Documente Academic
Documente Profesional
Documente Cultură
Pps
Încărcat de
haripriyaDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Pps
Încărcat de
haripriyaDrepturi de autor:
Formate disponibile
Online ISSN: 2349-6940
Review Article DOI: 10.17354/cr/2016/249
Preprosthetic Surgery: Review of Literature
Haripriya Chari1, Khadar Vali Shaik2
Assistant Professor, Department of Oral and Maxillofacial Surgery, Kamineni Institute of Dental Sciences, Nalgonda, Telangana, India, 2Assistant
1
Professor, Department of Oral and Maxillofacial Surgery, MNR Dental College and Hospital, Sangareddy, Telangana, India
Following the loss of natural teeth after extraction, the bone begins to resorb. The results of this resorption are accelerated by wearing dentures
and tend to aect the mandible more severely than the maxilla. Besides, general factors include the presence of nutritional abnormalities and
systemic bone disease such as osteoporosis; endocrine dysfunction may aect bone metabolism. Preprosthetic surgical treatment must begin
with a thorough history and physical examination of the patient. Sometimes, there are contraindications to surgery because the patient suers
from serious general disease. Specic attention should also be given to laboratory tests which could inform us as to a degree of bone resorption.
Successful treatment with removable prosthesis is dependent on many factors. One component that can profoundly aect treatment success
is the condition of the denture-bearing tissues. Every eort should be made to ensure that both the hard and soft tissues are developed in a
form that will enhance the patients ability to wear a denture. It is the responsibility of the practitioner to carefully evaluate and identify the
need for any alteration of the denture-bearing areas and to educate the patient as to the importance of accomplishing this vital procedure.
Keywords: Alveolar ridge, Alveoloplasty, Prosthesis, Ridge augmentation
INTRODUCTION service to a truly reconstructive surgery when Kazanjian3
reported on the prototype of labiobuccal vestibuloplasty
Preprosthetic surgery is defined as the surgical procedures procedures to provide an additional denture-bearing surface
designed to facilitate fabrication of prosthesis or to improve for increased denture stability. His technique was modified
the prognosis of prosthodontic care. Preprosthetic surgery by Godwin4 (1947), Clark5 (1953), and Obwegeser6 (1963)
involves operations aiming to eliminate certain lesions or using skin grafts. Most procedures were centered on soft
abnormalities of the hard and soft tissues of the jaws so tissue corrections that allowed prosthetic devices to fit more
that the subsequent placement of the prosthetic appliances securely and function more comfortably.
is successful. For many years, preprosthetic oral surgery
consisted of the removal of teeth and the reduction of OBJECTIVES
humps, bumps, and sharp edges. During the last 15 years,
there has been renewed interest in preprosthetic surgery The objective of preprosthetic surgery is to create proper
which has fostered the development of many new supporting structures for subsequent replacement of
techniques. prosthetic appliance. Some of the characteristics of this ideal
form which provide for maximum support and stability and
Willard1 (1853) credited with being the first American dentist minimum interference with function are:
to do the reduction of interdental gingival papillae and
alveolar margins after dental extractions. This procedure Ridges that are broad and flat with a vertical height
permi ed earlier construction of artificial dentures. In 1876, (minimum 5 mm) provided by nearly parallel, non-
Beers2 advocated excisions of alveolus after extraction of undercut, bony walls. A firm resilient mucosal covering
teeth. He also specifically described the cu ing away of with nicely shaped buccal and lingual sulci which are
the bone if the alveolar process is unnaturally prominent. uninterrupted by frena, scars, or redundant tissue folds.
Preprosthetic surgery emerged from a ridge trimming An interarch distance of minimum 16-18mm, that allows
room for the denture and its components, is required. In the
Access this article online severely bony deficient mandible, it is essential to provide
bone bulk for strength and protection for the neurovascular
Month of Submission : 07-2016 bundles in bony dehisced mandibular canals. Ideally an
Month of Peer Review : 08-2016 arched palatal vault has to be provided. To deliver a post-
Month of Acceptance : 09-2016 tuberosity (hamular) notching to enhance the posterior
Month of Publishing : 09-2016
border seal and resistance of the denture to anterior
www.ijsscr.com
dislodging forces and freedom from neoplastic disease.
Corresponding Author:
Dr. Khadar Vali Shaik, MNR Dental College and Hospital, Sangareddy, Telangana, India. Phone: 99669786. E-mail: khadar.shaik04@gmail.com
IJSS Case Reports & Reviews | September 2016 | Vol 3 | Issue 4 9
Chari and Shaik: Pre-prosthetic Surgery
By fulfilling these goals as nearly as possible, the resultant reduction of tori and exostosis, reduction of hyperplastic
stable, properly extended conventional prosthesis should mucosa, and sophisticated techniques such as augmentation
allow wide distribution of functionally generated forces. of ridge through grafts, osteotomies and distraction
This should reduce the incidence and rate of adverse bone osteogenesis, and implants.
and soft tissue changes and permit satisfactory function
and esthetics. Alveoloplasty
Shaping of alveolar process is alveoloplasty which is
DISCUSSION indicated after almost every tooth extraction, whether it is
single or multiple. Willard,1 in 1853, reduced the alveolar
Preprosthetic surgery is essentially the surgical preparation margin after dental extraction. In 1876, Beers2 described
of either a fully edentulous or partially edentulous alveolectomy where a large portion of alveolus is removed
mouth before construction of dentures. It has developed with forceps. Molt,8 in 1923, performed alveoloplasty
from simple dentoalveolar correction of irregularities, retaining the interdental septum. Dean,9 in 1936, performed
exostosis, and hyperplastic tissues, to various vestibular alveoloplasty by removing interseptal bone and collapsing
lowering procedures, to major surgery of onlay and inlay buccal cortical plate. Obwegeser10 modified this technique in
augmentation and then into an era of scientifically tested 1966, by fracturing both labial and palatal cortices to reduce
and successful implants. Depending on the problem premaxillary protrusion.
involved surgery may vary, but the objectives of surgery
are to eliminate disease, conserve oral structures wherever Maxillary Tuberosity Reduction
possible and to provide best residual tissue to withstand There can be vertical or lateral excess of the maxillary
masticatory stresses, maintain function and retain esthetics tuberosity. Vertical excess interferes with proper orientation
for denture patient. Loss of teeth results in a gradual of occlusal plane and teeth se ing. The lateral excess limit
resorption of the alveolar ridge which poses a major the thickness of the buccal flange of denture between
problem for prosthetic replacement. The general pa ern of itself and the coronoid process and also cause problems
this resorption has been described by Tallgren7 (1972). The in path of insertion. Examination of mounted diagnostic
denture-bearing area progressively reduces causing loss cast is mandatory to assess the amount of removal. Careful
of retention and stability of the prostheses. The degree of radiographic evaluation should be done to rule out any
resorption of alveolar bone in the mandible is four times as chance of sinus perforation. The reduction is initiated with
high as that in the maxilla. The other problems include bony an elliptical incision and reflection of mucoperiosteum
undercuts, exostosis, palatal and lingual tori, lack of bone to expose the tuberosity. Bone is removed with rongeurs
height and width, soft tissue deficiency and redundancies, or burs. Smooth the area with bone file and irrigate with
and inappropriate soft tissue attachment. A thorough copious amount of saline. The wound is closed primarily.
evaluation outlining the problems to be solved and a
detailed treatment plan should be developed. Patients past Prominent Mylohyoid Ridge Reduction
medical history and current medical status must be reviewed Resorption in ridge height of posterior mandible makes
with particular a ention to allergies, drug idiosyncrasies, the mylohyoid ridge prominent and limits the extension of
hemorrhagic tendencies or systemic disorders that would the denture in this area. This is a common area of painful
require hospitalization, complicate anesthetic procedures, denture irritation. At times, the tonicity of the mylohyoid
increase surgical risk or possibly even contraindicate the ridge itself can cause problems with denture retention.
contemplated surgical procedure. Clinical examination of Gillies11 (1956) states that the mylohyoid ridge should be
hard and soft tissues, radiographic survey (panoramic and reduced whenever the ridge is found to be at the same level
lateral cephalogram), and if indicated advanced imaging as or a higher level than the alveolar process.
techniques such as computed tomography should be used
to enumerate any pathologic lesion of hard and soft tissues Exostoses and Tori
which should be a ended before actual treatment planning. Buccal exostoses are usually encountered on the buccal side
One way to evaluate the status of supporting tissues is to of the upper ridge. They interfere with proper adaptation
compare the patients ridge of ideal shape and form that of the flanges and border seal. They also impede with
has adequate bony support, resilient mucoperiosteum, proper flange contouring and teeth setting. They are
with no bony prominences, spicules and undercuts, and managed by surgical reduction. Torus palatinus or palatal
no pathologic lesions. Preservation of alveolar ridge and torus is a benign, slowly growing, bony projection of the
preparing the alveolar ridge for denture construction should palatine processes of the maxillae and occasionally of the
be done. horizontal plates of the palatine bones. Their etiology is
unknown. Heredity, superficial trauma, malocclusion, and
Preprosthetic surgical procedures include basic procedures functional response to mastication have been suggested
such as alveoloplasty, frenectomy, vestibuloplasty, as possible etiological factors. It is usually composed of
10 IJSS Case Reports & Reviews | September 2016 | Vol 3 | Issue 4
Chari and Shaik: Pre-prosthetic Surgery
cortical bone. Some may also contain cancellous bone. The preserved. The management of such hypermobile tissue
surgical removal of the palatine torus is indicated in case includes elimination of inflammation by giving a period
of traumatized overlying mucosa, torus completely filling of tissue rest, occlusal correction of complete denture by
the palatal vault and extending onto the soft palate beyond the new interocclusal record and remounting, good oral
the post dam area or presence of deep bony undercuts or hygiene and denture hygiene, or by mucostatic impression
interference with speech and deglutition and psychological technique to minimize irritation from dentures. It can also
causes. be managed by a surgical correction which includes simple
trimming of the excessive tissue but not disturbing the
Torus mandibularis or mandibular torus is an exostosis that a ached tissue, electrosurgery, subperiosteal dissection.
usually occurs bilaterally on the medial surface of the body However, the mucoperiosteal reflection should be minimal
and alveolar process of the mandible. They are generally to reduce post-operative bone resorption.
located in the canine-premolar region but are also found
as multiple bony nodules extending from the incisor to the The vertical and lateral soft tissue excess at the maxillary
molar region. The etiology of mandibular tori is unknown, tuberosity may interfere with proper orientation of occlusal
but they are thought by some to be a functional reaction plane, border seal of the post molar pocket area, and the
to masticatory stresses. Mandibular tori are composed of path of insertion. In such cases, removal is accomplished by
dense cortical bone with minimal amounts of a medullary sharp dissection or electrosurgery. However, if the tissue
core. The overlying mucoperiosteum is very thin, as it is is firm and does not interfere with thickness of denture
on the entire medial surface of the mandible. Laceration flange, path of insertion and denture stability, removal is
or traumatic ulceration of the mucosa is not uncommon. not indicated.
Mandibular tori are removed (1) when they become so large
that they cause speech impairment or diculty in eating, Frenectomy
(2) when the covering mucosa ulcerates as a result of trauma High a ached frena can cause loss of border seal that
and fails to heal, and (3) to facilitate the construction of deprives the retention of the upper denture. The deep labial
removable partial and complete dentures. notch on the denture to accommodate such prominent frena
will weaken the denture and increase the chance of midline
Reduction of Genial Tubercles fracture. The correction is achieved by diamond excision,
As the mandible begins to undergo resorption, the area Z-plasty, or V-Y-advancement technique. Prominent lingual
of the attachment of the genioglossus muscle in the frenum can cause various problems such as instability
anterior portion of the mandible may become increasingly of lower denture. As a tongue function test, the patient
prominent. In some cases, the tubercle may actually function should be able to touch the upper lip with the tip of the
as a shelf against which the denture can be constructed, but tongue without dislodging the lower denture. Otherwise,
it usually requires reduction to construct the prosthesis frenectomy is indicated. After frenectomy, the lower
properly. Before a decision to remove this prominence denture is inserted as a stent to prevent post-operative
is made, consideration should be given to possible relapse. A prominent buccal frenum rarely interferes with
augmentation of the anterior portion of the mandible rather denture function, as it is compressible and flaccid and not
than reduction of the genial tubercle. If augmentation is strong enough to dislodge the denture. Hence, they require
the preferred treatment, the tubercle should be left to add surgical correction only rarely.
support to the graft in this area. Local anesthetic infiltration
and bilateral lingual nerve blocks should provide adequate Epulis Fissuratum
anesthesia. Epulis fissuratum is the hyperplasia of sulcular epithelium
due to chronic irritation from an ill-fitting denture or
SOFT TISSUE PROCEDURES denture that has se led due to resorption. The hyperplasia
is in the form of 2-folds one outer and another one inner
Hyper Mobile Ridge and the sulcus in between may be ulcerated.
Hypermobile ridge tissue results from resorption of the
residual ridge under an ill-fi ing denture with unbalanced Papillary Hyperplasia
occlusion. It is most commonly seen in anterior part of Papillary hyperplasia is the result of ill-fi ing denture,
knife edge mandibular ridge. In anterior maxilla, this low-grade infection with Candida or due to the presence
usually results from anterior hyper occlusion of maxillary of palatal relief chamber in the denture. These are seen as
complete denture opposing mandibular natural teeth or intensely red soft polypoid masses of multiple papillary
Class I removable partial denture. Although removal of projections. Most of the lesion will resolve itself with
such redundant crystal tissue is almost always necessary, sucient tissue rest, oral hygiene, and denture hygiene.
any possibility of bony augmentation should be considered Any residual lesions that fail to resolve require surgical
before excision. In every case, the a ached tissue should be removal. The various methods available are electrocautery,
IJSS Case Reports & Reviews | September 2016 | Vol 3 | Issue 4 11
Chari and Shaik: Pre-prosthetic Surgery
sharp excision, cryosurgery, laser excision, laser ablations, hospitalization, donor-site surgery, or prolonged periods
and cure age with large rotary burs. without a denture. Disadvantages include unpredictability
of the amount of relapse of the vestibular depth, scarring in
Mental Nerve Repositioning the depth of the vestibule, and problems with adaptation
In patients with gross atrophy of the mandibular alveolar of the peripheral flange area of the denture to the depth of
process, the mental foramen may be found at or near the the vestibule.
crest of the residual ridge. When this occurs, the mental
nerve may be subjected to pressure from a denture flange. In addition to the a achment of labial muscles and soft
Patients with this condition often complain of a dull, tissues to the denture-bearing area, the mylohyoid and
burning sensation or a sudden sharp, severe pain of short genioglossus muscles in the floor of the mouth present
duration is similar to the pain of trigeminal neuralgia. The similar problems on the lingual aspect of the mandible.
pain may be initiated during mastication; it may also be Trauner17 described detaching the mylohyoid muscles
produced by digital pressure on the mental foramen. Some from the mylohyoid ridge area and repositioning them
patients complain of both pain and numbness in the lower inferiorly, eectively deepening the floor of the mouth area
lip. For many patients, these symptoms can be eliminated and relieving the influence of the mylohyoid muscle on the
merely by relieving the denture to avoid pressure on the denture. The technique for extension of the labial vestibule
mental foramen. However, in some cases, relief of the is a modification of a labially pedicled supraperiosteal flap
denture flange alone is not sucient to provide relief. In described by Clark.5 After the two vestibular extension
these instances, the mental foramina should be enlarged, techniques, a skin graft can be used to cover the area
and the neurovascular bundles surgically repositioned. of denuded periosteum. The combination procedure
eectively eliminates the dislodging forces of the mucosa
Ridge Extension Procedures and muscle a achments and provides a broad base of fixed
Vestibuloplasty is the surgical procedure designed to restore keratinized tissue on the primary denture-bearing area.
alveolar ridge heights by lowering muscle a achment on Split-thickness skin grafting with the buccal vestibuloplasty
the buccal, labial, and lingual aspects of the residual ridges. and floor-of-mouth procedure is indicated when adequate
Kazanjian,12 in 1935, described a method for deepening the alveolar ridge for a denture-bearing area is lost, but at least
vestibule in which a labial flap pedicled o the alveolar 15 mm of mandibular bone height remains. The remaining
process was used to cover the newly exposed bone while bone must have adequate contour so that the form of the
the lip surface was permi ed to reepithelize. The major alveolar ridge exposed after the procedure is adequate for
disadvantage of all these procedures is that scar contracture denture construction. If gross bony irregularities exist, such
on the labial aspect results in loss of vestibular depth. To as large concavities in the superior aspect of the posterior
overcome this disadvantage Clark5 (1953) recommended mandible, they should be corrected through grafting or
a vestibuloplasty procedure in which the flap is pedicled minor alveoloplasty procedures before the soft tissue
off the lip, rather than the alveolar process. To limit procedure. The technique has the advantage of the early
the regression that occurs after Clarks vestibuloplasty, covering of the exposed periosteal bed, which improves
Tortorelli13 (1968) recommended horizontal fenestration patient comfort and allows earlier denture construction.
of the periosteum along the base of the newly created In addition, the long-term results of vestibular extension
vestibule. Howe14 (1966) and Kethley and Gamble15 (1978) are predictable.
have described a modification of Kazanjians vestibuloplasty
termed as lip switch procedure, in which a labial Maxillary alveolar bone resorption frequently results in
mucosal flap is developed and extended to the crest of mucosal and muscle a achments that interfere with denture
the ridge from an initial lip incision. In 1959, Obwegeser16 construction, stability, and retention. Because of the large
described a technique for vestibuloplasty in the areas where denture-bearing area of the maxilla, adequate denture
enough bone and healthy mucosa exist but where muscle construction and stability can often be achieved after an
a achments are close to the crest of the alveolar ridge. extensive bone loss. However, the excess soft tissue may
This technique is termed as submucosal vestibuloplasty. accompany bony resorption, or soft tissue may require
When adequate mandibular height exists, this procedure modification as an adjunct to previous augmentation
increases the anterior vestibular area, which improves surgery. Several techniques provide additional fixed mucosa
denture retention and stability. The primary indications for and vestibular depth in the maxillary denture-bearing
the procedure include adequate anterior mandibular height area. The submucosal vestibuloplasty as described by
(at least 15 mm), inadequate facial vestibular depth from Obwegeser18 may be the procedure of choice for correction
mucosal and muscular a achments in the anterior mandible, of soft tissue a achment on or near the crest of the alveolar
and the presence of an adequate vestibular depth on the ridge of the maxilla. This technique is particularly useful
lingual aspect of the mandible. These techniques provide when maxillary alveolar ridge resorption has occurred, but
adequate results in many cases and generally do not require the residual bony maxilla is adequate for proper denture
12 IJSS Case Reports & Reviews | September 2016 | Vol 3 | Issue 4
Chari and Shaik: Pre-prosthetic Surgery
support. In this technique, the underlying submucosal tissue inferior grafting is accomplished using iliac crest bone
is either excised or repositioned to allow direct apposition grafts, secured with rigid fixation. Indications for the use of
of the labiovestibular mucosa to the periosteum of the this technique, in addition to atrophy of the alveolar ridge
remaining maxilla. To provide adequate vestibular depth area, included the prevention and management of fractures
without producing an abnormal appearance of the upper of the atrophic mandible. However, this technique does
lip, adequate mucosal length must be available in this area. not address abnormalities of the denture-bearing areas,
such as the increased interarch distance, superior border
When insucient labiovestibular mucosa exists and lip irregularities, or exposed position of the mental nerve,
shortening would result from a submucosal vestibuloplasty which result from mandibular atrophy.
technique, other vestibular extension techniques must be
used. In such cases, a modification of Clarks5 vestibuloplasty In visor osteotomy, the mandible is split buccolingually,
technique using mucosa pedicled from the upper lip and and the lingual cortical plate is repositioned superiorly.
sutured at the depth of the maxillary vestibule after a Horizontal osteotomy with interpositional graft was
supraperiosteal dissection can be used. The denuded designed to permit elevation of the superior aspect of the
periosteum over the alveolar ridge heals by secondary ridge to a predetermined height and grafting of the resulting
epithelialization. Moderate discomfort can occur in the defect. Corticocancellous iliac crest and cancellous marrow
post-operative period, and a longer healing time is required serve as sources for the graft. Corticocancellous blocks are
(6-8 weeks) before denture construction. formed to a predetermined size for augmentation and are
inserted between the pedicled bone and the mandible.
Ridge Augmentation Commonly, one block is used in the midline, two in the
Augmentation involves on laying or inlaying a graft cuspid regions, and two in the molar regions. The void
material onto or into the atrophic alveolar bone. The various between the cortical struts and at the graft interface with
techniques range from simple subperiosteal tunneling the mandible is packed with corticocancellous chips and
to extensive osteotomies which increase appreciably the cancellous marrow. Baker and Connole 21 (1977) have
postsurgical morbidity. To increase the residual alveolar described a technique for the direct augmentation of the
ridge, several options such as bone grafts, allografts, and maxilla with a contoured rib. The interpositional bone
distraction osteogenesis have been proposed. The indication graft is an osteotomy performed spli ing the superior
of each option varies according to site, amount of residual and inferior dimensions of the residual jaw and bone is
alveolar bone, cause of resorption and compliance of the grafted into the osteotomy. The techniques include Le Fort
patient. Autogenous bone grafts are widely considered osteotomy in maxilla and horizontal sandwich technique
the gold standard for severe ridge deformities. In case of for the anterior mandible. The procedure for interpositional
severe atrophy, iliac crest and calvarial bone grafts can be augmentation of the atrophic maxilla was first reported
used to harvest a significant amount of autogenous bone. by Farrell et al.,22 in 1976, Bell et al.23 (1977), and Bell and
Membranous bone is superior to endochondral grafts in Buckles24 (1978). Le Fort I osteotomy is described by Bell
maintaining volume and a higher tendency to resorption and McBride25 (1977). Interpositional bone grafting in the
of the iliac onlay grafts compared with the calvaria is due maxilla is indicated in the bone-deficient maxilla, where
to the dierent embryonic origin. the palatal vault is found to be adequately formed but
ridge height is insucient. Anteroposterior and transverse
Superior border augmentation with a bone graft is discrepancies between the maxilla and mandible can also
occasionally indicated when severe resorption of the be corrected by interpositional bone grafting techniques.
mandible results in inadequate height and contour and Interpositional grafting techniques provide stable and
potential risk of fracture or when the treatment plan calls predictable results by changing the maxillary position in
for placement of implants in areas of insucient bone height the vertical, anteroposterior, and transverse directions and
or width. The use of autogenous corticocancellous blocks of may eliminate the need for secondary soft tissue procedures.
iliac crest bone was described by Clementschisch,19 in 1948, Disadvantages of this type of procedure include the need
for superior border augmentation. Currently, these blocks of to harvest bone from an iliac crest donor-site and possible
bone are frequently secured to the mandible with small rigid secondary soft tissue surgery. However, an extension of
fixation screws, minimizing graft mobility. Tissue-guided the maxillary sinuses into the alveolar ridge may prevent
regeneration with the use of a membrane is often combined placement of implants in the posterior maxillary area
with the bony augmentation. In some cases, implants can because of insucient bony support. A sinus lift procedure
be placed at the same time the bone graft augmentation is a bony augmentation procedure that places graft material
is completed. Sanders and Cox20 reported the first clinical inside the sinus and augments the bony support in the
use of an inferior border technique for augmentation of the alveolar ridge area. In this technique, an opening is made
atrophic mandible. This technique is rarely, if ever, used in the lateral aspect of the maxillary wall, and the sinus
on occasion the augmentation of mandibular bulk with lining is carefully elevated from the bony floor of the sinus.
IJSS Case Reports & Reviews | September 2016 | Vol 3 | Issue 4 13
Chari and Shaik: Pre-prosthetic Surgery
Allogeneic bone, autogenous bone, or a combination of segment to produce a force vectored to seat the condyle
these materials can be used as a graft source in these areas. in the glenoid fossa. Intraoral subcondylar osteotomy is
a reasonable procedure when the setback is no >10 mm.
Total maxillary osteotomy with interpositional bone Sagi al osteotomy is an excellent technique for correction
grafting procedure should be considered when patients of mandibular protrusion. The total setback should not
lack both anterior and posterior bone but has good palatal exceed 10 mm, and the correction should be symmetric.
vault form. Patients who demonstrate a relative Class III If significant mandibular asymmetry is present, another
deformity secondary to bone loss and maxillary transverse technique should be chosen, or the procedure must also
deficiency should also be considered for this procedure. The be designed to utilize body osteotomies to correct the
palatal vault osteotomy and elevation can be achieved by asymmetry. To permit unimpeded retrusion of the distal
dierent surgical approaches. A total maxillary osteotomy segment and to prevent displacement of the proximal
with palatal vault elevation or a palatal vault osteotomy can segment, the internal pterygoid muscle must be detached
be performed. Both provide increased stability and palatal from the proximal segment.
vault depth by relying on pseudo augmentation of the
alveolar ridge. The total maxillary osteotomy with palatal The retrognathic mandible, though less frequently a
vault elevation allows for placement of interpositional bone prosthodontic problem than prognathism, deserves
grafts, if desired. The palatal vault osteotomy was originally consideration, for its correction can provide an optimal jaw
described by Charest and Goodyear.26 relationship that will enhance prosthetic reconstruction.
Sagittal osteotomy, as described for correction of
MAXILLOMANDIBULAR RIDGE RELATIONSHIPS prognathism or arching osteotomy, is the procedures
that yield the most predictable results. Variations of the
When the teeth are lost, an abnormal ridge relationship arcing ramus osteotomy procedure are the L osteotomy
result that complicates construction of prosthetic appliances. and the C osteotomy with modification by the sagi al
In totally edentulous patients, the interarch space and the spli ing of the inferior border of the mandible. Maxillary
anteroposterior and transverse relationships of the maxilla malrelationships commonly fall into one or more of
and mandible must be evaluated with the patients jaw at four categories: (1) Retrusion, (2) protrusion, (3) vertical
the proper occlusal vertical dimension. This determination deficiency, and (4) vertical excess. The maxillary protrusion
in the diagnostic phase may require the construction of is frequently associated with anterior maxillary vertical
bite rims with proper lip support. Lateral cephalometric excess. A retrognathic position of the maxilla may represent
radiographs are also necessary in this evaluation to confirm a true skeletal deformity or may be a relative retrusion
the clinical impression. Segmental alveolar surgery in the secondary to severe resorption of the alveolar process. An
partially edentulous patient supraeruption of teeth and occasionally associated the problem is that of a deficient
bony segments into an opposing edentulous area may transverse dimension. Edentulous Class III jaw relationships
decrease interarch space and preclude the construction of historically have been managed by mandibular setback
an adequate fixed or removable prosthetic appliance in this procedures, however, maxillary osteotomies used to change
area. If segmental surgery is to be considered, the models skeletal relationships have proved stable and reliable.
can be cut and teeth repositioned in their desired location. Therefore, after confirmation by appropriate analysis,
The dentist responsible for the final prosthetic restoration the retrusive maxilla is best corrected using a Le Fort I
of the patient must make the final determination of the osteotomy. The edentulous maxillary bone is usually thin
placement of the segments on the articulated models. After and even in minimal advancement corticocancellous grafts
model surgery, a splint is fabricated to locate placement of are indicated and applied as an onlay along the osteotomy
segments precisely at the time of surgery and to provide sites and as a block interposed between the tuberosities and
stability during the post-operative healing period. the pterygoid plates. If vertical deficiency coexists, vertical
height may be gained by interpositional grafting.
Corrective surgery for an edentulous protrusive mandible,
with few exceptions, should be performed on the ramus or Although a less common finding, protrusion or vertical
ramus-body portion of the jaw. Maximal denture-bearing excess or a combination of the two can impede prosthetic
surface and the transverse dimension of the mandibular eorts. Le Fort I osteotomy for correction of vertical excess
ridges should be maintained. Extraoral subcondylar is an excellent procedure and has the added advantage of
osteotomy is indicated for considerable correction versatility whereby individual segments may be altered in
(>12 mm) and for significant mandibular asymmetry. This the transverse, anteroposterior, or superior plane. Epker and
approach gives ready access for removal of the coronoid Wolford27 described a procedure for superior repositioning
process, stripping of the internal pterygoid muscle and of the maxilla leaving the nasal floor intact; however, in the
modification of proximal and distal bony segments to edentulous patient, this tends to compromise the depth
ensure good approximation and permits wiring of the of the palatal vault. In most instances, bone grafting of
14 IJSS Case Reports & Reviews | September 2016 | Vol 3 | Issue 4
Chari and Shaik: Pre-prosthetic Surgery
osteotomy sites is unnecessary with superior repositioning medical care and will have a positive influence in the field
of the maxilla. of preprosthetic surgery. Cell culture technology, originally
described for cultured skin and mucosal grafts, has opened
Implants a new era in the field of oral reconstructive surgery. The
In recent years, dental rehabilitation of edentulous patients major advantage of cell culture is the expansion of a small
using implant-supported prostheses has presented a biopsy specimen into the transplantable mucosal tissue
significant treatment alternative to conventional restoration by two to three orders of magnitude within a few weeks.
with a meaningful improvement in masticatory function Palatal mucosa was cultured and transplanted to replace
and well-being of edentulous patients. Ideal conditions for gingival mucosa and demonstrated that 4 months later the
implant success are residual bone height more than 10 mm grafts had formed a well-dierentiated keratinizing mucosa
and width more than 6 mm, normal maxilla-mandibular similar to the palatal mucosa in situ. Studies on production
relation, and healthy peri-implant soft tissues. The use of ex vivo intraoral skin/mucosal graft gave promising
of autogenous bone grafts with osseointegrated implants results, however, the complexity of the procedure, time,
seems to significantly reduce bone resorption. and cost is questioned when simple and fast autogenous
grafting techniques are possible. The absence of donor-site
Lasers morbidity should be considered as the most advantageous
Today, increasingly versatile and sophisticated lasers point of ex vivo produced grafts.
are available. These lasers vary in an application based
on the choice of dierent technologies, materials (gas, CONCLUSION
solids, semi-conductors, colorants, etc.), and a diversity
of wavelengths. These various wavelengths have made it Preprosthetic surgery is a rapidly changing area of
possible for laser technology to become a safe, simplified, dentistry. Knowledge of the range, capabilities, and
and effective component in current oral surgery. As limitations of the commonly used surgical procedures
the laser has the ability to vaporize soft tissues without is a must for anyone treating a patient who will receive
bleeding, the wound heals without scar formation and complete denture prosthesis. It cannot be overemphasized
without any deformation of the healed site. Moreover, that the establishment of a clear treatment plan and close
there is no need for sutures, which is the most important coordination of all specialties involved in the reconstructive
eect in the field of preprosthetic surgery, as any loss in eort are essential to achieve the best overall result.
vestibule lengths provoked by the suture is avoided. This
wavelength is perfectly adapted for patients requiring soft REFERENCES
tissue preparation management.
1. Willard AT. Preparing the mouth for full sets of artificial teeth.
Dent Newsl 1853;6:238.
Alveolar Distraction Osteogenesis 2. Beers WG. Notes from practice. Dent Cosm 1876;18:118.
In larger defects, alveolar distraction osteogenesis is an 3. Kazanjian VH. Surgical operations are related to satisfactory
alternative treatment for bone and soft tissue reconstruction. dentures. Dent Cosm 1924;66:387.
4. Godwin JG. Submucous surgery for be er denture service. J Am
This process is based on the concept of bone distraction
Dent Assoc 1947;34:678-86.
along a vector that is transverse to the long axis of the bone, 5. Clark HB Jr. Deepening of labial sulcus by mucosal flap
which results in bone formation. It was later applied to the advancement: Report of a case. J Oral Surg 1953;11:165.
human mandible, and more recent clinical reports have 6. Obwegeser H. Die totalen mund bodenplastik. Schweiz Mschr
shown that alveolar distraction osteogenesis is eective for Zahnheilk 1963;73:565-71.
7. Tallgren A. The continuing reduction of the residual alveolar ridges
treating severe forms of alveolar ridge atrophy. A primary
in complete denture wearers: A mixed longitudinal study covering
advantage of distraction osteogenesis is that there is no need 25 years. J Prosthet Dent 1972;31:120-32.
for additional surgery at the donor site. Another benefit is 8. Molt FF. The anesthetic and surgical problems in alveolectomy.
the coordinated lengthening of the bone and associated Dent Summ 1923;45:854.
soft tissues. To obtain successful results both hard and 9. Dean OT. Surgery for the denture patient. J Am Dent Assoc
1936;23:2124.
soft tissues should be lengthened and widened. Alveolar
10. Obwegeser HO. Conference on Comprehensive Oral Surgery.
distraction osteogenesis is the best technique for soft tissue Washington, DC: American Society of Oral Surgeons; 1966.
lengthening in a defective alveolus. Especially in moderate 11. Gillies RL. A surgical aid to a prosthetic problem. Aust Dent J
and severe defects, this technique enables restoration of soft 1956;1:329.
tissues with desired quality and volume. 12. Kazanjian WH. Surgery as an aid to more ecient service with
prosthetic dentures. J Am Dent Assoc 1935;22:566.
13. Tortorelli AF. A technique for vestibular sulcus extension.
Tissue Engineering J Prosthet Dent 1968;20:14.
Tissue engineering, the science of growing living human 14. Howe GL. Preprosthetic surgery in the lower labial sulcus. Dent
tissue for transplantation, opens new perspectives in Pract Dent Rec 1965;16:119-24.
IJSS Case Reports & Reviews | September 2016 | Vol 3 | Issue 4 15
Chari and Shaik: Pre-prosthetic Surgery
15. Kethley JL Jr, Gamble J. The lipswitch: A modification of on a new concept of treatment. Oral Surg Oral Med Oral Pathol
Kazanjians labial vestibuloplasty. J Oral Surg 1978;36:701-5. 1977;43:485-98.
16. Obwegeser H. Die submukosevestibuloplastik, dtsch. Zahnaerztl Z 24. Bell WH, Buckles RL. Correction of the atrophic ridge by
1959;14:629-749. interpositional bone grafting: A progress report. J Oral Surg
17. Trauner R. Alveoloplasty with ridge extensions on the lingual side 1978;36:693-700.
of the lower jaw to solve the problem of a lower dental prosthesis. 25. Bell WH, McBride KL. Correction of long face syndrome by Le
Oral Surg Oral Med Oral Pathol 1952;5:340-6. Fort I osteotomy. A report on some new technical modifications
18. Obwegeser H. Surgical preparation of the maxilla for a prosthesis. and treatment results. Oral Surg Oral Med Oral Pathol
J Oral Surg Anesth Hosp Dent Serv 1964;22:127-34. 1977;44:493-520.
19. Clementschisch F. In: Pichler H, Trauner R, editors. Mund - Und 26. Charest A, Goodyear V. Palatal osteotomy: A simple approach to
Kiefer - Chirurgie. Wein: Verlag von Uban und Schwarzenberg; maxillary alveolar atrophy. J Oral Surg 1976;34:442-4.
1948. p. 524. 27. Epker BN, Wolford LM. Middle-third face osteotomies: Their use
20. Sanders B, Cox R. Inferior border rib grafting for augmentation in the correction of developmental and acquired dentofacial and
of atrophic edentulous mandible. J Oral Surg 1976;34:897-900. craniofacial deformities. J Oral Surg 1975;33:491-514..
21. Baker RD, Connole PW. Preprosthetic augmentation grafting--
autogenous bone. J Oral Surg 1977;35:541-51.
22. Farrell CD, Kent JN, Guerra LR. One stage interpositional bone
How to cite this article: Chari H, Shaik KV. Preprosthetic Surgery: Review
grafting and vestibuloplasty of the atrophic maxilla. J Oral Surg of Literature. IJSS Case Reports & Reviews 2016;3(4):9-16.
1976;34:901-6.
23. Bell WH, Buche WA, Kennedy JW 3 rd, Ampil JP. Surgical
Source of Support: Nil, Conflict of Interest: None declared.
correction of the atrophic alveolar ridge. A preliminary report
16 IJSS Case Reports & Reviews | September 2016 | Vol 3 | Issue 4
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Year 11 Physics HY 2011Document20 paginiYear 11 Physics HY 2011Larry MaiÎncă nu există evaluări
- 1 s2.0 S0266435616303370Document5 pagini1 s2.0 S0266435616303370haripriyaÎncă nu există evaluări
- Oral Presentations HandoutDocument5 paginiOral Presentations HandoutNikki M. ArapolÎncă nu există evaluări
- CUPDocument32 paginiCUPharipriyaÎncă nu există evaluări
- Surgery Long CasesDocument89 paginiSurgery Long CasesharipriyaÎncă nu există evaluări
- Does Janani Shishu Suraksha Karyakram Ensure Cost-Free Institutional Delivery? A Cross-Sectional Study in Rural Bankura of West Bengal, IndiaDocument7 paginiDoes Janani Shishu Suraksha Karyakram Ensure Cost-Free Institutional Delivery? A Cross-Sectional Study in Rural Bankura of West Bengal, IndiaharipriyaÎncă nu există evaluări
- Osteoradionecrosis UpdateDocument8 paginiOsteoradionecrosis UpdateAnuj AggarwalÎncă nu există evaluări
- Smoking and PolycythemiaDocument9 paginiSmoking and PolycythemiaharipriyaÎncă nu există evaluări
- Sterilization and DisinfectionDocument100 paginiSterilization and DisinfectionReenaChauhanÎncă nu există evaluări
- Office of The Court Administrator v. de GuzmanDocument7 paginiOffice of The Court Administrator v. de GuzmanJon Joshua FalconeÎncă nu există evaluări
- Helen Hodgson - Couple's Massage Handbook Deepen Your Relationship With The Healing Power of TouchDocument268 paginiHelen Hodgson - Couple's Massage Handbook Deepen Your Relationship With The Healing Power of TouchLuca DatoÎncă nu există evaluări
- Dealer DirectoryDocument83 paginiDealer DirectorySportivoÎncă nu există evaluări
- Tentative Seat Vacancy For CSAB Special Rounds-202Document92 paginiTentative Seat Vacancy For CSAB Special Rounds-202Praveen KumarÎncă nu există evaluări
- Product Manual: Control Cabinet M2001Document288 paginiProduct Manual: Control Cabinet M2001openid_6qpqEYklÎncă nu există evaluări
- Executive Support SystemDocument12 paginiExecutive Support SystemSachin Kumar Bassi100% (2)
- Beyond Digital Mini BookDocument35 paginiBeyond Digital Mini BookAlexandre Augusto MosquimÎncă nu există evaluări
- Transpetro V 5 PDFDocument135 paginiTranspetro V 5 PDFadityamduttaÎncă nu există evaluări
- Swedenborg's Formative Influences: Jewish Mysticism, Christian Cabala and PietismDocument9 paginiSwedenborg's Formative Influences: Jewish Mysticism, Christian Cabala and PietismPorfirio MoriÎncă nu există evaluări
- Zeng 2020Document11 paginiZeng 2020Inácio RibeiroÎncă nu există evaluări
- Marikina Polytechnic College Graduate School Scientific Discourse AnalysisDocument3 paginiMarikina Polytechnic College Graduate School Scientific Discourse AnalysisMaestro Motovlog100% (1)
- Syllabus Sibos CLTDocument5 paginiSyllabus Sibos CLTgopimicroÎncă nu există evaluări
- Inflammatory Bowel DiseaseDocument29 paginiInflammatory Bowel Diseasepriya madhooliÎncă nu există evaluări
- Balochistan Conservation Strategy VDocument388 paginiBalochistan Conservation Strategy VHãšãñ Trq100% (1)
- License Key Windows 8Document7 paginiLicense Key Windows 8Juned FahriÎncă nu există evaluări
- Understanding Learning Theories and Knowledge AcquisitionDocument38 paginiUnderstanding Learning Theories and Knowledge AcquisitionKarl Maloney Erfe100% (1)
- SyllabusDocument8 paginiSyllabusrickyangnwÎncă nu există evaluări
- Cover Me: Music By: B. Keith Haygood Arranged By: BKH Lyrics By: Based On Exodus 33Document8 paginiCover Me: Music By: B. Keith Haygood Arranged By: BKH Lyrics By: Based On Exodus 33api-66052920Încă nu există evaluări
- Gcu On Wiki PediaDocument10 paginiGcu On Wiki Pediawajid474Încă nu există evaluări
- Study Habits Guide for Busy StudentsDocument18 paginiStudy Habits Guide for Busy StudentsJoel Alejandro Castro CasaresÎncă nu există evaluări
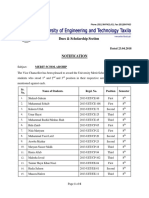
- Dues & Scholarship Section: NotificationDocument6 paginiDues & Scholarship Section: NotificationMUNEEB WAHEEDÎncă nu există evaluări
- Lucid Motors Stock Prediction 2022, 2023, 2024, 2025, 2030Document8 paginiLucid Motors Stock Prediction 2022, 2023, 2024, 2025, 2030Sahil DadashovÎncă nu există evaluări
- ToonHub - Articles of PartnershipDocument13 paginiToonHub - Articles of PartnershipKingÎncă nu există evaluări
- Bhikkhuni Patimokkha Fourth Edition - Pali and English - UTBSI Ordination Bodhgaya Nov 2022 (E-Book Version)Document154 paginiBhikkhuni Patimokkha Fourth Edition - Pali and English - UTBSI Ordination Bodhgaya Nov 2022 (E-Book Version)Ven. Tathālokā TherīÎncă nu există evaluări
- Senior Civil Structure Designer S3DDocument7 paginiSenior Civil Structure Designer S3DMohammed ObaidullahÎncă nu există evaluări
- Introduction To Alternative Building Construction SystemDocument52 paginiIntroduction To Alternative Building Construction SystemNicole FrancisÎncă nu există evaluări
- BMW E9x Code ListDocument2 paginiBMW E9x Code ListTomasz FlisÎncă nu există evaluări
- Hydrocarbon LawDocument48 paginiHydrocarbon LawParavicoÎncă nu există evaluări