Documente Academic
Documente Profesional
Documente Cultură
Pages From ASHRAE HVAC Design Manual For Hospitals & Clinics-2013 (Orignal)
Încărcat de
3obaydoof0 evaluări0% au considerat acest document util (0 voturi)
95 vizualizări1 paginăThis document discusses heating, ventilation, and air conditioning (HVAC) design for operating rooms in hospitals and clinics. It addresses sources of cooling loads in operating rooms and strategies for reducing energy usage, such as maintaining a constant air volume but reducing temperature setpoints during unoccupied periods. Current recommendations for air distribution design are based on research analyzing air change rates and velocities, with a maximum recommended face velocity of 25 to 30 feet per minute to avoid disrupting the thermal plume radiating from an open surgical site. Ongoing research questions whether a thermal plume could form at the low wound temperatures observed in orthopedic surgeries.
Descriere originală:
OR cooling loads sharing percent
Titlu original
Pages From ASHRAE HVAC Design Manual for Hospitals & Clinics-2013 (Orignal)
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentThis document discusses heating, ventilation, and air conditioning (HVAC) design for operating rooms in hospitals and clinics. It addresses sources of cooling loads in operating rooms and strategies for reducing energy usage, such as maintaining a constant air volume but reducing temperature setpoints during unoccupied periods. Current recommendations for air distribution design are based on research analyzing air change rates and velocities, with a maximum recommended face velocity of 25 to 30 feet per minute to avoid disrupting the thermal plume radiating from an open surgical site. Ongoing research questions whether a thermal plume could form at the low wound temperatures observed in orthopedic surgeries.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
95 vizualizări1 paginăPages From ASHRAE HVAC Design Manual For Hospitals & Clinics-2013 (Orignal)
Încărcat de
3obaydoofThis document discusses heating, ventilation, and air conditioning (HVAC) design for operating rooms in hospitals and clinics. It addresses sources of cooling loads in operating rooms and strategies for reducing energy usage, such as maintaining a constant air volume but reducing temperature setpoints during unoccupied periods. Current recommendations for air distribution design are based on research analyzing air change rates and velocities, with a maximum recommended face velocity of 25 to 30 feet per minute to avoid disrupting the thermal plume radiating from an open surgical site. Ongoing research questions whether a thermal plume could form at the low wound temperatures observed in orthopedic surgeries.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 1
162 HVAC DESIGN MANUAL FOR HOSPITALS AND CLINICS
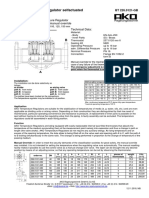
Figure 8-7 Sources of Operating Room Cooling Loads
and maintenance of pressurization. Many hospitals have decided that
the problems and risks of setback exceed the benefits.
8.3.2 Air Distribution A simple way to save energy in ORs is to maintain constant air
volume, but reduce room setpoint during unoccupied periods. This
will reduce reheat and often satisfy a surgeons desire for a cold room.
This strategy should be discussed with the clinical staff.
Current recommendations for air distribution design are based
heavily on the work on Memarzadeh and Manning (2002), which
included an analysis of air change rates as well as air velocity. The air
velocity recommendations are based on the theory of a small thermal
plume radiating up from an open surgical site. This plume, while not
necessarily aseptic, will, in theory, contain only the microbes that are
already present on or in the patient. If the thermal plume is undisturbed,
particles from the air supply and/or from the staff will be diverted and
not directly impact the surgical site. Thus, Memarzadeh and Manning
recommended a maximum face velocity of 25 to 30 fpm [0.13 to
0.15 m/s] so that the supply air will not disrupt the plume. This air
velocity is specified in ANSI/ASHRAE/ASHE Standard 170-2008.
Ongoing ASHRAE research project RP-1397, which is investigating
hospital operating room air distribution to verify CFD predictions of
conditions that sustain the thermal plume, indicates that wound
temperatures in orthopedic surgery are relatively low (80F [26.7C]).
These researchers, therefore, question if a thermal plume could be
created at such a low temperature. This research thus far indicates
S-ar putea să vă placă și
- KJLC Ed09 Sec03 Web200910Document122 paginiKJLC Ed09 Sec03 Web200910NickMoloÎncă nu există evaluări
- PSA Chapter 07Document95 paginiPSA Chapter 07anggit100% (1)
- Short-Term Forecasting Model For Electric Power Production of Small-HydroDocument8 paginiShort-Term Forecasting Model For Electric Power Production of Small-HydroNuno LeaoÎncă nu există evaluări
- STS Data SheetV2017.10Document4 paginiSTS Data SheetV2017.10Syed Furqan RafiqueÎncă nu există evaluări
- Astm E145 PDFDocument2 paginiAstm E145 PDFEnvi Tech0% (1)
- C1046Document9 paginiC1046dinhtung2210Încă nu există evaluări
- Psychrometrics ProblemsDocument10 paginiPsychrometrics ProblemsManish MahadevwalaÎncă nu există evaluări
- DMG - 20-The Heating of Large SpacesDocument55 paginiDMG - 20-The Heating of Large SpacesdanenicÎncă nu există evaluări
- Ashrae 62.2 Rick KargDocument64 paginiAshrae 62.2 Rick KargPS KingÎncă nu există evaluări
- Measumerent GroundingDocument3 paginiMeasumerent GroundingRamesh SrinivasanÎncă nu există evaluări
- Transformer Type & TutorialDocument106 paginiTransformer Type & TutorialHasan Basyaria100% (1)
- 1969 Rockefeller - Fault Protection With A Digital Computer PDFDocument27 pagini1969 Rockefeller - Fault Protection With A Digital Computer PDFOmar Chayña VelásquezÎncă nu există evaluări
- Indoor RMU ManualDocument20 paginiIndoor RMU Manualhardeepsingh_08Încă nu există evaluări
- Facts and Their ControlDocument25 paginiFacts and Their ControlNilesh KhareÎncă nu există evaluări
- NV11B Manual 01 2015Document205 paginiNV11B Manual 01 2015nknfiveÎncă nu există evaluări
- How Is Reactive Power Produced - What Are The Effects of Reactive Power in The Grid - QuoraDocument5 paginiHow Is Reactive Power Produced - What Are The Effects of Reactive Power in The Grid - QuoraMahesh Kumar BhattaÎncă nu există evaluări
- Dissolved Gas Analysis of Transformer: Cellulose Insulation Carbon OxidesDocument2 paginiDissolved Gas Analysis of Transformer: Cellulose Insulation Carbon OxidesheroÎncă nu există evaluări
- Ahsmrw00lna FM100Document9 paginiAhsmrw00lna FM100ibrahimÎncă nu există evaluări
- Interference of Power Line With Communication SystemDocument4 paginiInterference of Power Line With Communication SystemUsama Shafqat0% (1)
- Distributed Power Flow Controler (DPFC)Document44 paginiDistributed Power Flow Controler (DPFC)rajesh_d84Încă nu există evaluări
- SCADA Notes by Vijay Kumar Dubey (UNIT 1, 2 & 3)Document42 paginiSCADA Notes by Vijay Kumar Dubey (UNIT 1, 2 & 3)Muzammil KhanÎncă nu există evaluări
- Measurement of High VoltageDocument2 paginiMeasurement of High VoltageShahzaid AhmadÎncă nu există evaluări
- E&MDocument37 paginiE&Mrishabhbhagat100% (1)
- (Catalog Microturbine) Elliott 243694440 Ta 100 PDFDocument2 pagini(Catalog Microturbine) Elliott 243694440 Ta 100 PDFppourmoghaddamÎncă nu există evaluări
- Electrical FactsDocument8 paginiElectrical FactsS Bharadwaj ReddyÎncă nu există evaluări
- Power Line Carrier Detailed DocumentDocument51 paginiPower Line Carrier Detailed DocumentmuzammiliqbalÎncă nu există evaluări
- Hazem-Thesis-lowpass Broadband Harmonic Filter DesignDocument213 paginiHazem-Thesis-lowpass Broadband Harmonic Filter DesignSumindak Gultom100% (1)
- 3 Discrimination by Both Time and CurrentDocument9 pagini3 Discrimination by Both Time and CurrentEBEÎncă nu există evaluări
- Cymgrd 6.5 Reference Manual and Users Guide: July 2011Document126 paginiCymgrd 6.5 Reference Manual and Users Guide: July 2011Diego TerrazasÎncă nu există evaluări
- Protecciones de Tierra de TransformadoresDocument9 paginiProtecciones de Tierra de Transformadoresmaidenheavy1Încă nu există evaluări
- 0613CT0001 PDFDocument180 pagini0613CT0001 PDFhimanshu yadavÎncă nu există evaluări
- Performance Evaluation of GeneratorTransformer Unit Overall Differential ProtectionDocument9 paginiPerformance Evaluation of GeneratorTransformer Unit Overall Differential ProtectionAdam IbnuÎncă nu există evaluări
- Manual Book F6Document44 paginiManual Book F6Adib Darul QuthniÎncă nu există evaluări
- 04 0800 HVDC Plenary RashwanDocument24 pagini04 0800 HVDC Plenary RashwanDante FilhoÎncă nu există evaluări
- Synchronization Checklist PDFDocument8 paginiSynchronization Checklist PDFAdhyartha KerafÎncă nu există evaluări
- Lightning ParametersDocument13 paginiLightning ParametersJorge Alberto Ayala SanchezÎncă nu există evaluări
- Deration FactorDocument3 paginiDeration FactorAshutosh Kumar100% (1)
- Altitude Corrections For External Insulation Design Iec Standards and Engineering Applications 92 PaperDocument8 paginiAltitude Corrections For External Insulation Design Iec Standards and Engineering Applications 92 PaperDrakhoÎncă nu există evaluări
- Sistema de ProteccionDocument124 paginiSistema de Proteccionhector retuerto ramosÎncă nu există evaluări
- IEEE STD 1329-2010 IEEE Standard Method For Measuring Transmission Performance of Speakerphones PDFDocument101 paginiIEEE STD 1329-2010 IEEE Standard Method For Measuring Transmission Performance of Speakerphones PDFGreg Tsai100% (1)
- Motor Protection ToshibaDocument24 paginiMotor Protection ToshibaAriesFranandaPanjaitanÎncă nu există evaluări
- Calibration of Power Quality and Energy MetersDocument8 paginiCalibration of Power Quality and Energy MetersmarkgaloÎncă nu există evaluări
- Nema Ics 3.1 2019 WatermarkedDocument47 paginiNema Ics 3.1 2019 WatermarkedЕлена МаркеловаÎncă nu există evaluări
- สรุปความแตกต่าง 64 and 51NDocument1 paginăสรุปความแตกต่าง 64 and 51NRanchida PhuangphisÎncă nu există evaluări
- Aplicacion Tecnica - Paper N°4 - Circuit Breakers Inside LV Switchboards (Ingles) (1SDC007103G0201)Document56 paginiAplicacion Tecnica - Paper N°4 - Circuit Breakers Inside LV Switchboards (Ingles) (1SDC007103G0201)Eduardo ZapataÎncă nu există evaluări
- Shunt Reactor 0420101Document16 paginiShunt Reactor 0420101emy1188Încă nu există evaluări
- Effect of Capacitor Compensator On A Transmission LineDocument16 paginiEffect of Capacitor Compensator On A Transmission LineOhanyelu Okeoma DanielÎncă nu există evaluări
- Switchgear and Protection: Seminar Adaptive RelayingDocument16 paginiSwitchgear and Protection: Seminar Adaptive RelayingrajumohandasÎncă nu există evaluări
- Lab Notes Overcurrent GroundFault Protection v1Document7 paginiLab Notes Overcurrent GroundFault Protection v1srinivasaphanikiranÎncă nu există evaluări
- Wireless Power Transfer SynopsisDocument3 paginiWireless Power Transfer Synopsisa d100% (1)
- Patna Merto ProjectDocument37 paginiPatna Merto ProjectSonu RdÎncă nu există evaluări
- NUREG-0050 Recommendations Related To Browns Ferry FireDocument96 paginiNUREG-0050 Recommendations Related To Browns Ferry Firescott56794Încă nu există evaluări
- Approved Final Draft Spec TI SPC RCC SCADA 0134Document101 paginiApproved Final Draft Spec TI SPC RCC SCADA 0134Anurag SanodiaÎncă nu există evaluări
- Superimposed Components Based Sub-Cycle Protection of Transmission LinesDocument6 paginiSuperimposed Components Based Sub-Cycle Protection of Transmission LinesFabien CallodÎncă nu există evaluări
- App Note DC DC Stability V2Document17 paginiApp Note DC DC Stability V2ranjitheee1292Încă nu există evaluări
- 2013-05 LightingElectricalDocument45 pagini2013-05 LightingElectricalNERO_s_ALI6656Încă nu există evaluări
- Informe Del Departamento de Energía de Estados Unidos: "Soluciones de Energía Resiliente para La Red de Puerto Rico"Document59 paginiInforme Del Departamento de Energía de Estados Unidos: "Soluciones de Energía Resiliente para La Red de Puerto Rico"El Nuevo DíaÎncă nu există evaluări
- Saylors-Wind Farm Collector System GroundingDocument16 paginiSaylors-Wind Farm Collector System GroundingkcirrenwodÎncă nu există evaluări
- ASHRAE JOURNAL - Reducing Risks of SurgeryDocument6 paginiASHRAE JOURNAL - Reducing Risks of SurgeryBen MusimaneÎncă nu există evaluări
- 2012 Operating Room Design Manual: Heating and Air ConditioningDocument1 pagină2012 Operating Room Design Manual: Heating and Air ConditioningJosephRusselVizmanosÎncă nu există evaluări
- CHAPTER 9 Room Ventilation SystemsDocument6 paginiCHAPTER 9 Room Ventilation SystemsJuan IntriagoÎncă nu există evaluări
- ASHRAE Final Operating Room 508 PDFDocument13 paginiASHRAE Final Operating Room 508 PDFSilisteanu AndreiÎncă nu există evaluări
- A Numerical Investigation About The Air Quality in A Surgical Room at A HospitalDocument135 paginiA Numerical Investigation About The Air Quality in A Surgical Room at A HospitalHoàn LộcÎncă nu există evaluări
- Special Departmental HVAC Issues: Operating RoomsDocument6 paginiSpecial Departmental HVAC Issues: Operating RoomshadianatyaÎncă nu există evaluări
- The New Technology Behind COVID-19 RNA Vaccines and What This Means For Future OutbreaksDocument5 paginiThe New Technology Behind COVID-19 RNA Vaccines and What This Means For Future OutbreaksMike ReyesÎncă nu există evaluări
- Topic: Bioenergetics: Living OrganismsDocument9 paginiTopic: Bioenergetics: Living OrganismsNaiomiÎncă nu există evaluări
- UCA - BST.F.2019.18 (Assingment 01)Document11 paginiUCA - BST.F.2019.18 (Assingment 01)shehan harshithaÎncă nu există evaluări
- Experiment No 8 DP 2Document28 paginiExperiment No 8 DP 2Drw ArcyÎncă nu există evaluări
- BITZER Output Data: Created On: 16/05/2017 16:44:22Document5 paginiBITZER Output Data: Created On: 16/05/2017 16:44:22Hasan Syaiful IÎncă nu există evaluări
- Past-Papers 2019 03 29 09 20 38521 2019 03 29 19 58 PDFDocument51 paginiPast-Papers 2019 03 29 09 20 38521 2019 03 29 19 58 PDFAR Video ProductionÎncă nu există evaluări
- Fundamentals of Air Conditioning SystemsDocument387 paginiFundamentals of Air Conditioning Systemsberija1968Încă nu există evaluări
- W7 320 Furnace - Technology PDFDocument104 paginiW7 320 Furnace - Technology PDFAtiq Ur RehmanÎncă nu există evaluări
- 51371180104Document21 pagini51371180104GuillermoadairÎncă nu există evaluări
- Schematic Mounting of HERZDocument7 paginiSchematic Mounting of HERZRazvan GabyÎncă nu există evaluări
- Impact of Fire On Steel Reinforcement of R.C.C StructuresDocument18 paginiImpact of Fire On Steel Reinforcement of R.C.C StructuresLayali90Încă nu există evaluări
- CMAP Science 8Document5 paginiCMAP Science 8Janeyah Marie FuentesÎncă nu există evaluări
- Tar Removal With A Wet Electrostatic Precipitator (Esp) A Parametric StudyDocument8 paginiTar Removal With A Wet Electrostatic Precipitator (Esp) A Parametric StudyDeepankar KhawasÎncă nu există evaluări
- AKO Temperature Regulator SelfactuatedDocument1 paginăAKO Temperature Regulator SelfactuatedsudhirÎncă nu există evaluări
- 3.gaseous StateexerciseDocument50 pagini3.gaseous StateexerciseGomes RibeiroÎncă nu există evaluări
- Paddle Blade (Radial Blade) Forward Curved (Multi-Vane) Backward CurvedDocument2 paginiPaddle Blade (Radial Blade) Forward Curved (Multi-Vane) Backward CurvedEarl De La ChinaÎncă nu există evaluări
- Stefan-Boltzmann Law: Lab ReportDocument12 paginiStefan-Boltzmann Law: Lab ReportZeenat RanaÎncă nu există evaluări
- Energy and ChemistryDocument27 paginiEnergy and ChemistryterantejkÎncă nu există evaluări
- PHYS 1401 General Physics I Experiment 12 Specific Heat: H H I, H F C C F I, CDocument4 paginiPHYS 1401 General Physics I Experiment 12 Specific Heat: H H I, H F C C F I, CHafidzSecretzboyzÎncă nu există evaluări
- Y8 2 Heating and CoolingDocument77 paginiY8 2 Heating and Coolingqueenjose100% (1)
- G-R 25Document27 paginiG-R 25Duncan VanderwallÎncă nu există evaluări
- Center of Mass and The Motion of A SystemDocument13 paginiCenter of Mass and The Motion of A SystemNitin SharmaÎncă nu există evaluări
- The Art of Doing Ebook PDFDocument242 paginiThe Art of Doing Ebook PDFVamsiÎncă nu există evaluări
- Amende 2007Document6 paginiAmende 2007Warren PuthÎncă nu există evaluări
- Mechanical Systems BuildingsDocument6 paginiMechanical Systems BuildingsrasheedillikkalÎncă nu există evaluări