Documente Academic
Documente Profesional
Documente Cultură
Physical Therapy Clinical Management.9 PDF
Încărcat de
Claudia MicuTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Physical Therapy Clinical Management.9 PDF
Încărcat de
Claudia MicuDrepturi de autor:
Formate disponibile
S P E C I A L R E P O R T
Physical Therapy Clinical
Management Recommendations
for Children with Cerebral Palsy -
Spastic Diplegia: Achieving
Functional Mobility Outcomes
Margaret E. ONeil, PhD, PT, MPH, Maria A. Fragala-Pinkham, MS, PT, Sarah L. Westcott, PhD, PT, Karen Martin, PT,
M.Ed, Lisa A. Chiarello, PhD, PT, PCS, Joanne Valvano, PhD, PT, Rachel Unanue Rose, PhD, PT, PCS
Drexel University (M.E.ON., L.A.C.), Philadelphia, PA; Franciscan Hospital for Children (M.A.F-P.), Boston, MA;
University of Puget Sound (S.L.W.), Tacoma, WA; Federal Way Public Schools (K.M.), Federal Way, WA; University of
Colorado at Denver & Health Sciences Center, (J.V.) Denver, CO; University of Alabama (R.U.R.), Birmingham, AL
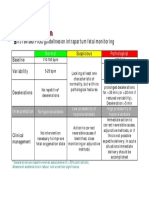
The purpose of this special report is to present recommendations for the clinical management of children with
cerebral palsy, spastic diplegia when increased functional mobility is the identified outcome. These recom-
mendations provide a framework that allows physical therapists to increase their accountability and promote
effective interventions for improved patient outcomes. The key components of this special report on clinical
management are: a) the Major Recommendations that provide the background and evidence for clinical
management; b) a flow chart to assist in clinical decision-making; and c) a Table of Tests and Measures for
information on useful tools in the management of children with spastic diplegia. These recommendations are
suggestions for clinical management, not an all-inclusive document on physical therapy for children with
cerebral palsy. These recommendations may help therapists develop systematic approaches to service delivery
and documentation. (Pediatr Phys Ther 2006;18:49 72) Key Words: adolescent, child, cerebral palsy, physical
therapy/procedures, practice guidelines
INTRODUCTION environment that is challenged by diminishing resources and
Clinical Management the call for increased accountability.1 Clinical management
includes recommendations for the care of patients/clients
Clinical management in physical therapy provides a with specific diagnoses or conditions. Clinical management is
framework to enhance the organizational capacity of services; important in and across all service delivery settings including
integrate evidence for best-practice; and improve outcomes. hospital, clinic, and community environments. Because a ma-
Recommendations for clinical management can be an effec- jority of pediatric physical therapy is provided in community-
tive method from which guidelines, pathways, and algorithms based settings, it is important that pediatric physical therapy
can be developed to improve quality of care in a health care clinical management includes communication across service
delivery settings to ensure quality patient care and maximize
outcomes.
0898-5669/06/1801-0049 An important function of clinical management is to ap-
Pediatric Physical Therapy
Copyright 2006 Lippincott Williams & Wilkins, Inc. and Section on ply evidence from the clinical and scientific literature to help
Pediatrics of the American Physical Therapy Association. the practitioner determine the appropriateness of selected in-
terventions and choices in patient management.1
Address correspondence to: Margaret E. ONeil, PhD, PT, MPH, Drexel Physical Therapy Clinical Management Recommen-
University, Programs in Rehabilitation Sciences, 245 N. 15th Street, Mail
Stop 502, Philadelphia, PA 19130; Email: moneil@drexel.edu dations for Children with Cerebral Palsy Spastic Diplegia
DOI: 10.1097/01.pep.0000202099.01653.a9
(PTCMR-SD), addresses a specific outcome, increased func-
tional mobility, for children and youth with spastic diplegia.
Pediatric Physical Therapy Clinical Management of Children with Spastic Diplegia 49
Why Develop Task Specific Clinical Management management for children with cerebral palsy, spastic diple-
Recommendations For Children With Cerebral gia. These recommendations were developed based on sev-
Palsy? eral resources and theoretical concepts. General informa-
Cerebral palsy is a neurodevelopmental condition that tion was gathered at focus groups to identify practice
begins in infancy or early childhood and is present through patterns during the Section on Pediatrics Research Round-
the lifespan.2 Cerebral palsy is the most frequently reported table Meetings at the American Physical Therapy Associa-
diagnosis for children who receive physical therapy.3 Spas- tions Combined Sections Meetings in 1999 and 2000.6 The
tic cerebral palsy is most common and includes diplegia Task Force then developed recommendations using data
and hemiplegia. Spastic diplegia is characterized by in- from these meetings, available evidence on best practice,
creased stiffness in the lower extremities, minimal involve- and clinical experience.7 This document on clinical man-
ment in the upper extremities and trunk weakness.4 Chil- agement is organized into three specific sections: 1) a nar-
dren with cerebral palsy most often receive physical rative with recommendations and supporting references,
therapy in the home, school or community.5 Because large 2) a general flow chart illustrating considerations in clini-
numbers of children with cerebral palsy receive physical cal decision-making and management and 3) a Table of
therapy services and children with spastic diplegia often Tests and Measures used in clinical management.
receive services in isolated community settings, recom-
mendations for clinical management may help therapists What Models Were Used To Develop This
develop a systematic plan of care for children with spastic Framework For Clinical Management?
diplegia. The Guide to Physical Therapist Practice8 (Guide) and
PTCMR-SD were developed to provide structure to the World Health Organization (WHO) International Classi-
physical therapy services for children and adolescents with fication of Function (ICF)9 were used to provide a structural
spastic diplegia across all settings (including home, school, framework to the PTCMR-SD and to identify components of
medical setting, community) and in all service delivery patient care. Brief definitions from the Guide and ICF are
models (community-based, home-based, clinic-based). provided in Table 1 and Table 2. Therapists are referred to
These recommendations should assist the new physical both documents for detailed information.
therapist (PT), the experienced PT and the PT who is not a Practice Pattern 5C in the Guide: Impaired motor
specialist in pediatrics. Potentially, more experienced pe- function and sensory integrity associated with non-pro-
diatric therapists could use these recommendations as a gressive disorders of the central nervous system congen-
quick checklist or resource to confirm or refine their clin- ital origin or acquired in infancy or childhood8 provided
ical management of children with spastic diplegia. Further, the structure for the intervention strategies included in
the recommendations may be helpful to PTs that are devel- these recommendations for clinical management. The fol-
oping clinical competence focusing on examination, eval- lowing concepts also were integrated into these recom-
uation, anticipated goals, and interventions for children mendations:
and adolescents with spastic diplegia. functional outcomes
the principles of family-centered care10,11
How Were These Clinical Management applications of task-oriented approaches to inter-
Recommendations Developed? vention1214
In 1999 the Section on Pediatrics, appointed a Task dynamic systems theory of motor learning and con-
Force to develop practice recommendations for clinical trol.1517
TABLE 1
Definitions of Terms used in the Guide to Physical Therapist Practice8
Examination A comprehensive screening and process of specific testing to determine a diagnosis or the need for referral to other
health practitioners. Three components of the examination are: the patient/client history; systems review; and tests
and measures.
Evaluation and PT A dynamic process in which the physical therapist evaluates and synthesizes the examination findings to help
Diagnosis determine prognosis and plan of care.
Prognosis and Plan of Identification of the optimal improvement level expected through intervention and the time needed to reach this level.
Care Plan of care includes definition of intensity of therapy (frequency and duration). This clinical management
framework includes identification of preventive approaches to plans of care for children with cerebral palsy.
Intervention The interaction between the therapist and the patient and other members of the patients health team as appropriate.
Intervention may occur on three levels:communication, coordination, and documentation; patient related
instruction; and procedural intervention.
Outcomes and The results of physical therapy intervention during an episode of care. Outcomes include anticipated goals and
Reexaminations expected outcomes as identified by the physical therapist and child/family. Reexaminations are conducted during
intervention to determine change in patient status and to revise the intervention plan as indicated.
Episode of Care A defined number or identified range of number of visits for physical therapy services provided by a physical therapist
in an unbroken sequence and related to interventions for a specific condition/problem or related to a patient, family
member or other providers request. Episodes of care may vary on level of intensity (frequency or duration).
50 ONeil et al Pediatric Physical Therapy
TABLE 2
The WHO Enablement Model (ICF): 9 Definitions of the levels of ability considered in the context of the patient/client social and physical environment
Body Structure/Function The limitations in anatomical structure and physiological function of the body (similar to the pathophysiology and
impairment levels of the NCMRR Disablement Model)
Activities The execution of a task or action by an individual (similar to the functional limitation level of the NCMRR
Disablement Model)
Participation Involvement in a life situation (similar to the disability/societal limitation levels of the NCMRR Disablement Model)
Components Of The Clinical Management prove outcomes and lead to more effective and efficient care
Recommendations for children with spastic diplegia.
The three components include: 1) Major Recommen-
dations (with references); 2) a Physical Therapy Clinical
Conclusion
Management Decision Making Flow Chart (Figure 1), and
the Appendix A: a Table of Tests and Measures. Again we would like to caution users of these recom-
It is important to note that these are recommendations mendations for physical therapy clinical management that
or suggestions for clinical management. This is not an all- this document is a guide and not all-inclusive for providing
inclusive document for providing physical therapy to chil- physical therapy services to children with cerebral palsy.
dren with cerebral palsy. These recommendations were de- We believe these recommendations will help therapists de-
veloped based on a specific task for which a physical velop systematic approaches to service delivery and docu-
therapist may be providing service. The specific task is mentation that will contribute to evidence-based practice
functional mobility, which may take different forms de- and enhanced outcomes. This document should help ther-
pending on the childs abilities, goals, and age. A task- apists become even more reflective practitioners and pro-
driven model was chosen to provide more functional rele- mote use of the most effective interventions.
vance to these recommendations for clinical management.
ACKNOWLEDGMENTS
Future Work The authors would like to thank the Executive Com-
We suggest that these recommendations for clinical mittee for the Section on Pediatrics of the American Phys-
management be revised periodically to reflect the current lit- ical Therapy Association for their support of this project.
erature and new trends in medical and rehabilitation manage- We would like to acknowledge the support of former Task
ment of children with spastic diplegia. In the future, the ref- Force members Carol Gildenberg Dichter, PhD, PT, PCS
erences could be coded according to the strength of scientific and Margo Orlin, PhD, PT, PCS for their contributions in
evidence as in Sacketts Levels of Evidence.18,19 If references the initial development of the Task Force activities. Also
are coded, this document could be used to identify research we would like to thank past graduates from Drexel Univer-
initiatives that are needed in clinical management of children sity, Victoria Gocha Marchese, PhD, PT and Beth Tieman,
with spastic diplegia. Additionally this document could pro- PhD, PT, for their assistance in the early stages of the Task
vide the foundation for clinical guidelines or pathways to im- Force.
Pediatric Physical Therapy Clinical Management of Children with Spastic Diplegia 51
Fig. 1.
52 ONeil et al Pediatric Physical Therapy
EXAMINATION law (IDEA Part C) and state laws, reexaminations may be
Examinations are conducted to identify the specific done at any time by parent request but are often conducted
functional mobility strengths and needs of the child and at six-month intervals in addition to a yearly full re-exam-
family using a functional outcomes or top down approach. ination.
The method used to conduct an examination is determined Special Considerations for Children and Youth (Three
by the purpose of the examination, the childs functional to 21 Years)
ability, the family and child needs, the childs age, and the In preschool and school settings, according to fed-
eral law (IDEA Part B) and state laws, formal reexamina-
service delivery setting.20
tions may be conducted annually but are required every
Where? Examinations occur in a variety of environ-
three years. Written family permission is required for for-
ments depending on the childs age, family preference, the
mal examinations in the school setting.
reason for examination, type of service delivery model, and
What?
agency/program in which the child is enrolled.
Examination is a comprehensive process with three
General Considerations for All Ages
components, including: 1) Patient history - interviewing
Infants, children and youth may receive services in a
or chart review to identify childs past and current func-
variety of settings (school, hospital, an outpatient facility
tional and health needs; 2) Systems review brief screen-
or community agency). Inpatient hospital services are of-
ing to identify functional mobility needs, which is the spe-
ten indicated after surgery while outpatient, home health
cific purpose of this task driven model and 3) Tests and
or other community settings may be appropriate for spe-
measures gathering specific data to establish plan of
cific episodes of care and for older children.
care.8
Special Considerations for Infants and Toddlers (Birth
How?
to Three Years)
Patient History. Histories are performed through a
Examinations may be initiated in the hospital set- structured family interview and systematic medical or ed-
ting (e.g. Neonatal Intensive Care Unit (NICU)) for infants ucational chart review.
born prematurely and/or with low birth weight. Infants General Considerations for All Ages
born premature or with low birth weight are at risk for Information about the childs mobility skills and
developing spastic diplegia.21 health status is obtained through a systematic child and
Infants with or at risk for spastic diplegia may be ex- family interview and chart review. Important medical in-
amined in an early intervention community setting as defined formation includes past surgeries, spasticity management
under the Individuals with Disabilities Education Act (IDEA), interventions, medications, and review of hip and spine
Part C. Examinations take place in natural environments, x-rays and gait studies. Important social/developmental/
which are often in the childs home but could also include educational information includes family and childs expe-
childcare settings or other community sites.22 riences and expectations and childs placement and partic-
Special Considerations for Preschoolers (Three to Five ipation in community or school settings.
Years) Special Considerations for Infants and Preschoolers
Under IDEA, Part B physical therapy examinations (Birth to Five Years)
usually take place in the community setting, preschool, or Family interview includes gathering information
childcare setting. Sometimes examinations take place in about an infant or young childs birth history including
the home if home-based services are warranted.22 prenatal and perinatal problems such as prematurity, low
Special Considerations for Children and Youth (Six to birth weight, periventricular leukomalacia, and intraven-
21 Years) tricular hemorrhage. Infants and children may not be for-
Under IDEA, Part B physical therapy examinations mally diagnosed with spastic diplegia until one to two years
usually take place in the school setting, which may include of age. Therefore, it is important to document risk factors
the classroom, school hallway, gymnasium, therapy room, commonly associated with spastic diplegia to help with
school cafeteria, or outdoors on school grounds.22 differential diagnosis.23 According to IDEA Part C, families
When? are asked to participate in a voluntary family assessment
General Considerations for All Ages often conducted by interview.
Examinations are conducted at convenient times for Special Considerations for Children and Youth (Six to
infants, children, and youth; their families; and school and 21 Years)
health personnel. An examination is performed initially Youth, family, and teacher interviews focus on func-
when the infant, child or youth is referred for services. In tional skills needed for school, home and community par-
the hospital setting, the schedule of reexaminations is de- ticipation and transition to adulthood. Interviews may be
pendent on the childs condition and medical status. In guided by specific concerns of the adolescent/young adult.
outpatient clinics, reexaminations often occur in accor- Systems Review. The purpose of the systems review
dance with hospital, clinic, and insurance policies. for PTCMR-SD is to identify the childs functional mobility
Special Considerations for Infants and Toddlers (Birth strengths and needs. Multiple systems are screened to de-
to Three Years) termine areas that require further testing. The systems
In early intervention settings, according to federal identified in the Guide (Musculoskeletal, Neuromuscular,
Pediatric Physical Therapy Clinical Management of Children with Spastic Diplegia 53
Cardiovascular/Pulmonary, Integumentary) are described mobility skills such as floor mobility, wheelchair mobility,
in the systems review and tests and measures section of the and/or ambulation.
PTCMR-SD. Other components such as Physical Environ- General Considerations for All Ages
ment, Medical systems, Developmental systems, and Fam- Choose appropriate tests to identify and measure
ily/Cultural Environment are important for children with specific functional mobility needs including observation
spastic diplegia and also are included in this PTCMR-SD. and standardized norm-referenced, and criterion-refer-
Tests and Measures. In this PTCMR-SD, tests and enced tests.
measures are organized according to the three dimensions Identify how assistive/adaptive devices and orthoses
on the personal level of the ICF: Participation, Activities, influence mobility task performance.
and Body Structure and Function.9 The Table of Tests and Consider clinical gait analysis, observing temporal-
Measures (see Appendix A) is organized in a top-down or spatial parameters.
functional outcomes approach beginning with tests and Body Structure and Function. This dimension of the
measures in the Participation dimension and ending with ICF refers to physiological functions of the body and ana-
tests and measures specific to the Body Structure and Func- tomical structures. In this PTCMR-SD, impairments reflect
tion dimension. Some tests and measures cover more than abnormalities of these physiological functions. General in-
one dimension of the ICF. Tests can be done solely by the formation on tests and measures is presented below. Spe-
physical therapist or in a team format where one profes- cific tests are presented according to age levels and the ICF
sional may have the prime responsibility for guiding the dimension in the Table of Tests and Measures in Appendix
child during the examination (i.e. arena examinations in A. (Table 3).
Early Intervention). The age range of each instrument is Musculoskeletal System
presented in the Table of Tests and Measures. Many re- 1. Range of Motion (ROM):
sources are identified in the Table of Tests and Measures General Considerations for All Ages
(Appendix A) but be aware that other resources are avail- Observe active ROM and measure passive ROM us-
able to the practitioner.22 ing goniometry or clinical observation.28 31
Consider specific testing for the following joint mo-
Findings from Tests and Measures of Medical Systems
tions and muscles32,33 hip abduction with knees flexed
will influence physical therapy patient management and
(flexibility of adductors-magnus, brevis, longus) and with
the plan of care. Physical therapy intervention strategies
knees extended (gracilis flexibility), hip extension
are designed to meet the childs individual functional and
(Thomas test position in supine) with knee extended (flex-
participation needs but must be modified if necessitated by
ibility of iliopsoas) and flexed (rectus femoris),34 knee ex-
the childs medical status. In the PTCMR-SD, functional
tension with hip flexion (popliteal angle- hamstring), an-
mobility is identified as the primary outcome and although
kle dorsiflexion with knees flexed (soleus) and extended
independent functional mobility may be a goal for all chil-
(gastrocnemius).
dren with spastic diplegia, the goal must be modified to
2. Strength Testing:
meet the childs medical and safety needs. General Considerations for All Ages
Participation. This dimension of the ICF refers to in- Observe child during age appropriate functional
volvement in life situations or ability to engage in commu- movements with gravity eliminated and against gravity
nity activities. (e.g. rolling, kicking, reaching, crawling, high kneeling,
General Considerations for All Ages squatting, walking, and climbing).35
Observe daily mobility routines. Specific Considerations for Preschoolers (Three to Five
Coordinate with other providers who work with the Years)
caregiver and child in school, community, and health care Consider manual muscle testing (MMT) and/or use of
system to identify mobility problems related to participa- hand-held dynamometry for children four to five years of age
tion in the specified setting.24,25 who can follow directions and attend to testing. Otherwise,
Identify barriers to community integration/partici- assess muscle strength in a functional context.36
pation. Conduct full lower extremity (LE) strength testing
Special Considerations for Infants and Children (Birth and screen upper extremities (UEs). Conduct full UE
to 12 Years) strength testing if screening results are not within normal
Observe play and caregiver-child interactions in a limits (WNL).
variety of environments. Conduct trunk strength testing to determine childs
Observe teacher-child interactions and peer interac- ability to flex and extend against gravity and isolate upper
tions. and lower trunk rotation and flexion and extension.
Special Considerations for Youth (13 to 21 Years) Specific Considerations for Children and Youth (Six to
Identify the youths mobility needs for transition to 21 Years)
adult services (e.g. educational, medical, and vocational Conduct LE strength testing, using MMT, hand-
services).26,27 held dynamometry37,38 and/or observation in functional
Activity. This dimension of the ICF refers to task per- context. Screen UE strength and conduct full UE strength
formance. In this PTCMR-SD, activity refers to functional testing if screening results are not WNL.
54 ONeil et al Pediatric Physical Therapy
3. Alignment and Posture: Document location of any skin irritations including
Specific Considerations for Infants and Preschoolers blisters or persistent redness and relationship to orthoses
(Birth Five Years) or adaptive equipment.
Observe for postural symmetry, test for hip joint Document skin characteristics such as abnormal
integrity, LE alignment, leg length discrepancy (LLD).32,39 temperature, color, and LE nail growth.
Specific Considerations for Children and Youth (Six to Medical Status; Physical Environment; Communi-
21 Years) cation/Behavior; Family/Culture Systems
Conduct scoliosis and LE alignment screening and General Considerations for All Ages
test for LLD. No specific physical therapy tests are currently
4. Growth: available.
General Considerations for All Ages Infants and young Obtain pertinent past medical history from care-
children with CP are at risk for poor nutrition.40
giver and child as appropriate; other team members/health
Review or document anthropometric (growth) mea-
providers; via medical, education or clinic chart review.51,52
sures during episodes of care. Measures may include head
Specific Considerations for Children and Youth (Birth
circumference, height, weight and calculation of Body
to 21 Years)
Mass Index.41
Obtain information on childs medications and im-
Neuromuscular System
General Considerations for All Ages plications for physical therapy.
Balance: Clinical observation of static and dynamic Document frequency and duration of seizure-like
balance, reactive and anticipatory postural control,42 dur- activity.
ing functional activities such as reaching and playing in Observe visual and auditory responses during func-
sitting, moving from floor to stand, reaching in standing, tional activities.
and walking. Document child/youths ability to follow simple and
Sensory Function: Clinical observation of childs complex commands.
responses and reactions to tactile, auditory, visual, and ves- Document communication methods used by child/
tibular stimuli.43 youth/family.
Motor Function: Clinical observation and/or Document child/youths ability to participate in age
video analysis of movement patterns during functional appropriate play.
tasks. Document safety, fitting, and functional use of adap-
Muscle Tone: Clinical observation to determine if tive/assistive equipment.
child has hypertonicity, hypotonicity, or dystonia includ- Perform home, school, and community visits as
ing fluctuating muscle tone. For more formal testing, con- needed to observe child in natural environments.
sider using the Modified Ashworth Scale.44,45 If more rigor- Discuss physical environment strengths/concerns/
ous measures are needed, consider Holts dynamic leg modifications with other team members/health providers
swing test46 or consultation with a research facility to per- once family permission is obtained.
form more sophisticated electronic testing. Screen child for possible nutritional concerns that
Specific Considerations for Infants and Toddlers (Birth may effect growth and health such as dysfunctional oral-
to Three Years): motor control associated with hypotonia, weak suck, de-
Clinical observation of primitive reflexes including layed/absent tongue lateralization; tongue thrust; weak lip
the Babinski reflex and clonus, muscle tone, and balance
closure; abnormal neurology maturation evidenced by un-
can be examined following protocols in the Movement As-
coordinated swallowing mechanism, tonic bite, hyperac-
sessment of Infants.
tive gag reflex; or poor seating posture during feeding/
Cardiopulmonary System47,48
meals due to an unstable trunk.53
General Considerations for All Ages
Endurance: Clinical observation of fatigue during
play, use of timed walking tasks,49 and use of activity mon- EVALUATION AND PHYSICAL THERAPY
itoring systems50 if available. DIAGNOSIS
Pulmonary function: respiratory rate; clinical obser-
vation of respiratory pattern, use of diaphragm, use of ac- The child and familys desires and articulated needs as
cessory muscles, color changes including cyanosis (lips, well as the results of the examination are considered to
skin, fingers). formulate the evaluation report. The physical therapy eval-
Cardiac Function: pulse/heart rate; blood pressure, uation reflects the examiners hypotheses for the basis of
color changes including cyanosis. the child and familys needs related to the childs current
Integumentary System movement problems. The physical therapy diagnosis is the
General Considerations for All Ages primary movement problem that has brought the child/
Document child or youths schedule for wearing family to seek physical therapy services and is the focus of
orthoses or positioning devices such as ankle-foot ortho- the planned episode of care. In the PTCMR-SD), the phys-
ses, dynamic splints or bivalved casts. ical therapy diagnosis is difficulty with functional mobility.
Pediatric Physical Therapy Clinical Management of Children with Spastic Diplegia 55
PROGNOSIS AND PLAN OF CARE (INCLUDING Children (three to 12 years): Physical therapy is a
FREQUENCY AND DURATION OF SERVICES) related service and is provided in the educational setting to
Developing a plan of care is a complex problem solv- allow children to access and participate in their educa-
ing activity, which requires integration of examination and tional program. Frequency and duration of PT is based on
evaluation findings and child and family goals. The physi- identified needs in the Individualized Education Program
cal therapist should incorporate components of the ICF (IEP) and may occur in periodic episodes of care. Fre-
enablement model when developing a plan of care. Primary quency and duration of PT are determined by the team. The
child may receive either direct or indirect (consultative)
outcomes should include functional activities and partici-
physical therapy services.
pation in lifes roles.
Youth (13 to 21 years): Frequency and duration of PT
Limited research findings are available to determine
is based on identified needs in the IEP and may occur in
the optimal amount of intervention required for the best/
periodic episodes of care. Physical therapy may be needed
most effective functional outcomes for infants, children
at a higher frequency when the transition plan is developed
and adolescents with cerebral palsy.54,55 Bower and col-
for the youth beginning at age 14 to16 years.
leagues56 58 have shown that short term (two to three
Expected Outcomes. Functional outcomes for chil-
weeks) intensive intervention does create short-term ben-
dren will vary greatly depending on the severity of spastic
efits in motor function, however the differences across a six
diplegia. Severity may be influenced by the childs muscle
month period between a higher (five times/week, 60
strength, sensory systems compromise, spasticity, cogni-
minute sessions) and a lower intensity of therapy were not
tive abilities, and medical status. Several researchers have
significantly different. Recently, Trahan and Malouin59 re-
studied the prediction of functional outcomes for children
ported on the use of intermittent intensive intervention:
with cerebral palsy. All of the studies included some chil-
four times per week for four weeks, followed by eight
dren with spastic diplegia. Montgomery65 reviewed several
weeks of no therapy. That frequency of therapy was shown of these studies66 71 and reported that persistence of prim-
to be feasible and led to improvements in motor function in itive reflexes, ability to maintain sitting, type of cerebral
children with cerebral palsy in Gross Motor Function Clas- palsy, age/maturation and level of cognition influenced
sification Systems Levels IV and V.59 Although results from ambulation potential. Based on outcomes from three stud-
their study cannot be generalized to children with spastic ies,67,70,72 Montgomery65 reported that 86-90% children
diplegia, they do provide some support for a variety of with spastic diplegia achieved some form of ambulation.
service delivery models. More research is needed in the More recently, Wu and colleagues73 have retrospectively
area of intensity of services. The frequency and duration of studied 5366 subjects with CP, 12.8% who could walk
physical therapy services noted below are based on current independently, and 18.4% who could walk with support.
common practice in the USA. Independent predictors of walking were early motor mile-
General Considerations for All Ages stones such as obtaining the ability to sit and pull to stand.
Outpatient setting: Frequency and duration of PT Motor Development Curves have been developed to pro-
should be individualized and based on child and family vide prognostic information about functional ability in
needs. When determining the frequency and duration of children with cerebral palsy.74 Although these curves are
PT, the goal of functional mobility and ways to enhance not specific for children with spastic diplegia, they still
participation and functional mobility should be consid- provide useful information. Longitudinal observations of
ered. Periodic and episodic care is used in the management motor ability included the ability to hold the head upright,
of children with spastic diplegia with follow-up appoint- maintain unsupported sitting, walk 10 steps unsupported
ments scheduled accordingly. Intensity of services may be and walk down four steps. The Gross Motor Functional
higher for children with increased impairment or those Classification System (GMFCS)75 was used to create the
who undergo selective dorsal rhizotomy (SDR)60,61 com- motor development curves. The GMFCS has five levels.
pared to children with milder impairments. Most children with spastic diplegia would be classified as
Inpatient setting: Frequency and duration of PT is Level I, II or III. Children classified in Level I walk without
based on the childs condition and need. Daily PT may be restrictions and have limitations in advanced gross motor
indicated for children in orthopedic post-operative care. skills. Level II is defined as walking without assistive de-
Specific Considerations for Infants and Toddlers (Birth vices and having limitations walking outdoors and in the
to Three Years) community. Level III is defined as walking with assistive
Early intervention setting: The team establishes the mobility devices and having limitations walking outdoors
plan of care. Frequency and duration of PT is based on and in the community. Children classified in Level IV have
identified needs in the Individualized Family Service Plan self-mobility limitations and are transported or use power
(IFSP) and may be provided as direct or indirect ser- mobility in the community. Level V includes children who
vice.62,63 Frequency is determined by the team and some are dependent for mobility. The GMFCS has also been
states may have specific recommendations. shown to correlate well with the Gross Motor Function
Specific Considerations for Children and Youth (Three Measure (GMFM), the Pediatric Orthopedic Data Collec-
to 21 Years) tion Instrument, temporal-spatial gait parameters, and ox-
School setting:64 ygen cost assessments.76
56 ONeil et al Pediatric Physical Therapy
General Considerations for All Ages Independent ability to negotiate through inside
As part of an IFSP or IEP, expected outcomes are doors and heavier doors leading to outside
developed by the team, which includes the child/youth, Independent ability to use appropriate/desired play-
family, physical therapist, teachers, and other early inter- ground equipment
vention or school personnel. Teacher/aides able to carry out/facilitate mobility
In hospital settings, goals or expected outcomes are and functional skills78
developed by the child/youth, family, and therapist and Family able to carry out/facilitate mobility and func-
other health professionals and focus on functional mobility tional skills
in the child/youths home or community setting. Increased/maintained flexibility, strength and en-
Specific Considerations for Infants and Toddlers (Birth durance for functional activities
to Three Years) Prevention of future deformity/pain
Outcomes should be measurable with a specific Development of initial skills in self advocacy and
timeframe (time limited).8 Outcome categories may in- self-determination.27,79
clude: Specific Considerations for Youth (13 to 21 Years)
Sitting function and mobility on the floor for play Outcomes may include:
Standing function and mobility for play Independent mobility around home, school, includ-
Ambulation indoors/outdoors with or without assis- ing stairs, bathroom, cafeteria, locker room, school and
tive device community buses, etc., with or without a device or using
Ambulation up and down stairs with assistance wheeled mobility
Appropriate positioning in stroller/high chair/bath Independent ability to negotiate in community for
chair/ride-on toy regular activity and job training
Family/caregiver independent in positioning Independent timely mobility between classes at
Family satisfaction with services school
Prevention of secondary impairments by increasing Independent participation in fitness and recre-
and/or maintaining flexibility, strength and endurance for ational movement program
functional activities. Self advocacy and self-determination27,79,80
Specific Considerations for Preschoolers (Three to Five Ability to maintain/increase flexibility, strength and
Years) endurance for functional activities
Outcomes may include: Ability to lead transition planning to adult services.
Independent household mobility (floor or wheel-
chair mobility) INTERVENTION
Independent household ambulation with or without A. Coordination, Communication, and Documenta-
devices, including stairs tion. These are processes intended to ensure high quality of
Independent age appropriate transitions/transfers care. They include working and communicating with all
for functional mobility parties involved with the child and family and document-
Assisted or independent community mobility ing services and care provided.8
Family able to carryout/facilitate mobility and func- General Considerations for All Ages
tional skills77 Maintain coordination of services and communica-
Prevention of secondary impairments by increasing tion with all team members or health providers that partic-
and/or maintaining flexibility, strength and endurance for ipate in the infant/child/youths care. Consider co-visits
functional activities. when appropriate. Document all levels of intervention that
Specific Considerations for Children (Six to 12 Years) the infant/child/youth and family engage in during therapy
Outcomes may include: sessions and for overall plan of care.63
Independent classroom or household ambulation Use documentation guidelines set by the work set-
with or without assistive devices ting and third party payers.
Independent community ambulation with or with- Communicate in writing to family and other provid-
out assistive devices for children classified as Levels I and II ers as appropriate. For physical therapists working in the
on the GMFCS. Some children classified as Level III on the school system, written permission from the childs parents/
GMFCS may require wheeled mobility for community dis- legal guardian is necessary prior to communicating with
tances healthcare providers outside of the school system.22 For
Independent ability to get on and off the bus or use therapists working in health or medical settings, be sure to
public transportation follow worksite guidelines on sharing patient information
Independent in toileting tasks (tub and toilet trans- under HIPAA (the Health Information Portability and Ac-
fers and clothes management) countability Act).
Independent age appropriate transitions/transfers Other providers that physical therapists communi-
for functional mobility cate with may include durable medical equipment vendors
Independent mobility on stairs with or without a and orthotists regarding assistive technology and orthoses.
railing Consider referral to other resources (such as family
Pediatric Physical Therapy Clinical Management of Children with Spastic Diplegia 57
support groups, public programs, advocacy groups) and healthcare providers is especially important as the child
community activities (such as centers for independent liv- transitions from an early intervention program to a pre-
ing and recreation centers) to support the familys and in- school program.
fants, childs, or youths identified outcomes. Therapists document examination findings as part
Assist with transition for discharge or to the next of the IFSP (birth to three years) and IEP (three to five
appropriate service system (i.e. from EI to school, from years). Therapists also routinely document a childs func-
school to adult services).80 tional status and progress on outcomes and objectives.
Engage child/youth in health care decisions to help For children receiving physical therapy in health
the child/youth develop self-advocacy and independent care settings, the therapist documents examination find-
living skills. ings, plan of care, intervention provided and functional
Communicate with families about spasticity man- status based on policies of the setting and third party pay-
agement options, which may improve childs function and ers.
participation. Spasticity management options include re- Specific Considerations for Children (Six to 21 Years)
ferral to a medical or rehabilitation team for evaluation and Ongoing communication with the child and the
recommendations for medical intervention (oral medica- childs team in a family-focused, culturally acceptable man-
tions, botulinum toxin injections and phenol blocks) or ner is important.90 Some youth may receive services at two
surgical interventions (orthopedic including muscle and different settings such as at school and an outpatient clinic/
bony procedures and neurosurgery including selective hospital setting and communication is coordinated across
dorsal rhizotomy and baclofen pump); coordination of settings.
therapy interventions after medical management for spas- Ongoing communication with the child or youths
ticity; and documentation of anticipated outcomes and team is important. The team may include but not be limited
childs progress/functional status in therapy.81 to parents, caregivers, MDs, orthotist, durable medical
Communicate with families about common ortho- equipment vendor, and school personnel (special educa-
pedic procedures such as femoral osteotomies and muscle tion teacher, regular education teacher, physical education
lengthening and participate in team decision making about teacher, counselor, psychologist, occupational therapist,
the procedures and the impact of functional mobili- speech therapist, etc).
ty.32,82 88 For youth 13 to 21 years: Communicate with job or
Observe and record/report seizure activity during high school/college guidance counselor, community work
PT sessions as per childs plan of care. place supervisor, and other community program advisors
Consider referral to improve oral-motor abilities as the youth moves towards school graduation.
when you determine/identify intervention strategies and Communication topics may include child or
outcomes.40 youths motor disability, safety and awareness during
Consider referral for nutritional evaluation if the mobility, behavioral control, medically related issues
child is overweight or underweight or at risk for over- such as seizure disorder, cardio-pulmonary disorders
weight or underweight. such as asthma, etc., medical management of muscle
Specific Considerations for Infants and Preschoolers tone (botulinum toxin, baclofen, SDR), ankle and foot
(Birth to Five Years) orthoses, adaptive equipment (crutches, walkers, wheel-
For physical therapists practicing under the Individ- chairs), musculoskeletal integrity, school physical edu-
uals with Disabilities Education Act [IDEA] (PL 105-17), it cation program, and opportunities for recreation such as
is strongly recommended that they communicate with swimming, therapeutic horseback riding, and other
state lead agencies and state and county Interagency Coor- sports or fitness programs.
dination Councils (ICCs) to become familiar with policies, For youth 13 to 21 years: Communication topics may
procedures, and resources that affect service delivery for include issues about specific motor skills required for var-
children and their families in their region of practice. ious jobs or negotiating college campuses.
This level of intervention involves direct collabora- Therapists participate in developing an IEP with the
tion with key individuals in the infant/childs life. These student, the parents and other school team members. Phys-
individuals include the infants/childs service coordinator ical therapists document a child or youths functional sta-
from the EI agency and other EI team members (family tus and yearly goals on the IEP. In addition, physical ther-
members, medical providers, and early childhood educa- apists provide yearly evaluations, three-year evaluations
tors).89 Also it is advisable to communicate with key indi- and quarterly reports on the status of goals.
viduals who may not be able to be present during interven- For youth 13 to 21 years: During the transition from
tion visits (i.e. parents if the child is served at a daycare or school to college or other community placements, physical
preschool; father if the mother is typically present when therapists participate in the meetings and documentation
the child is served in the home). required for transition planning.
For physical therapists serving children in health In healthcare settings, therapists document exami-
care settings, ongoing communication with the childs nation findings, plan of care, intervention provided and
health and early intervention providers is critical. functional status based on policies of the setting and third
Communication with family, teachers, and other party payers.
58 ONeil et al Pediatric Physical Therapy
B. Patient-related Instruction. This involves inform- gins with the child, so that he or she can gradually learn
ing, educating and training children, youth, families and about self and disability and choices to be made based on
caregivers for the purpose of promoting optimal care.8 In- his or her culture and values.27
struction may include providing information about the di- For youth 13 to 21 years: As part of self-awareness
agnosis of spastic diplegia, plan of care, transition from one and self-determination training, communication is focused
service delivery system to another, need for a health and on the youth, so that he/she can learn as much as possible
fitness program, and strategies to practice functional mo- about self and disability and choices to be made based on
bility during daily routines. his/her culture and values. If the youth is capable, he/she
General Considerations for All Ages will learn to communicate with his/her team members ef-
Discuss and identify areas in which the caregiver ficiently about the need for assistance, safety needs, pain
and child need support to participate in the physical ther- concerns, fitness, medical needs, interests, beliefs, and val-
apy plan of care ues. The youth will learn how to access community re-
Provide culturally appropriate instruction to the sources. Or if the youth is not capable of independently
caregiver and child in the manner that is best for them accessing the community, then the family or caregivers
(demonstration, written, verbal, video) to ensure that prac- learn to assist the youth in community participation.27
tice of functional activities occurs so the child can improve Family and caregiver instruction may include posi-
functional mobility and increase participation in home, tioning and handling techniques, stretching exercises, fa-
school, and community.91 Written and video instruction cilitating recreational activities, adapting task and environ-
may improve home and school program adherence. Ther- ment for optimal participation, assisting with exercise and
apists should also consider the stresses of caregivers when fitness needs, and providing information on community
developing a home program and requesting caregivers to resources.
carryout additional home activities.92,93 C. Procedural Intervention. This involves the use of
Specific Considerations for Infants and Preschoolers physical therapy procedures and techniques to produce an
(Birth to Five Years) improvement in the life and function of a child or youth
The majority of patient-related instruction is in the
with spastic diplegia. Procedural interventions address a
form of reciprocal information exchange between therapist
childs limitations in body and/or environmental systems
and family including parents, siblings, extended family,
and are focused on improving functional mobility out-
and childcare workers.
comes.8
Patient-related instruction may include but not be
Overall Purposes
limited to carrying, positioning and handling techniques,
Implement strategies to improve functional mobility
care-giving strategies for feeding, bathing, dressing;
and increase participation at home, in school and commu-
stretching exercises, parent child interactions and play
nity and in play situations
activities, task and environment adaptations.94 96
Adapt the tasks or movement experiences to meet
Physical therapists provide recommendations for
home program activities that are meaningful and under- the strengths and challenges of the individual child
standable to the family and can become a part of the childs Involve family and school staff to help reinforce and
typical day.97 Verbal, written and/or video instruction may generalize mobility skills
be provided.98,99 Address systems that may limit functional mobility
Specific Considerations for Children (Six to 21 Years) goals.
Patient-related instruction is provided to the care- 1. Musculoskeletal and Neuromuscular Systems - In-
givers including the child, parents, extended family, and cluding Strength, ROM, Alignment and Posture, Balance,
school and childcare workers. As children become older, Motor Function, Tone and Movement Patterns
primary patient-related instruction is directed to them and General Considerations for All Ages
designed to meet their needs. Musculoskeletal and neuromuscular systems are
For youth (13 to 21 years): Patient-related instruc- presented together because components of each system are
tion is provided primarily to the youth. interdependent.
Patient-related instruction may include but not be Intervention strategies are designed to improve the
limited to identifying health and fitness needs; teaching following areas:
self-ROM exercises; self-relaxation techniques (breathing, Neuromuscular system: balance, coordination, mo-
Feldenkrais, yoga, etc.); posture and body mechanics, tor learning, motor function, movement patterns, sensory
managing orthoses and adaptive equipment; and safety motor integration
awareness (e.g. safety issues for ambulation in crowded Musculoskeletal system: strength, ROM, alignment/
hallways, in public areas/stores, unusual environments, es- posture
calators, and understanding the need for assistance and When implementing any of the following activity-
how to ask for it). focused intervention strategies consider motor learning
Self-awareness and self-determination training: principles. Motor learning is a set of processes which lead
For children six to 12 years: As part of self-awareness to permanent changes in functional motor abilities. Exam-
and self-determination training, communication often be- ples of motor learning strategies include varied practice
Pediatric Physical Therapy Clinical Management of Children with Spastic Diplegia 59
schedules, use of augmented information including in- alone.127 Consider short leg bivalved casts or dynamic
struction, demonstration, verbal cues, manual guidance, splints for nighttime positioning to increase or maintain
visual, auditory and tactile feedback, and use of cognitive flexibility in gastrocnemius or soleus muscles. Children
strategies.99 103 with CP who use an equinus gait pattern may demonstrate
Intervention strategies are implemented in the con- shortening of these muscles, even if there is no contracture
text of functional activities to encourage independent mo- at the ankle.128
bility.104 Play is an important component of intervention Balance/Postural Control and Coordination Activi-
for children. ties
Specific Considerations for Infants and Preschoolers Exercise to increase balance and coordination for
(Birth to Five Years) function, such as hippotherapy,122124 neurodevelop-
Infants and toddlers (birth to three years): The follow- mental therapy techniques,129,130 self-generated and
ing procedural interventions are most often provided in the therapist generated perturbations in sit and stand and
home or childcare setting which is the natural environ- use of orthoses.131133,42
ment. Functional Activities
Preschoolers (three to five years): The following pro- Activities include floor mobility, sitting posture and
cedural interventions are most often provided in the pre- stability, transitions in/out of sitting, transitions to/from sit
school setting. to stand and ambulation. Practice mobility on rough un-
Specific Considerations for Children (Six to 12 Years) even ground through contrived or natural obstacle
The following procedural interventions may take courses, on stairs or ramps, and through doors. Provide
place in the school, home, or health care setting. instruction demonstration, guidance and feedback as indi-
Interventions cated.
Strengthening: Motor training and manual guidance for develop-
Infants and preschoolers (birth to five years): Strate- ment of functional movement patterns134,135
gies are introduced during play. Consider using therapy Treadmill walking136,137
balls, aquatic therapy and hippotherapy.105106 Computer assisted instruction to improve lower ex-
Children and youth (six to 21 years): Strengthening tremity function especially ankle function138
during play and/or direct resistive exercises. Consider us- Neuromuscular electrical stimulation during func-
ing theraband, cuff weights, free weights, weight machines, tional activity139 142
and other exercise equipment. Researchers have examined Ankle-foot orthoses to improve gait and functional
the intensity of strength training for children with spastic movements143145
diplegia. To demonstrate an increase in strength, recom- Referral for botulinum toxin injections to be accompa-
mendations include two to three times per week for six to nied by exercise to improve gait in children with CP146 148
10 weeks at 65% of maximum isometric strength or be- Consider bicycle riding, walking, swimming and
tween three to 10 repetitions maximum.107109 Continua- aquatic gait exercise, hippotherapy or recreational horse-
tion of strength training over 10 weeks is also recom- back riding.
mended for increasing or maintaining strength. Evidence Use of EMG feedback during gait, auditory feedback
supports that strengthening does not increase spastici- of gait parameters, and/or electrical stimulation during gait
ty.107,110 113 Evidence also supports that strength ability is could be beneficial for learning more efficient and flexible
correlated to ability to balance in children with CP.114 Pre- alignment and coordination patterns.99,118-120,149
liminary evidence suggests that strength training improves Teach the child strategies to deal with abnormal
gait in individuals with cerebral palsy.108,110,115,116 120 muscle tone during functional mobility.150
Other effective strengthening strategies include Specific Considerations for Children and Youth (6-21
electrical stimulation,109 111 bike riding,121 aquatics,106 and Years): Encourage youth to develop a movement practice
hippotherapy.122124 Hippotherapy has also recently been schedule involving movement through difficult terrains,
shown to improve muscle symmetry.125 on bleachers, escalators, bus steps, in moving vehicles such
Stretching Exercises as public transportation, stores and other community en-
Infants and preschoolers (birth to five years): Position- vironments.
ing and stretching to improve alignment, ROM, and func- Consider martial arts, adapted sports programs, bi-
tion (e.g. long sitting with protection of lumbar spine to cycle riding, track exercise, swimming and aquatic gait
stretch hamstrings and abducted sitting to stretch hip ad- exercise, hippotherapy or recreational horseback riding.
ductors) Improvements in hamstring length have been as- Provide consultation for the youth who desire to
sociated with improvement of temporal patterns during learn a new sport or motor activity.151,152
gait of both the semitendinosus and vastus lateralis mus- 2. Cardiopulmonary SystemIncluding Endurance,
cles.126 Pulmonary and Cardiac Function. Children with cerebral
Children and youth (six to 21 years): Begin teaching palsy may have compromised cardiopulmonary systems. In-
self ROM exercises. Consider serial casting in conjunction tervention strategies should include techniques to improve
with botulinum toxin A injections for gastrocnemius and cardio respiratory endurance. For typically developing chil-
soleus muscle tightness that does not respond to injections dren, 30 to 60 minutes of moderate to vigorous intensity
60 ONeil et al Pediatric Physical Therapy
physical activity, three to six times per week is recommended programs to focus on self-care and self-determination skill
for overall health benefits.61,153,154 Children with cerebral building.
palsy (CP) are considerably less active than their peers with- Teach youth to understand and control their health
out disability and do not exercise at high enough intensity to and fitness and maintain or improve compromised sys-
increase fitness.155157 Inactivity may be due to difficulty ac- tems.
cessing appropriate programs or availability of programs or Youth and family support and information exchange
accessible equipment. Several randomized control trials are are important to identify useful resources when developing
currently underway to assist in better determining outcomes recreational activities. School participation and activities
from fitness training for children with cerebral palsy (per- should be encouraged to enhance functional mobility, ex-
sonal communication: Fowler, EG, 2005). ercise for health and fitness, and develop interest in life
General Considerations for All Ages sport and other community activity.
Adapt interventions to account for the fact that chil- Due to lower activity levels, youth with compromise
dren with cerebral palsy usually have lower maximum ex- to these systems are at risk for being overweight and im-
ercise capacity, muscle power and endurance. They expe- pairments that lead to loss of functional mobility.
rience a higher metabolic cost during submaximal exercise Consult with a dietitian/MD/physical education
and fatigue faster than children who are typically develop- teacher and family to maintain youth/childs daily physical
ing.47,155,157159 activity levels.
Interventions that include endurance/aerobic train- Possible physical therapy activities include exercis-
ing for children with cerebral palsy may result in improved ing with a medicine ball and pulleys, walking on ground or
peak aerobic power.157 treadmill, bike riding, jump rope, trampoline, swimming,
During intervention sessions to improve cardiopul- other water games, and wheelchair propulsion.
monary function, monitor vital and clinical signs such as 3. Integumentary System
heart rate, rate of perceived exertion; dyspnea on exertion; General Considerations for All Ages
cyanosis; diaphoresis (as indications of systems under Consider movement strategies for activities, posi-
stress).47 tioning, and postures that will prevent skin breakdown,
Provide interventions to improve cardiopulmonary disturbed sensations, and relieve pain.8
endurance and tolerance for physical activity. Consider the Check skin during PT sessions for children who
childs age, developmental level, level of disability, cardio- have received new devices, have existing problems with
pulmonary compromise, and movement patterns when de- their orthoses or have had recent growth spurts.
signing an endurance program. Teach family/caregivers/child/youth how to don/doff
Provide instruction on endurance training i.e. orthoses and check skin.
proper use of cardio-training equipment such as tread- Adapt/adjust orthoses, casts, positioning devices or
mills, stationary bikes, recumbent bikes, elliptical trainers, contact orthotist or have family/youth contact orthotist.
and steppers, which equipment is best to prevent injury, Establish schedule for wearing orthoses considering
and how to adjust equipment for appropriate fit. Recom- childs/familys needs, setting etc. Assist family/caregivers
mend training intensity by using perceived exertion scales with establishing the schedule.
or training heart rate levels. Instruct the child in how to 4. Physical Environment - Including Home, School,
monitor his/her heart rate or perceived exertion.160 and Community Resources, Transportation Needs and
Provide instruction for energy conservation for task Equipment Needs
completion. General Considerations for All Ages
Older children should become involved in exercise Physical therapists prescribe and provide training in
decisions to include elements of self-care and self-determi- the use of adaptive equipment or orthotic devices to im-
nation in physical activities. prove child and environmental constraints to optimize
Special Considerations for Infants and Preschoolers functional mobility.36,133 Equipment needs are addressed in
(Birth 5 Years) light of all the identified physical, societal and emotional
Use a family-centered approach by including care- needs of the child, as well as the family home environment;
givers in activities and strategies to increase a childs phys- the childs school, transportation issues (public transit,
ical activity and to enhance cardiopulmonary capacity.90 school bus, car); and the necessity and importance of mov-
Play is an important intervention strategy to en- ing about and participating in community activities. Spe-
hance mobility and cardiopulmonary capacity. cific attention should be given to the need for different
It is hard to motivate younger children for long types of equipment for different mobility tasks that may be
periods of exercise, a goal of 10 to 15 minutes of intense influenced by the environmental demands.162
activity interspersed with recreational games for 30 to 45 Equipment considerations to improve alignment,
minutes for two sessions a week will result in a training ROM, and functional mobility include:32,36 lower extremity
effect in a few weeks.161 splinting, serial casting, orthotic devices163 and adaptive
Special Considerations for Children and Youth (Six to devices (such as seating systems, standing tables,164,165
21 Years) night splints for stretching,163 as well as walkers and
Involve children in choice and design of exercise crutches).
Pediatric Physical Therapy Clinical Management of Children with Spastic Diplegia 61
For children who need a walker, consider a poste- and for keeping up with peers (i.e. larger schools and need
rior rolling walker which may have the advantage of facil- to get to classes in a timely fashion; field trips with class).
itating upright positioning, increased gait velocity, and de- Child may undergo surgical interventions or may
creased double stance time as compared to anterior experience changes in ROM or muscle tone, which may
walkers.166,167 require new devices.
Teach youth self-management of these adaptive de- Child may worry about his/her appearance, or may
vices. Consider an episode of care for changes related to be exposed to more difficult environments in which to
growth spurt, pain syndrome, or for consultation about negotiate safely (ex. having to cross streets, participating in
orthoses.36 more complex sports activities/environments, etc.).
Consider a home visit or community visit (i.e. day Provide home or school modifications and equip-
care center) to assess childs physical environment and ment to meet the needs of the child (for example, a pow-
need for modifications, adaptations, accommodations, or ered chair). Modification and equipment information are
assistive devices.22 discussed with the child, family, and school personnel.
Consider the family transportation needs and assist Specialized vendors can help with equipment needs.
in obtaining the means to get the child/youth to participate D. Additional Considerations When Implementing
in community activities. Procedural Interventions
Determine equipment needs for the child in the 1. Medical SystemsSuch As Nutrition And Feed-
home and community with a goal to maximize functional ing; Seizure Activity; Vision And Hearing; Bowel And
independence or ease of caregiving for the parent. Possible Bladder Function
equipment for the home, school and community may in- Nutrition and Feeding
clude, bathroom equipment (shower chair, raised toilet General Considerations for All Ages
seat, grab bars), car seat, car/van adaptations, manual Children with CP are more likely than their peers to
wheelchair, power wheelchair or scooter. The child/youth have malnutrition, obesity, and adverse drug-nutrient in-
may require different equipment for mobility needs, such teractions168 171
Children with CP who are underweight may have
as a walker for short distances and a wheelchair for longer
low percent body fat and fat free mass,156 increased caloric
distances.
requirements,172 feeding problems,173,174 excessive energy
Teach the child/youth and family safe and efficient
consumption,175177 and fatigue.178 180
use of the adaptive equipment for negotiating different en-
Poor nourishment in children with CP is associated
vironments.
with increased hospitalization, decreased participation in
Assist the family and the child/youth in obtaining
typical activities, missed days at school.181
resources for environmental modifications as needed.
Bone Density
Specific Considerations for Infants and Preschoolers
General Consideration for All Ages
(Birth to Five Years)
Non-nutritional factors, such as reduced ambula-
An infant or child may require adaptive equipment tion, can contribute to decreased bone density.182 Reduced
or assistive devices to achieve functional mobility (i.e. pos- bone mineral density has been reported in the lumbar ver-
terior walker, ankle foot orthoses (AFOs).166,167 tebra and femoral neck183,184 of children with cerebral
Equipment needs are addressed based on childs palsy. Bone mineral density is correlated with ambulation
function and environmental needs. Examples: Does the status and age at which a child began to walk. Children
child need mobility (i.e. wheelchair, stroller, walker, push with better ambulatory status are more likely to have better
toy) or positioning (i.e. seating, stander) devices? Does the bone mineral density levels.184
family home have stairs? Does the family have a car or use Children with spastic diplegia and hemiplegia have
public transportation? similar levels of bone mineral density; both values are
Specific Considerations for Children or Youth (Six to lower than those for children who are typically developing
21 Years) but higher than for children with quadriplegia.184
As children age, they may need additional assistive Children with spastic cerebral palsy have shown
devices or modifications to current devices. Growth and increased bone mineral density after an eight-month phys-
environmental changes due to age and home, school, or ical activity program.183
community activities may warrant new or modified de- Bone mineral density also may be compromised by
vices. It is important that the child, family, school and nutritional problems and anti-convulsive medication.184
therapist monitor a childs need for and use of equipment. Seizure Activity
As the child ages, it is important that he/she understands General Considerations for All Ages
how to maintain and use assistive devices/adaptive equip- Research findings indicate that 43% of children with
ment appropriately and independently and how to make neonatal seizures and abnormal neurologic examinations
proper choices for equipment/device needs. were ultimately diagnosed with CP.185
Examples of times when child may need new or Be aware of a childs seizure history and activity and
modified assistive devices/adaptive equipment: seizure medications. Document any seizure activity during
Child may need mobility device for independence therapy sessions.
62 ONeil et al Pediatric Physical Therapy
Modify intervention strategies if a childs seizure Consider the family and physical environments that
activity is exacerbated by therapy. the child will experience as he/she ages with spastic diple-
Vision and Hearing gia.
General Considerations for All Ages Establish opportunities for peer interaction and
In a population-based study of children with CP, modeling in intervention sessions, especially for older chil-
both vision and hearing were significantly associated with dren.
GMFCS levels suggesting increased limitations in vision Focus on improving participation by decreasing
and hearing with increased severity of CP.186 functional limitations.
If a child has decreased vision, consider accommo- Take into account the child or youths age, learning
dations such as providing feedback with increased audi- style, maturity, and belief systems when planning interven-
tory, tactile, and light features. For younger children, use tions.
toys that provide these types of feedback. Acknowledge child and family values and culture
If a child has a hearing impairment, be aware of how when providing services.
to assist the child with using hearing aids or sign language. Regardless of intervention environment (home,
When providing instructions, use visual and manual guid- community, school, hospital) the intervention session
ance. For older children, use pictures or written instruc- needs to meet the learning style/abilities of the child and
tions for home programs if appropriate. family; provide meaningful activities to achieve child and
Bowel and Bladder Function family needs; and be integrated into the child and family
General Considerations for All Ages routines to be successful.
Constipation187 and neurogenic bladder (spastic 4. Transitions from Adolescence to Young Adult-
bladder) may be problematic for children with CP. Chil- hood. For young adults with special health care needs, a
dren who have mental retardation along with primary di- primary goal of transitions in health care is to maximize
agnosis of CP may not be able to be toilet trained and may function and lifelong potential by providing appropriate,
therefore, be dependent in toileting. uninterrupted health services.191 Physical therapists often
Encourage movement/exercise and upright posture provide health services to young adults with spastic diple-
which may improve digestive and elimination activity. gia in their transition from related services under IDEA to
2. Developmental SystemsSuch As Cognition, adult services. Physical therapists may take the role as a
Communication, Social/Emotional Issues, Affect, Behav- consultant and provide community-based interventions to fa-
ior and Temperament/Resiliency cilitate a students transition to successful participation in the
General Considerations For All Ages community as an adult. Essential elements of physical ther-
PT intervention is provided within the context of the apy services during this transition process include:192
childs identified developmental outcomes, respecting the An outcome oriented process to promote the move
childs development in all domains. from a school environment to post-school activities includ-
Consideration is given to the infants need to de- ing work-related activities;
velop competency in self-regulation. A focus on the individuals needs including prefer-
PT intervention is provided in a way to help the ences and interests;
child attend to task, to decrease distractibility while per- Provision of coordinated activities across team
forming and learning motor skills. members for successful therapy interventions;
Consider sensory integration and modulation when Promotion of the successful transition to the post-
observing or requesting a motor task from the child. secondary environment so that therapy interventions focus
PT intervention should be challenging and as age on students transition needs to typical community envi-
appropriate as possible given the childs abilities. Do not ronments.
overwhelm the child/youth but try to ensure success by
RE-EXAMINATION
achieving outcomes while challenging the child to learn
the functional skill. After an episode of care, a child and family should
Working toward automaticity of mobility functions undergo a reexamination to determine if outcomes/goals
is important for shared attention tasks in the functional have been achieved. If goals are achieved, then the child is
environment. discharged from service and may be referred to community
3. Family/Cultural EnvironmentIncluding Care- agency/resources for recreation or other physical activity
giver-Child Interaction, Supports And Resources, Learn- services. If goals are only partially achieved or not
ing Styles, Cultural Beliefs, Demographic Information, achieved, then the plan of care for the child and family is
And Family Constellation revised and services may be continued if appropriate.
General Considerations for All Ages References
Use a child/youth first approach in providing PT to
1. Sobo E, Kurtin P. Child Health Services Research: Applications, Inno-
a child and his/her family.79,188 190
vations and Insight. San Francisco: Jossey-Bass; 2003.
Foster parent-child interaction during intervention. 2. Executive Committee for the Definition of Cerebral Palsy. Proposed
Foster self-determination in children to encourage definition and classification of cerebral palsy, April 2005. Dev Med
independence in self-care. Child Neurol. 2005;47:571576.
Pediatric Physical Therapy Clinical Management of Children with Spastic Diplegia 63
3. Hayes M, McEwen I, Lovett D, et al. Next step: survey of pediatric es/physical disabilities. Seattle: Washington State Department of
physical therapists educational needs and perceptions of motor Health and the Division of Adolescent Medicine; 1995.
control, motor development and motor learning as they relate to 28. Allington N, Leroy N, Doneux C. Ankle joint range of motion mea-
services for children with developmental disabilities. Pediatr Phys surements in spastic cerebral palsy children: intraobserver and in-
Ther. 1999;11:164182. terobserver reliability and reproducibility of goniometry and visual
4. Ratliffe K. Clinical Pediatric Physical Therapy. Philadelphia: Mosby; estimation. J Pediatr Orthop. 2002;11:236239.
1998. 29. Gajdosik R, Bohannon R. Clinical measurement of range of motion:
5. Sweeney J, Heriza C, Markowitz R. The changing profile of pediatric Review of goniometry emphasizing reliability and validity. Phys
physical therapy: a 10-year analysis of clinical practice. Pediatr Phys Ther. 1987;67:18671872.
Ther. 1994;6:113118. 30. Norkin C, White D. Measurement of Joint Motion: A Guide to Goni-
6. Chiarello L, ONeil M, Dichter C, et al. Exploring physical therapy ometry. Philadelphia: FA Davis; 1985.
clinical decision making for children with spastic diplegia: Survey of 31. Stuberg W, Fuchs R, Miedaner J. Reliability of goniometric measure-
pediatric practice. Pediatr Phys Ther. 2005;17:4654. ments of children with cerebral palsy. Dev Med Child Neurol. 1988;
7. Tickle-Degnen L. Using research evidence in planning treatment for 30:657666.
the individual client. Can J Occup Ther. 1998;65:153159. 32. Bleck E. Orthopedic management in cerebral palsy. Philadelphia: JB
8. American Physical Therapy Association. Guide to physical therapist Lippincott; 1987.
practice, 2nd ed. Phys Ther. 2001;81:S1928. 33. Staheli L. Practice of Pediatric Orthopedics. Philadelphia: Lippincott
9. World Health Organization. International classification of function- Williams & Wilkins; 2001.
ing, disability and health. Geneva: World Health Organization; 2001. 34. Marks M, Alexander J, Sutherland D, et al. Clinical utility of the
10. Darrah J, Law M, Pollock N. Family-centered functional therapy A Duncan-Ely test for rectus femoris dysfunction during the swing
choice for children with motor dysfunction. Inf Young Children. phase of gait. Dev Med Child Neurol. 2003;45:763768.
2001;13:7987. 35. Barry M, Albright A, Shultz B. Intrathecal baclofen therapy and the
11. Kolobe THA, Sparling J, Daniels LE. Family-centered interventions. role of the physical therapist. Pediatr Phys Ther. 2000;12:7786.
In Campbell, SK, Vander Linden, DW, Palisano, RJ, eds. Physical 36. Olney S, Wright M. Cerebral palsy. In Campbell S, Vander Linden D,
Therapy for Children, Philadelphia: WB Saunders Co, 2000:881 Palisano R, eds. Physical Therapy for Children. Philadelphia: WB
909. Saunders; 2000.
12. Horak FB. Assumptions underlying motor control for neurologic 37. Berry S, Guiliani C, Damiano D. Intrasession and intersession reli-
rehabilitation. In Lister, MJ (Ed.). Contemporary Management of Mo- ability of handheld dynamometry in children with cerebral palsy.
tor Control Problems, Proceeding of the II Step Conference. Alexandria, Pediatr Phys Ther. 2004;16:191198.
VA: Foundation for Physical Therapy; 1991:1128. 38. Taylor N, Dodd K, Graham H. Test-retest reliability of hand-held
13. Bartlett DJ, Palisano RJ. A multivariate model of determinants of dynamometric strength testing in young people with cerebral palsy.
motor change for children with cerebral palsy. Phys Ther. 2000;80: Arch Phys Med Rehabil. 2004;85:7780.
598615. 39. Cusick B, Stuberg W. Assessment of lower extremity alignment in
14. Valvano J. Activity-focused motor interventions for children with the transverse plane: implications for management of children with
neurological conditions. Phys Occup Ther Pediatr. 2004;24:79107. neuromotor dysfunction. Phys Ther. 1992;72:315.
15. Darrah J, Bartlett D. Dynamic systems theory and management of 40. Campbell S, Wilhelm I, Slaton D. Anthropometric characteristics of
children with cerebral palsy: unsolved issues. Infants Young Child. young children with cerebral palsy. Pediatr Phys Ther. 1989;1:105
1995;8:5259. 108.
16. Kamm K, Thelen E, Jensen JL. A dynamical systems approach to 41. Department of Health and Human Services, Centers for Disease
motor development. Phys Ther. 1990;70:763775. Control and Prevention. http://www.cdc.gov/nccdphp/dnpa/bmi/
17. Heriza CB. Implications of a dynamical systems approach to under- bmi-for-age.htm; Accessed October 28, 2005.
standing infant kicking behavior. Phys Ther. 1991;71:222235. 42. Westcott S, Burtner P. Postural control for children: Implications for
18. Sackett DL. Rules of evidence and clinical recommendations on the pediatric practice. Phys Occup Ther Pediatr. 2004;24:555.
use of antithrombotic agents. Chest. 1986;89:2S3S. 43. Cherng R, Su F, Chen J, et al. Performance of static standing balance
19. Sackett D, Straus S, Richardson W, et al. Evidence-Based Medicine: in children with spastic diplegic cerebral palsy under altered sensory
How to Practice and Teach EBM. 2nd ed. New York: Churchill Liv- environments. Am J Phys Med Rehabil. 1999;78:336343.
ingstone; 2000. 44. Bohannon R, Smith M. Interrater reliability of a modified Ashworth
20. Long T, Toscano K. Handbook of Pediatric Physical Therapy, 2nd ed. scale of muscle spasticity: suggestion from the field. Phys Ther.
Philadelphia: Lippincott Williams & Wilkins; 2002. 1987;65:4647.
21. Pharoah P, Cooke T, Cooke R, et al. Birth weight specific trends in 45. Pandyan A, Johnson G, Price C, et al. A review of the properties and
cerebral palsy. Arch Dis Child. 1990;65:602606. limitations of the Ashworth and modified Ashworth Scales as mea-
22. McEwen I. Providing Physical Therapy Services under Parts B & C of sures of spasticity. Clin Rehabil. 1999;13:373383.
the Individuals with Disabilities Education Act (IDEA). Section on 46. Holt K, Butcher R, Fonseca S. Limb stiffness in active leg swinging of
Pediatrics. Alexandria, VA: American Physical Therapy Association; children with spastic hemiplegic cerebral palsy. Pediatr Phys Ther.
2000. 2000;12:5061.
23. Mayston M. People with cerebral palsy: effects of and perspectives 47. Rimmer J. Physical fitness levels of persons with cerebral palsy. Dev
for therapy. Neural Plasticity. 2001;8:5169. Med Child Neurol. 2001;43:208212.
24. King G, Law M, King S, et al. Parents and service providers percep- 48. Unnithan V, Clifford C, Bar-Or O. Evaluation by exercise testing of
tions of family-centeredness of childrens rehabilitation services. the child with cerebral palsy. Sports Med. 1998;26:239251.
Phys Occup Ther Pediatr. 1998;18:2140. 49. Pirpiris M, Wilkinson A, Rodda J, et al. Walking speed in children
25. Law M, Hanna S, King G, et al. Factors affecting family-centered and young adults with neuromuscular disease: comparison be-
service delivery for children with disabilities. Child Care Health Dev. tween two assessment methods. J Pediatr Orthop. 2003;23:302
2003;29:357366. 307.
26. Batshaw M, ed. Children with Disabilities. 4th ed. Toronto: Paul H. 50. Bjornson K. Physical activity monitoring in children and youths.
Brookes; 1997. Pediatr Phys Ther. 2005;17:3745.
27. Washington State Department of Health and the Division of Adoles- 51. Palisano R, Tieman B, Walter S, et al. Effect of environmental setting
cent Medicine. Health and Transition Project, Transition timeline for on mobility methods of children with cerebral palsy. Dev Med Child
children and adolescents with special health care needs: Chronic illness- Neurol. 2003;45:113120.
64 ONeil et al Pediatric Physical Therapy
52. Law M, King G, Russell D, et al. Measuring outcomes in childrens cerebral palsy: a multicenter study. Dev Med Child Neurol. 2004;46:
rehabilitation: decision protocol. Arch Phys Med Rehabil. 1999;80: 311319.
629636. 77. King G, King S, Rosenbaum P, et al. Family-centered caregiving and
53. Fung E, Samson-Fang L, Stallings V, et al. Feeding dysfunction is well-being of parents of children with disabilities: Linking process
associated with poor growth and health status in children with ce- with outcome. J Pediatr Psychol. 1999;24:4153.
rebral palsy. J Am Diet Assoc. 2002;102:361370. 78. Effgen S, Klepper S. Survey of physical therapy practice in educa-
54. Chen C, Heinemann A, Bode R, et al. Impact of pediatric rehabilita- tional settings. Pediatr Phys Ther. 1994;1:1521.
tion services on childrens functional outcomes. Am J Occup Ther. 79. Field D, Martin J, Miller R, et al. A Practical Guide to Teaching
2004;58:4453. Self-Determination. Arlington, VA: Council for Exceptional Chil-
55. Kaminker M, Chiarello L, ONeil M, et al. Decision making for dren Division on Career Development and Training; 1997.
physical therapy service delivery in schools: a nationwide survey of 80. Washington State Department of Health and the Division of Adoles-
pediatric physical therapists. Phys Ther. 2004;84:919933. cent Medicine. Adolescent Health and Transition Project, Transition
56. Bower E, McLellan D. Effect of increased exposure to physiotherapy timeline for children and adolescents with special health care needs:
on skill acquisition of children with cerebral palsy. Dev Med Child developmental disabilities. Seattle: Washington State Department of
Neurol. 1992;34:2539. Health and the Division of Adolescent Medicine; 1995.
57. Bower E, McLellan D, Arney J, et al. A randomized controlled trial of 81. Tilton A. Management of spasticity in children with cerebral palsy.
different intensities of physiotherapy and different goal-setting pro- Semin Pediatr Neurol. 2004;11:5865.
cedures in 44 children with cerebral palsy. Dev Med Child Neurol. 82. Pirpiris M, Trivett A, Baker R, et al. Femoral derotation osteot-
1996;38:226237. omy in spastic diplegia: Proximal or distal? J Bone Jt Surg. 2003;
58. Bower E, Mitchell D, Burnett M, et al. Randomized controlled trial of 85:265272.
physiotherapy in 56 children with cerebral palsy followed for 18 83. Davids J, Ounpuu S, DeLuca P, et al. Optimization of walking ability
months. Dev Med Child Neurol. 2001;43:415. of children with cerebral palsy. J Bone Jt Surg. 2003;85-A:2224
59. Trahan J, Malouin F. Intermittent intensive physiotherapy in chil- 2234.
dren with cerebral palsy: a pilot study. Dev Med Child Neurol. 2002; 84. Tachdjian M. Pediatric Orthopedics. Philadelphia: WB Saunders Co;
44:233239. 1990.
60. Ross S, Engsberg J, Olree K, et al. Quadriceps and hamstring 85. Gough M, Eve L, Robinson R, et al. Short-term outcome of multi-
strength changes as a function of selective dorsal rhizotomy surgery level surgical intervention in spastic diplegic cerebral palsy com-
and rehabilitation. Pediatr Phys Ther. 2001;13:29. pared with the natural history. Dev Med Child Neurol. 2004;46:116
61. US Department of Health and Human Services, Get Fit! A handbook 120.
for youth ages 6-17: how to get in shape to meet the Presidents chal- 86. Karol L. Surgical management of the lower extremity in ambulatory
lenge. Washington, DC: US Department of Health and Human Ser- children with cerebral palsy. J Am Acad Orthop Surg. 2004;12:196
vices; 2001. 203.
62. Hanft B, Place P. The Consulting Therapist: A Guide for OTs and PTs 87. Schwartz M, Viehweger E, Stout J, et al. Comprehensive treatment of
in Schools. San Antonio, TX: Therapy Skill Builders; 1996. ambulatory children with cerebral palsy: an outcome assessment. J
63. Rainforth B. An analysis of physical therapy practice acts: implica- Pediatr Orthop. 2004;24:4553.
tions for role release in educational settings. Pediatr Phys Ther. 1997; 88. Thomas S, Buckon C, Piatt J, et al. A 2-year follow-up of outcomes
9:5461. following orthopedic surgery or selective dorsal rhizotomy in chil-
64. Kaminker M. School-based physical therapy for a child with Meckel- dren with spastic diplegia. J Pediatr Orthop. 2004;13:358366.
Gruber Syndrome. Phys Ther Case Rep. 1999;2:188194. 89. Effgen S, Bjornson K, Chiarello L, et al. Competencies for physical
65. Montgomery P. Predicting potential for ambulation in children with therapists in early intervention. Pediatr Phys Ther. 1991;3:7780.
cerebral palsy. Pediatr Phys Ther. 1998;10:148155. 90. Kolobe T, Sparling J, Daniels L. Family-centered intervention. In:
66. Bleck E. Locomotor prognosis in cerebral palsy. Dev Med Child Neu- Campbell S, Vander Linden D, Palisano R, eds. Physical Therapy for
rol. 1975;17:1825. Children. Philadelphia: WB Saundes; 2000.
67. Watt J, Robertson C, Grace M. Early prognosis for ambulation of 91. Campbell S. Therapy programs for children that last a lifetime. Phys
neonatal intensive care survivors with cerebral palsy. Dev Med Child Occup Ther Pediatr. 1997;17:115.
Neurol. 1989;31:766773. 92. Rone-Adams S, Stern D, Walker V. Stress and compliance with a
68. da Paz AC, Jr. Burnett S, Braga L. Walking prognosis in cerebral home exercise program among caregivers of children with disabili-
palsy: a 22 year retrospective analysis. Dev Med Child Neurol. 1994; ties. Pediatr Phys Ther. 2004;16:140148.
36:130134. 93. Geralis E, ed. Children with Cerebral Palsy: A Parents Guide. Be-
69. Trahan J, Marcoux S. Factors associated with the inability of chil- thesda, MD: Woodbine House; 2001.
dren with cerebral palsy to walk at six years: a retrospective study. 94. Miller F, Bachrach S. Cerebral Palsy: A Complete Guide for Caregiv-
Dev Med Child Neurol. 1994;36:787795. ing. Baltimore: John Hopkins University; 1998.
70. Molnar G, Gordon S. Cerebral palsy: predictive value of selected 95. Batshaw M. Children with Disabilities, 5th ed. Toronto: Paul H
clinical signs for early prognostication of motor function. Arch Phys Brookes; 2002.
Med Rehabil. 1976;57:153158. 96. Hinojosa J. How mothers of preschool children with cerebral palsy
71. Bottos M, Puato M, Viancello A. Locomotion patterns in cerebral perceive occupational and physical therapists and their influence on
palsy syndromes. Dev Med Child Neurol. 1995;37:883899. family life. Occup Ther J Res. 1990;10:144162.
72. Badell-Ribera A. Cerebral palsy: postural locomotor prognosis in 97. Law M, King G. Parent compliance with therapeutic interventions
spastic diplegia. Arch Phys Med Rehabil. 1985;66:614619. for children with cerebral palsy. Dev Med Child Neurol. 1993;35:
73. Wu Y, Day S, Strauss D, et al. Prognosis for ambulation in cerebral 983990.
palsy: a population-based study. Pediatrics. 2004;114:12641271. 98. Piggot J, Paterson J, Hocking C. Participation in home therapy pro-
74. Rosenbaum P, Walter S, Hanna S, et al. Prognosis for gross motor grams for children with cerebral palsy: A compelling challenge. C
function in cerebral palsy: Creation of motor development curves. Qual Health Res. 2002;12:11121129.
JAMA. 2002;288:13571363. 99. Thorpe D, Valvano J. The effects of knowledge of performance and
75. Palisano R, Rosenbaum P, Walter S, et al. Development of the gross cognitive strategies on motor skill learning in children with cerebral
motor function classification system for children with cerebral palsy. Pediatr Phys Ther. 2002;14:215.
palsy. Dev Med Child Neurol. 1997;39:214223. 100. Goodgold-Edwards S, Gianutsos J. Coincidence anticipation perfor-
76. Oeffinger D, Tylkowski C, Rayens M, et al. Gross Motor Function mance of children with spastic cerebral palsy and nonhandicapped
Classification System and outcome tools for assessing ambulatory children. Phys Occup Ther Pediatr. 1991;10:4982.
Pediatric Physical Therapy Clinical Management of Children with Spastic Diplegia 65
101. Goodgold-Edwards S. Motor learning as it relates to the develop- 124. Sterba J, Rogers B, France A, et al. Horseback riding in children with
ment of skilled motor behavior: A review of the literature. Phys cerebral palsy: effect on gross motor function. Dev Med Child Neurol.
Occup Ther Pediatr. 1984;4:518. 2002;44:301308.
102. Gentile A. Skill acquisition: Action, movement, and neuromotor 125. Benda W, McGibbon N, Grant K. Improvements in muscle symme-
processes. In: Shepherd JCR, ed. Movement Science: Foundation for try in children with cerebral palsy after equine-assisted therapy
Physical Therapy in Rehabilitation. Rockville, MD: Aspen; 1987. (hippotherapy). J Altern Complement Med. 2003;9:817825.
103. Gentile A. The nature of skill acquisition: Therapeutic implications 126. Buurke J, Hermens H, Roetenberg D, et al. Influence of hamstring
for children with movement disorders. In: Forssberg E, Hirschfeld lengthening on muscle activation timing. Gait Posture. 2004;20:48
E, eds. Movement disorders in children: Medical Sport Science. Berlin: 53.
Karger; 1999. 127. Desloovere K, Molenaers G, Jonkers I, et al. A randomized study of
104. Chiarello L, Palisano R. Investigation of the effects of a model of combined botulinum toxin type A and casting in the ambulant child
physical therapy on mother-child interactions and the motor behav- with cerebral palsy using objective outcome measures. Eur J Neurol.
iors of children with motor delay. Phys Ther. 1998;78:180194. 2001;8:7587.
105. Peganoff S. The use of aquatics with cerebral palsied adolescents. 128. Lawrence R, Tennstedt S, Kasten L, et al. Intensity and correlates of
Am J Occup Ther. 1984;38:469473. fear of falling and hurting oneself in the next year. J Aging Health.
106. Thorpe D, Reilly M. The effect of an aquatic resistive exercise pro- 1998;10:267286.
gram on lower extremity strength, energy expenditure, functional 129. Butler C, Darrah J. AACPDM evidence report: Effects of neurode-
mobility, balance and self-perception in an adult with cerebral palsy: velopmental treatment (NDT) for cerebral palsy. 2001.
A retrospective case report. J Aquatic Phys Ther. 2000;8:1824. 130. Girolami G, Campbell S. Efficacy of a neuro-developmental treat-
107. Damiano D, Kelly L, Vaughn C. Effects of quadriceps femoris mus- ment program to improve motor control in infants born prema-
cle strengthening on crouch gait in children with spastic diplegia. turely. Pediatr Phys Ther. 1994;6:175184.
Phys Ther. 1995;75:658671. 131. Butler P, Thompson N, Major R. Improvement in walking perfor-
108. Damiano D, Abel M. Functional outcomes of strength training in mance of children with cerebral palsy: Preliminary results. Dev Med
spastic cerebral palsy. Arch Phys Med Rehabil. 1998;79:11925. Child Neurol. 1992;34:567576.
109. Dodd K, Taylor N, Damiano D. A systematic review of the effective- 132. Shumway-Cook A, Hutchinson S, Kartin D, et al. Effect of balance
ness of strength-training programs for people with cerebral palsy. training on recovery of stability in children with cerebral palsy. Dev
Arch Phys Med Rehabil. 2002;83:11571164. Med Child Neurol. 2003;45:591602.
110. MacPhail H, Kramer J. Effect of isokinetic strength training on func- 133. Burtner P, Woollacott M, Qualls C. Stance balance control with
tional ability and walking efficiency in adolescents with cerebral
orthoses in a group of children with spastic cerebral palsy. Dev Med
palsy. Dev Med Child Neurol. 1995;37:763775.
Child Neurol. 1999;41:748757.
111. Daichman J, Johnston T, Evans K, et al. The effects of a neuromus-
134. Ketelaar M, Vermeer A, Hart H, et al. Effects of a functional therapy
cular electrical stimulation home program on impairments and
program on motor abilities of children with cerebral palsy. Phys
functional skills of a child with spastic diplegic cerebral palsy: A case
Ther. 2001;81:15341545.
report. Pediatr Phys Ther. 2003;15:153158.
135. Valvano J. Activity-focused motor interventions for children with
112. Holland L, Steadward R. Effects of resistance and flexibility training
neurological conditions. Phys Occup Ther Pediatr. 2004;24:79107.
on strength, spasticity/muscle tone, and range of motion on elite
136. Richards C, Malouin F, Dumas F, et al. Early and intensive treadmill
athletes with cerebral palsy. Palaestra. 1990;Summer:2731.
locomotor training for young children with cerebral palsy: A feasi-
113. Fowler E, Ho T, Nwige A, et al. The effect of quadriceps femoris
bility study. Pediatr Phys Ther. 1997;9:158165.
muscle strengthening exercises on spasticity in children with cere-
137. Maltais D, Pierrynowski M, Galea V, et al. Minute-by-minute differ-
bral palsy. Phys Ther. 2001;81:12151223.
ences in co-activation during treadmill walking in cerebral palsy.
114. Lowes L, Westcott S, Palisano R, et al. Muscle force and range of
Electromyogr Clin Neurophysiol. 2004;44:477487.
motion as predictors of standing balance in children with cerebral
138. Toner L, Cook K, Elder G. Improved ankle function in children with
palsy. Phys Occup Ther Pediatr. 2004;24:5777.
115. Dodd K, Taylor N, Graham H. A randomized clinical trial of strength cerebral palsy after computer-assisted motor learning. Dev Med
training in young children with cerebral palsy. Dev Med Child Neu- Child Neurol. 1998;40:829835.
rol. 2003;45:652657. 139. Diachman J, Johnston T, Evans K, et al. The effects of a neuromus-
116. Eagleston M, Iams A, McDowell J, et al. The effects of strength cular electrical stimulation home program on impairments and
training on gait in adolescents with cerebral palsy. Pediatr Phys Ther. functional skills of a child with spastic diplegic cerebral palsy: A case
2004;16:2230. report. Pediatr Phys Ther. 2005;15:153156.
117. Bertoti D. Electrical stimulation: a reflection on current clinical 140. Johnston T, Finson R, McCarthy J, et al. Use of functional electrical
practices. Assist Technol. 2000;12:2132. stimulation to augment traditional orthopaedic surgery in children
118. Carmick J. Clinical use of neuromuscular electrical stimulation for with cerebral palsy. J Pediatr Orthop. 2004;24:283291.
children with cerebral palsy, Part 1: lower extremity. Phys Ther. 141. Postans N, Granat M. Effect of functional electrical stimulation,
1993;73:505513. applied during walking, on gait in spastic cerebral palsy. Dev Med
119. Carmick J. Managing equinus in children with cerebral palsy: elec- Child Neurol. 2005;47:4652.
trical stimulation to strengthen the triceps surae muscle. Dev Med 142. Pierce S, Laughton C, Smith B, et al. Direct effect of percutaneous
Child Neurol. 1995;37:965975. electrical stimulation during gait in children with hemiplegic cere-
120. Carmick J. Guidelines for the clinical application of neuromuscular bral palsy: A report of 2 cases. Arch Phys Med Rehabil. 2004;85:
electrical stimulation (NMES) for children with cerebral palsy. Pe- 339343.
diatr Phys Ther. 1997;9:128138. 143. Naslund A, Tamm M, Ericsson A, et al. Dynamic ankle-foot orthoses
121. King E, Gooch J, Howell G, et al. Evaluation of the hip-extensor as a part of treatment in children with spastic diplegiaparents
tricycle in improving gait in children with cerebral palsy. Dev Med perceptions. Physiother Res Int. 2003;8:5968.
Child Neurol. 1993;35:10481054. 144. Buckon C, Thomas S, Jakobson-Huston S, et al. Comparison of three
122. Haehl V, Giuliani C, Lewis C. Influence of hippotherapy on the ankle-foot orthosis configurations for children with spastic diplegia.
kinematics and functional performance of two children with cere- Dev Med Child Neurol. 2004;46:590598.
bral palsy. Pediatr Phys Ther. 1999;11:89101. 145. Park E, Park C, Chang H, et al. The effect of hinged ankle-foot
123. Bertoti D. Effect of therapeutic horseback riding on posture in chil- orthoses on sit-to-stand transfer in children with spastic cerebral
dren with cerebral palsy. Phys Ther. 1988;68:15051512. palsy. Arch Phys Med Rehabil. 2004;85:20532057.
66 ONeil et al Pediatric Physical Therapy
146. Balkrishnan R, Manuel J, Smith B, et al. Longitudinal examination of 170. Samson-Fang L, Stevenson R. Identification of malnutrition in chil-
health outcomes associated with botulinum toxin use in children dren with cerebral palsy: Poor performance of weight-for-height
with cerebral palsy. J Surg Orthop Adv.2004;13:7680. centiles. Dev Med Child Neurol. 2000;42:162168.
147. Gill C, Covington C, Padaliya B, et al. Successful treatment of child- 171. Stallings V, Charney E, Davies J, et al. Nutritional status and growth
hood spasticity to cerebral palsy using Botox. Tenn Med. 2003;96: of children with diplegic or hemiplegic cerebral palsy. Dev Med Child
511513. Neurol. 1993;35:9971006.
148. ONeil M, Fragala M, Dumas H. Physical therapy intervention for 172. Taylor S, Shelton J. Caloric requirements of a spastic immobile ce-
children with cerebral palsy who receive botulinum toxin A injec- rebral palsy patient: a case report. Arch Phys Med Rehabil. 1995;76:
tions. Pediatr Phys Ther. 2003;15:204215. 281283.
149. Dursun E, Dursun N, Alican D. Effects of biofeedback treatment on 173. Thommessen M, Kase B, Riis G, et al. The impact of feeding prob-
gait in children with cerebral palsy. Disabil Rehabil. 2004;26:116 lems on growth and energy intake in children with cerebral palsy.
120. Eur J Clin Nutr. 1991;45:479487.
150. Mauersberger K, Artz K, Duncan B, et al. Can children with spastic 174. Thommessen M, Riis G, Kase B, et al. Energy and nutrient intakes of
cerebral palsy use self-hypnosis to reduce muscle tone? A prelimi- disabled children: do feeding problems make a difference? J Am Diet
nary study. Integrated Med. 2000;2:9396. Assoc. 1991;91:15221525.
151. Rimmer J. Health promotion for individuals with disabilities: the 175. Duffy C, Hill A, Cosgrove A, et al. Energy consumption in children
need for a transitional model in service delivery. Dis Management with spina bifida and cerebral palsy: A comparative study. Dev Med
Health Outcomes. 2002;10:337343. Child Neurol. 1996;38:238243.
152. Rimmer J. Cerebral palsy and exercise. Chicago, IL: The National 176. Azcue M, Zello G, Levy L, et al. Energy expenditure and body com-
Center on Physical Activity and Disability; 2003. position in children with spastic quadriplegic cerebral palsy. J Pedi-
153. US Department of Health and Human Services. Promoting Better atr. 1996;129:870876.
Health for Young People through Physical Activity and Sports. Wash- 177. Rose J, Haskell W, Gamble J. A comparison of oxygen pulse and
ington DC: US Department of Health and Human Services; 2000. respiratory exchange ratio in cerebral palsied and nondisabled chil-
154. Baranowski T, Bar-Or O, Blair S, et al. Guidelines for school and commu- dren. Arch Phys Med Rehabil. 1993;74:702705.
nity Programs to Promote Lifelong Physical Activity among Young People. 178. Fernandez J, Pitetti K, Betzen M. Physiological capacities of individ-
Atlanta, GA: Centers for Disease Control and Prevention; 1997. uals with cerebral palsy. Hum Factors. 1990;32:457466.
155. van den Berg-Emons H, Saris W, de Barbanson D, et al. Daily phys- 179. Fernandez J, Pitetti K. Training of ambulatory individuals with ce-
ical activity of schoolchildren with spastic diplegia and of healthy rebral palsy. Arch Phys Med Rehabil. 1993;74:468472.
control subjects. J Paediatr. 1995;127:578584. 180. Jahnsen R, Villien L, Stanghelle J, et al. Fatigue in adults with cere-
156. Bandini L, Schoeller D, Fukagawa N, et al. Body composition and bral palsy in Norway compared with the general population. Dev
energy expenditure in adolescents with cerebral palsy or myelodys- Med Child Neurol. 2003;45:269303.
plasia. Pediatr Respir. 1991;29:7077. 181. Samson-Fang L, Fung E, Stallings V, et al. Relationship of nutri-
157. van den Berg-Emons R, Van Baak M, Speth L, et al. Physical training tional status to health and societal participation in children with
of school children with spastic cerebral palsy: effects on daily activ- cerebral palsy. J Pediatr. 2002;141:637643.
ity, fat mass and fitness. Int J Rehabil Res. 1998;21:179194. 182. Chad K, McKay H, Zello G, et al. Body composition in nutritionally
158. Parker D, Carriere L, Hebertreit H, et al. Muscle performance and adequate ambulatory and non-ambulatory children with cerebral
gross motor function of children with spastic cerebral palsy. Dev palsy and a healthy reference group. Dev Med Child Neurol. 2000;42:
Med Child Neurol. 1993;35:1723. 334339.
159. Unnithan V, Dowling J, Frost G, et al. Cocontraction and phasic 183. Chad K, Bailey D, McKay H, et al. The effect of weight-bearing
activity during gait in children with cerebral palsy. Electromyo- physical activity program on bone mineral content and estimated
graphic Clinical Neurophysiology 1996;36:487494. volumetric density in children with spastic cerebral palsy. J Pediatr.
160. American College of Sports Medicine. ACSMs Guidelines for Exer- 1999;135:115117.
cise Testing and Prescription, 6th ed. Baltimore: Lippincott, Williams 184. Henderson R, Lin P, Greene W. Bone-mineral density in children
& Wilkins; 2000. and adolescents who have spastic cerebral palsy. J Bone Joint Surg
161. Bar-Or O, Rowland T. Pediatric exercise medicine: from physiologic prin- Am. 1995;11:16711681.
ciples to health care application. Champaign, IL: Human Kinetics; 2004. 185. Brunquell P, Glennon C, DiMario F, et al. Prediction of outcomes
162. Tieman B, Palisano R, Gracely E, et al. Gross motor capability and based on clinical seizure type in newborn infants. J Pediatr. 2002;
performance of mobility in children with cerebral palsy: A compar- 140:707712.
ison across home, school, and outdoors/community settings. Phys 186. Kennes J, Rosenbaum P, Hanna S, et al. Health status of school-aged
Ther. 2004;84:419429. children with cerebral palsy: information from a population-based
163. Cusick B. Progressive Casting and Splinting for Lower Extremity De- sample. Dev Med Child Neurol. 2002;44:240247.
formities in Children with Neuromotor Dysfunction. Tucson, AZ: 187. Bosch J, Mraz R, Mashruch J, et al. Constipation in young children with
Therapy Skill Builders; 1990. developmental disabilities. Infants Young Child. 2002;15:6677.
164. Stuberg W. Considerations related to weight-bearing programs in 188. Field S, Hoffman A, Spezia S. Self-Determination Strategies for Ado-
children with developmental disabilities. Phys Ther. 1992;72:3540. lescents in Transition. Austin, TX: PRO-ED 1998:17.
165. Gudjonsdottir B, Mercer V. Effects of a dynamic versus a static prone 189. Powers L, Singer G, Sowers J, eds. On the Road to Autonomy: Promot-
stander on bone mineral density and behavior in four children with ing Self-Competence in Children and Youth with Disabilities. Balti-
severe cerebral palsy. Pediatr Phys Ther. 2002;14:3846. more: Paul H. Brookes Publishing; 1996.
166. Logan L, Byers HK, Ciccone C. Anterior versus posterior walkers: a 190. Sands D, Wehmeyer M, eds. Self-Determination Across the Lifespan:
gait analysis study. Dev Med Child Neurol. 1990;32:10441048. Independence and Choice for People with Disabilities. Baltimore: Paule
167. Greiner B, Czerniecki J, Deitz J. Gait parameters of children with H. Brookes; 1996.
spastic diplegia: a comparison of effects of posterior and anterior 191. American Academy of Pediatrics, American Academy of Family
walkers. Arch Phys Med Rehabil. 1993;74:381385. Practice, American College of Physicians-American Society of Inter-
168. Stevenson R, Hayes R, Cater L, et al. Clinical correlates of linear nal Medicine. A Consensus Statement on Health Care Transitions
growth in children with cerebral palsy. Dev Med Child Neurol. 1994; for Young Adults with Special Health Care Needs Pediatrics 2002;
36:135142. 110:13041306.
169. Gonzalez L, Nazario C, Gonzalez M. Nutrition-related problems of 192. American Physical Therapy Association. Intervention for Youth who
pediatric patients with neuromuscular disorders. P R Health Sci J. are in Transition from School to Adult Life. Alexandria, VA: American
2000;19:3538. Physical Therapy Association; 2004.
Pediatric Physical Therapy Clinical Management of Children with Spastic Diplegia 67
193. Law M, Baptiste S, Carswell A, et al. Canadian Occupational Perfor- 214. Watling R, Deitz J, White O. Comparison of Sensory Profile scores of
mance Measure, 2nd ed. Toronto: Canadian Association of Occupa- young children with and without autism spectrum disorders. Am J
tional Therapists; 1994. Occup Ther. 2001;55:416423.
194. Toomey M, Nicholson D, Carswell A. The clinical utility of the 215. Braun S. The Functional Independence Measure for Children
Canadian Occupational Performance Measure. Can J Occup Ther. (WeeFim instrument): Gateway to the WeeFIM system. J Rehabil
1995;62:242249. Outcomes Meas. 1998;2:6368.
195. Landgraf J, Abetz L. Measuring health outcomes in pediatric popu- 216. McAuliffe C, Wenger R, Schneider J, et al. Usefulness of the Wee-
lations: Issues in psychometrics and application. In: Spilker B, ed. Functional Independence Measure to detect functional change in
Quality of Life and Pharmacoeconomics in Clinical Trials. New York: children with cerebral palsy. Pediatr Phys Ther. 1998;10:2328.
Raven Press;1996:793802. 217. Msall M, DiGaudio K, Duffy L, et al. WeeFIM. Normative sample of
196. Landgraf J, Abetz L, Ware J. The Child Heath Questionnaire Users an instrument for tracking functional independence in children.
Manual. 2nd printing. Boston, MA: HealthAct; 1999. Clin Pediatr 1994;33:431438.
197. Samson-Fang L, Fung E, Stallings V, et al. Relationship of nutri- 218. Msall M, DiGaudio K, Rogers B, et al. The Functional Independence
tional status to health and societal participation in children with Measure for Children (WeeFIM). Conceptual basis and pilot use in
cerebral palsy. J Pediatr. 2002;141:637643. children with developmental disabilities. Clin Pediatr. 1994;33:421
198. Len C, Goldenberg J, Hilario M, et al. Crosscultural reliability of the 430.
Childhood Health Assessment Questionnaire. J Rheumatol. 1994;21: 219. Ottenbacher KJ, Msall ME, Lyon N, et al. Functional assessment and
23492352. care of children with neurodevelopmental disabilities. Am J Phys
199. Furlong W, Feeny D, Torrance G. Health Utilities Index (HUIR) Med Rehabil. 2000;79:114123.
Measurement System: Algorithm for Determining HUI Mark 2 (HUI2)/ 220. Azaula M, Msall M, Buck G, et al. Measuring functional status and
Mark 3 (HUI3) Health Status Classification Levels, Health States, Sin- family support in older school-aged children with cerebral palsy:
gle-Attribute Level Utility Scores and Overall Health-Related Quality of Comparison of three instruments. Arch Phys Med Rehabil. 2000;81:
Life Utility scores from Self-Complete, 4-Week, Health Status Ques- 307311.
tionnaire. Hamilton, ON: Health Utilities Inc; 1999. 221. Dodds T, Martin D, Stolov W, et al. A validation of the Functional
200. Horsman J, Furlong W, Feeny D, et al. The Health Utilities Index Independence Measurement and its performance among rehabilita-
(HUI): Concepts, measurement properties and applications. Health tion inpatients. Arch Phys Med Rehabil. 1993;74:531536.
Qual Life Outcomes. 2003;1:113. 222. McPherson KM, Pentland B, Cudmore SF, et al. An inter-rater reli-
201. Haley S, Coster W, Ludlow L, et al. Pediatric Evaluation of Disability ability study of the Functional Assessment Measure (FIM FAM).
Disabil Rehabil. 1996;18:341347.
Inventory (PEDI): Development, Standardization and Administration
223. Chau N, Daler S, Andre JM, et al. Inter-rater agreement of two
Manual. Boston: PEDI Research Group; 1992.
functional independence scales: the Functional Independence Mea-
202. McCarthy M, Silberstein C, Atkins E, et al. Comparing reliability
sure (FIM) and a subjective uniform continuous scale. Disabil Re-
and validity of pediatric instruments for measuring health and well-
habil. 1994;16:6371.
being of children with spastic cerebral palsy. Dev Med Child Neurol.
224. Linder M, Schindler G, Michaelis U, et al. Medium-term functional
2002;44:468476.
benefits in children with cerebral palsy treated with botulinum
203. Ostensjo S, Carlberg E, Vollestad N. Everyday functioning in young
toxin A: 1 year follow-up using Gross Motor Function Measure. Eur
children with cerebral palsy: functional skills, caregiver assistance,
J Neurol. 2001;8:120126.
and modifications of the environment. Dev Med Child Neurol. 2003;
225. Russell D, Avery L, Rosenbaum P, et al. Improved scaling of the
45:603612.
Gross Motor Function Measure for children with cerebral palsy:
204. Nordmark E, Jarnlo GB, Hagglund G. Comparison of the Gross
Evidence of reliability and validity. Phys Ther. 2000;80:873885.
Motor Function Measure and Pediatric Evaluation of Disability In-
226. Russell D, Rosenbaum P, Avery L, et al. Gross Motor Function Mea-
ventory in assessing motor function in children undergoing selec-
sure (GMFM-66 & GMFM-88) Users Manual. London: Mac Keith
tive dorsal rhizotomy. Dev Med Child Neurol. 2000;42:245252.
Press; 2002.
205. Steinbok P. Outcomes after selective dorsal rhizotomy for spastic 227. Russell D, Rosenbaum P, Cadman D, et al. The Gross Motor Func-
cerebral palsy. Childs Nerv Syst. 2001;17:118. tion Measure: a means to evaluate the effects of physical therapy.
206. Ketelaar M, Vermeer A, Helders P. Functional motor abilities of Dev Med Child Neurol. 1989;31:341352.
children with cerebral palsy: A systematic literature review of assess- 228. Russell D, Rosenbaum P, Gowland C. Gross Motor Function Measure,
ment measures. Clin Rehabil. 1998;12:369380. 2nd ed. Hamilton, ON: Gross Motor Measures Group; 1993.
207. Feldman A, Haley S, Coryell J. Concurrent and construct validity of 229. Darrah J, Piper M, Watt M. Assessment of gross motor skills of
the Pediatric Evaluation of Disability Inventory. Phys Ther. 1990;70: at-risk infants: predictive validity of the Alberta Infant Motor Scale.
602610. Dev Med Child Neurol. 1998;40:485491.
208. Nichols D, Case-Smith J. Reliability and validity of the Pediatric Eval- 230. Fetters L, Tronick E. Discriminative power of the Alberta Infant
uation of Disability Inventory. Pediatr Phys Ther. 1996;8:1524. Motor Scale and the Movement Assessment of Infants for prediction
209. Coster W, Deeney T, Haltiwanger J, et al. School Function Assess- of Peabody Gross Scale Scores in infants exposed in utero to cocaine.
ment. San Antonio, TX: Psychological Corporation, Harcourt Brace Pediatr Phys Ther. 2000;12:1623.
& Company; 1998. 231. Piper M, Pinnell L, Darrah J, et al. Construction and validation of the
210. Hwang J, Davies P, Taylor M, et al. Validation of School Function Alberta Infant Motor Scale (AIMS). Can J of Public Health. 1992;83:
Assessment with elementary school children. OTJR-Occupation Par- s46s50.
ticipation & Health. 2002;22:4858. 232. Blanchard Y, Neilan E, Busanich J, et al. Interrater reliability of early
211. Ermer J, Dunn W. The Sensory Profile: a discriminant analysis of intervention providers scoring the Alberta Infant Motor Scale. Pedi-
children with and without disabilities. Am J Occup Ther. 1998;52: atr Phys Ther. 2004;16:1318.
283290. 233. Miller L, Roid G. Sequence comparison methodology for the analy-
212. Kientz M, Dunn W. A comparison of the performance of children sis of movement patterns in infants and toddlers with and without
with and without autism on the Sensory Profile. Am J Occup Ther. motor delays. Am J Occup Ther. 1993;47:339347.
1997;51:530537. 234. Rahlin M, Rheault W, Cech D. Evaluation of the primary subtests of
213. Dunn W, Brown C. Factor analysis on the Sensory Profile from a Toddler and Infant Motor Evaluation: implications for clinical prac-
national sample of children without disabilities. Am J Occup Ther. tice in pediatric physical therapy. Pediatr Phys Ther. 2003;15:176
1997;51:490495. 183.
68 ONeil et al Pediatric Physical Therapy
235. Long T, Tieman B. Review of two recently published measure- 260. Fewell R, Folio R. Peabody Developmental Motor Scales, 1st ed. Allen,
ment tools: the AIMS and the T.I.M.E. Pediatr Phys Ther. 1998; TX: Developmental Learning Materials Teaching; 1983.
10:6266. 261. Fewell R, Folio R. Peabody Developmental Motor Scales, 2nd ed.
236. Case-Smith J. Analysis of current motor development theory and Austin, TX: Pro-Ed, Inc; 2000.
recently published infant motor assessments. Infant Young Child 262. Stokes N, Deitz J, Crowe T. The Peabody Developmental Fine Motor
1996;9:2941. Scale: an inter-rater reliability study. Am J Occup Ther. 1990;44:334
237. Bayley N. Bayley Scales of Infant Development, 2nd ed. San Antonio, 340.
TX: Psychological Corporation; 1993. 263. Zaino C, Marchese-Gocha V, Westcott S. Timed up and down stairs
238. Gauthier S, Bauer C, Messinger D, et al. The Bayley Scales of Infant as a new measure of functional mobility: Preliminary reliability and
Development II: Where to start? J Dev Behav Pediatr. 1999;20:75 validity. Pediatr Phys Ther. 2004;16:9099.
79. 264. Mackey A, Lobb G, Walt S, et al. Reliability and validity of the
239. Berls A, McEwen I. Battelle Developmental Inventory. Phys Ther. Observational Gait Scale in children with spastic diplegia. Dev Med
1999;79:776783. Child Neurol. 2003;45:411.
240. Glascoe F, Byrne K. The usefulness of the Battelle Developmental 265. DeGangi G, Greenspan S. Test of Sensory Functions in Infants. Los
Inventory Screening Test. Clin Pediatr. 1993;32:273280. Angeles: Western Psychological Services; 1989.
241. Newborg J, Stock J, Wnek L, et al. Battelle Developmental Inventory: 266. DeGangi G, Greenspan S. The development of sensory functions in
An Assessment Tool. Chicago: Riverside; 1984. infants. Phys Occup Ther Pediatr. 1988;8:2133.
242. Schafer D, Moersch M, Rogers S, et al. Early Intervention Develop- 267. DeGangi G. Assessment of sensory, emotional, and attentional problems
mental Profile. Ann Arbor, MI: University of Michigan Press; 1981. in regulatory disordered infants. Infants Young Child. 1991;3:18.
243. Kott K, Held S. Effects of orthoses on upright functional skills of 268. DeGangi G, Berk R, Greenspan S. The clinical measurement of sen-
children and adolescents with cerebral palsy. Pediatr Phys Ther. sory functioning in infants: A preliminary study. Phys Occup Ther
2002;14:199207. Pediatr. 1988;8:123.
244. Taylor M, Gunther J. Standardized walking obstacle course: prelim- 269. Ayres A. Sensory Integration and Praxis Tests. Los Angeles: Western
inary reliability and validity of a functional measurement tool. J Psychological Services; 1989.
Rehabil Outcomes Meas. 1998;2:1525. 270. Crowe T, Deitz J, Richardson P, et al. Inter-rater reliability of the
245. Graham H, Harvey A, Rodda J, et al. The Functional Mobility Scale Clinical Test for Sensory Interaction for Balance. Phys Occup Ther
(FMS). J Pediatr Orthop. 2004;24:514520.
Pediatr. 1990;10:127.
246. Campbell S, Hedeker D. Validity of the Test of Infant Motor Perfor-
271. Luyt L, Bodney S, Keller J, et al. Reliability of determining motor
mance for discriminating among infants with varying risk for poor
strategy used by children with cerebral palsy during the Pediatric
motor outcome. J Pediatr. 2001;139:546550.
Clinical Test of Sensory Interaction for Balance [abstract]. Pediatr
247. Flegel J, Kolobe T. Predictive validity of the Test of Infant Motor
Phys Ther. 1996;8:180.
Performance at school age [abstract]. Pediatr Phys Ther. 1999;11:
272. Westcott S, Crowe T, Deitz J, et al. Test-retest reliability of the
226.
Pediatric Clinical Test of Sensory Interaction for Balance (P-CTSIB).
248. Flegel J, Kolobe T. Predictive validity of the Test of Infant Motor
Phys Occup Ther Pediatr. 1994;14:122.
Performance as measured by the Bruininks-Oseretsky test of mo-
273. Bohannon R, Smith M. Inter-rater reliability of a modified Ashworth
tor proficiency at school age. Phys Ther. 2002;82:762771.
scale of muscle spasticity. Phys Ther. 1987;67:206207.
249. Campbell S, Kolobe T, Wright B, et al. Validity of the Test of Infant
274. Fosang A, Galea M, McCoy A, et al. Measures of muscle and joint
Motor Performance for prediction of 6-, 9- and 12-month scores on
performance in the lower limb of children with cerebral palsy. Dev
the Alberta Infant Motor Scale. Dev Med Child Neurol. 2002;44:263
Med Child Neurol. 2003;45:664670.
272.
250. Barbosa V, Campbell S, Sheftel D, et al. Longitudinal performance of 275. Boyd R, Graham H. Objective measurement of clinical findings in
infants with cerebral palsy on the Test of Infant Motor Performance the use of botulinum toxin type A for the management of children
and on the Alberta Infant Motor Scale. Phys Occup Ther Pediatr. with cerebral palsy. Eur J Neurol. 1999;6:S23S36.
2003;23:729. 276. Hislop H, Montgomery J. Daniels and Worthinghams Muscle Testing:
251. Murney M, Campbell S. The ecological relevance of the Test of Techniques of Manual Examination, 7th ed. Philadelphia: WB Saun-
Infant Motor Performance elicited scale items. Phys Ther. 1998;78: ders; 2002.
479489. 277. Rose J, Gamble J, Lee J, et al. The energy expenditure index: A
252. Harris S, Daniels L. Content validity of the Harris Infant Neuromo- method to quantitate and compare walking energy expenditure
tor Test. Phys Ther. 1996;76:727737. for children and adolescents. J Pediatr Orthop. 1991;11:571578.
253. Harris S, Daniels L. Reliability and validity of the Harris Infant Neu- 278. Rose J, Gamble J, Medeiros J, et al. Energy cost of walking in normal
romotor Test. J Pediatr. 2001;139:249253. children and in those with cerebral palsy: Comparison of heart rate
254. Unanue R, Westcott S, Tieman B, et al. Preliminary normative data and oxygen uptake. J Pediatr Orthop. 1989;9:276279.
on the Harris Infant Neuromotor Test (HINT) [abstract]. Pediatr 279. Enright P. The six-minute walk test. Respir Care. 2003;48 (8):783785.
Phys Ther. 1999;11:223. 280. Duncan P. Physical therapy assessment. In Rosenthal M, Kreutzer J,
255. Brander R, Kramer J, Dancsak M. Inter-rater and test-retest reliabili- Griffith E, et al, eds. Rehabilitation of the Adult and Child With Trau-
ties of the Movement Assessment of Infants. Pediatr Phys Ther. 1993; matic Brain Injury. Philadelphia, PA: FA Davis; 1990.
5:915. 281. Barlett D, Birmingham T. Validity and reliability of a pediatric reach
256. Chandler L, Andrews M, Swanson M. Movement Assessment of In- test. Pediatr Phys Ther. 2003;15:8492.
fants. Rolling Bay, WA: Rolling Bay Press 1980. 282. Niznik T, Turner D, Worrell T. Functional reach as a measurement
257. Harris S, Haley S, Tada W, et al. Reliability of observational mea- of balance for children with lower extremity spasticity. Phys Occup
sures of the Movement Assessment of Infants. Phys Ther. 1984;64: Ther Pediatr. 1995;15:115.
471477. 283. Donahoe B, Turner D, Worrell T. The use of functional reach as a
258. Bruininks R. Bruininks-Oseretsky Test of Motor Proficiency: Examin- measurement of balance in boys and girls without disabilities ages 5
ers manual. Circle Pines, MN: American Guidance Service; 1978. to 15 years. Pediatr Phys Ther. 1994;6:189193.
259. Wilson B, Polatajko H, Kaplan B, et al. Use of Bruininks-Oseretsky 284. Podsiadlo D, Richardson S. The timed up and go: A test of basic
Test of Motor Proficiency in Occupational Therapy. Am J Occup functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;
Ther. 1995;49:817. 39:142148.
Pediatric Physical Therapy Clinical Management of Children with Spastic Diplegia 69
285. Gocha Marchese V, Chiarello L, Lange B. Strength and functional 288. Berg K, Wood-Dauphinee S, Williams J. The balance scale: Reliabil-
mobility in children with acute lymphoblastic leukemia. Med Pediatr ity assessment with elderly residents and patients with acute stroke.
Oncol. 2003;40:230232. Scand J Rehabil Med. 1995;27:2736.
286. Siggeirsdottir K, Jonsson B, Jonsson H, et al. The timed Up & 289. Franjoine M, Gunther J, Taylor M. Pediatric Balance Scale: a
Go is dependent on chair type. Clin Rehabil. 2002;16:609616. modified version of the Berg Balance Scale for the school-age
287. Berg K, Wood-Dauphinee S, Williams J, et al. Measuring balance in the children with mild to moderate impairment. Pediatr Phys Ther.
elderly: Validation of an instrument. Can J Public Health. 1992;83:S7S11. 2003;15:114128.
70 ONeil et al Pediatric Physical Therapy
Appendix A
TABLE 3
Appendix A: Table of Tests and Measures
Level of Test Age Range Purpose of test Description
enablement
[WHO]
Participation Canadian Any age Identifies changes in parent or childs self-perception of performance Provides satisfaction and disability ratings for daily activities and routines, which are, identified by the child and
Occupational over time. family as an important part of daily life. Information is gathered through parent and/or child interview.
Performance
Measure
Pediatric Physical Therapy
(COPM)193, 194
Participation Child Health 2 months 17 years Measures quality of life Provides information on physical and psychosocial health concepts. The questionnaire is completed by parent and/or
Questionnaire child. There are several versions depending on the childs age, parent versus child report, and length of
(CHQ)195197 questionnaire.
Participation Child Health Any age Measures quality of life Developed primarily for children with arthritis but has been used for children with other physical disabilities.
Assessment Questionnaire in which ability to do various ADLs and amount of assistance required is rated by child and/or
Questionnaire caregiver.
(CHAQ)198
Participation Health Utilities Any age Measures childrens functional health status; can compute cardinal Questionnaire completed by caregiver in eight domains: Ambulation, Dexterity, Speech, Vision, Hearing, Cognition,
Index Mark 3 utility value to represent Health Related Quality of Life Emotion, and Pain
(HUI-3)199, 200
Participation/ Pediatric Evaluation 6 months to 7.5 years or Measures self-care and mobility capabilities and performance in the Functional Skills and Caregiver Assistance sections for each of the three domains of Self-care, Mobility and Social
Activity of Disability any age as long as home and community environments. Detects change over time and Function; Observed or rated through interview with child and/or caregiver. Normative and scaled scores are
Inventory mobility skills are can be used to monitor progress. available.
(PEDI)201208 under 7.5 years
Participation/ School Function Elemen-tary school Measures function in the school environment and can be used to Three parts: Participation in school activity settings; Task supports; Activity Performance. Includes physical and
Activity Assessment students guide program planning cognitive/behavioral tasks. Criterion-referenced and scaled scores are available. Designed to be used in an
(SFA)209,210 integrated setting and requires input from all team members in order to represent a students performance in a
variety of environments.
Participation/ Sensory Profile211214 3-10 years Determines which sensory processes contribute to performance Parent questionnaire, which rates childs sensory system responses to different activities/environments. Nine factors
Body Structure/ strengths and barriers in a childs life scored from care-givers ratings: Sensory seeking; Emotionally reactive; Low endurance/Tone; Oral sensory seeking;
Function Inattention/Distractibility; Poor registration: Sensory sensitivity; Sedentary; Fine motor/Perceptual
Activity Functional 6 months to 7 years Measures changes in mobility and ADL skills. Can be used for Performance in self-care, sphincter control, transfers, locomotion, communication and social cognition. Criterion-
Independence program evaluation and rehabilitation outcomes. referenced. Outcomes are sent to the Universal Data System for Medical Rehabilitation for outcome reporting and
Measure for external benchmarking.
Children (Wee
FIM)215220
Activity Functional 7 years through adulthood Measures changes in mobility and ADL skills. Can be used for Performance in self-care, sphincter control, transfers, locomotion, communication and social cognition. Criterion-
Independence program evaluation and rehabilitation outcomes. referenced. Outcomes are sent to the Universal Data System for Medical Rehabilitation for outcome reporting and
Measure external benchmarking.
(FIM)221 223
Activity Gross Motor Birth 5 years or Any age Measures gross motor skills and can be used to monitor progress of Criterion-referenced performance based test with five dimensions: Lying and rolling; Sitting; Crawling and Kneeling;
Function Measure as long as gross motor children with cerebral palsy and other disabilities. Standing; and Walking, Running, Jumping. There are 2 versions of the GMFM: one with 88 items and the other
(GMFM)224228 skills are less than 5 with 66 items. Scaled scores are available for the 66 item version.
years
Activity Alberta Infant Motor Birth to 18 months Identifies motor delays in infants and measures change in motor skills Performance based and norm referenced. Tests motor development in prone, supine, sitting and standing positions.
Scale (AIMS)229232 over time. Documents some quality of movement items such as posture and weight bearing. Norm-referenced.
Activity Toddler and Infant 4 months to 3.5 years Identifies children with mild to severe motor problems. Measures Contains five subtests: Mobility, Stability, Motor Organization, Functional Performance, and Social-emotional
Motor Evaluation sensory and motor development and can be used to monitor Abilities.
(TIME)233236 progress.
Activity Bayley Scales of 1-42 months Identifies developmental gross motor, fine motor, and cognitive Measures development on two scales: Mental which includes language and perceptual skills and Motor which includes
Infant delays. Can be used to monitor progress. gross motor and fine motor behavior. Norm-referenced
Development, 2nd
edition
(BSID-II)237, 238
Activity Battelle Birth to 8 years Identifies developmental level of infant or young child and can be Judgment or performance based measure administered through structured format, interviews with caregivers or
Developmental used to monitor changes over time. naturalistic observations. Contains Gross Motor, Fine Motor, Personal-social, Adaptive, Communication, and
Inventory 197, 239241 Cognition items. Norm-referenced.
Activity Early Intervention Birth 3 Developmental screening tool Provides information on the following areas: cognition, gross motor, language, perceptual/fine motor, self-care, social/
Developmental emotional development.
Profile 242
Activity Standardized Any age child or youth Measures stability and speed of gait in a natural and functional setting. The obstacle course is 12.2 meters long by 0.9 meters wide. The course requires negotiating three directional turns of
Walking Obstacle who is able to walk 30, 90 and 70 degrees, stepping over obstacle, walking on different surfaces, and moving from sit to stand and
Course243,244 independently stand to sit
Activity Functional Mobility Any age child or youth Measures speed of mobility across three distances. Functional mobility scored over three distances chosen to represent mobility in the home, school, and community
Scale (FMS)245 who is able to walk
independently Any age
Activity/ Body Test of Infant Motor 32 weeks gestational age to Provides early identification of motor delays; assesses postural control Two scales: Observed scale of infants spontaneous movements; and elicited scale of infants postural and movement
Structure/ Performance four months for early skill acquisition response to handling.
Function (TIMP)246251
Clinical Management of Children with Spastic Diplegia 71
TABLE 3
72
Continued.
Level of Test Age Range Purpose of test Description
enablement
[WHO]
Activity/ Body Harris Infant 0-12 months Screening tool; identifies neuromotor differences in Five item parent /caregiver section; 21 item infant assessment section including motor behaviors
ONeil et al
Structure/ Neuromotor Test infants aged 3 to 12 months. in supine-lying, prone-lying, transitions from prone and supine, supported sitting, and
Function (HINT)252254 supported standing; head circumference measurement; and a two part developmental and
qualitative judgment item.
Activity/ Body Movement Assessment of 0-12 months Identifies motor dysfunction in infants and can be Four sections: Muscle Tone, Primitive Reflexes, Automatic Reactions, and Volitional Movement.
Structure/ Infants (MAI)255257 used to monitor motor abilities in infants. Criterion referenced and normative information available for 4 and 8 month old infants only.
Function
Activity/Body Bruininks-Oseretsky Test 4.5 14.5 years Identifies motor abilities and can be used for program Gross Motor subtests include: Running Speed and Agility, Strength, Balance, and Coordination.
Structure/ of Motor Proficiency planning. Can also be used to monitor change over Norm-referenced.
Function (BOTMP)258259 longer periods of time for children with mild
disabilities.
Activity/Body Movement Assessment 4-12 years Identifies and describes impairments of motor This test consists of a Performance Test for a standardized assessment of manual dexterity, ball
Structure/ Battery for Children function skills, and static and dynamic balance and a Checklist used by parents, teachers, or other
Function (M- ABC)248250 professionals over a 1-2 week period to score items that are part of a childs daily routine and
ADLs. Norm referenced.
Activity/ Body Peabody Developmental Birth to 5 years Identifies gross and fine motor delays and can be used Has a gross motor and fine motor scale. Gross Motor Scale contains: Reflexes, Stationary,
Structure/ Motor Scales, to monitor progress. Locomotion, Object manipulation. Fine Motor contains: Grasping, Visual-motor integration.
Function 2nd ed (PDMS-2)260- Norm referenced.
262
Activity/Body Test of Gross Motor 3-10 years To determine a childs acquisition of selected gross Tests the areas of locomotion and object control with each item having three or four specific
Structure/ Development 2 motor tasks performance criteria to indicate childs skill maturity on the item. Test is administered using
Function (TGMD-2)248250 specific materials and standardized procedures.
Activity/Body Timed Up and Down Any age child or youth Measures time to ascend and descend stairs The child is timed while walking up and down a set of stairs. The gait pattern is also described.
Structure/ Stairs test (TUDS)263 who can walk
Function independently up and
down stairs
Body Structure/ Observational Gait Scale 6 yrs-adult Structured scale to rate gait parameters Modified version of the Physicians Rating Scale. Seven sections rated: Knee mid-stance; Initial
Function (OGS)264 foot contact; Foot contact mid-stance; Heel rise; Hind foot; Base of support; Assistive devices
Body Structure/ Test of Sensory Function 4-18 months Assists in diagnosing sensory processing dysfunction. Performance based test with five subtests: 1) reactivity to tactile deep pressure 2) vestibular
Function in Infants 265268 Identifies children ages 4-18 months who are at stimulation, 3)adaptive motor function, 4) visual tactile integration, and 5) oculomotor
risk for future developmental delay and learning control.
deficits.
Body Structure/ Sensory Integration and 4-8 yrs 11 months Measures the sensory systems contributions to balance Numerous tests of postural control, motor coordination and planning, fine and gross motor
Function Praxis Test 269 and motor coordination function, and sensory integration
Body Structure/ Pediatric Clinical Test of 4-10 years Measures sensory system effects on stationary standing Six conditions: Standing on floor with eyes open, eyes closed, and with dome (eyes open, but
Function Sensory Interaction postural control (balance) vision stabilized); Standing on foam with eyes open, eyes closed, and with dome (eyes open,
for Balance (P-CTSIB) but vision stabilized)
270272
Body Structure/ Tests for hip joint Any age Gross test to determine likelihood of dislocation Ortolanis sign: Manual movement of the hip joint. With child in supine and hips and knees
Function integrity 34 flexed to 90, therapist places thumb on medial thigh and finger over greater trochanter and
gently abducts hip. Will feel a clunk if hip is dislocated. Barlows sign: With the child in
supine and hips and knees flexed to 90, therapist also observes for asymmetrical skin folds,
limited hip abduction, and apparent shortening of one leg.
Body Structure/ Leg length discrepancy34 Any age Clinical measure of leg length Tape measurement from ASIS to medial malleoli while lying in supine.
Function
Body Structure/ Modified Ashworth Scale 4-5 years and older Measures resistance to passive movement associated Passive movement of a limb through range while judging the resistance to the movement.
Function (MAS)273,274 with spasticity Resistance is judged on an ordinal scale. Reliability of MAS in children is variable and should
be used with caution.
Body Structure/ Modified Tardieu 4-5 years and older Measures amount of joint range with passive Limb is moved quickly through the available range of motion and the joint position of initial
Function Scale275 movement and is associated with spasticity resistance to passive movement is recorded as the first catch (R1) and then the limb is moved
slowly to the end range (R2) and this joint position is also recorded.
Body Structure/ Manual Muscle Test 4-5 years and older Provides information about muscle strength Elicit contraction of muscles and if child is strong enough, apply manual resistance in gravity
Function (MMT)276 eliminated positions or against gravity. Strength is judged on an ordinal scale.
Body Structure/ Energy Expenditure 3 years and older Measures endurance level and can be used to monitor Calculation of heart rate (beats per minute), distance walked (meters) and time (minutes). EEI
Function Index (EEI)277,278 changes over time. Working HR - Resting Heart Rate Speed. Normative values for self-selected and fast paced
walking for children 5-15 years.
Body Structure/ Six Minute Walk Test 279 5 years and older Measures walking endurance and can be used to Distance walked in 6 minutes over level ground.
Function monitor change over time.
Body Structure/ Functional Reach Test 4 years and older Measures anticipatory postural control when reaching Measurement of the distance that the child can reach forward from a stationary standing position.
Function (FRT)280283 from standing Normative values available.
Body Structure/ Timed Up and Go 4 years and older Measures anticipatory standing balance, gait control, Measurement of the time it takes to rise from a chair, walk 3 meters, turn around and return to a
Function (TUG)284286 and motor function through a typical activity seated position in the chair.
Body Structure/ Pediatric (Berg) Balance 5 years and older Measures balance during movement activities 14 items including common movement activities such as sit to stand, transfers, picking an object
Function Test 287289 up from the floor, and walking and turning.
Pediatric Physical Therapy
S-ar putea să vă placă și
- Extremitas FormDocument2 paginiExtremitas FormAbdur RasyidÎncă nu există evaluări
- Lumbar Assessment Form 2017Document2 paginiLumbar Assessment Form 2017nsboyadzhievÎncă nu există evaluări
- Pediatric Physiotherapy Assessment Aidaaaaa 2Document15 paginiPediatric Physiotherapy Assessment Aidaaaaa 2Khaled M.A. AlqedraÎncă nu există evaluări
- Physiotherapy Advice After Your Kidney TransplantDocument8 paginiPhysiotherapy Advice After Your Kidney TransplantAlexander ScottÎncă nu există evaluări
- Reflex DR Arpana HazarikaDocument126 paginiReflex DR Arpana HazarikaDorin Pathak100% (1)
- Effect of Roods Approach in Diabetic PolyneuropathyDocument6 paginiEffect of Roods Approach in Diabetic Polyneuropathynandhini ragu100% (1)
- Process of Motor DevelopmentDocument33 paginiProcess of Motor Developmentmohitnet1327Încă nu există evaluări
- Down syndrome facts and clinical featuresDocument37 paginiDown syndrome facts and clinical featuresBenita DavidÎncă nu există evaluări
- Sensory Integration Processing Jargon GuideDocument4 paginiSensory Integration Processing Jargon Guideapi-660820048Încă nu există evaluări
- Physical Therapy Management of Congenital Muscular.2Document47 paginiPhysical Therapy Management of Congenital Muscular.2Katherine Valeska Sánchez MuñozÎncă nu există evaluări
- 2.operational Guidelines DEIC RBSKDocument100 pagini2.operational Guidelines DEIC RBSKChristopher Mala100% (1)
- 5 Senior ExercisesDocument3 pagini5 Senior Exercisestamaki55Încă nu există evaluări
- Effects of Physioball and Conventional Floor Exercises On Early Phase Adaptations in Back and Abdominal Core Stability and Balance in Women 2003Document5 paginiEffects of Physioball and Conventional Floor Exercises On Early Phase Adaptations in Back and Abdominal Core Stability and Balance in Women 2003rdkelsallÎncă nu există evaluări
- Soap NoteDocument2 paginiSoap Noteapi-382628487Încă nu există evaluări
- Suspension TherapyDocument43 paginiSuspension TherapyAnup Pednekar0% (1)
- Facilitation For A CP ChildDocument4 paginiFacilitation For A CP ChildpraveenÎncă nu există evaluări
- International Physical Activity Questionnaire - Short Form: Evaluation MeasuresDocument8 paginiInternational Physical Activity Questionnaire - Short Form: Evaluation MeasuresAyyÎncă nu există evaluări
- Immobilization SyndromeDocument24 paginiImmobilization SyndromeJuanitoCabatañaLimIII100% (1)
- Day 3 Principles of Rehabilitation in Elderly The NewestDocument43 paginiDay 3 Principles of Rehabilitation in Elderly The NewestaniendyawijayaÎncă nu există evaluări
- Key Responsibilities:: Occupational Therapist Job Description V-Jan/2020Document4 paginiKey Responsibilities:: Occupational Therapist Job Description V-Jan/2020MD Luthfy LubisÎncă nu există evaluări
- Rood Approach Muscle RehabilitationDocument33 paginiRood Approach Muscle RehabilitationCedricFernandez100% (1)
- Weekly Learning Activities: Prenatal To Age 2: Monday Tuesday Wednesday Thursday FridayDocument5 paginiWeekly Learning Activities: Prenatal To Age 2: Monday Tuesday Wednesday Thursday FridayCamara Cu ZambeteÎncă nu există evaluări
- Neurorehabilitasi Nyeri KronisDocument60 paginiNeurorehabilitasi Nyeri KronisWegrimel AriegaraÎncă nu există evaluări
- Bells Palsy Physio PDFDocument71 paginiBells Palsy Physio PDFडा. सत्यदेव त्यागी आर्यÎncă nu există evaluări
- Chapter 8Document30 paginiChapter 8Karla CarazoÎncă nu există evaluări
- Degenerative Joint Diseases - Admisson ExamDocument23 paginiDegenerative Joint Diseases - Admisson ExamNona NadimÎncă nu există evaluări
- Scapula Setting AnaIsabel AlmeidaDocument1 paginăScapula Setting AnaIsabel AlmeidaPeter ZachÎncă nu există evaluări
- Lumbar Herniation Case StudyDocument1 paginăLumbar Herniation Case Studyapi-238652699Încă nu există evaluări
- Praktikum PX Sensoris: Dr. Nisa Karima, M.SCDocument18 paginiPraktikum PX Sensoris: Dr. Nisa Karima, M.SCCaesarioÎncă nu există evaluări
- FxwsensorychildDocument31 paginiFxwsensorychildapi-534627445Încă nu există evaluări
- CIMT ManualDocument48 paginiCIMT ManualExternal100% (1)
- Brochure PhysiotherapyDocument4 paginiBrochure Physiotherapyfiore6Încă nu există evaluări
- Guide To Functional Assessment ScreeningDocument2 paginiGuide To Functional Assessment ScreeningStudent StudentÎncă nu există evaluări
- DR Luh - Role of PMR in NICUDocument50 paginiDR Luh - Role of PMR in NICUad putraÎncă nu există evaluări
- Motor MildstonesDocument13 paginiMotor MildstonesVaio Wolff AbendrothÎncă nu există evaluări
- Rehabilitation Priciples at Children With Cerebral Palsy After NDT Bobath ConceptDocument13 paginiRehabilitation Priciples at Children With Cerebral Palsy After NDT Bobath ConceptAndrei TîrziuÎncă nu există evaluări
- Gross Motor Development in Infants With Multiple ImpairmentsDocument11 paginiGross Motor Development in Infants With Multiple ImpairmentsAuliana FEÎncă nu există evaluări
- Developmental AssessmentDocument78 paginiDevelopmental AssessmentGayathri PriyadharshiniÎncă nu există evaluări
- Assessment of Sensory SystemDocument21 paginiAssessment of Sensory SystemDr. SyedaÎncă nu există evaluări
- Pediatric motor and visual assessments for occupational therapyDocument4 paginiPediatric motor and visual assessments for occupational therapyBea FloresÎncă nu există evaluări
- Physiotherapy's Role in Managing Spasticity for Children with Cerebral PalsyDocument3 paginiPhysiotherapy's Role in Managing Spasticity for Children with Cerebral PalsyKhusnah KhauliyaÎncă nu există evaluări
- Physiotherapy management of paediatric flat feetDocument20 paginiPhysiotherapy management of paediatric flat feetCalvina MizumiÎncă nu există evaluări
- Cerebral Palsy Info SheetDocument3 paginiCerebral Palsy Info Sheetapi-263996400100% (1)
- Estrategias Conductuales ASDDocument66 paginiEstrategias Conductuales ASDSuperfixenÎncă nu există evaluări
- Untitled - Susan BlumDocument65 paginiUntitled - Susan BlumnewÎncă nu există evaluări
- The Importance of Postural Control For Feeding. REVIEW PDFDocument5 paginiThe Importance of Postural Control For Feeding. REVIEW PDFViviana SalazarÎncă nu există evaluări
- Vojta Therapy: Reflex Creeping in A Prone Lying Position and Reflex Rolling From A Supine and Side LyingDocument7 paginiVojta Therapy: Reflex Creeping in A Prone Lying Position and Reflex Rolling From A Supine and Side LyingSonali SoumyashreeÎncă nu există evaluări
- Babinski & Parachute Reflex PPT Group 3 Bsn2aDocument23 paginiBabinski & Parachute Reflex PPT Group 3 Bsn2aPaula AbadÎncă nu există evaluări
- Sensation & Perception: Mr. Nabin BajracharyaDocument113 paginiSensation & Perception: Mr. Nabin BajracharyaRaunak PradhanÎncă nu există evaluări
- Physiotherapy For Stroke Patients - Physiotherapy Remedies For Victims of StrokeDocument9 paginiPhysiotherapy For Stroke Patients - Physiotherapy Remedies For Victims of StrokeHumaira RahmanÎncă nu există evaluări
- Bobath ConceptDocument5 paginiBobath ConceptdrprasantÎncă nu există evaluări
- AOPA Handout NewParadigms Sciences IMPDocument34 paginiAOPA Handout NewParadigms Sciences IMPAnup PednekarÎncă nu există evaluări
- Low Muscle Tone, Muscle Weakness or Poor Learning Strategies?Document5 paginiLow Muscle Tone, Muscle Weakness or Poor Learning Strategies?Ruztiqa Kasih Pramudya VardaniÎncă nu există evaluări
- Spinal Cord Assesment Form PTDocument8 paginiSpinal Cord Assesment Form PTSureaka PonnusamyÎncă nu există evaluări
- Assessment of HandDocument76 paginiAssessment of Handchirag0% (1)
- NDT in Children - Gina Rencken 2022 - PANDADocument20 paginiNDT in Children - Gina Rencken 2022 - PANDAGokul SriniÎncă nu există evaluări
- Family Observation Interview and ReflectionDocument10 paginiFamily Observation Interview and Reflectionapi-568085226Încă nu există evaluări
- Neurological Assessment in the First Two Years of LifeDe la EverandNeurological Assessment in the First Two Years of LifeGiovanni CioniÎncă nu există evaluări
- Movement Difficulties in Developmental Disorders: Practical Guidelines for Assessment and ManagementDe la EverandMovement Difficulties in Developmental Disorders: Practical Guidelines for Assessment and ManagementÎncă nu există evaluări
- Sentence SubjectsDocument3 paginiSentence SubjectsClaudia MicuÎncă nu există evaluări
- MACS Identification Chart Eng PDFDocument1 paginăMACS Identification Chart Eng PDFClaudia MicuÎncă nu există evaluări
- NSAA Only ManualVersion-2.0 May-2017Document19 paginiNSAA Only ManualVersion-2.0 May-2017Raghu NadhÎncă nu există evaluări
- Efficacy of Botulinum Toxin A in Children With Cerebral Palsy PDFDocument10 paginiEfficacy of Botulinum Toxin A in Children With Cerebral Palsy PDFClaudia MicuÎncă nu există evaluări
- Jie Zhao: Author'S ReplyDocument1 paginăJie Zhao: Author'S ReplyClaudia MicuÎncă nu există evaluări
- ACR 2011 Juvenile Idiopathic Arthritis Clinicians GuideDocument7 paginiACR 2011 Juvenile Idiopathic Arthritis Clinicians GuideAya SorayaÎncă nu există evaluări
- Abpmr Cert BoiDocument19 paginiAbpmr Cert BoiClaudia MicuÎncă nu există evaluări
- WristDocument7 paginiWristvenugopalarulÎncă nu există evaluări
- Enraf Nonius Curapuls 670Document69 paginiEnraf Nonius Curapuls 670Claudia MicuÎncă nu există evaluări
- Developmental Neurology and Neuro RehabilitationDocument2 paginiDevelopmental Neurology and Neuro RehabilitationClaudia MicuÎncă nu există evaluări
- AHA-ASA Guideline For Adult Stroke Rehab and RecoveryDocument73 paginiAHA-ASA Guideline For Adult Stroke Rehab and RecoveryAfifaFahriyaniÎncă nu există evaluări
- Pediatric Course Eular SiteDocument7 paginiPediatric Course Eular SiteClaudia MicuÎncă nu există evaluări
- Neuromuscular DisordersDocument98 paginiNeuromuscular DisordersClaudia MicuÎncă nu există evaluări
- Osteoporosis NOGG Guideline 2017Document36 paginiOsteoporosis NOGG Guideline 2017Claudia Micu100% (1)
- Physical Therapy Clinical ManagementDocument24 paginiPhysical Therapy Clinical ManagementClaudia MicuÎncă nu există evaluări
- Hildegard Peplau's Interpersonal Relations 101Document85 paginiHildegard Peplau's Interpersonal Relations 101Ynaffit Alteza Untal100% (1)
- Gestalt TherapyDocument35 paginiGestalt TherapyMary Grace Mojares100% (3)
- Couples Therapy Homework Planner PDFDocument4 paginiCouples Therapy Homework Planner PDFafnaecvbnlblac100% (1)
- Diet TherapyDocument2 paginiDiet TherapyR-Chian Jose GermanpÎncă nu există evaluări
- ClonazepamDocument2 paginiClonazepamjhezelle05100% (2)
- Bromhidrosis NdyagDocument5 paginiBromhidrosis Ndyagika_anggrainiÎncă nu există evaluări
- Nick Franks - Chapter 14 Instruments and Codes FN v2 - Rev 3 For Radionic Journal 17.4.15Document19 paginiNick Franks - Chapter 14 Instruments and Codes FN v2 - Rev 3 For Radionic Journal 17.4.15evandrojsilvaÎncă nu există evaluări
- Unlicensed youth programs pose risksDocument34 paginiUnlicensed youth programs pose risksAnthony PaulÎncă nu există evaluări
- Cabg Case Study FormDocument9 paginiCabg Case Study FormVlad ConstantinÎncă nu există evaluări
- Exploring Perfect PostureDocument8 paginiExploring Perfect Posturesquishyware100% (1)
- Wilderness Remote First Aid ManualDocument128 paginiWilderness Remote First Aid Manualcr4zyvi3t100% (3)
- Are You One of Them? Internet and Cell Phone AddictionDocument25 paginiAre You One of Them? Internet and Cell Phone AddictionApril PalamosÎncă nu există evaluări
- Dysfunctional Uterine Bleeding and Dysmenorrhea GuideDocument44 paginiDysfunctional Uterine Bleeding and Dysmenorrhea GuideonijinoÎncă nu există evaluări
- Does Music Therapy Really WorkDocument7 paginiDoes Music Therapy Really WorkCtÎncă nu există evaluări
- Management For Challenged ChildrenDocument7 paginiManagement For Challenged ChildrenUday Kumar50% (2)
- The How and Why of The Movement System As The Identity of Physical TherapyDocument8 paginiThe How and Why of The Movement System As The Identity of Physical TherapyValeria Javalera BatÎncă nu există evaluări
- Neonatal Resuscitation ProgramDocument6 paginiNeonatal Resuscitation ProgramRick Frea100% (5)
- Academic Stress and Emotion Regulation in The Iranian Female Students With High and Low Academic PerformanceDocument2 paginiAcademic Stress and Emotion Regulation in The Iranian Female Students With High and Low Academic PerformanceAitana ParrillaÎncă nu există evaluări
- REVALIDA EXAM 200 Answers With RationaleDocument17 paginiREVALIDA EXAM 200 Answers With Rationalexaileenx100% (1)
- Countertransference Hate in The Treatment of Suicidal PatientsDocument9 paginiCountertransference Hate in The Treatment of Suicidal PatientsSigmund GledeÎncă nu există evaluări
- FOCUS Hyperhidrosis and bromhidrosis guideDocument4 paginiFOCUS Hyperhidrosis and bromhidrosis guidePantelis PouliopoulosÎncă nu există evaluări
- UGH Syndrome After Lens Implantation PDFDocument2 paginiUGH Syndrome After Lens Implantation PDFkameliasitorusÎncă nu există evaluări
- Medical Revision PaperDocument106 paginiMedical Revision PaperDavin SugumarÎncă nu există evaluări
- Tooth Mobility PedoDocument47 paginiTooth Mobility PedoFourthMolar.comÎncă nu există evaluări
- Patho Intussusception RevisedDocument8 paginiPatho Intussusception RevisedPj Gabano60% (5)
- Project Appendix Freud's Use of The Concept of Regression, Appendix A To Project For A Scientific PsychologyDocument2 paginiProject Appendix Freud's Use of The Concept of Regression, Appendix A To Project For A Scientific PsychologybrthstÎncă nu există evaluări
- Relational TA - The Therapist Self-DisclosureDocument5 paginiRelational TA - The Therapist Self-DisclosureAdriana NicolaeÎncă nu există evaluări
- Stages of Gross Motor Development from Infancy to Age 12Document17 paginiStages of Gross Motor Development from Infancy to Age 12Gul RockzzÎncă nu există evaluări
- 7 Steps HealDocument17 pagini7 Steps HealAnonymous JkJ4CGwf100% (1)
- CTG classification 2015 FIGO guidelines fetal monitoringDocument1 paginăCTG classification 2015 FIGO guidelines fetal monitoringHerry SasukeÎncă nu există evaluări