Documente Academic
Documente Profesional
Documente Cultură
Mudit Khanna AIPGMEE 2008 Answers 1-99
Încărcat de
Abdullah AbdulRahman100%(1)100% au considerat acest document util (1 vot)
189 vizualizări59 paginiMudit Khanna AIPGMEE 2008 Answers 1-99
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentMudit Khanna AIPGMEE 2008 Answers 1-99
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF sau citiți online pe Scribd
100%(1)100% au considerat acest document util (1 vot)
189 vizualizări59 paginiMudit Khanna AIPGMEE 2008 Answers 1-99
Încărcat de
Abdullah AbdulRahmanMudit Khanna AIPGMEE 2008 Answers 1-99
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF sau citiți online pe Scribd
Sunteți pe pagina 1din 59
AIPGME EXAMINATION
ANSWERS
&
EXPLANATIONS
2008s
(CDM ROLLY Le)
ae ALCL
POT EO Me
eC ane ara eS
Na tA OY OR
constituents of the entire explanatory
text and have high probability of being
CMR NO LeeLee CL
eR CL
ortion of text marked “Q” as prefix
AOS LE
ANATOMY
1
Answer is B (Rectus femoris) : BDC II 64; Gray's 41"/849-853; Cunningham's Textbook of Anatomy (original edition) 671;
Grant's Method of Anatomy (old Edition ~ 1971)/ 353,
Adductor Magnus, Biceps femoris and Pectineus are all examples of composite muscles.
The rectus femoris muscle only forms one part of a composite muscle, the Quadriceps femoris (composite of four
‘muscles) but it has not been mentioned as a composite muscle in isolation,
Rectus femoris is the single best answer of exclusion
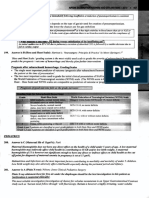
‘Composite Muscles
ae
Composite Individual Muscles ‘Composite Group of Muscles
These include muscles that have different origins (two ‘These include a composite of different individual muscles
heads) and different innervations forthe two heads. that function asa single muscle model
These muscles are also referred to as Hybrid muscles
Examples
© Adductor Magnus? © Quadriceps femoris
+ Biceps Femoris® (This is considered a composite of four individual
© Pectineus® muscles namely the rectus femoris, vastus lateralis ,
* Others all of which work in conjunction ato bring about
extension at the knee joint)
The existance of more than one nerve to a muscle indicates usually that the muscle is composite - Cunningham's
Text-Book of Anatomy (Old edition)
Adductor Magnus (Gray's 39/1467)
“Adduector magnus is a composite muscle and is doubly innervated by the obturator nerve and the tibial division of
sciatic nerve’ - Gray's
Biceps Femoris (Gray's 39/1469)
‘Biceps femoris is innervated by the sciatic nerve; the long head through tibial division and the short head through
the common peroneal division, which reflects the composite derivation from flexor and extensor musculature’
- Grays
Pectineus (BDC II/4*/ 64)
“The Pectineus muscle is of double origin and so it also has a double innervation. Its anterior fibres are supplied
by the femoral nerve and its posterior fibres by the anterior division of the obturator nerve or the acessory
obturator nerve. Such muscles are called Hybrid or composite muscles - BDC
The Pectineus supplied by the femoral and obturator nerves belongs to the composite class - Grants
Rectus femoris has not been mentioned as a composite muscle in isolation
Answer is D (Sternocleidomastoid): Gray's 41"/448-449; Clinically Oriented Anatomy by Moore 5"/32, 263 , Last’s
Anatomy 11/262
Digastric muscles refers to muscles with two bellies. Sternomastoid has two heads but it does not have two bellies and
hence this muscle cannot be termed as a digastric muscle.
Occipitofrontalis (Gray's 39"/ 500, 504)
Occipitofrontalis muscle has two bellies (digastric muscle)
+ Occipital belly of occipitofrontalis and
+ Frontal belly of occipitofrontalis
Omohvotd (Gray's 597538)
Omohyoid consists of two bellies united at an angle by an intermediate tendon
= _ Inferior belly of omohyoid
- Superior belly of omohyoid
204» AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
© Muscle fibres in ligament of Treitz (Gray's 39°/ 1165; Last's Anatomy 11'"/262; Moore 5/263)
Muscle fibres within the ligament of Treitz (Suspensary muscle of duodenum) contain two bellies
= belly (slip) of skeletal muscle fibres and
~ belly (slip) of smooth muscle fibres.
* Sternocleidomastoid: (Gray's 39/536; Moore 5*/ 32)
Sternocleidomastoid has two heads of origin but a single belly and hence it cannot be classified as a digastric
muscle.
Nomenclature of Muscles based on number of heads or bellies (Gray's 39%/114)
‘Number of Heads Number of Bellies
Two Heads : Biceps Two Bellies : Digastric
Three Heads : Triceps The belly is the fleshy contractile part of a
Four Heads : Quadriceps muscle
3. Answer is C (Till Respiratory Bronchioles) : Gray's 41°/968; BDC /6" /277
Bronchial arteries are branches of the descending thoracic aorta, They supply the bronchial wall as for as the
respiratory bronchioles. - Grays
Blood supply to Bronchopulmonary tissue
Samsayeense
Broachislieeastar 7) [Bronchial wee dival to the Rapa Orne eter
asthe Respiratory Broneiole (Alveolar ducts, Ata, Air
Bronchiole saceules,Alveli)
Pulmonary vessels) | Pulmonary vessels alone
and
Bronchial arteries ‘Not supplied by Bronchial Arteries
Purmonary pleura
Bronchial Artery and Arterial supply of Pulmonary tissues
‘© Bronchial Arteries supply nutrition to the bronchial tree and to the pulmonary tissue
‘© These arteries vary in number, size, and origin but arise from the descending thoracic aorta either directly or
indirectly
& Right side Left side TR
‘There is one bronchial artery? ‘These are two bronchial arteries®,
Arises indirectly? from the descending Arise directly? from the descending
thoracic aorta thoracic aorta
Either from:
~ Third Posterior Intercosal Artery, or
+ Upper left bronchial artery
‘+ These bronchial arteries accompany the bronchial tree along with the branches of pulmonary artery.
Each Broncho pulmonary segment receives a branch of the bronchial artery
©The bronchial artery supplies the bronchial tree as far as the respiratory bronchiole
‘Segments distal to Respiratory bronchiole je. alveolar ducts, airia, air saccules or alveoli are supplied By
branches from pulmonary artery and venis. (and not by branches from bronchial arteries) a
Answer is A (Femoral Nerve) : BDC 11/6"/ 91
|AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008 © 205
The skin overlying the region where a cut down is made to grant access to the great saphenous vein is supplied by the
saphenous nerve. The saphenous nerve isa branch of the femoral nerve which is thus the single best answer of
choice.
‘Venous cutdown of Great Saphenous Nerve
* The Great saphenous vein isthe ideal
Jocation® for peripheral venous cut down
because ofits superficial and consistent
position in both adults and children
Itis the most common site® for a cut down
‘+The best location fora cut -down is
approximately one finger breadth anterior
and superior to medial malleolus
* The region around the medial malleous is
supplied by the great saphenous nerve
(Branch of posterior division of Femoral
nerve)
‘© Injury to saphenous nerve (supplied by
Femoral nerve) is a known complication of
venous cut- down
‘Saphenous nerve
Answer is A (Straight tubules — Rete testes -> Efferent tubules) : BDC 11/6/24
The pathway of the sperm from within the testis to the epidydimis proceeds from the seminiferous tubules, to the
straight tubules to the rete testes to the efferent tubules and finally from the efferent tubules to the epidydimis,
‘Seminiferous tubules —> straight tubules —> rete testes —> efferent tubule —» Epidydimis
Structure of testis and pathway of sperm
‘© Sperms are formed in the seminiferous tubules
‘The glandular part of testes contains 200 — 300 lobules.
Each lobule contains highly coiled tubules called
seminiferous tubules. The spermatozoa (sperms) are first
formed in these seminiferous tubules
© — Seminiferous tubules continue into Straight tubules:
At the apices of the lobules the seminiferous tubules from all
lobules join together and form about 20 to 30 straight tubules
‘These tubules enter the mediastinum of the testis
‘© Straight tubules continue into the Rete testes
With the mediastinum of the tests, the straigt tubules
anastomose with each other and form a network of tubules
called the Rete testes
‘+ Rete testes continues into Efferent ductules
Rete testes gives rise to 12 to 30 Efferent ductules which
emerge near the upper pole of testes and join the epidydemis,
‘© Efferent ductules continue into the Epidydemis
Answer is A (Inferior Mesenteric vein): BDC 11/6%/281: Lasts Anatomy 11"/263,
The paraduodenal recess /fossa is present in about 20% of subjects. The inferior mesenteric vein lies in the free edge
of the peritonial fold - BDC
206 © AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
A
| Duodenal Fossae /Revesses =
'* Duodenal fossae are fossae or recesses that are created by folds of peritoneum
‘© These derive their significance by being potential sites of internal hernia that are prone to strangulation
‘© Lies tothe let of the DJ flexure and is orfie looks tothe
right (prevent in about 50%)
‘© The inferior mesentric vein lies In the free edge of the (No significant vascular relations)
peritoneal fold that forms the fossa (anterior wall)
© Significance (present in about 75%)
= An incarcerated hernia in this fossa may obstruct and (No significant vascular relation)
thrombose the vein Retroduodenal fossa
~ There is danger of dividing the vein during surgery for | | This is the largest duodenal recess
(No significant vascular relation)
Mesnterico Parietal Fossa of Waldayer
(present in 1%)
‘The most usual position of this fossa is in
the first part of meso jejunum.
The superior mesenteric vessels lie in the
fold of peritonium forming this fossa
Answer is C (Superior Vesical Artery) : BDC 11/6"/400
The ductus deferens is a thick walled muscular tube which transmits spermatozoa from the epidydimis to the ejaculatory
duct. The ductus deferens recieves its blood supply from the artery to ductus deferens which usually arises from the
superior vesical artery. Occasionally it may arise from the inferior vesical artery. ~ BDC
Internal Iliac Artery
oo)
‘Anterior Division Posterior Division
1. Superior Vesical Artery (Gives rise to artery of 1, SHiolumbar artery
ductus deferens) 2. Lateral sacral artery (2)
2. Obturator artery 3. Superior gluteal artery
3, Middle rectal artery
4, Inferior vesical artery (Replaced by vaginal artery
in females)
5. Inferior gluteal artery
6. Internal pudendal artery
7._Uterine artery (only in females)
‘Superior Vesical Artery and Inferior Vesical Artery are branches of Internal Mac Artery (Anterior Division)
Tn females the inferior vesical artery is
replaced by the vaginal artery and the uterine
an extra branch,
Answer is D (Deep Middle Cerebral Vein) : BDC III /6"/463
Deep Middle cerebral veins drain into the basal veins which drain into the Great cerebral veins that terminate in the
straight sinus. Deep Middle cerebral veins neither form direct incoming channels nor direct draining channels for
the cavernous sinuses. Deep Middle cerebral vein is therefore the single best answer of choice.
[AIPGME EXAMINATION ANSWERS AND EXPLANATIONS ~ 2008 © 207
Cavernous Sinus
Inoming Channels Draining Channels
‘Superior ophthalmic vein® * Superior Petrosal sinus
Inferior ophthalmic vein® (drain into Transverse sinus)
(A branch of this vein) * Inferior petrosal sinus
* Central vein of Retina® (Grain into Internal Jugular vein)
(may drain via superior opthalmic vein) # Emissiary veins®
* Superficial middle cerebral vein (drain into pterygoid plexus of veins)
# Inferior cerebral vein? # Superior ophthalmic vein®
# Sphenoparietal sinus? (Grains into facial vein)
* Middle meningeal vein® ‘© Inter cavernous vein® (sinuses)
(Frontal and Anterior Trunk) (communicate between the left & right
ccavemous sinuses)
Frontal and anterior runkof middle meningeal vein
Deep fcial vain
Side view of the tributaries and communication ofthe cavernous sinu
Answer is A (Develop around 8" week of gestation): Gray's 41"/440; Atlas of Vascular Anatomy by Uflacker 2" /71
The diploic veins develop after birth and not during intrauterine life within the diploe of cranial bones. These appear
‘about the fourth year of life and not around the 8" week of gestation.
iploe and Diploic Veins
© Classic structure of the cranial vault bone in an adult consists of an outer table and inner table of compact bone
with an intervening cancellous portion.
“This intervening cancellous and vascular portion is called the diploe and corresponds to the
cancellous portion of other bones.
‘© The diploe and the tables that are classical in adults, do not develop in intrauterine life and are absent at birth.
At birth the cranial vault is unilaminar (one lamina).
The tables and diploe (intervening cancellous portion) appears about the fourth year (with maximal
differentiation about 35 years)
* Diploic veins are veins present within the cranial vault bones that drain the diploe.
- These veins present no valves®,
- These veins have thin walls and consist only of endothelium surrounded by elastic tissues®
= These veins are of considerable size (large) and present dilatations at regular intervals
- These channel unite and enlarge once sutures are obliterated
= These veins anastomose externally with veins of the pericranium (pericranial veins) and internally with veins
of the meninges (meningeal veins) and sinuses of the dura mater (dural sinuses)
10.
uu.
‘* AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
= The major diploie veins include:
Frontal
Anterior temporal (parietal)
+ Posterior temporal (parietal)
Occipital
+ Numerous small diploic vein tributaries ofthe superior saggital sinus
= These veins are liable to inflammation after head injuries and may give rise to pus in the diploe and pye
(May give rise to visceral abscesses after head injury)
= These veins may be a source of significant bleeding after surgical vault fractures or surgical trephination.
Answer is B (Lacrimal bone): BDC 1/1 /6%/240
The lacrimal bone does not form part of the nasal septum
‘Nasal Septum
‘The Nasal septum is the osseo cartilaginous partition between the two halves of the nasal cavity
The Vomer
‘The perpendicular plate of.
Ethmoid
‘+ Nasal spine of the Frontal
bone
‘© Rostrum and rest of the
Sphenoid
‘* Nasal crest of the Nasal
Bone
+ Nasal crest of Palatine
bone
‘+ Nasal erest of Maxillary
bone
cartilage
Answer is A (Facial Nerve) : BDC III /6"/ 370
Facial nerve does not contain Somatic Efferents
General Somatic Efferents
# Septal process of
the inferior nasal
Incisorerest — Vomer
Me
wall ofthe nasal evity~the nasal septum
‘* Cranial Nerves that supply skeletal muscles of somatic origin contain somatic efferents
‘* These cranial nerves contain Somatic Efferent nuclei that supply these muscles.
‘* Skeletal muscles of somatic origin include the tongue muscles and the muscles that move the eyeball (obliques & Recti)
Cranial Nerves Containing Somatic Efferents:
(Nerves
Hypoglossal Nerve - CN XII
Occulomotor nerve - CN Il
Trochlear nerve - CN IV
Abducent nerve - CN VI
Nuclei
Hypoglossal nucleus
Occulomotor nucleus
Trochlear nucleus
Abducent nucleus
‘Muscles of somatic origin supplied)
Tongue muscles
Medial Rectus, Superior Rectus,
Inferior Rectus, Inferior Oblique
Superior Oblique
Lateral Rectus
2
13.
‘AIPGME EXAMINATION ANSWERS AND EXPLANATIONS ~2008 © 209
Motor functions of skeletal Motor funetions of mucles Motor function of smooth ]
muscles derived from somites | | derrived from branchial arches | | muscles and glands of head and
viscera that receive
Parasympathetic supply
+ + +
Referred to as Referred to as: Referred to as:
‘Cranial Nerves Cranial nerves a
TI (Occulomotor nucleus) V_ (Masticatory nucleus) TH (Edinger westphial nucleus | | 23
IV (Trochear nucleus) VI (Facial nucieus) VII (Superior salivatory nucleus) | |.
‘VI (Abducent nucleus) Ix IX (Inferior salivatory nucleus) 3
XII (Hypoglossal nucleus) x } (Ambiguous nucleus) X (Dorsal motor nucleus) R
x iu
XI (Spinal acessary nucleus) 2
&
=
Eacts to Remember
2CN containing Somatic Efferents or General somatic Efferents (SE/GSE) : CNIIII, IV, V1, XII
°CN containing Bronchial Efferents or Special Visceral Efferents (BE/SVE) CNY, VUl, IX, X, XT
2CN containing General visceral efjerents (GVE /VE) CNII, VIL, IX, X
Answer is B (Pons) : BDC III /6"/390; Neuroanatomy by Handelman (2000)/12
Facial Colticulus is an elevation in the floor of fourth ventricle produced by the abducent nucleus. It lies atthe level
of pons
Nerve nuclei
‘* The lower 10 cranial nerve (CNII to CN XII) arise from Nuclei within the brainstem
‘* The attachment site of each cranial nerve to the brainstem is a marker to the location of the cranial nerve nuclei
within the brainstem (in almost all cases)
* Occulomoor (CN) Trigeminal N (CNY) Glossopharyngeal (CN IX)
® Trochlear (CN IV) Abducent N(CN VD) Vagus (CN X)
# Facial N(CN VI) Acessary (CN XD)
‘© Vestbulacochlear (CN VII) Hypoglossal (CN XID
‘©The first two cranial nerve nuclei are evaginations of the brainstem itself and these two cranial nerves (CN I and
CN ID) do not originate from the brainstem
Answer is C (Mesencephalic nucleus of trigeminal nerve) Grays 41"/255-256; Neuroanatomy (BRS) 4/155 Clinical
Neuroanatomy (longe) 25/113
The reflex arc of Masseteric reflex involves two nuclei of the trigeminal nerve, namely, the mesencephalic nucleus
‘and the motor nucleus of CNV
As Motor nucleus of trigeminal nerve has not been provided in the options, the Mesencephal
best answer of choice
c nucleus is the single
210 © AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
‘The masseteric Reflex: Jaw Jerk
* The mesenteric reflex isa stretch reflex forthe massetor muscle
* Iisa monosynaptic reflex?
+ Gentle percussion with a reflex hammer generates
proprioreceptive impulses inthe first order neurons.
‘+ These proprioreceptive impulses are relayed t0 the
mesencephalic nucleus of CN V which sends excitatory
projections tothe motor nucleus of CN V.
‘© Efferent impulses ae carried from the motor nucleus of CN V to
the masseter muscle and produce the jerk
‘Naleus ofthe aferent lim is the mesencephalic nucleus of CN
Nice of he ele ib tenor mes of CH V8
miss run in the nerve CN VE
. Thpere (Brisk Jaw Jerk) indicates an upper motor neuron
lesion
PHYSIOLOGY
14, Answer is A (Histamine) : Skin Immune System by Bos 3/401, Ganong 22™/625; Chaudhuri 6/249; A Guide to
Allergies by Ramdass 2007 /141; Goodman and Gillman's 11/405; Katzung 25/258
Lewis Triple Response is caused primarily by the liberation of Histamine and other Related peptides.
Axon Reflex contributes only to the ‘Flare’ component of triple response and plays no role in the other two components
namely Red Reaction and Wheal.
Histamine is the single best answer of choice.
According to Lewis in his original description the Triple response was caused by a substance called ‘H substance’
which is identical with histamine or with a compound of Histamine.
Lewis Triple Response
‘Charachteristic three part response that develops when a pointed object is drawn firmly2over the skin
| Red Reaction Flare Response Wheal
| «This manifests inthe form of + This manifests in the form of spreading + This manifests inthe form of
| ared line at the point of redness that extends beyond the original __swelling or localized edema
contact with the skin (stroke) red line and occupies the same areas as
+ Results from transient + Results from stimulation of the Axon the red line
| localized vasodilation due to reflex that causes vasodilatation ‘+ Results from increased
release of histamine and indirectly. capillary permeability due to
related mediators at the point The Axon Reflex may actually be histamine and other related
of contact with the skin stimulated by released histamine along mediators
with other related peptides
Direct vasodilating effect of | { Indirect vasodilatory effect of histamine | | Histamine induced increased ]
histamine by stimulating the Axon Reflex permeabil
15. Answer is D (All of the above) : Ganong 22™ /107; Chaudhuri 6% /318 KDT 6"/ 151, 152, 153
Histamine may be present in the mast cells (mast cell histamine) and in other cells as in the gastric mucosa (non mast
cell histamine). Histamine increases gastric secretions (H; Receptors) and has been related to arousal, sexual
behavior, regulation of secretion of some anterior pituitary hormones, blood pressure, drinking, pain thresholds and in
the sensation of itch - Ganong
‘AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008 © 217
Histamine
‘© Histamine is an amine synthesized locally from amino acid Histidine?
‘Histamine is mainly found within storage granules of mast cells and basophils but it is also found in other tissues
‘Mast cell histamine ‘Mast cells? and Basophils®
Non Mast cell histamine : Gastric mucosa®, Brain
‘© Histamine receptors have been classified into three types — Hi, Hy and Hy,
‘Major Actions of Histainergie 5
Gastric glands Smooth muscles NS (Brain)
# Histamine causes marked inerease + Blood vessels. - dilatation Histamine has been related to
in gastric acid secretion” Histamine causes marked dilatation® — «Arousal
= This direct action on parietal of smal blood vessels * Sexual behavior
cells through 7; receptors? « Visceral smooth muscles -consiriction + Blood pressure
= Thisis a G-protein coupled? ‘Airway (Bronchoconstition) + Drinking
response mediated by Adenylate ‘Uterus + Pain thresholds
cyclase activation? and an Intestinal Sensation of itch
increase in cd
16. Answer is C (Increases gastric acid secretion) : Ganong 22/462
Gastrin decreases gastric acid secretion — Ganong 22™/ 486
‘© Secretin is secreted by ‘S" cells of the a
Secretin is homologous to glucagon® (Secretin — Glucagon family)
14 of the 27 aminoacids in secretin are same as those in glucagon).
Increases the secretion of bicarbonate? by the duct cells of Pancreas and biliary tract
(it causes secretion of a watery and alkaline pancreatic juice®)
(its action on pancreatic duct cells is Mediated via cAMP®)
‘© It augments the action of CCK® in producing pancreatic secretion of digestive enzymes”
© Itdecreases —gastric acid secretion by gastric parietal cells®
«ita the contraction of pyloric sphincter® (along with CCK)
‘© Acid (H+) in the lumen of the duodenum®
* Products of protein digestion® and fatty acids? in the lumen of duodenum
17. Answer is A (Tropomyosin): Ganong 22™/ 69; Chaudhuri 6" 6/486
In resting muscle tropomyosin covers the sites where myosin heads bind to actin — Ganong
Role of Troponin and Tropomvos
‘Tropomyosin a E 5 .
‘Tropomyosin is a long filament like protein ‘Troponin is a complex of three regulatory proteins
Tropomyosin covers the sites where myosin heads bind | | Troponin T: (T for Tropomyosin)
actin Attaches troponin complex to tropomyosin
+ Tropomyosin snot alowed to ove fom his positon in| | troponin Troponin binds he oponin complex to Actin
‘the relaxed muscle because troponin binds both: a
‘tropomyosin and actin concomitantly so that tropomyosin | | ‘Troponin C :(C for Ca"*) This is the calcium binding
remains serewed with actin troponin -
ee
‘Troponin — Tropomvosin complex
‘Together the troponin — tropomyosin complex inhibits the interaction between actin and myosin and
‘constitutes a relavin protein®
Role of Calcium
(Calcium s released fom the sarcoplasmic Reticuli in response tothe ation potential)
‘This calcium binds to toponic ‘and eases a confirmational change i the Troponin -Tropomyosin = Actin uni? such that
tropomyosin now shits poston and myosin ead binding sites of actin Become uncovered
212 © AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
18,
19,
20.
Answer is D (Perleean) : Ganong 22nd68 (fig 3.4): Harrison 17” (2683-2684
Perlecan is a large multidomain proteoglycan found in the Extracellular matrix. It is not a sarcolemmal protein.
Dystrophin, Sarcoglycan and Dystroglycan are all part of a large complex of sarcolemmal proteins and glycoproteins
Sarcolemmal Proteins
‘© Several important proteins and glycoproteins are related to the sarcolemma.
Important Proteins Related to Sarcolemma include
ee
‘Transmembrane Proteins localized to
sarcolemmal proteins the cytoplasmic face of
sarcolemma
1. Dystroglycans (f-dystroglycan) :
2 Sarcoglycans (a, f,v,a,6) 4. Dystrophin
3. Caveolin - 3 2. Dysferlin
4. Integrins (B, a) ae
‘+ These sarcolemmal proteins and glycoproteins form three important complexes
‘Sareolemmal proteins and Glycoproteins complexes
a el
Dystrophin-Dystroglyean — Dysferlin Caveotin complex Integrin complex
Sarcoglycan complex
* Defect in these sarcolemmal proteins and glycoproteins and their complexes results in selected muscular
dystrophies?
Answer is A (Factor XIII) : Ganong 22™/ $43; Harrisons 17" /364
Factor XII is also known as fibrin stabilizing factor. Activated factor XII (XIIla) covalently cross links and stabilizes
the fibrin clot — Harrison
The fibrin is initially a loose mesh of interlacing strands, It is converted into a dense, tight aggregate (Stabilization) by
the formation of covalent cross linkages. This reaction is catalyzed by activated factor XI and requires calcium.
= Harrison
Answer is D (Vascular endothelium is smooth and coated with glycocalyx) :Guyion 11"/ 463
Glycocalyx is an endothelial surface factor which repels clotting factors and platelets, thereby preventing activation
of clotting in the normal vascular system ~ Guyton
i in the normal Vascular System are? (
‘© The smoothness" of the endothelial cell surface
This prevents contact activation of the intrinsi clotting system?
© Layer of Glycocaly on the endothelium
Glycocalyx is a mucopolysacharide adsorbed to the surface of endothelial cells.
Glycocolyx repels clotting factors and platelets and thereby prevents activation of clotting.
© Throml {ulin on the endothelial membrane
‘Thrombomodulin is a protein bound with the endothelial membrane that binds thrombin
Binding of thrombin with thrombomodulin prevents clotting by
~ removing thrombin
= activating a plasma protein (Protein C) that acts as an anticoagulant by inactivating factor V and VIUL
a.
2.
‘AIPGME EXAMINATION ANSWERS AND EXPLANATIONS ~ 2008 © 213
Answer is B (Is higher than intraarterial pressure): Ganong 22™/ 590, Medicine for Anaesthetists 4"/ 285
Screening for Diseases by Snow (2004) /135]
Blood pressure measured by Sphygmomanometer with a standard cuff tend to overestimate ‘true’ arterial pressures
as measured by arterial cannulation, especialy in the elderly and the obese ~ Ganong.
Bl ssure Measurement with nometers
‘* Sphygmomanometer isa device that measures blood pressures indirectly.
‘External pressure is applied with a sphygmomanometer cuff to the overlying tissues and the
required to occlude the artery is assumed to be equal to the intra arterial pressure.
‘The sphygmomanometer will give accurate readings only if no pressure (zero mm. of mercury) is dissipated in
compressing the soft tissues overlying the artery.
However in practice, some pressure is always dissipated in compressing the blanket of soft tissues overlying the
artery and hence blood pressure measured by the sphygmomanometer are slightly higher than true intra arterial
Pressures.
«The amount by which the sphygmomanometer overestimates the true blood pressure is influenced by the amount of
overlying fat and the compressibility of the vessles.
[Overlying Soft tissue Blanket | [ Compressiblity of vessels Size of Cuff.
f= Thick overlying soft tissue | J» Vessels that are difficultto | |» Small (Narrow) cuff? leads to falsely
blanket leads to ‘compress lead to high blood pressure recordings
overestimation of blood ‘overestimation of blood (overestimation)
pressure pressure Large (wide) cuff leads to falsely lower
|» Obese individuals? havea | |» Elderly individuals® and blood pressure recordings
thick blanket of fat which Diabetics may have rigid (under estimation)
dissibates cuff pressure. sclerotic vessels that are + If the standard arm cuffs used to
Hence Blood pressure is difficult to compress. Blood measure blood pressure in the thigh
likely to be overestimated pressure measured in such falsely high blood pressure values will
when measured by individuals with be obtained (due to relatively smaller
sphygmomanometer and a sphygmomanometer will cuff size and greater soft tissue blanket).
standard cuff. result in over estimation of | |. [fthe standard arm cuffs used on the |
blood pressure forearm falsely lower blood pressure. |
(Pseudohypertension) values may be recorded. |
Note
‘More accurate pressure can be recorded in obese individuals by using a wider cuff size®
© More accurate pressure can be recorded in the thigh by using a wider cuff size®
Answer is D (During Exercise Systole is shortened more than diastole) : Ganong 22™ /566, 603; Chaudhuri
6°/191,202; KDT 6/478
During exercise the diastole is shortened more than the systole
‘The duration of systole is much more fixed than the duration of diastole, and when the heart rate is increased
(exercise) diastole is shortened to a much greater degree’ - Ganong 22/566
ic stimulation (Noradrenaline)
74
23.
24.
‘© AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008,
Control of Heart by
thetic (Noradrenaline) and
asympathetic (vagus) nerv
Force of cardiac contraction Decreased Increased
(norropic effec (mainly atria, litle effect on ventricle)
Conductivity Decreased Enhanced a
Rate of cardiae contraction Decreased (Bradyeardia) Increased (Tachycardia)
Vagal Parasympatheti) fibres are distebuted mai and not much tothe ventricles. Thus the major effect of vagal stimulation is to
dsereass the hear rate o ate of eadiae contraction (bradycardia). Negave inotropic effect of vagal stimaation i ess pronounced.
‘Sompatheic bres ars distipted to both he atria andthe ventricles. Thus Sympathetic stimulation has a strong eect on both, the heart rate
andthe force of era contraction,
© Complete de df i erease in the resting heart rate.
Efi Densreton fh hark (Ganong 27°60. Chart 9717-202
Node Inirinsie Rhythmic
“The normal heart rate at rest in young persons is about 70/minute (Range thmiciy
peoween 30- 100/min) ‘Sinuatrial node (SAN) 100/min'
Atrio Ventricular node O/min®
‘© The sinuatrial node (SAN) is the normal pacemaker of the heart and MaPenenaint 3. tolan?
generates a rhythm of about 100éminute
‘The normal heart rate of about 70/min in a young adult is maintained as a result of autonomic influences on the SAN
‘When both vagal & sympathetic nerves are removed (denervated hear), the sinuatrial node becomes fre from all
autonomic (sympathetic & parasympathetic) influences and starts generating its normal rhythm of about 100/min
+ As the normal resting heart rate is usualy less, about 70/min, complete denervation of the heart would cause an
increases inthe heart rate from 7W/nin to 100/min.
‘+ During exercise the diastole is shortened more than systole.
Changes in Duration of Systole and Diastole, when heart rate is increased (Exercise),
+ Exercise is associated with an increase in the heart rate
+ Cardiac muscle has the unique property of contracting and repolarizing faster when the heart rate is high
‘+ This leads to a decrease in duration of both systole and diastole
“However the duration of systole is much more fixed than that of diastolic and when the heart rate is
increased (eg. exercise) diastole is shortened to a much greater degree” - Ganong
‘+ This longer duration of diastole enables :
‘Superior coronary blood flow to the cardiac musculature?
Superior ventricular filling?
Answer is B (Temperature lower than core body temperature): Ganong 22/427
Spermatogenesis requires a temperature considerably lower than that of the interior of the body — Ganong
‘© Spermatogenesis requires a temperature lower than the core body temperature
Tesies are normally maintained at a temperature of about 32°C. This lower temperature is maintained by:
- air circulating around the testes
~ heat exchange in a counter current fashion between spermatic arteries and veins
+ Factor which raise scrotal temperature® can impair’ is and lead to infertilit
‘These include:
- Ectopic or undescended testes (intraabdominal)?
- Wearing of tight scrotal support®
~ Presence of varicocele®
~ Occupations involving exposure to excessive heat, such as men working in blast furnaces
Answer is C (The tubes are lined by ciliated epithelium) Guyton 11/1028, 1029; Dutta 6/7, Williams Obstetrics
22/27; Shaw's Gynaecology 14"/ 177, 178.
The fallopian tubes are lined by.
ted epithelium.
+ ‘The fallopian tubes are lined by ciliated columnar epithelium.
‘The fallopian tubes are lined by a single layer of columnar cells. Some of them are ciliated and others are secretory.
The ciliated cells are most abundant at the fimbriated extremity, elsewhere they are found in discrete patches
Williams 22/27
25.
‘AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008 © 215
© Thecilia always beat towards the uterus ~ (Guyton)
The transport of fertilized ovum through the fallopian tube into the cavity of uterus is effected by:
1. A feeble fluid current in the tube resulting from epethelial secretion and the action of tubal cilia. The cilia
‘always beat towards the uterus, such that the direction of flow is towards the uterine cavity-Guyton, Williams
2. Tubal persistalss, resulting from rhythmic contractions of the tubal musculature
‘© Eertilization of ovum occurs in the fallopian tubes,
and not in the uterus (Guyton)
Fertilization must occur within a few hours, and no
‘more than 24 hours® after ovulation
‘+ Implantation of the fertilized ovum occurs
between 5-7 days af t afte
2A hours) (Guyton)
‘After fertilization has occurred, an additional 3-5
days is normally required for transport of the
fertilized ovum through the fallopian tube into the
cavity of uterus
Implantation occurs at the stage of ‘blastocyst’?
Answer is D > A (Massage of foot > Increased with change from supine to standing position) : Guyton 11'%/192;
Ganong 22"/ 593, Concepts in Medical Physiology by Seifier (2005)/ 163, 164
Any external factor that causes intermittent compression of lymph vessels (Massage of foot) causes pumping of the
lymphatics and improves (increases) the rate of lymph flow.
Factors that increase interstitial fluid pressure (change from supine to standing position) also increase the rate of
Lymph flow if lymph vessels are functioning normally.
Thus both, option A and option D are correct statements. However prolonged standing tends to worsen lymphoedema
‘and hence if we have to pick one single correct answer from amongst the options provided, massage of the foot would
probably be the single best answer of choice.
Fluid efflux from tissues exceeds the fluid influx across tissue capillaries and
constitutes the Intertial fluid
Lymph is derived from this interstitial fluid and is returned back to the central
circulation (subclavian vein) through iymphatic vessels.
+
Factors Controlling Rate of Lymph Flow
Interstitial Fluid Pressure Lymphatic Pump Suction forces ‘Other Factors
‘Any factor that increases interstitial fluid ‘Any factor that causes intermitten | |e Intrins
pressure also inereases Iymph flow compression of lymph vessels causes contractility of
pumping of lymphatics and Lymphatic
Lymph Flow is thus increased by: improves the rate of ymph flow capillaries
+ Ted capillary hydrostatic pressure increases rate of
+ Led plasma colloid osmotic pressure | | Lvsmph slow is thus inreased by. lymph flow
+ Ted interstitial fluid colloid osmotic | |* Active striated muscle a.
— ‘+ Movement of parts of the body nervous system
+ Ped permeability of capillaries ‘© Pulsation of arteries adjacent to stimulation
Deep vein valve incompetence increases the lymphatics through the action
‘venous stasis and impairs the ability of + Compression of tissues by of catecholamines
venous end of capillaries to reabsorb objects outside the body on aand
fluid. Tis increases the amount of (massage of foot) adrenergic
interstitial fluid and enhances the rate of | | « Rhythmic changes of intra receptors
Iymph flow abdominal and intra thoracie increases rate of
(Edema results once volume of fluid pressure caused by respiration ene q
exceeds the capacity of the lymphatics) (suction forces) ym! |
216
‘© AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
Standing from supine position: Effect on Lymph formation and flow
‘When an individual goes from a supine to standing position water and filtrable substances move from the intravascular
space to the interstitial compartment thereby raising the interstitial fluid pressure,
“Any factor that increases interstitial fluid pressure also increases lymph flow ~ Guyton 1792 1
This should therefore also enhance or increase the rate of lymph flow
When a person stands up from a recumbent position, the amount of lymph production per unit of time may increase upto 40% in
the area ofsyprafascial lymph vessel ofthe lower leg ~ old's Textbook of Lymphology (2007) /199
26. Answer is A (Does not change) : Ganong 22" /634
Cerebral blood flow is maintained at constant levels (does not change) in response to moderate exercise
‘Changes in Blood Flow in Response to moderate exercise (Isotonic)
Cd
creased Decreased ‘Maintained (No change)
© Active Skeletal ‘© Inactive Skeletal Muscle ‘© Brain (cerebral)
Muscles © Kidney © Skin (cutaneous)
© Liver
Gastrointesinal tract
Other Organ systems
27. Answer is A (Fine Touch) : Ganong 22” /138; Guyton 11/588
Fine touch is transmitied through the Dorsal /Posterior column
. ons requiing fine gradients of intensity /high degre of loalizaion
‘+ Fine Pressure (Fine degrees of judgement of pressure intensity)
© Vibration
Joint Position Sense
‘SGisations Transmitied by Anterolateral Column /Spinothalamic Tract” NaN
© Oude Touck®
* Crude pressure?
© Pain (Pin Prick)?
¢ Temperature? __
“Anterior” Spinothalamic Tract (Ventral) | [Lateral Spinothalamie Tract
Crude Touch® Pain (Pin Prick)®
Crude Pressure? Temperature?
BIOCHEMISTRY
28, Answer is D (HMP Pathway) : Harper 27" /177, 189 Lippincott's 4" / 104, 113, 192
‘The pentose phosphat pathway or hexose monophosphate shunt (HMP) is an alternate route for the metabolism of
glucose, other than glycolysis. It does not lead to formation of ATP - Harper 278/177
No ATP is directly consumed or prduced in the hexose monophosphate shunt (HMP) ~ Lippincott's 4/145
‘AIPGME EXAMINATION ANSWERS AND EXPLANATIONS -2008 © 217
‘ATP Generation from important Metbolie cycles
Glycolysis Tricarboxylic Acid Cycle Fatty acid oxidation
(ca)
Oxidation of fatty acids produces a large
eecinea para 12 molecules of ATP per quantity of ATP — Harper
bau hycolye molecule of Acetyl CoA —_(The net energy yield from oxidation of one
2moleculesof 8 molecules of molecule of palmitate is 129 ATP —Lippincott)
ATP foreach ATP for each
molecule of molecule of
glucose glucose
29, Answer is B (Muscle) : Harper 27" /142; Chatterjee 7/328; Lippincott 4"/128, 129, 130
Muscle glycogen cannot contribute directly to plasma glucose since muscle lacks glucose 6-phosphatase — Harper
Glycogenolysis in Liver and Musel
* Breakdown of glycogen into glucose is called glycogenolysis
‘© When glycogen is degraded the primary product is glucose 1- phosphate®, obtained by breaking a (1-4) glycosidic
bonds?
‘© This reaction is catalyzed by enzyme ‘phosphorylase’ (Rate limiting and key enzyme in glycogenolysis®)
Glycogen phosphorylase
(Present in both Muscle and Liver)
Phosphoglucomutase
(Present in both Liver and Muscle)
(Glucose 6 =F)
Further
=o 00]
‘InLiver (and kidney) a specific enzyme glucose 6— In Muscle, enzyme glucose 6- phosphatase is absent
Phos is present ; ‘
Free glucose can therefore not form in muscle directly and
This enzyme removes the phosphate (PO, from vi
Meee cnabtng te oonaten offrelucse, —Hetee Glycogenolysis in muscle does nt contribue directly to
This free glucose is free to diffuse from the hepatic load glucose,
cells to extracellular spaces including blood. This glucose 6- P can enter the glycolytic cycle and form
Gtycogenolysis in Liver thus contributes directly to pyruvate and lactic acid, Indirectly, lactic acid may go to
blood glucose glucose formation in the liver
30. Answer is D (Insulin) : Harper 27" /161, 162, 163 Chatterjea 6"/326, 327
Insulin inhibits the activation of phosphorylase b. It does this by increasing the uptake of glucose, leading t0
increased formation of glucose 6- Phosphate, which is an inhibitor of phosphorylase kinase — Harper
Factors maintaining phosphorylase ints active form | [Factors maintaining phosphorylase in its inactive form
(phosphorylase a) (phosphorylase b) 2
* cAMP © Insulin
© Calcium © Protein phosphatase
+ ATP + Glucose 6 phosphate
218 © AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
Phosphorvlase enzyme and its regulation
‘* Phosphorylase is the most important and rate limiting enzyme of glycogenolysis®
* Phosphorylase enzyme is found in two forms, active (phosphorylase a ) and inactive (phosphorylase b).
‘Active phosphorylase (phosphorylated form) : Phosphorylase a
Inactive phosphorylase (dephosphorylated form) : Phosphorylase b
‘© The active form of phosphorylase (phosphorylase a) catalyses the following reaction
Glyeogen +, Glycogen, + Glucose 1-P
‘The inactive form of phosphorylase (phosphorylase b) is activated into the active form (phosphorylase a) by a
CAMP / calcium dependent enzyme ~ phosphoryl kinase (a) (active) as depicted in the following flow chart.
+ Novepinepine
Epinephrine
° * Glucagon TeAMP
Thyroid hormone:
CAMP dependent
Protein Kinase Calcium
ADP Phosphorylase a
@ C) (active) 1,0
o ® Protein
Phosphoryl kinase (b) Phosphoryl kinase (a) Je G6P<*—[Insutin} ¥ phosphatase
(inactive) (Active)
arp] ADP p
Phosphorylase b ‘
ATP ‘Anactive)
1. CAMP and hormones that increase cyclic AMP
‘concentrations ie... Epinephrine , Norepinephrine
Glucagon, Thyroid hormones
‘These activate cyclic AMP dependent protein kinase
‘which intur activates phosphoryl kinase and
subsequently converts phosphorylase b to active
phosphorylase a
2° Calcium
Calcium activates the caleium dependent unit (g
subunit) of phosphoryl kinase and subsequently
converts phosphorylase b to active phosphorylase a
3. ATP
ATP donates the "Pi for required for phosphorylation
‘of phosphorylkinase b and phosphorylase b into their
respective active (a) forms
2. Protein
1. Glucose 6 phosphate
Glucose 6 phosphate is an inhibitor of phosphorylase
kinase
rosphatase
Protein phosphatase converts active phosphorylase (2)
into inactive phosphorylase (b) by dephosphorylation
(removing iP). It also dephosphorylates active
phosphoryikinase (a) to inactive phosphoryl kinase (b)
3. Insuli
Insulin inhibits activation of phosphorylse b. It does
this by increasing uptake of glucose leading to
increased formation of glucose 6 phosphate which is
an inhibitor of phosphorylkinase
Insulin also increases Protein Phosphatase activity
Answer is D (Chaperones) : Harper 27" / 515, 516, 517, Ganong 22™ /25, 297, Chattarjee 7"/251
Chaperones an proteins that play a role in proper folding of other proteins without themselves being components of
‘the latter - Harper
‘Chaperones:
CChaperones are proteins that play a role in the assembly and proper folding of synthesized proteins so that the latter
proteins gain biological activity
These proteins enable proper folding of other proteins without themselves being components of the latter®
32.
33.
|AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008 © 219
haperon proteins _
Present in a wide range of species from bacteria to humans, ‘BP (immunoglobulin binding protein)
Many are so-called heat shock proteins (HSP) GRP94 (glucose — regulated protein)
Some are inducible by conditions that cause unfolding of newly
synthesized proteins (eg. clevated temperature and various
chemicals)
They bind to predominantly hydrophobic regions of unfolded
Calnerin
Calreticutin
and ageregated proteins.
They actin part as a quality control or editing mechanism for
detecting misfolded or otherwise defective proteins
Most chaperones show associated ATPase activity, with ATP or
ADP being involved in the protein-chaperone interaction
Found in various cellular compartments such as cytosol,
mitochondria, and the lumen ofthe endoplasmic reticulum.
Proteosomes (Ubiquitin ~ Proteosome pathway) or Endoplasmic Reticulum Associated Degeneration (ERAD)
'* Proteosomes® are organelles involved in degradation of misfolded proteins and regulatary enzymes that have short
half lives
‘© — Ubiquitin® is a small, highly conserved protein that plays a key role in marking various proteins for furthur
degradation in proteosomes (Ubiquitin tags proteins for degradation)
‘© Prior to entering proteosomes most proteins are ubiquinated and are escorted to proteosomes by polyubiqutin —
binding proteins
| Pathways for Protein degeneration
in Eukaryotes
[Protein degradation in Lysosomes (Protein degradation in proteosomes
‘* Involves Lysosomal proteases * Invoves by Ubiquitin ~ Proteosome pathway
'* This process does not require ATP? ‘+ This process requires ATP (ATP dependent)?
Proteases:
Proteases are enzymes that catalyse the hydrolysis of proteins into their component amino acids (Harper 27/7)
‘Templates:
‘Template is a strand of DNA which is copied during RNA synthesis. In the double stranded DNA molecule, the genetic
information resides in the sequence of nucleotides on one strand called the template strand (Harper 274/312)
Answer is A (Golgi bodies): Harper 27" /506, 518
The Golgi apparatus is involved in glycosylation and sorting of proteins — Harper 27%/518
‘Many studies have shown that the Golgi apparatus plays a major role in sorting of proteins for their correct
destinations — Harper 277506
‘The rough endoplasmic reticulum branch of protein storing.
‘+ Newly synthesized proteins are inserted into the ER membrane or lumen from membrane-bound polyribosomes.
+ Proteins then pass through the various subcompartments of the Golgi until they reach the Trans - Golgi Network
(TGN), the exit side of Golgi.
+ Inthe TGN, proteins are sorted and seggregated.
Answer is C (Enterokinase) : Chatterjee 7"/435; Harper 279/597
Enterokinase is a glycoprotein enzyme that activates trypsin
220 © AIPGMEEXAMINATION ANSWERS AND EXPLANATIONS - 2008
oe
3
Trypsin
Trypsin isa proteolytic enzyme (proteinase) involved in the digestion of proteins
‘Activators of Trypsin Tnhibitors of trypsin
Enterokinase” © Alpha Antiproteinase or Alpha-l Antritrypsin®
Caleium® * Di isopropy! fluro phosphate (DFP)
Trypsin itself” © Egg white?
(Egg white contains water soluble mucoprotein which
Trypsin acts nan alka is a potent inhibitor of trypsin)
‘medium ‘+ Human and bovine colostrum
‘+ Raw soyabeans
Alpha Antiproteinase is Synonymous with a, Antitrypsin
Itis synthesized by hepatocytes and macrophages and is the principal inhibitor of serine proteases in human plasma
inhibits trypsin, elastase and certain other proteases by forming complexes with them.
Answer is C (Apoprotein CII inhi Harper 27 / 217, 218 Chaterjee 6/383;
Apoprotein CII acts as an activator of lipoprotein lipase. It is required as a cofactor for lipoprotein lipase activity
its lipoprotein lipase):
Li
jrotenemia)
‘+ Lipoprotein Lipase is n extracellular enzyme attached
to the capillary endothelium of most tissue (Adult
Liver does not have this enzyme”) by heparan
sulphate
‘Lipoprotein Lipase activated by Apo C Il (and Apo C
1) on circulating lipoprotein particles hydrolyzes the
triacyl glycerol contained in these particles to yield
fatty acids and glycerol
+ Patients with a deficiency of Li
Apoprotein C II show a dramatic accumulation of
chylomicrons in the plasma
(bypertriacylglycerolemia)
= Type Hyperlipoprotenemia or familial
lipoprotein lipase deficiency
‘What ipoproteins / Apoproteins : Review
‘Apoproteins / Apotipoproteins are the protein moieties of Lipoprotiens.
The plasma lipoproteins are spherical macromolecular complexes of lipids and specific proteins called apoproteins
Functions of Apolipoproteins ®
+ Lipoprotein Lipase activators: ‘Apo ~ CH (Most important) and Apo — CI
+ Lipoprotein Lipase inhibitors : Apo Cll, Apo A It
+ Lecithin - Cholesterol Aeyl Transferase (CAT) Activators: Apo ~ Al
+ LDL Receptors? ~ Apo B100, ApoE
+ HDL Receptor® + Apo AI
© Remnant Receptor? = ApoE
(LDL Receptor related protein)
Form part of the structure of lipoproteins
B Apoprotin B Structural protein for ehylomlront VLDIs IDls LDL.
= Apoprotein A -1 :_ Structural protein for HDL SD ili Eli
35.
‘AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008 © 221
Defect in biosynthesis / secretion of Apoppoprotein B results in Abetalipoproteinemia and Homozygous
‘Hypobetalipoprotonemia i.e. absence of chylomicrons, VLDL, IDL and LDL (Malabsorption & Neurological defects)
Defect in biosyntsis ‘secretion of Apolipoprotein AL results in virtual absence of plasma HDL. and premature heart disease?
Answer is C (II) : Harrisons 17"/ 2419
Type III hyper lipoprotenemia (Familial Dysbetalipoprotenemia or familial broad fi disease) is characterized by
mixed hyperlipidemia due to accumulation of ‘remnant’ lipoprotein porticles of VLDL and chylomicrons.
~ Harrisons 17/2419
Apoprotein E present on chylomicron and VLDL
remnants is required for their removal via hepatic
lipoprotein receptors. Type III hyper
lipoprotenemia results from a defect in
Apoprotein E as a result of which VLDL and
chylomicron remnants are not removed
‘adequately and accumulate in the circulation
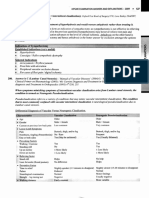
Frederickson Classification of Hyperlipoproteinemias
Laboratory Features
(Borin vst Chyomisons LDL LDeand VBL” Chyloicrons VLDL Chylomirons
B end VEDL fd VIDE
i remnants
Tigers tote - ” wore + a
Choteser tos pg HO Ra Sa HHT
LDL-cholesterol + + + + + +
WDLetoleserol +++ + w ¥ + a
Plammmperece Lakota Clee Tubid ——Tubid——_Lactescent
Clinica ears
Xantbomss ewe Tendon, bes None Palmar, None Epi
bevenptve
Pancreas He o o ° ° os
Coronary ° oe ve ” “
erasers
espe! o ‘ + * *% a
tetra
Molecular ict & Genetic nomenlare
Moker defects LPLandpo-C-ll LD Leer ApoB-10, Unknown Apel AOA and. ApoA-V and
PCSKO, ARH, ABCOS a Chino Unknown
BCG
Gensticnomeciate FCS FH, FDB,ADH,ARH,——FCHL fa ATG TG
Sloeolenia
+ FCS (lami cylomicranemiasadrome) + FDB Gala defective apoB)
{FH Gail ypercholeserotemia) {ARI (atosomalrecesvehypercholesterlemia)
© ADH (atasomel dominant hypercholestrolemia) + ECHL Gala combined hyperpidemta)
© FDBL familial dsbetalpopretenemia) { FHTG Gamal perrighceridemi).
© LPL Aipoproten lipase «Apo apolipoproten)
‘222 © AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
36.
Answer is A (ds DNA) : Harper 27" /335, 336, 337 Lippincow 4/406
Okazaki fragments are short segments of DNA synthesized on the lagging strand, during the process of replication of
a double stranded DNA (dsDNA)
lication of jed DNA
Helicase ‘The process of replication of double stranded DNA requires the ds
‘Unwinds ds DNA to provide ss DNA DNA to unwind into single stranded DNA (ssDNA) template as
a replication can occur only from a single stranded DNA template
(ssDNA template isa step inthe process of replication of dsDNA)
Relieves torsional stain that results from helicase mae
induced unwinding
Formation of replication fork
and identification of two strands Single spond binding
(leading strand /lagging strand) proteins’
Prevent premature rannealing
Initiation of DNA synthesis ofds DNA
fo) aR Lagging Stand
primase? # RNA Primer is RNA primer in synthesized to prime
Initiates synthesized to prime synthesis of new DNA
syntheses of synthesis of new DNA
new RNA J
primer ‘*DNA is then synthesized « DNA is then synthesized in multiple short
continuously in $'-3" fragments ~ Okazaki fragments in S'-3"
direction by DNA direction by DNA polymerase I?
polymerase II?
Ueyuesting ‘© RNA primer is then excized by DNA
DNA only in polymerase I
se ‘© DNA gap between Okazaki fragments is
direction? filled by DNA polymerase [°
‘* Remaining nicks are sealed by DNA ligase!
Removal of RNA primer and filling of the resulting “gaps” by DNA polymesare I
37.
38.
AIPGME EXAMINATION ANSWERS AND EXPLANATIONS ~ 2008 * 223
Answer is A (Folic Acid) : Harper 27" /490, 496 ~ Lippincott’s 4/373
Folic acid isa water soluble vitamin.
Nine vitamins (Folic acid, cobalamine, ascorbic acid, pyridoxine, thiamine, niacin, riboflavin, biotin and
pantothenic acid) are classified as water soluble, whereas four vitamins (Vitamin A, D, E and K) are termed fat
soluble-Lippincott 4/373
Classification of Vitamins:
+ Vitamin A (retinol, B-carotene)
as + Vitamin D (cholecalciferol)
+ Vitamin K (phylloquinones, menaquinones)
Ascorbic acd (vitamin C) + Vitamin E (tocopherols)
a ato Pro Other See
‘Thiamine (vitamin B,) * Folicacid —» Pyridoxine (vitamin B6)
«+ Riboflavin (vitamin B,) ¢ Vitamin By
+ Niacin (vitamin B,)
+ Biotin
+ Pantothenic acid
Answer is D (Vitamin k) : Harper 27"/495 Lippincott 4%/389
The principle role of vitamin K is in the post translational modification of various blood clotting factors, in which it
serves as a coenzyme in the carboxylation of certain glutamic acid residues present in these proteins ~ Lippincott
Role of vita blood coagulation
‘© Vitamin k is required in the hepatic synthesis of prothrombin and blood clotting factors Il, VII, IX and X®
‘These proteins are initially synthesized as inactive precursor molecules
The activation of these molecules requires carboxylation of their glutamic acid residues
Vitamin K acts as a coenzyme during this carboxylation reaction”
COs,
Precursors of clotting factors \ Carboxylase
1H, VIL, 1X, ‘Mature clotting factors Il, VII, IX, X
(Inactive Glutamyl residues) Vitamin K (Active y-carboxy-glutamyl Gla residues)
of _iyiroxyquinone)
This reaction requires 0,00, and the hyroxyquinone form of vitamin K?
This carboxylation reaction is sensitive to inhibition by dicumarot® and warfarin?
Dicumarol isa natural analog of vitamin K
Warfarin isa synthetic analog of vitamin K
* The carboxylated glutamyl residues (Gla) on mature clotting factors confer on them the capacity to bind Ca”* and
to get bound to phospholipid surfaces.
These properties enable participation of mature clotting factors in the coagulation cascade
‘© Vitamin K is the only fat soluble
vitamin® that functions as a coenzyme? (Lippincott)
Vitamin K exists in three forms = Vitamin K,, Kp and Ky
Vitamin Ky Phylioquinoney: Normal derry source found n green vegetables
Vitamin K; (Menaquinone) : This form is synthesized by intestinal bacteria®
Vitumin K; (Menadione) : These ae synthetic compounds? that canbe metabolized vitamin K (phylloguinones)®
‘224 © AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
39.
40.
© Funct : :
Role in blood Role in synthesis of Role in Oxidative
‘ongsaton atu ining protein Pisepherieon
Vitamin K is | | Vitamin K is required for synthesis of two proteins present | | Vitamin K is necessary co-
required in in bone; factor in oxidative
hepatic synthesis ||- Osteocalcin phosphorvlation® being
ofprothrombin | |_ Bone matrix Gla protein. associated with mitochondrial
jand blood Treatment of pregnant women with Warfarin is known to lipids
cloning, Jacior ‘cause fetal bone abnormalities (fetal warfarin syndrome).
1, Vi, IX and X°) | This may be explained by deficiency of vitamin K secondary | | Dicumarol2, an antagonist of
to warfarin use, which inturn leads to bone abnormalities | | vitamin kis known to act as
due to defective synthesis of bone calcium binding proteins. | |@n uncoupler of oxidative
phosphorylation
Answer is A (lonised): Chatterjea 7" /875, Harrisons 17" /286
Ionized calcium isthe physiologically active form of calcium ~ Chatterjea 7/875
Total Calcium
eed
Tonized calcium Protein bound calcium
(Ditfusible calcium) (Non diffusible calcium)
+ About 50% of total calcium is ionized ‘+ Remaining 50% of total calcium is bound, mainly to
* Ionized calcium is the physiologically albumin,
active form of calcium + Protein bound calcium is not physiologically active
Facts to Remember®:
Normal level of plasma calcium is 9 ~ 11 mg/dl
The frst step in diagnostic evaluation of hyper or hypocalcemia is to ensure that the alteration in serum calcium
level is not due to abnormal albumin concentration’
‘When serum albumin concentration is reduced, the concentration of ionized, free or active calcium is increased and
hence serum calcium values need to be ‘corrected’
‘Corrected’ calcium level calculations require measurement of total calcium and albumin and subsequent
application of a mathematical correction.
Corrected calclum concentration is calculated by adding 0.8 mg/dl (0.2mM) to the total
‘calcium level for every decrement in serum albumin of 1.0 g/dl, below the reference value of
4.1g/dl of albumin, and conversely for elevation in serum albumin® - Harrison
Answer is C (Simple Diffusion) : Harper 27"/424, 108, 433, Ganong 22™/31
Absence of charge over molecules (Uncharged / Neutral molecules) favours their transport by simple diffusion.
‘Small neutral molecules are usually transported freely across
plasma membranes by simple diffusion.
Diffusion is the single best answer amongst the options provided.
‘Transport of Neutral / Uncharged Molecules
‘Small Neutral (Uncharged) Molecules Large Neutral (Uncharged) Molecules
© Free Diffusion ‘© Channel Proteins (Simple diffusion)
(Simple Diffusion) ‘© Carrier Proteins (Facilitated diffusion or Active transport)
‘Some selected small uncharged molecules may be transported through channels or pores
‘AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008 #225
[actors Favouring Transport of Molecules via Simple Diffusion
Charge 2 Absence of charge (Neutrality) favours transport by Simple diffusion
© Size Small size favours transport by Simpe diffusion
‘© Polarity Absence of polarity (Non Polar nature) favours transport by Simple diffusion
© Hydrophobicity Lipid solubiliy/Hydrophobicity favours transport by Simple diffusion
(Lipid Solubitiy)
PATHOLOGY
41, Answer is B (NADPH Oxidase) : Robbins 9" /47-48
Oxygen dependent killing is largely mediated through Reactive Oxygen Intermediates (ROD).
The generation of reactive oxygen intermediates is due to the rapid activation of an oxidase,
NADPH oxidase ~ Robbins
Catalase, superoxide dismutase and Glutathione peroxidase are radical scavenging enzymes that prevent oxygen
‘mediated injury.
nD killing of infectious agents and necrotic cells crronsou
ing i gue ome
+ Oxygen dependent killing is largely mediated through the generation of ie od
Reactive oxygen intermediates® —
‘+ The most important enzyme involved in generation of reactive oxygen won ta ec,
intermediates is NADPH oxidase. <=
+ NADPH oxidase leads directly to the generation of superoxide anion and a 7 |
indirectly to the generation of Hydrogen peroxide (H, O;), Hydroxylation tora fe
(OH) and hypochlorite (HOCI), with the help of Myeloperoxidase enzyme oa oA
‘within azurophilic granules of neutrophills. Sa
Radical generating Reactive oxygen we Radical scavenging enzymes
enzymes intermediates (Protective)
‘NADPH oxidase (Most ‘Superoxide anion (>) Catalase
important) Hydrogen per oxide (H:0:) ' Superoxide dismutase
Xanthine oxidase (In some cells) Hydroxyl radical (OH) Glutathione peroxidase
[NADPH + Myeloperoxidase Hypochlorite (HOCI)
Hydrogen peroxide - Myeloperoxidase — Halide system: Most efficient bactericidal system
+ The most efficient bacterecidal system mediating oxygen dependent killing is HO;~ MPO Halide system in
neutrophils?
© This system requires NADPH oxidase, Myeloperoxidase and halide ions®
= NADPH oxidase system generates H;0>
= Mycloperoxidase within azurophilic granules of phagocytes in presence of halide & ions converts H3O3 into
HOC.
= HOC is the potent antimicrobial agent that destroys microbes by halogenation and for oxidation -
42. Answer is D (Direct effect of injuring agent): Robbins 9 /74; Pathology by Holliman 4/22
Delayed prolonged leakage is believed to be caused either by the direct effect of injurious agent or by cytokine
‘mediated endothelial retraction.
Itis not casued by cytokine mediated vasodilatation and cytokine mediated endothelial retraction is not provided in
the options. Direct effect of injuring agent is therefore the single best answer of choice
“The mechanism of delayed prolonged leakage is unclear. It may result from the direct effect of injurious agent leading
10 delayed endothelial cell damage (perhaps by apoptosis) or the effect of cytokines causing endothelial retraction’
Robbins
226 AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
43.
Patterns of Altered Permeabilit
Increased vascular permeability” is the hallmark of Acute inflammation
Increased permeability in acute inflammation may occur in three patterns
‘Delayed Prolonged Leakage Immediate sustained leakage
+* Occurs in response to mild injuries * Occurs in response to moderate injuries ‘* Occurs in response to severe
+ Permeability (Leakage) begins * Permeability (Leakage) begins after 2- 12 injury
Immediately after exposure to hours and lasts for several hours or even days. ¢ Permeability (Leakage) begins
mediators and is usually reversible ‘immediately after injury and is
and short lived oF transient (15 to sustained ata high level for
30 minutes) + Affects venules as well as capillaries several hours until the damaged
« Affects venules alone. Capillaries vessels are thrombosed or
and arterioles remain unaffected © Caused by physical injuries such as thermal repaired
+ Caused by chemical mediators injury, X-Ray or UV radiation and certain Affecis venules, capillaries and
such as histamine, bradykinin bacterial toxins arterioles
Jeukotrenes and substance P © Caused by direct endothelial
# Mechanism not clear. damage due to severely injurious
© Mechanism: Believed to result from direct efect ofthe stimuli such as in burs or
Gaps in the endothelial lining ‘injurious agent leading to delayed endothelial _ severe neorotizing / lytic
from endothelial contraction cell damage (pethaps by apoptosis) may be bacterial infections
caused by cytokine mediated endothelial © Mechanism:
retraction which is usually delayed (in Direct endothelial injury
‘comparison to endothelial contraction caused _resultin in endothelial cell
by histamine et) necrosis and detachment
Fact to remember:
The most common pattern of increased permeability is Immediate Transient leakage®
Answer is A (Causes Pain) : Robbins 9" /39
Bradykinin increases vascular permeability, causes contraction of smooth muscles (bronchoconstriction), dilatation
‘of blood vessels and pain - Robbins 7/65
Bradykini
‘© Increased Vascular ‘© Vasodilatation
Permeability © Contraction of smooth muscles
© Pain (bronchoconstriction)
Role of Mediators in Different Reactions of Inflammation,
Tncreased vascular permeability Vasoactive amines?
(C3a and C5a (through liberaing amines) ©
Bradykinin®
Leukotrienes Cy Dy EX
PAFe
Substance Pe
Noe
Oxygen metabolites?
‘Chemotaxis, leukocyte recruitment and Ca
activation Leukotriene BE :
Chemokines?
IL-1, TNF
Bacterial products?
Fever IL-1 (and 1L6)®
TNEe
Prostaglandins
Ee Prostaglandins?
E- Bradykinin®
Tissue damage ‘Neutrophil and macrophage lysosomal enzymes®
Oxygen metabolites?
Nitric oxide®
45.
[AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008 © 227
Answer is C (T-cells): Current Occupational and Environmental Medicine 3" /193; Tumor Immunology by Parmiani
and Lotze (2002) /48; Biotherapy by Rieger 2™ /48
‘Antigen presenting cells include Macrophages, Dendritic cells in lymphoid tissue, Langerhans cells in the skin,
Kupffer cells in the liver, Microglia cells in the nervous system and B lymphocytes?
= Current Occupational and Environmental Medicine 3rd /193 (The CMDT series of books by Lange publications)
‘Antigen Presenting cells
* Monocyte? - Macrophages? © Dendritic cells® in Lymphoid tissue Activated
= Kupfer cells® in liver * Langerhans celis® in the skin B Lymphocytes?
= Microglia® in nervous system
~ Alveolar macrophages in lungs
= Splenic macrophages
Other References to support B lymphocytes (Exact lines quoted)
“Antigens are processed by specialized Antigen — Presenting — cells (APC) eg Dendritic cells, monocytes, B-cells’.
~ Tumor Immunology (2002) /48
“The best defined Antigen presenting cells are Dendritic cells, Macrophages and Activated B lymphocytes’.
—Biotherapy 2"/48
‘Three types of cells of bone marrow origin are now established as MHC — class I! expressing Antigen Presenting cells.
These are B lymphocytes, Macrophages and dendritic cells’ — Clinical Oral Science (1997)/250
‘Tivmphoeytes are not Antigen Presenting cells
T cells ean only recognize an already processed antigen displayed by an antigen presenting cell. For any cell to function
‘as an Antigen presenting cell it should have the ability to internalize the antigenic substance / protein by phagocytosis /
pinocytosis, process the endocytosed antigenic structure and then display the antigenic fragments of the native protein
‘on its surface. T cells do not have the ability to internalize and process such native antigens, and hence they can not act
as antigenic presenting cells. T cells however perform the critical step of recognizing such processed antigens on the
surface of APC’s
Answer is A (8, Microglobulin) ; Robbins 7/260, 261 Repeat (AI ~2007)
Patients on long term hemodialysis for renal failure develop amyloidosis due o deposition of f, microglobulin
(Robbins)
‘The most important amyloid proteins and their relevant clinical scenarious include:
‘This is derived from plasma cells and contains Itis a unique non immunoglobulin protein synthesized by
{immunoglobulin ight chains. Reticuloendothelal cells of Liver & It is associated with Secondary
It's associated with Primary amyloidosis © amyloidosis & reactive systemic amyloidosis ®
+ Immunocyte dyscrasias with amyloidosis such as * Chronic Inflammatory conditions:
Maltiple myeloma ® ~ Tuberculosis, @
‘+ Other monoclonal B-cells proliferation. ~ Bronchiectasis,®
Osteomyelitis 2
+ Connective Tissue Disorders
~ Rheumatoid Anhits ° (most common),
= Ankylosing spondylitis,
= 1PBilliary cirhosis ®
+ Non immune derived tumours
= Renal cll carcinoma, ®
= Hodgkins Lymphoma &
228 © AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
Br Transthyretin Islet amyloid Atrial natriuretic factor
mlcroglobulin protein (AB) (ATTR) associated peptide (ALAPP) associated amyloid
(Bam) isloid (A cal) (ANF)
is@ « Senile cerebral’ « Familial ‘* Medullary CA # Type I ++ Isolated atrial amyloidosis
‘associated — + Alzheimer's? amyloidotic Thyroid? diabetes® + Misfolded prion protein
disease neuropathies? (PsPse) Prion disease
; «Systemic senile
: camyloidosis®
46. Answer is D (sis): Robbins 8% 281; Devita 6"/13,
‘sis? oncogene is a growth factor.
The protooncogene ‘sis’ encodes the ( B chain of) Platelet Derived Growth Factor (PDGF) - Robbins 7" /293
‘mye, jun and fos oncogene are all nuclear regulatory proteins.
Selected Oncogenes with their Modes of Action
+ erb (EGFR) Brotsin tyosine kinases
|» fins (CSF-1 Receptor)
| + rer (Receptor for
Neurotrophic factor)
+ kit (Receptor for stem
cel factor)
+ ros (Insulin receptor) rine “Threonine
1 erb A (Related 19 kinases
thyroid hormone ras proteins (H, KN)
receptor)
(953 antagonist)
CDK4 (Cyclin
dependent kinases)
PDGF (Platelet derived Growih factor), FOF (FibroBlast Growth actor),
EGFR (Epidermal Growth Factor Receptor)
47. Answer is D (Wild type is associated with tumors) : Harrisons 17"/ 499, 500; Devita's Principle and Practices of
Oncology 6"/19; Robbins 7"/ 302, Harsh Mohan 5/216, 217.
Wild type of pss gene refers to the Normal (Non-mutated) form of ps; gene. The wild type of pss gene (Normal /Non-
mutated) is a tumor supressor gene that maintains the genetic integrity of cells and prevents the development of
tumors. Itis the mutated form of pss gene (and not the wild type) that is associated with tumors (Devita 6" /19)
Gene (Guardian of the Genome) (Molecular policeman
‘The pss Gene is located on the short arm (p) of chromosome 17° (17p 13.)
© The pss gene derrives its name from its apparent molecular mass (It is a $3 k D, protein)?
‘Normal (Wild type)
«The Normal ps; gene (Wild type) functions as a tumor supressor gene® and functions as a critical gatekeeper
against the development of cancer (Molecular policemen / Guardian of the genome®)
‘© The psy gene is located in the nucleus and functions as a nuclear transcription factor?
‘* Two major functions of ps gene are,
A. Inblocking mitotic activity : pss gene inhibits cyclins and cyclin dependent kinases (CDK) and prevents the
cell to enter G, phase transiently®. This allows the normal cell to repair the DNA domage
B. Inpromoting Apoptosis”: psy gene acts together with another anti-oncogene (RB gene) and identifies the
genes that have damaged DNA which cannot be repaired by in built system.
Ps; gene directs such cells to Apoptosis® by activating apoptosis inducing BAX Genes, and thus brings the
defective cells to an end. This process operates in the cell cycle at G, and Gz phase before the cell enters the S
or M phase
48.
49,
Mutant P53 gene
(Mutant pss gene)
‘AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008 ©
Most pss mutations are acquired in somatic cells and affect both psy alleles.
= Some psy mutations (less common) may be inherited in the germ line, These mutations usually affect a single
allele (Such individuals are said to have ps type Li Fraumeni® syndrome and have a 25 fold greater chance of
developing a malignant tumor by the age of 50 years than the general population)
(Inheritance of one mutant pss allele predisposes individuals to develop malignant tumors because only one
additional ‘hit is needed to inactivate the second normal
29
The wild type of pss gene may undergo mutations that inactivate or alter the normal function of p® gene
llele ~ “Second hit phenomenon’)
‘© Mutations in both alleles of ps; (Homozygous loss of ps, activity) can give rise to several human cancers
“Most common genetic alteration found in human cancer (>50%) is on acquired mutation in p gene® (Harrison)
‘Tris likely that all kuman cancers have genetic alterations that inactivate the Rb and p53 tumor supressor
pathway.
* Presence of mutant ps; genes in tumor cells predicts a poor response to radiotherapy and chemotherapy?
(poor prognostic factor)®
Tumors expressing mutant pss gene are more resistant? to radiation therapy and chemotherapy than tumors with
wild type pss Harrison)
Answer is A (Melanoma) ; Harrisons 16" /563, 439, Harrisons 17"/615
HMB ~ 45 is an immunohistological marker for Melanoma
‘© —S—100 (90% of Melanomas are positive for S - 100)
*__ HMB ~ 45 (HMB ~ 45 is more specific but less sensitive than S ~100)
‘Miscellaneous Tumor Markers : (Harrisons)
Tumor Markers
[Cancer
Gestational trophoblastic disease,
Human chorionic gonadotropin
sonadal germ cell tumor
Calcitonin Medullary cancer ofthe thyroid |
Catscholamines Pheochromocytoma
‘Antigens | Cancer rs
Alphafetoproein Hepatocellular carcinoma, gonodal |
germ cell tumor |
Carcinoembryonic antigen | Adenocarcinoma ofthe colon, |
pancreas, lng, breast, ovary
[Eieymes (Cancer ae
Prostatic acid phosphatase | Prostate cancer
[Neuron specific enolase | Small ell eancer ofthe lung,
neuroblastoma
Lactate dehydrogenase Lymphoma, Ewing’s sarcoma
imor-ASsoclated Proveins | Cancer =
Prostate ~ specific antigen
‘Monoclonal immunoglobulin
CA~ 125
IcA- 19-9
CD30
cps
Prostate cancer
Myeloma
Ovarian cance, some lymphomas
Colon, pancreatic, breast cancer
Hodgkin's disease, anaplastic large
cll lymphoma
Hairy cell eukemia, adult T cll
leukemia /Iymphoma
PSA / prostatic acid phosphatase
Placena alkaline phosphatase
Gross esti Hid protein
Factor Vil
‘Thyroid transcription factor ~ 1
(rte=1)
Actine myosin filaments
Calretinn, Mesothelin
|Chromogranin, Synaptophysin
Neuron specific enolase
[BRST 1
Progesterone & Estrogen Receptors
[cDx2
Answer is A (t x; 18) : Robbins 8" / 1233, Harrisons 16% /563
Cancer
Lymphoid neoplasm
Hodgkin's disease
Carcinoma
Lymphoid neoplasm
[Neuroendocrine tumor, Melanoma
Breast, sweat gland
Kaposi’s sarcoma, angissreoma
Lung adenocarcinoma, thyroid
Rhabdornyosarcoma
Neuroendocrine tuners
Carcinoma
Melanoma
Bladder cancer
Mesotielioma
"Neuroendocrine tumours
Breast cancer|
Breast cancer|
Gastrointestinal eancer
‘Most synovial sarcomas show a charachteristic chromosomal translocation t (x; 18) - Robbins 7/1323
AIPGMEE 2008 - EXPLANATIONS.
230 © AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
female ssa
Facts to Remember : Harrisons 16"/ 563; 645 Devita's 6"/ 1844, 2412
111322) wing's Sarcoma Family
* Classical Ewing's Sarcoma
+ Peripheral neuectodermal Tumor (PNET)
= Askin’s Tumor
1(12;22) Clear Cell Sarcoma
‘Malignant Melanoma of Soft tissues e
141216) Myroidlposarcoma
1aiB Alveolar Rhabdomosarcoma RIED
0x: 18) Synovial cell sarcoma
Cytogenetic Markers
ies) Mantle Cell Lymphoma
(14; 18) Follicular Lymphoma
814) 184] Burki'sExmphoma (8 cell ALL)
1118) MALT Lymphoma
uals 15) CLL/ Small mphocytic Lyomphoma
49:2) Precursor B cell ALL (Pre-B- ALL)
Chron Myeloid Levbaemia (CML)
ease) ‘Acute Promyclocytic Leukaemia (AML M3)
18:21) “eae NicloblateLesacnta th motration ASS
5
50. Answer is A (CD15 and CD30) : Robbins 7/688, Harrisons / 16" /655
The tumor cells in Hodgkins Lymphoma are characteristically positive for CD15 and CD30 and negative for CD45.
Robbins 7/688
Lymphocyte predominance Hodgkins Lymphoma is the only histological subtype that does not express CD15 and CD30,
This subtype expresses CD45 and is often considered as an entirely distinct category from classical Hodgkin's disease
(Harrisons)
(HAGEL ¥mphionia”—— Tmmunopheno type
"Nodular Sclerosis DIS +, CD30+ EBV -Ve Lacuna cells? (Occasional RS-cels)
ee eD1s +, cD30+ HELV CONTERIS Cie eal Sirnis
[Lymphocyte depletion DIS +, CD30+ EBV +Ve2 Reticular variant?
(Frequent R-S cells)
Pinon coh ern a
re TH “| CD30- EBV —
eS
51, Answer is A (Retinoblastoma) : Khurana 4" /281: Robbins 8/1365
Rosettes are characteristic in retinoblastomas.
Microscopic features of well differentiated Retinoblastomas include, Flexor ~ Wintersteiner Rosettes (characteristic of
Retinoblastomas), Homer -Wright Rosettes (characteristic of neuroblastoma & medulloblastoma)
Pseudorosettes and fleurette formation.
Rosettes: Review (‘Neuropathology for the Neuroradiologists’: Pathology Review by Wippold and Perry)
52.
/AIPGME EXAMINATION ANSWERS AND EXPLANATIONS ~ 2008 ¢ 231
What are rosettes?
Rosettes are pathological findings characterized by a
halo or spoke whee! arrangement of cells surrounding
acentral core or hub.
What is the significance of rosettes”
The presence of primary rosettes often suggests a given diagnosis (charachteristic finding), however this finding alone
is not considered absolutely specific or pathognomic for one specific tumor type
Common type of rosettes?
Fleaner Winterstelner Homer Wright ‘True Epeniymal Perivascalar
Rosettes Rosettes wowette pocuteroeties
+ Anal ofcels surounds a + Aaloofeellssuroundss © Ahuloofeells _* All of cells surounds a blood ves
largely empty central hub ceniral hub that contains a surrounds an empty _* The term ‘pseudo’ is used because the
but small eoplasmic meshwork of fibres area central structure is not formed from the
extensions from cells (Neutrophil rich centre) tumor itself, and represents a nonneo
project In the men plastic eletent
CS oS, 2 wwe SO)
x ao ee é oe Se
Flexner Wintersteiner Homer Wright rosettes are Truc Ependymal rosettes Pseudorosettes are not considered
rosetes are characteristic of om NEM ‘mechancterisicof characteristic of any particular
Retinoblastomas® Renan and Ependymomas ‘These may be seen in
Medulloblastomas = Ependymomas
Meuioem = Means = Medullobsoras
Medulolastomas Meekeos + Primitive Neuroectoderma tumors
Pineoblastomas Tumors (PNET) ~ Central Neurocytoma,
- Pineoblastomas = Gliablastomas
= Retinoblastoma
Retinoblastomas * Monomorphous pilomyxoid
asteetenae
‘Summary of rosette patterns and associated tumors
Homer Wright rosette ‘Neuroblastoma, medulloblastoma, primitive
neuroectodermal tumor, pineoblastoma
(Flexner-Wintersteiner rosette Retinoblastoma, pineoblastoma, medulloblastoma 4@
True ependymal rosette Ependymoma
-ular pseudorosette Ependymoma, medulloblastoma, primitive 4
neuroectodermal tumor, central neurocytoma,
‘ glioblastoma, monomorphous pilomyxoid astrocytomas |
Pineocytomatous rosette Pineocytoma
(Neurocytic rosette Central neurocytoma |
Answer is D (Hyaline Arteriosclerosis) : Robbins 9/490; Harsh Mohan 5"/ 711, 712, 713
Hyaline arteriosclerosis isa feature of Benign Nephrosclerosis assciated with benign phase of Hypertension. It is not
4 feature of Malignant Hypertension,
232 © AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
‘Benign Nephrosclerosis
This tem is used to describe the changes in kidney
associated with benign phase of hypertension
Gross
© Kidney size is either normal” or may be
moderately reduced”
© Grain leather appearance? : The cortical surface
has a fine even granularity
| Microscopic (Vascular Changes & Parenchymal Changes)
© Hyaline Arteriosclerosis °
‘Narrowing of the lumens of arterioles and small
arteries caused by thickening and hyalnization
of the walls
© Fibroelastic Hyperplasia®: in the intima (intimal
thickenning®), duplication of elastic lamina and
hypertrophy of the ‘media’
‘+ Parenchymal changes (due to ischaemic)
Variable degree of Atrophy of parenchyma due
to ischaemia
| Malignant Nephro:
slerosis
This term is used to describe the changes in kidney
associated with malignant or accelerated hypertension
Gross
© Kidney size is variable? May be smaller in size
(when superimposed on benign nephrosclerosis) or
Larger in size (enlarged)° than normal (patients
‘who develop malignant hypertension in pure form)
© Flea bitten appearance®:
The cortical surface may show multiple small
peticheal haemorrhages? from rupture of arterioles
‘or glomerular capillaries.
Microscopic (Vascular Changes & Parenchymal Changes) 11)
+ Fibrinoid necrosis of arterioles® (Necrotizing
carterioliis®)
‘The vessel wall shows fibrinoid necrosis.
Represents an acute event and necrosis is usually
‘not accompanied by intense inflammation
+ Hyperplastic intimal sclerosis® / Onion ~ Skinning
Concentric laminae of proliferated smooth muscle
cells, collagen and basement membrane (producing
intimal thickenning)
‘* Parenchymal changes (due to ischaernia)
Variable degree of atrophy of paranchyma due to
ischaemia. Infarction necrosis distal to abnormal
vessels may be seen
Answer is D (Alports syndrome): Robbins 9/913; Harrison 17"/1785
Alports syndrome is not associated with Rapidly Progressive Glomerulonephritis or Crescentric Glomerulonephritis
“Harrison 17° /1785
Rapid jJomerulonephritis (RPGN) / Crescentric Glomerulonephritis
Crescentric Glomerulonephritis isa histopathological diagnosis based upon the presence of ‘crescents’ in most of the
Glomeruli. This type of histopathological picture (crescents) is seen in cases of Rapidly Progressive Glomerulonephritis
(RPGN) and hence RPGN and Crescentric Glomerulo-nephrtis are often used synonymous.
Causes of Crescenteric Glomerulonephritis (RPGN
[ype I RPGN (Anti - GBM Antibody) ee
‘© Idiopathic Anti Glomerular Basement membrane disease
# Good pasture's Syndrome
‘Dope RPGN (immune Compiex) 2
Idiopathic
Acute Post Streptococcal Glomerulonephritis (PSGN)
Lupus Glomerulonephritis (SLE)
Henoch Schonlein Purpura (HSP)
IgA Nephropathy
Membranoproliferative Glomerulonephritis (Harrisons 17" / 1785)
Cryoglobulinemia (Harrision 17"/ 1785)
Post infectious (After subacute Bacterial Endocarditis) Glomerulonephritis
Wegener's granulomatosis,
2 Microscopie polyangitis
Churg ~ Strauss syndrome
58.
‘AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008 * 233
Renal disease in Alport’s syndrome (Harrisons 17" /1794)
Patients with Alport’s syndrome develop thinning and splitting of Glomerular basement membrane®, and chronic
glomerulosclerosis®, leading to renal failure. (Clinically present with hematuria & proteinuria)
Rapidly progressive Glomerulonephritis or crescentric glomerulonephritis is not associated with Alport’s syndrome.
Harrisons 18° /2344; Chandrasoma Taylor 3" /708
Mesangiocapillary Glomerulonephrits is the other name for Membranoproliferative glomerulonephritis. Itis a type
of proliferative Glomerulonephritis. (Harrisons 17” /1789)
Answer is B (Mesangiocapillary Glomerulonephi
Proliferative changes in Glomerulonephritis (Refer: Chandrsoma Taylor 3"! /702, 708)
‘* Glomerulus contains Endothelial cells, Epethelial cells, and Mesangial cells. Any of the three cell types may
undergo proliferation in different types of Proliferativ Glomerulonephritis.
‘© Proliferative changes are not to Membranoproliferative and Mesangioproliferative Glomerulonephritis,
bbut may be seen in several other forms of Glomerulonephritis
Glomerulonephritis and Proliferative changes
el
‘Glomerulonephritis without proliferative changes Glomerulonephritis with proliferative changes
“Glomerulonephritis | Proliferative changes [[Glomerulonephritis Proliferative changes
‘Minimal change Disease | - (Absent) Post streptococcal GN + (Crescent)
Membranous = (Absent) “Antbasement membrane disease | + (Crescents)
Glomerulonephritis (Good — pasture’s syndrome)
Diabetic Nephropathy ~ (Absent), ‘IgA Nephropathy (Berger's) + (Mesangial)
Amploidosis = (Absen!) Henoch Schonlein Purpura __| + (Mesangial)
Focal segmental + Variants with protiferaive | | Mesangioproliferative GN + (Mesangial)
Glomeruloscerosis | lesions have heen described | | Membranoproliterative GN | + (Endothelial &
including cellular lesions with | | (Mesangiocapilary GN) Mesangial)
‘endocapillary hyperceliutarity- | | Focal Glomerulonephits + Focal)
(Harrisons) ‘Secondary Glomerulonephritis | + Variable
SLE/PAN
Note : Crescents represent proliferation of epethelial cells
Answer is C (Nephrin): Robbin's 7"/981, 983, 984
““A mutation in the Nephrin gene causes a hereditary form of congenital Nephrotic syndrome (Finnish type) with
‘minimal change glomerular morphology”- Robbins 7"/981
+ Nephrin is a key component of the slit diaphragm
«+ Itis a zipper like structure between podocyte foot
processes that might control glomerular permeability
+ The Nephrin gene maps to chromosome 19q13 and is
termed as NPHS1
+ Several type of Mutations of the NPHSI gene have been
identified and they give rise to congenital nephritic
syndrome of the Finnish type.
No
‘+ ‘Podocin’ has also been recognized as a component of the slit diaphragm.
‘+ Podocin is encoded by a gene termed as NPHS 2 and maps to chromosome 1425-31
‘+ Mutation in the podocin gene or NPHS2 lead to an autosomal recessive form of focal segmental
glomerulosclerosis.
234 © AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
56. Answer is C (Fibromatosis) : Robbins 8° /1251
Fundamentals of Diagnostic Radiology by Brant & Helms 3/542, Pediatric Hematology by Arceci Hann and Smith 3”!
(/373, Nelson's 18/2148 (Askin Tumors)
Fibromatosis can be defined as a group of conditions associated with either benign tumors (desmoid tumors) or
tumor like conditions (eg peyronie’s disease). These conditions represent benign lesions and are not malignant.
Askin Tumors, Chloromas and Plasmacytomas are all Malignant tumors
Askin Tumor : (Differentic is in Orthopedic Oncology by Greenspan 2" 323; Nelsons 18"/2146)
Askin tumor is a rare malignant neoplasm arising from the chest wall of children and young adults
‘© These tumors arise from primitive neurectodermal rests in the chest wall and are grouped into the Ewing’s sarcoma
family of tumors (Ewing’s sarcoma along with PNET (Primitive Neurectodermal Tumors) and Askin tumor)
‘These lesions are very aggressive and associated with a high mortality rate
Ch lary Leukaemia or Granulocytic sarcoma)
© Chloromas can be described as extramedullary masses of leukaemic cells that are commonly seen in patients with
Acute Myeloid Leukemia, (AML)
* They represent malignant tumors and are also called granulocytic sarcomas
~The most common site of chloromas is the Orbit / Periorbital region®
= They are also frequently noted in the skin®
= They may involve the spinal cord and may present with symptoms of cord compression®
= They ate most commonly seen with M, and Ms AML® but may also be seen with M, and Mz subtypes
Plasmacytomas (Harrisons 17” /704)
. Plasmacytomas are malignant tumors of plasma cells.
‘+ They are best described as variants of Multiple Myeloma and usually occur in two forms:
Solitary Bone Plasmacytoma: Single Lytic bone lesion without marrow plasmacytosis,
Extramedullary Plasmacytomas: Usually involve the submucosal lymphoid tissue of the nasopharynx or paranasal
sinuses without marrow plasmacytosis
‘M component in < 30% of cases® ae
Associated Median survival 2 10 years®
Affect younger individuals?
Eibromatosis
+ Fibromatosis represent a group of fibrous benign tumors or tumor like conditions and are classified into
superficial & deep fibromatosis. Fibromatosis are not malignant lesions
© These are better described as tumor like lesions
Deep fibromatoses represent a group of fibrous
rather than true tumors. tumors that are benign but locally aggressive
‘© These conditions include a group of fibrous ‘They do not metastasize and hence are not
tissue lesions that are more bothersome than considered malignant despite their locally
serious aggressive nature
- Palmar fibromatoses (Depuytren contracture) © ‘They may however recur after surgical excision
~ Plantar fibromatoses (due to their locally infiltrative nature)
= Penile fibromatoses (Peyronie's disease) ‘+ Example includes Desmoid tumors
57, Answer is A (Genomic imprinting): Harrisons 16"/ 375; Robbins 9"/ 172
58.
/AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008 © 235
The phenomenon referred to as genomic imprinting leads to preferential expression of an allele depending on its
‘parental origin — Harrison 16%/ 375
‘Genomic imprinting
Imprinting refers to selective inactivation of a gene or set of genes on either the
‘maternal chromosome or the paternal chromosome
7
Maternal genomic imprinting Paternal genomic imprinting
Inactivation of maternal allele ie. inactivation of Inactivation of gene on paternal allele i.e. inactivation of a
‘a gene on maternal chromosome gene on paternal chromosome
‘Thus the only functional alleles are now provided by either the paternal or maternal chromosomes (ie. only
‘one parent)
Y
Deletion of the only functional allele results in genetic syndromes
+ Prader Willi syndrome: deletion on paternally derived chromosome®
+ Angelman syndrome: deletion on maternally derived chromosome?
| Prader WilliSvndrome || Angleman Willi Syndrome.
Maternal Patera Maternal Patemal
Prader Will Angelman
gene gene
Gesomic
‘inpiting
imprinted imprinted Active
(aac) Active Prader Goativ) Angelman
radet Wil Willi gene Angelman
gene gene ome
‘The only functional gene ‘The only functional gene
is provided bythe is provided bythe
paternal chromosome paternal chromosome
Deletion on paternal Deletion on pateral
chromosome chromosome
imprinted imprinted
inactive) Ainative Jeeted inactive
water Deke intve mater agenan gos
Prader Wit Prader Willi gene “Angelman cima gs
a! “|
Prader Willi Syndrome Angelman Syndrome
‘+ Deletion occurs exclusively on paternal + Deletion occurs exclusively on maternal chromosome 15,
chromosome 15 (deletion of tand q 12 in long
arm of chromosome 15)
= Features 2 Features
= Diminished fal activity — Hypotonia
= Hypotonia? — Mental retardation
= Obesity? - Seizures
= Mental retardation Ataxia
= Shor stature — Inappropriate laughter (Happy puppets)
= _Hypogonadotropic hypogonadism
Answer is A > D (Antibody) > (Glycoprotien): Harrisons 17” /2155, Davidsons 20/1074
A Rheumatoid factor is an antibody (auto-antibody) of any immunoglobulin class directed against a specific region
of the Fe fragment of human IgG. - Davidson
Rheu
236
60.
‘© AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008,
* A Rheumatoid Factors is an antibody (auto-antibody) of any immunoglobulin class (directed against Fe fragment
of human IgG)
© Rheumatoid factor in Rheumatoid Arthritis belongs to the IgM class ° (directed against Fc fragment of IgG)?
(IgM Rheumatoid factor is positive in about 80% of patients with Rheumatoid arthritis (Harrisons 17"/2155)
Q
‘© Antibodies are glycoproteins and immunoglobulins are also glycoproteins
© A Rheumatoid factor is an antibody and because antibodies are glycoproteins, it would not be incorrect to say that
Rheumatoid Factors are glycoproteins.
If Antibody / Auto- antibody is not provided amongst the options Glycoprotein would be the best correct answer,
Answer is B (Occurs when donor cells are immunocompromised) : Robbins 9/236, Harrisons 17/715, 716
Graft versus host disease occurs when immunologically competent donor cells (not immunocompromised donor
cells) are transplanted into immunologically crippled (immunocompromised) hosts and the transferred cells
recognize host cells as alloantigens, (Robbins 17"/ 222)
Graft Versus Host Disease (GVHD)
‘© The Graft Versus Host Disease (GVHD) was first recognized in animal studies on mice, when it was termed Runt
disease, (Blood' by Handin, Lux, Stossel 2"/2133)
‘+ Graft versus Host Disease may occur in any situation in which Immunocompetent cells or their precursors are
transplanted into Immunosupressed recipients
Graft versus Host disease occurs because the immunocompetent T-cells present in the donors recognize the HLA.
antigens in the host as ‘foreign’ and react against them.
* GVH disease occurs most commonly in the setting of allogenic bone marrow transplantation, but may also follow
transplantation of solid organs rich in lymphoid cells (eg Liver) or after transfusion of unirradiated blood
‘within 3 months posttransplant
or persisting beyond 3 months post transplant
* GVHD most commonly presents with changes in Skin, Gut or Liver disease®
PER eS 0A eR Ol
Rash Elevated Bilirubin Persstant Anorexia
Exythroderma Elevated ASTALT Persistant Diarrhoea
Desquamation & Bullae Elevated Alkaline phosphatase Both
* Diagnosis usually requires Biopsy from Skin, Liver or Gut (endoscopic)?
Answer is C (Binds to the cleft in the MHC II Molecule): Harissons 18"/2671-72; Essentials of Clinical
Immunology 4"/ 40, 41; Immunology by 1°/ 88, 90
The Cleft in the MHC I molecule represents the
Antigen binding groove where conventional
peptide antigens or ‘simple? antigens are
presented. Superantigens do not bind to the cleft
or the antigen binding groove in the MHC II
‘molecule. They bind ata site which is distinct from
the cleft and located on the lateral side of the cleft.
‘Superantigens
‘© Super-antigens are protein molecules produced by some bacteria and viruses that do not require to be processed
tracellularly by Antigen presenting cells before they activate the T cells.
‘Simple Antigens (Conventional antigens) are first processed by Antigen presenting cells and
‘the processed antigens are then presented on the surface of the APC. These processed antigens
are presented in the Antigen binding groove (cleft) of the MHC II molecules. The T cell
Receptors om the surface of T cells ean only recognize peptide antigens that are displayed on
the antigen binding groove of the MHC.
61.
|AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008 «237
© They bind directly to MHC of APC and T cells at a site distinct [waperameyen
from the cleft or antigen binding groove.
This is possible because superantigens have two binding sites. One
binding site is for the class If MHC molecules found on the surface —se
‘of APC, and the other binding site is found outside the Antigen ete
binding site on the T cell Receptor. Binding of superantigen to re
MHC I of APC and T cell causes T cell activation.
ed cosa Te
‘* Because the superantigen does not bind to the specific antigen binding site on the TCR, super-antigens select all
T celts (carrying a particular T cell Receptor V i gene) regardless of the T cell antigen specificity.
This widespread T cell activation results in massive release of inflammatory cytokines and hence clinical
‘manifestations of hypotension and shock are often associated
istinguishing features between Simple antigens and Super-antigens
= ees ar
+ Need tobe processed intracellularly by APC before they» Do not need to be processed intracellularly
can activate the T cells
* Bind to MHC class 11 molecule in the Antigen binding © Bind to MHC class IL molecule directly to the lateral
groove or cleft (groove of the af hetrodimer) portion Antigen binding groove or cleft
Bind to the Tcells.at the T cell Receptor region (TCR) ‘Bind to the T cel in the lateral portion of the T cell
(V region of the TCR a and f chains) Receptor (Lateral portion of TCR 8 chain)
+ Stimulation of T cells is dependent on the antigenic * Stimulation of Tceltsis independent of T cell antigenic
specificity of T cells (Only those T cells that have the T ‘specificity Al cells cerying a particular T cell Receptor V
cell Receptor (TCR) appropriate to the MHC antigen B gene are stimulated regardless ofthe T cell antigenic
complex are stimulated ~ specific) specifciyy
‘© Stimulate smaller number of T cells ‘Stimulate larger number of T cells
(Activate about 1 in 10,000 T cells) (Activate about 1 in $0 T cells)
‘+ The release of inflammatory eytokines is less marked «The release of inflammatory cytokines is massive/marked.
(monokines / Lymphokines) (monokines & lymphokines)
This is often associated with hypotension & shock.
© Examples include + Examples include
‘Normal cell mediated immune reactions Toxic shock syndrome
(Staphylococcal, Streptococcal, Clostridial, Yersinial)
Role of super antigens is also been investigated for
Kawasaki disease
(No organism yet identified but superantigen association is
‘based on eytokine profile)
Answer is B (Asbestosis) : Robbins 9"/691; Chandrasoma Taylor 3/541
Ferruginous bodies are most commonly seen in Asbestosis ~ Chandrasoma Taylor 3/541
Ferruginous bo
+ These bodies represent foreign inorganic or organic fibres coated by complexes of iron and glycoproteins
(fibre + iron — glycoprotein coat).
+ While ferruginous bodies are most commonly seen in Asbestosis they are not diagnostic because a similar
iron — glycoprotien coat may form on any other type of inhaled fibre.
‘+ Ferruginous bodies are best seen in sections that have been stained for iron with prussian blue
‘+ Microscopically Ferruginous bodies give a shish kebab appearance®.
‘A thin central asbestos fibre (5- 10 1 mlong) encased in an iron containing glycoprotein coat which is brown and
typically beaded (like a shish kebab)
ts to Remember
Schaumann's bodies and Asteroid bodies are seen in sarcoidosis”
Russell bodies (cytoplasmic) and Dutcher bodies (nuclear) are seen in Multiple Myeloma?
Psammona bodies may be seen in Meningiomas, Papillary Carcinoma Thyroid, Serous Cystadeno Carcinoma of
Ovary, and Renal cell carcinoma
Pick’s bodies® are sen in Fronto temporal dementia (Pick’s disease)
Paschen bodies® and Gunari bodies® are seen in Small Pox or Vaccinia
Negri bodies® are seen in Rabies
238 © AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
‘Mooser’s bodies® are seen in Endemic Typhus fever (Caused by Rick Hsia typhi)
Miyagawa’s bodies® are seen in infection with Chlamydia Trachomalis
Lafora bodies® are seen in Familial Myoclonic Epilepsy.
Donovan bodies® are seen in infection with Calymmatobacterium granulomatis
CCivatte bodies? are seen Lichen Planus
Call - Exner bodies® are seen Ovarian Granulosa Cell Tumors
Aschoff bodies® are seen in Rheumatic Carditis
Tuffstone bodies® are seen in Metachromatic leukodystrophy
62, Answer is D (Metalloproteinses) : Robbins 8"/ 105
“Degradation of collagen and other ECM proteins is achieved by a family of Matrix.
Metallo proteinases (MMP) which are dependent on Zinc ions for their activity’ ~ Robbins / 110
Basement membrane is a component of ECM and largely consists of collagen (Type IV).
Matrix: Metaloproteins MMP9 and MMP? are collagenases that cleave type IV collagen of epithelial and vascular
basement membranes’ ~ Robbins / 312
jasement Membrane and Matrix Metalloprotein (MMI
Basement membrane consists of a network of amorphous Non fibrillar collagen (mostly type 1V)® Laminin, heparan
sulphate, proteoglycans and other glycoproteins, (Robbins / 103)
“Matrix metalloproteinases (MMP) is a family of enzymes which includes more than 20 members
These include enzyme that are involved in degradationof Basement Mebrane such as:
+ MMP 2 & 9, Gelatinases/Collagenases) which degrade amorphous collagen and fibronectin (Basement Membrane)
+ MMP 3, 10 & 11 (Stromelysins) which degrade proteoglycans, laminin, fibronetin and amorphous collagens
(Basement membrane components)
MICROBIOLOGY
63. Answer is B (Prions) : ‘Antisepsis, Disinfection and Sterelization' by Mc Donnell 1“ (2007)/33,
Prions are most resistant organisms to antiseptics.
Prions Serie, Creuzfeldt-Jakob disease, Chronie Wasting Disease
Baceral spores Bacillus, Costidium
Protzoal oocysts ‘Gryposporiium
"| Feimintheges “Ascaris, Entrobins
~ [ Mycobacteria ‘Mycobacterium wubureulosis (other myeobaeteria)
| Small nonenveloped vines | Polio vin, parvoviruses, papilloma virus
Protozoal ats Giardia, Acanthamoeba
Fungal spores “Aspergillus, Penicillin
Gram negative bacteria Pseudomonas, Providencia, Escherchia
Vegetative fingi and algae ‘Asperillus, Tichophyton, Candida, Calomierons
Vegetative nelminths & protozoa | Ascaris, Cryposporidium. Giardia
Large nonenveloped viruses ‘Adenoviruses, rota viruses
‘Gram: postive bacteria Siaphyfococeus, Sweploeoccus, Enterococcus
Enveloped vinses | Human immunodeficiency virus, hepatitis B virus, hemes simplex virus |
64, Answer is C (Most Enterococci are sensitive to Peni }: Ananthnarayanan 9/217
Enterococcii are frequently resistant to Penicillin
© Enterococci are frequently resistant to penicillin, (Ananthanarayan 7/212)
Enterococcal strains resistant to penicillin occur frequently - Ananthnarayana 7"/212
Enterococci are more resistant to Penicillin than other streptococci.
Resistance o Penicillin may occur either due to B lactamase production or due to altered Penicillin binding proteins
Enterococeii may also be resistant to Aminoglycosides, Cephalosporins, Monobactems, and Vancomycin®
‘AIPGME EXAMINATION ANSWERS AND EXPLANATIONS =2008 © 239
‘* Micrococci are oxidase positive (Ananthanarayanan 7"/200, 201)
Micrococci are gram positive cocci which occur mostly in pair, tetrads or irregular clusters
Micrococci are
Aerobic®
Oxidase positive ®
Catalase positive ®
Oxidase positive nature fferentiate mien staphylococci
‘Hugh and Leifson’s oxidation — fermentation test (Laboratory test)
Micrococci show oxidative pattern while staphylococci show: fermentative pattern®
‘* Pneumococci are capsulated. (Ananthanarayanan 7"/217)
Pheumococci posess a type specific polysacharide capsule. This is the most important antigen? of the
pheumococeus. The capsule may be demonstrated as a clear halo in India Ink preparation
‘© Non Motile® © Bile soluble’
+ Non sporing® © Optochin
© Capsulated® (Specific polysaccharide capsule) sensitive?
‘© Smail slightly elongate cocci Catalase
(flame shaped®, Lanccolate® appearance) Negative?
© Arragned in pairs (Diplococci)® Oxidase
G
positive Negative
‘* Staphylococcus saprophyticus may cause UTI (Ananthnarayanan 7"/200)
Staph saprophyticus belongs to the group of coagulase negative® staphylococci
‘They constitute major components of the normal flora?
‘+ They are normally non pathogenic but may cause disease
+ Urinary tract infection particularly in sexually active young women is characteristic
(Men are infected much less common)
They are usually sensitive to common antibiotics?
Answer is A (Capsular Hyaluranie acid): Ananthnarayanan 9/212
Capsular Hyaluronic acid from streptococcus pyogenes cross-reacts with human synovial fluid.
Antigenic eross reactions betwe s & Human Tissues
Various structural components of streptococcus pyogenes exhibit antigenic cross reactions with different tissues of the
‘human body
‘These cross reactions are believed to account for some of the manifestations of streptococcal diseases where the tissue
have been damaged by immunological manifestations (eg Rheumatic fever)
Capsular Hyaluronic Acid Synovial fluid
Cell Wall protein Myocardium
Group A carbohydrate Cardiac Valves
Cytoplasmic Membrane Antigen Vascular Intima
Peptidoglycans ‘Skin
Answer is C (It is universally susceptible to penicillin): Ananthnarayanan 9"/217; Jawetz 23% /243; Harrisons 179/889
Enterococci are not universally susceptible to penicillin. They may be resistant to penicillin. Resistance to penicillin
may occur either due to lactamase production or due to altered penicillin binding proteins - Harrisons 17" (889
They are more resistant to penicillin G than streptococcii — Jawetz 23/243
‘Strains resistant to penicillin occur frequently ~ Ananthnarayanan 7" /212
240 © AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
67.
‘The enterococci posess the Group D (Lancefield) c
I wall specific antigen and therefore are often class
Lancefield Group D streptococcii®
sd as
‘© There are atleast 12species of enterococci, but Emerococcus fecalis and Enterococcus faecium are the most
‘common
[Enterococcus fecalis : Most common® (causes 85-90% of infections)
[Enterococcus faecium = Second most common® (causes 5-10% of infections)
‘© Enterococei are part of normal enieric flora? (Present in intestine, genital tract and saliva)
Enterococci are amongst she most frequent causes of nosocomial infections particularly inthe Inensive care
Units
Endocarditis
Intra abdominal abscess®
Peritonitis”
Meningitis in neonates
The most common mode of transmission of enterococci is on the hands of hospital personnel?
(May occasionally be transmitted on medical devices)
Enterococci are frequently resistant to Antibiotics
Major problem with enterococci is that they can be highly resistant to antibiotics?
‘* Enterococii may be resistant to Aminoglycosides (Streptomycin > Gentamycin), Cephalosporins, Penicillins, and
even Vancomycin, and other antibiotics.
= Most wide spread resistance is seen with streptomycin® (Harrison)
= Strains resistant to penicillin occur frequently? (Ananthanarayanan)
= Vancomycin resistant enterococci have become common® (Harrison)
Answer is D (Produces 01 Lipopolysaccharide): Ananthnarayanan 9"/306; Jawetz 23/270; Harrisons 168/909, 910
¥. cholerae 0139 does not produce the O1 Lipopolysacharide and does not have all the genes necessary to make this
antigen’ ~ Jawet:
. V. cholerae 0139 biotype was first isolated from a cholera out break in Chennai (Madras) as a novel
strain of V- cholerae and was then termed as a Non 01 V. cholerae.
(This strain subsequently spread via the coast of Bay of Bengal reaching Bangladesh designated as V-cholerae
0139 Bengal)
. Clinical manifestations and epidemiological features of the disease caused by V. cholerae 0139 Bengal are
indistinguishable from those of the O1 cholera — Harrison
. V. cholerae 0139 does not produce the 01 Lipopolysacharide.
V. cholerae 0139 is very similar to V. cholerae 01 Eltor biotype, but there are certain differences?
[Wichilerae 0139 Bengal Nel eee YE
‘+ Novel O antigen that does not produce O1 1 Lipopolysaccharide is produce
ipopolysaccharide — Jawetz
-apsulated? + Non capsulated?
. cholerae 0139 makes a polysacharide capsule like *V. cholerae O1 does not make a capsule
other non O1 V. cholerae strains’-Jawetz
Immunity to V. cholerae O1 ElTor is not protective against the V, cholerae 0139 biotype®
+ All vibrio cholerae possess a common flagellar H antigen
+ Vibrio cholerae possess different Lipopolysaccharide O antigens which forms the basis of classification.
/AIPGME EXAMINATION ANSWERS AND EXPLANATIONS ~ 2008 ¢ 241
Those that agelutinate Ol antisera are called OI V. cholerae and those that do not are called Non Ol V.
cholerae.
+ V. cholerae O1 are distinguished into two biotypes * Classical and E1~Tor.
Each biotype is further divided into three serotypes ‘Inaba’, ‘Ogawa’ and ‘Hikojima’
+ Non V. cholerae O1 are broadly subgrouped into 0/39 V. Cholerae strains that have been associated with
epidemic cholera and Non 01 /Non 0139 V. cholerae that are not known to cause epidemics or pandemics of
cholera.
Vibrio cholerae (common H Antigen)
O1V. cholerae Non—O1 Vibriocholerae
(Agglutinate in 01 antiserum) (Do not agglutinate in O1 antiserum)
Classical El Tor
=a
i 1 i ‘Non known to cause
Ogawa Inaba Hikolima Epidemic and :
Pandemic cholera | | Epidemic/Pandemic cholera
Sones Gees Chloera like diarrhea
Epidemic and Pandemic cholera Bibs deatee) a
Rarely extraintestinal infection
(a) Answer is A (Usually associated with CMV infection): Washingion manual of Pulmonary Medicine (2006) 104
Harriosns 16%/ 1194, 1195; Jawetz 24"/ 648, 649; ‘Pneumocystic Pneumonia’ by Wolzer & Cushion 34418; CT sean ofthe body by
Mathias /362
Pneumocystis Jiroveci may be associated with CMV infection but itis not usually associated with CMV infection.
‘Pheumocystis Jiroveci is the new nomenclature for human infection with Pneumocystic carini (which is now used for
organisms found in rats)
Pneumocystis infection in Humans : P. diroveci
Pneumocystis infection in Rats: P. Carini
Pneumoevstie Jirovecii dis immunosupression
‘Pneumocystis Jiroveci does not cause disease in the absence of immuno supression’ Jawetz 24°'/648
Note
Pneumocystic Jiroveci may infect immunocompetent hosts but the disease (pncumocystis pneumonia) occurs only
when the host is immunosupressed
‘Most individuals are infected in early childhood But pneumonia occurs in immunocompromised patients only either
due 10 reactivation or new wie
“Acquired Immunodeficier ase (eg AIDS)
* Patients Recieving /mmunosupressive therapy (especially Glucocorticoids) for cancer, organ transplantation etc
* Children with primary immunodeficiency diseases
‘+ Premature malnourished infants (immunodeficient)
Pneumocystic Pneumonia : Diagnosis
Diagnosis of Pneumocystic Pneumonia is based on specific identification of organism in respiratory specimen with
appropriate histological staining
+ Pneumocystis infection is usuall sed by sputum examination
‘Sputum samples should always be obtained by induction (with hypertonic saline)
Routine sputum specimen is often inadequate (Washington manual of Pulmonary medicine)
+ BAL forms the mainstay of diagnosis for Pneumoeystic Pneumonia
Iorganisms are not seen on induced sputum examination a Bronchoalveolar lavage specimen should be
obtained. BAL forms the mainstay of diagnosis for Pneumocystic Pneumonia - Harrisons 16°
242+ AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
Poremocyte orsmona Suspected
Chest Radiograph
Reiouar or gma opctin L
Sputum by Induction
(reve) Negative
Bronchoscopy with BAL
oc
Treat Observe
Treat
‘* Pneumocystic Pneumonia and CMV infection (‘Pneumocystic Pneumonia’ by Wolzer & Cushion 3418)
‘Several studies have indicated that CMV is a risk factor for Pneumocystis Pneumonia in Renal transplant patients
These is however no convincing evidence to show a direct effect of the CMV virion on Pneumocystis’
‘Thuswe conclude
Pheumocystic may be associated with CMV infection but ina few selected cases and special circumstances lke Renal
tansplantation. CMV isnot usually associated with pneumocystic pneumonia.
‘+ Pneumocystis Pneumonia and Pneumatocele
Pneumocystic Pneumonia may be associated with pneumotocele formation but Pneumatoceles are not associated
in all cases of Pneumocystic pneumonia
Sa ier Ooms er oneticad
+ Peumocystc®
++ Post traumatic (Laceration )
1s After treatment of metastasis (rafe)
68. (b) Answer is B (Usually diagnosed by Sputum examination) : Refer previous question
Pneumocystis Jirovect is usually diagnosed by sputum examination. This is the single best answer of choice amongst
the options provided.
‘© Pneumocystic infection is usually diagnosed by sputum examinatio
neumoeystic infection is Bronchoscopy with BAL
Sputum examination is the initial procedure of choice to confirm the presence of Pneumocystic Jiroveci infection
mainstay of diagnosis for
P. Jirovect infection is usually diagnosed by histopathological staining of an induced sputum specimen
But 4 BUT
‘Sputum examination is not the mainstay of diagnosis of P. Jiroveci infection.
Fibreoptic Bronchoscopy with BAL which is more sensitive than sputum examination remains the mainstay of
| Pneumocystis diagnosis — Harrison 17"/1195
'* Pneumocystis infection may occur in healthy individuals but disease due to Pneumocystic infection does not
‘occur in the absence of Immunosupression
“Serological endence suggests that most individuals are infected in early childhood” — Jawetz 24°/648
“Most healthy children have been exposed to the organism by 3 to 4 years of age’ — Harrisons 16/1194
BuT 4 BUT
‘In the absence of immunosupression P. Jiroveci does not casue disease’ ~ Jawetz 24th/ 648
‘© Pneumocystic Jiroveci infection may be associated with CMV infection and may present with Pneumatocele
‘(Not always) (Refer previous question)
/AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008 ¢ 243
Remember : Facts: Confusing state
* Pneumocystis infection is usually diagnosed by sputum examination. : True
© Pneumocystis infection is usually diagnosed by routine sputum examination 2 False
Routine sputum specimen are often inadequate. Sputum samples should be obtained
bby induction with hypertonic saline - Washington Manual
‘© Sputum examination is the mainstay of diagnosis for Pneumocystis 2 False
Bronchoscopy with BAL is the mainstay of diagnosis — Harrison
‘© Pneumocystis infects only the immunocompromised host False
‘Most healthy individuals are infected with pneumocystis in early childhood — Jawetz
© Pneumocystic pneumonia occurs only in the immunocompromised host True
P. Jiroveci does not cause disease in the absence of immunsupression ~ Jawetz
Answer is A (They are infectious proteins): Ananthnarayanan 9%/557; Harrisons 16/2495; Jawetz 24/581
Prions are infectious proteins devoid of any nucleic acid - Harrisons
Prions and Prion associated diseases
‘+ Prions are infectious proteins devoid of any nucleic acid (RNA or DNA)®
(Prions are the only known infectious agents that are devoid of nucleic acid®)
‘© Prion diseases result from the accumulation of the abnormal prion protein ‘Pr P“'@
* Prions are most resistant to physical and chemical agents such as heat, irradiation and formaline®.
‘©The diseases caused by Prions include diseases in human & animals
Prion diseases
Human Animals
+ Creutsfeldt Jakob disease® + Scrapie (sheep) ®
* Gerstmann — Straussier Scheinker ‘+ Bovine Spongiform Encephalopathy (cattle) 2
disease? «| Mink Encephalopathy (Mink) ®
+ Faral Familial Insomnia® + Chronic Wasting Disease (Mule, Deer, Elk) ®
© Kun ‘+ Feline Spongiform Encephalopathy ( Cats) 2
‘+ Prion Diseases share several distinguishing hallmarks
‘The disease is confined to the Nervous system® (Although agent may be recoverable from other organs)
The basic features are Neurodegeneration and Spongiform® changes
‘* Amyloid plaques may be present
* Ch illness is preceded by a long incubation period® (months to decades)
Onset of clinical illness is followed by chronic progressive disease® (weeks to years)
The disease is always fatal® with no known cases of remission® or recovery
'* The host shows no inflammatory response and no immune response®
~ Agents do not appear to be antigenic?
- No production of interferon is elicited
= There is no effect on host B cell or T cell function
= _Immunosupression of the host has no effected on pathogenesis
‘244 © AIPGMEEXAMINATION ANSWERS AND EXPLANATIONS - 2008
70. Answer is A (Bird Flu Virus): Molecular Medicine by Trent 3"/209,210; Clinical Infectious Disease by Schlossberg (2008) /1290
HSN1 is the Avian Flue Influenza A virus, also called the Bird Flu virus
New A virus
‘+ The Influenza A viruses undergo constant antigenic variations, (Antigenic shift or Antigenic drift)
‘+ Because of these antigenic variations immunity to the influenza virus is partial and temporary
‘+ Antigenic variations mainly involve the two external glycoproteins of the virus, Haemoglutinin (H) and
Neuraminidase (N)
‘+ Antigenic ‘Shifts’ result from genetic reassortments and produce immunologically novel strains of the influenza
virus. These novel strains occur sporadically and herald longer epidemics & pandemics
The ‘HSNT’ strain is one such novel strain found in human infections, that was previously known fo cause
luenca out breaks only in birds — Avian Flu virus (First isolated in 1997 from China)
The HSN1 avian flue is a particularly virulent type of infection that causes wide spread organ damage and
death rapidly
Other strains causing outbrakes of bird flu include, H7 N3, HSN2, H7N2, H2N2
© Important animal to human and human to human out breaks that have been recorded recently include.
HSNI > 1997 and 2004 ©The range of Influenza A glycoproteins in human
HON2 1999 include
HIN2 2003 (Also 2002) ‘Species Haemaeglutinin -Neuraminidase
HINT 2003 ‘Humans | Hl -H3, HS, H7, H9 | NI, N2,N7
71. Answer is C (Ankylostoma): Harrisons 16/1257, 1271
Biliary obstruction may be seen in infection with Clonorchis, Fasciola and Ascaris. It has not been mentioned in
infections with Ankylostoma duodenale, which is the single best answer of choice.
“In individuals with chronic infection bile duct obstruction and biliary cirrhosis are infrequently demonstrated.
Ascaris (1160/1257)
“A large worm can enter and ocelude the biliary tree’.
Ankylostoma
Biliary obstruction has not been mentained even as a rare manifestation in ankylostoma infections (Hook worm)
Facts to Remember
Biliary (Hepatic) Flukes include ‘Cholangio-carcinoma® has been reported with
‘© Clonorchis (Sinensis) * Clonorchis Sinensis®
© Opithorchis® (Viverrini, Felineus) © Opithorchs Viverrini®
+ Fasciola (Hepatica, Gigantica)
PHARMACOLOGY
72. Answer is A (Therapeutic Efficacy) : Katzung 10/69, 70, 71 Goodman & Gillman 10"/60
Phase I1 in clinical drug trials is done to study the drug kinetics and metabolism and to establish its Therapeutic
Efficacy and Dose range
2B.
‘AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008 © 245
Phase 1 Phase re
(Open label/Non Blind) —_(Single ‘Double Blind). \
Normal volunteers Selected patients — Patients given drug for
Special populations (renal patient therapy
and hepatic impairment)
Why)” Human Pharmacology.& Therapeutic Exploration & "Therapeutic confirmation "Post marketing
Safety Dseranging ‘and comparison ‘suneillance
Safety, biological effects, Therapeutic efficacy, dose Confirm safety and efficacy Adverse reactions,
metabolism, kinetics, dug range, kinetics, metabolism Establish value of drug in patterns of drug
interactions relation to existing therapy —tilization, additional
Heel cod
BE Rea ieaa aaa Bs eae
Ethical Approval is not required for phase IV of clinical testing®.
PRECLINICAL TESTING
Studies in vio Animal Short 1.5 yeas
Testing Tom Long Goceage 26 eam)
Term
FDA30day
Safety Review
Who? Nomal volunteers, pil popsltions
(ronal and hepatic impairment
Wy? Sty, lel efit metabolism
nets, ru ineratons.
5y whom Clink pharmaco
Piast
Who! sect patints 1
‘Why? Therapeutic efficacy, dose range, |{
‘Bnet, metabolism i
By whom? Cie pharmacalogssand ff]
‘ial vets 4
3 i
i
aaa CUIICALTESTING [12
z
20 years
(verge 56 yeas)
‘Who? Large sample of selected patient
Why? Safely and efficacy
By whom? Cla investigator:
NDA Submision
2 months -7 yes
(Areage 26 yea)
= NDA Approved
POSTMARKETING SURVEILLANCE mas
PHASES
Who? Patients given drug for therapy
patterns of drug
tional indications
‘By whom? All physicians.
Answer is A (Safety): KDT 9/55; Lippincott's Pharmacology 3 /33
Therapeutic index is a measure of a drug’s safety - Lippincott's /KDT
‘Therapeutic index
+ Therapeutic index of a drug isthe ratio of the [Therapeutic index (TD)= 22%
dose that produces toxicity to the dose that EDSO
luces a clinically desired or effect
population
‘© The therapeutic index is a measure of a drug's ED 50 Dose that produces a desired effect in half the
safety population
‘© A llarge value indicates that there is a wide
‘margin between doses that are effective and
doses that are toxic.
246 © AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
Therapeutic Range
Therapeutic Range refers to the range that binds
the dose which produces the minimal therapeutic
effect and the dose that produces maximal
acceptable adverse effect
* Therapeutic range is also a measure of the
— drug's safety
+ A wider therapeutic range indicates a ‘safer’
drug
Answer is C (Potency) : KDT 9"/57; Katzung 10"/28
The concentration of drug that produces fifty percent of that drug's maximum effect is called ECSO or EDSO. This is
a measure of the potency of that drug
Potency of a drug
‘© Potency of drug refers to the amount (dose) of a drug needed
to produce a certain therapeutic effect.
‘© Itis measured by plotting the Dose Response curve (DRC) for
the concerned drug and the desired therapeutic effect.
© Potency is then defined as the concentration (ECS0) or
dose(EDS0) of a drug required to produce 50% of that drugs
Percentage of maximal effect
‘maximal therapeutic effect.
© The position of *ED50° on the dose axis of DRC determines
its potency.
© The furthur right ward the EDS0 is located the lower is its
oe ss The ECS0 is the concentration of the drug that
produces a response equal to fifty percent of the
‘maximal response. (Potency )
The smaller the EC50 the more potent the drug.
Drug A is more potent then Drug B
Efficacy of a drug
Ene (A)
‘© Efficacy ofa drug is refers to the maximal response that can i —= Eaux (Drug A)
be elicited by that drug 3
* This is also measured by plotting the dose response curve i
(DRC) for the concerned drug and the desired therapeutic Response | &
effect 3
‘© Efficacy is then defined as the maximal response achieved by 3
that drug on the response axis (upper limit of the DRC) and is 3
indicated as Emax =
© The height of the DRC curve de fficacy.
een permeate Emax is the maximum response produced by the
‘© The lower the height (limit) ofthe curve the lower is its ‘drug (efficacy).
efficacy (Emax) The larger the Emax the higher the efficacy.
Drug A has higher efficacy than Drug B.
5.
‘AIPGME EXAMINATION ANSWERS AND EXPLANATIONS ~ 2008 «
.eview of questions on potency and efficacy of dru
7
other
and efficacies of dru
Drug B is less potent but equally efficacious as Drug A.
Drug C is less potent and less efficacious than Drug B.
Drug D is more potent than Drug A, B & C but less
efficacious than drugs A & B and equally efficacious as
Drug
ive to each
Percentage of maximal effect
Answer is B (Reactivation of Cholinesterase) : KDT 9°/111
Pralidoxime is a cholinesterase reactivator used in anticholinesterase poisoning - KDT 6/105
Anticholinesterase Poisoning and Pralidoxime
‘+ Anticholinesterases are agents which inhibit the enzyme cholinesterase
(Cholinesterase is responsible for removing ACH by hydrolysis)
‘© Anticholinesterases thus protect ACH from hydrolysis and produce cholinergic effects
‘© _Anticholinesterase poisoning results from excessive exposure to these anticholinesterases and clinical
manifestations include effects of cholinergic stimulation
Anticholinesterases
Dyflos
Echothiophate
Parathion,
Malathion
Diazenon
Tabum
Sarin
Somun
# Physostigmine
© Neostigmene
© Pyridostigmine
# Edrophonium
+ Rivastigmine
* Galontamine
Irreversible
© Carbaryl (sevin)
‘+ _Propoxur (Baygon)
‘© Specific Antidotes to Anticholinesterase poisoning include Atropine & Cholinesterase Reactivators (Pralidoxime)
Le
Atropine
Atropine serves as an antidote for
anticholinesterase poisoning with
both organophasphates and
‘carbamates
Atropine however does not
reverse the peripheral muscular
paralysis? in Anti CHE
poisoning which isa nicotinic
action
es Cholinesterase Reactivators (Pralidoximey)
+ These serve as Antidotes, but only to anticholinesterase poisoning
‘with organophosphates?
+ These are ineffective as antidotes to anticholinesterase poisoning
with carbamates?
Infact ‘oximes’ (pralidoxime) are contraindicated in
anticholinsterase poisoning due to carbamates® as these do not
reactivate the carbamylated enzyme and may infact worsen the
condition due to a weak anti- CHE activity of their own
AIPGMEE 2008 - EXPLANATIONS
248 © AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
16.
71.
Answer is B (Urinary Retention): KD 9"/ 13-116
Ipratropium bromide is an anticholinergic agent. Anlicholinergic agents promote urinary retention and hence are
contraindicated in cases of urinary retention, Although Ipratropium bromide is poorly absorbed into the circulation
and its systemic effect (including urinary retention) are not prominent, it should still not be used when urinary retention
is an obvious presentation. Urinary retention isthe single best answer amongst the options provided.
mucus and hence
is not contraindicated in peptic ulcer disease
ds apg tere any masked be on Blood area
Cause bronchodilation®, Lacrimal secrition® Tachycardia |_| stimulant action
specially in patients with May cause Dry eye® Used for ~ Stimulates many
COPDY and Asthma treatment of ‘medullary centres
GIT (Oral cavity 3 (vagal, vasomotor,
Relieve smooth muscle spasm®™ | || Sativa secretion® They are more effective in COPD than bronchial asthma’
Bronchial Asthma! They are better suited for regular prophylactic use than for control of an acute attack
copp® Inhaled, spium are the bronchodilators of choice in COPD wxore*222)
‘© These agents are not absorbed (poorly absorbed) from the lungs and GIT and hence systemic anticholinergic side
effects are rare.
78.
1.
|AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008 * 249
Answer is D (Tiotropium) : Katzung 10/15 KDT 9"/117; The Overactive Bladder by kredger (2007) /127
Tiotropium is an anticholinergic used as an inhalational drug in asthma and COPD.
Itis poorty absorbed from the lungs and GIT and systemic effects including relaxant effects on the bladder are
‘minimal. Tiotropium bromide has not been used for urinary disorders.
Oxybutynin, Tolterodine and Darifenacin and are vesicoselective (Bladder selective) antimuscaranic agents with high
selectivity for m3 receptors and may be used to relieve bladder spasm (urinary spasm) after urologic procedures.
Oxybutynin (Ditropan)
Tolterodine (Betrol)
Flavoxate (Urispas)
Darifenacin
Solifenacin
Trospiuun isan unselectve antagonist thai has also been approved
Atropine has also been used, but it causes other anticholinergic side effects
Dicylomine and Imipramine may also be used as they have strong antimuscaranie actions.
Propantheline has also been used.
Anticholinergics for urinary disorders
‘©The human urinary bladder predominantly shows M2 and M3 muscaranic receptors
‘* The M3 subtype mediates direct contraction of the bladder
(The M2 subtype acts indirectly by inhibiting relaxation by Non epinephrine & Epinephrine)
Selective M3 receptor antagonists (Anticholinergics with selectivity for M3 receptors) may thus be used to relieve
urinary disorders such as
Bladder spasms (Bladder spasm is common after urological procedures like TURP)
Urinary urgency / incontinance
Answer is C (Ischaemic Heart Disease) : Katzung 10*/274; KDT 9"/176
Ergotamine is a vosoconstrictive agent (used most commonly for aborting migraine headaches. Vasoconstriction
induced by Ergotomine is usually severe and prolonged and difficult to reverse. They are therefore contraindicated
in Ischaemic Heart Disease
Ergotamine
Obstructive Vascular Disease 1. Migraine (Major indication) | | Ergotamine / dihydroergotamine
= Ischaemic heart disease 2. Postpartum Haemorthage Ergonovine (Ergometrine)
- Peripheral Vascular Diasease (May be used) Dihydroergotoxine
itraindications (Relative) [ses of other Ergot alkaloids | | Bromocriptine
‘* Pregnancy Hyperprolactine ISD
© Hypertension (Bromocritine) Methyl sergide
‘© Liver and kidney disease + Senile cerebral insufficiency
Sepsis (Dihydroergotoxine)
There is no evidence that ordinary » Postpartum Haemorrhage
use of ergotamine for migraine in (Ergonovine) .
Ppregrancy is hazardous, However + Diagnosis of variant angina
‘most clinicians counsel restraint in (Ergonovine)
the use of ergot drivatives by
| pregnant patients (Katzung) _
Answer is B (Binds estrogen receptors and prevents negative feedback at hypothalamus) ; KDT 9/312
Clomiphene citrate binds to both Estrogen receptors (ER a and fi) and acts as a pure estrogen antogonist, in all
human tissues. It induces Gn secretion in women by Blocking estrogenic feedback inhibition of pituitary. This
increases the amount of LH and FSH released at each secretory pulse ~ KDT 6"/303
250
2008 - EXPLANATIONS
pa
82.
‘© AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
reat _— . marae
© Clomiphine citrate is classified as an Antiestrogen®
Mechanism of Action Betis
© Pure estrogen antagonist at Estrogen Receptors (ER a and ERB )®
‘© Blocks estrogenic feed back inhibition of pitutary®
© Induces gonadotrophin secretion® and the amount of LH/FSH released at each secretory pulse
+ Promotes ovulation®
Use z
‘© Induction of ovulation for anovular infertility® (chief use)
‘+ May be used to aid in vitro fertilization (causes synchronous maturation of several ova)
‘+ May be used to promote spermatogenesis and testesterone secretion in males may be used for male
infertility?
Adverse effects
‘© Polycystic ovaries? © Hotflushes® — * ~— May increase risk of ovarian tumors
‘© Multiple pregnancy? Gastric upset. Vertigo /Allergic dermatitis
Answer is A (Diazepam antagonist) : KDT 9"/ 401;(Repeat) Katzume 10/354
Flumazenit is an antagonist for Benzodiazepines (Diazepam). It is an antagonist at the Benzodiazepine binding site
on the GABA receptors. It competes with Benzodiazepine agonists as well as inverse agonists and reverses their
depressent or stimulant effects respectively
‘Agonists GABA Receptors lL. Tnverse Agonists
Benzodiazipines i (BZD binding site) eg Beta carbolines
Facilitate GABA actions and| {| ve -ve}} Impede GABA actions and
produce CNS depressant produce CNS stimulant
actions Flumazenil actions
Competitive antagonist for
Agonists and Inverse Agonists
J+ Reverses CNS depressant action
of Agonists”
+ Reverses CNS stimulant action of
Inverse agonists®
Answer is A (Risperidone): KDT 9"/440-446
Risperidone is an antipsychotic drug and is not used as an antianxieety agent.
Selective Serotonin Reuptake Inhibitor (SSRL) are antidepressant agents but they are effectively used in many types of
severe generalized anxiety disorder (including OCD, Panic attack and Phobias)
Buspirone and Clonazepam (BZD) are classified as Antianxiety drugs.
Benzodiazepines Azapirones ‘Sedative Anthistaminie Beta Blockers
+ Diazepam Buspirone Hydroxyzine
+ Chlordiazepoxide Gepizone Propancol
+ Oxazepam Isapirone |
+ Lorazepam Selective Serotonin Reuptake Inhibitors |
+ Alprazolam [SSRI are effective in Obsessive
Compulsive disorders (OCD), phobias,
Soca wih ponand man pps ofseee
ominent antiepileptic ‘generalized anxiety disorders - KDT
H howev neg
action. It may however be |
used as an antianxiety agent.
‘AIPGME EXAMINATION ANSWERS AND EXPLANATIONS ~ 2008 251
83. Answer is C (Tetracycline) : KDT 9/689; Repeat
Tetracyclines act by inhibiting protein synthesis. They do not inhibit cell wall synthsis
Cephalosporins® (includes cefotetan)
Cyeloserine?
Vancomycin?
Bacitracin®
84. Answer is A (Piperacillin
KDT 9/724; Ref: Q-88 (Al -2006); Q 96 (AI -2004)
Piperaceltin is an antipseudomonal penicillin belonging to the group of ureidopenicillins
Oxycillin and Nafeillin are penicillinase resistant penicillin active against pencillinase producing bacteria. They are
however narrow spectrum penicillins, with activity primarily limited to Gram positive bacteria. They are not active
‘against pseudomones
Amoxgcillin is an extended spectrum penicillin with activity against many Gram negative bacteria but it is mot active
‘against pseudomonas.
Ey
Narrow spectrum penicillins Extended spectrum penicillins
Activity is limited primarily to Gram positive Activity is extended to include Gram negative
bacteria bacteria as well
‘Spectrum include: ‘Spectrum include:
‘Most gram positive bacteria ‘Most Gram positive bacteria
‘Most gram negative bacteria are Many Gram negative bacteria
not susceptible?
(Non Pseudomonal) ® Depending on whether the gram
negative spectrum includes
co—__| pseudomonas, these may be
Sait PSG further classified as follows.
susceptible Resistant
“Extended spectrum Extended spectrum
Penicillin G Methicillin penicillins not active penicillin active against
Penicillin V Cloxacillin against Pseudomonas Pseudomonas
Oxacillin (Non Pseudomonal) (Pseudomonal)
Dicloxacillin
Flucloxacillin + Ampiciltin + Carboxypenicillins
Nafeillin + Amoxyillin ~ Carbencillin
~ Tiearcillin
‘+ Ureido penicillins
~ Piperacillin
= Meclocillin
85. Answer is A (Can be given orally) : KDI 9/718
Penicillin G is acid labile and is destroyed by gastric acid. It can only be used parentrally and not by the oral route.
‘+ Penicillin G can not be given orally
Penicillin G is acid labile and is destroyed by gastric acid®
Iris not available for oral administration ©
Penicillin G can be is either intravenously or ‘cer
‘© Procaine Penicillin G ‘Crystalline Penicillin G or
‘+ Benzathine Penicillin G Sodium Penicillin G
(These penicillins release PnG slowly atthe
site of injection)
252. © AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
86.
Orally administered / Acid Resistant Penicllin similar to penicillin G is Penicllin V° or Phenoxymethyl penicillin
(differs from PnG only in that itis acid stable)
‘+ Penicillin G is primarily active against gram positive bacteri
PnG has a narrow spectrum of acti
- Itis primarily active against Gram positive bacteria® (Cocii® and Bacill®)
- Itis usually inactive against Gram negative bacili'
= Gram negative cocii are however usually sensitive® (Meningococet® & Gonococi®)
= Bacteriodes fragilis is resistant?
* Mycobacterium TB is resistan®®
- Rickettsia, chlamydia, protozoa, fungi, viruses are totally insensitive to PnG®
‘+ Penicillin G is a 8 Lactam antibiotic and mechanism of action involves interference with the synthesis of,
bacterial cell wall.
Pencillin G is sensitive to penicillinase or B Lactamase and | Lactamase producing bacteria inactivate PnG by
‘opening the 8 Lactam ring.
‘© Probenecid given along with PnG increases its duration of action
PnG is primarily excreted via the kidney by tubular secretion (90%)
Probenecid tends to block the tubular secretion of PnG
This results in higher and longer lasting plasma concentrations and increased duration of action.
(a) Answer is A (Resistance is produced as a result of alteration in Penicillin Binding Proteins): Katzung 10"/727
‘Methicillin Resistent Staph Aureus by Catterkey (1992) /22-25 Schaechter’s Mechanism of Microbial Disease 4"/60
Essentials of Diagnostic Microbiology by Shimeld & Rodgers (1999)/109; Current Critical Care Diagnosis &
Treatment (CCCDT) 2/426
Altered target Penicillin Binding Proteins (PBP) are the basis of Methicillin resistance in staphylococcii (MRSA)
~ Katzung
Resistance to methicillin occurs due to altered Penicillin Binding Proteins (PBP-2A).
This is transmitted via the MeC A gene. Mec A gene is a chromosomal gene (not a plasmid).
Expression of Resistance is enhanced by lowering temperatures to 535°C.
Most common mec! in Resistance to Antibacte nts
Yes ‘Hydrolysis of s Lactam ring by i-lactamase
he No Aeron n Pence a ea
fechanism of Microbial disease 4"%60
Resistance in MRSA results from altered Pencillin Binding Protein ~2 (PBP--
(Intrinsic Resistance due to PBP-2A and MeC-A gene)
+ Penicillin binding Proteins (PBP) are integral cell wall proteins that catalyze various reactions in cell wall synthesis
+ Beta Lactam antibiotics (Methicillin) bind to the enzymatic sites on these PBP and thereby disrupt bacterial cell wall
synthesis (Mechanism of action)
+ Methicillin Resistant strains of Staph, aureus (MRSA) escape Methicillin by synthesizing an extra PBP called PBP 2A
which carries out the functions of those PBP’s that are inactivated by methicillin
PBP-2A is also a Penicillin binding protein but itis only bound at extremely high concentrations of methicillin (or
other # lactam antibiotics) which lie well above the therapeutic range. Hence PBP-2A is not inactivated at therapeutic
doses.
«+ PBP-2 production is encoded on a gene called MeC A gene
‘+ MeC A gene transmits resistance chromosomally (and not via plasmids)
86.
[AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008 © 253
Possible mechanism (Border line Methicillin Resistance)
‘Hyperproduction of Beta Lactamase (Beta lactamase production is encoded by plasmids-plasmid mediated)
‘Hyperproduction of Beta lactamase can lead to Borderline Methicillin Resistance but this should not be
confused with true methicillin Resistance’ ~ Essentials of Diagnostic Microbiology by Shimeld & Rodgers (1999)/109
sistance is enhanc ‘the te ‘of incubation to less th ier than.
which is used routinely)
Although most MRSA are easy to identify by conventional susceptibility testing, some isolates (heteroresistance) with
low level resistance may be difficult to identify. Such samples require special conditions of incubation that enhance
phenolypic expression of resi
Factors which enhance phenotypic expression OF ‘National commitiee for Clinical Laboratory Standards
Resistance in MRSA (NCCLS) Guidelines
* Reduced Temperature of incubation (<35°C Guidelines for susceptibility testine in MRSA.
rather than 38°C 10 37°C)
Prolonged incubation (>24 hours) fe 2s ome nee
Increasing the amount of inoculum * Use a salt supplemented medium
‘© Addition of sodium chloride (2-4%) to the solid © Temperature of incubation no higher than 35°
susceptibility medium
(b) Answer is C (Resistance is primarily mediated via plasmids)
Resistance is not primarily mediated via plasmids
Resistance is primarily mediated via chromosomal MeC-A gene which codes for altered PBP ~ 2A. Borderline
resistance to methicillin may be produced as a result of hyper production of Beta Lactamases, but this is not the
‘Primary mechanism, Low resistance to MRSA (heteroresistance) may be missed at 37°C and temperature of incubation
‘no higher than 35°C is recommended - Refer previous question for references
Answer is D (Are not known to be teratogenic): KDT 9/736; Katzung 10/748
Tetracyclins are known to have teratogenic effects. Tetracycline use during pregnancy may cause dental enamel
dysplasia and bony deformities in the child
‘Tetracveline and its use in pregnane ih
* Tetracyclines should not be used in pregnancy, lactation and in children
© Tetracycline have chelating property and therefore can bind to calcium deposited in newly formed Bone & Teeth
Effect on Teeth Effect on Bone mA
Deposited on fetal teeth (deciduous teeth) Deposited in bone, itcan cause bony
leading to fluoresence, brown discolouration, deformities and growth supression
‘enamel dysplasia and illformed teeth that are (Teratogenic effect)
‘more susceptible o caries (Teratogenic effect)
‘Prolonged use in children < 8 years of age may result in similar changes as described above and
hence Tetracyclines are considered contraindicated for use in young children (< 8years)
rr damage (May precipitate Acute hepatic Necrosis in pregnancy)’
* Kidney damage (May produce Fanconi syndrome®)
(Tetracycline which does not enhance renal failure® ~ Doxycycline)
‘Vestibular Toxicity (Transient, ataxia, vertigo, nystagmus) 2
Phototoxicity (sunburn like rash)?
Teeth damage (Discolouration, enamel dysplasia) ®
Bene damage (Growth supression & deformities) ®
Diabetes insipidus (Demeclocycline antagonizes ADH action & causes diabetes insipidus.?
(Has been used therapeutically for Syndrome of Inappropriate ADH secretion ®)
© Antianabolic effect
‘254 © AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008,
89.
90.
Increased intracranial pressure (noted in some infants)
Hypersensitivity
‘Superinfection : -Tetracyelines are the most common antibiotics responsible for superinfection?
= Intestinal superinfection with candida albicans is most prominent ©
- Pseudomemiranous colitis may occur
+ Imitative effects: (Not dose related)
= Initative diarrhea (also, nausea, vomiting)
= Iritative esophageal ulceration and epigastic pain
= _ Pain on intramuscular injection & thrombophlebitis of injected vein
Answer is D (Doxycycline): KDT 9"/735, 736
Doxycycline is metabolized and excreted via the liver in bile, It is not excreted via the kidney and is not considered
Nephrotoxic
‘All tetracyclines except doxycycline accumulate and enhance renal failure’ - KDT 6""/ 713
‘+ Aminogivcosides (Gentamycin and Strepte
Alll Aminoglycosides are considered nephrotoxic (KDT 6/721)
‘Note
Streptomycin is the least nephrotoxic aminoglycoside antibiotic. (but it is nephrotoxic)
Nephrotoxicity caused by aminoglycosides is essentially reversible® (provided the drug is promptly discontinued)
+ Totracvelines
‘All tetracyclines are nephrotoxic except Doxycycline (KDT 6"/713)
© Polvmixin B
Polymyxins have high systemic toxicity when used parentrally. Systemic toxicity includes marked kidney damage
(Nephrotoxicity) - KDT 6°/734
Answer is A (Erythromycin): Park 18/104, Park 19"/106, Harrison 17/893.
The options for chemoprophylaxis of diphtheria include. Erythromycin (7-10 days oral course) or Benzathine
Penicillin G (single intramucular dose)
‘Chemoprophylaxis for Diphtheris
‘© Close contacts of dephtheria cases should undergo throat cultures to determine whether they are carriers.
‘* After samples for throat cultures are obtained, antimicrobial prophylaxis should be considered for all close contacts
‘even those who are culture negative?
Options include
* Oral course of Erythromycin for 7-10 days
© One dose of LM Benzathine Penicilline G
(1.2 Million units for person > 6 years; 600,000 units for children <6 years)
‘Chemoprophylaxis for common diseases (Park 19°/106)
Powel “Tetracycline? oF Furazolidone (for household contacts) NNN
Bacterial Conjunctivitis Erythromycin ophthalmic ointment
Diptheria Erythromycin®
(Also initiate first dose of vaccine)
Influenza A Amantadine® (for contacts suffering from chronic diseases),
Meningococcal meningitis ‘Sulphadiazine® (for house-hold and close community contacts),
(Also initiate immunization against serogroups A & C)
Pneumonic Plague Tetracycline®
Answer is A (Amikacin): Harrisons 179/959.
Amikacin is not used in the treatment of Enteric fever.
Ciprofloxacin is the drug of choice for Enteric fever, Cotrimaxazole is an alternative agent for treatment of Enteric
“fever and Ceftriaxone is used for treatment of multidrug resistant enteric fever
a1.
92.
‘AIPGME EXAMINATION ANSWERS AND EXPLANATIONS 2008 © 255
© Amoxyeillin (second line)
© Chloramphenicol
© Cotrimaxazole
Azithromycin
* Ceftriaxone * Ciprofloxacin (DOO)
© Azithromycin © Amoxyeillin (second choice) «
© Chloromphenicol
* — Cotrimaxazole
Answer is B (Procaine Penicillin G) : Harrison's 16%/983 ; Harrison's 17/1044
Procaine Penicillin G is the alternative agent of choice and the single best answer amongst the options provided.
Ceftriaxone (or other third generation cephalosporins)
+ Ciprofloxacin
Ceftriaxone
© Azithromycin
é
3
The drug of choice for treatment of Neurosyphillis is Acqueous or Crystalline Penicillin G. |
Patients with confirmed Penicilin Allergy
tent infected with HIV:
a EINE pincer ARE
Primary, Secondary or Penicillin G benzathine Tetracycline hydrochloride or doxycyetine
Early latent
Late latent (or uncertain duration) Ev F after Lumbar puncture Evaluate CSF after Lumbar puncture
peciomncie. oF CSE normal: Penicilin G benzathine CSF normal and patient not infected with HIV:
ee CCSE abnormal: Treat as neurosyphilis Tetracycline hydrochloride
(CSF normal and
Desensitization and treatment with penicillin if
compliance cannot be ensured
CSF abnormal: Treat as neurosyphils
‘Neurosyphils Aqueous peniclilin G or Desensitization and treatment with penicillin
(asymptomatic or symptomatic) Aqueous penicillin G Procaine plus
probenecid
‘Syphilis in pregnancy ‘According to stage Desensitization and treatment with penicillin
Answer is D (Clofazimine) : KDT 9'/781-782, 787; Kateung 10/772, 779
Clofazimine is not an antifungal drug. It
Mycobacterium Tuberculosis (Katzung)
in antibacterial drug active against Mycobacterium Leprae and
“Antifungal Drugs
T
T T 1
+ Griesofulvin
+ Miconazole
* Oriconazole
+ Ketoconazole
(Systemic)
Antibiotics Antimetabolites Azoles Allylamines Other Topical Agents
Polyenes Flucytosine (SFC) Triazoles (systemic) + Terbinafine + Tolnftate
+ Amphoterecin B + Fluconazole + Natifne + Undecylenic acid
+ Nystatin + Itraconazole + Ciclopiroxolamine
+ Hamycin + Vonconazole + Quinodochlor
+ Natamycin (Pimaricin) Imidazoles (Topical) + Benzoic acid
+ Clotrimazole + Butenafine
Heterocyclic Benzofuran + Econazole + Sodium Thiosulphate
256 © AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
93.
95.
Answer is A (Bleomycin): KDT 9°/898, 689; Katzung 10" /895
Bleomycin is a small peptide (glycopeptide) antibiotic with potent antineoplastic activity (katzung /KDT)
Bleomycin is a small peptide (glycopeptide) with antineoplastic activi
Doxorubicin is an ‘anthracycline’ with antineoplastic activity
L-Asparginase is an enzyme with antineoplastic activity (enzymes are proteins)
Yalinomycin is a Depsipeptide antibiotic but no clinical application has yet been described for valinomycin
(Experimental drug) (Reference Dictionary of Antibiotics and Related substances)
Glycopeptide Antibiotics
Polymyxin B
Colistin
Bacitracin
Tyrothricin
Answer is D (Stabilization of tubules) : KDT 9°/865-866
Paclitaxel acts by Stabilization of microtubules.
‘Mechanism of action of Taxanes (Paclitaxel / Docetaxel)
‘© Tubulin isa protein found in microtubules within cells,
‘+ Paclitaxel emhaces polymerization of tubulin which results in the stabilization of microtubules
‘© This stability in tum results in inhibition of normal dynamic reorganization of the microtubular network which is,
essential for vital interphase and mitotic functions
‘© Taxanes thus exert their anticancer actions by acting as mitotic inhibitors
‘Anticancer drugs that act as mitotic inhibitors” include Vinca Alkaloids and Taxanes
|Amticancer drugs that act by inkibition of microtubules (tubulin): Vince Alkaloids (Vincristine/Vinblastin) ©
|Anticancer drugs that act by stabilization of microtubules (tubulin): Taxanes (Paclitaxel /Docataxel)®
Answer is A (Methotrexate): KDT 9"/611; Lippincott’sPharmacology 3/458
Leucoverin or Folinic
cid is used with Methotrexate to counteract its toxicity
Methotrexate Toxicity : Mechanism ter Reducing Methotrexate toxicity:
‘ton (Leucoverin Rescue
‘¢ Methotrexate exerts its antineoplastic {
and immuno — suptessant action by
acting as an antagonist to Folic acid
(DHFRase) the enzyme that converts
folic acid into its active coenzyme
‘The cells can be rescued by two
Mechanisms
This requires a thousand
{oem tetatiydrofoate (FE) fold excess ofthe natural
# FHS isan essential coenzyme substrate Dihydrofolate
required for de novo purine synthesis (FH2) (Not practical)
(Adenine, Guanine, Thymidine) and
amino acid interconversions
(Methionine / Serine)
[Required for one Carbon transfer
reactions]
This requires administration
This leads to depressed DNA, RNA of Folinic acid or
and protein synthesis and ultimately Teucoverin (NS Formyl
to cel death, (Mechanism of action) ‘Leucovorin rescue FH) (Cirrovorum factor)
Tey. netnone
96.
97.
/AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008 ¢ 257
Answer is B (Hirsuitism): Harrisons 17/1987
Tacrolimus does not cause hirsuitism or gingival hyperplasia - Harrison's 17"/ 1987
Tacrolimus and Cyclosporine
# Tacrolimus (FK506) is a macrolide lactone antibiotic that is isolated from a Japanese fungus streptomyces
tsukubaensis and has immunosupressant properties.
‘© Ithas the same mechanism of action as cyclosporin but is chemically different
‘Chemically a macrolide lactone antibiotic ‘© Chemically different
“Mechanism of action same as cyclosporin © Caleineurin inhibitor
Cateineurin inhibitor
‘* More potent action than cyclosporin * Less potent
(10-100 times more potent)
‘© Oral absorption of Tacrolimus is more predictable than,
ral absorption less predictable
AIPGMEE 2008 - EXPLANATI
cyclosporine
* Primarily used for prevention & treatment of Graft ‘¢ Primarily used for prevention and treatment of
rejection Initially used for ‘rescue’ therapy for patients in _graft rejection.
‘whom rejection occurred despite the use of cyclosporine Still continues to be the most commonly used
(Now tacrolimus is beginning to replace cyclosporine for _—_drug for prevention and treatment of graft
primary immunosupression in many transplant centres) rejections (but trend is shifting towards use of
tacrolimus)
‘© Overall more toxie than eyclosp © Overall ess toxic than tacrolimus
= More Nephrotoxie (Dose it ‘Less Nephrotoxic (Dose limiting toxicity)
- More Neurotoxic = Less neurotoxic
(Tremor, Seizures, Hallucinations & Coma)
~ More likely to precipitate Diabetes ~ Less likely 10 precipitate Diabetes
= More likely to cause Alopecia / Diarrhea ~ Less likely 10 cause Alopecia / Diarrhea
Certain adverse effects are less prominent /absent Certain adverse effects are more
= Hirsuitism (Absent according to H17th) Prominent 00
= Gum Hyperplasia (Absent; H-17") > Hirsuitism
= Hypertension = Gum Hyperplasia
= Hypertension
Answer is B (Imiquimod): Katzung 10/816, 817, 996
Imiquimod is an immunomodulator shown to be effective in the treatment of external genital and perianal warts,
— Katzung 10/816
‘© Imiquimod is an immune response modifier or immunomodulator agent
‘© Ithas been approved forthe treatment of :
+ External genital and perianal warts in adults?
+ Actinic keratosis on the face & scalp
+ Superficial Basal cell carcnoma on trunk neck & extremities
‘+ The mechanism of action is unknown but is thought to be due to
~ Stimulation of peripheral mononuclear cells to release IFN
= Stimulation of macrophages to release IL-1, IL-6, IL-8 and TNF-a
‘© Iisavailable as an agent for Topical Application (Percutaneous absorption is minimal)
Adverse side effects consist mainly of local inflammatory reactions including pruritis, erythema and superficial
erosions
258. © AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
98. Answer is A (Cytochrome oxidase) : Godman & Gillman 11/44; Harper 27633
Cytochrome oxidase is not mentioned as an enzyme in the metabolism of xenobiotics,
Cytochrome P450 and Hydroxylation reactions are involved in Phase ~1 metabolic reactions while Methylation forms
Part of phase Il reactions during metabolism of xenobiotics.
‘Xenobiotics and Their Metabolism
* Xenobiotics refer to all compounds that are foreign to the body. These include a variety of compounds such as drugs,
‘chemical carcinogens, insecticides ete.
‘* These compounds are usually metabolized in the human body before being excreted
‘© Several different enzymes (atleast 30) catalyze reactions involved in the metabolism of these xenobiotics
+ The purpose of metabolism is to increase their water solubility (polarity) and thus enhance their excretion from the body
‘+ The metabolsm of Xenobioties is best described in two phase
‘© Inphase I the xenobiotics undergoes their first
‘metabolic biochemical reactions
© The major reaction is Hydroxylation.
‘Hydroxylation is catalyzed by members of a
‘group of enzymes called monooxygenases or
cytochrome P450's
* Hydroxylation may terminate the action ofthe
xenobiotic or the metabolized xenobiotic may
enter phase II of metabolism
‘© Inphase II the hydroxylated or other compounds
produced in phase I are converted into various polar
‘metabolites
‘+ The major reactions in phase II metabolism include
= Conjugation (with glucoronic acid, sulphate,
acetate, glutathione or certain amino acids) and
- Methylation
‘+ These reactions tend to increase the polarity or
‘water solubility of xenobiotics to aid in their
excretion from the body.
[BiSiobiotic Metabotizing Enzymes
Enzymes Reactions
Phase I “oxygenases” Reactions
Cytochrome P450s (P450 or CYP)
Flavin —containing monoxygenases (FMO)
Epoxide hydrolases (mEH. sEH)
Phase 2 ‘transferases’
Sulfotransferases (SULT)
‘UDP - glucuronosyltransferases (UGT)
Glutathione ~ S-transferases (GST)
1N-acetyltransferases (NAT)
‘Methyltransferase (MT)
Other enzymes
Alcohol dehydrogenases
Aldehyde dehydrogenases
NADPH -quinone oxidoreductase (NQO)
FORENSIC
Hydroxylation® / C and O oxidation, dealkylation, others
N, Sand P oxidation
Hydrolysis® of epoxides
Reactions
Addition of sulfate (Sulfation)
Addition of glucuronic acid (Glucuroindation)
Addition of glutathione (Glutathione Conjugation
Addition of acetyl group (Acetylation)
Addition of Methyl group (Methylation)
Reactions
Reduction of alcohols
Reduction of aldehydes
Reduction of quinines
99. Answer is D (Throttling) : Reddy 27/312, 229, 315, 317, 318, Parikh 6 /3.57, 3.40-3.62
Suffocation is a form of asphyxia where death occurs primarily due to mechanical obstruction to the passage of air into
respiratory tract other than constriction of neck or drowning
Throttling involves compression of neck by human hands, and is a form of strangulation (and not suffocation)
Death from throtling occurs due to occlusion of carotid arteries. Occlusion of airways plays a minor role.
— Reddy 27/312.
|AIPGME EXAMINATION ANSWERS AND EXPLANATIONS - 2008
259
Hanging
Hanging is a form of death
that results from constriction
of neck by a ligature and
suspension of the body. The
weight of the body acts as
the constricting force.
‘Asphyxial Deaths
a
Suffocation
Strangulation
‘Strangulation is a form of
asphyxia that result from
constriction of neck by any
‘means without suspending
Asphyxia
Hlanging is not a form of
strangulation
(Complete weight ofthe
body is not essential Weight
of the head alone may be
sufficient)
Suffocation is a form of
deprivation of oxygen in the
‘environment or from
Drowning
Drowning is a form
of Asphyxia in
which access of air
into the lungs
that results from
the body obstruction of air passages prevented by
by means other than submersion of the
‘Sirangulation does not | constriction of neck or body in water or
include hanging drowning other fluid medium
mae (Complete
‘Strangulation Suffocation does not submersion is not
"+ Ligature Strangilation
+ Throtting (Manual
include drowning or
constriction of neck
necessary, sufficient
fluid to cover the
strangulation with hands)
+ Mugging Suffocation is sufficient to cause
+ Garrotting + Smothering drowning)
+ Bansdola + Gagging
+ Choking
+ Overlaying
+ Burking
Traumatic Asphyxi
nostrils and mouth
100. Answer is A (Strangulation) : Reddy 27/311, Parikh 6"/ 3.53
Bruising of neck muscles, fracture of thyroid cartilage and hyoid bone are more common in Strangulation than in
Hanging. Strangulation is the single best answer of choice
Ligature Mark
"Abrasions and ecchymoses
{about the edges of ligature mark)
Bruising of Neck Muscles
‘Neck
‘Subcutaneous tissues
‘Hyoid bone fracture
Thyroid cartilage fracture
Larynx and Trachea
Emphysematous bullae
‘Carotid arteries
Face
Signs of asphyxia
Tongue
(Saliva
Bleeding from nose, mouth & ears
([Seminal fui at glans
5 =
Itis oblique
Does not completely encircle the neck;
Usually seen high up in the neck between
the chin and larynx,
‘The base is pale, hard & parchment-like
Not common
Less common
Stretched and elongated
White, hard & glistening under the mark
[Not present on the surface ofthe lungs
Damage may be seen
Usually pale & petchiae are not common
Extemnal signs less marked
‘Swelling and protrusion is less marked
Often runs out of mouth
‘Not common
More common
eiliGa SRO
Itis transverse,
Usually completely encircling the neck
Usually seen below the thyroid cartilage
‘The base is soft and reddish,
Common
More common
[Not stretched or elongated
Ecchymosed under the mark
‘May occur
(Not rare in manual Strangulation/ Throttling)
‘More common
Fracture may be found
Very common on the surface of the lungs
Damage is rare
Congested, livid and marked with petechiae
External signs well marked
‘Swelling and protrusion is more marked.
Absent
Common
Less common
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Mudit Khanna AIPGMEE 2015-16 QuestionsDocument21 paginiMudit Khanna AIPGMEE 2015-16 QuestionsAbdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2015-16 Answers 1-99Document66 paginiMudit Khanna AIPGMEE 2015-16 Answers 1-99Abdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2011 Answers 200-300Document55 paginiMudit Khanna AIPGMEE 2011 Answers 200-300Abdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2011 Answers 1-101Document59 paginiMudit Khanna AIPGMEE 2011 Answers 1-101Abdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2012 Answers 199-300Document57 paginiMudit Khanna AIPGMEE 2012 Answers 199-300Abdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2013-14 Answers 200-300Document43 paginiMudit Khanna AIPGMEE 2013-14 Answers 200-300Abdullah AbdulRahman100% (1)
- Mudit Khanna AIPGMEE 2013-14 Answers 1-99Document57 paginiMudit Khanna AIPGMEE 2013-14 Answers 1-99Abdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2015-16 Answers 100-199Document63 paginiMudit Khanna AIPGMEE 2015-16 Answers 100-199Abdullah AbdulRahman100% (1)
- Mudit Khanna AIPGMEE 2011 Answers 102-199Document58 paginiMudit Khanna AIPGMEE 2011 Answers 102-199Abdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2013-14 Answers 100-199Document55 paginiMudit Khanna AIPGMEE 2013-14 Answers 100-199Abdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2012 Answers 100-198Document62 paginiMudit Khanna AIPGMEE 2012 Answers 100-198Abdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2011 QuestionsDocument24 paginiMudit Khanna AIPGMEE 2011 QuestionsAbdullah AbdulRahman33% (3)
- Mudit Khanna AIPGMEE 2010 Answers 201-300Document62 paginiMudit Khanna AIPGMEE 2010 Answers 201-300Abdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2013-14 QuestionsDocument22 paginiMudit Khanna AIPGMEE 2013-14 QuestionsAbdullah AbdulRahman100% (1)
- Mudit Khanna AIPGMEE 2010 QuestionsDocument24 paginiMudit Khanna AIPGMEE 2010 QuestionsAbdullah AbdulRahman67% (3)
- Mudit Khanna AIPGMEE 2008 Answers 100-200Document56 paginiMudit Khanna AIPGMEE 2008 Answers 100-200Abdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2012 QuestionsDocument24 paginiMudit Khanna AIPGMEE 2012 QuestionsAbdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2012 Answers 1-99Document63 paginiMudit Khanna AIPGMEE 2012 Answers 1-99Abdullah AbdulRahman100% (1)
- Mudit Khanna AIPGMEE 2015-16 Answers 200-300Document58 paginiMudit Khanna AIPGMEE 2015-16 Answers 200-300Abdullah AbdulRahman100% (1)
- Mudit Khanna AIPGMEE 2010 Answers 1-99Document59 paginiMudit Khanna AIPGMEE 2010 Answers 1-99Abdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2009 QuestionsDocument21 paginiMudit Khanna AIPGMEE 2009 QuestionsAbdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2010 Answers 100-201Document54 paginiMudit Khanna AIPGMEE 2010 Answers 100-201Abdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2009 Answers 200-300Document52 paginiMudit Khanna AIPGMEE 2009 Answers 200-300Abdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2008 Answers 201-300Document58 paginiMudit Khanna AIPGMEE 2008 Answers 201-300Abdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2007 Answers 100-201Document48 paginiMudit Khanna AIPGMEE 2007 Answers 100-201Abdullah AbdulRahman100% (1)
- Mudit Khanna AIPGMEE 2009 Answers 101-199Document48 paginiMudit Khanna AIPGMEE 2009 Answers 101-199Abdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2009 Answers 1-100Document58 paginiMudit Khanna AIPGMEE 2009 Answers 1-100Abdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2006 Answers 199-300Document36 paginiMudit Khanna AIPGMEE 2006 Answers 199-300Abdullah AbdulRahmanÎncă nu există evaluări
- Mudit Khanna AIPGMEE 2008 QuestionsDocument21 paginiMudit Khanna AIPGMEE 2008 QuestionsAbdullah AbdulRahmanÎncă nu există evaluări