Documente Academic
Documente Profesional
Documente Cultură
Effectiveness and Safety of Standard-Dose Nonvitamin K Antagonist Oral Anticoagulants and Warfarin Among Patients With Atrial Fibrillation With A Single Stroke Risk Factor
Încărcat de
Roberto López MataTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Effectiveness and Safety of Standard-Dose Nonvitamin K Antagonist Oral Anticoagulants and Warfarin Among Patients With Atrial Fibrillation With A Single Stroke Risk Factor
Încărcat de
Roberto López MataDrepturi de autor:
Formate disponibile
Research
JAMA Cardiology | Original Investigation
Effectiveness and Safety of Standard-Dose Nonvitamin K
Antagonist Oral Anticoagulants and Warfarin Among Patients
With Atrial Fibrillation With a Single Stroke Risk Factor
A Nationwide Cohort Study
Gregory Y. H. Lip, MD; Flemming Skjth, MSc, PhD; Peter Brnnum Nielsen, MSc, PhD;
Jette Nordstrm Kjldgaard, BSc; Torben Bjerregaard Larsen, MD, PhD
Supplemental content
IMPORTANCE The randomized clinical trials comparing nonvitamin K antagonist oral
anticoagulants (NOACs) vs warfarin largely focused on recruiting high-risk patients with atrial
fibrillation with more than 2 stroke risk factors, with only the trials testing dabigatran or
apixaban including few patients with 1 stroke risk factor. Despite this, regulatory approvals of
all NOACs have been based on stroke prevention for patients with atrial fibrillation with 1 or
more stroke risk factors.
OBJECTIVE To compare the effectiveness and safety study of standard-dose NOACs
(dabigatran at 150 mg twice daily, rivaroxaban at 20 mg once daily, and apixaban at 5 mg
twice daily) and warfarin in patients with atrial fibrillation with 1 low-risk, nonsex-related
stroke risk factor.
DESIGN, SETTING, AND PARTICIPANTS This nationwide observational cohort study used data
from Danish registries to determine the inverse probability of treatment-weighted
comparative effectiveness and safety of standard-dose NOACs (dabigatran at 150 mg twice
daily, rivaroxaban at 20 mg once daily, and apixaban at 5 mg twice daily) compared with
treatment with warfarin among 14 020 patients with atrial fibrillation with 1 low-risk, nonsex-
related stroke risk factor.
MAIN OUTCOMES AND MEASURES Rates of ischemic stroke/systemic embolism, death, and
bleeding.
RESULTS Of 14 020 participants, 5151 (36.7%) were women, and the median age for
participants was 66.5 years. For the principal effectiveness end point of ischemic
stroke/systemic embolism, no significant differences of the NOACs compared with treatment
with warfarin across strata were evident. For the end point of any bleeding, this was
significantly lower for treatment with apixaban (hazard ratio [HR], 0.35; 95% CI, 0.17-0.72)
and dabigatran (HR, 0.48; 95% CI, 0.30-0.77) compared with warfarin in the main analysis, Author Affiliations: Aalborg
Thrombosis Research Unit,
and was not significantly different for treatment with rivaroxaban vs warfarin (HR, 0.84; 95%
Department of Clinical Medicine,
CI, 0.49-1.44). There was broad consistency across most subgroups in the sensitivity analyses Faculty of Health, Aalborg University,
and whether 1- or 2.5-year follow-up periods were analyzed. However, falsification end points Aalborg, Denmark (Lip, Skjth,
generally did not falsify, indicating the possible presence of residual confounding across these Nielsen, Kjldgaard, Larsen);
Institute of Cardiovascular Sciences,
comparisons, presumably related to selective prescribing and unobserved covariates. University of Birmingham,
Birmingham, England (Lip); Unit of
CONCLUSIONS AND RELEVANCE In this Danish cohort study of patients with atrial fibrillation Clinical Biostatistics, Aalborg
and a single stroke risk factor, there was no difference between NOACs compared with University Hospital, Aalborg,
treatment with warfarin in terms of the risk of having an ischemic stroke/systemic embolism. Denmark (Skjth); Department of
Cardiology, Aalborg University
For any bleeding, this was lower for treatment with apixaban and dabigatran compared with Hospital, Aalborg, Denmark (Nielsen,
warfarin. These data do not allow for a definitive statement of the comparative effectiveness Kjldgaard, Larsen).
or safety of NOACs because of the possible residual confounding that was unmasked with Corresponding Author: Gregory Y.
falsification outcomes. H. Lip, MD, University of Birmingham
Institute of Cardiovascular Sciences,
City Hospital, Birmingham,
JAMA Cardiol. doi:10.1001/jamacardio.2017.1883 West Midlands B18 7QH, England
Published online June 14, 2017. (g.y.h.lip@bham.ac.uk).
(Reprinted) E1
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/cardiology/0/ by Silverchair University, Roberto Lopez Mata on 06/15/2017
Research Original Investigation Effectiveness and Safety of Standard-Dose Nonvitamin K Antagonist Oral Anticoagulants and Warfarin
I
n the respective randomized clinical trials of nonvitamin
K antagonist oral anticoagulants (NOACs) for stroke pre- Key Points
vention in atrial fibrillation (AF), the focus was on recruit-
Question What is the effectiveness and safety study of
ing patients with AF with 2 or more stroke risk factors, and only standard-dose nonvitamin K antagonist oral anticoagulants
the trials testing treatment with dabigatran or apixaban in- (NOACs) and warfarin among patients with atrial fibrillation with 1
cluded a minority of patients with 1 stroke risk factor.1,2 To our stroke risk factor?
knowledge, specific randomized clinical trials including pa-
Findings In this nationwide observational cohort study, no
tients with AF with only 1 stroke risk factor have not been per- significant differences of the NOACs compared with warfarin
formed, and there is a low likelihood for such trials to be across strata were evident for the principal effectiveness end point
conducted. The objective of this study was to investigate the of ischemic stroke/systemic embolism. The end point of any
comparative effectiveness and safety of standard-dose bleeding was significantly lower for patients treated with
NOACs (dabigatran at 150 mg twice daily, rivaroxaban at 20 mg apixaban and dabigatran and not significantly different for
patients treated with rivaroxaban vs warfarin; however, there was
once daily, and apixaban at 5 mg twice daily) compared with
possible residual confounding across these comparisons that was
treatment with warfarin among such patients in the Danish unmasked with falsification outcomes.
registries.
Meaning Our data show no significant differences of the NOACs
compared with treatment with warfarin for ischemic
stroke/systemic embolism, but for any bleeding, this was lower
Methods for treatment with apixaban and dabigatran.
We conducted an observational cohort study of Danish citi-
zens initiating OAC treatment for stroke prevention in AF with Efficiency was investigated by the occurrence of ischemic
1 stroke risk factor. To align with previous randomized clini- stroke or systemic embolism. All-cause death was included as
cal trials, we focused on standard-dose NOAC agents only a lone end point. The safety of the treatments was investigated
and used Danish nationwide databases (eMethods in the by the following bleeding events: intracranial, gastrointesti-
Supplement).3-5 nal, traumatic intracranial, and clinically relevant nonmajor
The study was based on new users of OACs with no his- bleeding reported in total as any bleeding and more specifi-
tory of treatment for other indications than AF. For this analy- cally for intracranial (including traumatic) and gastrointesti-
sis, we only recruited patients with 1 nonsex-related stroke risk nal bleeding (see eTable 1 in the Supplement for International
factor that was assigned 1 point in the CHA2DS2-VASc score (ie, Statistical Classification of Diseases and Related Health Prob-
congestive heart failure or left ventricular disease, hyper- lems, Tenth Revision [ICD-10] discharge codes).7,8
tension, 65 years age <75 years, and diabetes or vascular A patients baseline comorbidities and comedications when
diseases such as myocardial infarction, aortic plaque or treatment was initiated were ascertained (Table 1) (eTable 1 in
peripheral aortic disease), thus excluding patients with prior the Supplement). The overall risk of bleeding was assessed by
strokes, systemic embolisms/transient ischemic attacks, or the hypertension, abnormal renal and liver function, stroke,
those who were younger than 75 years. bleeding, labile international normalized ratio, elderly, drugs
Nonvitamin K antagonist oral anticoagulants were re- or alcohol (HAS-BLED) score (eTable 2 in the Supplement).9 The
stricted to standard doses: apixaban at 5 mg twice daily, dabi- Danish registries are well-validated with a sufficiently high
gatran at 150 mg twice daily, and rivaroxaban at 20 mg once positive predictive value (>80%) of included comorbidities and
daily. To establish an OAC-naive cohort, we excluded pa- outcomes.10
tients previously treated with OAC-inclusive doses approved
for other indications within 1 year. Eventually, we excluded pa- Statistical Analysis
tients with prior diagnoses of valvular AF or a venous throm- A time to event analysis was used to compare the risk of an end
boembolism. Also, patients with contraindications for stan- point between treatment groups, measuring risk time from the
dard NOAC dose regimens because of renal impairment were patient receiving their initial prescription and until the rel-
excluded. This population formed the main cohort for the evant event, emigration, death, or end of follow-up (which-
analyses. Sensitivity analyses were reported on the subgroup ever came first). An intent-to-treat approach was applied for
with prior diagnoses of AF. To increase homogeneity6 across the main analyses. This was supplemented by a continuous
patient groups, we also performed a sensitivity analysis in treatment analysis by censoring the follow-up if the patient was
which patients with prior heart failure, chronic pulmonary dis- prescribed another treatment than what was initiated.
ease, or cancer were excluded. Crude incidence rates were calculated as the number of
events divided by the person-time. Cox regressions with a ro-
End Points and Variable Definitions bust variance estimator were used to compare event rates be-
Clinical end points were extracted from hospital discharge tween the treatment groups, with warfarin as the primary ref-
codes with follow-up until April 30, 2016 (eTable 1 in the erence. To address confounding by indication of treatment, an
Supplement). Primary and secondary discharge codes from inverse probability of treatment weighted (IPTW) analysis was
nonemergency wards were extracted. We only analyzed end applied.11,12 We used weights that enabled estimates represent-
points obtained as discharge codes from hospitalizations and ing mean population treatment effects. The underlying pro-
did not include codes from ambulatory visits. pensity models included the following treatment predictors: age
E2 JAMA Cardiology Published online June 14, 2017 (Reprinted) jamacardiology.com
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/cardiology/0/ by Silverchair University, Roberto Lopez Mata on 06/15/2017
Effectiveness and Safety of Standard-Dose Nonvitamin K Antagonist Oral Anticoagulants and Warfarin Original Investigation Research
Table 1. Participant Characteristics at Treatment Initiation According to Treatment
No. (%)
Characteristic Apixaban Dabigatran Rivaroxaban Warfarin All
No. of patients 1470 3272 1604 7674 14 020
Women 589 (40.1) 1160 (35.5) 609 (38.0) 2793 (36.4) 5151 (36.7)
Age, median (IQR) 67.4 (62.5-70.9) 66.2 (61.3-69.8) 67.2 (62.4-70.7) 66.2 (60.5-70.4) 66.5 (61.1-70.4)
Heart failure or LVD 31 (2.1) 90 (2.8) 17 (1.1) 232 (3.0) 370 (2.6)
Hypertension 411 (28.0) 1134 (34.7) 471 (29.4) 2430 (31.7) 4446 (31.7)
65 age <75 y 963 (65.5) 1884 (57.6) 1037 (64.7) 4435 (57.8) 8319 (59.3)
Diabetes 44 (3.0) 96 (2.9) 41 (2.6) 271 (3.5) 452 (3.2)
Vascular disease 21 (1.4) 68 (2.1) 38 (2.4) 306 (4.0) 433 (3.1)
Prior AF diagnosis 1042 (70.9) 2300 (70.3) 1037 (64.4) 4114 (53.6) 8489 (60.5)
Cancer 206 (14.0) 345 (10.5) 217 (13.5) 1079 (14.1) 1847 (13.2)
HAS-BLED score, mean (SD)a 1.5 (0.6) 1.5 (0.6) 1.5 (0.6) 1.5 (0.7) 1.5 (0.7)
Hepatic dysfunction <0.3 (<5) <0.1 (<5) 0.3 (5) 0.4 (29) 0.3 (39)
Alcohol 38 (2.6) 83 (2.5) 55 (3.4) 264 (3.4) 440 (3.1)
CPD 128 (8.7) 237 (7.2) 115 (7.2) 665 (8.7) 1145 (8.2)
Previous bleeding 128 (8.6) 224 (6.8) 128 (8.0) 521 (6.8) 999 (7.1)
Aspirin 342 (23.3) 960 (29.3) 437 (27.2) 2316 (30.2) 4055 (28.9)
Ticagralor <0.3 (<5) 0.4 (12) <0.2 (<5) 0.4 (31) 0.3 (49)
Clopidogrel 28 (1.9) 55 (1.7) 34 (2.1) 181 (2.4) 298 (2.1)
-blockers 914 (62.2) 2175 (66.5) 931 (58.0) 4408 (57.4) 8428 (60.1)
NSAIDs 339 (23.1) 806 (24.6) 386 (24.1) 2053 (26.8) 3584 (25.6)
Statins 359 (24.4) 817 (25.0) 387 (24.1) 2053 (26.8) 3616 (25.8)
ACE/ARB inhibiters 396 (26.8) 1000 (30.6) 430 (26.8) 2118 (26.8) 3944 (28.1)
Loop diuretics 97 (6.6) 200 (6.1) 94 (5.9) 680 (8.9) 1071 (7.6)
Concomitant cardiovascular
drugs, No.b
None 641 (43.6) 1288 (39.4) 627 (39.1) 3019 (39.3) 5575 (39.8)
1 341 (23.2) 727 (22.2) 394 (24.6) 1713 (22.3) 3175 (22.6)
2 259 (17.6) 602 (18.4) 298 (18.6) 1403 (18.3) 2562 (18.3)
3 127 (8.6) 369 (11.3) 177 (11.0) 901 (11.7) 1574 (11.2)
4 102 (6.9) 286 (8.7) 108 (6.7) 638 (8.3) 1134 (8.1)
a
Abbreviation: ACE/ARB, angiotensin converting enzyme inhibitor/angiotensin HAS-BLED: score ranging from 0 to 9, which reflects the risk of bleeding in
receptor blocker; AF, atrial fibrillation; CPD, chronic pulmonary disease; patients with atrial fibrillation undergoing anticoagulant therapy (eTable 2 in
HAS-BLED, hypertension, abnormal renal and liver function, stroke, bleeding, the Supplement).
labile international normalized ratio, elderly, drugs or alcohol; IQR, interquartile b
Cardiovascular drugs covers all Anatomical Therapeutic Chemical codes in
range; NSAIDs, non-steroidal anti-inflammatory drugs; LVD, left ventricle groups B and C.
disease.
(continuous); binary indicators for sex, prior bleeding, vascu- of first receiving a prescription. In addition, as there may be
lar disease, hypertension, diabetes, renal disease, chronic pul- confounding because of differences in the health status of pa-
monary disease, heart failure, cancer, and a recent prescrip- tients, we also reported results of analyses in which patients
tion for aspirin, -blockers, nonsteroidal anti-inflammatory with high-mortality conditions (heart failure, cancer, or chronic
drugs, statins, or loop diuretics; and the HAS-BLED score. pulmonary disorder) at the time treatment was initiated were
Balances between treatment populations were evaluated excluded. Eventually, the results of the IPTW analysis were
by the standardized differences of all baseline covariates, using compared with a trimmed analysis that removed 5% of the ex-
a threshold of 0.1 to indicate an imbalance.13 treme weights as well as with an ordinary crude and adjusted
To evaluate the potential for residual confounding, analysis (data not shown).
falsification analysis was performed by applying the The analyses on the entire population were supple-
propensityweighted cohort in the analyses on (falsifica- mented by stratified analyses on the populations with 1 of the
tion) end points that a priori should be expected not to be frequent risk factors who were older than 65 and patients with
associated with the effects of treatment.14 For this study, we hypertension; additionally, the results of the analyses were re-
considered pneumonia, hip fractures, cancer, and urinary ported for men and women separately. Stata/MP, version 14
tract infections. (StataCorp) and R version 3.1.1 (The R Foundation) were used
We repeated the analyses on the subgroup with a hospi- for the statistical analysis. A 2-tailed P value of less than .05
tal discharge diagnosis for AF either before or within 30 days was considered statistically significant.
jamacardiology.com (Reprinted) JAMA Cardiology Published online June 14, 2017 E3
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/cardiology/0/ by Silverchair University, Roberto Lopez Mata on 06/15/2017
Research Original Investigation Effectiveness and Safety of Standard-Dose Nonvitamin K Antagonist Oral Anticoagulants and Warfarin
Table 2. Number of Events and Crude and Weighted Event Rates According to Treatmenta
Apixaban Dabigatran Rivaroxaban Warfarin
Rate Rate Rate Rate
Events Crude Weighted Events Crude Weighted Events Crude Weighted Events Crude Weighted
1-y Follow-up
Ischemic stroke/SE 10 0.68 0.83 22 0.70 0.65 14 1.09 1.20 57 0.79 0.81
All-cause death 19 1.62 1.52 51 1.62 1.84 26 2.01 1.67 249 3.45 3.11
Any bleeding 8 0.68 0.57 23 0.74 0.73 17 1.33 1.38 109 1.52 1.53
Intracranial/gastrointestinal <5 0.09 0.06 6 0.19 0.16 <5 0.23 0.29 39 0.54 0.54
bleeding
2.5-y Follow-up
Ischemic stroke/SE 14 0.85 0.85 41 0.61 0.58 16 0.75 0.81 109 0.70 0.69
All-cause death 22 1.32 1.21 91 1.33 1.48 49 2.28 2.10 428 2.71 2.47
Any bleeding 11 0.67 0.56 44 0.65 0.65 22 1.04 1.09 202 1.30 1.31
Intracranial/gastrointestinal <5 0.12 0.12 17 0.25 0.21 6 0.28 0.30 72 0.46 0.45
bleeding
Abbreviations: IPTW, inverse probability of treatment weighed; SE, systemic embolism.
a
Crude rates are events divided by person time per 100 years; weighted rates are based on IPTW population and express population mean treatment rates per 100
years. Main analysis.
Ethical Considerations nant factor for inclusion was being 65 to 74 years (n = 8319,
No ethical approval is required for anonymous register stud- 59.3%). Patients initiated with dabigatran or warfarin were
ies in Denmark. The study was approved by the Danish Data slightly younger; 1884 patients (57.6%) were treated with dabi-
Protection Agency (J. No. File No. 2012-41-0633). gatran and 4435 (57.8%) were older than 65 years compared
with 963 patients (65.5%) treated with apixaban and 1037 pa-
tients (64.7%) treated with rivaroxaban who were older than
65 years. Hypertension, which affected 4446 participants
Results (31.7%), was lowest among the 411 patients (28.0%) initiated
We identified 240 360 unique OAC users in the inclusion with apixaban and 471 patients (29.4%) treated with rivaroxa-
period, 59% of whom (n = 142 307) either prevalently used ban and highest among the 1134 patients (37.4%) using dabi-
vitamin K antagonists or had an indication for treatment gatran. The remaining 1255 patients (8.9%) were included
because of other reasons than nonvalvular AF. Of the because they received a diagnosis of vascular diseases (eg, myo-
remaining OAC users (n = 98 053), we excluded 22% cardial infarction, peripheral artery disease, or aortic plaques),
(n = 21 456) because of treatment with reduced-dose NOACs diabetes, or heart failure. Diabetes was the primary reason
or because of the presence of prior discharge codes for renal among the NOACs, whereas they were distributed more evenly
impairment. Thus, the study population covers 76 597 new among patients treated with warfarin. Notably, 8750 patients
users of OAC treatment for AF, with either standard-dose (62.4%) had a prescription history with either 0 or only 1
NOACs or warfarin. Of these, 82% (n = 62 57 7) were drug within the Anatomical Therapeutic Chemical chapters
excluded because they had either 0 or more than 1 nonsex- B or C, which cover multiple cardiovascular indications.
related stroke risk factor or because their risk factors had Apixaban had the highest proportion (n = 982, 66.8%) and
scored a 2-point CHA2DS2-VASc score. warfarin (n = 4732, 61.6%) and dabigatran (n = 2015, 61.6%)
The final study population (n = 14 020) was distributed had a lower proportion. Approximately 1134 patients (8%)
according to treatment type: warfarin (n = 7674 [54.7%]), were intensively treated, with 4 or more different drugs pre-
dabigatran (n = 3272 [23.3%]), rivaroxaban( n = 1604 scribed, ranging from 108 patients (6.7%) in the group
[11.4%]), and apixaban (n = 1470 [10.5%]) (eFigure 1 in the treated with rivaroxaban to 286 patients (8.7%) in the group
Supplement). The mean (SD) follow-up was 2.6 (1.6) years, treated with dabigatran.
with the shortest follow-up for the group treated with After weighing the study populations using the IPTW
apixaban (mean [SD] follow-up, 1.1 [0.7] years) reflecting its method, all baseline differences were less than 0.08 standard-
later market introduction. ized differences at maximum (eFigure 2 in the Supplement).
Baseline information about the initial study population An inspection of individual propensity score distributions
before weighing is shown in Table 1. The 5151 women (36.7%) showed a sufficient overlap between treatment populations to
included in the study population were separated into treat- obtain a valid comparison (eFigures 3-5 in the Supplement).
ment groups: 1160 (35.5%) were treated with dabigatran, 589
(40.1%) were treated with apixaban, 2793 (36.4%) were treated Effectiveness: Stroke and Systemic Embolism
with warfarin, and 609 (38.0%) were treated with rivaroxa- Event count and crude or weighted rates for the different
ban. All patients had 1 nonsex-related and 1 point-valued stroke NOACs and warfarin are shown in Table 2, for 1 and 2.5 years
risk factor according to the CHA2DS2-VASc score. The domi- follow-up. Falsification analysis, described below, found that
E4 JAMA Cardiology Published online June 14, 2017 (Reprinted) jamacardiology.com
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/cardiology/0/ by Silverchair University, Roberto Lopez Mata on 06/15/2017
Effectiveness and Safety of Standard-Dose Nonvitamin K Antagonist Oral Anticoagulants and Warfarin Original Investigation Research
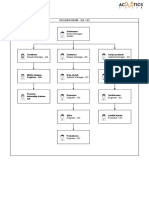
Figure 1. Propensity Weighted Cox Hazard Ratios for 1-Year Follow-Up for Nonvitamin K Antagonist Anticoagulants Compared With Warfarian for
Effectiveness, Safety, and Death End Points.
Ischemic
Strata/ Stroke/SE Favors Favors Any Bleeding Favors Favors Death Favors Favors
Treatment HR (95% CI) Alternative Warfarin HR (95% CI) Alternative Warfarin HR (95% CI) Alternative Warfarin
Entire cohort with AF
(main analysis)
Apixaban 1.01 (0.51-2.01) 0.35 (0.17-0.72) 0.47 (029-0.76)
Dabigatran 0.81 (0.49-1.34) 0.48 (0.30-0.77) 0.59 (0.43-0.81)
Rivaroxaban 1.46 (0.79-2.70) 0.84 (0.49-1.44) 0.52 (0.34-0.79)
Cohort hospitalized with AF
(sensitivity analysis)
Apixaban 1.06 (0.51-2.19) 0.46 (0.22-0.97) 0.58 (0.33-1.02)
Dabigatran 0.69 (0.39-1.23) 0.46 (0.27-0.77) 0.69 (0.47-1.02)
Rivaroxaban 1.27 (0.64-2.52) 0.72 (0.38-1.37) 0.62 (0.36-1.08)
Low mortality cohort
(sensitivity analysis)
Apixaban 1.39 (0.65-2.95) 0.31 (0.12-0.78) 0.74 (0.39-1.43)
Dabigatran 1.03 (0.59-1.80) 0.44 (0.25-0.77) 0.92 (0.58-1.47)
Rivaroxaban 1.28 (0.61-2.68) 0.72 (0.37-1.37) 0.39 (0.17-0.91)
Age >65 y (supplementary analysis)
Apixaban 0.89 (0.37-2.13) 0.41 (0.17-0.96) 0.56 (0.33-0.96)
Dabigatran 0.96 (0.53-1.76) 0.55 (0.31-0.99) 0.59 (0.40-0.86)
Rivaroxaban 1.07 (0.49-2.23) 0.76 (0.41-1.42) 0.69 (0.44-1.08)
Hypertension
(supplementary analysis)
Apixaban 1.46 (0.47-4.54) 0.47 (0.11-2.02) 0.45 (0.14-1.42)
Dabigatran 0.83 (0.31-2.23) 0.47 (0.19-1.16) 0.49 (0.24-1.04)
Rivaroxaban 1.50 (0.41-5.46) 0.79 (0.23-2.65) 0.11 (0.01-0.82)
Men (supplementary analysis)
Apixaban 0.96 (0.39-2.36) 0.44 (0.19-0.98) 0.56 (0.31-1.01)
Dabigatran 0.90 (0.49-1.66) 0.50 (0.29-0.86) 0.61 (0.42-0.90)
Rivaroxaban 1.01 (0.43-2.37) 0.95 (0.53-1.71) 0.67 (0.40-1.12)
Women (supplementary analysis)
Apixaban 1.20 (0.40-3.59) 0.14 (0.02-1.04) 0.29 (0.13-0.68)
Dabigatran 0.72 (0.28-1.84) 0.46 (0.19-1.12) 0.57 (0.32-1.02)
Rivaroxaban 2.17 (0.89-5.31) 0.29 (0.07-1.25) 0.34 (0.16-0.75)
0.2 1.0 6.0 0.01 0.1 1.0 3.0 0.01 0.1 1.0 3.0
Ischemic Stroke/SE Any Bleeding Death
HR (95% CI) HR (95% CI) HR (95% CI)
The corresponding results for a follow-up of 2.5 years are provided in eFigure 8. AF indicates atrial fibrillation; SE, systemic embolism.
these end points did not falsify, indicating residual confound- observed. The number of events and the event rates for the sen-
ing. Survival analyses are first described below. sitivity analyses on the configuration of the study cohorts are
For the principal effectiveness end point of ischemic stroke/ provided in Table 3.
systemic embolism, 103 events (80.5% as primary diagnoses)
were observed within the first year, representing a rate be- All-Cause Mortality
tween 0.65 and 1.20 per 100 person-years among the IPTW There was an apparent significant lower risk of all-cause mor-
population. The estimated effect sizes in terms of hazard ra- tality, death, across all treatment groups compared with war-
tios (HR) of the NOACs ranged between 0.81 (95% CI, 0.49- farin, although effect sizes shifted toward unity and became
1.34) and 1.46 (0.79-2.70), with all treatment groups display- nonsignificant when restricted to patients who were hospi-
ing statistically nonsignificant differences compared with talized with AF (Figure 1).
warfarin (Figure 1). The primary effectiveness outcome was al- When restricting the study population to patients with-
most exclusively composed of ischemic stroke, and only 3 out conditions associated with increased mortality (ie, exclud-
events were systemic embolism (data not shown). ing patients with heart failure, chronic pulmonary disease, or
In sensitivity analyses restricted to patients with a his- cancer), all effect estimates were lower for NOAC agents com-
tory of AF discharge codes or to the cohort with a low mortal- pared with warfarin, while only treatment with rivaroxaban
ity for the composite end point of ischemic stroke/systemic em- reached a statistically significant lower death rate (HR, 0.39;
bolism at 1 year, the findings from the main analysis were 95% CI, 0.17-0.91).
generally in agreement, and no statistically significant differ- Excluding approximately 3084 patients (22%) with a
ences between NOAC agents compared with warfarin were conjectured high mortality risk resulted in a pronounced
jamacardiology.com (Reprinted) JAMA Cardiology Published online June 14, 2017 E5
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/cardiology/0/ by Silverchair University, Roberto Lopez Mata on 06/15/2017
Research Original Investigation Effectiveness and Safety of Standard-Dose Nonvitamin K Antagonist Oral Anticoagulants and Warfarin
Table 3. Number of Events and Crude and Weighted Event Rates at 1-Year Follow-up According to Treatment for Main End Points
and Selected Study Cohortsa
Apixaban Dabigatran Rivaroxaban Warfarin
Rate Rate Rate Rate
End
Point/Cohort Events Crude Weighted Events Crude Weighted Events Crude Weighted Events Crude Weighted
Ischemic Stroke/SE
Main analysis 10 0.86 0.83 22 0.70 0.65 14 1.09 1.20 57 0.79 0.81
cohort
Cohort 9 1.01 1.07 17 0.69 0.66 11 1.25 1.29 41 0.94 0.96
hospitalized
with AF
Low mortality 9 1.00 1.00 19 0.75 0.79 10 0.97 0.92 38 0.68 0.70
cohort
All-Cause Death
Main analysis 19 1.62 1.52 51 1.62 1.84 26 2.01 1.67 249 3.45 3.11
cohort
Cohort 14 1.56 1.40 36 1.46 1.60 15 1.69 1.50 107 2.44 2.33
hospitalized
with AF
Low mortality 11 1.21 0.96 26 1.02 1.14 6 0.58 0.50 69 1.24 1.24
cohort
Any Bleeding
Main analysis 8 0.68 0.57 23 0.74 0.73 17 1.33 1.38 109 1.52 1.53
cohort
Cohort 8 0.90 0.79 18 0.74 0.72 12 1.36 1.24 69 1.58 1.59
hospitalized
with AF
Low mortality 5 0.55 0.44 15 0.59 0.58 11 1.06 1.02 70 1.26 1.32
cohort
Abbreviations: AF, atrial fibrillation; IPTW, inverse probability of treatment weighed; SE, systemic embolism.
a
Crude rates are events divided by person time per 100 years; weighted rates are based on IPTW population and express population mean treatment rates per 100
years.
reduction in the absolute number of deaths (from 345 to 112) with NOACs (ie, no more than 6 events in each treatment group)
across treatment groups (eFigure 1 in the Supplement). The re- (Table 2). Fifty five bleeding events (35%) were observed. When
sults of the supplementary analyses generally align with the compared with warfarin, each NOAC exhibited a lower rela-
main analysis, but should be interpreted with caution in light tive risk of intracranial bleeding with estimates (ie, HRs) rang-
of the sensitivity analysis on the group with low mortality rates. ing from 0.11 (95% CI, 0.01-0.78) to 0.53 (95% CI, 0.15-1.87).
The low event numbers resulted in wide confidence inter-
Bleeding Events vals, which preclude any statistically significant conclusions.
A total of 157 events (90% primary diagnoses) of the com- Results for a follow-up of 2.5 years (eFigure 8 in the Supple-
bined end point of any bleeding were observed during the ment) aligned with these results, as did the trimmed IPTW
first year of follow-up. The weighted event rates ranged be- analyses when compared with the adjusted Cox regression on
tween 0.57 (apixaban) to 1.53 (warfarin). the unweighted population (data not shown).
When compared with warfarin, apixaban and dabigatran
were associated with lower bleeding events (HR, 0.35; 95% CI, Falsification Analysis
0.17-0.72; and HR, 0.48; 95% CI, 0.30-0.77, respectively) For the falsification outcomes analyses on the associated treat-
(Figure 1). This was statistically nonsignificant for the ment-exposure relationship, the a priori null-hypothesis of
comparison of rivaroxaban vs warfarin (HR, 0.84; 95% CI, neutral associations was generally rejected, indicating a pos-
0.49-1.44). sible persistent bias. In the subgroup analysis of the cohort hos-
In sensitivity analyses restricted to patients with AF with pitalized with AF and the cohort with low mortality rates, the
an AF hospital discharge code or to the cohort with low mor- associations between exposure and studied falsification out-
tality rates, the rates were overall lower in the latter cohort, comes were neutral, indicating a low likelihood of persistent
although altogether the direction of associations from the bias (Figure 2, eFigure 8, and eTable 9 in the Supplement).
main analysis was generally maintained. For the supplemen-
tary subgroup analyses, the smaller sample sizes led to more
uncertain effect estimates, although they were aligned with
the main analyses (eTables 3-8 and eFigures 6 and 7 in the
Discussion
Supplement). In this study of patients with AF with 1 nonsex-related
After analyzing the outcomes of intracranial (including CHA2DS2-VASc risk factor, our principal findings were as fol-
traumatically induced) bleeding and gastrointestinal bleed- lows: (1) for ischemic stroke/systemic embolism, no signifi-
ing, few events were observed among the populations treated cant differences of the NOACs compared with warfarin were
E6 JAMA Cardiology Published online June 14, 2017 (Reprinted) jamacardiology.com
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/cardiology/0/ by Silverchair University, Roberto Lopez Mata on 06/15/2017
Effectiveness and Safety of Standard-Dose Nonvitamin K Antagonist Oral Anticoagulants and Warfarin Original Investigation Research
Figure 2. Inverse Probability of Treatment Weighted Cox Hazard Ratios for 1-Year Follow-up for Nonvitamin K Antagonist Oral Anticoagulants
Compared With Warfarin for Falsification Analysis
Cancer Favors Favors Hip Fractures Favors Favors
Strata/Treatment HR (95% CI) Alternative Warfarin Strata/Treatment HR (95% CI) Alternative Warfarin
Entire AF cohort (main analysis) Entire AF cohort (main analysis)
Apixaban 0.67 (0.480.93) Apixaban 0.64 (0.401.02)
Dabigatran 0.66 (0.53-0.82) Dabigatran 0.69 (0.510.93)
Rivaroxaban 0.68 (0.510.90) Rivaroxaban 0.67 (0.451.00)
AF hospitalized cohort (sensitivity analysis) AF hospitalized cohort (sensitivity analysis)
Apixaban 0.73 (0.501.05) Apixaban 0.69 (0.411.17)
Dabigatran 0.72 (0.550.93) Dabigatran 0.75 (0.521.08)
Rivaroxaban 0.73 (0.511.05) Rivaroxaban 0.71 (0.421.20)
Low mortality cohort (sensitivity analysis) Low mortality cohort (sensitivity analysis)
Apixaban 0.76 (0.481.21) Apixaban 0.75 (0.401.40)
Dabigatran 0.72 (0.511.00) Dabigatran 1.02 (0.661.57)
Rivaroxaban 0.74 (0.471.17) Rivaroxaban 0.51 (0.241.08)
0.1 1.0 10 0.1 1.0 10
Cancer HR (95% CI) Hip Fractures HR (95% CI)
Urinary Tract
Pneumonia Favors Favors Infection Favors Favors
Strata/Treatment HR (95% CI) Alternative Warfarin Strata/Treatment HR (95% CI) Alternative Warfarin
Entire AF cohort (main analysis) Entire AF cohort (main analysis)
Apixaban 0.94 (0.701.27) Apixaban 0.64 (0.411.00)
Dabigatran 0.69 (0.550.87) Dabigatran 0.73 (0.560.96)
Rivaroxaban 0.63 (0.470.86) Rivaroxaban 0.71 (0.501.03)
AF hospitalized cohort (sensitivity analysis) AF hospitalized cohort (sensitivity analysis)
Apixaban 0.93 (0.671.29) Apixaban 0.63 (0.381.04)
Dabigatran 0.74 (0.570.96) Dabigatran 0.83 (0.601.16)
Rivaroxaban 0.79 (0.551.14) Rivaroxaban 0.86 (0.551.36)
Low mortality cohort (sensitivity analysis) Low mortality cohort (sensitivity analysis)
Apixaban 1.11 (0.751.63) Apixaban 0.85 (0.481.51)
Dabigatran 0.93 (0.681.27) Dabigatran 1.01 (0.691.48)
Rivaroxaban 0.53 (0.320.88) Rivaroxaban 0.68 (0.381.22)
0.1 1.0 10 0.1 1.0 10
Pneumonia HR (95% CI) Urinary Tract Infection HR (95% CI)
AF indicates atrial fibrillation.
evident; (2) death was significantly lower for all 3 NOACs com- edoxaban, compared with warfarin) can benefit from obser-
pared with warfarin, but this appears mainly driven by intrin- vational cohort studies. As mentioned, the lack of clinical trial
sic selective prescription patterns that warrant cautious inter- data has led to some guidelines that express a preference
pretation; and (3) any bleeding was significantly lower for for treatment with dabigatran or apixaban for patients with 1
apixaban and dabigatran compared with warfarin and showed stroke risk factor, with the other NOACs or warfarin as
nonsignificant differences between rivaroxaban and warfa- alternatives.20,21 However, the current analysis cannot firmly
rin. Nonetheless, the falsification end points generally did not support these preferences, and prescribing physicians are also
falsify, indicating some residual confounding across these com- encouraged to evaluate each patient with AF individually to
parisons that was presumably related to selective prescribing select the preferred agent.22
and unobserved comorbidities. Many guidelines have expressed a preference for NOACs
In patients with a CHADS2 score of 0 to 1, ancillary analy- over warfarin for treating patients with AF with 1 or more stroke
ses from the RELY, ARISTOTLE, and AVERROES clinical trials risk factors. The current threshold for OAC for stroke preven-
show that there was no significant interaction for the efficacy tion has been quoted as a stroke rate of 1.7%year for warfarin,
and safety data on NOACs (ie, dabigatran or apixaban) com- and 0.9%/year for an NOAC, reflecting the change in tipping
pared with warfarin or aspirin.15-17 However, the randomized point for treatment with the availability of NOACs.23 Even this
clinical trials for rivaroxaban (ROCKET-AF) or edoxaban treatment threshold of 1.7%/year with warfarin could be low-
(ENGAGE-AF) did not include patients with 1 stroke risk fac- ered with good-quality anticoagulation control with a time in
tor; for example, the inclusion criteria for ROCKET-AF was con- therapeutic range of more than 70%.24 Given the lack of spe-
fined to patients with a CHADS2 score of 2 or more or having cific randomized clinical trial data in an exclusive patient popu-
experienced a prior stroke, and even those with a CHADS2 score lation with 1 stroke risk factor, guidelines have suggested that
of 2 were capped at 10%.18,19 Hence, the relative effective- OACs should be considered (grade IIa recommendation) for
ness and safety of these 2 NOAC agents (ie, rivaroxaban or those with 1 risk factor (CHA2DS2-VASc score of 1 in men or 2
jamacardiology.com (Reprinted) JAMA Cardiology Published online June 14, 2017 E7
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/cardiology/0/ by Silverchair University, Roberto Lopez Mata on 06/15/2017
Research Original Investigation Effectiveness and Safety of Standard-Dose Nonvitamin K Antagonist Oral Anticoagulants and Warfarin
in women) whereas OACs are recommended (grade I recom- effectiveness or safety outcomes were generally maintained.
mendation) for patients with 2 or more stroke risk factors.25 While these (sensitivity) analyses do not guarantee that our
Nevertheless, there has been controversy regarding the ac- analyses are completely unbiased, it does provide some reas-
tual stroke event rates with 1 stroke risk factor, given the likely surance and indicates that the observed associations may be
differences of risk associated with different risk factors. Also, true associations.
different study settings (eg, hospitalized vs community), races/ Concisely, observational studies are inherently subject to
ethnicities (Asian vs non-Asian) and methods of analyses may confounding and may lead to biased estimates. However, we
be relevant factors.26,27 Indeed, some studies28,29 putatively systematically and analytically investigated confounding and
reporting low event rates excluded patients who ever took biases in sensitivity analyses and falsification outcomes, and
OACs, hence conditioning analyses on the future, and artifi- in general, our approaches pointed toward causal associa-
cially biasing results toward low event rates.26 Even 1 stroke tions between treatment exposure and effectiveness and safety
risk factor has a positive net clinical benefit for OAC treat- outcomes.
ment compared with aspirin or no treatment.30 Also, stroke risk The main analysis of the end point of any bleeding in-
among patients with AF not a static phenomenon, and clini- dicated that it was significantly lower for apixaban and dabi-
cal scores like the CHA2DS2-VASc scores are reductionist and gatran compared with warfarin but was nonsignificant for the
a simplification.27 comparison of rivaroxaban vs warfarin. Again, this is broadly
The observation on the lower risk of death among pa- consistent with prior analyses.33-35 Ancillary analyses of ran-
tients who received NOAC treatment compared with warfa- domized clinical trial cohorts for the minority of patients with
rin requires attention. This difference in conclusion is likely a CHADS2 score of 0 to 1 show consistency between the effect
because of selective prescribing by physicians; these analy- sizes of NOAC vs warfarin and the main trial observations.15-17
ses could suggest that rivaroxaban may be preferred for frailer There was broad consistency across most subgroups in our sen-
patients compared with the other treatment alternatives. sitivity analyses and whether 1- or 2.5-year follow-up periods
Causes of death available in real-world data analyses are in gen- were analyzed.
eral not adjudicated and either cerebral imaging or post mor-
tems are not mandated. It is evident that some deaths could Limitations
be because of fatal strokes, as there is an increased risk of stroke The main limitation of this study relates to the observational
in AF. Nonetheless, both stroke and death has been shown to nature of the data, and residual or unmeasured confounding
be significantly reduced by treatment with warfarin vs probably persists. A propensity weighing approach to ac-
placebos/controls.31 For mortality rates, there is even an added count for baseline differences were used; however, the full ex-
10% reduction with treatment with NOACs over warfarin.32 tent and effect of different prescribing behavior may not be fully
Our falsification end points generally did not falsify, indi- captured and may have caused biased effect estimates. In-
cating the presence of residual confounding across these com- deed, because we investigated rare outcomes, even a few er-
parisons. Indeed, there are multiple considerations that indi- roneously coded outcomes could shift the direction of asso-
cate confounding. For example, there are important variables ciations. Nevertheless, the outcomes ascertained have been
that are known to influence treatment selection that are not previously validated with a high-positive predictive value (eg,
present in the data set, such as body mass index (calculated 97%-100% for ischemic stroke).36
as weight in kilograms divided by height in meters squared), The presented sensitivity analysis on the cohort with low
actual blood pressures, heart rate, smoking status, estimated mortality rates suggests selective prescribing and warrants cau-
glomerular filtration rate, hematocrit, New York Heart Asso- tion on the conclusions drawn on mortality rates. Indeed, end
ciation class, left ventricle ejection fraction, and type of AF. points were not adjudicated (unlike among a clinical trial co-
For the results to be totally unconfounded, these factors would hort) and postmortems were not mandated, which leaves the
need to be unrelated to the treatment assignment. Successful possibility that some deaths could be because of fatal strokes
falsification does not prove a lack of confounding, as the uncertain. Information on the time in therapeutic range among
sources of confounding may be different for different out- people treated with warfarin was not available, nor did we have
comes. However, the failure to falsify (as in our study) raises detailed information on laboratory (eg, serum creatinine), an-
the likelihood that unmeasured confounders exist, and may thropometric, or socioeconomic data. Thus, our confounder
well be relevant to our outcomes of interest and, perhaps add adjustment was partially determined by the information avail-
bias toward NOACs. able in the registries. Patient adherence to the NOACs and pre-
Indeed, our analyses indicate that some selective prescrib- scribing practices was not considered, but may be a potential
ing may contribute to an important bias of the rates, and cau- driver of the differences between drugs, and differences in a
tion concerning conclusions on effects associated with death patients medical experience may influence his or her adher-
is warranted. Indeed, the analyses on falsification outcomes ence to treatment. Our data apply to a predominantly white
could not provide a reassurance of unbiased estimates, rec- European population, and differential efficacy and safety ben-
ognizing the findings of positive associations in the 4 investi- efits may be evident among Asian and non-Asian people.37,38
gations of false outcomes. However, when investigating fal- Indeed, these limitations could nullify the possible benefits of
sified outcomes among the cohort with low mortality rates, we NOACs, notwithstanding that our data show that at the very
observed neutral associations when contrasting exposure minimum, the NOACs have a similar effectiveness to warfa-
groups, while the associations on treatment exposure and rin with trends toward a better safety profile.
E8 JAMA Cardiology Published online June 14, 2017 (Reprinted) jamacardiology.com
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/cardiology/0/ by Silverchair University, Roberto Lopez Mata on 06/15/2017
Effectiveness and Safety of Standard-Dose Nonvitamin K Antagonist Oral Anticoagulants and Warfarin Original Investigation Research
experiencing an ischemic stroke/systemic embolism. For any
Conclusions bleeding, this was lower for apixaban and dabigatran com-
pared with warfarin. These data do not allow for a definitive
In this Danish observational cohort study of patients with AF statement regarding the comparative effectiveness or safety
and a single stroke risk factor, there was no difference be- of NOACs because of possible residual confounding un-
tween NOACs compared with warfarin in the risk of patients masked with falsification outcomes.
ARTICLE INFORMATION 5. Pedersen CB. The Danish Civil Registration score: a subgroup analysis of the RE-LY trial. Ann
Accepted for Publication: April 28, 2017. System. Scand J Public Health. 2011;39(7)(suppl): Intern Med. 2011;155(10):660-667.
22-25. 18. Patel MR, Mahaffey KW, Garg J, et al; ROCKET
Published Online: June 14, 2017.
doi:10.1001/jamacardio.2017.1883 6. Shrank WH, Patrick AR, Brookhart MA. Healthy AF Investigators. Rivaroxaban versus warfarin in
user and related biases in observational studies of nonvalvular atrial fibrillation. N Engl J Med. 2011;
Author Contributions: Drs Lip and Skjth had full preventive interventions: a primer for physicians. 365(10):883-891.
access to all of the data in this study and take J Gen Intern Med. 2011;26(5):546-550.
responsibility for the integrity of the data and the 19. Giugliano RP, Ruff CT, Braunwald E, et al;
accuracy of the data analysis. 7. Larsen TB, Gorst-Rasmussen A, Rasmussen LH, ENGAGE AF-TIMI 48 Investigators. Edoxaban
Concept and design: Lip, Skjth, Nielsen, Larsen. Skjth F, Rosenzweig M, Lip GYH. Bleeding events versus warfarin in patients with atrial fibrillation.
Acquisition, analysis, or interpretation of data: All among new starters and switchers to dabigatran N Engl J Med. 2013;369(22):2093-2104.
authors. compared with warfarin in atrial fibrillation. Am J Med. 20. Ogawa S, Aonuma K, Tse H-F, et al. The
Drafting of the manuscript: Lip, Skjth, Nielsen. 2014;127(7):650-656.e5. APHRSs 2013 statement on antithrombotic therapy
Critical revision of the manuscript for important 8. Holster IL, Valkhoff VE, Kuipers EJ, Tjwa ETTL. of patients with nonvalvular atrial fibrillation.
intellectual content: All authors. New oral anticoagulants increase risk for J Arrhythmia. 2013;29(3):190-200. doi:10.1016/j.joa
Statistical analysis: Skjth, Nielsen. gastrointestinal bleeding: a systematic review and .2013.03.002
Obtained funding: Lip, Larsen. meta-analysis. Gastroenterology. 2013;145(1): 21. JCS Joint Working Group. Guidelines for
Administrative, technical, or material support: Lip, 105-112.e15. pharmacotherapy of atrial fibrillation (JCS 2013).
Nielsen, Kjaeldgaard, Larsen. 9. Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Circ J. 2014;78(8):1997-2021.
Supervision: Lip, Larsen. Crijns HJGM, Lip GYH. A novel user-friendly score 22. Shields AM, Lip GYH. Choosing the right drug to
Conflict of Interest Disclosures: All authors have (HAS-BLED) to assess 1-year risk of major bleeding fit the patient when selecting oral anticoagulation
completed and submitted the ICMJE Form for in patients with atrial fibrillation: the Euro Heart for stroke prevention in atrial fibrillation. J Intern Med.
Disclosure of Potential Conflicts of Interest. Dr Lip Survey. Chest. 2010;138(5):1093-1100. 2015;278(1):1-18.
has received consulting fees from Bayer/Janssen, 10. Schmidt M, Schmidt SA, Sandegaard JLJ,
BMS/Pfizer, Biotronik, Medtronic, Boehringer 23. Eckman MH, Singer DE, Rosand J, Greenberg
Ehrenstein V, Pedersen L, Srensen HT. The Danish SM. Moving the tipping point: the decision to
Ingelheim, Microlife and Daiichi-Sankyo. Speaker for National Patient Registry: a review of content, data
Bayer, BMS/Pfizer, Medtronic, Boehringer anticoagulate patients with atrial fibrillation. Circ
quality, and research potential. Clin Epidemiol. Cardiovasc Qual Outcomes. 2011;4(1):14-21.
Ingelheim, Microlife, Roche, and Daiichi-Sankyo. Dr 2015;7:449-490.
Larsen has served as an investigator for Janssen 24. Proietti M, Lip GYH. Major outcomes in atrial
Scientific Affairs, LLC, and Boehringer Ingelheim 11. Robins JM, Hernn MA, Brumback B. Marginal fibrillation patients with one risk factor: impact of
and received speaking fees from Bayer, BMS/Pfizer, structural models and causal inference in time in therapeutic range observations from the
Boehringer Ingelheim, MSD, and AstraZeneca. Mr epidemiology. Epidemiology. 2000;11(5):550-560. SPORTIF trials. Am J Med. 2016;129(10):1110-1116.
Nielsen has received speaking fees from Boehringer 12. Strmer T, Wyss R, Glynn RJ, Brookhart MA. 25. Kirchhof P, Benussi S, Kotecha D, et al. 2016
Ingelheim, consulting fees from Bayer; and grant Propensity scores for confounder adjustment when ESC guidelines for the management of atrial
support from BMS/Pfizer. Dr Skjth has received assessing the effects of medical interventions using fibrillation developed in collaboration with EACTS.
consulting feed from Bayer. No other disclosures nonexperimental study designs. J Intern Med. Eur Heart J. 2016;37(38):2893-2962.
are reported. 2014;275(6):570-580.
26. Nielsen PB, Larsen TB, Skjth F, Overvad TF,
Funding/Support: The Obel Family Foundation 13. Austin PC. Some methods of propensity-score Lip GYH. Stroke and thromboembolic event rates in
partially funded this research through an matching had superior performance to others: atrial fibrillation according to different guideline
unrestricted grant. The Danish Health Data results of an empirical investigation and Monte treatment thresholds: a nationwide cohort study.
Authority provided the data material. Carlo simulations. Biom J. 2009;51(1):171-184. Sci Rep. 2016;6:27410.
Role of the Funder/Sponsor: The Obel Family 14. Lipsitch M, Tchetgen Tchetgen E, Cohen T. 27. Lip GYH, Nielsen PB. Should patients with atrial
Foundation had no role in the design and conduct Negative controls: a tool for detecting confounding fibrillation and 1 stroke risk factor (CHA2DS2-VASc
of the study; collection, management, analysis, and and bias in observational studies. Epidemiology. score 1 in men, 2 in women) be anticoagulated? yes:
interpretation of the data; and preparation, review, 2010;21(3):383-388. even 1 stroke risk factor confers a real risk of stroke.
or approval of the manuscript. 15. Lopes RD, Al-Khatib SM, Wallentin L, et al. Circulation. 2016;133(15):1498-1503.
Efficacy and safety of apixaban compared with 28. Friberg L, Skeppholm M, Ternt A. Benefit of
REFERENCES warfarin according to patient risk of stroke and of anticoagulation unlikely in patients with atrial
1. Connolly SJ, Ezekowitz MD, Yusuf S, et al; RE-LY bleeding in atrial fibrillation: a secondary analysis of fibrillation and a CHA2DS2-VASc score of 1. J Am
Steering Committee and Investigators. Dabigatran a randomised controlled trial. Lancet. 2012;380 Coll Cardiol. 2015;65(3):225-232.
versus warfarin in patients with atrial fibrillation. (9855):1749-1758.
N Engl J Med. 2009;361(12):1139-1151. 29. Aspberg S, Chang Y, Atterman A, Bottai M, Go
16. Lip GYH, Connolly S, Yusuf S, et al; ERROES AS, Singer DE. Comparison of the ATRIA, CHADS2,
2. Connolly SJ, Eikelboom J, Joyner C, et al; Investigators. Modification of outcomes with and CHA2DS2-VASc stroke risk scores in predicting
AVERROES Steering Committee and Investigators. aspirin or apixaban in relation to CHADS(2) and ischaemic stroke in a large Swedish cohort of
Apixaban in patients with atrial fibrillation. N Engl J CHA(2)DS(2)-VASc scores in patients with atrial patients with atrial fibrillation. Eur Heart J. 2016;37
Med. 2011;364(9):806-817. fibrillation: a secondary analysis of the AVERROES (42):3203-3210.
3. Kildemoes HW, Srensen HT, Hallas J. The study. Circ Arrhythm Electrophysiol. 2013;6(1):31-38.
30. Lip GYH, Skjth F, Rasmussen LH, Nielsen PB,
Danish National Prescription Registry. Scand J Public 17. Oldgren J, Alings M, Darius H, et al; RE-LY Larsen TB. Net clinical benefit for oral
Health. 2011;39(7)(suppl):38-41. Investigators. Risks for stroke, bleeding, and death anticoagulation, aspirin, or no therapy in
4. Lynge E, Sandegaard JL, Rebolj M. The Danish in patients with atrial fibrillation receiving nonvalvular atrial fibrillation patients with 1
National Patient Register. Scand J Public Health. dabigatran or warfarin in relation to the CHADS2 additional risk factor of the CHA2DS2-VASc score
2011;39(7)(suppl):30-33. (beyond sex). J Am Coll Cardiol. 2015;66(4):488-490.
jamacardiology.com (Reprinted) JAMA Cardiology Published online June 14, 2017 E9
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/cardiology/0/ by Silverchair University, Roberto Lopez Mata on 06/15/2017
Research Original Investigation Effectiveness and Safety of Standard-Dose Nonvitamin K Antagonist Oral Anticoagulants and Warfarin
31. Hart RG, Pearce LA, Aguilar MI. Meta-analysis: propensity weighted nationwide cohort study. BMJ. 36. Krarup L-H, Boysen G, Janjua H, Prescott E,
antithrombotic therapy to prevent stroke in 2016;353:i3189. Truelsen T. Validity of stroke diagnoses in a national
patients who have nonvalvular atrial fibrillation. 34. Lip GYH, Keshishian A, Kamble S, et al. register of patients. Neuroepidemiology. 2007;28
Ann Intern Med. 2007;146(12):857-867. Real-world comparison of major bleeding risk (3):150-154.
32. Ruff CT, Giugliano RP, Braunwald E, et al. among non-valvular atrial fibrillation patients 37. Wang K-L, Lip GYH, Lin S-J, Chiang C-E,
Comparison of the efficacy and safety of new oral initiated on apixaban, dabigatran, rivaroxaban, or NonVitamin K. Non-vitamin k antagonist oral
anticoagulants with warfarin in patients with atrial warfarin. a propensity score matched analysis. anticoagulants for stroke prevention in Asian
fibrillation: a meta-analysis of randomised trials. Thromb Haemost. 2016;116(5):975-986. patients with nonvalvular atrial fibrillation:
Lancet. 2014;383(9921):955-962. 35. Lozano-Velasco E, Hernndez-Torres F, Daimi meta-analysis. Stroke. 2015;46(9):2555-2561.
33. Larsen TB, Skjth F, Nielsen PB, Kjldgaard JN, H, et al. Pitx2 impairs calcium handling in a 38. Chiang C-E, Wang K-L, Lip GYH. Stroke
Lip GYH. Comparative effectiveness and safety of dose-dependent manner by modulating Wnt prevention in atrial fibrillation: an Asian
non-vitamin K antagonist oral anticoagulants and signalling. Cardiovasc Res. 2016;109(1):55-66. perspective. Thromb Haemost. 2014;111(5):789-797.
warfarin in patients with atrial fibrillation:
E10 JAMA Cardiology Published online June 14, 2017 (Reprinted) jamacardiology.com
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/cardiology/0/ by Silverchair University, Roberto Lopez Mata on 06/15/2017
S-ar putea să vă placă și
- Border Collie Training GuidelinesDocument12 paginiBorder Collie Training GuidelinespsmanasseÎncă nu există evaluări
- Chemical Engineering Projects List For Final YearDocument2 paginiChemical Engineering Projects List For Final YearRajnikant Tiwari67% (6)
- Effectiveness and Safety of Dabigatran, Rivaroxaban, and Apixaban Versus Warfarin in Nonvalvular Atrial FibrillationDocument18 paginiEffectiveness and Safety of Dabigatran, Rivaroxaban, and Apixaban Versus Warfarin in Nonvalvular Atrial FibrillationgaryÎncă nu există evaluări
- Graham The American Journal of MedicineDocument21 paginiGraham The American Journal of MedicinemadrugagalanfÎncă nu există evaluări
- Comparison of Dabigatran Versus Warfarin TreatmentDocument7 paginiComparison of Dabigatran Versus Warfarin TreatmentDivyesh AmarsedaÎncă nu există evaluări
- Ecr 12 1 40Document6 paginiEcr 12 1 40Ahmed MohammedÎncă nu există evaluări
- Effectiveness and Safety of Dabigatran, Rivaroxaban, and Apixaban Versus Warfarin in Nonvalvular Atrial FibrillationDocument18 paginiEffectiveness and Safety of Dabigatran, Rivaroxaban, and Apixaban Versus Warfarin in Nonvalvular Atrial FibrillationJUAN SEBASTIAN CLAVIJO CASTELLANOSÎncă nu există evaluări
- Jeong DKK, 2019Document8 paginiJeong DKK, 2019sri noviyanty yusufÎncă nu există evaluări
- Apixaban For Patients With Atrial Fibrillation On Hemodialysis: A Multicenter Randomized Controlled TrialDocument11 paginiApixaban For Patients With Atrial Fibrillation On Hemodialysis: A Multicenter Randomized Controlled TrialMedicina UPBÎncă nu există evaluări
- Ischemic Stroke and Intracranial Hemorrhage With Aspirin, Dabigatran, and WarfarinDocument9 paginiIschemic Stroke and Intracranial Hemorrhage With Aspirin, Dabigatran, and WarfarinNur Syamsiah MÎncă nu există evaluări
- Editorial Caravaggio Apixaban en Cáncer y ETVDocument3 paginiEditorial Caravaggio Apixaban en Cáncer y ETVSANTIAGO FOREROÎncă nu există evaluări
- 345 FullDocument8 pagini345 FullwisgeorgekwokÎncă nu există evaluări
- PIONEERstudy 2016Document12 paginiPIONEERstudy 2016Jose Enrique Valecillos MorenoÎncă nu există evaluări
- Rivaroxaban Vs Warfarin Sodium in The Ultra-Early Period After Atrial Fibrillation-Related Mild Ischemic StrokeDocument10 paginiRivaroxaban Vs Warfarin Sodium in The Ultra-Early Period After Atrial Fibrillation-Related Mild Ischemic StrokeRoberto López MataÎncă nu există evaluări
- Review of Clinical Studies On Angiotensin II Receptor Blockers and Risk of CancerDocument6 paginiReview of Clinical Studies On Angiotensin II Receptor Blockers and Risk of CancerRisa MuthmainahÎncă nu există evaluări
- 28720644: Effects of Non-Vitamin K Antagonist Oral Anticoagulants Versus Warfarin in Patients With Atrial Fibrillation and Valvular Heart Disease A Systematic Review and Meta-AnalysisDocument12 pagini28720644: Effects of Non-Vitamin K Antagonist Oral Anticoagulants Versus Warfarin in Patients With Atrial Fibrillation and Valvular Heart Disease A Systematic Review and Meta-AnalysisaleksÎncă nu există evaluări
- Selective Serotonin Reuptake Inhibitors and Bleeding Risk in Anticoagulated Patients With Atrial FibrillationDocument9 paginiSelective Serotonin Reuptake Inhibitors and Bleeding Risk in Anticoagulated Patients With Atrial FibrillationGiancarlos GuzmanÎncă nu există evaluări
- Rivaroxaban Versus Apixaban For Stroke Prevention in Atrial FibrillationDocument10 paginiRivaroxaban Versus Apixaban For Stroke Prevention in Atrial FibrillationRicardo BarcoÎncă nu există evaluări
- Rivaroxavan en Fa ValvularDocument5 paginiRivaroxavan en Fa Valvularcarlos pardoÎncă nu există evaluări
- Anticoagulantes Orales e Infarto Agudo Miocardio 2018 Carta EditorialDocument2 paginiAnticoagulantes Orales e Infarto Agudo Miocardio 2018 Carta EditorialRenzo RosalesÎncă nu există evaluări
- Rivaroxaban Versus Dabigatran or Warfarin in Real-World Studies of Stroke Prevention in Atrial FibrillationDocument21 paginiRivaroxaban Versus Dabigatran or Warfarin in Real-World Studies of Stroke Prevention in Atrial FibrillationMerDeKÎncă nu există evaluări
- Re LyDocument13 paginiRe LyDilawar JanÎncă nu există evaluări
- 361 2012 LaHayeDocument9 pagini361 2012 LaHayeOscar PonceÎncă nu există evaluări
- Aer 04 100Document8 paginiAer 04 100I Al WÎncă nu există evaluări
- 2020 Asociación Entre El Uso de Warfarina para La Fibrilación Auricular y Los Resultados Entre Pacientes Con Enfermedad Renal en Etapa TerminalDocument13 pagini2020 Asociación Entre El Uso de Warfarina para La Fibrilación Auricular y Los Resultados Entre Pacientes Con Enfermedad Renal en Etapa TerminalbernardoÎncă nu există evaluări
- Assessing The Risk of Bleeding in Patients With Atrial FibrillationDocument8 paginiAssessing The Risk of Bleeding in Patients With Atrial FibrillationAngga Aryo LukmantoÎncă nu există evaluări
- Enoxaparin Versus Unfractionated Heparin in Elective Percutaneous Coronary InterventionDocument12 paginiEnoxaparin Versus Unfractionated Heparin in Elective Percutaneous Coronary InterventionMuhammad FarisÎncă nu există evaluări
- Effect of Rivaroxaban Vs Enoxaparin On Major Cardiac Adverse Events and Bleeding Risk in The Acute Phase of Acute Coronary Syndrome PDFDocument13 paginiEffect of Rivaroxaban Vs Enoxaparin On Major Cardiac Adverse Events and Bleeding Risk in The Acute Phase of Acute Coronary Syndrome PDFKardiologi ManadoÎncă nu există evaluări
- Riva Rox AbanDocument11 paginiRiva Rox AbanMr. LÎncă nu există evaluări
- Doacs in Patients With Mitral Stenosis and Atrial FibrillationDocument3 paginiDoacs in Patients With Mitral Stenosis and Atrial FibrillationNasriÎncă nu există evaluări
- Rivaroxaban in Rheumatic Heart Disease - Associated Atrial FibrillationDocument11 paginiRivaroxaban in Rheumatic Heart Disease - Associated Atrial FibrillationEstevão CaminhaÎncă nu există evaluări
- Antagonist Oral AnticoagulantsDocument66 paginiAntagonist Oral Anticoagulantsbagheera316Încă nu există evaluări
- NEJM 2017 Comentario Braunwald2017Document2 paginiNEJM 2017 Comentario Braunwald2017Francisca Javiera Yáñez VidalÎncă nu există evaluări
- Commander HFDocument11 paginiCommander HFhairos.izhaÎncă nu există evaluări
- JAH3 11 E025723Document36 paginiJAH3 11 E025723ResidenPatKlin Juli2022Încă nu există evaluări
- Fsurg 10 1285553Document11 paginiFsurg 10 1285553William ChokÎncă nu există evaluări
- J Ahj 2006 06 024Document7 paginiJ Ahj 2006 06 024Alexandra RosaÎncă nu există evaluări
- Afire Articulo OriginalDocument11 paginiAfire Articulo OriginalElvira AnitaÎncă nu există evaluări
- Rivaroxaban in Patients With Atrial Fibrillation and A Bioprosthetic Mitral ValveDocument11 paginiRivaroxaban in Patients With Atrial Fibrillation and A Bioprosthetic Mitral ValveJuan JoseÎncă nu există evaluări
- Comparisons Between Oral Anticoagulants Among Older Nonvalvular Atrial Fibrillation PatientsDocument10 paginiComparisons Between Oral Anticoagulants Among Older Nonvalvular Atrial Fibrillation PatientsmadrugagalanfÎncă nu există evaluări
- Matanalisis ACODocument8 paginiMatanalisis ACOMarcelo AbrahamÎncă nu există evaluări
- TCP15 11MarcyTruongRaiDocument14 paginiTCP15 11MarcyTruongRaiadri20121989Încă nu există evaluări
- 10 1001@jamacardio 2020 4390Document9 pagini10 1001@jamacardio 2020 4390William ChokÎncă nu există evaluări
- Matsumoto2014 PDFDocument6 paginiMatsumoto2014 PDFNur Syamsiah MÎncă nu există evaluări
- Antithrombotic Therapy After Revascularization in Patients With Peripheral Arterial Disease: What Is Here, What Is NextDocument12 paginiAntithrombotic Therapy After Revascularization in Patients With Peripheral Arterial Disease: What Is Here, What Is NextenviÎncă nu există evaluări
- COMPASS by RISK STRATDocument10 paginiCOMPASS by RISK STRATMiguel GonzalezÎncă nu există evaluări
- Effectiveness and Safety of Direct Oral Anticoagulants in The Secondary Stroke Prevention of Elderly PatientsDocument9 paginiEffectiveness and Safety of Direct Oral Anticoagulants in The Secondary Stroke Prevention of Elderly PatientsLiam HudnikÎncă nu există evaluări
- Strokeaha 120 032704Document11 paginiStrokeaha 120 032704Norlando RuizÎncă nu există evaluări
- Circulation 2015 Avezum 624 32Document10 paginiCirculation 2015 Avezum 624 32Ernesto Ventura QuirogaÎncă nu există evaluări
- AC After StrokeDocument6 paginiAC After StrokeDileepa chathurangaÎncă nu există evaluări
- Unanswered Questions During The Live EventDocument9 paginiUnanswered Questions During The Live Eventyash_acharya007Încă nu există evaluări
- Health Services and Outcomes ResearchDocument10 paginiHealth Services and Outcomes ResearchRJMÎncă nu există evaluări
- The Reply AjmDocument2 paginiThe Reply AjmRaynolds Geraldy's photoÎncă nu există evaluări
- Jama Sidhu 2022 Oi 220087 1668452383.53768Document9 paginiJama Sidhu 2022 Oi 220087 1668452383.53768Karina AngelÎncă nu există evaluări
- Stroke Prevention in Atrial Fibrillation A Systematic ReviewDocument13 paginiStroke Prevention in Atrial Fibrillation A Systematic ReviewSebastian PierreÎncă nu există evaluări
- Debus Et Al 2021 Effect of Rivaroxaban and Aspirin in Patients With Peripheral Artery Disease Undergoing SurgicalDocument13 paginiDebus Et Al 2021 Effect of Rivaroxaban and Aspirin in Patients With Peripheral Artery Disease Undergoing SurgicalWilliam ChokÎncă nu există evaluări
- Apixaban With Antiplatelet Therapy After Acute Coronary SyndromeDocument10 paginiApixaban With Antiplatelet Therapy After Acute Coronary SyndromeAndi Soraya PurnamandaÎncă nu există evaluări
- Rivaroxaban ArticleDocument12 paginiRivaroxaban ArticleA. RaufÎncă nu există evaluări
- Anticoagulant in Atrial Fibrillation Patients With Prior IntracranialDocument7 paginiAnticoagulant in Atrial Fibrillation Patients With Prior IntracranialWilliam BarreraÎncă nu există evaluări
- 235 FullDocument8 pagini235 Fullsri noviyanty yusufÎncă nu există evaluări
- Complementary and Alternative Medical Lab Testing Part 3: CardiologyDe la EverandComplementary and Alternative Medical Lab Testing Part 3: CardiologyEvaluare: 1 din 5 stele1/5 (1)
- Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Synopsis of The 2017 American College of Cardiology:American Heart Association Hypertension GuidelineDocument10 paginiPrevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Synopsis of The 2017 American College of Cardiology:American Heart Association Hypertension GuidelineRoberto López MataÎncă nu există evaluări
- Best Clinical Practice: AnaphylaxisDocument6 paginiBest Clinical Practice: AnaphylaxisputriÎncă nu există evaluări
- 2017 ACC Expert Consensus Decision Pathway For Optimization of Heart Failure TreatmentDocument30 pagini2017 ACC Expert Consensus Decision Pathway For Optimization of Heart Failure TreatmentRoberto López MataÎncă nu există evaluări
- Hyperglycemic CrisisDocument9 paginiHyperglycemic CrisisRoberto López MataÎncă nu există evaluări
- HTN Emergencies and UrgenciesDocument14 paginiHTN Emergencies and UrgenciesRoberto López MataÎncă nu există evaluări
- Necrotizing Soft-Tissue InfectionsDocument13 paginiNecrotizing Soft-Tissue InfectionsRoberto López MataÎncă nu există evaluări
- Top 10 Myths Regarding The Diagnosis and Treatment of CellulitisDocument8 paginiTop 10 Myths Regarding The Diagnosis and Treatment of CellulitisRoberto López MataÎncă nu există evaluări
- ADA 2018 Diabetes CareDocument150 paginiADA 2018 Diabetes CareRoberto López Mata100% (1)
- Fluid Therapy Options and Rational SelectionDocument13 paginiFluid Therapy Options and Rational SelectionRoberto López MataÎncă nu există evaluări
- Update On The Management of Venous ThromboembolismDocument8 paginiUpdate On The Management of Venous ThromboembolismRoberto López MataÎncă nu există evaluări
- Diagnosis and Treatment of HyperkalemiaDocument9 paginiDiagnosis and Treatment of HyperkalemiaRoberto López MataÎncă nu există evaluări
- Uric Acid Is A Strong Risk Marker For Developing Hypertension From PrehypertensionDocument16 paginiUric Acid Is A Strong Risk Marker For Developing Hypertension From PrehypertensionRoberto López MataÎncă nu există evaluări
- The Use of Cephalosporins in Penicillin-Allergic Patients - A Literature ReviewDocument9 paginiThe Use of Cephalosporins in Penicillin-Allergic Patients - A Literature ReviewRoberto López MataÎncă nu există evaluări
- Pathophysiology of Septic ShockDocument19 paginiPathophysiology of Septic ShockRoberto López MataÎncă nu există evaluări
- The Dark Sides of Fuid Administration in The Critically Ill PatientDocument3 paginiThe Dark Sides of Fuid Administration in The Critically Ill PatientRoberto López MataÎncă nu există evaluări
- A Test in Context - D-DimerDocument10 paginiA Test in Context - D-DimerRoberto López MataÎncă nu există evaluări
- Sudden Cardiac Arrest During Participation in Competitive SportsDocument11 paginiSudden Cardiac Arrest During Participation in Competitive SportsRoberto López MataÎncă nu există evaluări
- Hepatitis B Vaccination, Screening, and Linkage To Care - Best Practice Advice From The American College of Physicians and The Centers For Disease Control and PreventionDocument12 paginiHepatitis B Vaccination, Screening, and Linkage To Care - Best Practice Advice From The American College of Physicians and The Centers For Disease Control and PreventionRoberto López MataÎncă nu există evaluări
- Atrial Fibrillation and HypertensionDocument17 paginiAtrial Fibrillation and HypertensionRoberto López MataÎncă nu există evaluări
- Diuretic Treatment in Heart FailureDocument12 paginiDiuretic Treatment in Heart FailureRoberto López Mata100% (1)
- The Role of Nitroglycerin and Other Nitrogen Oxides in Cardiovascular TherapeuticsDocument18 paginiThe Role of Nitroglycerin and Other Nitrogen Oxides in Cardiovascular TherapeuticsRoberto López MataÎncă nu există evaluări
- Rivaroxaban Vs Warfarin Sodium in The Ultra-Early Period After Atrial Fibrillation-Related Mild Ischemic StrokeDocument10 paginiRivaroxaban Vs Warfarin Sodium in The Ultra-Early Period After Atrial Fibrillation-Related Mild Ischemic StrokeRoberto López MataÎncă nu există evaluări
- Effects of Acarbose On Cardiovascular and Diabetes Outcomes in Patients With Coronary Heart Disease and Impaired Glucose Tolerance (ACE) - A Randomised, Double-Blind, Placebo-Controlled TrialDocument10 paginiEffects of Acarbose On Cardiovascular and Diabetes Outcomes in Patients With Coronary Heart Disease and Impaired Glucose Tolerance (ACE) - A Randomised, Double-Blind, Placebo-Controlled TrialRoberto López MataÎncă nu există evaluări
- Acute Monocular Vision LossDocument9 paginiAcute Monocular Vision LossRoberto López MataÎncă nu există evaluări
- 2015 ESC Guidelines For The Diagnosis and Management of Pericardial DiseasesDocument44 pagini2015 ESC Guidelines For The Diagnosis and Management of Pericardial DiseasesRoberto López MataÎncă nu există evaluări
- Synopsis of The 2017 U.S. Department of Veterans Affairs: Management of Type 2 Diabetes MellitusDocument10 paginiSynopsis of The 2017 U.S. Department of Veterans Affairs: Management of Type 2 Diabetes MellitusRoberto López MataÎncă nu există evaluări
- Effects on the Incidence of Cardiovascular Events of the Addition of Pioglitazone Versus Sulfonylureas in Patients With Type 2 Diabetes Inadequately Controlled With Metformin (TOSCA.it)- A Randomised, Multicentre TrialDocument11 paginiEffects on the Incidence of Cardiovascular Events of the Addition of Pioglitazone Versus Sulfonylureas in Patients With Type 2 Diabetes Inadequately Controlled With Metformin (TOSCA.it)- A Randomised, Multicentre TrialRoberto López MataÎncă nu există evaluări
- Evaluation and Management of Lower-Extremity UlcersDocument9 paginiEvaluation and Management of Lower-Extremity UlcersRoberto López MataÎncă nu există evaluări
- Dual Antithrombotic Therapy With Dabigatran After PCI in Atrial FibrillationDocument12 paginiDual Antithrombotic Therapy With Dabigatran After PCI in Atrial FibrillationRoberto López MataÎncă nu există evaluări
- 2020 ROTH IRA 229664667 Form 5498Document2 pagini2020 ROTH IRA 229664667 Form 5498hk100% (1)
- Lab Manual PDFDocument68 paginiLab Manual PDFSantino AwetÎncă nu există evaluări
- Organogram - Qa / QC: Srinivasan SrinivasanDocument4 paginiOrganogram - Qa / QC: Srinivasan SrinivasanGowtham VenkatÎncă nu există evaluări
- 10 2005 Dec QDocument6 pagini10 2005 Dec Qspinster40% (1)
- Lesson 1 - Intro To Highway EngineeringDocument15 paginiLesson 1 - Intro To Highway EngineeringSaoirseÎncă nu există evaluări
- HUM110 Gilgamesh EssayDocument4 paginiHUM110 Gilgamesh EssaynsmeganÎncă nu există evaluări
- Fill The Gaps With The Correct WordsDocument2 paginiFill The Gaps With The Correct WordsAlayza ChangÎncă nu există evaluări
- Standards Spec Brochure ME WEBDocument44 paginiStandards Spec Brochure ME WEBReza TambaÎncă nu există evaluări
- Method StatementDocument29 paginiMethod StatementZakwan Hisyam100% (1)
- Blueprint Huynh My Ky Duyen 2022 McDonald'sDocument2 paginiBlueprint Huynh My Ky Duyen 2022 McDonald'sHuỳnh Mỹ Kỳ DuyênÎncă nu există evaluări
- Marine Trans Owners Manual 1016313 RevH 0116 CDDocument200 paginiMarine Trans Owners Manual 1016313 RevH 0116 CDMarco Aurelio BarbosaÎncă nu există evaluări
- Fast FashionDocument9 paginiFast FashionTeresa GonzalezÎncă nu există evaluări
- Penilaian Akhir TahunDocument4 paginiPenilaian Akhir TahunRestu Suci UtamiÎncă nu există evaluări
- Ras Shastra PPT 6Document10 paginiRas Shastra PPT 6Soham BhureÎncă nu există evaluări
- Parche CRP 65 - Ficha Técnica - en InglesDocument2 paginiParche CRP 65 - Ficha Técnica - en IngleserwinvillarÎncă nu există evaluări
- Psychoanalysis AND History: Freud: Dreaming, Creativity and TherapyDocument2 paginiPsychoanalysis AND History: Freud: Dreaming, Creativity and TherapyJuan David Millán MendozaÎncă nu există evaluări
- Tamilnadu Shop and Establishment ActDocument6 paginiTamilnadu Shop and Establishment ActShiny VargheesÎncă nu există evaluări
- NG Teng Fong Discharge DocumentsDocument14 paginiNG Teng Fong Discharge DocumentsAnonymous yGwMIPJRawÎncă nu există evaluări
- Sop For Enlistment of Engineering ConsultantsDocument1 paginăSop For Enlistment of Engineering Consultantssatheb319429Încă nu există evaluări
- Yogananda Scientific HealingDocument47 paginiYogananda Scientific HealingSagar Pandya100% (4)
- Heteropolyacids FurfuralacetoneDocument12 paginiHeteropolyacids FurfuralacetonecligcodiÎncă nu există evaluări
- Itrogen: by Deborah A. KramerDocument18 paginiItrogen: by Deborah A. KramernycÎncă nu există evaluări
- Transfer and Business Taxation SyllabusDocument5 paginiTransfer and Business Taxation SyllabusamqqndeahdgeÎncă nu există evaluări
- Rules For State Competitions and Iabf Approved TournamentsDocument56 paginiRules For State Competitions and Iabf Approved TournamentsQuality management systems documentsÎncă nu există evaluări
- Sav4747 PDFDocument49 paginiSav4747 PDFAndres Antonio Moreno CastroÎncă nu există evaluări
- Iomm VFD-3 030112Document100 paginiIomm VFD-3 030112Alexander100% (1)
- Dr. Nastiti K - Manajemen Asma Pada Anak 2018 PDFDocument72 paginiDr. Nastiti K - Manajemen Asma Pada Anak 2018 PDFagnesspratiwiÎncă nu există evaluări
- Current Concepts of Enzyme Histochemistry in Modern PathologyDocument11 paginiCurrent Concepts of Enzyme Histochemistry in Modern PathologyRosa AquinoÎncă nu există evaluări