Documente Academic
Documente Profesional
Documente Cultură
Efek Amniotomi Awal Partus Spontan
Încărcat de
Lauren RenDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Efek Amniotomi Awal Partus Spontan
Încărcat de
Lauren RenDrepturi de autor:
Formate disponibile
Effect of early amniotomy on the outcome of spontaneous labour: a randomized
controlled trial of pregnant women in Enugu, South-east Nigeria
Livinus N. Onah,1 Cyril C. Dim,2 Uchenna I. Nwagha,2 Benjamin C. Ozumba2
1. Departments of Obstetrics and Gynaecology, College of Medicine Enugu State
University of Science and Technology, Enugu Nigeria
2. Departments of Obstetrics and Gynaecology, College of Medicine University of Nigeria Enugu Campus, Ni-
geria
Abstract
Background: Early amniotomy is common in obstetric practice but, its effectiveness has not been proven.
Objectives: To determine the effects of early amniotomy on the duration of labour, and other maternal / neonatal out-
comes of uncomplicated pregnancies in Enugu, South-east Nigeria.
Methods: A randomized controlled study of 214 consenting term pregnant women at the University of Nigeria Teaching
Hospital Enugu, Nigeria. Intervention group received amniotomy early in active labour while the control group had their
membranes conserved.
Results: Mean duration of labour for the amniotomy group (279.4 53.7 minutes) was significantly lower than that of con- trol
group (354.4 67.5 minutes), (t = -8.988, p <0.001). Three (3.8%) women in amniotomy group needed oxytocin aug-
mentation as against 21 (19.6%) women in the control group RR = 0.14, (CI 95%: 0.04 0.46), NNT = 16. The two groups did
not vary with respect to cesarean section rate, newborn Apgar scores, and need for new born special care unit admission.
Conclusion: Early amniotomy when compared to fetal membrane conservation reduced the duration of labour and need
for oxytocin augmentation among term singleton pregnant women in Enugu, Nigeria. Its routine use in well selected cases may
reduce prolonged labour and its complications.
Keywords: Early amniotomy, duration of labour, oxytocin augmentation, term pregnancy, caesarean section rate, Enugu-
Nigeria.
DOI:http://dx.doi.org/10.4314/ahs.v15i4.7
Cite as: Onah LN, Dim CC, Nwagha UI, Ozumba BC. Effect of early amniotomy on the outcome of spontaneous labour : a randomized controlled trial of
pregnant women in Enugu, South-east Nigeria. Afri Health Sci. 2015;15(4):1097-103. http://dx.doi.org/10.4314/ahs. v15i4.7
Introduction as active phase when the cervical dilation is 4 cm and
The aim of labour management is to deliver healthy above3. Early amniotomy is one of the most common-
babies to healthy mothers with minimum adverse ef- ly performed procedures in modern obstetric practice
fects1. This objective is achieved by close monitoring with the aim of enhancing the progress of labour and
of maternal and fetal conditions during labour with ap- preventing dystocia in women in spontaneous labour4,5.
propriate interventions when necessary. One of these However, the effectiveness of this intervention in aug-
interventions introduced in labour management with- menting labour has not been proven4, so it remains a
out much evidence is early amniotomy2 which can be subject for debate and further research.
described as the elective rupture of fetal membranes
early in active phase of labour. Labour is described Early amniotomy may be beneficial in the early iden-
tification of problems during labour and for early in-
tervention. For instance, it allows for close monitoring
Corresponding author: of the liquor, placement of electrodes and intrauter-
Cyril C. Dim, ine pressure catheter6. On the other hand, it may be
Departments of Obstetrics and Gynaecology, associated with increased risks of fetal heart rate ab-
College of Medicine University of Nigeria normalities, cord prolapse, pains with request for anal-
Enugu Campus, Nigeria gesia, caesarean section rate, and infection because of
P.M.B. 01129, Enugu. 400001. Nigeria increased rate of vaginal examination7-9. Furthermore, as
Email: cyril.dim@unn.edu.ng part of prevention of vertical transmission of ma-
Tel: +234 803 334 1960 ternal infections, the procedure has relative contraindi-
1097 African Health Sciences Vol 15 Issue 4, December 2015
cations in women living with HIV/AIDS3,10. It is also bour duration from a previous study13, assumed stand-
avoided in patients with high fetal presenting part, cord ardized effect size of 0.4, power of 80% at 95% confi-
presentation, placenta praevia, transverse lie and vasa dence level, and drop-out rate of 10%.
praevia11. Though, early amniotomy is a component To reduce the difficulties associated with counseling
of active management of labour proposed to reduce women in labour as well as late presentation, screen-
rate of caesarean section for dysfunctional labour7, its ing of pregnant women for the study was done at the
effect on the duration of labour has not been consist- antenatal clinic of the hospital and those that met the
ent. Some studies have shown significant reduction of above eligibility criteria (except being in labour) were
labour duration but, no effect on other outcome meas- identified and counseled individually about the study.
ures12,13, while few have shown no consistent effect of Each consenting woman was reminded of the symp-
the intervention on labour duration and other outcome toms of labour and encouraged to present to the labour
measures4,14. A randomized trial of 128 women in Ile- ward early in labour. Also, she was issued an identifier
Ife, South-western Nigeria13, showed that the duration which she submitted at the labour ward of the hospi-
of labour in women that had early amniotomy was sig- tal when in labour. On presentation of the identifier,
nificantly shorter than the non-amniotomy group. But, her eligibility was re-confirmed by a trained assistant
there was no difference in the caesarean section rates, (senior resident doctor) and a written consent obtained.
oxytocin use, and other outcomes between the groups13. Afterwards, a sequential study number was assigned
In view of the inconsistencies inherent in the findings to the woman then, a medical intern on duty retrieved
of previous studies; there is need for further research in the envelope bearing the participants number, and the
this subject area. Therefore, this study was aimed at de- woman was allocated to the group concealed in the en-
termining the effects of early amniotomy on the dura- velope. Thus the sample size per group represents only
tion of labour, and other maternal / neonatal outcomes eligible women that arrived in labour ward before dilat-
of women with uncomplicated pregnancies in Enugu, ing beyond 5 cm.
South-east Nigeria.
Women assigned to the intervention group received
Methods amniotomy at a cervical dilatation of 4 - 5cm13. Before
This was a randomized controlled study of consenting the procedure, each woman was allowed to empty her
pregnant women admitted in the labour ward of Uni- bladder and pre-amniotomy fetal heart rate assessed.
versity of Nigeria Teaching Hospital (UNTH), Enugu, Observing aseptic procedure, the perineum was cleaned
South-eastern Nigeria, from November 2012 to April with dilute chlorhexidine and digital vaginal examina-
2013. All singleton term pregnant women in spontane- tion carried out to assess cervical dilatation and other
ous active labour with intact fetal membranes were eli- Bishop Score parameters. After that, amniotomy was
gible for the study. Exclusion criteria included abnormal performed with Kochers forceps using the standard
presentations, cervical dilation of 6cm or more, previ- method3 followed by post-amniotomy fetal heart rate
ous caesarean section, cord presentation, and medical assessment.
complications in pregnancy such as diabetes mellitus,
preeclampsia, and HIV infection. The ethical commit- Participants assigned to the control group had their fe-
tee of the hospital approved the study. tal membranes conserved. For both groups, labour was
monitored actively with partograph, using the standard
Participants randomization into the intervention (amni- protocol of the hospital thus: the fetal heart rate was
otomy) or control (No-amniotomy) group was accom- monitored quarter hourly by intermittent auscultation,
plished by an independent statistician using a computer uterine contractions and maternal vital signs were as-
generated random number sequence that were placed sessed half hourly, while vaginal examination was done
into consecutively numbered opaque, sealed envelopes. every 4 hours (and 2hourly for those on oxytocin aug-
These envelopes were kept in a secure locker in the la- mentation). Appropriate standard obstetric interven-
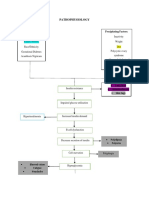
bour ward. The randomization flow chart is shown in tions were used to manage abnormalities in labour.
Figure 1. Oxytocin augmentation was commenced for every par-
ticipant that had cervical dilatation of 2cm or less in 4
The sample size (n) for the study was 107 women per hour (slow progress) and stable feto-maternal condition
group; it was based on standard deviation of mean la- irrespective of her group. However, for the no-amniot-
African Health Sciences Vol 15 Issue 4, December 2015 1098
omy group with slow progress, amniotomy was done pants randomization to delivery of the baby.
and oxytocin infusion started at the same time. The Statistical package for social sciences (SPSS) version
oxytocin augmentation followed a standard protocol; 15.0 for windows was used for data entry and analy-
starting with 4miu/min and increasing at interval of 30 sis. Data analysis was by intention to treat. Associations
minutes to achieve adequate uterine contraction pattern were tested with chi square test (categorical data) and
of 3-5 contractions in 10 minutes, each lasting 40-60 independent t-test (continuous data) at 95% confidence
seconds7. level. A p-value of < 0.05 was considered as statistically
The primary outcome measure was the duration of la- significant.
bour in both arms of the study. The secondary outcome
measures were all-cause cesarean section rate, need for Results
oxytocin argumentation, Apgar scores, and need for A total of 214 women were enrolled for the study and
New Born Special Care Unit (NBSCU) admission. randomized equally into intervention (amniotomy)
For the purpose of this study, duration of labour was group (n=107) and control (no-amniotomy) group
defined as the time interval in minutes from a partici- (n=107). All participants completed the study and were
analyzed (figure 1)
Figure 1: Flow chart of the Study
Assessed for eligibility
(n = 260)
Excluded
(n = 46)
Women Randomized
(n = 214)
Allocated to amniotomy group Allocated to non-amniotomy group
(n = 107) (n = 107)
Loss to Loss to
follow-up follow-up
(n = 0) (n = 0)
Analyzed Analyzed
(n = 107) (n = 107)
African Health Sciences Vol 15 Issue 4, December 2015
1099
Participants basic characteristics such as age groups, women were married (86.0%, 92/107 versus 82.2%,
parity, gestational age, and neonatal birth weight were 88/107), nulliparous (32.7%, 35/107 versus 35.5%,
similar between the two groups (tables 1 and 2). For 38/107), and aged 35-39 years (45.8%, 49/107 versus
both intervention and control groups, majority of 42.1, 45/107).
Table 1: Basic characteristics of participants
Amniotomy Control
(n = 107) (n = 107)
Characteristics Sub-group P-value
Freq (%) Freq (%)
Age groups (years) 20 24 9(8.4) 12 (11.2)
25 29 18(16.8) 22 (20.6)
30 34 9(8.4) 11 (10.3) 0.765
35 39 49(45.8) 45 (42.1)
40 44 22(20.6) 17 915.9)
Marital status Single 15(14.0) 19(17.8)
Married 92(86.0) 88(82.2) 0.56
Parity groups Para 0 35(32.7) 38(35.5)
1 24(22.4) 27(25.2)
24 28(26.2) 19(17.8) 0.526
5 20(18.7) 23(21.5)
Table 2: Other basic characteristics of participants
Amniotomy Control
(n = 107)
Characteristics P value
(n = 107)
Mean SD Mean SD
Parity 2.51.370 2.5 1.383 0.67
Gestational age (weeks) 38.81.26 39.11.38 0.20
Cervical dilation at randomization (cm) 4.60.49 4.70.46 0.15
Birth weight (kg) 3.2.493 3.1.418 0.17
The mean cervical dilatation at randomization for the was 279.4 53.7 minutes while that of the control was
amniotomy group was 4.6 0.49 median = 5 (range 4 354.4 67.5 minutes. The observed difference (74.9
-5) cm while that of the control group was 4.7 0.46 minutes) between the 2 groups was statistically signif-
median = 5 (range 4 -5) cm. The observed difference icant (t = -8.988, p <0.001). For nulliparous women,
was not statistically significant (t = -1.437, p = 0.152). the duration of labour for the amniotomy and control
There was no maternal death or neonatal death in either groups were 287.1 66.54 and 358.6 60.64 respec-
group during the study period. tively (t = -4.785, p <0.001), while the values for similar
The mean duration of labour for the amniotomy group groups of parous women (para 1) were 275.7 46.2
and 352.0 71.3 (t = -7.507, p <0.001).
African Health Sciences Vol 15 Issue 4, December 2015 1100
The over-all oxytocin augmentation rate for the study Thirteen (12.1%) and 17 (15.9%) babies had low 1st
was 11.2% (24/214). Three (3.8%) women in amnioto- minute Apgar score (< 7) in the amniotomy and control
my group needed oxytocin augmentation as against 21 groups respectively. The observed difference was not
(19.6%) women in the no-amniotomy group RR = 0.14, statistically significant (p = 0.431). Likewise, the pro-
(CI 95%: 0.04 0.46), p < 0.001, NNT = 16 portion of babies with low 5th minute Apgar score did
In all, the cesarean section rate among participants was not differ between the two groups (0.9%, 1/107 versus
5.6% (12/214). The incidence of emergency cesarean 2.8%, 3/107, p = 0.62). Also, the proportion of neonates
section among women in the amniotomy group (6.5%, that needed New Born Special Care Unit (NBSCU) did
7/107) did not differ from that of the control group not differ between the amniotomy and control groups
(4.7%, 5/107) RR = 1.4, (CI 95%: 0.46 4.27), p = (p > 0.05). Further details of the association between
0.768. early amniotomy during labour and selected maternal /
neonatal variables are shown in table 3.
Table 3: Early Amniotomy verses Apgar Scores / Admissions to New-born special care unit
Amniotomy Control
Variable Variable (n = 107) (n =1 07) P value RR (CI 95%)
category Freq (%) Freq (%)
Oxytocin Yes 3 (2.8) 21 (19.6) <0.001 0.14 (0.04, 0.46)
augmentation
No 104 (97.2) 86 (80.4)
Emergency C/S Yes 7 (6.5) 5 (4.7) 0.77 1.4 (0.46, 4.27)
No 100 (93.5) 102 (95.3)
1st minute Apgar <7 13 (12.1) 17 (15.9) 0.43 0.76 (0.39, 1.50)
7 94 (87.9) 90 (84.1)
5th minute Apgar <7 1 (0.9) 3 (2.8) 0.62 0.33 (.04, 3.15)
7 106 (99.1) 104 (97.2)
NBSCU admission Yes 11 (10.3) 9 (8.4) 0.64 1.22 (0.53, 2.83)
No 96 (89.7) 98 (91.6)
Discussion including Nigeria, characterized by high maternal/per-
The provision of effective obstetric services for the inatal morbidity and mortality. The significant shorter
management of common obstetric conditions is a nec- duration of labour associated with amniotomy in this
essary means of reducing maternal morbidity and mor- study is similar to the findings of the only identifiable
tality especially in developing countries. As demonstrat- ed related study from Nigeria13. While we encourage more
in this study, early amniotomy may be included into the studies in the subject from other populations of the
list of such effective practices which may explain why it country, the available evidence suggests that this simple
was introduced as an element of active manage- ment of intervention (early amniotomy) may be effective in the
labour15. The observed reduction in the dura- tion of wider Nigerian population when utilized appropriately.
labour in the amniotomy group of this study has been Furthermore, the observed shorter duration of labour
attributed to the increased efficiency of uterine associated with amniotomy in our study, is similar to the
contraction and prevention of labour dysfunction4,16. reports of related studies outside Nigeria12,14,17,18. How-
Therefore, early amniotomy may be considered as a ever, it contrasts the reports of other related studies
low-cost accessible intervention to reduce prolonged that showed no significant association between amniot-
labour and its associated complications this observa- omy and the duration of labour4,19. A recent systematic
tion has practical implication in low resourced settings review of 15 studies involving 5583 women had noted
1101 African Health Sciences Vol 15 Issue 4, December 2015
no clear association between amniotomy and duration tionship with early amniotomy in labour which suggests
of labour which holds for both primiparous and mul- that the procedure does not add to the complications
tiparous sub-groups; however, the observed high heter- of normal labour. This observation was noted in relat-
ogeneity among the included trials might have impacted ed studies13,17. No case of umbilical cord prolapse was
on the outcome of the review4. observed in this study despite the possible causal rela-
tionship it appears to have with amniotomy2 this find-
This study also demonstrated less need for oxytocin use ing may also support the safety of the early amniotomy in
when amniotomy was done when compared with the uncomplicated labour.
non-amniotomy group, which is in line with the report Outside the limitation of small sample size and restric-
of a related study12. This finding may not be surprising tion of the study to low risk pregnant women discussed
considering the suggested effect of amniotomy on the earlier, the study could only measure randomization to
efficiency of uterine contraction discussed earlier. In delivery interval because of the difficulty in determin-
fact, according to this study, sixteen women needed to ing the actual time at which a labouring woman reached
receive early amniotomy in labour in order to prevent full cervical dilatation. Furthermore, contamination was
one case of oxytocin augmentation. Though this num- inevitable for the few participants in the control group
ber needed to treat (NNT) does not appear very low, that had amniotomy at cervical dilation of less than 6
it may have positive practical impact in resource poor cm due to slow progress of labour however; the effect
settings prevalent in developing countries. For instance, on the primary outcome was likely to be very minimal.
the reduction in oxytocin requirement implies that the
extra financial cost of procuring oxytocin as well as the Conclusion
intense pain resulting from oxytocin use in labour can Early amniotomy when compared to fetal membrane
be reduced by early amniotomy of eligible women. This conservation reduced the duration of labour and the
possible cost reduction effect of early amniotomy is need for oxytocin augmentation among term singleton
most important in our setting where payment for ma- pregnant women in Enugu, Nigeria. It also has no neg-
ternal and neonatal health care services is usually out of ative effect on caesarean section rate and neonatal out-
pocket because of lack of functional community comes. Therefore, its routine use in the management of
health insurance system. Unfortunately, our study did uncomplicated labour may reduce prolonged labour and
not cover these outcomes therefore; we suggest that fu- its attendant effects on maternal and neonatal health.
ture studies in this subject in under-resourced settings
should consider including indicators on cost assess- Acknowledgment
ment, clients pain perception and satisfaction. Authors acknowledge our research assistants, midwife-
It is noteworthy that the study population used for this ry and other staff of antenatal clinic and labour ward
study was essentially low risk pregnant women so, it is of the UNTH, Enugu, Nigeria.
probable that the effect of early amniotomy in this
group may differ for high risk pregnant sub-group. Conflict of interest
The authors declare no conflicts of interest.
Like the study from South-western Nigeria13, the in-
cidence of emergency caesarean section in our study References
has no association with early amniotomy in labour. 1. Orhue AAE (2005) Normal labour. In: Agboola A
This finding is unfortunate for our environment where (ed) Textbook of Obstetrics & Gynaecology for Med-
aversion for caesarean section exists20-22. Though, these ical Students, 2nd edn. Heinemann Educational Books
studies findings are consistent with the result of a re- PLC, Ibadan, pp 283-302
cent systematic review4, the effect of small sample size 2. Cohain JS (2013) The less studied effects of Amniot-
cannot be ruled out because caesarean section rate was a omy J Matern Fetal Neonatal Med 26:1687-1690
secondary measure in the studies; so, there is a need for 3. World Health Organization (WHO) (2000) Manag-
a large sample multicenter collaborative study to clarify ing complication in pregnancy and childbirth: A guide-
their findings especially the secondary measures. Lastly, line for midwives and doctors WHO, Geneva
the neonatal outcome in terms of the low Apgar scores, 4. Smyth RM, Markham C, Dowswell T (2013). Am-
and need for NBSCU admission had no rela- niotomy for shortening spontaneous labour. Cochrane
Database Syst Rev 6: CD006167
African Health Sciences Vol 15 Issue 4, December 2015 1102
5. Rogers R, Gilson GJ, Miller AC, Izquierdo LE, Cur- 14. Johnson N, Lilford R, Guthrie K, Thornton J, Bark-
ret LB, Qualls CR (1997). Active management in labour. er M, Kelly M (1997) Randomized trial comparing a
Does it make a difference? Am J Obstet Gynecol 177:599- policy of early amniotomy with selective amniotomy in
605 uncomplicated labour at term. Br J Obstet Gynaecol
6. Archie CL, Roman AS (2013) Normal & Abnormal 104:340-346
Labor & Delivery. In: Decherney AH, Nathan L, Laufer 15. O'Driscoll K, Foley M, MacDonald D (1984) Active
N, Roman AS (eds) Current Diagnosis & Treatment in management of labor as an alternative to cesarean sec-
Obstetrics & Gynecology 11th edn McGraw-Hill Com- tion for dystocia. Obstet Gynecol 63: 485-490
panies, New York, pp 154 162 16. Busowski JD, Parsons MT (1995) Amniotomy to in-
7. ACOG Practice Bulletin No. 107 (2009) Induction of duce labor. Clin Obstet Gynecol 38: 246-258
labor. ACOG Committee on Practice Bulletins -- Ob- 17. UK Amniotomy Group (1994) A multicentre rand-
stetrics Obstet Gynecol 114: 386-397 omized trial of amniotomy in spontaneous first labour
8. Goffinet F, Fraser W, Marcoux S, Breart G, Moutquin at term. Br J Obstet Gynecol 101:307-309
JM, Daris M (1997) Early amniotomy increases the fre- 18. Barrett JF, Savage J, Philips K, Lifford RJ (1992)
quency of fetal heart rate abnormalities. Br J Obstet Gy- Randomised trial of amniotomy in labour versus the
naecol 104:548-553. intention to leave membranes intact until second stage.
9. Busowski JD, Parsons MT (1995) Amniotomy to in- Br J Obstet Gynaecol 99: 5-9
duce labour. Clin Obstet Gynecol 38: 246-58. 19. Fraser WD, Sauve R, Parboosingh IJ, Fung T, Sokol
10. Federal Ministry of Health (FMOH) Nigeria (2010) R, Persaud D (1991) A randomized controlled trial of
National Guidelines for Prevention of Mother-To- early amniotomy. Br J Obstet Gynaecol 98: 8491
Child Transmission of HIV (PMTCT) FMOH Abuja 20. Okonkwo NS, Ojengbede OA, Morhason_Bello IO,
11. Baskett TF, Calder AA, Arulkumaran S (2007) Mun- ro Adedokun BO (2012) Maternal demand for cesarean
Kerrs Operative Obstetrics. 11th edn Elsevier Ltd, section: perception and willingness to request by Nige-
Edinburgh rian antenatal clients. Int J Womens Health 4: 141-8
12. Fraser WD, Marcoux S, Moutquin JM, Christen A 21. Sunday_Adeoye I, Kalu C (2011) Pregnant Nigerian
(1993) Effect of early amniotomy on the risk of dysto- womens view of cesarean section. Niger J Clin Pract 14:
cia in nulliparous women. The Canadian Early Amniot- 276-9
omy Study Group. N Engl J Med 328: 1145- 1149 22. Nkwo PO, Onah HE (2009) Does a preference for
13. Ajadi MA, Kuti O, Orji E,O. Ogunniyi SO, Sule SS symphysiotomy over caesarean section reduce the oper-
(2006) The effect of amniotomy on the outcome of ative delivery rate? Trop Doct 39: 198-200
the spontaneous labour in uncomplicated pregnancy. J
Obstet Gynaecol 26: 631-634
1103 African Health Sciences Vol 15 Issue 4, December 2015
S-ar putea să vă placă și
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- Treatment Plan TemplatesDocument2 paginiTreatment Plan TemplatesShalini Dass100% (3)
- Psychiatric NursingDocument21 paginiPsychiatric NursingFreeNursingNotes92% (38)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Medics PHC Protocols 3rd EditionDocument102 paginiMedics PHC Protocols 3rd EditionLee HillÎncă nu există evaluări
- Basic Hematologic TestsDocument9 paginiBasic Hematologic TestsdtimtimanÎncă nu există evaluări
- Based on the clinical scenario and peripheral blood smear findings, this patient has now developed secondary myelofibrosis as a progression of his previously diagnosed polycythemia veraDocument22 paginiBased on the clinical scenario and peripheral blood smear findings, this patient has now developed secondary myelofibrosis as a progression of his previously diagnosed polycythemia veraAdeena RayÎncă nu există evaluări
- DISCHARGE INSTRUCTIONSDocument7 paginiDISCHARGE INSTRUCTIONSJyselle Domingo100% (4)
- ATLSPracticeTest3 PDFDocument10 paginiATLSPracticeTest3 PDFRodrigo Sanjines75% (4)
- Comm 1010 Informative Full-Sentence Speech Outline InstructionsDocument2 paginiComm 1010 Informative Full-Sentence Speech Outline Instructionsapi-270505782Încă nu există evaluări
- Jadwal Jaga Dokter Internship Igd RSK Ngesti Waluyo: Bulan DESEMBER 2018Document1 paginăJadwal Jaga Dokter Internship Igd RSK Ngesti Waluyo: Bulan DESEMBER 2018Lauren RenÎncă nu există evaluări
- ADocument1 paginăALauren RenÎncă nu există evaluări
- Sindroma Serebral: DR - Rejeki Andayani R, Sppd-Kger SemarangDocument7 paginiSindroma Serebral: DR - Rejeki Andayani R, Sppd-Kger SemarangLauren RenÎncă nu există evaluări
- Bimbingan IPD - DR - MarshellDocument32 paginiBimbingan IPD - DR - MarshellLauren RenÎncă nu există evaluări
- Jadwal Jaga Dokter Internship Igd RSK Ngesti Waluyo: Bulan Januari 2019Document1 paginăJadwal Jaga Dokter Internship Igd RSK Ngesti Waluyo: Bulan Januari 2019Lauren RenÎncă nu există evaluări
- Acls AlgorithmsDocument8 paginiAcls Algorithmsdydy_7193Încă nu există evaluări
- Evaluation of The Efficacy and Safety of Foley Catheter Pre-Induction of LaborDocument2 paginiEvaluation of The Efficacy and Safety of Foley Catheter Pre-Induction of LaborLauren RenÎncă nu există evaluări
- ADocument1 paginăALauren RenÎncă nu există evaluări
- Poor Spontaneous and Oxytocin-Stimulated Contractility in Human Myometrium From Postdates PregnanciesDocument11 paginiPoor Spontaneous and Oxytocin-Stimulated Contractility in Human Myometrium From Postdates PregnanciesLauren RenÎncă nu există evaluări
- Bimbingan IPD - DR - MarshellDocument32 paginiBimbingan IPD - DR - MarshellLauren RenÎncă nu există evaluări
- Indikator NulliDocument8 paginiIndikator NulliLauren RenÎncă nu există evaluări
- A Retrospective Study of Ovarian Cysts: Shivaji Neelgund, Panchaksharayya HiremathDocument5 paginiA Retrospective Study of Ovarian Cysts: Shivaji Neelgund, Panchaksharayya HiremathLauren RenÎncă nu există evaluări
- Acute Abdomen in Early Pregnancy Caused by Torsion of Bilateral Huge Multiloculated Ovarian CystsDocument4 paginiAcute Abdomen in Early Pregnancy Caused by Torsion of Bilateral Huge Multiloculated Ovarian CystsLauren RenÎncă nu există evaluări
- Clinicopathological Profile of Ovarian Tumors in The Age Group 10-20 YearsDocument4 paginiClinicopathological Profile of Ovarian Tumors in The Age Group 10-20 YearsLauren RenÎncă nu există evaluări
- Vetebrobasiler StrokeDocument1 paginăVetebrobasiler StrokeLauren RenÎncă nu există evaluări
- A Retrospective Study of Ovarian Cysts: Shivaji Neelgund, Panchaksharayya HiremathDocument5 paginiA Retrospective Study of Ovarian Cysts: Shivaji Neelgund, Panchaksharayya HiremathLauren RenÎncă nu există evaluări
- 127 FullDocument9 pagini127 FullCho HyumiÎncă nu există evaluări
- 01 MynckeDocument10 pagini01 MynckeIrina DesyatykhÎncă nu există evaluări
- Dinakaran 2017Document16 paginiDinakaran 2017Chirac OanaÎncă nu există evaluări
- Rice DiseaseDocument23 paginiRice DiseaseRayge HarbskyÎncă nu există evaluări
- Schreibman - Radiology of Joint Disease - My Practical ApproachDocument16 paginiSchreibman - Radiology of Joint Disease - My Practical ApproachborstÎncă nu există evaluări
- Pathophysiology: Predisposing Factors: Precipitating FactorsDocument2 paginiPathophysiology: Predisposing Factors: Precipitating FactorsJemsMei Comparativo MensuradoÎncă nu există evaluări
- Mendelson SyndromeDocument6 paginiMendelson SyndromeResa PutraÎncă nu există evaluări
- The Cotton DriverDocument2 paginiThe Cotton DriverDanny Eduardo RomeroÎncă nu există evaluări
- Study On Effect of Wet Cupping (Hijama) On Blood Lipid Profile in Human at Aldyssah-Alshati, LibyaDocument4 paginiStudy On Effect of Wet Cupping (Hijama) On Blood Lipid Profile in Human at Aldyssah-Alshati, LibyaMohammed Ramzy GhifariÎncă nu există evaluări
- Approved HIV AIDS Rapid Test KitsDocument2 paginiApproved HIV AIDS Rapid Test KitsAnonymous HtkC5Ef64Încă nu există evaluări
- Cancer: Get A Cancer Cover of ' 20 Lakhs at Less Than ' 4 / DayDocument6 paginiCancer: Get A Cancer Cover of ' 20 Lakhs at Less Than ' 4 / DayUtsav J BhattÎncă nu există evaluări
- CA125: A Marker for Ovarian Cancer Detection and MonitoringDocument3 paginiCA125: A Marker for Ovarian Cancer Detection and Monitoringडा. सत्यदेव त्यागी आर्यÎncă nu există evaluări
- Breast Augmentation and Breast ReductionDocument13 paginiBreast Augmentation and Breast ReductionDjlatino LatinoÎncă nu există evaluări
- Cigarette Smoking Harms HealthDocument2 paginiCigarette Smoking Harms HealthevangelineÎncă nu există evaluări
- Management of Intraocular Foreign BodiesDocument7 paginiManagement of Intraocular Foreign BodiesdebbyÎncă nu există evaluări
- Fundamentals of Rheumatoid Arthritis and Various Homoeopathic Trials in Patients of Rheumatoid Arthritis: An UpdateDocument6 paginiFundamentals of Rheumatoid Arthritis and Various Homoeopathic Trials in Patients of Rheumatoid Arthritis: An UpdateHomoeopathic PulseÎncă nu există evaluări
- Seminar: Annelies Wilder-Smith, Eng-Eong Ooi, Olaf Horstick, Bridget WillsDocument14 paginiSeminar: Annelies Wilder-Smith, Eng-Eong Ooi, Olaf Horstick, Bridget WillsAlexander ArguelloÎncă nu există evaluări
- Diseases of The Bone Marrow and Blood Conditions That Can Occur When The Blood-Forming Cells in The Bone Marrow Become AbnormalDocument4 paginiDiseases of The Bone Marrow and Blood Conditions That Can Occur When The Blood-Forming Cells in The Bone Marrow Become AbnormalLuqman QadirÎncă nu există evaluări
- Gulan 2003 Klinicka - I - Radioloska - Prezentacija - Kostanih Medri - 1319 Publishedversion H0k4iq SDocument10 paginiGulan 2003 Klinicka - I - Radioloska - Prezentacija - Kostanih Medri - 1319 Publishedversion H0k4iq SMuxoliniÎncă nu există evaluări
- 04.02 Assignment FinishedDocument5 pagini04.02 Assignment Finishedjazzmine andesonÎncă nu există evaluări
- Fucidin®: Product MonographDocument21 paginiFucidin®: Product MonographLeonita SabrinaÎncă nu există evaluări
- BREAST CANCER CLINICAL PHARMACY PRESENTATIONDocument21 paginiBREAST CANCER CLINICAL PHARMACY PRESENTATIONfrankÎncă nu există evaluări
- Micro-503 - (T) - Course Outline and ScheduleDocument2 paginiMicro-503 - (T) - Course Outline and ScheduleUmer AliÎncă nu există evaluări
- D5imb IvDocument1 paginăD5imb IvSeno HyeonÎncă nu există evaluări