Documente Academic
Documente Profesional
Documente Cultură
Pleural Infection - Past, Present, and Future Directions
Încărcat de
Camilo VidalTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Pleural Infection - Past, Present, and Future Directions
Încărcat de
Camilo VidalDrepturi de autor:
Formate disponibile
Series
Pleural disease 1
Pleural infection: past, present, and future directions
John P Corcoran, John M Wrightson, Elizabeth Belcher, Malcolm M DeCamp, David Feller-Kopman, Najib M Rahman
Pleural space infections are increasing in incidence and continue to have high associated morbidity, mortality, and need Lancet Respir Med 2015;
for invasive treatments such as thoracic surgery. The mechanisms of progression from a non-infected, pneumonia- 3: 56377
related eusion to a conrmed pleural infection have been well described in the scientic literature, but the route by This is the rst in a Series of
two papers about pleural disease
which pathogenic organisms access the pleural space is poorly understood. Data suggests that not all pleural infections
can be related to lung parenchymal infection. Studies examining the microbiological prole of pleural infection inform See Editorial page 497
antibiotic choice and can help to delineate the source and pathogenesis of infection. The development of radiological See Comment page 505
methods and use of clinical indices to predict which patients with pleural infection will have a poor outcome, as well as See Online for a discussion with
Nick Maskell and Najib Rahman
inform patient selection for more invasive treatments, is particularly important. Randomised clinical trial and case
Oxford Centre for Respiratory
series data have shown that the combination of an intrapleural tissue plasminogen activator and deoxyribonuclease
Medicine (J P Corcoran MRCP,
therapy can potentially improve outcomes, but the use of this treatment as compared with surgical options has not been J M Wrightson DPhil,
precisely dened, particularly in terms of when and in which patients it should be used. N M Rahman DPhil) and
Department of Cardiothoracic
Surgery (E Belcher PhD), Oxford
Introduction clinical and laboratory research, and future areas of
University Hospitals NHS Trust,
Despite advances in medical diagnostic and therapeutic investigation for management of this disorder. Oxford, UK; University of
strategies, pleural infection (empyema or complex Oxford Respiratory Trials Unit,
parapneumonic eusion) is an important problem Pathophysiology Churchill Hospital, Oxford, UK
(J P Corcoran, J M Wrightson,
worldwide that continues to be associated with substantial Parapneumonic eusions occur in up to half of all
N M Rahman); NIHR Oxford
morbidity and mortality. This disorder was reliably cases of community-acquired pneumonia, with about Biomedical Research Centre,
described by Hippocrates more than two millennia ago 10% of these eusions becoming complex due to University of Oxford, Oxford,
and has claimed many lives since that time, including co-infection of the pleural space.19,20 The initial UK (J M Wrightson,
N M Rahman); Division of
those of medical luminaries such as Guillaume formation of a parapneumonic eusion is thought to be Thoracic Surgery,
Dupuytren (17771835) and William Osler (18491919). caused by increased permeability of the visceral pleural Northwestern Memorial
The basic principles of treating pleural infection, which membranes and leakage of interstitial uid in response Hospital, Northwestern
include adequate drainage of the infected uid collection, to inammation of the underlying lung parenchyma. University Feinberg School of
Medicine, Chicago, IL, USA
nutritional support, and an appropriate antibiotic therapy, The promotion of neutrophil migration together with (Prof M M DeCamp MD); and
have remained constant since the mid 20th century. the release of pro-inammatory cytokines, including Division of Pulmonary and
The incidence of pleural infection in both adult and interleukin-6, interleukin-8, and tumour necrosis Critical Care Medicine, Johns
paediatric populations continues to rise inexorably.15
Postulated reasons for this rise include an improvement
in clinical awareness and diagnostics, a replacement Key messages
phenomenon associated with widening use of The incidence of pleural infection continues to rise and this disease remains
multivalent pneumococcal vaccines,3,6,7 and a vulnerable associated with a poor clinical outcome, with up to 20% of patients requiring surgery
ageing population living with chronic disease. One in or dying
ve patients will need surgical intervention to adequately The process by which bacteria translocate the infected lung and multiply in the pleural
treat their pleural infection,8,9 whereas the 1-year mortality space is incompletely understood, but there is an increasing understanding of the
from the disorder has remained steady at about 20% for inammatory pathways associated with progression from simple to complex,
more than two decades.5,810 Of particular concern is that brinous infected eusion
the greatest increase in caseload is in patients aged older A score to predict clinical outcome at baseline in pleural infection has been derived and
than 65 years1 and immunocompromised patients, might be helpful in the future to plan treatment escalation and invasive interventions
whose mortality from pleural infection is above 30%,1,8,9,11 The microbiological prole of pleural infection suggests a dierent set of organisms to
related to frail health and comorbidity. There are any those seen in pneumonia, with oropharyngeal and microaspiration potential sources
number of potential reasons for the failure of treatments Conventional microbiological analysis is only slightly sensitive for the identication of
to have a substantial and lasting eect on key clinical causative organism, and this can be improved by the inoculation of pleural uid into
outcomes. These reasons might include variability in culture media bottles, and potentially in the future by the use of molecular
clinical practice and disagreement about how these microbiological techniques
patients are best managed,1217 despite the availability of Intrapleural tPA and DNase has been shown to signicantly improve drainage and can
consensus guidelines.5,18 have important eects on reducing surgical requirement and hospital stay
This Series paper addresses our understanding of Surgery remains a key treatment modality in selected cases, but the precise surgical
pleural infection, specically its pathophysiology, diag- method of choice, patient selection, and timing are not well dened
nosis, and treatment, together with developments in
www.thelancet.com/respiratory Vol 3 July 2015 563
Series
Hopkins Hospital, Baltimore,
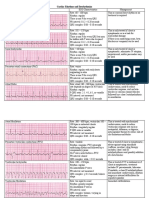
Proposed mechanism of pleural infection development in association with pneumonia
MD, USA (D Feller-Kopman MD)
Potential routes of bacterial Pneumonia-associated
Correspondence to:
entry into the pleural space inammation
Dr Najib M Rahman,
Release of pleural proinammatory cytokines
Oxford Centre for Respiratory
(eg, IL-6, IL-8, MCP, TNF, VEGF) within pleural space
Medicine, Churchill Hospital,
Oxford OX3 7LE, UK Development of sterile simple
najib.rahman@ndm.ox.ac.uk parapneumonic eusion
Inux of neutrophils and
monocytes into pleural space Increased pleural permeability
Pleural uid accumulation
1 Transpleural from adjacent consolidated lung
Pronounced role of oral anaerobes Bacterial translocation Characteristic
into pleural space Bacterial replication biochemistry
and neutrophil phagocytosis of pleural infection
2 Visceral pleural defects or stulae (low pH, low glucose,
Lung cancer, post radiotherapy, postoperative high LDH)
Fibrin deposition
(eg, broncial stump dehiscence) Suppression of septations, pleural thickening
Necrotising pneumonia, tuberculosis, fungal brinolysis (raised PAI)
Development of TGF, PDGF
pleural infection
Fibrous inelastic pleural peel
3 Haematogenous spread (bacteraemia)
5 Spread from mediastinum Uncertain whether more probable in presence of
Oesophageal rupture or other pre-existing uid (eg, hepatic hydrothorax)
4 Penetrating injury across parietal visceral pleura
Trauma
Iatrogenic (eg, post chest tube insertion)
6 Transdiaphragmatic spread
Intra-abdominal infections
Transcolonic followed by transdiaphragmatic
bacterial translocation (eg, alcoholic cirrhosis)
Figure 1: Development of pleural infectionpossible routes and mechanisms
IL-6=interleukin-6. IL-8=interleukin-8. MCP=monocyte chemoattractant protein. TNF=tumour necrosis factor-. VEGF=vascular endothelial growth factor.
TGF=tumour growth factor-. PDGF=platelet-derived growth factor. LDG=lactate dehydrogenase. PAI=plasminogen activator inhibitor.
factor- (TNF), result in the development of capable of translocating through visceral mesothelial
intercellular gaps between pleural mesothelial cells21,22 cells from the parenchyma to pleural space, thereby
that facilitate the accumulation of excess pleural uid. instigating the inammatory cell and cytokine responses
During this early exudative stage, the uid is associated with pleural infection.
uncomplicated and shows no microbiological or As bacteria multiply, various changes occur within the
biochemical features of pleural infection. In most pleural space (gure 1), resulting in the characteristic
cases, the parapneumonic eusion will simply resolve clinical and biochemical features associated with a
with appropriate antibiotic therapy for the underlying complicated parapneumonic eusion, so-called because
pneumonia. of the adverse clinical outcomes seen unless the
The reasons why and means by which secondary collection is drained. Bacterial metabolism and
bacterial invasion of the pleural space occurs are neutrophil phagocytic activity result in the production
incompletely understood, a knowledge gap that is likely of lactic acid and carbon dioxide production, causing in
to be one of the barriers to therapeutic progress. turn a decrease in pleural uid pH and glucose
Although studies in animals frequently rely on articial concentration,28,29 both of which are clinically used as
infection of the pleural space via a percutaneous route laboratory markers of pleural infection.5,30 The continued
(rather than due to co-infected lung parenchyma), release of inammatory cytokines such as interleukin-6,
practical and ethical limitations exist in clinical research, interleukin-8, TNF, vascular endothelial growth factor
notably the need for repeated invasive sampling to study (VEGF), and monocyte chemotactic protein (MCP),
the evolution of pleural infection.23 An additional which are all linked to ongoing excess uid production,
complication is that pleural infection can arise occurs together with rising levels of brinolysis
spontaneously without underlying lung consolidation,2426 inhibitors such as tissue plasminogen activator inhibitor
implying contamination of the pleural space by another (PAI).31 This depression of brinolytic activity is unique
route (eg, haematogenous seeding of bacteria). to infected eusions,31 resulting in brin deposition that
Nonetheless, a study using a murine in-vivo model both coats the visceral and parietal pleural surfaces and
together with in-vitro cell line studies27 has shown that divides the space into separate pockets. Finally, purulent
Streptococcus pneumonia (S pneumonia), a common uid (empyema) develops in the context of bacterial and
cause of pleural infection in both adults and children, is leucocytic cell death and lysis.
564 www.thelancet.com/respiratory Vol 3 July 2015
Series
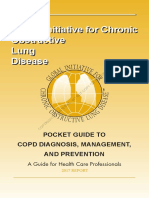
Clinical presentation consistent with pleural infection Risk stratication using baseline
(eg, fever, pleurisy, malaise, dyspnoea) physiological and biochemical parameters
Diagnostic imaging studies
Thoracic ultrasound Computed tomography
Risk stratication using thoracic Risk stratication using CT
ultrasoundeg, septations, eg, loculation, pleural
pleural thickening thickening/enhancement
Diagnostic thoracentesis with guidance
of thoracic ultrasound
Conrmed pleural infectioneg, pleural uid pH <72 or glucose <3 mmol/L;
Nucleic acid amplication frankly purulent Intermittent therapeutic
techniques for rapid thoracentesis
bacterial identication
Pleural uid for diagnostic Drainage of infected pleural
microbiology (plain and collection Thoracoscopic (surgical/
blood culture bottle culture) medical) drainage in selected
Biopsies of parietal pleura
(eg, stratied as high risk)
to increase diagnostic yield
cases
Modify antibiotics on the basis
of positive culture results and
Risk stratication on clinical response
Early combination intrapleural
basis of bacteriology Chest tube insertion with therapy in selected cases
Broad spectrum antibiotics based guidance of thoracic
on local practice and microbiology ultrasound
Intrapleural antibiotics High volume pleural irrigation
Monitor response to initial treatment during 4872 h
Treatment success: ie, clinical, radiographic Treatment failure: eg, signicant
and biochemical recovery residual collection, ongoing sepsis
Medical thoracoscopy Escalation of antibiotic therapy Referral for surgical intervention
as rescue therapy
Combination intrapleural therapy
(tPA + DNase) if surgery either
inappropriate or delayed
Choice of surgical intervention Surgical drainage and obliteration
(eg, local vs general anaesthetic; of infected pleural space
partial debridement vs full (video-assisted thoracoscopic
decortication) surgery or thoracotomy)
Figure 2: Diagnostic and therapeutic pathway for the patient with pleural infection
Black boxes, text & arrows represent established treatment pathway; red boxes, text & arrows represent potential future directions for clinical care and research.
tPA=tissue plasminogen activator.
As the infection progresses from an acute to a varies greatly between individuals, with data from
chronic state, broblast proliferation occurs along the rabbit and mouse models of pleural infection or
established brin matrix. This proliferation creates brosis suggesting a role for signalling proteins such
dense inelastic septations and collagenous thickening as platelet-derived growth factor (PDGF) and
within and around the pleural cavity, walling o transforming growth factor- (TGF),32 which oers
residual infection but also restricting lung expansion the prospect of a novel therapeutic target for future
and compliance. The rate at which this change occurs investigation.33 Although surgical intervention is
www.thelancet.com/respiratory Vol 3 July 2015 565
Series
almost certainly needed by this point to ensure Once the diagnosis of pleural infection has been
adequate clearance of infected material from the conrmed, standard treatment consists of drainage of the
pleural space, clinical outcomes are unpredictable, infected collection, usually via a percutaneous chest drain,
with some patients having no long-term sequelae and and broad-spectrum antibiotics.5 A small but substantial
others showing permanent impairment of lung proportion of patients will either not improve with this
function. conservative approach and need surgical intervention, or
will die within a year of their initial diagnosis.8,9 The
Diagnosis and outcome prediction identication of individuals who are at increased risk of
The diagnosis and treatment of pleural infection morbidity and mortality early in their treatment is of
depends on the awareness of the clinician assessing the crucial importance so that appropriate resources can be
patient (gure 2). An absence of improvement despite used to improve clinical outcome. However, clinicians
adequate antibiotic therapy for apparently uncomplicated have no reliable means by which to risk stratify patients
(assumed by the clinician) pneumonia or presentation with pleural infection. Studies on this topic have
with a pleural eusion alongside symptoms that vary implicated features including uid purulence, loculation
from those specic for infection (fever, rigours) to those of or septations within a collection, low pleural uid white
non-specic for infection (malaise, anorexia) should all cell count, pathogenic organism, and delayed presentation
prompt suspicion for a potential diagnosis of pleural and drainage, as all having a potential eect on
infection. This situation is especially true in elderly and outcome.12,37,3941 However, none of the studies were pros-
nursing-home patients who often present with an pectively validated or provided an easily accessible,
indolent course characterised by a so-called failure specic, and systematic approach to patient assessment.
to thrive, anaemia, and weight loss.34 The delayed In view of the increasingly widespread use of bedside
recognition and subsequent treatment of pleural thoracic ultrasound by respiratory clinicians, particular
infection inevitably negatively aects morbidity and interest in sonographic surrogates of poor response to
mortality,10,12 inspiring the often repeated maxim that the medical therapy in pleural infection exists.42,43 Two
sun should never set on a parapneumonic eusion. studies40,41 have directly addressed such surrogates and
In the absence of any reliable alternative means to have suggested that the presence of septations is
determine which parapneumonic eusions are either predictive of poor outcome in pleural infection. This
already infected or will probably become infected, probably supports the suggestion that the septations in
pleural uid sampling is always indicated. Current pro-brotic infected pleural collections lead to diculty
guidelines5 strongly recommend the use of thoracic in percutaneous tube drainage, and therefore ineective-
ultrasound to guide any intervention for pleural uid ness of medical therapy. However, results from these
(gure 2). With evidence showing how thoracic two studies are weak due to their unblinded design.
ultrasound reduces the risk of iatrogenic complications,35,36 Consequently, more prospective studies are needed to
blind thoracentesis in this clinical scenario is almost elucidate the clinical meaning and relevance of
impossible to justify. Ultrasound guidance is additionally septations within the infected pleural space as identied
useful in the context of suspected infection when by thoracic ultrasound. Furthermore, ultrasound is
collections might be septated, in small volume, or operator-dependent, and the expertise of the individual
multi-loculated. clinician at the bedside is probably an additional con-
The diagnosis of pleural infection can be conrmed if founding factor when applying this technique on a wide
appropriate laboratory investigations are requested and basis to guide clinical care.
correctly interpreted. If pus or microbiologically positive A prediction model,44 reported in 2014, derived from
uid (by Gram staining or culture) is clearly noted, two large prospective randomised trials8,9 of patients with
diagnosis conrmation is straightforward. However, pleural infection, oers promise in potentially allowing
almost half of infected pleural eusions turn out to the risk stratication of patients with pleural infection,
be microbiologically negative.37 The potential delay in and is being studied by a large multicentre observational
waiting for a positive culture result when infection is study (ISRCTN 50236700) to ascertain its validity. Whether
already suspected is clinically unacceptable. Therefore, this or another outcome prediction model will have any
in most cases, clinicians use pleural uid pH and inuence on either morbidity or mortality from pleural
glucose concentration as biochemical surrogates of infection is unclear. However, the availability of a validated
bacterial infection to make a diagnosis.5,30 Pleural uid risk stratication score will certainly have an eect on the
pH is most sensitive in isolation, but is also prone to way patients with a pleural infection are managed as has
instability and contamination depending on how and been the case in other respiratory diseases.
when it is analysed;38 if concerns regarding the accuracy
of a pH result exist, then pleural uid glucose can be Microbiological overview
used as a more stable and reliable measure. Ultimately, Development of pleural infection
any test should be interpreted by taking into account the The means by which bacteria enter the pleural space is
clinical presentation. being investigated.27 In view of the association between
566 www.thelancet.com/respiratory Vol 3 July 2015
Series
pleural infection and pneumonia, bacterial spread across Transient bacteraemia, together with the impaired
the visceral pleura from consolidated lung probably has reticuloendothelial phagocytic activity associated with
a substantial role in pleural infection. Such a concept, cirrhosis, are proposed to cause bacterial seeding of the
however, might be a considerable oversimplication hepatic hydrothorax.Transcolonic translocation followed
since the two diseases have substantially dierent by transdiaphragmatic translocation of bacteria to the
bacteriological patterns. pleural space is another possible mechanism for pleural
Animal models of pleural infection provide useful space entry.
insight into the development of infection. Experimental More studies are needed to clarify the ability of dierent
inoculation of bacteria directly into the pleural space of bacteria to enter and cause disease within the pleural
rabbits creates biochemically and histocytologically space, particularly in view of the dierent bacteriological
similar patterns of pleural infection to human disease, features of pleural infection and pneumonia. Whereas
although substantial challenges remain in closely S pneumoniae and atypical organisms (ie, Mycoplasma
modelling human pleural infection. One challenge is that and Legionella spp) account for most community-
bacterial inoculation alone often results in either bacterial acquired pneumonia, the Streptococcus milleri (S milleri)
clearance or animal death from sepsis unless additional group, Staphylococcus aureus (S aureus), and aerobic
experimental steps are taken to allow a localised empyema Gram-negative organisms have a much larger role in
to develop. For example, nutrient broth has been injected patients with pleural infection, especially in pleural
together with the bacterial inoculant (to encourage infection acquired in hospital (see section on overall
bacterial replication within the pleural space), parenteral bacteriology). Vaccine studies in humans suggest that
antibiotics have been given (to prevent animal death from pneumococcal serotypes vary in their propensity to cause
sepsis),45 and other techniques have been used to cause pleural infection.47 Additionally, experimental evidence
pleural inammation (thereby creating an initial exudative suggests that host responses (including cytokine release
pleural eusion, proposed to sustain initial bacterial prole and mesothelial cell death) vary depending on
replication).29,46 The second challenge is that these models bacterial species, after these have gained access to the
of disease failed to reproduce the initial pneumonia often pleural space.48,49
associated with pleural infection. However, one mouse
model of pleural infection has successfully used intranasal Overall bacteriology
inoculation with S pneumoniae to cause consolidation and Large multicentre studies have characterised the
pleural infection, with a pattern similar to human bacteriological features of pleural infection and show key
disease.27 Early brinous adhesions were noted, as were dierences between community-acquired and hospital-
characteristic visceral pleural mesothelial cell changes acquired infections. Bacterial isolate data from the MIST1
(and eventual cell necrosis) and bacteria in close proximity study,8,37 the largest multicentre randomised trial of pleural
to the submesothelial cell layer. Importantly, in-vitro infection in adults with 454 participants, showed that
studies using mesothelial cells and confocal microscopy community-acquired infection in adults is most commonly
suggested that S pneumoniae crosses the mesothelial cell streptococcal (52%), with 24% from the S milleri group
layer using an intracellular route, rather than a paracellular (Streptococcus anginosus-constellatus-intermedius) and 21%
route. These ndings, taken together, are highly suggestive from S pneumonia, 20% from anaerobic microbes, 10%
of a transpleural spread of infection, at least for from S aureus, and 8% from Enterobacteriaceae (including
S pneumoniae in this mouse model of disease. Escherichia coli and Proteus spp). Hospital-acquired
With increasing use of cross-sectional imaging, pleural infection in adults is most commonly caused by S aureus
infection without adjacent consolidation has become a (35%), particularly methicillin-resistant S aureus, 18%
recognised event, although it only occurs in a few cases from Enterobacteriaceae, 18% from Streptococcus spp
(about 30% in an unreported analysis of the MIST2 (7% from the S milleri group, 5% from S pneumoniae), 12%
cohort9). This pattern of disease suggests that other from Enterococcus spp, and 8% from anaerobes. Similar
mechanisms are also responsible for bacterial entry into patterns have been observed in other studies9,50 and
the pleural space, including haematogeneous spread, highlight the importance of including methicillin-resistant
transdiaphragmatic spread, or spread from oesophageal S aureus and resistant Gram-negative coverage in empirical
or mediastinal disease (gure 1). antibiotic choice for hospital-acquired infection. Pleural
Animal models of pleural infection show that tuberculosis causes a type 4 hypersensitivity reaction
sustained pleural space bacterial replication is more within the pleural space, and is a common cause of pleural
likely in the presence of uid. Patients with pre-existing eusion in high-prevalence settings, but is beyond the
pleural eusions might therefore be at higher risk of scope of this Series paper.
pleural infection than those patients without pre- Age-dependent variation in the type of bacterial
existing pleural eusions. Indeed, spontaneous bacterial infection has also been shown, with a strikingly higher
empyema is increasingly recognised as a complication rate of S pneumoniae (up to 85%) and Streptococcus
of hepatic hydrothorax in patients with cirrhosis, pyogenes in children.51,52 Although patterns of pleural
analogous to spontaneous bacterial peritonitis.24,26 infection in adults are similar in the UK,9,37 Scandinavia,53
www.thelancet.com/respiratory Vol 3 July 2015 567
Series
Brims et al Meyer et al Meyer et al Lin et al Maskell et al Rahman et al Marks et al
(2014)50 (2011)53 (2011)53 (2010)55 (2006)37 (2011)9 (2012)12
Country Australia Denmark Taiwan Taiwan UK UK UK
Total number of patients or isolates 713 patients 291 isolates 139 isolates 169 isolates 396 isolates 97 isolates 406 patients
Staphylococcus aureus 12 18 6 14 16 16
Viridans streptococci 9 25 27 18
Streptococcus milleri group 7 19 21 21 4
Streptococcus pneumoniae 7 4 19 25 10
Anaerobes 17 27 18 7 6
Haemophilus inuenzae 1 4
Enterobacteriaceae 12 34 9 9 6
Klebsiella pneumoniae 3 24 24
Enterococcus spp 4 1 3 3
Pseudomonas spp 5 2 2 4
Yeasts 2 2
Mycobacterium spp 1 3 9
Values shown are expressed as % of isolates (or patients). =not reported.
Table: Representative bacteriological analysis from large international studies of pleural infection
and Australia,50 substantial geographical variation occurs vaccine) has added six further serotypes (1, 3, 5, 6A, 7F,
in Asia, where Klebsiella pneumoniae is often the most and 19A), and the consequent eects on pleural infection
common pathogen, causing up to 25% of cases (table).54,55 will be of interest for the health-care community,
Patient risk stratication might be achieved by although preliminary data have not shown an eect on
knowledge of bacterial causes, since specic mortality rates of pleural infection.62
proles are associated with each bacterial pattern. One
study showed that one-year mortality values varied Oropharyngeal commensals
depending on bacterial subtype: 17% with Streptococcal The role of oropharyngeal bacteria in pleural infection
spp, 20% with anaerobes, 45% with Gram-negative has long been recognised, particularly those bacteria
bacteria, 44% with S aureus, and 46% with mixed aerobic reported in the gingival crevices. Studies from the
bacteria.37 These ndings appear to hold true beyond the 1920s investigated the polymicrobial anaerobic and
confounding eects of whether infection was community facultatively anaerobic bacteria seen in lung abscesses
or hospital acquired; however, they do not provide and empyema. Noting these bacteria to be very similar
denitive evidence that the organisms are the cause of to gingival crevice bacteria, Smith63 inoculated the
the variation in mortality. trachea of animals with human periodontal material,
successfully causing lung abscess and empyema. This
Pneumococcal disease suggested that aspiration of these bacteria probably has
Most studies suggest that the incidence of pneumococcal a role in disease development.
infections have increased in the past 1015 years.56,57 An The S milleri group of bacteria are the most frequent
emergence of virulent serotypes, including serotypes 1, cause of community-acquired pleural infection and are
7F, and 19A, associated with pleural infection has also facultatively anaerobic commensals of the oropharynx.
taken place.58,59 One study suggested a four-fold increase They are infrequent causes of pneumonia and their
in serotype 19A,59 which is particularly associated with overrepresentation in pleural infection is therefore of
prolonged duration of fever, need for intensive care interest. Nucleic acid amplication techniques (NAAT)
admission, and surgical treatment for pleural infection.60 have reported co-localisation of S milleri and anaerobes
The original seven-valent pneumococcal conjugate in pleural infection,64 and experimental evidence
vaccine introduced in the USA in 2000 covered suggests that they are synergistic.65 Routine laboratory
serotypes 4, 6B, 9V, 14, 18C, 19F, and 23F. Studies culturing of pleural uid samples probably under-
have suggested that widespread vaccination programmes estimates anaerobes, given their fastidious nature and
might have caused a replacement phenomenon with possible prior antibiotic use in the patient. In NAAT and
non-vaccine serotypes becoming increasingly responsible enhanced culture studies, anaerobes were noted in
for diseasein Utah, non-vaccine serotypes accounted 3374% of cases.64,66 NAAT studies have also identied
for 62% of cases of paediatric pneumococcal empyema substantial polymicrobiality associated with anaerobic
before introduction of the seven-valent pneumococcal infection, identifying many species previously not
conjugate vaccine, rising to 98% in 2007.61 The updated reported in the pleural space but almost all recognised
conjugate vaccine (13-valent pneumococcal conjugate as oropharyngeal commensals.64 Other oropharyngeal
568 www.thelancet.com/respiratory Vol 3 July 2015
Series
bacteria previously isolated include Eikenella corrodens common respiratory viruses in community-acquired
(a facultatively anaerobic Gram-negative bacillus), pleural infection. One study75 used NAAT to search for
Gemella morbillorum (a microaerophilic Gram-positive nine groups of viruses in forty-eight pleural uid samples
coccus), Capnocytophaga spp (a carbon dioxide-dependent (only twelve of which were parapneumonic), but showed
Gram-negative bacillus), and Mycoplasma salivarium.64,6770 no evidence of viral infection. Another study76 reported
The frequent role and polymicrobiality of oropharyngeal evidence of a novel torque teno mini virus in pleural
bacteria in pleural infection adds to the evidence that infection, the relevance of which is unclear given the
aspiration plays a key part in the development of pleural ubiquity of such viruses in human beings and the
infection. The defective mucociliary clearance and low absence of a clear association with disease. Pleural
oxygen tension associated with an atelectatic or eusions are associated with adenovirus, hantavirus,
consolidated lung could create the ideal conditions to cytomegalovirus, and herpes viruses.
allow oropharyngeal anaerobes to ourish in the lung Although outside the scope of this Series paper, many
and potentially spread into the pleural space. protozoa can cause pleural infection including
Entamoeba histolytica, Toxoplasma gondii (particularly
Atypical pneumonia pathogens and other unusual in immunosuppressed individuals), and Trichomonas
pleural space pathogens spp. Trichomonas tenax is of particular interest, being
Despite the high frequency with which atypical organisms an oropharyngeal commensal; it is unlikely to be seen
cause pneumonia, these organisms are rarely identied as a lone pathogen since its reproduction is reliant
in pleural infection, suggesting an absence of tropism for on bacteria to provide nutrients.77 Other parasites,
the pleural space and also that routine atypical antibiotic including hydatid disease (Echinococcus spp), lariasis
coverage is not necessary for pleural infection.5,37,53 Other (Wuchereria bancrofti), Paragonimus westermani, and
bacteria reported to rarely cause pleural infection (usually Strongyloides stercoralis, have also been reported to
in immunosuppressed patients), include Pasteurella cause pleural disease.
multocida (usually associated with animal bites or
scratches), non-typhoidal salmonella, Nocardia spp, and Microbiological diagnostic yield in pleural infection
non-tuberculous mycobacteria such as Mycobacterium In view of positive culture tests in only 3040% of cases of
abscessus, chelonae, and kansasii. pleural infection,9,37 studies have addressed methods to
improve bacterial aetiological diagnosis. One study
Cirrhosis-associated spontaneous bacterial empyema showed that bedside inoculation of pleural uid into blood
Data for pathogens noted with cirrhosis-associated culture bottles (besides conventional aerobic and
spontaneous bacterial empyema are restricted to case anaerobic culture) might increase sensitivity by about
series. However, the patterns of infection are clearly not 20%.78 Diagnosis of pneumococcal disease can be
typical of either community-acquired or hospital-acquired improved by testing pleural uid using commercially-
pleural infection. Bacteria reported in these cases are available immunochromatographic pneumococcal anti-
mostly associated with the gastrointestinal tract, including gen tests. Studies have shown these tests to have sensitivity
Enterococcus spp, Salmonella enteritidis, Clostridium greater than 84% and specicity greater than 94%.79,80
perfringens, Pasteurella multocida, and Aeromonas spp.24,26 NAAT, which can amplify and detect DNA (or RNA)
present in clinical samples, has been studied in
Non-bacterial causes aetiological diagnosis. NAAT has signicant theoretical
Fungal pleural infection is associated with substantial advantages. Unlike culture tests, organism detection is
mortality and is usually iatrogenic or associated with less susceptible to prior antibiotic use. Furthermore,
comorbidities or immunosuppression.71 Candidal pleural these techniques will not suer from the methodological
infection is particularly suggestive of oesophageal diculties associated with culture of fastidious
rupture (either spontaneous or malignant) with Candida organisms. Particular success has been achieved using
albicans seen most frequently and with Candida glabrata NAAT in paediatric pleural infection to amplify
or Candida tropicalis seen less frequently. Other fungi, pneumococcal gene targets, such as the autolysin and
mostly Aspergillus spp, are also occasionally isolated pneumolysin genes.51,81,82 Besides techniques targeting
particularly in patients who have received lung single pathogens, multiplex polymerase chain reaction
transplants.71,72 Despite the ubiquity of Pneumocystis assays can test for many pathogens in a single NAAT
jirovecii in the upper and lower respiratory tract, one experiment.83 Quantication of bacterial load can likewise
study73 reported no evidence of this fungus in pleural be achieved with quantitative NAAT assays. Polymerase
infection using highly sensitive quantitative NAAT. chain reaction-based estimates of bacterial load are
Although bacterial pleural infection is associated with associated with conventional pleural uid parameters
epidemics of inuenza (eg, the 2009 H1N1 inuenza A such as pH, glucose, lactate dehydrogenase, purulence,
epidemic was associated with increased rates of and culture status. Such estimates might be associated
pneumococcal and S pyogenes pleural infection),74 only a with key clinical outcomes such as length of hospital stay
few small studies have addressed the direct role of or duration of pleural drainage.84
www.thelancet.com/respiratory Vol 3 July 2015 569
Series
Technological advances and decreasing costs of nucleic might be of relevance; this mediator not only directly
acid sequencing have led to interest in the role of inhibits streptokinase but has also been shown in an
sequencing-based strategies for the diagnosis of animal model of pleural injury to contribute to the
infection. Nucleic acid sequencing, unlike other NAAT, severity of loculation and poor outcomes with intrapleural
provides a relatively assumption-free strategy for the brinolytic therapy.89,90 This principle is rearmed in a
identication of pathogens, including the recognition follow-up study by the same group in rabbits, which has
of unknown or unsuspected pathogens. A common shown that direct inhibition of PAI-1 signicantly
sequencing target used for bacterial identication is the increases the duration and ecacy (as measured by
16S ribosomal RNA gene, present in all bacteria. In the breakdown of intrapleural septations) of streptokinase.91
past, capillary-based sequencing of the 16S ribosomal Although this pathway merits further investigation as a
RNA gene was methodologically restricted in being able potential future therapeutic target, this investigation is
to identify only one pathogen per clinical sample unless presently hindered by the absence of any widely available
expensive cloning techniques were used.37,85 These means of monitoring or understanding the baseline
limitations have been overcome with next-generation PAI-1 activity in human participants with pleural
sequencing capable of identifying thousands of species infection. Since streptokinase is dependent on the
in one sample.64 physiological availability of plasminogen to form its active
complex, clinicians should consider whether it might be
Intrapleural therapies the wrong choice of brinolytic agent when used in
Besides appropriate antibiotic coverage based on local isolation. Additionally, because streptokinase has no
microbiological prevalence and resistance patterns, the eect on uid viscosity, this disadvantage together with
treatment of pleural infection necessitates adequate the development of intrapleural septations represents
drainage of the infected collection. Since most patients another barrier to successful drainage.
are initially managed with a percutaneous chest tube, To achieve successful drainage, in-vitro studies
great importance is placed on maximising the success eectively show the need to not only break down the
of this approach and limiting treatment failure. physical barrier created by brinous septations, but also
Clinicians have been interested in the potential value of to modify the viscosity of pleural uid, which is frequently
intrapleural brinolytic drugs for over half a century increased in infection as a consequence of cell
and how these drugs might prevent the progression of degradation products. Results from a study of human-
pleural infection to its more chronic brotic state.86 This derived samples of purulent uid incubated with
interest has focused on the physiological changes streptokinase, urokinase, combination streptokinase and
that occur in the infected pleural space, notably strepdornase (streptococcal deoxyribonuclease, DNase),
the depression of intrinsic brinolytic activity and or saline showed that only the uid incubated with the
consequent increase in brin load.31 Reversal of this combination streptokinase and strepdornase achieved
process has been assumed to facilitate both drainage of liquefaction.92 Similar results were seen in a larger study93
the collection by disrupting septations (further assumed of purulent pleural uid derived from an experimental
to correlate with relevant clinical outcomes) and reduce rabbit model of empyema proving the importance of
the burden of brous thickening that might otherwise DNase specically in reducing uid viscosity. The
restrict the underlying lung. combination of intrapleural direct tissue plasminogen
Streptokinase and urokinase were the rst brinolytic activator (tPA)a brinolytic agent that avoids the
drugs to be widely available and used in both adult and plasminogen complex step needed by streptokinase
paediatric pleural infection, with several case series and and DNase in another study23 that used the same animal
trials showing promise but without being able to provide model suggests additional promise in reducing the
denitive proof of eect on patient morbidity or anatomical sequelae of pleural infection.
mortality.87 An exception to this was a single, small, but For the translation of in-vitro results to a human adult
well-designed trial demonstrating reduced need for population, the MIST2 study9 was designed as a double-
surgery and reduced mortality with intrapleural strepto- placebo randomised controlled trial in pleural infection,
kinase.88 However, subsequent reporting of a large using tPA as a directly-acting brinolytic drug to disrupt
multi-centre randomised controlled trial8 of intrapleural septations and DNase with the aim of reducing uid
streptokinase versus placebo (MIST1) with 454 participants viscosity within the pleural space and enhancing drainage.
showed no evidence of a signicant improvement in key This four group study with 210 participants showed that
outcomes including death, rate of surgical referral, length combination tPA and DNase intrapleural therapy
of hospital stay, or lung function. Postulated reasons for signicantly reduced chest radiographic opacication
this include recruitment of patients who have already (the primary outcome), whereas tPA or DNase alone had
progressed to the late stages of their infection, and failure no eect compared with placebo. In the combination
to stratify for the presence or absence of septations on therapy group, secondary outcome measures including
ultrasound. Heterogeneity within the study population surgical referral rate and length of hospital stay showed
regarding the intrapleural activity of endogenous PAI-1 trends for a reduction but these were not statistically
570 www.thelancet.com/respiratory Vol 3 July 2015
Series
signicant.9 Intrapleural drugs given alone showed no therapeutic lavage of the pleural space and aiding the
benet and DNase alone was actually associated with an clearance of infected materialthis would be consistent
increased surgical referral rate. No signicant increases with a pilot study that has shown a potential benet from
in mortality or adverse event rate in any experimental saline irrigation via the intercostal chest drains of people
study group were shown when compared with placebo,9 with pleural infection.96 MCP-1 is already known to have
implying a good safety prole for the combination a potential role in mechanisms of repair following
intrapleural treatment. This nding was further re- pleural injury, as well as inducing endothelial perm-
armed in a later retrospective case series.94 eability and the co-activation of other inammatory
The results of the MIST2 study9 were consistent with pathways.22,97 Scientic research is needed to better dene
those of MIST18 in ruling out a role for single agent the mechanisms of this pathway and identify potential
brinolytics in pleural infection. Therefore, the com- translational uses for clinical benet.
bination of DNase to reduce uid viscosity together with
a brinolytic such as tPA to lyse septations is probably Surgical management
most ecacious at maximising drainage. Randomisation Current guidelines5,18 advocate the use of surgery as a
of participants in the MIST2 study9 was minimised (to rescue therapy in cases of pleural infection that have
prevent imbalances between the treatments received by either failed to respond to standard medical treatment (ie,
patients in specied sub-groups) by purulence of pleural percutaneous drainage and antibiotics) or if progression
uid in view of a previous study that suggested that this to an advanced brotic state is suspected with extensive
characteristic might be associated with variation in key pleural thickening requiring decortication. The timing of
clinical outcomes from pleural infection.39 However, the surgical intervention to ensure adequate clearance of
presence of purulence was not reported to be directly infected material from the pleural space is crucial and has
associated with the ecacy of combination intrapleural been shown to be potentially life-saving in this selected
therapy in the MIST2 study. This nding implies that the population of patients. Although randomised trial data8,9
mechanism of action of DNase is not associated with a have shown that most patients (around 80%) can be
crude macroscopic measure of the likely DNA load successfully managed medically, surgery is a rst-line
within the pleural space, assuming that purulent uid treatment for pleural infection and empyema, particularly
will contain more DNA than non-purulent uid. in the USA. This approach of early surgical intervention
Therefore, small amounts of DNA within infected pleural has been justied on the basis of improved clinical
uid are possibly of some clinical relevance, either by outcome and shorter hospital stays for patients managed
causing a degree of increased uid viscosity, or perhaps in this way.12,15,98100
supporting the yet unproven hypothesis that biolm Although surgical treatment for pleural infection used
formation by bacteria within the pleural space aects to necessitate open thoracotomy, most cases are now
outcome. This theory might also explain the increased managed using video-assisted thoracoscopic surgery
surgical referral rate seen in those study participants who (VATS). This less invasive approach potentially widens
were randomised to intrapleural DNase alone. DNase the population who might be suitable for surgical
might have lysed biolms and released bacteria that therapy,100 although large case series2,12 from both the
could not be drained in the absence of tPA, increasing USA and UK show a continued preference to operate on
local and systemic inammation and thereby prompting younger and less comorbid individuals than seen in an
surgical referral. unselected population of patients with pleural infection.8,9
Nonetheless, the means by which brinolytics improve Nonetheless, a meta-analysis101 has suggested that VATS
clearance of infected material from the pleural space is is superior to thoracotomy with respect to length of
almost certainly more complex than mere mechanical hospital stay, postoperative morbidity and complication
disruption. Data from animal23 and human94 studies rate, and similar from the perspective of disease
show that the administration of intrapleural tPA is resolution. Surgical clearance of potentially infected
associated with up to a ten-fold increase in pleural uid material from the pleural space need not be perfect, but
output. A study using an in-vivo mouse model of pleural rather sucient to allow the patient to recover. A more
infection95 has shown this to be a class eect with conservative debridement without full decortication
streptokinase, urokinase, and tPA all stimulating excess might be adequate in selected cases to avoid
pleural uid formation. Contemporaneous studies by the compromising key long-term outcomes.102 For patients
same group using cell lines in vitro and the same murine who are not t for general anaesthesia, thoracoscopic
model suggest that this is mediated via MCP-1 expression drainage can still be used with sedation and local
and protein release by mesothelial cells, with pleural anaesthesia. This approach has been applied successfully
uid levels of this cytokine directly correlating with by thoracic surgeons103 and also physicians with expertise
volume of uid produced. Furthermore, blockade of in medical thoracoscopy but only in small studies.104,105
MCP-1 activity results in loss of the uid stimulating Compared with larger studies that have assessed the
eect of tPA in mice.95 This potent stimulation of uid ecacy of intrapleural brinolytics with or without
production might have additional benets by causing a DNase, few data are available on the use of surgery and
www.thelancet.com/respiratory Vol 3 July 2015 571
Series
specically VATS as a rst-line intervention. In a small need for radical chest wall mobilisation and mutilation.116
randomised trial106 of 20 participants, which compared Open window thoracotomy remains a potentially
VATS with intercostal drainage plus intrapleural life-saving option for patients with persistent pleural space
streptokinase, VATS was successful as a rst-line therapy infection after thoracic surgical proceduresfor example,
in 91% of participants as compared with 44% in the pneumonectomy or lobectomy. Techniques centre on
streptokinase group, with patients not needing any resection of two or more ribs with marsupialisation to
additional invasive therapeutic intervention. VATS was facilitate open drainage and are associated with acceptable
also associated with a signicant reduction in the long-term outcomes in high-risk population.117 The use of
duration that a chest tube remained in situ, decreased vacuum-associated closure devices might enhance the
lengths of intensive care unit and hospital stays, and a care of these patients by accelerating recovery118 and this
reduction in overall costs.106 Other small studies107,108 of approach merits further assessment. The chronically
early surgery (ie, on or very soon after admission to infected pleural space unsuitable for additional surgical
hospital) in adults with pleural infection have also interventionfor example, in the setting of severe
suggested that this is associated with reduced hospital comorbidity or poor performance statuscan also be
lengths of stay and cost. However, these studies and managed using long-term thoracostomy. This can take the
other reported studies relating to this approach recruited form of a wide-bore drain with one-way (Heimlich) valve
small participant numbers and were underpowered as a or tunnelled catheter.119,120 In all these circumstances,
result. Nevertheless, delayed referral for surgical long-term antibiotic suppression therapy is probably
treatment does clearly result in more dicult procedures needed as an adjunct to achieve adequate sepsis control.
including a higher rate of conversion of VATS to From a practical perspective, clinicians should consider
thoracotomy.109 both the available data as well as local resources (ie, the
The surgical data in adults seem to contradict data presence of a thoracic surgeon skilled in minimally
from children with pleural infection, for whom a series invasive surgery) when devising a cogent treatment plan
of larger randomised studies110112 have shown no clinical for patients with pleural infection. A short illness of less
benet and increased cost of VATS compared with chest than 10 days without gross purulence together with the
tube drainage in brinolytic therapy. A smaller study113 absence of septations on ultrasound examination or many
that randomised 18 paediatric patients to VATS or tube locules detected by CT favours a conservative approach
thoracostomy (with or without brinolytics as indicated) using chest tube drainage with or without intra-
did nd that surgery was associated with a shorter pleural brinolytics. However, a combination of features
hospital admission. This dierence might be the result including symptom duration of more than 2 weeks, gross
of diering microbiological organisms,109 with most purulence on thoracentesis, pleural loculation, or a sign of
paediatric pleural infection being caused by S pneumoniae split pleura with pleural enhancement on CT examination
as opposed to the many dierent organisms seen in adult might suggest the presence of a visceral cortex and the
pleural infection. This dierence raises the question of need for surgical debridement to re-expand the aected
whether microbiological analysis might be one means by lung and obliterate the infected pleural space. Regardless
which patients could be stratied as low risk or high of this, although surgery remains a key intervention in
risk for morbidity or mortality. The high-risk group, the management of pleural infection, more large-scale
which potentially includes patients with Gram-negative randomised trials are needed to dene when and how it
organisms or hospital-acquired infections, is suitable for should be used in this population.
early aggressive therapy including surgery with the aim
of improving relevant clinical outcomes. However, this Future directions
paradigm of using less invasive treatment options for Although avoidance of thoracotomy is clearly a desired
patients deemed to be of low risk according to their outcome, avoidance of surgery might not be the outcome
microbiological prole might be changing with the measure that should be examined in future studies of
increasing prevalence of empyema complicating treatment in pleural infection. If VATS can be the denitive
pneumococcal pneumonia in both children and therapeutic procedure for empyema and permit discharge
adults.114,115 This alarming trend has been seen despite an from hospital in less than a week (whereas the average
increasing uptake of the multivalent pneumococcal hospital length of stay for patients receiving combination
conjugate vaccine,3,57 with the rate of pneumococcal tPA and DNase in the MIST2 trial was 12 days),9 VATS
pneumonia admissions falling at the same time as might become the procedure of choice as a rst-line
empyema increases, potentially as a result of selection of treatment advised immediately on admission to hospital.
more invasive serotypes. Additionally, since the drug cost alone of tPA and DNase
For patients in whom decortication fails, empyema intrapleural therapy is roughly 1000, early VATS might
recurs, or who have a bronchopleural stula, thoracoplasty achieve substantial cost savings in the UK and also other
might be a good surgical option in a highly selected group countries where VAT is easily available. A cost analysis of
of patients. Modern techniques using muscle aps to the MIST2 trial is underway, although a multicentre trial
eliminate residual pleural space issues have reduced the comparing early VATS with combination tPA and DNase
572 www.thelancet.com/respiratory Vol 3 July 2015
Series
intrapleural therapy assessing key clinical outcomes in
pleural infection is needed, and being planned by the Search strategy and selection criteria
authors to answer these questions. We searched Embase and Medline for peer-reviewed articles
In view of the therapeutic primacy of achieving published in English from Jan 1, 2000 to Dec 31, 2014, using
successful drainage of infected material from the pleural the search terms pleural empyema, pleural eusion,
space, most studies have focused on how this might be empyema, parapneumonic eusion, pleural infection,
best achieved, for example, through chest tube drainage pleural collection, and parapneumonic infection.
(with or without intrapleural brinolytics) or by surgical Reference lists of identied articles deemed to be of relevance
intervention. A subset of patients might exist, however, were searched. Other studies including conference abstracts
in whom outpatient management using therapeutic that were known to the authors to be relevant but not
thoracentesis only whenever needed or for whom identied by this search strategy were also screened.
drainage is not even necessary, is an acceptable strategy.121
The development of a method for the identication of
these patients using a combination of clinical, radiological, Another aspect of the MIST2 protocol that is under
biochemical, and microbiological data might help reduce investigation is the dosing regimen. In the MIST2 study,9
treatment costs through avoidance of hospital admission. tPA was given and the chest drain clamped for one hour,
However, this will only be possible once our understanding followed by administration of DNase and further
of the pathogenesis and progression of pleural infection clamping of the chest drain for another hour, with this
is improved. pattern being repeated twice daily for three days. This
The primary outcome in the MIST2 study9 was labour-intensive practice has led some treatment centres
improvement in the chest radiograph (a surrogate marker to combine the drugs as part of an abridged administration
for successful clearance of the infected collection) and the protocol;94 however, we do not recommend this approach
study was underpowered to assess for signicant improve- on the basis of evidence available. More studies are
ments in mortality and morbidity from pleural infection. needed to ascertain the optimum doses of tPA and
Future large multicentre trials should address this key DNase. If a lower dosing regimen than that used in the
question and other patient-centred endpoints. Since about MIST2 study can be shown to be equally ecacious, the
70% of patients can avoid surgery, future trials should try cost-benet analysis would substantially change and
to identify patients in whom medical therapy is likely to might make combination intrapleural therapy a more
fail to enable them to be sent for surgery early during their attractive and widely available option.
admission. Likewise, the identication of patients who As with tuberculous eusions, the pleural uid might
might do well with medical therapy would be useful so not be the best type of sample to undertake culture tests.
that surgery can be avoided in these individuals (regardless Parietal pleural biopsies used in culture tests might
of the outcome of any cost-benet analysis comparing substantially increase the diagnostic microbiological yield
medical and surgical treatment pathways). in pleural infection (thereby reducing the number of
The development and validation of a risk stratication culture negative cases that have to be treated with
model for patients with pleural infection based on empirical or blind use of antibiotics), and a specic study
biochemical and physiological parameters at initial to assess this possibility is planned. Dierent antibiotics
presentation to hospital is already in progress.44 However, have the ability to penetrate the pleural space at widely
other easily accessible biomarkers could provide dierent rates, with some of them not achieving
additional prognostic information. These biomarkers therapeutic levels as shown in rabbits,123125 particularly for
might include radiological features such as septation spaces that are multiloculated with pus and brin.
density on ultrasound, pleural thickening or loculation on Continued investigation in both the laboratory setting
CT, or microbiological cause. These biomarkers have all and with human participants addressing the precise
been shown to have potential value in retrospective pharmacokinetics of intravenous antibiotics and how this
studies10,37,122 and merit prospective assessment on a wider translates across to the infected pleural space is necessary
scale. Newer biomarkers including MCP-195 and PAI-191 to inform clinicians. These data might aect antibiotic
are still being investigated in the laboratory setting and choice, dosing regimens, and duration of therapy. Data
are unlikely to reach the bedside for several years are also scarce regarding the intra-pleural administration
however, they oer promise as both therapeutic targets of antibiotics and whether this direct approach (as
and a means of monitoring response to treatment. Future opposed to waiting for antibiotics administered intra-
laboratory studies involving these and other biomarkers venously to gradually diuse into the pleural space) might
should also investigate the precise mechanisms by which accelerate sterilisation of the pleural space; further
intrapleural brinolytics act. An increased understanding investigation is necessary focusing on experimental
of these pathways might help us stratify patients into models together with translational studies at the bedside.
those who are likely to respond to intrapleural brinolytics Another potential therapeutic adjunct that has been
and those who might be better served by surgery in the reported and needs additional study is the use of pleural
event that initial medical treatment fails. irrigation, either with saline96 or povidone-iodine.126
www.thelancet.com/respiratory Vol 3 July 2015 573
Series
Fundamental for the improvement of management of Contributors
patients with pleural infection is an understanding of JPC and NMR conceived and designed the Series paper. JPC and JMW
did the scientic literature search and contributed equally to the
the progression from pneumonia to an infected pleural collection and analysis of the results. JPC wrote the sections on
space, where parenchymal infection is present. Little introduction, pathophysiology, diagnosis and outcome prediction, and
robust data exists describing how this process might intrapleural therapies. JMW wrote the section on microbiology. EB and
occur. We propose that the factors associated with the MMDC wrote the section on surgical management. DF-K and NMR
wrote the sections on future directions, conclusion, and revised the
development of pleural infection are probably related to article. All authors approved the nal version of the article.
host inammatory and immune status or variation, and
Declaration of interests
bacterial characteristics. Translational studies addressing JPC is study coordinator for PILOT (ISRCTN 50236700), an observational
bacterial translocation, uid formation, and the est- study of pleural infection funded by the Medical Research Council, UK.
ablishment of infectious niches within the pleural space DF-K has provided consultancy services to Spiration, Inc. NMR has
in parallel to host assessments are necessary. The provided consultancy services for Rocket Medical UK and was
corresponding author for the MIST2 study, which was supported by an
changing aspects of pneumococcal infection,3,6,7,57,115 as a unrestricted educational grant from Roche UK to the University of Oxford.
result of serotype selection after the introduction of NMR is also chief investigator for the PILOT study and is director of the
multivalent vaccines, might be one way to increase our University of Oxford Respiratory Trials Unit that published the MIST1 and
MIST2 studies. JMW, EB, and MMDC declare no competing interests.
understanding of how and why pleural infection
develops in dierent settings. Acknowledgments
No external funding was sought or needed for the production of this
The prevalence of pleural infection continues to
article. JMW and NMR are funded by the National Institute of Health
increase with substantial long-term mortality, rising as Research Oxford Biomedical Research Centre.
high as 30% in the most elderly patients with pronounced
References
frailty or comorbidity. This high mortality is probably due 1 Grijalva CG, Zhu Y, Nuorti JP, Grin MR. Emergence of
not only to the eect of medical comorbidity but also to a parapneumonic empyema in the USA. Thorax 2011; 66: 66368.
chronic inammatory eect and alteration in immune 2 Farjah F, Symons RG, Krishnadasan B, Wood DE, Flum DR.
Management of pleural space infections: a population-based
response similar to that seen in other respiratory analysis. J Thorac Cardiovasc Surg. 2007; 133: 34651.
infections, which include exacerbations of chronic 3 Li ST, Tancredi DJ. Empyema hospitalizations increased in US
obstructive pulmonary disease and community-acquired children despite pneumococcal conjugate vaccine. Pediatrics 2010;
125: 2633.
pneumonia.127131 The identication of strategies by which 4 Roxburgh CS, Youngson GG, Townend JA, Turner SW. Trends in
this legacy eect can be modied, for example, by pneumonia and empyema in Scottish children in the past 25 years.
optimising the management of comorbidities such as Arch Dis Child 2008; 93: 31618.
5 Davies HE, Davies RJ, Davies CW, and the BTS Pleural Disease
diabetes, ischaemic heart disease, and airways disease, is Guideline Group. Management of pleural infection in adults:
probably crucial in altering the long-term outlook after British Thoracic Society Pleural Disease Guideline 2010.
pleural infection. Thorax 2010; 65 (suppl 2): ii4153.
6 Muoz-Almagro C, Jordan I, Gene A, Latorre C, Garcia-Garcia JJ,
Pallares R. Emergence of invasive pneumococcal disease caused by
Conclusion nonvaccine serotypes in the era of 7-valent conjugate vaccine.
Despite pronounced advances in medical and surgical Clin Infect Dis 2008; 46: 17482.
treatment, pleural infection remains an important and 7 Koshy E, Murray J, Bottle A, Sharland M, Saxena S. Impact of the
seven-valent pneumococcal conjugate vaccination (PCV7)
morbid clinical challenge. Our understanding of the programme on childhood hospital admissions for bacterial
pathophysiological process whereby organisms gain pneumonia and empyema in England: national time-trends study,
19972008. Thorax 2010; 65: 77074.
access to the pleural space and establish infection is
8 Maskell NA, Davies CW, Nunn AJ, et al, and the First Multicenter
incomplete. Future studies that address the progression Intrapleural Sepsis Trial (MIST1) Group. U.K. Controlled trial of
of pleural infection might shed light on how intrapleural streptokinase for pleural infection. N Engl J Med 2005;
interventions can reduce the substantial morbidity and 352: 86574.
9 Rahman NM, Maskell NA, West A, et al. Intrapleural use of tissue
mortality associated with this disease. Study on the plasminogen activator and DNase in pleural infection.
microbiological prole of pleural infection suggests a N Engl J Med 2011; 365: 51826.
broad range of causative organisms that are distinct 10 Nielsen J, Meyer CN, Rosenlund S. Outcome and clinical
characteristics in pleural empyema: a retrospective study.
from the causes of lung parenchymal infection. Clinical Scand J Infect Dis 2011; 43: 43035.
scoring systems to predict poor outcome in patients 11 Desai G, Amadi W. Three years experience of empyema thoracis in
with pleural infection are being assessed and might association with HIV infection. Trop Doct 2001; 31: 10607.
provide not only a method of risk stratication at 12 Marks DJ, Fisk MD, Koo CY, et al. Thoracic empyema: a 12-year
study from a UK tertiary cardiothoracic referral centre.
baseline, but also the potential to select patients early PLoS One 2012; 7: e30074.
that need more invasive and expensive treatments. 13 Davies HE, Rosenstengel A, Lee YC. The diminishing role of
Although promising data exist regarding the use of surgery in pleural disease. Curr Opin Pulm Med 2011; 17: 24754.
14 Corcoran JP, Rahman NM. Point: should brinolytics be routinely
intrapleural tPA and DNase treatment for pleural administered intrapleurally for management of a complicated
infection, the exact role of these treatments is uncertain, parapneumonic eusion? Yes. Chest 2014; 145: 1417.
especially compared with early VATS. More studies 15 Suchar AM, Zureikat AH, Glynn L, Statter MB, Lee J, Liu DC.
are necessary to dene the role of these treatments Ready for the frontline: is early thoracoscopic decortication the new
standard of care for advanced pneumonia with empyema?
more clearly. Am Surg 2006; 72: 68892.
574 www.thelancet.com/respiratory Vol 3 July 2015
Series
16 Scarci M, Zahid I, Bill A, Routledge T. Is video-assisted 40 Huang HC, Chang HY, Chen CW, Lee CH, Hsiue TR. Predicting
thoracoscopic surgery the best treatment for paediatric pleural factors for outcome of tube thoracostomy in complicated
empyema? Interact Cardiovasc Thorac Surg 2011; 13: 7076. parapneumonic eusion for empyema. Chest 1999; 115: 75156.
17 Lee SF, Lawrence D, Booth H, Morris-Jones S, Macrae B, Zumla A. 41 Chen CH, Chen W, Chen HJ, et al. Transthoracic ultrasonography
Thoracic empyema: current opinions in medical and surgical in predicting the outcome of small-bore catheter drainage in
management. Curr Opin Pulm Med 2010; 16: 194200. empyemas or complicated parapneumonic eusions.
18 Colice GL, Curtis A, Deslauriers J, et al. Medical and surgical Ultrasound Med Biol 2009; 35: 146874.
treatment of parapneumonic eusions : an evidence-based 42 Havelock T, Teoh R, Laws D, Gleeson F, and the BTS Pleural
guideline. Chest 2000; 118: 115871. Disease Guideline Group. Pleural procedures and thoracic
19 Strange C, Sahn SA. The denitions and epidemiology of pleural ultrasound: British Thoracic Society Pleural Disease Guideline
space infection. Semin Respir Infect 1999; 14: 38. 2010. Thorax 2010; 65 (suppl 2): ii6176.
20 Chalmers JD, Singanayagam A, Murray MP, Scally C, Fawzi A, 43 Rahman NM, Singanayagam A, Davies HE, et al. Diagnostic
Hill AT. Risk factors for complicated parapneumonic eusion and accuracy, safety and utilisation of respiratory physician-delivered
empyema on presentation to hospital with community-acquired thoracic ultrasound. Thorax 2010; 65: 44953.
pneumonia. Thorax 2009; 64: 59297. 44 Rahman NM, Kahan BC, Miller RF, Gleeson FV, Nunn AJ,
21 Nasreen N, Mohammed KA, Hardwick J, et al. Polar production of Maskell NA. A clinical score (RAPID) to identify those at risk for
interleukin-8 by mesothelial cells promotes the transmesothelial poor outcome at presentation in patients with pleural infection.
migration of neutrophils: role of intercellular adhesion molecule-1. Chest 2014; 145: 84855.
J Infect Dis 2001; 183: 163845. 45 Sasse SA, Causing LA, Mulligan ME, Light RW. Serial pleural uid
22 Kroegel C, Antony VB. Immunobiology of pleural inammation: analysis in a new experimental model of empyema. Chest 1996;
potential implications for pathogenesis, diagnosis and therapy. 109: 104348.
Eur Respir J 1997; 10: 241118. 46 Strange C, Allen ML, Harley R, Lazarchick J, Sahn SA. Intrapleural
23 Zhu Z, Hawthorne ML, Guo Y, et al. Tissue plasminogen activator streptokinase in experimental empyema. Am Rev Respir Dis 1993;
combined with human recombinant deoxyribonuclease is eective 147: 96266.
therapy for empyema in a rabbit model. Chest 2006; 129: 157783. 47 Fletcher MA, Schmitt HJ, Syrochkina M, Sylvester G.
24 Xiol X, Castellv JM, Guardiola J, et al. Spontaneous bacterial Pneumococcal empyema and complicated pneumonias: global
empyema in cirrhotic patients: a prospective study. Hepatology 1996; trends in incidence, prevalence, and serotype epidemiology.
23: 71923. Eur J Clin Microbiol Infect Dis 2014; 33: 879910.
25 Jae A, Calder AD, Owens CM, Stanojevic S, Sonnappa S. Role of 48 Varano Della Vergiliana JF, Lansley SM, Porcel JM, et al.
routine computed tomography in paediatric pleural empyema. Bacterial infection elicits heat shock protein 72 release from
Thorax 2008; 63: 897902. pleural mesothelial cells. PLoS One 2013; 8: e63873.
26 Tu CY, Chen CH. Spontaneous bacterial empyema. 49 Lee Y, Varnao J, Rashwan R, Waterer G, Townsend T, Kay I.
Curr Opin Pulm Med 2012; 18: 35558. Staphylococcus aureus, but not other bacterial empyema
27 Wilkosz S, Edwards LA, Bielsa S, et al. Characterization of a new pathogens, induce the release of selected cytokines from
mouse model of empyema and the mechanisms of pleural invasion mesothelial cells. Respirology 2014; 19 (suppl 2): 128.
by Streptococcus pneumoniae. Am J Respir Cell Mol Biol 2012; 50 Brims F, Rosenstengal A, Yogendran, et al. The bacteriology of
46: 18087. pleural infection in Western Australia. Am J Respir Crit Care Med
28 Light RW, MacGregor MI, Ball WC Jr, Luchsinger PC. Diagnostic 2014; 189: A5472.
signicance of pleural uid pH and PCO2. Chest 1973; 64: 59196. 51 Blaschke AJ, Heyrend C, Byington CL, et al. Molecular analysis
29 Sahn SA, Reller LB, Taryle DA, Antony VB, Good JT Jr. The improves pathogen identication and epidemiologic study of pediatric
contribution of leukocytes and bacteria to the low pH of empyema parapneumonic empyema. Pediatr Infect Dis J 2011; 30: 28994.
uid. Am Rev Respir Dis 1983; 128: 81115. 52 Eastham KM, Freeman R, Kearns AM, et al. Clinical features,
30 Hener JE, Brown LK, Barbieri C, DeLeo JM. Pleural uid chemical aetiology and outcome of empyema in children in the north east of
analysis in parapneumonic eusions. A meta-analysis. England. Thorax 2004; 59: 52225.
Am J Respir Crit Care Med 1995; 151: 170008. 53 Meyer CN, Rosenlund S, Nielsen J, Friis-Mller A. Bacteriological
31 Idell S, Girard W, Koenig KB, McLarty J, Fair DS. Abnormalities of aetiology and antimicrobial treatment of pleural empyema.
pathways of brin turnover in the human pleural space. Scand J Infect Dis 2011; 43: 16569.
Am Rev Respir Dis 1991; 144: 18794. 54 Chen KY, Hsueh PR, Liaw YS, Yang PC, Luh KT. A 10-year
32 Mutsaers SE, Kalomenidis I, Wilson NA, Lee YC. Growth factors in experience with bacteriology of acute thoracic empyema: emphasis
pleural brosis. Curr Opin Pulm Med 2006; 12: 25158. on Klebsiella pneumoniae in patients with diabetes mellitus.
Chest 2000; 117: 168589.
33 Kunz CR, Jadus MR, Kukes GD, Kramer F, Nguyen VN,
Sasse SA. Intrapleural injection of transforming growth 55 Lin YT, Chen TL, Siu LK, Hsu SF, Fung CP. Clinical and
factor-beta antibody inhibits pleural brosis in empyema. microbiological characteristics of community-acquired thoracic
Chest 2004; 126: 163644. empyema or complicated parapneumonic eusion caused by
34 El Solh AA, Alhajjhasan A, Ramadan FH, Pineda LA. A comparative Klebsiella pneumoniae in Taiwan.Eur J Clin Microbiol Infect Dis 2010;
study of community- and nursing home-acquired empyema 29: 100310.
thoracis. J Am Geriatr Soc 2007; 55: 184752. 56 Hendrickson DJ, Blumberg DA, Joad JP, Jhawar S, McDonald RJ.
35 Diacon AH, Brutsche MH, Solr M. Accuracy of pleural puncture Five-fold increase in pediatric parapneumonic empyema since
sites: a prospective comparison of clinical examination with introduction of pneumococcal conjugate vaccine.
ultrasound. Chest 2003; 123: 43641. Pediatr Infect Dis J 2008; 27: 103032.
36 Mercaldi CJ, Lanes SF. Ultrasound guidance decreases complications 57 Burgos J, Lujan M, Falc V, et al. The spectrum of pneumococcal
and improves the cost of care among patients undergoing empyema in adults in the early 21st century. Clin Infect Dis 2011;
thoracentesis and paracentesis. Chest 2013; 143: 53238. 53: 25461.
37 Maskell NA, Batt S, Hedley EL, Davies CW, Gillespie SH, Davies RJ. 58 Grau I, Ardanuy C, Calatayud L, et al. Invasive pneumococcal
The bacteriology of pleural infection by genetic and standard disease in healthy adults: increase of empyema associated with the
methods and its mortality signicance. Am J Respir Crit Care Med clonal-type Sweden(1)-ST306. PLoS One 2012; 7: e42595.
2006; 174: 81723. 59 Thomas MF, Sheppard CL, Guiver M, et al. Emergence of
38 Rahman NM, Mishra EK, Davies HE, Davies RJ, Lee YC. Clinically pneumococcal 19A empyema in UK children. Arch Dis Child 2012;
important factors inuencing the diagnostic measurement of 97: 107072.
pleural uid pH and glucose. Am J Respir Crit Care Med 2008; 60 Lai CY, Huang LM, Lee PY, Lu CY, Shao PL, Chang LY. Comparison
178: 48390. of invasive pneumococcal disease caused by serotype 19A and
39 Davies CW, Kearney SE, Gleeson FV, Davies RJ. Predictors of non-19A pneumococci in children: more empyema in serotype 19A
outcome and long-term survival in patients with pleural infection. invasive pneumococcal disease. J Microbiol Immunol Infect 2014;
Am J Respir Crit Care Med 1999; 160: 168287. 47: 2327.
www.thelancet.com/respiratory Vol 3 July 2015 575
Series
61 Byington CL, Hulten KG, Ampofo K, et al. Molecular epidemiology 86 Tillett WS, Sherry S. The eect in patients of streptococcal
of pediatric pneumococcal empyema from 2001 to 2007 in Utah. brinolysin (streptokinase) and streptococcal desoxyribonuclease on
J Clin Microbiol 2010; 48: 52025. brinous, purulent, and sanguinous pleural exudations.
62 Thomas MF, Sheppard C, Guiver M, et al. Paediatric pneumococcal J Clin Invest 1949; 28: 17390.
empyema serotypes have not changed following introduction of the 87 Cameron R, Davies HR. Intra-pleural brinolytic therapy versus
13 valent pneumococcal vaccine. Thorax 2013; 68: A39. conservative management in the treatment of parapneumonic
63 Smith DT. Experimental aspiratory abscess. Arch Surg 1927; 14: 23139. eusions and empyema. Cochrane Database Syst Rev 2004: CD002312.
64 Wrightson JM, Wray JA, Street TL, Chapman SJ, Crook DW, 88 Diacon AH, Theron J, Schuurmans MM, Van de Wal BW, Bolliger CT.
Rahman NM. S114: Previously unrecognised oral anaerobes in Intrapleural streptokinase for empyema and complicated
pleural infection. Thorax 2014; 69 (suppl S2): A6162. parapneumonic eusions. Am J Respir Crit Care Med 2004; 170: 4953.
65 Shinzato T, Saito A. A mechanism of pathogenicity of 89 Komissarov AA, Florova G, Azghani A, Karandashova S,
Streptococcus milleri group in pulmonary infection: synergy with Kurdowska AK, Idell S. Active -macroglobulin is a reservoir for
an anaerobe. J Med Microbiol 1994; 40: 11823. urokinase after brinolytic therapy in rabbits with tetracycline-
66 Boyanova L, Djambazov V, Gergova G, et al. Anaerobic induced pleural injury and in human pleural uids.
microbiology in 198 cases of pleural empyema: a Bulgarian study. Am J Physiol Lung Cell Mol Physiol 2013; 305: L68292.
Anaerobe 2004; 10: 26167. 90 Karandashova S, Florova G, Azghani AO, et al. Intrapleural
67 Hourmont K, Klingler PJ, Wetscher G, Kafka R, Gadensttter M, adenoviral delivery of human plasminogen activator inhibitor-1
Bonatti H. Capnocytophaga pleural empyema following exacerbates tetracycline-induced pleural injury in rabbits.
laparoscopic Nissen fundoplication. A rare complication, a rare Am J Respir Cell Mol Biol 2013; 48: 4452.
pathogen. Surg Endosc 2000; 14: 866. 91 Florova G, Azghani A, Karandashova S, et al. Targeting of
68 Valipour A, Koller H, Setinek U, Burghuber OC. Pleural empyema plasminogen activator inhibitor 1 improves brinolytic therapy for
associated with Gemella morbillorum: report of a case and review tetracycline-induced pleural injury in rabbits.
of the literature. Scand J Infect Dis 2005; 37: 37881. Am J Respir Cell Mol Biol 2015; 52: 42937.
69 Baracaldo R, Foltzer M, Patel R, Bourbeau P. Empyema caused by 92 Simpson G, Roomes D, Heron M. Eects of streptokinase and
Mycoplasma salivarium. J Clin Microbiol 2012; 50: 180506. deoxyribonuclease on viscosity of human surgical and empyema
pus. Chest 2000; 117: 172833.
70 Hoyler SL, Antony S. Eikenella corrodens: an unusual cause of
severe parapneumonic infection and empyema in 93 Light RW, Nguyen T, Mulligan ME, Sasse SA. The in vitro ecacy
immunocompetent patients. J Natl Med Assoc 2001; 93: 22429. of varidase versus streptokinase or urokinase for liquefying thick
purulent exudative material from loculated empyema. Lung 2000;
71 Ko SC, Chen KY, Hsueh PR, Luh KT, Yang PC. Fungal empyema
178: 1318.
thoracis: an emerging clinical entity. Chest 2000; 117: 167278.
94 Piccolo F, Pitman N, Bhatnagar R, et al. Intrapleural tissue
72 Wahidi MM, Willner DA, Snyder LD, Hardison JL, Chia JY,
plasminogen activator and deoxyribonuclease for pleural infection.
Palmer SM. Diagnosis and outcome of early pleural space infection
An eective and safe alternative to surgery.
following lung transplantation. Chest 2009; 135: 48491.
Ann Am Thorac Soc 2014; 11: 141925.
73 Wrightson JM, Rahman NM, Novak T, et al. Pneumocystis jirovecii in
95 Lansley SM, Cheah HM, Varano Della Vergiliana JF, Chakera A,
pleural infection: a nucleic acid amplication study. Thorax 2011;
Lee YG. Tissue plasminogen activator potently stimulates pleural
66: 45051.
eusion via an MCP-1 Dependent Mechanism.
74 Ampofo K, Herbener A, Blaschke AJ, et al. Association of 2009 Am J Respir Cell Mol Biol 2014; published online Dec 4. DOI:10.1165/
pandemic inuenza A (H1N1) infection and increased rcmb.2014-0017OC.
hospitalization with parapneumonic empyema in children in Utah.
96 Hooper AJ, Wallis AJ, Clive AO et al. Pleural Irrigation Trial (PIT):
Pediatr Infect Dis J 2010; 29: 90509.
standard care versus pleural irrigation, a randomised controlled
75 Sevin CM, Peng S, Skouras V, et al. Do viral infections cause pleural trial in patients with pleural infection. Thorax 2012; 67: A11.
eusions? Am J Respir Crit Care Med 2009; 179: A4459 (abstr).
97 Nasreen N, Mohammed KA, Galy G, Ward MJ, Antony VB.
76 Galms J, Li Y, Rajoharison A, et al. Potential implication of new MCP-1 in pleural injury: CCR2 mediates haptotaxis of pleural
torque teno mini viruses in parapneumonic empyema in children. mesothelial cells. Am J Physiol Lung Cell Mol Physiol 2000;
Eur Respir J 2013; 42: 47079. 278: L59198.
77 Lewis KL, Doherty DE, Ribes J, Seabolt JP, Bensadoun ES. 98 Solaini L, Prusciano F, Bagioni P. Video-assisted thoracic surgery
Empyema caused by trichomonas. Chest 2003; 123: 29192. in the treatment of pleural empyema. Surg Endosc 2007;
78 Menzies SM, Rahman NM, Wrightson JM, et al. Blood culture bottle 21: 28084.
culture of pleural uid in pleural infection. Thorax 2011; 66: 65862. 99 Chung JH, Lee SH, Kim KT, Jung JS, Son HS, Sun K. Optimal
79 Le Monnier A, Carbonnelle E, Zahar JR, et al. Microbiological timing of thoracoscopic drainage and decortication for empyema.
diagnosis of empyema in children: comparative evaluations by Ann Thorac Surg 2014; 97: 22429.
culture, polymerase chain reaction, and pneumococcal antigen 100 Schweigert M, Solymosi N, Dubecz A, et al. Surgical management
detection in pleural uids. Clin Infect Dis 2006; 42: 113540. of pleural empyema in the very elderly. Ann R Coll Surg Engl 2012;
80 Strachan RE, Cornelius A, Gilbert GL, et al, and the Australian 94: 33135.
Research Network in Empyema (ARNiE). A bedside assay to detect 101 Chambers A, Routledge T, Dunning J, Scarci M. Is video-assisted
Streptococcus pneumoniae in children with empyema. thoracoscopic surgical decortication superior to open surgery in the
Pediatr Pulmonol 2011; 46: 17983. management of adults with primary empyema?
81 Strachan RE, Cornelius A, Gilbert GL, et al. Pleural uid nucleic Interact Cardiovasc Thorac Surg 2010; 11: 17177.
acid testing enhances pneumococcal surveillance in children. 102 Kho P, Karunanantham J, Leung M, Lim E. Debridement alone
Respirology 2012; 17: 11419. without decortication can achieve lung re-expansion in patients with
82 Falguera M, Lpez A, Nogus A, Porcel JM, Rubio-Caballero M. empyema: an observational study. Interact Cardiovasc Thorac Surg
Evaluation of the polymerase chain reaction method for detection of 2011; 12: 72427.
Streptococcus pneumoniae DNA in pleural uid samples. Chest 2002; 103 Tacconi F, Pompeo E, Fabbi E, Mineo TC. Awake video-assisted
122: 221216. pleural decortication for empyema thoracis.
83 Wrightson JM, Rahman NM, Crook DW, Wray JA. Improving Eur J Cardiothorac Surg 2010; 37: 594601.
pathogen identication in pleural infectionapplication of molecular 104 Brutsche MH, Tassi GF, Gyrik S, et al. Treatment of
techniques. Am J Respir Crit Care Med 2012; 185: A5244 (abstr). sonographically stratied multiloculated thoracic empyema by
84 Muoz-Almagro C, Gala S, Selva L, Jordan I, Tarrag D, Pallares R. medical thoracoscopy. Chest 2005; 128: 330309.
DNA bacterial load in children and adolescents with pneumococcal 105 Ravaglia C, Gurioli C, Tomassetti S, et al. Is medical thoracoscopy
pneumonia and empyema. Eur J Clin Microbiol Infect Dis 2011; ecient in the management of multiloculated and organized
30: 32735. thoracic empyema? Respiration 2012; 84: 21924.
85 Saglani S, Harris KA, Wallis C, Hartley JC. Empyema: the use of 106 Wait MA, Sharma S, Hohn J, Dal Nogare A. A randomized trial of
broad range 16S rDNA PCR for pathogen detection. empyema therapy. Chest 1997; 111: 154851.
Arch Dis Child 2005; 90: 7073.
576 www.thelancet.com/respiratory Vol 3 July 2015
Series
107 Bilgin M, Akcali Y, Oguzkaya F. Benets of early aggressive 119 Davies HE, Rahman NM, Parker RJ, Davies RJ. Use of indwelling
management of empyema thoracis. ANZ J Surg 2006; 76: 12022. pleural catheters for chronic pleural infection. Chest 2008;
108 Lim TK, Chin NK. Empirical treatment with brinolysis and early 133: 54649.
surgery reduces the duration of hospitalization in pleural sepsis. 120 Corcoran JP, Ahmad M, Mukherjee R, Redmond KC. Pleuro-
Eur Respir J 1999; 13: 51418. pulmonary complications of rheumatoid arthritis. Respir Care 2014;
109 Lardinois D, Gock M, Pezzetta E, et al. Delayed referral and 59: 5559.
gram-negative organisms increase the conversion thoracotomy rate 121 Sasse S, Nguyen T, Teixeira LR, Light R. The utility of daily
in patients undergoing video-assisted thoracoscopic surgery for therapeutic thoracentesis for the treatment of early empyema.
empyema. Ann Thorac Surg 2005; 79: 185156. Chest 1999; 116: 170308.
110 Sonnappa S, Cohen G, Owens CM, et al. Comparison of urokinase 122 Chen KY, Liaw YS, Wang HC, Luh KT, Yang PC. Sonographic
and video-assisted thoracoscopic surgery for treatment of childhood septation: a useful prognostic indicator of acute thoracic empyema.
empyema. Am J Respir Crit Care Med 2006; 174: 22127. J Ultrasound Med 2000; 19: 83743.
111 Marhuenda C, Barcel C, Fuentes I, et al. Urokinase versus VATS 123 Teixeira LR, Sasse SA, Villarino MA, Nguyen T, Mulligan ME,
for treatment of empyema: a randomized multicenter clinical trial. Light RW. Antibiotic levels in empyemic pleural uid. Chest 2000;
Pediatrics 2014; 134: e130107. 117: 173439.
112 St Peter SD, Tsao K, Spilde TL, et al. Thoracoscopic decortication vs 124 Saroglou M, Tryfon S, Ismailos G, et al. Pharmacokinetics of
tube thoracostomy with brinolysis for empyema in children: Linezolid and Ertapenem in experimental parapneumonic pleural
a prospective, randomized trial. J Pediatr Surg 2009; 44: 10611. eusion. J Inamm (Lond) 2010; 7: 22.
113 Kurt BA, Winterhalter KM, Connors RH, Betz BW, Winters JW. 125 Liapakis IE, Kottakis I, Tzatzarakis MN, et al. Penetration of newer
Therapy of parapneumonic eusions in children: video-assisted quinolones in the empyema uid. Eur Respir J 2004; 24: 46670.
thoracoscopic surgery versus conventional thoracostomy drainage. 126 Mullins MM, Walker I, Standridge RD. Using povidone-iodine to
Pediatrics 2006; 118: e54753. treat empyema. J Wound Care 2001; 10: 15556.
114 Grijalva CG, Nuorti JP, Zhu Y, Grin MR. Increasing incidence of 127 Suissa S, DellAniello S, Ernst P. Long-term natural history of
empyema complicating childhood community-acquired pneumonia chronic obstructive pulmonary disease: severe exacerbations and
in the United States. Clin Infect Dis 2010; 50: 80513. mortality. Thorax 2012; 67: 95763.
115 Grabenstein JD, Musey LK. Dierences in serious clinical outcomes 128 Schmidt SA, Johansen MB, Olsen M, et al. The impact of
of infection caused by specic pneumococcal serotypes among exacerbation frequency on mortality following acute exacerbations
adults. Vaccine 2014; 32: 2399405. of COPD: a registry-based cohort study. BMJ Open 2014; 4: e006720.
116 Botianu PV, Dobrica AC, Butiurca A, Botianu AM. Complex space- 129 Guertler C, Wirz B, Christ-Crain M, Zimmerli W, Mueller B,
lling procedures for intrathoracic infectionspersonal experience Schuetz P. Inammatory responses predict long-term mortality risk
with 76 consecutive cases. Eur J Cardiothorac Surg 2010; 37: 47881. in community-acquired pneumonia. Eur Respir J 2011; 37: 143946.
117 Reyes KG, Mason DP, Murthy SC, Su JW, Rice TW. Open window 130 Bruns AH, Oosterheert JJ, Cucciolillo MC, et al. Cause-specic
thoracostomy: modern update of an ancient operation. long-term mortality rates in patients recovered from
ThoracCardiovasc Surg 2010; 58: 22024. community-acquired pneumonia as compared with the general
118 Palmen M, van Breugel HM, Geskes GG, et al. Open window Dutch population. Clin Microbiol Infect 2011; 17: 76368.
thoracostomy treatment of empyema is accelerated by vacuum- 131 Restrepo MI, Faverio P, Anzueto A. Long-term prognosis in
assisted closure. Ann Thorac Surg 2009; 88: 113136. community-acquired pneumonia. Curr Opin Infect Dis 2013; 26: 15158.
www.thelancet.com/respiratory Vol 3 July 2015 577
S-ar putea să vă placă și
- Basics and modern practice of nasal high-flow therapyDe la EverandBasics and modern practice of nasal high-flow therapyEvaluare: 5 din 5 stele5/5 (1)
- Medication Error 2017Document51 paginiMedication Error 2017Christina100% (1)
- D01 Pink Floyd Shine On You Crazy DiamondDocument1 paginăD01 Pink Floyd Shine On You Crazy Diamond박승길Încă nu există evaluări
- Screening and Early Detection: Epidemiological Basis For Disease Control - Fall 2001Document28 paginiScreening and Early Detection: Epidemiological Basis For Disease Control - Fall 2001Kharisma Rizqiah WahyuniÎncă nu există evaluări
- A. Complete The Dialogue With These WordsDocument19 paginiA. Complete The Dialogue With These WordsAnaMariaRamirezNavarrete100% (1)
- Epi Confounding AssignmentDocument4 paginiEpi Confounding Assignmentcharles100% (2)
- 06 Due 13th JanDocument9 pagini06 Due 13th JanWinson LauÎncă nu există evaluări
- 11U Poetry Analysis Four LevelsDocument1 pagină11U Poetry Analysis Four Levelsseiranhoj0901100% (1)
- Warfarin: Prof DR Shah MuradDocument63 paginiWarfarin: Prof DR Shah Muradshahmurad653376Încă nu există evaluări
- Warfarin Q and ADocument40 paginiWarfarin Q and AAbdul-Rhman Hamdy KishkÎncă nu există evaluări
- Name: Abdirahman Sheikh Abdillahi Farah Faculty: Clinical Officers (CO8) Course: Pediatric Lecturer: DR Amin Assingment: Pleural EffusionDocument46 paginiName: Abdirahman Sheikh Abdillahi Farah Faculty: Clinical Officers (CO8) Course: Pediatric Lecturer: DR Amin Assingment: Pleural EffusionAbdirahman Abdillahi FarahÎncă nu există evaluări
- PT InrDocument3 paginiPT InrJeniah Lerios OcsioÎncă nu există evaluări
- Stability Studies: A Measure of How A Pharmaceutical Product Maintains Its Quality Attributes Over TimeDocument99 paginiStability Studies: A Measure of How A Pharmaceutical Product Maintains Its Quality Attributes Over TimeFitsum DemissieÎncă nu există evaluări
- Screening Case Study Exercises - Hannah TurnerDocument4 paginiScreening Case Study Exercises - Hannah Turnerapi-457299309Încă nu există evaluări
- Basic Medical Wide QRS ArrhythmiaDocument39 paginiBasic Medical Wide QRS ArrhythmiaJee JunpyoÎncă nu există evaluări
- Thrombocytopenia Thrombocytopenia Thrombocytopenia ThrombocytopeniaDocument12 paginiThrombocytopenia Thrombocytopenia Thrombocytopenia ThrombocytopeniaRashed ShatnawiÎncă nu există evaluări
- Measures of Disease Frequency NOTESDocument22 paginiMeasures of Disease Frequency NOTESSJ Jung100% (1)
- Textbook Reference-Unit VI (p449) : Part 1 of 3Document53 paginiTextbook Reference-Unit VI (p449) : Part 1 of 3glenn johnstonÎncă nu există evaluări
- Immanuel KantDocument11 paginiImmanuel KantAshira GrevindaÎncă nu există evaluări
- Basic Clinical UrologyDocument7 paginiBasic Clinical Urologyreza sakaÎncă nu există evaluări
- Urinary Tract Infections PowerpointDocument22 paginiUrinary Tract Infections Powerpointsamdhathri100% (1)
- Lecture 07 Complex NumbersDocument30 paginiLecture 07 Complex NumbersOnofre Algara JrÎncă nu există evaluări
- Nephrostomy ReportDocument4 paginiNephrostomy ReportPatrick Lloyd Merino Jackson100% (1)
- Retroperitoneal and Soft TissueDocument59 paginiRetroperitoneal and Soft TissueLucas Phi100% (1)
- Glascow Coma ScaleDocument15 paginiGlascow Coma ScalePaul Henry RoxasÎncă nu există evaluări
- Solving Absolute Value Equation An D InequalitiesDocument7 paginiSolving Absolute Value Equation An D InequalitiesMohamed ArafaÎncă nu există evaluări
- Peripheral Vascular Medicine - Dr. Deduyo PDFDocument14 paginiPeripheral Vascular Medicine - Dr. Deduyo PDFMedisina101Încă nu există evaluări
- Pressure Ulcers and Wounds: by Monica Warhaftig, D.O. Assistant Professor of Geriatrics N.S.UDocument64 paginiPressure Ulcers and Wounds: by Monica Warhaftig, D.O. Assistant Professor of Geriatrics N.S.UEvaÎncă nu există evaluări
- ECG Interpretation UnismaDocument178 paginiECG Interpretation UnismadefinaÎncă nu există evaluări
- Coronary Artery Bypass Graft CabgsurgeryDocument26 paginiCoronary Artery Bypass Graft Cabgsurgeryfatha100% (1)
- Blood Coagulation and FibrinolysisDocument63 paginiBlood Coagulation and FibrinolysisNora AboshanadyÎncă nu există evaluări
- Calculus Practice Test: Directions: Solve The Following Problems. Show All Your WorkDocument5 paginiCalculus Practice Test: Directions: Solve The Following Problems. Show All Your WorkteachopensourceÎncă nu există evaluări
- Epidural Analgesia - A Self-Directed Learning Module 3rdDocument41 paginiEpidural Analgesia - A Self-Directed Learning Module 3rdAnnisa Chaerani BurhanuddinÎncă nu există evaluări
- Lesson1 PartI (Complex)Document59 paginiLesson1 PartI (Complex)Jayson Jonson AraojoÎncă nu există evaluări
- Vascular Surgery TNDocument4 paginiVascular Surgery TNVictor Matias BarriosÎncă nu există evaluări
- 13-Methods of RandomisationDocument4 pagini13-Methods of Randomisationhalagur75Încă nu există evaluări
- Complex NumbersDocument15 paginiComplex NumbersAnonymous jUaHPNGx9lÎncă nu există evaluări
- Introduction To Vascular SurgeryDocument13 paginiIntroduction To Vascular Surgeryapi-3858544100% (1)
- Parapneumonic Effusion - Case Study Adult IDocument59 paginiParapneumonic Effusion - Case Study Adult IJunior Future-Gastroenterologist Henry100% (1)
- Incidence and Prevalence PDFDocument9 paginiIncidence and Prevalence PDFSreya SanilÎncă nu există evaluări
- 08 - Abnormalities of R Wave ProgressionDocument3 pagini08 - Abnormalities of R Wave ProgressionSharan Murugaboopathy100% (1)
- Bundle Branch BlockDocument37 paginiBundle Branch BlocksyukronchalimÎncă nu există evaluări
- Basic Ecg: in The Eyes of NURSEDocument112 paginiBasic Ecg: in The Eyes of NURSESam jr TababaÎncă nu există evaluări
- ECG Interpretations DR RPDocument109 paginiECG Interpretations DR RPArnis Putri RosyaniÎncă nu există evaluări
- MATH 1F - 1 Real and Imaginary NumbersDocument3 paginiMATH 1F - 1 Real and Imaginary NumbersJay-pÎncă nu există evaluări
- Pharmacology QuestionsDocument15 paginiPharmacology QuestionsAnant KhotÎncă nu există evaluări
- Pressure Ulcers: Jorge G. Ruiz, MD, FACPDocument71 paginiPressure Ulcers: Jorge G. Ruiz, MD, FACPRomilPatelÎncă nu există evaluări
- Bladder IrrigationDocument19 paginiBladder IrrigationDwight Kristian CruzÎncă nu există evaluări
- Cardiac DysrhythmiasDocument3 paginiCardiac DysrhythmiasWilbert GuerreroÎncă nu există evaluări
- Dr. SK Mathur High Flow Nasal Oxygen TherapyDocument20 paginiDr. SK Mathur High Flow Nasal Oxygen TherapyAnish H Dave100% (1)
- Left Bundle Branch BlockDocument10 paginiLeft Bundle Branch BlockMochamad BasriÎncă nu există evaluări
- Diabetes MellitusDocument25 paginiDiabetes MellitusjljoioiuÎncă nu există evaluări
- FIX Leg UlcerDocument59 paginiFIX Leg UlcerDekka Andra100% (2)
- Sample ThesisDocument31 paginiSample ThesisPauline JaleaÎncă nu există evaluări
- Practice Quiz 2Document4 paginiPractice Quiz 2shivi250450% (2)
- Perioperative Management of AnticoagulationDocument33 paginiPerioperative Management of Anticoagulationmonge20Încă nu există evaluări
- EssayDocument7 paginiEssayIrma ImamovicÎncă nu există evaluări
- Anticoagulants 161120143945Document29 paginiAnticoagulants 161120143945Roshan SahuÎncă nu există evaluări
- Surgical Prophylaxis and SSIsDocument37 paginiSurgical Prophylaxis and SSIsTop Vids100% (1)
- K.5 CVS-K5 - Dynamics of Blood & Lymph Flow - EditedDocument36 paginiK.5 CVS-K5 - Dynamics of Blood & Lymph Flow - EditedWinson ChitraÎncă nu există evaluări
- Emergency Medicine Approach To Pleural EffusionDocument60 paginiEmergency Medicine Approach To Pleural EffusionCamilo VidalÎncă nu există evaluări
- Fibromyalgia - Revista NatureDocument16 paginiFibromyalgia - Revista NatureCamilo VidalÎncă nu există evaluări
- SSC GuidelinesDocument61 paginiSSC GuidelinesZfgZ*Încă nu există evaluări
- Acute Coronary SyndromesDocument1 paginăAcute Coronary SyndromesCamilo VidalÎncă nu există evaluări
- Jaundice-Applying Lessons PDFDocument8 paginiJaundice-Applying Lessons PDFCamilo VidalÎncă nu există evaluări
- Pathophysiology of Insulin ResistanceDocument8 paginiPathophysiology of Insulin ResistanceCamilo VidalÎncă nu există evaluări
- HaemMon and MGT 8 April 2013 Final PDFDocument95 paginiHaemMon and MGT 8 April 2013 Final PDFnadyajondriÎncă nu există evaluări
- Wms GOLD 2017 Pocket Guide 1 PDFDocument42 paginiWms GOLD 2017 Pocket Guide 1 PDFL P PutriÎncă nu există evaluări
- Capitulo Movimiento Voluntario-Corteza Motora PrimariaDocument26 paginiCapitulo Movimiento Voluntario-Corteza Motora PrimariaCamilo VidalÎncă nu există evaluări
- Acute PancreatitisDocument10 paginiAcute PancreatitisAndrés Menéndez RojasÎncă nu există evaluări
- CKD Etapa IV NjemDocument10 paginiCKD Etapa IV NjemCamilo VidalÎncă nu există evaluări
- Maxwell Quick Medical Reference PDFDocument35 paginiMaxwell Quick Medical Reference PDFAnonymous fj68Ms100% (10)
- The Sympathetic Nervous System in Heart FailureDocument18 paginiThe Sympathetic Nervous System in Heart FailureCamilo VidalÎncă nu există evaluări
- Pathophysiology of Portal HYPERTENSION PDFDocument11 paginiPathophysiology of Portal HYPERTENSION PDFCamilo VidalÎncă nu există evaluări
- Insuficiencia Cardiaca - The LancetDocument15 paginiInsuficiencia Cardiaca - The LancetCamilo VidalÎncă nu există evaluări
- A Case of Acute Myocardial Infarction Due To The Use PDFDocument3 paginiA Case of Acute Myocardial Infarction Due To The Use PDFCamilo VidalÎncă nu există evaluări
- Guia Angina Estable 2014 Acc AhaDocument21 paginiGuia Angina Estable 2014 Acc AhaCamilo VidalÎncă nu există evaluări
- NMS Pathology PDFDocument560 paginiNMS Pathology PDFGheorghiuManuela100% (8)
- Heart Failure and Kidney Dysfunction PDFDocument14 paginiHeart Failure and Kidney Dysfunction PDFCamilo VidalÎncă nu există evaluări
- 2011 Anticoagulant Pocket GuideDocument4 pagini2011 Anticoagulant Pocket GuideDragoljubJesenicÎncă nu există evaluări
- Recurrent Syncope in The Emergency DepartmentDocument3 paginiRecurrent Syncope in The Emergency DepartmentRoberto López MataÎncă nu există evaluări
- Acute Coronary SyndromesDocument1 paginăAcute Coronary SyndromesCamilo VidalÎncă nu există evaluări
- Internal MedicineDocument1.591 paginiInternal MedicineRina_Fatimah_Nuriila96% (46)
- Nasogastric Intubation Technique - Placement of Nasogastric Tube, ComplicationsDocument10 paginiNasogastric Intubation Technique - Placement of Nasogastric Tube, ComplicationsCamilo VidalÎncă nu există evaluări
- Fractura de EscafoidesDocument37 paginiFractura de EscafoidesCamilo Vidal100% (1)
- Taquiarritmias Supraventriculares NEJMDocument11 paginiTaquiarritmias Supraventriculares NEJMCamilo VidalÎncă nu există evaluări
- Ketone Bodies-A Review of Physiology, Pathophysiology and Application of Monitoring To DiabetesDocument15 paginiKetone Bodies-A Review of Physiology, Pathophysiology and Application of Monitoring To DiabetesCamilo VidalÎncă nu există evaluări
- Scaphoid Fracture - Overview and Conservative Treatment PDFDocument7 paginiScaphoid Fracture - Overview and Conservative Treatment PDFCamilo VidalÎncă nu există evaluări
- Molecular Physiology of Water BalanceDocument10 paginiMolecular Physiology of Water BalanceCamilo Vidal100% (1)
- Bio FilmDocument3 paginiBio FilmpbeomontÎncă nu există evaluări
- Chen Et Al 2009Document7 paginiChen Et Al 2009Hossein BesharatiÎncă nu există evaluări
- Ec RemovalDocument11 paginiEc Removalabhishek tippaÎncă nu există evaluări
- Ultimate Vaxx Detox Guide - Reverse Damage From The Deadly COVID VaccineDocument44 paginiUltimate Vaxx Detox Guide - Reverse Damage From The Deadly COVID Vaccinevitaolga7100% (2)
- Ict 1Document20 paginiIct 1meghaÎncă nu există evaluări
- NEET Biology Chapter Wise Mock Test - Biological Classification - CBSE TutsDocument17 paginiNEET Biology Chapter Wise Mock Test - Biological Classification - CBSE Tutssreenandhan 2017Încă nu există evaluări
- Foundation Course in Make Up ArtistryDocument118 paginiFoundation Course in Make Up ArtistrySUJAYÎncă nu există evaluări
- Microbiology Principles and Explorations 9Th Edition Black Solutions Manual Full Chapter PDFDocument29 paginiMicrobiology Principles and Explorations 9Th Edition Black Solutions Manual Full Chapter PDFlloydkieran71epfi100% (10)
- Microorganisms in Food PDFDocument22 paginiMicroorganisms in Food PDFLisnandaÎncă nu există evaluări
- Lactobacillus Acidophilus - Wikipedia, The Free EncyclopediaDocument5 paginiLactobacillus Acidophilus - Wikipedia, The Free Encyclopediahlkjhlkjhlhkj100% (1)
- Full Download Test Bank For Microbiology For The Healthcare Professional 2nd Edition Karin C Vanmeter Robert J Hubert PDF Full ChapterDocument35 paginiFull Download Test Bank For Microbiology For The Healthcare Professional 2nd Edition Karin C Vanmeter Robert J Hubert PDF Full Chaptertwistingafreetukl3o100% (18)
- Sbi3u Mini Test 2 Unit 1 AnswersDocument2 paginiSbi3u Mini Test 2 Unit 1 Answerschriston.mÎncă nu există evaluări
- Concept of Food Contamination and Food-Borne IllnessDocument88 paginiConcept of Food Contamination and Food-Borne IllnessSheirra SantosÎncă nu există evaluări
- Guidelines For Slaughtering Meat Cutting and Further ProcessingDocument148 paginiGuidelines For Slaughtering Meat Cutting and Further ProcessingAnh ThiÎncă nu există evaluări
- Comparisons of The Growth of Six Diatom Species Between Two Configurations of PhotobioreactorsDocument10 paginiComparisons of The Growth of Six Diatom Species Between Two Configurations of PhotobioreactorsJordan IsmaelÎncă nu există evaluări
- Sewage Fungus - A Field and Microscopic Guide (Version 3)Document33 paginiSewage Fungus - A Field and Microscopic Guide (Version 3)Chris WestÎncă nu există evaluări
- DNH Qualicon Brochure Ribo 1A-0771 1212 WEB PDFDocument11 paginiDNH Qualicon Brochure Ribo 1A-0771 1212 WEB PDFpatricioÎncă nu există evaluări
- Bio L 100 Bacterial Trans LabDocument11 paginiBio L 100 Bacterial Trans LabRohit ReddyÎncă nu există evaluări
- Otitis Media Paper 2024Document10 paginiOtitis Media Paper 2024shakeel.ahmedÎncă nu există evaluări
- Engineering Technology ComputerScienceDocument138 paginiEngineering Technology ComputerScienceprateek vyasÎncă nu există evaluări
- Bowel Nosodes - John PatersonDocument25 paginiBowel Nosodes - John PatersonIkram Manzoor100% (1)
- 1 Cell - Basics QP - Gcse Edexcel BiologyDocument5 pagini1 Cell - Basics QP - Gcse Edexcel BiologyChandrasekaran SubramaniamÎncă nu există evaluări
- EPRI Closed Cooling Water Chemistry Guideline, Revision 1Document182 paginiEPRI Closed Cooling Water Chemistry Guideline, Revision 1jycortes100% (7)
- YÖKDİL Fen Bilimleri Deneme Sınavı 3 PDFDocument18 paginiYÖKDİL Fen Bilimleri Deneme Sınavı 3 PDFSalmaanCadeXaajiÎncă nu există evaluări
- Koi Pond BeginnersDocument20 paginiKoi Pond BeginnersjackÎncă nu există evaluări
- Methods of Isolation of BacteriaDocument17 paginiMethods of Isolation of Bacteriarashmi regmiÎncă nu există evaluări
- Chemosensation of Bacterial Secondary Metabolites Modulates Neuroendocrine Signaling and Behavior of C. ElegansDocument14 paginiChemosensation of Bacterial Secondary Metabolites Modulates Neuroendocrine Signaling and Behavior of C. ElegansGülsüm YıldırımÎncă nu există evaluări
- 3M Solutions Biopharmaceutical Process Development - Manuf - ProcessMonitoringDocument13 pagini3M Solutions Biopharmaceutical Process Development - Manuf - ProcessMonitoringSergioÎncă nu există evaluări
- Corynebacterium Dyphtheriae: Corynebacterium Diphtheria Is A Pathogenic Gram Positive Bacillus Causing DiphtheriaDocument3 paginiCorynebacterium Dyphtheriae: Corynebacterium Diphtheria Is A Pathogenic Gram Positive Bacillus Causing DiphtheriaknedhÎncă nu există evaluări
- Pengertian & Guan TripalaDocument4 paginiPengertian & Guan Tripaladesti suci wulandariÎncă nu există evaluări
- The Obesity Code: Unlocking the Secrets of Weight LossDe la EverandThe Obesity Code: Unlocking the Secrets of Weight LossEvaluare: 4 din 5 stele4/5 (6)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe la EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityEvaluare: 4 din 5 stele4/5 (28)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDe la EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsÎncă nu există evaluări
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe la EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeEvaluare: 2 din 5 stele2/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDe la EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDEvaluare: 5 din 5 stele5/5 (2)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDe la EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionEvaluare: 4 din 5 stele4/5 (404)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDe la EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsEvaluare: 5 din 5 stele5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDe la EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisEvaluare: 4.5 din 5 stele4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedEvaluare: 5 din 5 stele5/5 (81)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDe la EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsEvaluare: 3.5 din 5 stele3.5/5 (3)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDe la EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisEvaluare: 4 din 5 stele4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDe la EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityEvaluare: 4 din 5 stele4/5 (3)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDe la EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningDe la EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningEvaluare: 4 din 5 stele4/5 (3)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)De la EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Încă nu există evaluări
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDe la EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisEvaluare: 3.5 din 5 stele3.5/5 (2)
- Gut: the new and revised Sunday Times bestsellerDe la EverandGut: the new and revised Sunday Times bestsellerEvaluare: 4 din 5 stele4/5 (393)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDe la EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryEvaluare: 4 din 5 stele4/5 (44)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.De la EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Evaluare: 4.5 din 5 stele4.5/5 (110)
- The Marshmallow Test: Mastering Self-ControlDe la EverandThe Marshmallow Test: Mastering Self-ControlEvaluare: 4.5 din 5 stele4.5/5 (58)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDe la EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessEvaluare: 4.5 din 5 stele4.5/5 (328)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingDe la EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingEvaluare: 4 din 5 stele4/5 (1138)
- Troubled: A Memoir of Foster Care, Family, and Social ClassDe la EverandTroubled: A Memoir of Foster Care, Family, and Social ClassEvaluare: 4.5 din 5 stele4.5/5 (27)