Documente Academic
Documente Profesional
Documente Cultură
6 Diuretics Unlocked
Încărcat de
Soodn Kang SoodnDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
6 Diuretics Unlocked
Încărcat de
Soodn Kang SoodnDrepturi de autor:
Formate disponibile
Diuretics 2011/2012
DIURETICS
Definition:
drugs that increase urine volume.
Classification:
a) Pre-renal (Extra-renal) diuretics:
They increase urine output without acting on the nephrons, examples include:
1. Methylxanthines (theobromine, theophylline, caffeine), dopamine, dobutamine, and
cardiac glycosides (digitalis) increase renal blood flow and glomerular filtration rate
(GFR) by increasing COP and/or causing renal vasodilatation.
(Methylxanthines have also renal action- Cardiac glycosides have diuretic action in
patients with heart failure only).
2. Water and ethyl alcohol inhibit A.D.H.
3. Plasma expanders as dextran.
b) Renal diuretics: they act on the nephrons and may be classified into:
1. Thiazide diuretics: they are moderate efficacy- they inhibit Na+ transport in proximal
segment of distal convoluted tubules (DCT).
2. Loop diuretics: they are high efficacy diuretics- they inhibit Na+ transport in the loop of
Henle.
3. K+-sparing (retaining=conserving) diuretics: they are low efficacy diuretics- they are
either aldosterone antagonists as spironolactone, or non-aldosterone antagonists as
amiloride and triamterene.
4. Carbonic anhydrase inhibitor(CAIs): they inhibit Na+/H+ exchange in proximal
convoluted tubules (PCT) mainly. They are low efficacy and are self-limiting because
they cause acidosis (see later).
5. Acidifying diuretics: as NH4Cl, they are also self-limiting diuretics due to acidosis.
6. Osmotic diuretics: as Mannitol.
N.B.:
Thiazide diuretics, loop diuretics, K+-sparing diuretics, and CAIs are known as "Natriuretics"
or "Saluretics" because they increase urinary excretion of Na+ with its iso-osmotic water.
1 Dr.Ahmed Abdel Rahman www.medadteam.org
Diuretics 2011/2012
Thiazide Diuretics
Source: Synthetic.
Chemistry: Related to sulphonamides.
Pharmacokinetics:
1. Well absorbed orally.
2. Pass placental barrier and may cause teratogenicity.
3. Excreted in PCT to (act from the inner side of the nephron) by active secretion thus
reducing secretion of uric acid leading to hyperuricemia. Probenicid reduces active
transport of thiazides and reduces their diuretic action.
Pharmacodynamics:
1. Diuretic action: characterized by:
a) Onset: delayed onset (thiazides are given only orally so they are not useful in
emergencies).
b) Duration: some thiazides are short acting as hydrochlorothiazide and others are long
acting as metolazone.
c) Efficacy: moderate efficacy.
d) Site of action: act on the proximal segment of DCT inhibiting Na+, Cl- and water
reabsorption which will be excreted in urine. The sulphonamide structure inhibits
carbonic anhydrase enzyme which causes very mild additional diuretic action.
e) Part of Na+ reaching DCT is reabsorbed in exchange for K+ (mainly) and H+ (to a less
extent).
f) Urine will also contain excess Mg2+ and lesser amounts of Ca2+.
g) In conclusion, thiazides will produce the following changes in urine and in blood:
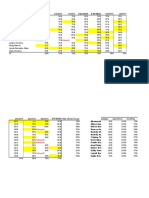
URINE BLOOD
1. Excess Na+ (natriuresis). 1. Hyponatremia.
2. Excess water (diuresis). 2. Hypovolemia (moderate).
3. Excess Cl- (chloruresis). 3. Hypochloremia.
4. Excess K+ (kaluresis). 4. HYPOKALEMIA.
5. Excess H+ (acidic urine). 5. Alkalosis.
6. Excess Mg2+. 6. Hypomagnesemia.
7. Less Ca2+. 7. Hypercalcemia.
8. Less uric acid. 8. Hyperuricemia.
2 Dr.Ahmed Abdel Rahman www.medadteam.org
Diuretics 2011/2012
2. Thiazides reduce Renal Blood Flow (RBF):
a) They are contraindicated in patients with renal impairment.
b) Reduction RBF leads to reduction of Glomerular Filtration Rate (GFR) and accordingly
thiazide act as Anti-diuretics only in patients with nephrogenic Diabetes Insipidus
(which may be induced by some drugs as Lithium, Methoxyflurane, and
Demeclocycline).
3. Antihypertensive action:
a) Arteriolar V.D.: this is the most important mechanism and can be explained by:
Depletion of Na+ from the wall of arterioles thus reducing the vasoconstrictor
(pressor) response to noradrenaline and angiotensin.
Increasing synthesis of vasodilator PGs (that is why NSAIDs may partially
antagonize the antihypertensive action of thiazides).
Opening of K+ channels leading to hyperpolarization and V.D.
Block of Ca2+ channels in arterioles causing V.D.
b) Diuretic action: this is of little importance in the antihypertensive action of thiazides.
4. Hyperuricemia: Thiazides reduce active tubular secretion of uric acid in PCT.
5. Hyperlipidemia: Thiazides increase LDL-cholesterol and triglycerides.
6. Hyperglycemia: Thiazides open K+ channels in B-cells of islets of Langerhans
Hyperpolarization
Therapeutic uses:
1. Treatment of edema which is either: Cardiac (in mild and moderate congestive heart
failure), Renal, or Hepatic edema.
2. Treatment of mild and moderate hyperternsion: thiazides are preferred to loop diuretics
because they are arteriodilators Except in cases of emergency hypertension and in
patients with renal impairment where loop diuretics are preferred (loop diuretics can be
given I.V. and they increase renal blood flow).
3. Treatment of nephrogenic diabetes insipidus.
4. Treatment of idiopathic hypercalciurea and recurrent calcium stones.
5. Treatment of pre-menstrual tension syndrome.
3 Dr.Ahmed Abdel Rahman www.medadteam.org
Diuretics 2011/2012
Adverse Effects Contraindications (precautions)
1. Hypokalemia (causes fatigue, headache, 1. With Digitalis (hypokalemia
and cardiac arrhythmias). induces digitalis toxicity).
2. Hyponatremia (causes muscle cramps).
3. Hypovolemia.
4. Hypomagnesemia (may also precipitate
digitalis toxicity).
5. Hypochloremic alkalosis.
6. Hypotension. 2. Hypotension.
7. Hypersensitivity (purpura, dermatitis, 3. Allergy to thiazides and
photosensitivity, necrotizing vasculitis or sulphonamides.
bone marrow depression) and cross allergy
with sulphonamides.
8. Hyperlipidemia.
9. Hyperglycemia. 4. Diabetes mellitus.
10.Hyperuricemia and may precipitate acute 5. Gout.
gouty attacks.
11.Decrease renal blood flow. 6. Renal insufficiency
12.Teratogenicity. 7. Pregnancy.
13.May lead to hepatic coma in hepatic 8. Hepatic insufficiency.
insufficiency.
14.Gut upsets. 9. With steroids (as cortisol): see
later.
4 Dr.Ahmed Abdel Rahman www.medadteam.org
Diuretics 2011/2012
How to Avoid Hypokalemia?:
1. Addition of a K+-sparing diuretic (amiloride-triamterene-spironolactone) or ACE
inhibitors.
2. Dietary potassium (in fruits and vegetables).
3. K+ supplements: K+ tablets (cause GIT irritation) or syrup (less irritant).
4. Intermittent use of diuretics.
Drug interactions:
1. With digitalis: Hypokalemia is the most important precipitating factor of digitalis toxicity.
2. With steroids: steroids cause Na+ and water retention thus antagonize the diuretic effect
of thiazides but more seriously they cause hypokalemia.
3. With sulphonamides: cross allergy.
4.
With K+-sparing diuretics: synergism and correction of serum K+.
5. With ACE inhibitors and AT1 antagonists: synergism and correction of serum K+.
6. With insulin and oral hypoglycemic drugs: thiazides antagonize the action of these drugs.
7. With uricosuric drugs (drugs that increase uric acid excretion in urine): thiazides
antagonize the action of these drugs.
8. With Probenicid: probenicid decreases active transport of thiazides and antagonizes their
diuretic action.
9. With NSAIDs: NSAIDs antagonize the antihypertensive action of thiazides because they
cause Na+ and water retention and inhibit the synthesis of vasodilator PGs.
Preparations:
1. Short acting thiazides:
Chlorthiazide and Hydrochlorothiazide (given/6-12 hours).
2. Long acting thiazides:
Chlorthalidone, Metolazone, and Polythiazide (given once daily).
3. Thiazide analogues: they are similar to thiazides in action but not in chemical structure.
Examples include:
a) Indapamide: weak diuretic but it causes arteriodilatation as thiazides (most probably
due to calcium channel block. Used in treatment of hypertension in sub-diuretic dose,
and is excreted in bile (long acting given once daily).
b) Diazoxide: it is a vasodilator drug (opens K+ channels) related to thiazides but is Not a
diuretic. It is given I.V. in emergency hypertension.
c) Metolazone.
5 Dr.Ahmed Abdel Rahman www.medadteam.org
Diuretics 2011/2012
Loop Diuretics (High efficacy = High Ceiling Diuretics)
1. Source: synthetic.
2. Chemistry:
some are related to sulphonamides as frusemide (they inhibit carbonic anhydrase which
contributes very mildly to their diuretic action but may cause allergic reactions and cross
allergy with sulphonamides) but others are not sulphonamide derivatives as ethacrynic
acid.
3. Pharmacokinetics:
Well absorbed orally, and can be given by I.V. and I.M. injection (useful in
emergencies).
Highly bound to plasma proteins and can displace other drugs as warfarin leading to
toxicity (bleeding in case of warfarin).
Pass placental barrier and may cause teratogenicity (fetotoxicity).
Loop diuretics are actively secreted in PCT and-as thiazides- act from the inner side of
the nephron. They interfere with active tubular secretion of uric acid leading to
hyperuricemia, and probenicid reduces their diuretic effect.
Partly metabolized by the liver.
4. Pharmacodynamics:
1. Diuretic action: characterized by:
a) Onset: rapid onset.
b) Duration: short duration.
c) Efficacy: high efficacy (the most potent available diuretics).
d) Site of action: loop diuretics inhibit reabsorption of Na+, K+, and 2Cl- (co-transport)
from the thick segment of the ascending limb of loop of Henle leading to excess
excretion of these electrolytes in urine with iso-osmotic water. In addition; loop
diuretics decrease osmolarity of the medulla of the kidney and consequently
decrease water reabsorption from the collecting tubules causing potent diuresis.
e) Part of excess Na+ reaching DCT is reabsorbed in exchange for K+ (mainly) and H+
(to a less extent).
f) Urine will also contain excess Mg2+ and excess Ca2+.
In conclusion loop diuretics will produce the following changes in urine and in blood
6 Dr.Ahmed Abdel Rahman www.medadteam.org
Diuretics 2011/2012
Urine Blood
1. Excess Na+ (natriuresis). 1. Hyponatremia.
2. Excess water (diuresis). 2. Hypovolemia (marked).
3. Excess Cl- (chloruresis). 3. Hypochloremia.
4. Excess K+ (kaluresis). 4. HYPOKALEMIA.
5. Excess H+ (acidic urine). 5. Alkalosis.
6. Excess Mg2+. 6. Hypomagnesemia.
7. Excess Ca2+ (calciurea). 7. Hypocalcemia.
8. Less uric acid. 8. Hyperuricemia.
2. Loop diuretics increase renal blood flow: they are the diuretics of choice in renal
insufficiency. This is because loop diuretics increase synthesis of vasodilator PGs (PGE
and PGI) in the kidney, this action is antagonized by NSAIDs. (Remember that
thiazides reduce RBF and GFR).
3. Antihypertensive action: this is due to their diuretic action and NOT due to
arteriodilatation.
(In contrast to thiazides; loop diuretics cause venodilatation but not arteriodilatation).
4. Hyperlipidemia: as thiazides; loop diuretics increase LDL-cholesterol and triglycerides.
5. Hyperglycemia: loop diuretics decrease insulin release from the pancreas less
markedly than thiazides.
5. Therapeutic uses:
a) Edema: loop diuretics are used in severe, acute, and refractory edema (combined
with K+-sparing diuretics) which may be cardiac (due to congestive heart failure),
renal, or hepatic edema.
b) Loop diuretics are given I.V. in acute left ventricular failure (LVF) as they cause
diuresis and venodilatation which decreases pre-load). Also used in cerebral edema.
c) Hypertension: loop diuretics are preferred to thiazides in the following conditions:
Hypertension in patients with renal insufficiency.
Emergency hypertension.
Resistant hypertension.
Severe hypertension, especially with other antihypertensive drugs that may cause
Na+ and water retention as arteriodilators.
d) Acute renal failure.
e) Hypercalcemia.
7 Dr.Ahmed Abdel Rahman www.medadteam.org
Diuretics 2011/2012
Adverse effects Contraindications
1. Hypokalemia. 1. With Digitalis: hypokalemia
precipitates digitalis toxicity.
2. Hypovolemia and dehydration.
3. Hyponatremia.
4. Hypomagnesemia.
5. Hypotension. 2. Hypotension.
6. Hypochloremic alkalosis.
7. Hypocalcemia.
8. Hypersensitivity (and cross 3. Allergy to loop diuretics and
allergy with sulphonamides with sulphonamides.
some loop diuretics).
9. Hyperglycemia. 4. Diabetes mellitus.
10.Hyperuricemia. 5. Gout.
11.Hyperlipidemia.
12.Teratogenicity. 6. Pregnancy.
13.Ototoxicity: damage of the 8th 7. With other ototoxic drugs as
cranial nerve which may cause aminoglycosides.
deafness, especially if given
concomitantly with other
ototoxic drugs as
aminoglycosides (streptomycin)
or in renal impairment.
8. Liver insufficiency: may precipitate
hepatic coma.
14.Gut upset. 9. With steroids as Cortisol.
8 Dr.Ahmed Abdel Rahman www.medadteam.org
Diuretics 2011/2012
6. Drug interactions:
1. With Digitalis: Hypokalemia and hypomagnesemia induce digitalis toxicity.
(How to avoid hypokalemia?).
2. With steroids: see thiazide diuretics.
3. With sulphonamides: see thiazide diuretics.
4. With K+-sparing diuretics and ACE inhibitors (or AT1-antagonists): see thiazide
diuretics.
5. With NSAIDs: NSAIDs antagonize partially the diuretic action of loop diuretics because
they reduce vasodilator PGs which increase RBF, and they cause Na+ and water
retention.
6. With insulin and oral hypoglycemic drugs: see thiazide diuretics.
7. With probenicid: see thiazide diuretics.
8. With uricosuric drugs: see thiazide diuretics.
9. With Ototoxic drugs as Aminoglycosides: severe ototoxicity.
10.Reduce renal clearance of lithium (anti-manic and mood stabilizing agent) leading to
acute lithium toxicity (see CNS pharmacology).
Preparations:
1. Sulphonamide derivatives: Frusemide (Lasix)- Bumetanide- Torsemide.
2. Non-sulphonamide derivatives: Ethacrynic acid.
Very Important Note:
K+-Losing (depleting) diuretics are commonly used in treatment of heart failure with digitalis
but never allow hypokalemia in these patients because it is the most important factor
precipitating digitalis toxicity.
9 Dr.Ahmed Abdel Rahman www.medadteam.org
Diuretics 2011/2012
Thiazide Diuretics Loop Diuretics
1-Chemistry: Sulphonamide derivatives. Sulphonamide derivatives
and non-sulphonamides.
2-Route: Oral only. Oral and parenteral.
3-Onset and Slow onset, may be short acting, Rapid onset and short
duration: or long acting. duration.
4-Efficacy: Moderate efficacy. High efficacy.
5-Site of action: Proximal segment of DCT. Thick segment of ascending
limb of loop of Henle.
6-Diuretic action: Must be actively secreted into Must be actively secreted
PCT, inhibit Na+ , Cl-, and water into PCT, inhibit Na+, K+,
reabsorption from proximal and 2Cl- reabsorption from
segment of DCT leading to: Loop of Henle leading
Natriuresis- diuresis-chloruresis- to:Natriuresis-diuresis-
kaluresis-acidic urine-excess chloruresis-kaluresis-acidic
Mg2+- urine-excess Mg2+-excess
less Ca2+-less uric acid. Ca2+ -less uric acid.
7-RBF and GFR: Decrease RBF and GFR: Increase RBF
Contraindicated in renal (by increasing PG synthesis)
impairment. and GFR. They are the
Useful in nephrogenic diuretics of choice in renal
diabetes insipidus. impairment.
8-Antihypertensive Mainly by arteriodilatation. Only by diuresis and no
action: Less importantly by diuresis. arteriodilatation.
9-Therapeutic uses: 1. Mild and moderate edema 1. Severe, refractory, and
(Cardiac edema due to heart acute edema (acute
failure-Renal-Hepatic). LVF).
2. Mild and moderate 2. Emergency, severe, and
hypertension. resistant hyperternsion.
3. Nephrogenic diabetes 3. Acute renal failure.
insipidus. 4. Hypercalcemia.
4. Idiopathic hypercalciurea.
5. Pre-menstrual tension.
10 Dr.Ahmed Abdel Rahman www.medadteam.org
Diuretics 2011/2012
10-Adverse effects: Hypokalemia-Hypovolemia- Hypokalemia-Hypovolemia
Hyponatremia-Hypotension- and Dehydration-
Hypomagnesemia- Hyponatremia-
Hypersensitivity-Hyperglycemia- Hypotension-
Hyperlipidemia-Hyperuricemia- Hypomagnesemia-
Teratogenic-Decrease RBF- Hypersensitivity-
Hypercalcemia- Hyperlipidemia-
Hepatic coma in liver Hyperglycemia-
insufficiency. Hyperuricemia-
Teratogenic-Hypocalcemia-
Hepatic coma in liver
insufficiency-Ototoxicity.
11Contraindications Digitalis toxicity-Hypotension- Digitalis toxicity-
(Precautions): Allergy-Diabetes mellitus-Gout- Hypotension-Allergy-
Pregnancy-Renal impairment- Diabetes mellitus-Gout-
Liver insufficiency-With steroids. Pregnancy-Liver
insufficiency-With steroids-
With other ototoxic drugs.
12-Preparations: Short acting: Sulphonamides:
Chlorothiazide- Frusemide-Bumetanide-
Hydrochlorothiazide- Torsemide.
Long acting: Non-sulphonamides:
Chlorthalidone-Metolazone. Ethacrynic acid.
N.B: thiazides and loop diuretics are "K+ depleting diuretics".
Drugs causing Hypokalemia:
1. Thiazide diuretics (chlorothiazide-hydrochlorothiazide).
2. Loop diuretics (frusemide-bumetanide-ethacrynic acid).
3. Steroids: cortisol (glucocorticoid)-aldosterone (mineralocorticoid).
4. Adrenaline (by stimulation of renin release and 2-stimulation in skeletal muscles
increasing potassium uptake).
11 Dr.Ahmed Abdel Rahman www.medadteam.org
Diuretics 2011/2012
Drugs causing Hyperkalemia:
1. K+-sparing diuretics: spironolactone (aldosterone antagonist)-amiloride and triamtertene
(non-aldosterone antagonists).
2. ACE inhibitors (captopril) and AT1-receptor antagonists (losartan).
3. -blockers as propranolol (by inhibition of renin release and blocking 2-receptors).
4. Succinylcholine (depolarizing NMB) especially in renal impairment, burns, and severe
tissue damage.
5. Heparin (inhibits aldosterone synthesis).
Potassium Sparing Diuretics
Common Characteristics:
1. Route of administration: they are given orally only.
2. Onset of action: delayed, not useful in emergencies.
3. Efficacy: they have low efficacy (weak diuretic action).
4. Site of action: distal segment of DCT and cortical collecting tubules.
5. Diuretic action: inhibit Na+/K+ exchange mainly and inhibit Na+/H+ exchange to a lesser
extent. This causes excretion of Na+, Cl-, and water in urine and retention of K+
(hyperkalemia) and H+ (metabolic acidosis).
6. They are contraindicated in renal impairment to avoid severe hyperkalemia.
7. Unlike thiazides and loop diuretics: they do not cause hyperglycemia, hyperlipidemia, or
hyperuricemia (they have mild uricosuric action) and are not related to sulphonamides
(no cross allergy and no carbonic anhydrase inhibition).
8. Classification: they are classified according to their mechanism of action into 2 groups:
a) Aldosterone antagonists: e.g. Spironolactone- Canrenone (active metabolite of
spironolactone) Eplerenone.
They are competitive antagonists with aldosterone for specific intraceullar
(cytoplasmic) mineralocorticoid receptors in cells of DCT and collecting tubules.
b) Non-Aldosterone antagonists: e.g. Amiloride and Triamterene: they inhibit Na+ influx
by blocking Na+-channels in the luminal membrane of DCT and collecting tubular cells.
12 Dr.Ahmed Abdel Rahman www.medadteam.org
Diuretics 2011/2012
1) Aldosterone Antagonists:
a) Spironolactone (Aldactone):
1. Source: Synthetic.
2. Chemistry: Steroid.
3. Pharmacokinetics:
Absorbed orally.
Converted in the liver into canrenone (active metabolite).
Delayed onset and long duration.
Passes B.B.B.
4. Pharmacodynamics:
Mechanism of action:
Competitive antagonists with aldosterone for mineralocorticoid receptors in DCT and
cortical collecting tubules leading to inhibition of Na+/K+ exchange (mainly) and
inhibition of Na+/H+ exchange.
5. Pharmacological actions:
a) Low efficacy diuretic action by increasing Na+,Cl-, and water excretion in urine.
b) Retention of K+ in blood leading to "Hyperkalemia".
c) Retention of H+ in blood leading to "Metabolic acidosis" and decrease H+ excretion
in urine causing slight alkalinization of urine.
d) No hyperuricemia, hyperglycemia, or hyperlipidemia (unlike thiazides and loop
diuretics).
6. Therapeutic uses:
a) Being weak diuretics they are usually combined with thiazide diuretics or loop
diuretics in treatment of edema and hypertension; to achieve synergism and
maintain normal blood potassium.
b) Treatment of refractory edema and resistant hypertension due to
Hyperaldosteronism which is either primary (Conn's syndrome) or more commonly
secondary to liver cirrhosis, nephrotic syndrome, and congestive heart failure.
They are given alone or combined with thiazide or loop diuretics.
c) Alternative to thiazides and loop diuretics whenever they are contraindicated in
allergy to sulphonamides, D.M., and gout.
13 Dr.Ahmed Abdel Rahman www.medadteam.org
Diuretics 2011/2012
7. Adverse effects:
a) Hyperkalemia especially in: renal impairment-drugs that inhibit renin release as -
blockers, NSAIDs (inhibit PGI2 which stimulates renin release)-ACE inhibitors and
AT antagonists.
b) Metabolic acidosis.
c) Hypersensitivity reactions as skin rash.
d) Gut upset: gastritis, diarrhea, gastric bleeding.
e) CNS disturbances: headache, drowsiness, confusion, and lethargy.
f) Feminization (Gynecomastia) and impotence in males, and irregular menstruation
and masculanization in females (deepening of voice and hirsutism) due to steroid
structure.
8. Drug interactions:
a) With thiazide and loop diuretics: synergism in diuretic action and maintain normal
blood K+.
b) With ACE inhibitors, AT antagonists, -blockers, and NSAIDS: severe hyperkalemia.
c) With Carbenoxolone( aldosterone-like drug derived from liquorice and acts as a
mucosal protective agent in treatment of peptic ulcer): spironolactone antagonizes
the action of liquorice on the stomach.
b) Eplerenone:
Similar to spironolactone but is non-steroid and accordingly no gynecomastia or
menstrual disturbances occur.
2) Non-Aldosterone Antagonists:
1. Source: Synthetic.
2. Pharmacokinetics:
Absorbed orally.
Amiloride is excreted unchanged in urine. Triamterene is mainly metabolized in
the liver (shorter duration of action).
3. Pharmacodynamics:
Mechanism of action: inhibit Na+ influx by blocking Na+ channels in DCT and cortical
collecting tubules (they do not compete with aldosterone) thus reducing Na+/K+
exchange and to a lesser extent Na+/H+ exchange.
14 Dr.Ahmed Abdel Rahman www.medadteam.org
Diuretics 2011/2012
4. Actions:
As Spironolactone:
Weak diuretic action- Hyperkalemia- Metabolic acidosis.
5. Therapeutic uses:
a) Amiloride and Triamterene are added to thiazides or loop diuretics in treatment of
edema (cardiac edema due to heart failure-renal edema - hepatic edema) to achieve
synergism and more importantly to correct hypokalemia induced by thiazides and
loop diuretics.
b) Amiloride can be used in lithium-induced nephrogenic diabetes insipidus.
6. Adverse effects:
a) Hyperkalemia especially in renal impairments and other drugs (see
Spironolactone).
b) Metabolic acidosis.
c) Hypersensitivity reactions: photosensitivity.
d) Gut upset.
e) Triamterene causes renal stones and may precipitate acute renal failure if given
with indomethacin (NSAID).
Carbonic Anhydrase Inhibitors
Therapeutic doses:
1. Glaucoma: in open angle glaucoma local CA inhibitors as dorzolamide and brinzolamide
are used, in narrow angle glaucoma acetazolamide is also given systemically.
2. Treatment of metabolic alkalosis.
3. Absence seizures (petit-mal epilepsy).
4. To alkalinize the urine, as in treatment of acute toxicity of acidic drugs as salicylates and
barbiturates.
5. Rarely used as diuretics (low efficacy and self-limiting).
Osmotic Diuretics:
They are pharmacologically inert substances.
They are freely filtered by the glomeruli but are not or incompletely-reabsorbed, so
they are excreted in urine with iso-osmotic water and diuresis occurs. They increase
urinary Na+, Cl-, K+, Mg2+, HCO3- and Ca2+.
15 Dr.Ahmed Abdel Rahman www.medadteam.org
Diuretics 2011/2012
Examples:
a) Mannitol:
Polysaccharide given by I.V.infusion.
Uses:
1. Acute elevation of intra-cranial pressure (ICP).
2. Acute elevation of IOP (acute narrow angle glaucoma=acute congestive glaucoma).
3. Prevent Acute renal failure.
Adverse effects:
Nausea and vomiting-Allergy-Transient expansion of extracellular fluid volume and
may aggravate acute heart failure.
Contraindications:
Acute L.V.F. (acute pulmonary edema=cardiac asthma).
b) Glucose I.V.
c) Glycerin and isosorbide: given orally in acute narrow angle glaucoma.
Methylxanthines:
Examples:
Caffeine,Theobromine, Theophylline, and Aminophylline.
Diuretic action:
1. Pre-renal action by increasing COP and V.D. of renal blood vessels.
2. Renal action: inhibit Na+ reabsorption from PCT.
Uses:
Aminophylline is given very slowly I.V. in acute L.V.F.
Cardiac glycosides:
Cardiac glycosides (digitalis) have diuretic action only in patients with congestive heart
failure by pre-renal action as they increase COP in these patients (see CVS pharmacology).
Dopamine:
Diuretic action occurs with moderate rate of infusion (stimulates D1-receptors causing renal
V.D. and increase renal blood flow) and with moderate rate of infusion (stimulate 1-
receptors causing increased COP).
16 Dr.Ahmed Abdel Rahman www.medadteam.org
Diuretics 2011/2012
Anti-Diuretics
1. ADH and drugs that increase release of ADH as morphine, nicotine, barbiturates, and
yohimbine.
2. Thiazide diuretics are anti-diuretics only in nephrogenic diabetes insipidus.
3. Amiloride is anti-diuretic in lithium-induced diabetes insipidus.
4. Chlorpropamide (anti-diabetic) is ADH like and is used in pituitary diabetes insipidus.
5. Vasoconstrictors as adrenaline and serotonin decrease renal blood flow and act as anti-
diuretics.
ADH Antagonists
1. Lithium carbonate: Antimanic and mood stabilizer. It induces nephrogenic diabetes
insipidus which is treated by amiloride.
2. Methoxyflurane: Inhalation halogenated general anaesthetic which may induce
nephrogenic diabetes insipidus.
3. Demeclocycline: Tetracycline antibiotic that may cause nephrogenic diabetes insipidus,
and is used to treat excess ADH secretion (Syndrome of Inappropriate ADH=SIADH).
Remember That:
Diuretics causing Hypokalemia: Thiazides Loop diuretics CA inhibitors.
Diuretics causing Hyperkalemia: Aldosterone antagonists (Spironolactone) and Non-
aldosterone antagonists (Amiloride and Triamterene).
Diuretics causing Hypochloremic alkalosis: Thiazides and Loop diuretics.
Diuretics causing Hyperchloremic Acidosis: CA inhibitors (Acetazolamide) and Acidifying
diuretics (NH4Cl).
Self-Limiting diuretics: CA inhibitors and NH4Cl (due to acidosis).
17 Dr.Ahmed Abdel Rahman www.medadteam.org
S-ar putea să vă placă și
- Business English Course BookDocument250 paginiBusiness English Course BookSoodn Kang Soodn100% (5)
- GlaucomaDocument24 paginiGlaucomaSoodn Kang SoodnÎncă nu există evaluări
- Uveal TractDocument11 paginiUveal TractSoodn Kang SoodnÎncă nu există evaluări
- ScleraDocument2 paginiScleraSoodn Kang SoodnÎncă nu există evaluări
- Lacrimal SystemDocument13 paginiLacrimal SystemSoodn Kang SoodnÎncă nu există evaluări
- OrbitDocument9 paginiOrbitSoodn Kang SoodnÎncă nu există evaluări
- RetinaDocument19 paginiRetinaSoodn Kang SoodnÎncă nu există evaluări
- Eyelid 2011Document25 paginiEyelid 2011Soodn Kang SoodnÎncă nu există evaluări
- Pharm DR Ahmed Abd AlrahmanDocument24 paginiPharm DR Ahmed Abd AlrahmanAmrAliTahaÎncă nu există evaluări
- 10 CNS UnlockedDocument51 pagini10 CNS UnlockedSoodn Kang SoodnÎncă nu există evaluări
- Surgery McqsDocument10 paginiSurgery McqsSoodn Kang SoodnÎncă nu există evaluări
- ConjunctivaDocument23 paginiConjunctivaSoodn Kang SoodnÎncă nu există evaluări
- Antidote List 2009: Beaumont Hospital, P.O. BOX 1297, Beaumont Road, Dublin 9Document27 paginiAntidote List 2009: Beaumont Hospital, P.O. BOX 1297, Beaumont Road, Dublin 9Soodn Kang SoodnÎncă nu există evaluări
- AntiarritmiasSzerek 2016-2-8Document30 paginiAntiarritmiasSzerek 2016-2-8Soodn Kang SoodnÎncă nu există evaluări
- Local Anaesthetics Mcqs From LouisDocument2 paginiLocal Anaesthetics Mcqs From LouisSoodn Kang SoodnÎncă nu există evaluări
- Nem-Szteroid Gyulladásgátlók (Nsaids) : 1. Gyulladásgátlás 2. Fájdalomcsillapítás 3. LázcsillapításDocument34 paginiNem-Szteroid Gyulladásgátlók (Nsaids) : 1. Gyulladásgátlás 2. Fájdalomcsillapítás 3. LázcsillapításSoodn Kang SoodnÎncă nu există evaluări
- Pharm Cvs McqsDocument30 paginiPharm Cvs McqsSoodn Kang Soodn100% (3)
- LokalKeringesfokozok B12 Folsav STB ANGOL 2016-2-12Document14 paginiLokalKeringesfokozok B12 Folsav STB ANGOL 2016-2-12Soodn Kang SoodnÎncă nu există evaluări
- Epidemiology of CholeraDocument26 paginiEpidemiology of CholeraSoodn Kang SoodnÎncă nu există evaluări
- Diagnosis 3Document10 paginiDiagnosis 3Soodn Kang SoodnÎncă nu există evaluări
- Hallgatok VeglegesDocument3 paginiHallgatok VeglegesSoodn Kang SoodnÎncă nu există evaluări
- CardiologyDocument10 paginiCardiologySoodn Kang SoodnÎncă nu există evaluări
- DermatologyDocument21 paginiDermatologySoodn Kang SoodnÎncă nu există evaluări
- 2011 - Patient PresentationDocument12 pagini2011 - Patient PresentationSoodn Kang SoodnÎncă nu există evaluări
- Angol Oktatás - VTVSSVTDocument5 paginiAngol Oktatás - VTVSSVTSoodn Kang SoodnÎncă nu există evaluări
- Case Studies in The Management of Acs With GP Iib/Iiia InhibitorsDocument47 paginiCase Studies in The Management of Acs With GP Iib/Iiia InhibitorsSoodn Kang SoodnÎncă nu există evaluări
- Autonomic Drugs Flash CardsDocument16 paginiAutonomic Drugs Flash CardsSoodn Kang SoodnÎncă nu există evaluări
- ورق مذاكره Ent في 100 صفحه بسDocument100 paginiورق مذاكره Ent في 100 صفحه بسSoodn Kang SoodnÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- D. NegligenceDocument11 paginiD. NegligenceKing GeorgeÎncă nu există evaluări
- TOPICS in Health Care ConceptDocument41 paginiTOPICS in Health Care ConcepthageguroÎncă nu există evaluări
- Coronary Artery DiseaseDocument22 paginiCoronary Artery DiseaseApil BhutaniÎncă nu există evaluări
- Hypokalemic Periodic ParalysisDocument21 paginiHypokalemic Periodic ParalysisVarun VarnÎncă nu există evaluări
- Cardiovascular CirculatoryStudentDocument89 paginiCardiovascular CirculatoryStudentTess MohamedÎncă nu există evaluări
- Exercise Prescription For Health & Fittness For Patients With ObesityDocument1 paginăExercise Prescription For Health & Fittness For Patients With ObesityWasemBhatÎncă nu există evaluări
- Medical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 47Document13 paginiMedical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 47sarasjunkÎncă nu există evaluări
- Management of Primary Dysmenorrhoea by Dry Cupping: A ReviewDocument5 paginiManagement of Primary Dysmenorrhoea by Dry Cupping: A ReviewWilyanto YangÎncă nu există evaluări
- Influenza 1918.0910Document19 paginiInfluenza 1918.0910RafaelÎncă nu există evaluări
- The Right To Health, by Thomas SzaszDocument11 paginiThe Right To Health, by Thomas SzaszNicolas Martin0% (1)
- Vetlexicon News Update - Feb 2020Document2 paginiVetlexicon News Update - Feb 2020TheBoss 20Încă nu există evaluări
- Detailed Lesson Plan BPPDocument8 paginiDetailed Lesson Plan BPPDa Real SoroteÎncă nu există evaluări
- The Mind Into The BodyDocument375 paginiThe Mind Into The BodyΣτάθης Λάζαρης100% (1)
- Case Report DinofilariaDocument4 paginiCase Report DinofilariaKamendra SinghÎncă nu există evaluări
- Example of Nursing Care Plan (Pathophysiology)Document5 paginiExample of Nursing Care Plan (Pathophysiology)Elizabeth ZamoraÎncă nu există evaluări
- Rating The Risk Factors For Breast Cancer: ReviewDocument9 paginiRating The Risk Factors For Breast Cancer: ReviewPratamasari InsaniÎncă nu există evaluări
- Subclinical Thyroid Dysfunction: Diagnosis and Management: Budiman Darmowidjojo, Lucia Dwi AntikaDocument11 paginiSubclinical Thyroid Dysfunction: Diagnosis and Management: Budiman Darmowidjojo, Lucia Dwi AntikaMuhammad Reyhan HidayatÎncă nu există evaluări
- Temperature: Oral, Rectal, Tympanic and Axillary: Using Digital ThermometersDocument4 paginiTemperature: Oral, Rectal, Tympanic and Axillary: Using Digital ThermometersStephanie LopezÎncă nu există evaluări
- TERMINOLOGI 2 ST - PencernaanDocument61 paginiTERMINOLOGI 2 ST - PencernaanSarah Suzanna Sitepu0% (1)
- Chest Trauma DikaDocument46 paginiChest Trauma DikaOnyedika EgbujoÎncă nu există evaluări
- The Only Way To Achieve Harmony Is Through Practicing MindfulnessDocument8 paginiThe Only Way To Achieve Harmony Is Through Practicing MindfulnessAnn ZhyhalkinaÎncă nu există evaluări
- Advanced Writing SkillsDocument74 paginiAdvanced Writing SkillsThaiHoa9100% (1)
- Proceeding 4th Aceh Surgery UpdateDocument83 paginiProceeding 4th Aceh Surgery UpdateUNS KAMERA BELAKANGÎncă nu există evaluări
- FAD DIETS PowerPointDocument48 paginiFAD DIETS PowerPointTechnoShindoÎncă nu există evaluări
- NANDA LIST of N.DiagnosesDocument3 paginiNANDA LIST of N.DiagnosesHasan KasiÎncă nu există evaluări
- Subiecte Oral Engleza BilingvDocument3 paginiSubiecte Oral Engleza BilingvRadu Bortes100% (1)
- MCQ Ped EndocvsDocument2 paginiMCQ Ped EndocvsManveerÎncă nu există evaluări
- Anesthesia MCQ 425Document4 paginiAnesthesia MCQ 425dungulu50% (2)
- Practice Essentials: Essential Updates: Distinguishing Between Left-And Right-Sided Atrial TachycardiaDocument28 paginiPractice Essentials: Essential Updates: Distinguishing Between Left-And Right-Sided Atrial TachycardiaRully SyahrizalÎncă nu există evaluări
- Princess Diana SpeechDocument5 paginiPrincess Diana SpeechPasca AlexÎncă nu există evaluări