Documente Academic
Documente Profesional
Documente Cultură
Dss
Încărcat de
Fitria SorayaDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Dss
Încărcat de
Fitria SorayaDrepturi de autor:
Formate disponibile
A 49-year-old woman was admitted to hospital with fever for 5 days.
She had no
significant previous medical history. Her main symptoms were body aches,
headache, loss of appetite, vomiting, and high fever. On day 5 of the illness, a
full blood count showed a platelet count of 45,000 mm 3. She was admitted to the
ICU. On admission, she was conscious and alert, but was restless and looked ill.
She had a diffuse cutaneous blanching erythema. Her pulse rate was 120 beats
per minute and blood pressure 130/80mmHg, with a postural drop of 20 mmHg.
The heart sounds were normal. Her respiratory rate was 28/min, and her lungs
were clear. Her abdomen was soft, with no free fluid; epigastric and right
hypochondrial tenderness was present. She was neurologically normal. Her
electrocardiogram (ECG) was normal, apart from sinus tachycardia. DHF was the
likely clinical diagnosis. Intravenous (IV) Hartmann solution 2 ml/kg/h was
commenced in view of the postural drop in blood pressure. She became
hypotensive 4 h after admission, with blood pressure falling to 70/40 mmHg, and
her heart rate increased to 140/min. A repeat ECG showed diffuse T wave
inversions. An urgent echocardiogram showed global hypokinesia, with an
ejection fraction of 40%. Based on a clinical diagnosis of dengue shock syndrome
(DSS) plus myocarditis, dobutamine and noradrenaline infusions were started.
Repeat platelet count was 22,000mm3 and the hematocrit 48%. Fluids were
given with caution, and fresh frozen plasma (FFP) and platelet transfusion was
commenced. She then had coffee grounds aspirate through the nasogastric tube
and was therefore started on omeprazole 80 mg bolus followed by 8 mg/h
infusion. She remained in intractable shock, with no response to inotropes or
intravenous hydrocortisone, and required ventilation due to worsening
pulmonary edema. Her ECG now showed widespread T wave inversions with first-
degree heart block. She progressively deteriorated, became anuric, and
developed adult respiratory distress syndrome (ARDS). She also developed
complete heart block, for which a temporary pacemaker was inserted. Although
rate control was achieved, her blood pressure remained low on maximum
inotropes. She was started on IV immunoglobulins 0.4 mg/kg by infusion. Her
condition continued to deteriorate, and blood pressure became unrecordable.
External cardiac massage alone seemed to raise the blood pressure to recordable
levels. Repeat echocardiogram showed a dilated, globally hypokinetic heart, and
it appeared that the myocardium was not responding to inotropes at all. She died
in asystole shortly afterwards, 15 h after admission. Investigation results
received after the patients death showed positive IgM and IgG antibodies to
dengue. Dengue PCR was also positive. All bacterial cultures were negative.
Serum cortisol levels were normal.
Box 1: WHO case definitions for dengue shock[1]
Features of dengue hemorrhagic fever
Fever, or history of acute fever, lasting 27 days, occasionally biphasic
Hemorrhagic tendencies, evidenced by at least one of the following
A positive tourniquet test
Petechiae, ecchymoses, or purpura
Bleeding from the mucosa, gastrointestinal tract, injection sites, or other
locations
Hematemesis or melena
Thrombocytopenia (100000/mm3 or less)
Evidence of plasma leakage due to increased vascular permeability, manifested by at
least one of the following;
A rise in hematocrit 20% above the average for age, sex and population
A drop in hematocrit following volume replacement equal to or greater than
20% of the baseline
Signs of plasma leakage such as pleural effusion, ascites or hypoproteinemia
All four of the above PLUS evidence of circulatory failure, manifested by
Rapid weak pulse, and
Narrow pulse pressure (<20mmHg) OR
Hypotension for age, and
Cold, clammy skin, and restlessness
S-ar putea să vă placă și
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- GBSDocument19 paginiGBSRahma ArsellaÎncă nu există evaluări
- Chapter 32 - Stop-Controlled Intersections Supp - 600Document74 paginiChapter 32 - Stop-Controlled Intersections Supp - 600Ana María Lira CastroÎncă nu există evaluări
- ECAM2015 324369 PDFDocument6 paginiECAM2015 324369 PDFLuiz Otavio CostaÎncă nu există evaluări
- 1000 Calorie ChallengesDocument25 pagini1000 Calorie ChallengesFrancesco Iavarone100% (3)
- CalculationsDocument9 paginiCalculationssantthana100% (1)
- Communication Boards in Critical CareDocument9 paginiCommunication Boards in Critical CareSeresolÎncă nu există evaluări
- MLP by StateDocument12 paginiMLP by StateFlor OMÎncă nu există evaluări
- Resume-Perry Duane GriceDocument4 paginiResume-Perry Duane Griceapi-297972018Încă nu există evaluări
- Pacificgoldenplover Microbe Mission Practice TestDocument5 paginiPacificgoldenplover Microbe Mission Practice TestsandeeptaraÎncă nu există evaluări
- Zambia Medicines Regulatory AuthorityDocument5 paginiZambia Medicines Regulatory AuthoritydaviesÎncă nu există evaluări
- Detailed Job Description - RaqsDocument3 paginiDetailed Job Description - RaqsBarga John0% (1)
- The Tragedy of Schizophrenia Without PsychotherapyDocument30 paginiThe Tragedy of Schizophrenia Without PsychotherapyRachel AHÎncă nu există evaluări
- Chapter 4 Marketing Department: Company 1-Apollo Hospitals Enterprises LTD (Apollo)Document20 paginiChapter 4 Marketing Department: Company 1-Apollo Hospitals Enterprises LTD (Apollo)TYB92BINDRA GURSHEEN KAUR R.Încă nu există evaluări
- Al-Hijamah (Cupping) - Healing The Sunnah Way - Amjad Ahsan AliDocument194 paginiAl-Hijamah (Cupping) - Healing The Sunnah Way - Amjad Ahsan Alihal bannaÎncă nu există evaluări
- Manila Central University College of Medicine Department of PediatricsDocument7 paginiManila Central University College of Medicine Department of PediatricsKirstie de LunaÎncă nu există evaluări
- Cancer Bush 2013Document2 paginiCancer Bush 2013mghaffarzadehÎncă nu există evaluări
- Coliform Analysis in Wastewater 2012Document24 paginiColiform Analysis in Wastewater 2012engrbvgÎncă nu există evaluări
- Global Developmental DelayDocument2 paginiGlobal Developmental DelayAtlerÎncă nu există evaluări
- HIV & TBDocument51 paginiHIV & TBRhea DerijeÎncă nu există evaluări
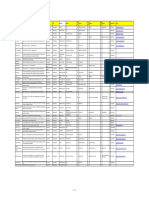
- Name Clinic/Hosp/Med Name &address Area City Speciality SEWA01 Disc 01 SEWA02 DIS C02 SEWA03 Disc 03 SEWA04 DIS C04 Contact No. EmailDocument8 paginiName Clinic/Hosp/Med Name &address Area City Speciality SEWA01 Disc 01 SEWA02 DIS C02 SEWA03 Disc 03 SEWA04 DIS C04 Contact No. EmailshrutiÎncă nu există evaluări
- Acid Base WorkshopDocument71 paginiAcid Base WorkshopLSU Nephrology Transplant Dialysis AccessÎncă nu există evaluări
- Anterior Teeth Arrangement 2Document1 paginăAnterior Teeth Arrangement 2Muhammed MansoorÎncă nu există evaluări
- The Aptitude HandbookDocument295 paginiThe Aptitude HandbookSomesh SharmaÎncă nu există evaluări
- Chapter Review: True or FalseDocument2 paginiChapter Review: True or FalseJames Gabriel SalardaÎncă nu există evaluări
- Pain Management: Dr. Prabowo Wicaksono Span Bagian/Smf Anestesi FK Unissula/Rsisa 2007Document27 paginiPain Management: Dr. Prabowo Wicaksono Span Bagian/Smf Anestesi FK Unissula/Rsisa 2007Fendy PrasetyoÎncă nu există evaluări
- Osnove FarmakokinetikeDocument46 paginiOsnove Farmakokinetikeapi-3814389Încă nu există evaluări
- CHAPTER 11: The History and Physical Examination: An Evidence Based ApproachDocument5 paginiCHAPTER 11: The History and Physical Examination: An Evidence Based ApproachReda SoÎncă nu există evaluări
- Anatomi CT Scan AbdomenDocument17 paginiAnatomi CT Scan Abdomenwawan saifullahÎncă nu există evaluări
- AA Dermatologia in MCC 2018Document61 paginiAA Dermatologia in MCC 2018marviÎncă nu există evaluări
- Drugs Used in The Management of COPDDocument6 paginiDrugs Used in The Management of COPDASWINI GÎncă nu există evaluări