Documente Academic
Documente Profesional
Documente Cultură
Puerperium, Breastfeeding
Încărcat de
ina17_eaglerTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Puerperium, Breastfeeding
Încărcat de
ina17_eaglerDrepturi de autor:
Formate disponibile
THE PUERPERIUM
(from Williams, APMC, and SGD)
March 03, 2009 / KC Chua Sec A 2011
PUERPERIUM
period of confinement during and just after birth * Afterpains
usually includes the 6 subsequent weeks (or 42 days (APMC)) Primiparas = uterus remains tonically contracted
immediately after delivery of placenta return of reproductive Multiparas = uterus contracts vigorously at intervals afterpains
organs to normal non-pregnant condition (APMC) parity, suckling ( oxytocin) = afterpains
rd
3 day = afterpains decrease in intensity
Clinical and Physiological Aspects of the Puerperium Afterpain helps to keep the uterus involuted (APMC)
1. Uterine Changes * Lochia
Vaginal discharge of variable quantity
a. Uterine Vessels From sloughing of decidual tissue
After delivery caliber of extrauterine vessels Persists for up to 4 weeks
decreases to equal, or at least closely approximates, May stop and resume up to 8 weeks after delivery
that of the prepregnant state The following DO NOT influence duration of lochia
Larger blood vessels are obliterated by hyaline o Maternal age
changes, gradually resorbed, and replaced by smaller o Parity
ones o Infant weight
Minor vestiges of the larger vessels may persist for o Breast feeding
years Oxytocic agents = do NOT diminish blood loss & does NOT hastens
uterine involution
b. Cervix and Lower Uterine Segment Composition of lochia: (BEES)
Cervical opening few days immediately after labor = o Bacteria
readily admits two fingers o Erythrocytes
End of the first week = narrowed thickens canal o Epithelial cells
reforms o Shredded decidua
External os does NOT completely resume its pregravid 3 Types of Lochia (RSA)
appearance o Rubra (Day 1 4 or 5)
o Wider Red vaginal discharge
o Bilateral depressions at the site of First few days after delivery
lacerations = jagged transverse slits = fish o Serosa (Day 6 8 or 9)
mouth appearance (APMC) Pale, pinkish
th
o Cervical epithelium undergoes remodeling o Alba (after about the 10 day)
White / yellowish-white / creamy
Lower segment
Color attributed to:
o converted into a barely discernible uterine
isthmus located between the uterine Leukocytes (Williams)
corpus above and the internal cervical os Reduced fluid content (Williams)
below Cervical mucous (APMC)
o narrowed & collapsed (APMC) Debris from healing tissues (APMC)
c. Involution of the Uterine Corpus d. Endometrial Regeneration
Involution process by which the uterus returns to Within 2 or 3 days after delivery = remaining decidua
normal size, tone, and position (APMC) differentiated into two layers
Nulliparas = faster; multiparas = slower (APMC) Superficial layer = necrotic, sloughed
Immediately after placental expulsion = fundus of the Basal layer = intact, source of new
contracted uterus slightly below the umbilicus endometrium
Due to vessel compression by contracted myometrium Endometrium arises from proliferation of the
= uterus appears ischemic (when compared with the endometrial glandular remnants and the stroma of
reddish-purple hyperemic pregnant organ) the interglandular connective tissue
Rate of uterine involution = 1-2 cm / day (APMC) Rapid except at placental site
2 days after delivery = uterus shrinks Within 1 week = free surface covered by epithelium
rd
2 weeks after delivery = uterus descended into the 3 week = restoration of entire endometrium
cavity of the true pelvis Histological endometritis, acute salphingitis = part of
4 weeks after delivery = regains its previous the normal reparative process; inflammatory changes
nonpregnant size do NOT reflect infection
Immediately postpartum = 1000 g
* Subinvolution
1 week postpartum = 500 g
Arrest or retardation of involution
2 weeks postpartum = 300 g
Observations:
Nonpregnant g = 100 g
o Prolongation of lochial discharge
6 weeks postpartum = 70 g (APMC)
o Irregular or excessive uterine bleeding
Decrease in size, not number of cells o Uterus = larger and softer than expected
Spongy layer = sloughed Causes:
Decidua basalis = not sloughed o Retention of placental fragments
Has striking variations in thickness o Pelvic infection
Has irregular jagged appearance 1/3 of cases = Chlamydia trachomatis
Infiltrated with blood Rx: azithromycin & doxycycline
Failure of uterus to contract: (PACID) (APMC) Usually amenable to early diagnosis and treatment = Ergonovine
1) Retained Placental cotyledons or methylergonovine = efficacy is questionable
2) Uterine Atony Metritis responds to oral antimicrobial therapy
3) Clot formation
4) Infections e. Placental Site Involution
5) Inadequate Drainage of tissues 6 weeks = complete extrusion of the placental site
takes
Interference = late-onset puerperal hemorrhage (APMC)
Immediately after delivery = placental site about the
size of the palm rapidly decreases
End of the 2nd week = 3 to 4 cm in diameter
Involving a process of exfoliation = brought about by
the undermining of implantation site by growth of
endometrial tissue both extension and
downgrowth of endometrium development of Rupture of elastic fibers in the skin and the prolonged
endometrial tissue distention abdominal wall remains soft and flaccid
Involution is not brought about by absorption in situ Recovery is aided by exercise
Consequence of sloughing of infarcted and necrotic Except for silvery striae (striae abdominis), the abdominal
superficial tissues followed by a reparative process wall usually resumes its prepregnancy appearance
Atonic muscles lax abdominal wall marked separation
f. Late Postpartum Hemorrhage of rectus muscles = diastasis recti
1 to 2 weeks into the puerperium o the midline abdominal wall is formed only by
Causes: peritoneum, attenuated fascia, subcutaneous fat,
o Abnormal involution of the placental site and skin.
(most common)
o Retention of a portion of the placenta 5. Blood and Fluid Changes
Retained piece necrosis Marked leukocytosis and thrombocytosis
form placental polyp eschar o leukocyte count = 30,000/L (predominantly
detaches from myometrium granulocytes); 15,000/L at first week is common as
hemorrhage defense against infections and for tissue repair
Best initial treatment = control of the bleeding with o Relative lymphopenia and an absolute eosinopenia
intravenous oxytocin, ergonovine, methylergonovine, Hgb & Hct = fluctuate moderately
or prostaglandins RBC count below prelabor values = blood loss
Prompt curettage = treatment of late postpartum 1 week postpartum = return of non-pregnant blood volume
hemorrhage but may worsen the hemorrhage by 2 days postpartum = cardiac output remains elevated due to
traumatizing the implantation site and inciting more increased stroke volume from venous return; heart rate falls
bleeding. Curettage is carried out only if appreciable 2 weeks postpartum = cardiac output return to normal
bleeding persists or recurs after medical management. 1 week postpartum = ESR & plasma fibrinogen
st
2. Urinary Tract Changes * Weight Loss
UT returns to normal 4 to 6 weeks postpartum (APMC) 5 to 6 kg = via uterine evacuation and normal blood loss
Between 2 and 5 day = Postpartum diuresis =
nd th
Further decrease of 2 to 3 kg = via diuresis and diaphoresis
physiological reversal of increase of extracellular water (integumentary loss (APMC))
during pregnancy 6 months postpartum = attain non-pregnant weight (APMC)
Corresponds with loss of residual pregnancy
hypervolemia
Preeclampsia = fluid retention and diuresis BREAST / LACTATION / BREAST FEEDING
Bladder = capacity, overdistention, incomplete
emptying, residual urine I. Breast Anatomy
Overdistention avoided by emptying Composed of 15 to 25 lobes arranged radially
bladder at least every 6 to 8 hours (APMC) Lobe > lobules > alveoli > small ducts > large ducts > opens to
Analgesics (epidural & spinal blocks) = paralyzing effect nipples
contributes to UT changes Alveolar secretory epithelium = synthesizes the various milk
Within 3 days = ketonuria (due to starvation) disappears constituents.
(APMC)
st
1 week = glucosuria due to lactose production of
II. Breast Feeding
breast (APMC)
nd
2 day postpartum = colostrum deep lemon-yellow-
2 to 8 weeks after delivery = dilated ureters and renal
colored liquid
pelvis return to non-pregnant state (Williams)
Minerals and protein colostrum > mature milk ( globulin,
Monitor excessive residual urine to avoid
sugar and larger fat globules)
o Urinary tract infection
o Bladder atony Colostrum: (APMC)
1) Ideal food starter
st
Urinary retention may occur in the 1 24 hours due to:
(APMC) 2) Natural newborn laxative
o Edema and congestion of vulva, urethra, and 3) Help baby get rid of meconium
bladder trigone Colostrum secretion persists for about 5 days
o Edema and reflex spasm of urethral sphincter Colostrum mature milk takes 4 weeks (gradual
o Bladder atony conversion starts in about 5 days (APMC))
Incomplete emptying of bladder caused by: Immunoglobulin A (IgA) may offer protection for the
o Prolonged labor newborn against enteric pathogens
o Birth trauma Other host resistance factors that are found in colostrum
o Vaginal lacerations and milk include:
o Episiotomy o Complement
o Analgesia & anesthesia o Macrophages
o Lymphocytes
* Incontinence o Lactoferrin
3 to 6 months after delivery o Lactoperoxidase
Stress incontinence after delivery o Lysozymes
o length of second-stage labor
o infant head circumference III. Milk
o birthweight Suspension of fat and protein in a carbohydrate-mineral
o episiotomy solution
Proposed pathophysio = Impaired muscle function in or around Gestational weight gain has little, if any, impact on the
the urethra as a result of vaginal delivery subsequent milk quantity or quality
Volume of milk per day = 600 mL
3. Vaginal Outlet Relaxation and Uterine Prolapse Isotonic with plasma
Rarely returns to nulliparous dimensions Lactose accounts for half of the osmotic pressure
3 week = vaginal rugae reappear (Williams)
rd
Major proteins:
4 week = vaginal rugae reappear (APMC)
th
o -lactalbumin
Hymen = represented by several small tags of tissue = during o -lactoglobulin
cicatrization converted to myrtiform caruncles (Williams) o casein
Hymenal tags remnants = caruncle myrtiformes (APMC) Essential amino acids = from blood,
Extensive laceration of perineum relaxation of vaginal Nonessential amino acids = from blood or synthesized in the
outlet predispose to uterine prolapsed and urinary stress mammary gland
incontinence Most milk proteins are unique and not found elsewhere
1 to 2 weeks = fully healed lacerations & episiotomy; return Whey = IL-6 = local IgA production by the breast
of fallopian tubes and ovaries to the pelvis (APMC) 30 to 40 hours postpartum = sudden lactose kidneys
glucosuria
4. Peritoneum and Abdominal Wall
Broad and round ligaments
Has ALL vitamins except Vitamin K (Vitamin K administration o The following do NOT contraindicate breast
to the infant soon after delivery is required to prevent feeding:
hemorrhagic disease of the newborn) maternal cytomegalovirus infection
(virus and antibodies are present in
IV. Endocrinology of Lactation breast milk)
Hormones that stimulate growth and development of hepatitis B virus (not contraindicated
mammary glands lactation: if hepatitis B immune globulin is given
o Progesterone to infants of seropositive mothers)
o Estrogen maternal hepatitis C infection
o Placental lactogen herpes simplex virus (if there are no
o Prolactin breast lesions and if particular care is
o Cortisol directed to hand washing before
o Insulin nursing)
With delivery = progesterone & estrogen removes
the inhibitory influence of progesterone on production of - X. Care
lactalbumin by the rough endoplasmic reticulum - Cleaning of the areola with water and mild soap = dried milk
lactalbumin stimulates lactose synthase milk lactose is likely to accumulate and irritate the nipples
Progesterone withdrawal = allows prolactin to act For irritated nipples = use nipple shield for 24 hours or
unopposed in its stimulation of -lactalbumin production longer
Intensity and duration of lactation = controlled by repetitive Inverted or retracted nipples = gently pull with the finger
stimulus of nursing and thumb (best begun during pregnancy to prepare the
Women with extensive pituitary necrosis, or Sheehan nipples for subsequent nursing)
syndrome, do not lactate Proper technique for positioning the mother and infant
Suckling prolactin-inhibiting factor (hypothalamus) Proper techniques for latch-on of the infant during suckling
prolactin secretion milk production
Suckling neurohypophysis secretes oxytocin cause XI. Drugs Secreted in Milk
contraction of myoepithelial cells in the alveoli and small Factors that influence drug excretion in milk:
milk ducts milk letdown reflex / milk ejection o concentration of drugs in plasma
Milk let down provoked = cry of infant o degree of protein binding
Milk let down inhibited = fright or stress o plasma and milk pH
o degree of ionization
V. Immunological Consequences of Breast Feeding o lipid solubility
Antibodies are poorly absorbed, if at all, by infants o molecular weight
Secretory IgA = predominant immunoglobulin in milk The amount of drug ingested by the infant typically is small
IgA has important antimicrobial functions Milk-to-plasma drug-concentration ratio = ratio of drug
IgA exerts its action by preventing bacterial adherence to concentrations in breast milk to those in maternal
epithelial cell surfaces, thus preventing tissue invasion Most drugs have a milk-to-plasma ratio of 1 or less
Human milk also provides protection against rotavirus
a
infections Drug Reported Effect
Milk contains both T and B lymphocytes Acebutolol Hypotension, bradycardia, tachypnea
5-Aminosalicylic Diarrhea
VI. Nursing acid
Human milk is ideal food for neonates Aspirin (salicylates) Metabolic acidosis
Mothers milk is natures best food for babies (APMC) Atenolol Cyanosis, bradycardia
It provides species- and age-specific nutrients for the infant Bromocriptine Suppresses lactation, may be hazardous to the
In addition to the proper balance of nutrients, mother
immunological factors, and antibacterial properties, human Clemastine Drowsiness, irritability, refusal to feed, high-pitched
milk contains factors that act as biological signals for cry, neck stiffness (one case)
promoting cellular growth and differentiation Cyclophosphamide Interfere with the cellular metabolism of the infant
65% of women who have undergone augmentation Cyclosporine and potentially cause immune suppression or
mammoplasty have lactation insufficiency Doxorubicin neutropenia, affect growth, or, at least theoretically,
Methotrexate increase the risk of cancer
VII. Lactation Inhibition Ergotamine Vomiting, diarrhea, convulsionsdoses used in
Elect not to breast feed migraine medications
Breast pain Lithium A third to half therapeutic blood concentration in
Engorgement infants
3 to 5 days postpartum = Milk leakage, engorgement, and Phenindione Anticoagulant increased prothrombin and partial
breast pain peak thromboplastin time in one infant not used in
Bromocriptine = drug for lactation inhibition United States
Measures to alleviate breast pain: Phenobarbital Sedation; infantile spasms after weaning from milk
o Well-fitting brassiere containing phenobarbital; methemoglobinemia
o Ice packs Primidone Sedation, feeding problems
Sulfasalazine Bloody diarrhea
o Oral analgesics for 12 to 24 hours
VIII. Contraception for Breast Feeding Women XII. Breast Fever
3 weeks postpartum = ovulation may resume First 24 hours after commencement of lactation
Ovulation resumption depends on: Puerperal fever from breast engorgement is common
o individual biological variation Fever ranging from 37.8 to 39C
o intensity of breast feeding Fever seldom persisted for longer than 4 to 16 hours
Progestin-only contraceptivesmini-pills and depot Other causes of fever, especially those due to infection,
medroxyprogesterone do NOT affect the quality or must be excluded
decrease milk volume = hormonal contraceptives of choice Treatment consists of:
for breast feeding women by the American College of o supporting the breasts with a binder or brassiere
Obstetricians and Gynecologists (2000) o applying an ice bag
o analgesics
IX. Contraindications to Breast Feeding o pumping of the breast or manual expression of
Taking street drugs milk
Alcohol use may be necessary at first, but in a few
Infants with galactosemia days the condition is usually alleviated
HIV and the infant is able to nurse
TB normally
Undergoing treatment for breast CA
XIII. Mastitis Anesthesia, episiotomy, & lacerations = bladder sensation
Rare & capability to empty spontaneously
Occasionally observed during the puerperium and lactation Urinary retention with bladder overdistention is a common
rd th
Symptoms appear at the 3 or 4 week postpartum, seldom complication of the early puerperium
st
before the end of 1 week postpartum Prevent bladder overdistention
Infection almost invariably is unilateral Woman should void within 4 hours after delivery
Marked engorgement usually precedes the inflammation o Hematomas of the genital tract must be
1st sign of inflammation = chills or actual rigor (followed by considered.
fever and tachycardia) o > 200mL urine in bladder = urine retention =
Breast becomes hard and reddened catheterize
Severe pain o Bacteriuria = Rx: short course of antimicrobial
10 percent of women with mastitis develop an abscess therapy
Most common organism = Staphylococcus aureus
o Rx: Dicloxacillin 500mg every 6 hours (4x a day) V. Subsequent Discomfort
o Erythromycin penicillin-sensitive patients Afterpains
rd
o Vancomycin MRSA Episiotomy (healed by 3 week)
Source of organism = infants nose & throat Lacerations
Breast engorgement
XIV. Breast Abscess Postspinal puncture headache
From failure of defervescence within 48 to 72 hours Rx: codeine, 60 mg; aspirin, 600 mg; or acetaminophen, 500
Development of a palpable mass mg, preferably in combinations, at intervals as frequent as
Traditional therapy = surgical drainage every 3 hours during the first few days after delivery.
Uterine contractions are commonly accentuated during
XV. Galactocele nursing, giving rise at times to troublesome afterpains.
Result of clogging of a duct by inspissated secretion Application of an ice bag may minimize swelling and
Milk may accumulate in one or more lobes of the breast. discomfort
Excess may form a fluctuant mass pressure symptoms Severe discomfort
st
Resolve spontaneously or require aspiration o Within 1 day or so = hematoma
rd th
o 3 or 4 day = infection
XVI. Supernumerary Breasts
One or more accessory breasts (polymastia) VI. Depression
Usually below the main breasts Postpartum blues = remits after 2 3 days, sometimes
Also found in the axillae persists up to 10 days
rd
3 day or baby blues (APMC)
XVII. Abnormalities of the Nipples Consequence of a number of factors:
Lactiferous ducts open directly into a depression at the o Emotional letdown that follows the excitement
center of the areola and fears that most women experience during
Severely depressed nipples = nursing not possible pregnancy and delivery
Depression not very deep = use breast pump o Discomforts of the early puerperium
Inverted nipples = traction with fingers o Fatigue from loss of sleep during labor and
postpartum
Fissures = render nursing painful; portal of entry for
o Anxiety over her capabilities for caring for her
pyogenic bacteria = use nipple shield & topical medication
infant after leaving the hospital
and empty regularly with a suitable pump until the lesions
o Fears that she has become less attractive
are completely healed
o Jealousy and insecurity (APMC)
o Inability to satisfy husbands needs (APMC)
XVIII. Abnormalities of Secretion
Effective treatment:
Mostly dependent on the development of the glandular
o Anticipation
portions of the breasts
o Recognition
Agalactia complete lack of mammary secretion
o Assurance
Polygalactia mammary secretion is excessive
VII. Abdominal Wall Relaxation
Flabby abdomen = girdles
CARE OF THE MOTHER DURING PUERPERIUM Exercise after soreness diminishes
I. Hospital Care VIII. Gastrointestinal Tract (APMC)
BP & PR = take every 15 minutes Atony = from prolonged labor; manifested by tympanism
Monitor amount of vaginal bleeding Constipation = from patients inactivity, decreased
Palpate fundus if well-contracted (if relaxed = massage intraabdominal pressure, and painful perineum
abdominal wall) Mild cathartics may be given after 48 hours
Trained attendant should remain with the mother for at
least 1 hour after delivery = risk of postpartum hemorrhage IX. Diet
No dietary restrictions
II. Early Ambulation
2 hours after a normal vaginal delivery = woman should be
Within a few hours after delivery allowed to eat if she desires
Advantages of early ambulation: Diet should be increased in calories and protein
o bladder complications
If mother does not breast feed = non-pregnant woman diet
o constipation
Iron supplementation = at least 3 months postpartum
o frequency of puerperal venous thrombosis
o pulmonary embolism
X. Thromboembolic Disease
Half of thromboembolic events associated with pregnancy
III. Care of the Vulva
develop in the puerperium
Cleanse the vulva from anterior to posterior (vulva anus)
Frequency of deep venous thrombosis and pulmonary
An ice bag applied to the perineum = reduce edema and
embolism complicating pregnancy and the puerperium has
discomfort during the first several hours after episiotomy
decreased in recent years
repair
24 hours after delivery = moist heat (warm sitz baths) used
XI. Obstetrical Neuropathies
to reduce local discomfort
2 months, with a range of 2 weeks to 18 months
Tub bathing after uncomplicated delivery is allowed (Williams)
Intense neuralgia / cramplike pains = due to pressure on
Tub baths are not allowed (APMC)
lumbosacral nerve plexus
Lateral femoral cutaneous neuropathies = most common
IV. Bladder Function
Independent rist factors for nerve injury
Oxytocin, in doses that have an antidiuretic effect, is
o nulliparity
commonly infused after placental delivery
o prolonged second-stage of labor
Sudden withdrawal oxytocin = rapid bladder filling
XII. Pelvic Joint Separation By the time of discharge, women who had a normal delivery
Separation of the symphysis pubis or one of the sacroiliac and puerperium can resume most activities, including
synchondroses during labor may be followed by pain and bathing, driving, and household functions.
marked interference with locomotion Care and nurturing of the neonate should be provided by
Treatment = rest in a lateral decubitus position and an the mother with ample help from the father
appropriately fitted pelvic binder For the mother to provide this care, her presence at home
with the infant precludes her early return to full-time work
XIII. Immunizations or school
D-negative woman whose infant is D-positive = given 300 g
of anti-D immune globulin shortly after delivery ~kc 03/03/09
MMRI vaccine before discharge
diphtheria-tetanus toxoid booster injection (unless
contraindicated)
XIV. Time of Discharge
Hospital stay = about 48 hours (2 days)
Primiparas = 2 3 days (APMC)
Multiparas = 1 2 days (APMC)
Woman should receive instructions concerning the
anticipated normal physiological changes of the puerperium:
o lochia patterns
o weight loss from diuresis
o when to expect milk let-down
o what to do if she:
becomes febrile
has excessive vaginal bleeding
develops leg pain, swelling, or
tenderness
Instruct regarding self-care, baby care, breast feeding,
breast care/self-examination, and parenthood (APMC)
Any shortness of breath or chest pain warrants immediate
concern.
XV. Contraception
If no breast feeding = menses return within 6 to 8 weeks
(55-60 days; range: 20-120 days (APMC))
Ovulation = less frequent in women who breast feed
Menses may not appear if the infant is nursed
There is delayed resumption of ovulation with breast
feeding
Other findings:
Resumption of ovulation was
frequently marked by return of
normal menstrual bleeding
Breast feeding episodes lasting 15
minutes 7x each day delayed
resumption of ovulation
Ovulation can occur without bleeding
Bleeding can be anovulatory
HOME CARE
I. Coitus
No definite time after delivery when coitus should be
resumed
Resumption of intercourse too soon = unpleasant, painful
due to incomplete healing of the episiotomy or lacerations
Perineal repair = 1 2 weeks; coitus should be avoided until
all wounds have healed (APMC)
After 2 weeks = coitus may be resumed based on the
patient's desire and comfort
Breast feeding causes a prolonged period of suppressed
estrogen production vaginal atrophy and dryness
decreased vaginal lubrication during sexual arousal
II. Infant Follow-Up
Neonate discharged early should be:
o Term
o Normal
o Have stable vital signs.
Initial hepatitis B vaccine should be administered,
Include testing for hypothyroidism and phenylketonuria
(PKU).
III. Late Maternal Morbidity
Possible sequelae of labor epidural analgesia
IV. Follow-Up Care
rd
Follow-up at 3 week postpartum
o To identify abnormalities
o Initiate contraceptive practices
Estrogen plus progestin oral contraceptives started at this
time have proven to be effective without increased
morbidity
S-ar putea să vă placă și
- Organ Anatomy Notes 1Document8 paginiOrgan Anatomy Notes 1ELIANA CARIS CABILDOÎncă nu există evaluări
- AEGIS 2015 - Photoshoot PrimerDocument20 paginiAEGIS 2015 - Photoshoot Primerina17_eaglerÎncă nu există evaluări
- Doctor High Yield Obgyn - Not AnnotatedDocument34 paginiDoctor High Yield Obgyn - Not AnnotatedEmanuella Gomez100% (2)
- Paul Marik Vitamin C CHESTDocument10 paginiPaul Marik Vitamin C CHESTIrwan YongnardiÎncă nu există evaluări
- Mbdqor345235235 PDFDocument482 paginiMbdqor345235235 PDFM HaidarÎncă nu există evaluări
- Fetomaternal Organ FunctionsDocument21 paginiFetomaternal Organ FunctionsHem Kumari75% (4)
- AYUSHDocument39 paginiAYUSHSujatha J Jayabal88% (8)
- Nurse's Pocket GuideDocument11 paginiNurse's Pocket GuideRaf_Harold_427Încă nu există evaluări
- Newborn NotesDocument3 paginiNewborn NotesSharlotte EbayÎncă nu există evaluări
- Seminar On Shock: IndexDocument37 paginiSeminar On Shock: IndexGayathri R100% (1)
- No-Risk Abs: A Safe Workout Program for Core StrengthDe la EverandNo-Risk Abs: A Safe Workout Program for Core StrengthÎncă nu există evaluări
- Clinical Guide to OB ChangesDocument7 paginiClinical Guide to OB ChangesAllan Christian AlnÎncă nu există evaluări
- Case Study of Ruptured Appendicitis With Localize Peritonitis (Final)Document76 paginiCase Study of Ruptured Appendicitis With Localize Peritonitis (Final)DRJC82% (22)
- Assessment and Management of Women During Post-Natal PeriodDocument82 paginiAssessment and Management of Women During Post-Natal Periodsweta0% (1)
- Normal Labor and Delivery ProcessesDocument10 paginiNormal Labor and Delivery ProcessesManjula100% (1)
- Puerperium (Trans)Document7 paginiPuerperium (Trans)Charlie65129Încă nu există evaluări
- 01 EnemaDocument4 pagini01 Enemabunso padillaÎncă nu există evaluări
- Postpartum CareDocument13 paginiPostpartum CareChristian100% (11)
- Micromedex 360 Care Insights BrochureDocument9 paginiMicromedex 360 Care Insights BrochureSteve ArendÎncă nu există evaluări
- History of SurgeryDocument35 paginiHistory of SurgeryImolaBakosÎncă nu există evaluări
- NCM204 Page 361-471Document43 paginiNCM204 Page 361-471Charlie AbagonÎncă nu există evaluări
- Ob FinalDocument5 paginiOb Finalsofiapanlilio32Încă nu există evaluări
- Fourth Stage of LaborDocument5 paginiFourth Stage of LaborAjay DÎncă nu există evaluări
- IIII :::: : S EsentDocument22 paginiIIII :::: : S EsentCharlie AbagonÎncă nu există evaluări
- Post Partum SF 1 - 1Document19 paginiPost Partum SF 1 - 1John MajanÎncă nu există evaluări
- NCM 107 MidtermDocument34 paginiNCM 107 MidtermChiaraÎncă nu există evaluări
- Onset of LaborDocument4 paginiOnset of LaborK louiseÎncă nu există evaluări
- MCN 80 114Document35 paginiMCN 80 114Jianne CaloÎncă nu există evaluări
- NCA - 2.5 - Postpartum Complications-Labordo-saldana-serrano-sabejon-sarsozaDocument7 paginiNCA - 2.5 - Postpartum Complications-Labordo-saldana-serrano-sabejon-sarsozaFranz Earl Niño AlbesaÎncă nu există evaluări
- PuerperiumDocument16 paginiPuerperiumLi FaungÎncă nu există evaluări
- Obstetrics Maternal Physiology Dra. Marla Llanto: UterusDocument12 paginiObstetrics Maternal Physiology Dra. Marla Llanto: UterusIsabel CastilloÎncă nu există evaluări
- Pediatrics HandoutsDocument9 paginiPediatrics HandoutsSerafin Jr. GarcianoÎncă nu există evaluări
- OB HandoutsDocument9 paginiOB Handoutsjewa100% (1)
- 3 - Female PelvisDocument27 pagini3 - Female PelvisKandula KasunÎncă nu există evaluări
- Module 6 - MCN MaternalDocument5 paginiModule 6 - MCN MaternalChristine DuqueÎncă nu există evaluări
- Maternal and Child NursingDocument7 paginiMaternal and Child NursingErjen Alexandria SiaÎncă nu există evaluări
- Puerperium: Puja Agung AntoniusDocument25 paginiPuerperium: Puja Agung AntoniusWinda LiraÎncă nu există evaluări
- Emailing PDX-BREAST-AND-AXILLADocument7 paginiEmailing PDX-BREAST-AND-AXILLAIsabel CastilloÎncă nu există evaluări
- Anatomy of the Female BreastDocument18 paginiAnatomy of the Female Breasthabtsh habshaÎncă nu există evaluări
- Postpartum Changes Postpartal Period (Puerperium) - Refers To The 6 Weeks Period After ChildbirthDocument12 paginiPostpartum Changes Postpartal Period (Puerperium) - Refers To The 6 Weeks Period After ChildbirthGrace CruzÎncă nu există evaluări
- PT 1011: Back Region Secondary Curves and Abnormal Spinal CurvesDocument21 paginiPT 1011: Back Region Secondary Curves and Abnormal Spinal Curveschynne ongÎncă nu există evaluări
- Maternal Last Topic (Jam)Document1 paginăMaternal Last Topic (Jam)Jamilah BanglanÎncă nu există evaluări
- MCNDocument11 paginiMCNArienne Janine MalabananÎncă nu există evaluări
- CORNELL NOTE Physical and Developmental Disorders in NewbornDocument4 paginiCORNELL NOTE Physical and Developmental Disorders in NewbornMargareth DandanÎncă nu există evaluări
- Human Development TransesDocument5 paginiHuman Development TransesReign SaplacoÎncă nu există evaluări
- Obstructed LaborDocument4 paginiObstructed Laborkhadzx100% (2)
- Maternal Health: Pregnancy Signs and StagesDocument9 paginiMaternal Health: Pregnancy Signs and StagesjisooÎncă nu există evaluări
- Ca 1: Obstetric Nursing: Female ReproductiveDocument7 paginiCa 1: Obstetric Nursing: Female ReproductiveannÎncă nu există evaluări
- Pediatrics SamplesDocument50 paginiPediatrics SamplesErik Judika2Încă nu există evaluări
- DR NotesDocument3 paginiDR Notesnoreen ellie100% (2)
- Maternal PhysiologyDocument6 paginiMaternal Physiologyhk5vnxp2x5Încă nu există evaluări
- Growing Beans Handout - Plant Growth Scientific ExperimentDocument2 paginiGrowing Beans Handout - Plant Growth Scientific ExperimentMariah Alexis EncinaÎncă nu există evaluări
- Midterm Task 4Document8 paginiMidterm Task 4Rosevick BadocoÎncă nu există evaluări
- Midterm - Ob Normal LectureDocument44 paginiMidterm - Ob Normal LectureLeslie John PalaposÎncă nu există evaluări
- Day 12 - Ncm-109 7b InfancyDocument59 paginiDay 12 - Ncm-109 7b InfancySheena Patricia ArasulaÎncă nu există evaluări
- SMR 4 - Genital Prolapse and Urinary IncontinenceDocument21 paginiSMR 4 - Genital Prolapse and Urinary IncontinenceGrumpy TrollÎncă nu există evaluări
- Normal PuerperiumDocument64 paginiNormal PuerperiumBilisummaa OromooÎncă nu există evaluări
- NCM 107 - MATERNAL & CHILD HEALTH NURSING 1st SEMESTER MIDTERM REVIEWERDocument4 paginiNCM 107 - MATERNAL & CHILD HEALTH NURSING 1st SEMESTER MIDTERM REVIEWERskoolrkiveÎncă nu există evaluări
- Obstetrics and Gynecology: Normal Labor ExplainedDocument3 paginiObstetrics and Gynecology: Normal Labor ExplainedLuis PadillaÎncă nu există evaluări
- 1656070458546558Document102 pagini1656070458546558aldeeray01Încă nu există evaluări
- 006 CMED121 Anatomy of The BreastDocument5 pagini006 CMED121 Anatomy of The BreastDavid MarasiganÎncă nu există evaluări
- CHAPTER 9-Body CavitiesDocument3 paginiCHAPTER 9-Body CavitiespraiseginelcÎncă nu există evaluări
- Ncma217 Week 10Document7 paginiNcma217 Week 10Polly ArcheronÎncă nu există evaluări
- Week 2 Sex and FertDocument17 paginiWeek 2 Sex and FertAbmil Ching TinggalongÎncă nu există evaluări
- Postpartum 1 2Document8 paginiPostpartum 1 2Arbie SuaybaguioÎncă nu există evaluări
- Phy PuerperiumDocument27 paginiPhy PuerperiumDevuchandana RÎncă nu există evaluări
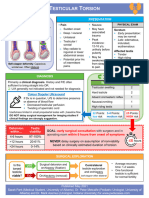
- Testicular Torsion, Peds Cases NotesDocument1 paginăTesticular Torsion, Peds Cases NotesdzalhcÎncă nu există evaluări
- Sharks of the Open Ocean: Biology, Fisheries and ConservationDe la EverandSharks of the Open Ocean: Biology, Fisheries and ConservationMerry D. CamhiÎncă nu există evaluări
- Tips For 3rd YearDocument4 paginiTips For 3rd YearCharles Jeffrey TanÎncă nu există evaluări
- Tips and Tricks To Survive Junior YearDocument5 paginiTips and Tricks To Survive Junior Yearina17_eaglerÎncă nu există evaluări
- Physical/Biologic Development in Early AdolescenceDocument2 paginiPhysical/Biologic Development in Early Adolescenceina17_eaglerÎncă nu există evaluări
- Health System Failure: Malnutrition / Disease ContractionDocument4 paginiHealth System Failure: Malnutrition / Disease Contractionina17_eaglerÎncă nu există evaluări
- According To A Study by MoynihanDocument1 paginăAccording To A Study by Moynihanina17_eaglerÎncă nu există evaluări
- #8 Ipinapahayag Ang Diwa NG Pananalig Sa Mga Katagang "Nananalig Ako Sa Iyo... ", at Hindi Sa "Naniniwala Ako Na... "Document3 pagini#8 Ipinapahayag Ang Diwa NG Pananalig Sa Mga Katagang "Nananalig Ako Sa Iyo... ", at Hindi Sa "Naniniwala Ako Na... "ina17_eaglerÎncă nu există evaluări
- UST Medicine I Schedule 2016-2017Document6 paginiUST Medicine I Schedule 2016-2017ina17_eaglerÎncă nu există evaluări
- Physical/Biologic Development in Early AdolescenceDocument2 paginiPhysical/Biologic Development in Early Adolescenceina17_eaglerÎncă nu există evaluări
- Critically Appraised Topic Title: Notes On The TitleDocument8 paginiCritically Appraised Topic Title: Notes On The Titleina17_eaglerÎncă nu există evaluări
- Application Form AlfabetDocument10 paginiApplication Form Alfabetina17_eaglerÎncă nu există evaluări
- School of Science and Engineering 3rd Year Random NumbersDocument11 paginiSchool of Science and Engineering 3rd Year Random Numbersina17_eaglerÎncă nu există evaluări
- IntentionsDocument1 paginăIntentionsina17_eaglerÎncă nu există evaluări
- Thesis Statement #8: Justice InviolabilityDocument3 paginiThesis Statement #8: Justice Inviolabilityina17_eaglerÎncă nu există evaluări
- A Summary of The ArticleDocument1 paginăA Summary of The Articleina17_eaglerÎncă nu există evaluări
- Interview QuestionsDocument3 paginiInterview Questionsina17_eaglerÎncă nu există evaluări
- A Forty Year Old ManDocument4 paginiA Forty Year Old Manina17_eaglerÎncă nu există evaluări
- Calculating Energy Released When Water and Steam are Spilt on the HandDocument5 paginiCalculating Energy Released When Water and Steam are Spilt on the Handina17_eaglerÎncă nu există evaluări
- LokiDocument21 paginiLokiina17_eaglerÎncă nu există evaluări
- A Summary of The ArticleDocument1 paginăA Summary of The Articleina17_eaglerÎncă nu există evaluări
- Sample Calculations 1. Calculating For Experimental KDocument2 paginiSample Calculations 1. Calculating For Experimental Kina17_eaglerÎncă nu există evaluări
- Acid Peptic Disease (APD)Document73 paginiAcid Peptic Disease (APD)Uma MounaÎncă nu există evaluări
- Medical Specialty Recruitment Applicant Handbook 2021 v1.1Document50 paginiMedical Specialty Recruitment Applicant Handbook 2021 v1.1SamÎncă nu există evaluări
- CPD Book and Patient PictureDocument6 paginiCPD Book and Patient PicturePriyaÎncă nu există evaluări
- Andrew Idoko Group 332 Variant 14 Explain The Pathogenesis of Clinical Signs and Symptoms of Fanconi AnemiaDocument2 paginiAndrew Idoko Group 332 Variant 14 Explain The Pathogenesis of Clinical Signs and Symptoms of Fanconi AnemiadreÎncă nu există evaluări
- Banner HealthcareDocument6 paginiBanner HealthcareValÎncă nu există evaluări
- Ais Student Medical and Health Declaration Form 2023-24Document7 paginiAis Student Medical and Health Declaration Form 2023-24hafizvy6Încă nu există evaluări
- Deficient Knowledge - NCPDocument2 paginiDeficient Knowledge - NCPEmmeline Dycangchon-GarmaÎncă nu există evaluări
- Care of Low Birth Weight BabiesDocument102 paginiCare of Low Birth Weight Babiesvarshasharma050% (2)
- Antimony Gluconate-1Document13 paginiAntimony Gluconate-1humag143100% (3)
- Diabetes Care Guidelines - ADA 2014Document9 paginiDiabetes Care Guidelines - ADA 2014Manish Chandra PrabhakarÎncă nu există evaluări
- Ayurveda Fact Sheet AustraliaDocument2 paginiAyurveda Fact Sheet AustraliaRaviÎncă nu există evaluări
- Nurs 452 Caring Situation Paper 2Document7 paginiNurs 452 Caring Situation Paper 2api-338133673Încă nu există evaluări
- NIV and HFNCDocument16 paginiNIV and HFNCMarceline GarciaÎncă nu există evaluări
- HIV Case (Week 2) - Antao, Alvarez, Hasan, Sanaani, UsmanDocument15 paginiHIV Case (Week 2) - Antao, Alvarez, Hasan, Sanaani, UsmanNUR-HATHI SANAANIÎncă nu există evaluări
- DivocDocument1 paginăDivocCarrackÎncă nu există evaluări
- Katie's story of recovery from anorexiaDocument8 paginiKatie's story of recovery from anorexiaAinjhel CalaraÎncă nu există evaluări
- Calvary Public Bruce Campus MapDocument2 paginiCalvary Public Bruce Campus MapAlana TindaleÎncă nu există evaluări
- YAWAADocument10 paginiYAWAAZyrene CapulongÎncă nu există evaluări
- Stem Cell Therapy For Rotator Cuff InjuriesDocument12 paginiStem Cell Therapy For Rotator Cuff InjuriesAthenaeum Scientific PublishersÎncă nu există evaluări
- 1 1 6 Final DiagnosisDocument1 pagină1 1 6 Final Diagnosisapi-261996621Încă nu există evaluări
- Exploratory Laparotomy Procedure ExplainedDocument5 paginiExploratory Laparotomy Procedure ExplainedChristopher Timothy100% (1)
- Body Art Consent and Health Disclosure Form For Tattooing and PiercingDocument1 paginăBody Art Consent and Health Disclosure Form For Tattooing and PiercingDanielÎncă nu există evaluări
- DR Drug StudyDocument5 paginiDR Drug StudyJosephNawenÎncă nu există evaluări