Documente Academic
Documente Profesional
Documente Cultură
Document PDF
Încărcat de
Fahrizal Kusuma WTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Document PDF
Încărcat de
Fahrizal Kusuma WDrepturi de autor:
Formate disponibile
Urinary tr
tract
act infection in under 16s:
diagnosis and management
Clinical guideline
Published: 22 August 2007
nice.org.uk/guidance/cg54
NICE 2007. All rights reserved.
Urinary tract infection in under 16s: diagnosis and management (CG54)
Your responsibility
The recommendations in this guideline represent the view of NICE, arrived at after careful
consideration of the evidence available. When exercising their judgement, professionals are
expected to take this guideline fully into account, alongside the individual needs, preferences and
values of their patients or service users. The application of the recommendations in this guideline
are not mandatory and the guideline does not override the responsibility of healthcare
professionals to make decisions appropriate to the circumstances of the individual patient, in
consultation with the patient and/or their carer or guardian.
Local commissioners and/or providers have a responsibility to enable the guideline to be applied
when individual health professionals and their patients or service users wish to use it. They should
do so in the context of local and national priorities for funding and developing services, and in light
of their duties to have due regard to the need to eliminate unlawful discrimination, to advance
equality of opportunity and to reduce health inequalities. Nothing in this guideline should be
interpreted in a way that would be inconsistent with compliance with those duties.
NICE 2007. All rights reserved. Page 2 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
Contents
Overview .............................................................................................................................................................................. 5
Who is it for? .................................................................................................................................................................................... 5
Introduction ........................................................................................................................................................................ 6
Child-centred care ............................................................................................................................................................ 7
Key priorities for implementation .............................................................................................................................. 8
1 Guidance ........................................................................................................................................................................... 11
1.1 Diagnosis.................................................................................................................................................................................... 11
1.2 Acute management................................................................................................................................................................ 17
1.3 Imaging tests............................................................................................................................................................................. 19
1.4 Surgical intervention............................................................................................................................................................. 22
1.5 Follow-up ................................................................................................................................................................................... 23
1.6 Information and advice for children, young people and parents or carers...................................................... 23
2 Notes on the scope of the guidance ....................................................................................................................... 25
3 Implementation in the NHS....................................................................................................................................... 26
4 Research recommendations ..................................................................................................................................... 27
4.1 Diagnosis.................................................................................................................................................................................... 27
4.2 Antibiotic prophylaxis........................................................................................................................................................... 27
4.3 Surgical intervention............................................................................................................................................................. 28
4.4 Long-term risk.......................................................................................................................................................................... 28
5 Other versions of this guideline............................................................................................................................... 29
5.1 Full guideline............................................................................................................................................................................. 29
5.2 Information for the public ................................................................................................................................................... 29
6 Related NICE guidance................................................................................................................................................ 30
7 Updating the guideline ................................................................................................................................................ 31
Appendix A: The Guideline Development Group................................................................................................. 32
National Collaborating Centre for Women's and Children's Health staff .............................................................. 33
NICE 2007. All rights reserved. Page 3 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
Acknowledgements....................................................................................................................................................................... 33
Appendix B: The Guideline Review Panel................................................................................................................ 34
About this guideline ......................................................................................................................................................... 35
NICE 2007. All rights reserved. Page 4 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
This guideline is the basis of QS36 and QS64.
Ov
Overview
erview
This guideline covers diagnosing and managing first or recurrent upper or lower tract urinary tract
infection in infants, children and young people. It aims to achieve more consistent clinical practice,
based on accurate diagnosis and effective management.
Who is it for?
Healthcare professionals
Commissioners
Infants and children from birth up to the age of 16 years with urinary tract infection, their
families and carers
NICE 2007. All rights reserved. Page 5 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
Introduction
In the past 3050 years, the natural history of urinary tract infection (UTI) in children has changed
as a result of the introduction of antibiotics and improvements in healthcare. This change has
contributed to uncertainty about the most appropriate and effective way to manage UTI in
children, and whether or not investigations and follow-up are justified.
UTI is a common bacterial infection causing illness in infants and children. It may be difficult to
recognise UTI in children because the presenting symptoms and signs are non-specific, particularly
in infants and children younger than 3 years. Collecting urine and interpreting results are not easy
in this age group, so it may not always be possible to unequivocally confirm the diagnosis.
Current management, which includes imaging, prophylaxis and prolonged follow-up, has placed a
heavy burden on NHS primary and secondary care resources. It is costly, based on limited evidence
and is unpleasant for children and distressing for their parents or carers. The aim of this guideline is
to achieve more consistent clinical practice, based on accurate diagnosis and effective
management.
NICE 2007. All rights reserved. Page 6 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
Child-centred care
This guideline offers best practice advice on the care of infants, children and young people younger
than 16 years with UTI.
Treatment and care should take into account children's needs and preferences, as well as those of
their parents or carers. Children with UTI should have the opportunity to make informed decisions
about their care and treatment in partnership with their healthcare professionals, but this depends
on their age and capacity to make decisions. It is good practice for healthcare professionals to
involve children and their parents or carers in the decision-making process. Where a child is not old
enough or does not have the capacity to make decisions, healthcare professionals should follow the
Department of Health's advice on consent and the code of practice that accompanies the Mental
Capacity Act. In Wales, healthcare professionals should follow advice on consent from the Welsh
Government.
If the patient is under 16, healthcare professionals should follow the guidelines in the Department
of Health's Seeking consent: working with children.
Good communication between healthcare professionals and children and their parents or carers is
essential. It should be supported by evidence-based written information tailored to the person's
needs. Treatment and care, and the information given about this, should be culturally appropriate.
It should also be accessible to people with additional needs such as physical, sensory or learning
disabilities, and to people who do not speak or read English.
Parents or carers should have the opportunity to be involved in decisions about their child's care
and treatment. Parents or carers also need to give consent to their child's care.
Parents or carers should also be given the information and support they need.
NICE 2007. All rights reserved. Page 7 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
Key priorities for implementation
Symptoms and signs
Infants and children presenting with unexplained fever of 38C or higher should have a urine
sample tested after 24 hours at the latest.
Infants and children with symptoms and signs suggestive of urinary tract infection (UTI) should
have a urine sample tested for infection. Table 1 is a guide to the symptoms and signs that
infants and children present with.
Urine collection
A clean catch urine sample is the recommended method for urine collection. If a clean catch
urine sample is unobtainable:
Other non-invasive methods such as urine collection pads should be used. It is
important to follow the manufacturers' instructions when using urine collection pads.
Cotton wool balls, gauze and sanitary towels should not be used to collect urine in
infants and children.
When it is not possible or practical to collect urine by non-invasive methods, catheter
samples or suprapubic aspiration (SPA) should be used.
Before SPA is attempted, ultrasound guidance should be used to demonstrate the
presence of urine in the bladder.
Urine testing
The urine-testing strategies shown in tables 25 are recommended.[ ] 1
History and e
examination
xamination on confirmed UTI
The following risk factors for UTI and serious underlying pathology should be recorded:
poor urine flow
history suggesting previous UTI or confirmed previous UTI
recurrent fever of uncertain origin
antenatally-diagnosed renal abnormality
NICE 2007. All rights reserved. Page 8 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
family history of vesicoureteric reflux (VUR) or renal disease
constipation
dysfunctional voiding
enlarged bladder
abdominal mass
evidence of spinal lesion
poor growth
high blood pressure.
Acute management
Infants younger than 3 months with a possible UTI should be referred immediately to the care
of a paediatric specialist. Treatment should be with parenteral antibiotics in line with Feverish
illness in children(NICE clinical guideline 47).
For infants and children 3 months or older with acute pyelonephritis/upper urinary tract
infection:
consider referral to a paediatric specialist
treat with oral antibiotics for 710 days. The use of an oral antibiotic with low
resistance patterns is recommended, for example cephalosporin or co-amoxiclav
if oral antibiotics cannot be used, treat with an intravenous (IV) antibiotic agent such as
cefotaxime or ceftriaxone for 24 days followed by oral antibiotics for a total duration
of 10 days.
For infants and children 3 months or older with cystitis/lower urinary tract infection:
treat with oral antibiotics for 3 days. The choice of antibiotics should be directed by
locally developed multidisciplinary guidance. Trimethoprim, nitrofurantoin,
cephalosporin or amoxicillin may be suitable
the parents or carers should be advised to bring the infant or child for reassessment if
the infant or child is still unwell after 2448 hours. If an alternative diagnosis is not
NICE 2007. All rights reserved. Page 9 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
made, a urine sample should be sent for culture to identify the presence of bacteria and
determine antibiotic sensitivity if urine culture has not already been carried out.
Antibiotic proph
prophylaxis
ylaxis
Antibiotic prophylaxis should not be routinely recommended in infants and children following
first-time UTI.
Imaging tests
Infants and children who have had a UTI should be imaged as outlined in tables 6, 7 and 8.
[1]
Assess the risk of serious illness in line with Feverish illness in children (NICE clinical guideline 47)
to ensure appropriate urine tests and interpretation, both of which depend on the child's age and
risk of serious illness.
NICE 2007. All rights reserved. Page 10 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
1 Guidance
The following guidance is based on the best available evidence. The full guideline gives details of
the methods and the evidence used to develop the guidance (see section 5 for details).
1.1 Diagnosis
1.1.1 Symptoms and signs
1.1.1.1 Infants and children presenting with unexplained fever of 38C or higher should
have a urine sample tested after 24 hours at the latest.
1.1.1.2 Infants and children with an alternative site of infection should not have a urine
sample tested. When infants and children with an alternative site of infection
remain unwell, urine testing should be considered after 24 hours at the latest.
1.1.1.3 Infants and children with symptoms and signs suggestive of urinary tract
infection (UTI) should have a urine sample tested for infection. Table 1 is a guide
to the symptoms and signs that infants and children present with.
Table 1 Presenting symptoms and signs in infants and children with UTI
Age group Symptoms and signs
Most common ------------------> Least common
Infants yyounger
ounger than 3 months Fever Poor feeding Abdominal
Vomiting Failure to thrive pain
Lethargy Jaundice
Irritability Haematuria
Offensive
urine
NICE 2007. All rights reserved. Page 11 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
Infants and children, 3 months or Pre
Prevverbal Fever Abdominal pain Lethargy
older Loin tenderness Irritability
Vomiting Haematuria
Poor feeding Offensive
urine
Failure to
thrive
Verbal Frequency Dysfunctional Fever
Dysuria voiding Malaise
Changes to Vomiting
continence
Haematuria
Abdominal pain
Offensive
Loin tenderness urine
Cloudy urine
1.1.2 Assessment of risk of serious illness
1.1.2.1 The illness level in infants and children should be assessed in accordance with
recommendations in Feverish illness in children (NICE clinical guideline 47).
1.1.3 Urine collection
1.1.3.1 A clean catch urine sample is the recommended method for urine collection. If a
clean catch urine sample is unobtainable:
Other non-invasive methods such as urine collection pads should be used. It is
important to follow the manufacturer's instructions when using urine collection pads.
Cotton wool balls, gauze and sanitary towels should not be used to collect urine in
infants and children.
When it is not possible or practical to collect urine by non-invasive methods, catheter
samples or suprapubic aspiration (SPA) should be used.
Before SPA is attempted, ultrasound guidance should be used to demonstrate the
presence of urine in the bladder.
NICE 2007. All rights reserved. Page 12 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
1.1.3.2 In an infant or child with a high risk of serious illness it is highly preferable that a
urine sample is obtained; however, treatment should not be delayed if a urine
sample is unobtainable.
1.1.4 Urine preservation
1.1.4.1 If urine is to be cultured but cannot be cultured within 4 hours of collection, the
sample should be refrigerated or preserved with boric acid immediately.
1.1.4.2 The manufacturer's instructions should be followed when boric acid is used to
ensure the correct specimen volume to avoid potential toxicity against bacteria
in the specimen.
1.1.5 Urine testing
1.1.5.1 The urine-testing strategies shown in tables 25 are recommended.[ ] 2
As with all diagnostic tests there will be a small number of false negative results; therefore clinicians should
use clinical criteria for their decisions in cases where urine testing does not support the findings.
Table 2 Urine-testing str
strategy
ategy for infants yyounger
ounger than 3 months
All infants younger than 3 months with suspected UTI (see table 1) should be referred to
paediatric specialist care and a urine sample should be sent for urgent microscopy and culture.
These infants should be managed in accordance with the recommendations for this age group
in Feverish illness in children (NICE clinical guideline 47).
Table 3 Urine-testing str
strategies
ategies for infants and children 3 months or older but yyounger
ounger than 3 years
Urgent microscopy and culture is the preferred method for diagnosing UTI in this age group;
this should be used where possible.
If the Urgent microscopy and culture should be arranged and antibiotic treatment
infant or should be started.
child has When urgent microscopy is not available, a urine sample should be sent for
specific microscopy and culture, and antibiotic treatment should be started.
urinary
symptoms
NICE 2007. All rights reserved. Page 13 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
If the For an infant or child with a high risk of serious illness: the infant or child should
symptoms be urgently referred to a paediatric specialist where a urine sample should be
are non- sent for urgent microscopy and culture. Such infants and children should be
specific to managed in line with Feverish illness in children (NICE clinical guideline 47).
UTI
For an infant or child with an intermediate risk of serious illness: if the situation
demands, the infant or child may be referred urgently to a paediatric specialist.
For infants and children who do not require paediatric specialist referral,
urgent microscopy and culture should be arranged. Antibiotic treatment should
be started if microscopy is positive (see table 5). When urgent microscopy is not
available, dipstick testing may act as a substitute. The presence of nitrites
suggests the possibility of infection and antibiotic treatment should be started
(see table 4). In all cases, a urine sample should be sent for microscopy and
culture.
For an infant or child with a low risk of serious illness: microscopy and culture
should be arranged. Antibiotic treatment should only be started if microscopy
or culture is positive.
Table 4 Urine-testing str
strategies
ategies for children 3 years or older
Dipstick testing for leukocyte esterase and nitrite is diagnostically as useful as microscopy and
culture, and can safely be used.
If both The child should be regarded as having UTI and antibiotic treatment should be
leuk
leukocyte
ocyte started. If a child has a high or intermediate risk of serious illness and/or a past
ester
esterase
ase history of previous UTI, a urine sample should be sent for culture.
and nitrite
are positiv
positivee
If leuk
leukocyte
ocyte Antibiotic treatment should be started if the urine test was carried out on a
ester
esterase
ase is fresh sample of urine. A urine sample should be sent for culture. Subsequent
negativ
negative e management will depend upon the result of urine culture.
and nitrite is
positiv
positivee
NICE 2007. All rights reserved. Page 14 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
If leuk
leukocyte
ocyte A urine sample should be sent for microscopy and culture. Antibiotic treatment
ester
esterase
ase is for UTI should not be started unless there is good clinical evidence of UTI (for
positiv
positivee and example, obvious urinary symptoms). Leukocyte esterase may be indicative of an
nitrite is infection outside the urinary tract which may need to be managed differently.
negativ
negative e
If both The child should not be regarded as having UTI. Antibiotic treatment for UTI
leuk
leukocyte
ocyte should not be started, and a urine sample should not be sent for culture. Other
ester
esterase
ase causes of illness should be explored.
and nitrite
are negativ
negativee
Table 5 Guidance on the interpretation of microscop
microscopyy results
Microscop
Microscopyy Pyuria positiv
positivee Pyuria negativ
negativee
results
Bacteriuria The infant or child should be The infant or child should be regarded
positiv
positivee regarded as having UTI as having UTI
Bacteriuria Antibiotic treatment should be The infant or child should be regarded
negativ
negativee started if clinically UTI as not having UTI
1.1.6 Indication for culture
1.1.6.1 Urine samples should be sent for culture:
in infants and children who have a diagnosis of acute pyelonephritis/upper urinary
tract infection (see 1.1.8.1)
in infants and children with a high to intermediate risk of serious illness
in infants and children under 3 years
in infants and children with a single positive result for leukocyte esterase or nitrite
in infants and children with recurrent UTI
in infants and children with an infection that does not respond to treatment within
2448 hours, if no sample has already been sent
NICE 2007. All rights reserved. Page 15 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
when clinical symptoms and dipstick tests do not correlate.
1.1.7 History and e
examination
xamination on confirmed UTI
1.1.7.1 The following risk factors for UTI and serious underlying pathology should be
recorded:
poor urine flow
history suggesting previous UTI or confirmed previous UTI
recurrent fever of uncertain origin
antenatally-diagnosed renal abnormality
family history of vesicoureteric reflux (VUR) or renal disease
constipation
dysfunctional voiding
enlarged bladder
abdominal mass
evidence of spinal lesion
poor growth
high blood pressure.
1.1.8 Clinical differentiation between acute p pyyelonephritis/upper urinary tr
tract
act
infection and cystitis/lower urinary tr
tract
act infection
1.1.8.1 Infants and children who have bacteriuria and fever of 38C or higher should be
considered to have acute pyelonephritis/upper urinary tract infection. Infants
and children presenting with fever lower than 38C with loin pain/tenderness
and bacteriuria should also be considered to haveacute pyelonephritis/upper
urinary tract infection. All other infants and children who have bacteriuria but
no systemic symptoms or signs should be considered to have cystitis/lower
urinary tract infection.
NICE 2007. All rights reserved. Page 16 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
1.1.9 Labor
Laboratory
atory tests for localising UTI
1.1.9.1 C-reactive protein alone should not be used to differentiate acute
pyelonephritis/upper urinary tract infection from cystitis/lower urinary tract
infection in infants and children.
1.1.10 Imaging tests for localising UTI
1.1.10.1 The routine use of imaging in the localisation of a UTI is not recommended.
1.1.10.2 In the rare instances when it is clinically important to confirm or exclude acute
pyelonephritis/upper urinary tract infection, power Doppler ultrasound is
recommended. When this is not available or the diagnosis still cannot be
confirmed, a dimercaptosuccinic acid (DMSA) scintigraphy scan is
recommended.
1.2 Acute management
Note that the antibiotic requirements for infants and children with conditions that are outside the scope of
this guideline (for example, infants and children already known to have significant pre-existing uropathies)
have not been addressed and may be different from those given here.
1.2.1.1 Infants and children with a high risk of serious illness should be referred
urgently to the care of a paediatric specialist.
1.2.1.2 Infants younger than 3 months with a possible UTI should be referred
immediately to the care of a paediatric specialist. Treatment should be with
parenteral antibiotics in line with Feverish illness in children (NICE clinical
guideline 47).
1.2.1.3 For infants and children 3 months or older with acute pyelonephritis/upper
urinary tract infection:
consider referral to a paediatric specialist
treat with oral antibiotics for 710 days. The use of an oral antibiotic with low
resistance patterns is recommended, for example cephalosporin or co-amoxiclav
NICE 2007. All rights reserved. Page 17 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
if oral antibiotics cannot be used, treat with an intravenous (IV) antibiotic agent such as
cefotaxime or ceftriaxone for 24 days followed by oral antibiotics for a total duration
of 10 days.
1.2.1.4 For infants and children 3 months or older with cystitis/lower urinary tract
infection:
treat with oral antibiotics for 3 days. The choice of antibiotics should be directed by
locally developed multidisciplinary guidance. Trimethoprim, nitrofurantoin,
cephalosporin or amoxicillin may be suitable.
the parents or carers should be advised to bring the infant or child for reassessment if
the infant or child is still unwell after 2448 hours. If an alternative diagnosis is not
made, a urine sample should be sent for culture to identify the presence of bacteria
and determine antibiotic sensitivity if urine culture has not already been carried out.
1.2.1.5 For infants and children who receive aminoglycosides (gentamicin or amikacin),
once daily dosing is recommended.
1.2.1.6 If parenteral treatment is required and IV treatment is not possible,
intramuscular treatment should be considered.
1.2.1.7 If an infant or child is receiving prophylactic medication and develops an
infection, treatment should be with a different antibiotic, not a higher dose of
the same antibiotic.
1.2.1.8 Asymptomatic bacteriuria in infants and children should not be treated with
antibiotics.
1.2.1.9 Laboratories should monitor resistance patterns of urinary pathogens and make
this information routinely available to prescribers.
1.2.2 Pre
Prevvention of recurrence
1.2.2.1 Dysfunctional elimination syndromes and constipation should be addressed in
infants and children who have had a UTI.
1.2.2.2 Children who have had a UTI should be encouraged to drink an adequate
amount.
NICE 2007. All rights reserved. Page 18 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
1.2.2.3 Children who have had a UTI should have ready access to clean toilets when
required and should not be expected to delay voiding.
1.2.3 Antibiotic proph
prophylaxis
ylaxis
1.2.3.1 Antibiotic prophylaxis should not be routinely recommended in infants and
children following first-time UTI.
1.2.3.2 Antibiotic prophylaxis may be considered in infants and children with recurrent
UTI.
1.2.3.3 Asymptomatic bacteriuria in infants and children should not be treated with
prophylactic antibiotics.
1.3 Imaging tests
1.3.1.1 Infants and children with atypical UTI (see box 1) should have ultrasound of the
urinary tract during the acute infection to identify structural abnormalities of
the urinary tract such as obstruction, as outlined in tables 6, 7 and 8. This is to
ensure prompt management.
1.3.1.2 For infants younger than 6 months with first-time UTI that responds to
treatment, ultrasound should be carried out within 6 weeks of the UTI, as
outlined in table 6.
1.3.1.3 For infants and children aged 6 months and older with first-time UTI that
responds to treatment, routine ultrasound is not recommended unless the
infant or child has atypical UTI, as outlined in tables 7 and 8.
1.3.1.4 Infants and children who have had a lower urinary tract infection should
undergo ultrasound (within 6 weeks) only if they are younger than 6 months or
have had recurrent infections.
1.3.1.5 A DMSA scan 46 months following the acute infection should be used to detect
renal parenchymal defects, as outlined in tables 6, 7 and 8.
1.3.1.6 If the infant or child has a subsequent UTI while awaiting DMSA, the timing of
the DMSA should be reviewed and consideration given to doing it sooner.
NICE 2007. All rights reserved. Page 19 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
1.3.1.7 Routine imaging to identify VUR is not recommended for infants and children
who have had a UTI, except in specific circumstances, as outlined in tables 6, 7
and 8.
1.3.1.8 When a micturating cystourethrogram (MCUG) is performed, prophylactic
antibiotics should be given orally for 3 days with MCUG taking place on the
second day.
1.3.1.9 Infants and children who have had a UTI should be imaged as outlined in
tables 6, 7 and 8.
Table 6 Recommended imaging schedule for infants yyounger
ounger than 6 months
Test Responds well to treatment Atypical Recurrent
within 48 hours UTIa UTIa
Ultrasound during the acute No Yesc Yes
infection
Ultrasound within 6 weeks Yesb No No
DMSA 46 months following the No Yes Yes
acute infection
MCUG No Yes Yes
a
See box 1 for definition
b
If abnormal consider MCUG
c
In an infant or child with a non-E. coli-UTI, responding well to antibiotics and with no other
features of atypical infection, the ultrasound can be requested on a non-urgent basis to take
place within 6 weeks
Table 7 Recommended imaging schedule for infants and children 6 months or older but yyounger
ounger
than 3 years
Test Responds well to treatment Atypical Recurrent
within 48 hours UTIa UTIa
Ultrasound during the acute No Yes c No
infection
NICE 2007. All rights reserved. Page 20 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
Ultrasound within 6 weeks No No Yes
DMSA 46 months following the No Yes Yes
acute infection
MCUG No Nob Nob
a
See box 1 for definition
b
While MCUG should not be performed routinely it should be considered if the following
features are present:
dilatation on ultrasound
poor urine flow
non-E. coli-infection
family history of VUR.
c
In an infant or child with a non-E. coli-UTI, responding well to antibiotics and with no other
features of atypical infection, the ultrasound can be requested on a non-urgent basis to take
place within 6 weeks
Table 8 Recommended imaging schedule for children 3 yyears
ears or older
Test Responds well to treatment Atypical Recurrent
within 48 hours UTIa UTIa
Ultrasound during the acute No Yesb c No
infection
Ultrasound within 6 weeks No No Yesb
DMSA 46 months following the No No Yes
acute infection
MCUG No No No
NICE 2007. All rights reserved. Page 21 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
a
See box 1 for definition
b
Ultrasound in toilet-trained children should be performed with a full bladder with an estimate
of bladder volume before and after micturition.
c
In a child with a non-E. coli-UTI, responding well to antibiotics and with no other features of
atypical infection, the ultrasound can be requested on a non-urgent basis to take place within
6 weeks
Bo
Boxx 1 Definitions of atypical and recurrent UTI
Atypical UTI includes:
seriously ill (for more information refer to Feverish illness in children [NICE clinical
guideline 47])
poor urine flow
abdominal or bladder mass
raised creatinine
septicaemia
failure to respond to treatment with suitable antibiotics within 48 hours
infection with non-E. coli organisms.
Recurrent UTI:
two or more episodes of UTI with acute pyelonephritis/upper urinary tract infection, or
one episode of UTI with acute pyelonephritis/upper urinary tract infection plus one or more
episode of UTI with cystitis/lower urinary tract infection, or
three or more episodes of UTI with cystitis/lower urinary tract infection.
1.4 Surgical intervention
1.4.1.1 Surgical management of VUR is not routinely recommended.
NICE 2007. All rights reserved. Page 22 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
1.5 Follow-up
1.5.1.1 Infants and children who do not undergo imaging investigations should not
routinely be followed up.
1.5.1.2 The way in which the results of imaging will be communicated should be agreed
with the parents or carers or the young person as appropriate.
1.5.1.3 When results are normal, a follow-up outpatient appointment is not routinely
required. Parents or carers should be informed of the results of all the
investigations in writing.
1.5.1.4 Infants and children who have recurrent UTI or abnormal imaging results should
be assessed by a paediatric specialist.
1.5.1.5 Assessment of infants and children with renal parenchymal defects should
include height, weight, blood pressure and routine testing for proteinuria.
1.5.1.6 Infants and children with a minor, unilateral renal parenchymal defect do not
need long-term follow-up unless they have recurrent UTI or family history or
lifestyle risk factors for hypertension.
1.5.1.7 Infants and children who have bilateral renal abnormalities, impaired kidney
function, raised blood pressure and/or proteinuria should receive monitoring
and appropriate management by a paediatric nephrologist to slow the
progression of chronic kidney disease.
1.5.1.8 Infants and children who are asymptomatic following an episode of UTI should
not routinely have their urine re-tested for infection.
1.5.1.9 Asymptomatic bacteriuria is not an indication for follow-up.
1.6 Information and advice for children, young people and parents or carers
1.6.1.1 Healthcare professionals should ensure that when a child or young person has
been identified as having a suspected UTI, they and their parents or carers as
appropriate are given information about the need for treatment, the importance
NICE 2007. All rights reserved. Page 23 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
of completing any course of treatment and advice about prevention and
possible long-term management.
1.6.1.2 Healthcare professionals should ensure that children and young people, and
their parents or carers as appropriate, are aware of the possibility of a UTI
recurring and understand the need for vigilance and to seek prompt treatment
from a healthcare professional for any suspected reinfection.
1.6.1.3 Healthcare professionals should offer children and young people and/or their
parents or carers appropriate advice and information on:
prompt recognition of symptoms
urine collection, storage and testing
appropriate treatment options
prevention
the nature of and reason for any urinary tract investigation
prognosis
reasons and arrangements for long-term management if required.
[2]
Assess the risk of serious illness in line with Feverish illness in children (NICE clinical guideline 47)
to ensure appropriate urine tests and interpretation, both of which depend on the child's age and
risk of serious illness.
NICE 2007. All rights reserved. Page 24 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
2 Notes on the scope of the guidance
NICE guidelines are developed in accordance with a scope that defines what the guideline will and
will not cover.
The guideline has been developed with the aim of providing guidance on several aspects of UTI in
infants and children from birth up to the age of 16 years, including: when to consider the diagnosis
of UTI in sick and/or symptomatic infants and children who were previously healthy; urine
collection for the diagnosis of UTI in infants and children; tests to establish or exclude UTI;
treatment, including symptomatic reinfection; use of prophylactic antibiotics and investigations to
assess the structure and function of the urinary tract; referral to secondary and tertiary care;
surgical intervention; long-term follow-up; and advice to give to parents or carers, including what
to do if another UTI occurs.
Areas not addressed by the guideline include children with urinary catheters in situ, children with
neurogenic bladders, children already known to have significant pre-existing uropathies, children
with underlying renal disease (for example, nephrotic syndrome), immunosupressed children, and
infants and children in intensive care units. It also does not cover preventive measures or long-term
management of sexually active girls with recurrent UTI.
How this guideline was de
devveloped
NICE commissioned the National Collaborating Centre for Women's and Children's Health to
develop this guideline. The Centre established a Guideline Development Group (see appendix A),
which reviewed the evidence and developed the recommendations. An independent Guideline
Review Panel oversaw the development of the guideline (see appendix B).
There is more information about how NICE clinical guidelines are developed on the NICE website.
A booklet, 'How NICE clinical guidelines are developed: an overview for stakeholders, the public
and the NHS' is available.
NICE 2007. All rights reserved. Page 25 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
3 Implementation in the NHS
The Healthcare Commission assesses the performance of NHS organisations in meeting core and
developmental standards set by the Department of Health in 'Standards for better health', issued in
July 2004. Implementation of clinical guidelines forms part of the developmental standard D2.
Core standard C5 says that national agreed guidance should be taken into account when NHS
organisations are planning and delivering care.
NICE has developed tools to help organisations implement this guidance (listed below).
Slides highlighting key messages for local discussion.
Costing tools
Costing report to estimate the national savings and costs associated with
implementation.
Costing template to estimate the local costs and savings involved.
Implementation advice on how to put the guidance into practice and national initiatives that
support this locally.
Audit criteria to monitor local practice.
The National Collaborating Centre for Women's and Children's Health and the Guideline
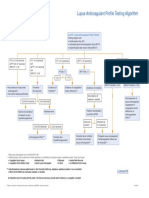
Development Group have also devised an algorithm.
NICE 2007. All rights reserved. Page 26 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
4 Research recommendations
The Guideline Development Group has made the following recommendations for research, based
on its review of evidence, to improve NICE guidance and patient care in the future. The Guideline
Development Group's full set of research recommendations is detailed in the full guideline (see
section 5).
4.1 Diagnosis
Further investigation of leukocyte esterase and nitrite dipstick tests alone and in combination,
stratified by age and method of urine collection, is required to determine their accuracy in
diagnosing UTI.
Wh
Whyy this is important
Traditionally, the diagnosis of UTI has been dependent on microscopy and culture over
2448 hours. Microscopy can be carried out immediately, but results are not always reported until
culture is available. Microscopy at the bedside is effective but requires skills that are not widely
available and requires quality assurance. This means that infants and children with distressing
symptoms have often been left untreated for 23 days while awaiting treatment. Dipsticks for
nitrite and leukocyte esterase have been shown to be as effective as microscopy and much easier to
use. There is a risk of missing a proportion of cases of acute UTI in infants and children younger
than 3 years when using dipsticks. This is because frequent bladder emptying leads to a lack of
urinary nitrate. Contaminated urine is common in non-invasive samples collected from infants and
children who are not toilet trained. The effect of this on microscopy and dipstick needs to be
evaluated.
4.2 Antibiotic prophylaxis
Well-designed randomised, double-blind, placebo-controlled trials are required to determine the
effectiveness of prophylactic antibiotics for preventing subsequent symptomatic UTIs and renal
parenchymal defects in children.
Wh
Whyy this is important
A high proportion of girls and a minority of boys with UTI develop further infections which may be
acutely distressing, associated with systemic illness and possible subsequent renal damage. Renal
damage is most likely in children with high grade VUR and this is the reason for some of the imaging
NICE 2007. All rights reserved. Page 27 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
tests previously recommended. Prophylactic antibiotics have been used on the assumption that
they prevent these problems. However, chronic antibiotic use has a number of disadvantages for
the individual as well as the population as a whole. Formal evaluation of whether prophylactic
antibiotics can prevent the distressing symptoms and scarring associated with recurrent UTI would
affect not only the use of antibiotics, but also the imaging investigations recommended.
4.3 Surgical intervention
Well-designed randomised placebo-controlled trials are required to determine the effectiveness of
prophylaxis or various surgical procedures for the management of VUR in preventing recurrent UTI
or renal parenchymal defects.
Wh
Whyy this is important
Management strategies for children with recurrent UTI have been based on the assumption that
prevention of UTI and/or renal parenchymal defects by surgery or prophylaxis is more effective in
preventing renal damage than treating symptomatic infections promptly whenever they occur. In
addition, there have been recent developments in minimally invasive surgery which have been
shown to be relatively safe and effective in reducing or eliminating VUR. Studies comparing these
interventions with adequate controls are recommended to establish the benefit of surgery in
preventing recurrent symptomatic infection and renal damage.
4.4 Long-term risk
A well designed cohort study investigating long-term outcomes including renal scarring and renal
function of children who have had UTI should be conducted in the UK.
Wh
Whyy this is important
UTI and VUR in young children have been shown to be associated with both congenital and
acquired renal damage. Progressive scarring is well documented in children with high grade VUR
and recurrent UTI. Scarring has been associated with severe hypertension, proteinuria,
complications in pregnancy and progression to established renal failure (ERF). These risks are likely
to be greater in children with bilateral renal parenchymal defects. However, the frequency and
magnitude of these risks for children with unilateral and bilateral renal damage are unclear.
Knowledge of the risk of serious or progressive complications would be useful to determine the
management of children with first-time and recurrent UTIs.
NICE 2007. All rights reserved. Page 28 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
5 Other vversions
ersions of this guideline
5.1 Full guideline
The full guideline, Urinary tract infection: diagnosis, treatment and long-term management of
urinary tract infection in children, contains details of the methods and evidence used to develop the
guideline. It is published by the National Collaborating Centre for Women's and Children's Health.
5.2 Information for the public
NICE has produced information for the public explaining this guideline.
We encourage NHS and voluntary sector organisations to use text from this information in their
own materials.
NICE 2007. All rights reserved. Page 29 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
6 Related NICE guidance
Feverish illness in children: assessment and initial management in children younger than 5 years.
NICE clinical guideline 47 (2007).
NICE 2007. All rights reserved. Page 30 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
7 Updating the guideline
NICE clinical guidelines are updated as needed so that recommendations take into account
important new information. We check for new evidence 2 and 4 years after publication, to decide
whether all or part of the guideline should be updated. If important new evidence is published at
other times, we may decide to do a more rapid update of some recommendations.
NICE 2007. All rights reserved. Page 31 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
Appendix A: The Guideline De
Devvelopment Group
Kate V
Verrier
errier Jones
Reader in Child Health, Retired (Guideline Development Group leader), University Hospital of
Wales, Cardiff
Ja
Jayy Banerjee
Consultant in Adult and Paediatric Emergency Medicine, University Hospitals of Leicester NHS
Trust
Su-Anna Boddy
Consultant Paediatric Urologist, St Georges Hospital, London
Da
David
vid Grier
Consultant Radiologist, United Bristol Healthcare NHS Trust
Lyda Jadresic
Consultant Paediatrician, Gloucestershire Hospitals Foundation NHS Trust
James Larcombe
General Practitioner, Sedgefield
Julie Marriott
Patient/carer representative
Jeni Senior
Paediatric Urology Specialist Nurse, Leicester Royal Infirmary
Kjell T
Tullus
ullus
Consultant Paediatric Nephrologist, Great Ormond Street Hospital
Sue V
Vernon
ernon
Senior Paediatric Nurse, UTI Direct Access Service, Sir James Spence Institute of Child Health
University of Newcastle and Royal Victoria Infirmary
Cr
Craig
aig Williams
Consultant Microbiologist, Royal Hospital for Sick Children, Glasgow
NICE 2007. All rights reserved. Page 32 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
National Collaborating Centre for Women's and Children's Health staff
Monica Lakhanpaul, Clinical Co-Director in Children's Health
Michael Cork
Corkett,
ett, Senior Information Specialist
Rosie Crossle
Crossleyy, Work Programme Coordinator
Anita Fitzger
Fitzgerald,
ald, Research Fellow
Rintaro Mori, Research Fellow (Project Manager)
Jeff Round, Health Economist
Samantha V
Vahidi,
ahidi, Work Programme Coordinator
Acknowledgements
Additional support was received from: Phil Alderson, Anna Burt, Martin Dougherty, Chia-Wen Lee,
Sue Lee, Neil McIntosh, Wendy Riches, Marie Westwood, and other colleagues at the National
Collaborating Centre for Women's and Children's Health.
NICE 2007. All rights reserved. Page 33 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
Appendix B: The Guideline Re
Review
view P
Panel
anel
The Guideline Review Panel is an independent panel that oversees the development of the
guideline and takes responsibility for monitoring adherence to NICE guideline development
processes. In particular, the panel ensures that stakeholder comments have been adequately
considered and responded to. The Panel includes members from the following perspectives:
primary care, secondary care, lay, public health and industry.
Dr Robert W
Walk
alker
er Chair
General Practitioner, Workington, Guideline Review Panel Chair from
June 2006
Dr John Y
Young
oung
Medical Director, Merck Sharp & Dohme Ltd
Dr John Harle
Harleyy
Clinical Governance and Prescribing Lead and General Practitioner, North Tees PCT
Mrs Ailsa Donnelly
Patient Representative
NICE 2007. All rights reserved. Page 34 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
About this guideline
NICE clinical guidelines are recommendations about the treatment and care of people with specific
diseases and conditions in the NHS in England and Wales.
The guideline was developed by the National Collaborating Centre for Women and Children's
Health. The Collaborating Centre worked with a group of healthcare professionals (including
consultants, GPs and nurses), patients and carers, and technical staff, who reviewed the evidence
and drafted the recommendations. The recommendations were finalised after public consultation.
The methods and processes for developing NICE clinical guidelines are described in The guidelines
manual.
We have produced information for the public explaining this guideline. Tools to help you put the
guideline into practice and information about the evidence it is based on are also available.
Changes after publication
June 2012: minor maintenance
Novmber 2013: minor maintenance
Your responsibility
This guidance represents the view of NICE, which was arrived at after careful consideration of the
evidence available. Healthcare professionals are expected to take it fully into account when
exercising their clinical judgement. However, the guidance does not override the individual
responsibility of healthcare professionals to make decisions appropriate to the circumstances of
the individual patient, in consultation with the patient and/or guardian or carer, and informed by
the summary of product characteristics of any drugs they are considering.
Implementation of this guidance is the responsibility of local commissioners and/or providers.
Commissioners and providers are reminded that it is their responsibility to implement the
guidance, in their local context, in light of their duties to avoid unlawful discrimination and to have
regard to promoting equality of opportunity. Nothing in this guidance should be interpreted in a
way that would be inconsistent with compliance with those duties.
Cop
Copyright
yright
NICE 2007. All rights reserved. Page 35 of 36
Urinary tract infection in under 16s: diagnosis and management (CG54)
National Institute for Health and Clinical Excellence 2007. All rights reserved. NICE copyright
material can be downloaded for private research and study, and may be reproduced for educational
and not-for-profit purposes. No reproduction by or for commercial organisations, or for
commercial purposes, is allowed without the written permission of NICE.
Contact NICE
National Institute for Health and Clinical Excellence
Level 1A, City Tower, Piccadilly Plaza, Manchester M1 4BT
www.nice.org.uk
nice@nice.org.uk
0845 0o3 7780
Accreditation
NICE 2007. All rights reserved. Page 36 of 36
S-ar putea să vă placă și
- 43861Document29 pagini43861Min-Joo Esther ParkÎncă nu există evaluări
- 23 Paediatric Urology LR FullDocument110 pagini23 Paediatric Urology LR FullRetma Rosela NurkayantyÎncă nu există evaluări
- Gupea 2077 41837 1 PDFDocument75 paginiGupea 2077 41837 1 PDFFahrizal Kusuma WÎncă nu există evaluări
- 1 s2.0 S0302283814011816 Main PDFDocument13 pagini1 s2.0 S0302283814011816 Main PDFFahrizal Kusuma WÎncă nu există evaluări
- Rekap Pasien RegistrasiDocument68 paginiRekap Pasien RegistrasiFahrizal Kusuma WÎncă nu există evaluări
- Presentasi KTI Ijal Yg FixDocument20 paginiPresentasi KTI Ijal Yg FixFahrizal Kusuma WÎncă nu există evaluări
- TB Hivmodule23.05.07Document104 paginiTB Hivmodule23.05.07Pratiwi TiwiÎncă nu există evaluări
- Maaf Banget Dho Ak Bru Kirim SKRNG, Maaf Juga Klo Seandainya Kgak Lengkap, Ntar Kamu Tambah2in Ya, Sorry BangetDocument1 paginăMaaf Banget Dho Ak Bru Kirim SKRNG, Maaf Juga Klo Seandainya Kgak Lengkap, Ntar Kamu Tambah2in Ya, Sorry BangetFahrizal Kusuma WÎncă nu există evaluări
- Analisis Pengaruh Kualitas Pelayanan Terhadap KepuasanDocument23 paginiAnalisis Pengaruh Kualitas Pelayanan Terhadap KepuasanFahrizal Kusuma WÎncă nu există evaluări
- Urinalysis: Urine Test, Hahaa Ultrasonography:: UltrasoundDocument2 paginiUrinalysis: Urine Test, Hahaa Ultrasonography:: UltrasoundFahrizal Kusuma WÎncă nu există evaluări
- Izhal - Ef@yahoo - Co.id: Jl. Kusumanegara, Semaki (Belakang SPBU) Kodya Neza Aninda Mirza Sony RollyDocument3 paginiIzhal - Ef@yahoo - Co.id: Jl. Kusumanegara, Semaki (Belakang SPBU) Kodya Neza Aninda Mirza Sony RollyFahrizal Kusuma WÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- BASF Excipients For Orally Disintegrating Tablets Make Medication EasyDocument5 paginiBASF Excipients For Orally Disintegrating Tablets Make Medication EasyVõ Đức TrọngÎncă nu există evaluări
- Umibilical Cord - ProlapsDocument22 paginiUmibilical Cord - ProlapsAtikah PurnamasariÎncă nu există evaluări
- Brody Hall - Exercício Terapêutico Na Busca Da Função, 3 Ed, 2011 (Inglês)Document802 paginiBrody Hall - Exercício Terapêutico Na Busca Da Função, 3 Ed, 2011 (Inglês)SerenelaÎncă nu există evaluări
- William S. Breitbart - Meaning-Centered Psychotherapy in The Cancer Setting - Finding Meaning and Hope in The Face of Suffering (2017, Oxford University Press)Document425 paginiWilliam S. Breitbart - Meaning-Centered Psychotherapy in The Cancer Setting - Finding Meaning and Hope in The Face of Suffering (2017, Oxford University Press)Nicole Marie-Madeleine Alberto100% (2)
- Natures Hidden Health MiracleDocument38 paginiNatures Hidden Health MiracleGorneau100% (2)
- Lupus Anticoagulant Profile Testing AlgorithmDocument1 paginăLupus Anticoagulant Profile Testing Algorithmsalamon2tÎncă nu există evaluări
- 5 - Formal ReportDocument16 pagini5 - Formal ReportJacob MarczakÎncă nu există evaluări
- OTC and PRESCRIPTION DRUGS Ppt. (TANTICO)Document10 paginiOTC and PRESCRIPTION DRUGS Ppt. (TANTICO)Ladyfair TanticoÎncă nu există evaluări
- Refresher Course: Preboard Examination Nursing Practice III: Care of Clients With Physiologic and Psychosocial Alterations (Part A)Document9 paginiRefresher Course: Preboard Examination Nursing Practice III: Care of Clients With Physiologic and Psychosocial Alterations (Part A)Jastine Sabornido0% (1)
- Practice TestDocument2 paginiPractice TestMinh Châu NguyễnÎncă nu există evaluări
- LOGIQ P5 BrochureDocument8 paginiLOGIQ P5 BrochureHery Afrianto TariganÎncă nu există evaluări
- Gynera: Coated TabletsDocument67 paginiGynera: Coated TabletsOdeke VascoÎncă nu există evaluări
- 01-2020 - Tactical Emergency Casualty Care (TECC)Document5 pagini01-2020 - Tactical Emergency Casualty Care (TECC)pibulinÎncă nu există evaluări
- Qing 2019Document9 paginiQing 2019santi lestariÎncă nu există evaluări
- Womens Knowledge Regarding Symptoms of Menopause in Al Najaf CityDocument9 paginiWomens Knowledge Regarding Symptoms of Menopause in Al Najaf CityakankshaÎncă nu există evaluări
- Management of Acute Glomerulonephritis in Children: Children's Services Medical GuidelinesDocument7 paginiManagement of Acute Glomerulonephritis in Children: Children's Services Medical GuidelinesdaypranitaÎncă nu există evaluări
- Pediatrics PDFDocument33 paginiPediatrics PDFChellapandyaÎncă nu există evaluări
- The Effects of Exercise On The Nervous SystemDocument2 paginiThe Effects of Exercise On The Nervous SystemramadanÎncă nu există evaluări
- Features of Visualization of Chronic Obstructive Pulmonary Disease in Diabetes MellitusDocument4 paginiFeatures of Visualization of Chronic Obstructive Pulmonary Disease in Diabetes MellitusCentral Asian StudiesÎncă nu există evaluări
- Delirium in Critical Care, 2nd EditionDocument248 paginiDelirium in Critical Care, 2nd EditionDuk Han KimÎncă nu există evaluări
- Getting The Most Out of The Fit Note GP GuidanceDocument28 paginiGetting The Most Out of The Fit Note GP GuidanceLaurensia Erlina NataliaÎncă nu există evaluări
- Our Lady of Fatima University College of Nursing - Cabanatuan CityDocument3 paginiOur Lady of Fatima University College of Nursing - Cabanatuan CityDanica FrancoÎncă nu există evaluări
- Quitnet Presentation-Csu StanislausDocument14 paginiQuitnet Presentation-Csu StanislausMaria Carmela CabalquintoÎncă nu există evaluări
- Salubris Medical Center: National Highway, Brgy. Roxas, Solano, Nueva VizcayaDocument10 paginiSalubris Medical Center: National Highway, Brgy. Roxas, Solano, Nueva Vizcayajulie ann afanÎncă nu există evaluări
- Maklumat Vaksinasi: Vaccination DetailsDocument2 paginiMaklumat Vaksinasi: Vaccination DetailsNORFADHLI ARIFÎncă nu există evaluări
- Certificate: of EU Product NotificationDocument2 paginiCertificate: of EU Product NotificationJsamCondoriÎncă nu există evaluări
- UntitledDocument14 paginiUntitledsyntacs skÎncă nu există evaluări
- Powerpoint TaeniasisDocument23 paginiPowerpoint TaeniasisAyshaShariff0% (1)
- Vergo 16: Betahistine Dihydrochloride Tablet 16 MGDocument4 paginiVergo 16: Betahistine Dihydrochloride Tablet 16 MGmegha_okztÎncă nu există evaluări
- Investigatory Project On AnalgesicsDocument30 paginiInvestigatory Project On AnalgesicsAnurag Singh100% (1)