluări
- Journal 2.Document5 paginiJournal 2.Dha Dina SevofrationÎncă nu există evaluări
- Oral and Dental HealthDocument10 paginiOral and Dental HealthannisaramadantiÎncă nu există evaluări
- Parameters of Care Supplement: Parameter On "Refractory" PeriodontitisDocument2 paginiParameters of Care Supplement: Parameter On "Refractory" PeriodontitisEllis E. RamadianÎncă nu există evaluări
- NOVA Classificação Das Doenças Periodontais 2017Document9 paginiNOVA Classificação Das Doenças Periodontais 2017Isabelle AlvesÎncă nu există evaluări
- Brianna HDocument32 paginiBrianna Hapi-462204210Încă nu există evaluări
- ISSN: 0975-833X: Case StudyDocument4 paginiISSN: 0975-833X: Case StudyantonÎncă nu există evaluări
- A New Classification Scheme For Periodontal and Peri and Conditions - Introduction and Key Changes From The 1999 ClassificationDocument8 paginiA New Classification Scheme For Periodontal and Peri and Conditions - Introduction and Key Changes From The 1999 ClassificationOner Man0% (1)
- Antibiotice in PericoroniteDocument2 paginiAntibiotice in PericoroniteGabriela Cocieru MotelicaÎncă nu există evaluări
- ANUG in A HIV Seronegative Patient - A Case ReportDocument6 paginiANUG in A HIV Seronegative Patient - A Case ReportPringgo EfbiÎncă nu există evaluări
- Open Drainage or NotDocument6 paginiOpen Drainage or Notjesuscomingsoon2005_Încă nu există evaluări
- Perio PBLKasvuGingivalOvergrowthDocument32 paginiPerio PBLKasvuGingivalOvergrowthDraspiÎncă nu există evaluări
- 243 674 1 PB PDFDocument2 pagini243 674 1 PB PDFsurgaÎncă nu există evaluări
- PERIIMPLANTITIS RESUMEN Berglundh - Et - Al-2018-Journal - of - Clinical - PeriodontologyDocument12 paginiPERIIMPLANTITIS RESUMEN Berglundh - Et - Al-2018-Journal - of - Clinical - PeriodontologyDaniela RojasÎncă nu există evaluări
- Laporan Jurnal Reading IKGA - Amana Fitria ChusaeniDocument36 paginiLaporan Jurnal Reading IKGA - Amana Fitria ChusaeniAmana FitriaÎncă nu există evaluări
- Crid2014 741402Document4 paginiCrid2014 741402karenafiafiÎncă nu există evaluări
- 2022 - TenOrio - Oral Manifestations of Autoimmune Polyglandular Syndrome Type 1Document5 pagini2022 - TenOrio - Oral Manifestations of Autoimmune Polyglandular Syndrome Type 1NATALIA SILVA ANDRADEÎncă nu există evaluări
- Nasal Polyp Nasa Arsha Management Through Ayurveda A Single Case StudyDocument4 paginiNasal Polyp Nasa Arsha Management Through Ayurveda A Single Case StudyEditor IJTSRDÎncă nu există evaluări
- Antibiotics in Endodontics: A ReviewDocument16 paginiAntibiotics in Endodontics: A ReviewHisham HameedÎncă nu există evaluări
- 12 Sequel To Renal Transplant An Oral Physician's PerspectiveDocument5 pagini12 Sequel To Renal Transplant An Oral Physician's PerspectivevinhannyÎncă nu există evaluări
- Berglundh 2018 Peri Implant Diseases and ConditionsDocument6 paginiBerglundh 2018 Peri Implant Diseases and ConditionsPatricia CastellanosÎncă nu există evaluări
- Ramsay Hunt Syndrome With Oral Findings - A Rare Case - CASE REPORT KEDUA BAGUSDocument7 paginiRamsay Hunt Syndrome With Oral Findings - A Rare Case - CASE REPORT KEDUA BAGUSfoto pasienÎncă nu există evaluări
- Caton Et Al-2018-Journal of PeriodontologyDocument8 paginiCaton Et Al-2018-Journal of PeriodontologyIsabel Escobar MinotasÎncă nu există evaluări
- Contents 2020 Dermatologic-ClinicsDocument3 paginiContents 2020 Dermatologic-Clinicsandifarra281002Încă nu există evaluări
- The Prevention of Periodontal Disease-An Overview: Frank A. Scannapieco - Eva GershovichDocument5 paginiThe Prevention of Periodontal Disease-An Overview: Frank A. Scannapieco - Eva GershovichLauraBotnariÎncă nu există evaluări
- Pe Rich On DR It Is of The Auricle and Its ManagementDocument6 paginiPe Rich On DR It Is of The Auricle and Its ManagementmitaÎncă nu există evaluări
- Papillon Lefevre Syndrome-A Literature Review and Case ReportDocument7 paginiPapillon Lefevre Syndrome-A Literature Review and Case ReportnadhiracindyÎncă nu există evaluări
- Trismus and Oral Cavity Stenosis After Caustic Ingestion Surgical Management - December - 2022 - 6954990186 - 5805221Document1 paginăTrismus and Oral Cavity Stenosis After Caustic Ingestion Surgical Management - December - 2022 - 6954990186 - 5805221Nishant GillÎncă nu există evaluări
- Chapple Et Al-2018-Journal of Clinical Periodontology Grupo 1Document10 paginiChapple Et Al-2018-Journal of Clinical Periodontology Grupo 1Genesis Lopez torresÎncă nu există evaluări
- Lichen Planus Article PDFDocument3 paginiLichen Planus Article PDFSuresh KumarÎncă nu există evaluări
- 10 Squamouspapilloma-ReportoftwocasesDocument7 pagini10 Squamouspapilloma-ReportoftwocasesAyik DarkerThan BlackÎncă nu există evaluări
- Polak Et Al-2015-Journal of Clinical Periodontology PDFDocument13 paginiPolak Et Al-2015-Journal of Clinical Periodontology PDFChristine HacheÎncă nu există evaluări
- Generalized Aggressive Periodontitis in A 51 Year Old.Document7 paginiGeneralized Aggressive Periodontitis in A 51 Year Old.respikÎncă nu există evaluări
- J Clinic Periodontology - 2018 - Chapple - Periodontal Health and Gingival Diseases and Conditions On An Intact and ADocument10 paginiJ Clinic Periodontology - 2018 - Chapple - Periodontal Health and Gingival Diseases and Conditions On An Intact and AAndreaÎncă nu există evaluări
- Effect of Morinda Citrifolia L. Fruit Juice On Gingivitis/periodontitisDocument7 paginiEffect of Morinda Citrifolia L. Fruit Juice On Gingivitis/periodontitisMuhamad Vicki SyahrialÎncă nu există evaluări
- Recent Advancements in Management of Alveolar Osteitis (Dry Socket)Document5 paginiRecent Advancements in Management of Alveolar Osteitis (Dry Socket)International Journal of Innovative Science and Research TechnologyÎncă nu există evaluări
- Oral Candidiasis: A Short Review and A Case Report: December 2018Document5 paginiOral Candidiasis: A Short Review and A Case Report: December 2018RAfii KerenÎncă nu există evaluări
- Management of Oral Manifestations in A Case of Cushing's HabitusDocument4 paginiManagement of Oral Manifestations in A Case of Cushing's HabitusAzzÎncă nu există evaluări
- CLASIFICACION RESUMEN Caton - Et - Al-2018-Journal - of - Clinical - PeriodontologyDocument12 paginiCLASIFICACION RESUMEN Caton - Et - Al-2018-Journal - of - Clinical - PeriodontologyDaniela RojasÎncă nu există evaluări
- G BehavGuide PDFDocument9 paginiG BehavGuide PDFAzi Pertiwi HussainÎncă nu există evaluări
- Ijss Oct Ra02 PDFDocument4 paginiIjss Oct Ra02 PDFAzi Pertiwi HussainÎncă nu există evaluări
- Turner HypoplasiaDocument5 paginiTurner HypoplasiaAzi Pertiwi HussainÎncă nu există evaluări
- Enamel Defect DentititionDocument17 paginiEnamel Defect DentititionAzi Pertiwi HussainÎncă nu există evaluări
- Turner's HypoplasiaDocument4 paginiTurner's HypoplasiaAzi Pertiwi HussainÎncă nu există evaluări
- Ipi 109881Document1 paginăIpi 109881Azi Pertiwi HussainÎncă nu există evaluări
- Open Bite: A Review of Etiology and Management: Peter Ngan, DMD Henry W. Fields, DDS, MS, MSDDocument8 paginiOpen Bite: A Review of Etiology and Management: Peter Ngan, DMD Henry W. Fields, DDS, MS, MSDAzi Pertiwi HussainÎncă nu există evaluări
- Rheumatoid Arthritis: Muhammad Afif Bin Mansor Andini Pratiwi Islami SupervisorDocument19 paginiRheumatoid Arthritis: Muhammad Afif Bin Mansor Andini Pratiwi Islami SupervisorAfif MansorÎncă nu există evaluări
- HIFUDocument1 paginăHIFUKaye RabadonÎncă nu există evaluări
- Drugs That May Unmask or Worsen Myasthenia GravisDocument2 paginiDrugs That May Unmask or Worsen Myasthenia GravisnuriajiÎncă nu există evaluări
- 162 - 4187 - Hermina Novida - GalleyDocument5 pagini162 - 4187 - Hermina Novida - Galleyaulia fikriÎncă nu există evaluări
- Myasthenia Gravis. SURYADocument41 paginiMyasthenia Gravis. SURYANofilia Citra CandraÎncă nu există evaluări
- Impact of Covid 19 On EnvironmentDocument20 paginiImpact of Covid 19 On EnvironmentRamkishan JaiswarÎncă nu există evaluări
- COVID 19 - Self Attestation Form (OHC)Document1 paginăCOVID 19 - Self Attestation Form (OHC)Cristina SilistraruÎncă nu există evaluări
- Intestinal Obstruction Wit Pic2Document2 paginiIntestinal Obstruction Wit Pic2matrixtrinityÎncă nu există evaluări
- Mitral Valve SurgeryDocument2 paginiMitral Valve SurgeryLena MarieÎncă nu există evaluări
- IV. Modul 10 - Pengelolaan NyeriDocument97 paginiIV. Modul 10 - Pengelolaan NyeriGrace Noviyanthi SinambelaÎncă nu există evaluări
- Medical SpecialistsDocument2 paginiMedical SpecialistsArvin Dela CrÜzÎncă nu există evaluări
- What Is Hiv/Aids?: Human Immunodeficiency Virus (Hiv)Document2 paginiWhat Is Hiv/Aids?: Human Immunodeficiency Virus (Hiv)Rockie Geronda EsmaneÎncă nu există evaluări
- Urinary Tract Infection (UTI) in Males: Signs and SymptomsDocument33 paginiUrinary Tract Infection (UTI) in Males: Signs and Symptomssyak turÎncă nu există evaluări
- Placenta Previa ManagementDocument28 paginiPlacenta Previa ManagementAhsan AuliyaÎncă nu există evaluări
- Diagnostic Report: Patient Name: Abhinay Desaraju ABHIM21018727 0065UC002076Document2 paginiDiagnostic Report: Patient Name: Abhinay Desaraju ABHIM21018727 0065UC002076Karthikeya MoorthyÎncă nu există evaluări
- The Family NeisseriaceaeDocument8 paginiThe Family NeisseriaceaeVatha NaÎncă nu există evaluări
- 2 Months Well Child CheckDocument3 pagini2 Months Well Child CheckJanelleÎncă nu există evaluări
- Chronic Kidney Disease (Newly Identified) : Clinical Presentation and Diagnostic Approach in AdultsDocument23 paginiChronic Kidney Disease (Newly Identified) : Clinical Presentation and Diagnostic Approach in AdultsNesreden Jemal KedirÎncă nu există evaluări
- Drug Study (Schizo)Document5 paginiDrug Study (Schizo)aliannaÎncă nu există evaluări
- Drug Study For TetanusDocument10 paginiDrug Study For TetanusMei PayumoÎncă nu există evaluări
- Fluid and Electrolyte Therapy During Vomiting and DiarrheaDocument22 paginiFluid and Electrolyte Therapy During Vomiting and Diarrheafernin96Încă nu există evaluări
- Proposal RawDocument12 paginiProposal RawSedem StanisloveÎncă nu există evaluări
- Bosu 2015Document24 paginiBosu 2015José Carlos Sánchez-RamirezÎncă nu există evaluări