Documente Academic
Documente Profesional
Documente Cultură
Maternal Deaths in The UK Pre Eclampsia Deaths Are Avoidable - 2017 - The Lancet PDF
Încărcat de
fujimeisterTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Maternal Deaths in The UK Pre Eclampsia Deaths Are Avoidable - 2017 - The Lancet PDF
Încărcat de
fujimeisterDrepturi de autor:
Formate disponibile
Comment
Maternal deaths in the UK: pre-eclampsia deaths are avoidable
Being pregnant in the UK has never been safer. The and mental health problems is clearly still a vital
latest Condential Enquiries into Maternal Deaths concern.
and Morbidity1 reported that fewer than one in In addition to ongoing surveillance of triennial
10 000 women died in or around pregnancy in the UK maternal deaths, the report examined deaths related
during 201214 (241 women within the triennium), to cardiovascular and hypertensive diseases, early
the lowest rate recorded since such surveillance began pregnancy problems, and critical care between
in 1952 in England and Wales. This maternal mortality 2009 and 2014. Indirect maternal deaths, related to
rate is lower than age-matched male death rates underlying conditions exacerbated by pregnancy, are
(517 per 10 000 population for men aged 2044 years increasingly important and now represent 59% of total
in England and Wales, 2014) such that a man is more maternal deaths; 153 women died from heart disease
likely to die while his partner is pregnant than she is.2 between 2009 and 2014, representing about a third
Several important messages emerge from the of all maternal deaths.1 Specialist multidisciplinary care
latest Condential Enquiries into Maternal Deaths for women with known heart disease, particularly with
and Morbidity: cardiac disease is the leading cause prosthetic valves, together with prompt action when
of indirect maternal death, while thrombosis and women present with chest symptoms or breathlessness
thromboembolism continues to feature as a major remain key to avoiding further deaths. Health-
issue and is the leading cause of direct deaths. Suicide service provision must also focus on pre-pregnancy
is, however, the leading cause of direct maternal counselling, and uptake of contraception and provision
deaths within a year after the end of pregnancy.1 of termination services to limit future mortality among
Two-thirds of maternal mortality is due to a medical women with known heart disease. Other causes of
or mental health condition. Therefore, the need for death both indirect and direct (resulting from obstetric
specialist care for women with pre-existing medical complications of pregnancy) have been stable, with the
exception of pre-eclampsia, which has substantially
reduced since the last report and is now the least
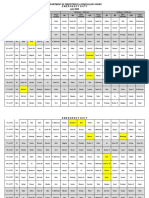
25 Indirect causes of death
Direct causes of death represented category (gure).
Only two women died from pre-eclampsia and
20
eclampsia during pregnancy in the UK during 201214.1
Rate per 100 000 maternities
In the previous two reports, there were 19 and ten
15
maternal deaths from pre-eclampsia in 200608 and
200911, respectively.1 This reduction is remarkable
10 since hypertensive diseases have consistently been a
leading direct cause of death in pregnancy. Maternal
05 deaths from pre-eclampsia have been associated with
substandard care,3 suggesting they are avoidable. In the
0 latest Condential Enquiries into Maternal Deaths and
e
is*
ct
ia
ia
ica
Morbidity, fewer than one woman per million women
th
cie
as
ag
ric
es
ps
re
lis
lis
ps
se
ea
og
at
rh
an
i
sth
lam
bo
bo
nd
Se
di
yd
hi
or
ol
gn
em
em
ae
ri
yc
iac
ec
ur
em
nc
died from hypertensive-related disorders during
ali
he
An
Ps
Ne
e-
bo
rd
id
na
Ha
m
Ot
Pr
flu
Ca
eg
ct
o
ic
re
pr
pregnancy in the UK and there was less than one such
hr
ot
di
dt
rly
ni
In
Ea
an
Am
death per year.1
is
s
bo
m
ro
The low rate of maternal deaths from pre-eclampsia
Th
Figure: Maternal mortality by cause from 2012 to 2014 in the UK in the UK is in stark contrast with the global setting
*Rate for direct sepsis (genital tract sepsis and other pregnancy related infections) is shown in pale and rate for where an estimated 40 000 women die each year from
indirect sepsis (inuenza, pneumonia, others) in dark bar. Rate for suicides is shown in pale and rate for indirect
psychiatric causes (drugs/alcohol) in dark bar. Source: MBRRACE-UK. Reproduced from Saving lives, improving this condition,4 which equates to about ve deaths
mothers caresurveillance of maternal deaths in the UK 201214 and lessons learned to inform maternity care
from the UK and Ireland Condential Enquiries into Maternal Deaths and Morbidity 200914.1 National Perinatal
every hour. The proportion of maternal deaths from
Epidemiology Unit, University of Oxford. hypertensive disorders of pregnancy is 28% in the
582 www.thelancet.com Vol 389 February 11, 2017
Comment
UK (201113),1 74% in the USA (201113),5 and if identied and well managed. However, as delivery
14% globally (2013).4 remains the mainstay of treatment, preterm birth
Deaths from hypertensive diseases of pregnancy are and its ensuing perinatal morbidity will continue
largely due to treatable pathology, the elements of to be a challenge. The contribution of hypertensive
which are important to dene if other countries are to diseases of pregnancy to the 26 million stillbirths that
emulate the reduction in the UK. The largest triennial occur annually across the globe was highlighted in
fall in maternal deaths from these diseases in England the Lancets Ending Preventable Stillbirths Series.11 If
and Wales occurred between the 1950s (200 deaths) services are to impact on perinatal outcomes, therapies
and 1970s (fewer than 40 deaths); this reduction that ameliorate established disease at early gestations
was related to improved surveillance, diagnosis, and safely maintain pregnancy will become increasingly
and timely delivery. From the 1980s onwards, the important. Novel therapies such as statins and other
condential enquiries showed that deaths in women drugs targeting various pathophysiological pathways
with hypertensive diseases of pregnancy were related have been proposed and are under evaluation in clinical
to pulmonary oedema and intracerebral events, trials.12
particularly haemorrhage. The subsequent introduction In the latest Condential Enquiries into Maternal
of uid-restricting management protocols meant Deaths and Morbidity about a quarter of pregnant
pulmonary oedema was no longer a cause of maternal women who died in 201214 were born outside
death in the UK in 2002.6 Intracerebral haemorrhage the UK, but maternal death rates were similar in
remained a fairly common cause of death, and these women and those born in the UK (885 vs
substandard care was often associated with inadequate 787 per 100 000 maternities; relative risk 112;
treatment of severe hypertension, a likely causative 95% CI 080156),1 even when their origins were from
factor.6 a low-income setting, which suggests that universal
Have further improvements in management pregnancy care provision, rather than background
caused this latest reduction in deaths? Pre-eclampsia demographics, inuence the reduction of maternal
can be partly prevented by prophylactic use of mortality rates. Antenatal care and many therapeutic
low-dose aspirin.7 Since 2010, aspirin has been and management interventions for pregnancy
routinely recommended for higher risk women hypertensive disorders can be provided at relative
by the UK National Institute for Health and Care inexpensive cost and are potentially available in low-
Excellence,8 which also underlines the judicious use income settings. The challenge is implementation.
of antihypertensive medication with lower target
thresholds (now to less than 150/100 mm Hg). The *Andrew H Shennan, Marcus Green, Lucy C Chappell
use of anticonvulsant therapies has increasingly Womens Health Academic Centre, Kings College London,
London SE1 7EH, UK (AHS, LCC); and Action on Pre-eclampsia,
been introduced into practice for women with pre-
Evesham, UK (MG)
eclampsia in the past few decades, after trials showed andrew.shennan@kcl.ac.uk
the ecacy of magnesium sulfate for the prevention MG is Chief Executive Ocer of Action on Pre-eclampsia and contributed to the
of eclamptic ts.9 More recently, planned delivery lay summary of the lastest Condential Enquiries into Maternal Deaths and
Morbidity. AHS and LCC declare no competing interests.
from 37 weeks gestation has been shown to reduce
1 Knight M, Nair M, Tunell D, et al, eds, on behalf of MBRRACE-UK. Saving
morbidity,10 and has become a standard of care in the lives, improving mothers caresurveillance of maternal deaths in the UK
UK.8 The introduction of the UK National Health Service 201214 and lessons learned to inform maternity care from the UK and
Ireland Condential Enquiries into Maternal Deaths and Morbidity
evidence-based guidelines that have focused on the 200914. Oxford: National Perinatal Epidemiology Unit, University of
Oxford, 2016
systematic use of interventions may be the catalyst 2 Oce for National Statistics. Death registrations summary tablesEngland
that has reduced deaths from hypertensive diseases of and Wales. 2014. https://www.ons.gov.uk/
peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/
pregnancy. datasets/deathregistrationssummarytablesenglandandwales
referencetables (accessed Jan 5, 2017).
The maternal deaths that remain still seem
3 Shennan AH, Redman C, Cooper C, Milne F. Are most maternal deaths from
to be largely avoidable, and are often related to pre-eclampsia avoidable? Lancet 2012; 379: 168687.
4 WHO. World health statistics 2015. Geneva, Switzerland: World Health
poor detection. However, we must guard against Organization, 2015.
complacency. Pre-eclampsia is only safe for the mother
www.thelancet.com Vol 389 February 11, 2017 583
Comment
5 Division of Reproductive Health National Center for Chronic Disease 9 Altman D, Carroli G, Duley L, et al. Do women with pre-eclampsia, and their
Prevention and Health Promotion. Pregnancy mortality surveillance babies, benet from magnesium sulphate? The Magpie Trial: a randomised
system. 2016. https://www.cdc.gov/reproductivehealth/ placebo-controlled trial. Lancet 2002; 359: 187790.
maternalinfanthealth/pmss.html (accessed Jan 5, 2017). 10 Koopmans CM, Bijlenga D, Groen H, et al. Induction of labour versus
6 Condential Enquiry into Maternal and Child Health. Why mothers die expectant monitoring for gestational hypertension or mild pre-eclampsia
20002002: the sixth report of the Condential Enquiries into Maternal after 36 weeks gestation (HYPITAT): a multicentre, open-label randomised
Death in the United Kingdom. London: Royal College of Obstetricians and controlled trial. Lancet 2009; 374: 97988.
Gynaecologists Press, 2004. 11 Lawn JE, Blencowe H, Waiswa P, et al. Stillbirths: rates, risk factors, and
7 Duley L, Henderson-Smart DJ, Meher S, King JF. Antiplatelet agents for acceleration towards 2030. Lancet 2016; 387: 587603.
preventing pre-eclampsia and its complications. Cochrane Database Syst Rev 12 Cottrell EC, Sibley CP. From pre-clinical studies to clinical trials: generation
2007; 2: CD004659. of novel therapies for pregnancy complications. Int J Mol Sci 2015;
8 National Institute for Health and Care Excellence. Hypertension in 16: 1290724.
pregnancy: the management of hypertensive disorders during
pregnancy. London: National Institute for Health and Care
Excellence, 2010.
Research misconduct and the INTERGROWTH-21st study
On Oct 20, 2016, a statement appeared on the WHO (INTERGROWTH-21st) and the WHO Multicentre
website, announcing that An independent review Study for the Development of Growth Standards from
commissioned by WHO has found that research Fetal Life to Childhood. Both protocols were drawn up
ethics misconduct occurred in a study on foetal in response to a 1995 WHO Expert Committee report6
growth standards.1 The study in question was the that recommended, among other things, Assessment
INTERGROWTH-21st study, led by researchers at and development of fetal growth reference data
the University of Oxford, UK, funded by the Bill & suitable for international applications. Both protocols
Melinda Gates Foundation (BMGF), and reported also built on the methods of the WHO Multicentre
in several journals, including our own.25 Such a Growth Reference Study,7 which produced growth
judgment by the worlds foremost global health agency curves for children from birth to 5 years. Much of
was serious, casting damaging light on a study of the bases of the protocols are therefore in the public
international importance. domain. Kennedy and Villar are accused of having
On Nov 16, 2016, we wrote to Ian Smith, Executive plagiarised the WHO Multicentre Study protocol in
Director of the Oce of the WHO Director-General, developing the INTERGROWTH-21st protocol and of
to request a copy of the review report, but were told obtaining rival funding while still involved with the
that it was condential and had been supplied only to WHO work.
the University of Oxford, BMGF, and the UK General McKendricks responses to us, on Nov 29, 2016, and
Medical Council, which was considering whether to Dec 13, 2016, were robust. It is clear from this response
open an investigation of its own. that the University of Oxford looked into these serious
We then wrote, on Nov 23, 2016, to the researchers, allegations at a high level, methodically dissected
Stephen Kennedy and Jos Villar at the University the claims, closely examined four pairs of protocols
of Oxford, to request their response to the reviews at dierent stages of development, engaged with
ndings. We subsequently received a letter from the the WHO Director-General, and retrieved supporting
Universitys Registrar, Ewan McKendrick, reiterating documentation before concluding that the allegations
the history of the dispute, which (as we were aware) were unfounded. The Oxford researchers clearly stated
dates back to 2008 and has been the subject of the methodological foundations of INTERGROWTH-
previous investigations by the University of Oxford, 21st in their reports.
the Committee on Publication Ethics (COPE), and We were aware, however, that we had only heard
other journals. In brief, the dispute surrounds the Universitys version of events, and again pressed
allegations of plagiarism and disputes over intellectual WHO for their inquiry report. This document was
ownership concerning two research protocols with eventually shared with us in condence on Jan 16, 2017,
joint origins: those of the International Fetal and but we found it disappointingly insubstantial. We
Newborn Growth Consortium for the 21st Century have therefore concluded that its far-reaching judgment
584 www.thelancet.com Vol 389 February 11, 2017
S-ar putea să vă placă și
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- APGODocument49 paginiAPGOiamdonutÎncă nu există evaluări
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Basic Antenatal Care Handbook ISBNDocument59 paginiBasic Antenatal Care Handbook ISBNAuliamusy100% (1)
- MCN PartographDocument2 paginiMCN PartographAlec AnonÎncă nu există evaluări
- Obstetrics & Gynaecology 2019-2008 Regular-Supplementary Group Wise Question Papers WBUHS PDFDocument14 paginiObstetrics & Gynaecology 2019-2008 Regular-Supplementary Group Wise Question Papers WBUHS PDFAditya BarmanÎncă nu există evaluări
- Caesarean SectionDocument48 paginiCaesarean SectionStaen KisÎncă nu există evaluări
- Placenta Previa Case StudyDocument7 paginiPlacenta Previa Case StudyphearlieÎncă nu există evaluări
- Wits Obstetrics 2008Document134 paginiWits Obstetrics 2008Muvenn Kannan100% (1)
- Postpartum QuestionsDocument2 paginiPostpartum QuestionsRayMendez100% (4)
- Placenta: J.L. James, S. Srinivasan, M. Alexander, L.W. ChamleyDocument8 paginiPlacenta: J.L. James, S. Srinivasan, M. Alexander, L.W. ChamleyfujimeisterÎncă nu există evaluări
- Expression of Epithelial Markers by Human Umbilical Cord Stem Cells A Topographical Analysis 2014 PlacentaDocument7 paginiExpression of Epithelial Markers by Human Umbilical Cord Stem Cells A Topographical Analysis 2014 PlacentafujimeisterÎncă nu există evaluări
- In Vitro Transdifferentiation of Umbilical Cord Stem Cells Into Cardiac Myocytes: Role of Growth FactorsDocument8 paginiIn Vitro Transdifferentiation of Umbilical Cord Stem Cells Into Cardiac Myocytes: Role of Growth FactorsfujimeisterÎncă nu există evaluări
- Cord Blood Revelations The Importance of Being A First Born Girl Big On Time and To A Young Mother 2007 Early Human DevelopmentDocument9 paginiCord Blood Revelations The Importance of Being A First Born Girl Big On Time and To A Young Mother 2007 Early Human DevelopmentfujimeisterÎncă nu există evaluări
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument7 paginiEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyfujimeisterÎncă nu există evaluări
- Banking Obstetric Related Tissues and Cells What Every Maternity Unit Must Know 2008 Obstetrics Gynaecology Reproductive MedicineDocument4 paginiBanking Obstetric Related Tissues and Cells What Every Maternity Unit Must Know 2008 Obstetrics Gynaecology Reproductive MedicinefujimeisterÎncă nu există evaluări
- Birth Weight As A Risk Factor For Cancer in Adulthood The Stem Cell Perspective 2011 MaturitasDocument3 paginiBirth Weight As A Risk Factor For Cancer in Adulthood The Stem Cell Perspective 2011 MaturitasfujimeisterÎncă nu există evaluări
- Cell Salvage in Obstetrics 2008 International Journal of Obstetric AnesthesiaDocument9 paginiCell Salvage in Obstetrics 2008 International Journal of Obstetric AnesthesiafujimeisterÎncă nu există evaluări
- Poster Session VDocument1 paginăPoster Session VfujimeisterÎncă nu există evaluări
- Effect of Preeclampsia On Umbilical Cord Blood Hematopoietic Progenitor Stem Cells 2001 American Journal of Obstetrics and GynecologyDocument5 paginiEffect of Preeclampsia On Umbilical Cord Blood Hematopoietic Progenitor Stem Cells 2001 American Journal of Obstetrics and GynecologyfujimeisterÎncă nu există evaluări
- Review Endothelial Progenitor Cells in Pregnancy and Obstetric Pathologies 2013 PlacentaDocument6 paginiReview Endothelial Progenitor Cells in Pregnancy and Obstetric Pathologies 2013 PlacentafujimeisterÎncă nu există evaluări
- Stem Cells in Gynecology 2012 American Journal of Obstetrics and GynecologyDocument8 paginiStem Cells in Gynecology 2012 American Journal of Obstetrics and GynecologyfujimeisterÎncă nu există evaluări
- Social Science & Medicine: Julie KentDocument10 paginiSocial Science & Medicine: Julie KentfujimeisterÎncă nu există evaluări
- Impact of Reduced Intensity Conditioning Allogeneic Stem Cell Transplantation On Women S Fertility 2013 Clinical Lymphoma Myeloma and LeukemiaDocument7 paginiImpact of Reduced Intensity Conditioning Allogeneic Stem Cell Transplantation On Women S Fertility 2013 Clinical Lymphoma Myeloma and LeukemiafujimeisterÎncă nu există evaluări
- Optimizing Umbilical Cord Blood Collection Impact of ObstetricDocument3 paginiOptimizing Umbilical Cord Blood Collection Impact of ObstetricGhada AlÎncă nu există evaluări
- Giving To Receive The Right To Donate in Umbilical Cord Blood Banking For Stem Cell Therapies 2012 Health PolicyDocument8 paginiGiving To Receive The Right To Donate in Umbilical Cord Blood Banking For Stem Cell Therapies 2012 Health PolicyfujimeisterÎncă nu există evaluări
- Vitamin D Deficiency Among Adolescent Females With Polycystic Ovary Syndrome 2015 Journal of Pediatric and Adolescent GynecologyDocument4 paginiVitamin D Deficiency Among Adolescent Females With Polycystic Ovary Syndrome 2015 Journal of Pediatric and Adolescent GynecologyfujimeisterÎncă nu există evaluări
- Factors Predicting The Hematopoietic Stem Cells Content of The Umbilical Cord Blood 2013 Transfusion and Apheresis ScienceDocument6 paginiFactors Predicting The Hematopoietic Stem Cells Content of The Umbilical Cord Blood 2013 Transfusion and Apheresis SciencefujimeisterÎncă nu există evaluări
- Utility of The Oral Glucose Tolerance Test To Assess Glucose Abnormalities in Adolescents With Polycystic Ovary Syndrome 2016 Journal of Pediatric andDocument5 paginiUtility of The Oral Glucose Tolerance Test To Assess Glucose Abnormalities in Adolescents With Polycystic Ovary Syndrome 2016 Journal of Pediatric andfujimeisterÎncă nu există evaluări
- Endometriosis - Pathogenesis, Clinical Features, and Diagnosis - UpToDateDocument39 paginiEndometriosis - Pathogenesis, Clinical Features, and Diagnosis - UpToDatefujimeisterÎncă nu există evaluări
- Obstetric Predictors of Placental Umbilical Cord Blood Volume For Transplantation 2003 American Journal of Obstetrics and GynecologyDocument7 paginiObstetric Predictors of Placental Umbilical Cord Blood Volume For Transplantation 2003 American Journal of Obstetrics and GynecologyfujimeisterÎncă nu există evaluări
- Treatment of PCOS in Adolescence 2006 Best Practice Research Clinical Endocrinology MetabolismDocument20 paginiTreatment of PCOS in Adolescence 2006 Best Practice Research Clinical Endocrinology MetabolismfujimeisterÎncă nu există evaluări
- Polycystic Ovary Syndrome An Under Recognized Cause of Abnormal Uterine Bleeding in Adolescents Admitted To A Children S Hospital 2016 Journal of PediDocument7 paginiPolycystic Ovary Syndrome An Under Recognized Cause of Abnormal Uterine Bleeding in Adolescents Admitted To A Children S Hospital 2016 Journal of PedifujimeisterÎncă nu există evaluări
- Utility of Ultrasound in The Diagnosis of Polycystic Ovary Syndrome in Adolescents 2014 Fertility and SterilityDocument7 paginiUtility of Ultrasound in The Diagnosis of Polycystic Ovary Syndrome in Adolescents 2014 Fertility and SterilityfujimeisterÎncă nu există evaluări
- What Is The Risk of Metabolic Syndrome in Adolescents With Normal BMI Who Have Polycystic Ovary Syndrome 2015 Journal of Pediatric and Adolescent GynDocument4 paginiWhat Is The Risk of Metabolic Syndrome in Adolescents With Normal BMI Who Have Polycystic Ovary Syndrome 2015 Journal of Pediatric and Adolescent GynfujimeisterÎncă nu există evaluări
- Whither PCOS The Challenges of Establishing Hyperandrogenism in Adolescent Girls 2008 Journal of Adolescent HealthDocument3 paginiWhither PCOS The Challenges of Establishing Hyperandrogenism in Adolescent Girls 2008 Journal of Adolescent HealthfujimeisterÎncă nu există evaluări
- Polycystic Ovary Syndrome A Review For Dermatologists Part I Diagnosis and Manifestations 2014 Journal of The American Academy of DermatologyDocument10 paginiPolycystic Ovary Syndrome A Review For Dermatologists Part I Diagnosis and Manifestations 2014 Journal of The American Academy of DermatologyfujimeisterÎncă nu există evaluări
- Using The Androgen Excess PCOS Society Criteria To Diagnose Polycystic Ovary Syndrome and The Risk of Metabolic Syndrome in Adolescents 2013 The JournDocument5 paginiUsing The Androgen Excess PCOS Society Criteria To Diagnose Polycystic Ovary Syndrome and The Risk of Metabolic Syndrome in Adolescents 2013 The JournfujimeisterÎncă nu există evaluări
- The Utility of Ultrasonography in The Diagnosis of Polycystic Ovarian Syndrome PCOS in Adolescents 2014 Journal of Pediatric and Adolescent GynecologyDocument1 paginăThe Utility of Ultrasonography in The Diagnosis of Polycystic Ovarian Syndrome PCOS in Adolescents 2014 Journal of Pediatric and Adolescent GynecologyfujimeisterÎncă nu există evaluări
- Conclusions: Background:: Oral Abstracts / J Pediatr Adolesc Gynecol (2013) E47ee53 E49Document2 paginiConclusions: Background:: Oral Abstracts / J Pediatr Adolesc Gynecol (2013) E47ee53 E49fujimeisterÎncă nu există evaluări
- Postnatal Care at The Health Post and in The CommunityDocument23 paginiPostnatal Care at The Health Post and in The CommunityGreggy Francisco LaraÎncă nu există evaluări
- Management of The Third Stage of LaborDocument12 paginiManagement of The Third Stage of Laborayu_pieterÎncă nu există evaluări
- NOTES RLE - Care of Mother, Child at Risk or With Problems (Acute and Chronic)Document2 paginiNOTES RLE - Care of Mother, Child at Risk or With Problems (Acute and Chronic)SteffiÎncă nu există evaluări
- Scaff 1 in SciDocument1 paginăScaff 1 in SciANGEL JASMINE CABADINGÎncă nu există evaluări
- Midwife Skills TrainingDocument3 paginiMidwife Skills TrainingMarjorie Sta. TeresaÎncă nu există evaluări
- Bahasa Inggris Bu YuliDocument8 paginiBahasa Inggris Bu YuliNova FitriaÎncă nu există evaluări
- Bayrampour HamidehDocument267 paginiBayrampour HamidehRohamonangan TheresiaÎncă nu există evaluări
- Pregnancy With Previous LSCS: Vishal Final YearDocument21 paginiPregnancy With Previous LSCS: Vishal Final YearAdit RockÎncă nu există evaluări
- Pengaruh Pijatan Perineum Dan Senam Kegel Terhadap Pengurangan Ruptur Perineum Pada Ibu BersalinDocument7 paginiPengaruh Pijatan Perineum Dan Senam Kegel Terhadap Pengurangan Ruptur Perineum Pada Ibu BersalinPristika wiyarnaÎncă nu există evaluări
- Water BirthDocument17 paginiWater BirthFania PutriÎncă nu există evaluări
- Department of Obstetrics & Gynecology-Wwrc Emergency Duty July 2020Document3 paginiDepartment of Obstetrics & Gynecology-Wwrc Emergency Duty July 2020noorÎncă nu există evaluări
- 72 Surrogacy CanDocument10 pagini72 Surrogacy CanTamara MoralesÎncă nu există evaluări
- Induction and Augmentation of LaborDocument23 paginiInduction and Augmentation of Laborkevin jonathanÎncă nu există evaluări
- K Rickman ResumeDocument2 paginiK Rickman Resumeapi-286973443Încă nu există evaluări
- CTG Monitoring of Foetal Heart and Uterine ActivityDocument6 paginiCTG Monitoring of Foetal Heart and Uterine ActivityChinedu H. DuruÎncă nu există evaluări
- Uterine Inversion Guide - Causes, Symptoms, TreatmentDocument12 paginiUterine Inversion Guide - Causes, Symptoms, TreatmentElvis NgÎncă nu există evaluări
- Labour Interventions ReportDocument20 paginiLabour Interventions Reportdwi handayaniÎncă nu există evaluări
- 1 - Introduction To MNCHN EINC - 14june2012Document25 pagini1 - Introduction To MNCHN EINC - 14june2012DoyTanÎncă nu există evaluări
- Ahammer Halla Schneeweise JHE 2019Document20 paginiAhammer Halla Schneeweise JHE 2019Grace HallaÎncă nu există evaluări
- Understanding Cephalo-Pelvic Disproportion & Contracted PelvisDocument38 paginiUnderstanding Cephalo-Pelvic Disproportion & Contracted PelvisAltynaiÎncă nu există evaluări
- Soal Bahasa Ingris No 3Document5 paginiSoal Bahasa Ingris No 3Rugas PribawaÎncă nu există evaluări
- Ectopic Pregnancy Diagnosis GuideDocument7 paginiEctopic Pregnancy Diagnosis GuideDr-Saja O. DmourÎncă nu există evaluări