Documente Academic
Documente Profesional
Documente Cultură
Jurnal
Încărcat de
Laras Asri FatahaniTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Jurnal
Încărcat de
Laras Asri FatahaniDrepturi de autor:
Formate disponibile
Otolaryngology: Open Access Sami et al.
, Otolaryngol (Sunnyvale) 2017, 7:1
DOI: 10.4172/2161-119X.1000294
Research Article OMICS International
Response to Combination Intranasal Corticosteroid and Intranasal Antihistamine
in Allergic Rhinitis, A Questionnaire Based Study in ENT Outpatients
Amtul Salam Sami1*, Sabahat Ahmed2, Nida Ahmed3
1Department of ENT and Allergy, University Hospital Lewisham, Lewisham and Greenwich NHS Trust, UK
2GKT School of Medicine, Kings College, UK
3London North West Healthcare NHS Trust, UK
*Corresponding author: Amtul Salam Sami, MBBS, BSc, ODTC, MCPS, MA, M.Sc., Department of ENT and Allergy, University Hospital Lewisham, Lewisham and
Greenwich NHS Trust, UK, Tel: 020 7474 2595; E-mail: amtul_salam@hotmail.com
Received date: February 02, 2017; Accepted date: February 21, 2017; Published date: February 28, 2017
Copyright: 2017 Sami AS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim: To analyse the effect of combination intranasal corticosteroid and antihistamine spray in patients suffering
from proven Allergic Rhinitis who have failed primary care therapy.
Background: Allergic Rhinitis is prevalent in the community and worldwide, with a rising trend, it also impacts on
health related quality of life, sleep and (in appropriate age groups) school attendance.
Method: The MSNOT-20 is a validated and reliable questionnaire for use in Rhinitis. It was used in two 4 month
periods (2014 and 2016) in patients with Allergic Rhinitis who have failed primary care treatment. They were then
commenced on a combination nasal spray of azelastine hydrochloride (antihistamine) and fluticasone propionate
(corticosteroid).
Results: There was improvement in overall symptom severity score (MSNOT-20 score) for each patient, with
improvement in all five subgroups; nasal, paranasal, sleep, social and emotional. The MSNOT-20 score is closely
correlated with sleep, social and paranasal subgroups. The top 5 most severe symptoms identified by MSNOT-20
questionnaire objectively were also identified by patients as their most troublesome symptoms and include (in
descending order); blocked nose, need to blow nose, sneezing, runny nose, post nasal discharge.
Conclusion: Allergic rhinitis has widespread impact on different domains of the patients life. This combination
treatment is an effective treatment regime for patients who have failed primary care and has been proven to be of
benefit in seasonal and perennial Allergic Rhinitis by improving all symptom subgroups.
Keywords: Allergic rhinitis; Nasal spray; Corticosteroid; Anti-allergy Skin Prick Testing (SPT) is used to identify allergens patients are
drugs allergic to and has been shown to be superior to patient-reported
allergen identification or allergens as identified on allergy history take
Introduction [8]. One meta-analysis reported that on SPT the top three allergens
identified in 15 developed countries (covering Europe including the
UK, USA and Australia) were house dust mite, grass pollen and cat
Allergic rhinitis (median prevalence across all centres 21.7%, 16.9% and 8.8%,
Rhinitis means inflammation of the nasal mucous membrane; when respectively) [9].
this is caused by an abnormal IgE-mediated response to an otherwise Epidemiological data suggests that worldwide 400 million people
innocuous stimulant, i.e., an allergen, this is known as allergic rhinitis are currently suffering from allergic rhinitis and that its prevalence is
and is the most common form of non-infectious rhinitis [1-4]. on the rise globally [1]. Though the cause for this rising trend is
Affecting 1 in 4 people seasonal allergic rhinitis, also known as hay unknown, contributing factors include a higher concentration of air
fever [5], presents with nasal congestion, rhinorrhea, itching and/or borne allergens, poor air quality due to pollution, poor indoor
sneezing. Allergic rhinoconjucntivitis is the associated watery eyes, ventilation, smoking and a more sedentary lifestyle among others [10].
itching, burning/irritability, redness and injection of the conjunctiva
which has been documented in 71% of European patients who Treatment of allergic rhinitis
concurrently had nasal symptoms [6].
The British Society of Allergy and Clinical Immunology (BSACI)
Importantly, Allergic Rhinitis has consequences beyond its have developed a pathway for the treatment of Rhinitis, adapted in
prevailing symptoms by having significant impact on quality of life and Figure 1 [2].
social life, these include mood changes, anxiety, depression and
impairment of cognitive function [7].
Otolaryngol (Sunnyvale), an open access journal Volume 7 Issue 1 1000294
ISSN:2161-119X
Citation: Sami AS, Ahmed AS, Ahmed N (2017) Response to Combination Intranasal Corticosteroid and Intranasal Antihistamine in Allergic
Rhinitis, A Questionnaire Based Study in ENT Outpatients. Otolaryngol (Sunnyvale) 7: 294. doi:10.4172/2161-119X.1000294
Page 2 of 7
Figure 1: BSACI algorithm for the treatment of rhinitis, SPT: Skin Prick Test; LTRA: Leukotriene Receptor Antagonist.
Primary care has an increasingly heavy burden of Allergic Rhinitis, propionate) in patients suffering from proven allergic rhinitis who
in England primary care prescriptions for Allergic Rhinitis have gone have failed primary therapy in the GP setting.
up by 41.7% from 2001-2005, which includes antihistamines and
Secondary aims included subgroup analysis as defined by the
topical nasal corticosteroids (also includes topical nasal antihistamine
MSNOT-20 questionnaire and exploring symptom responsiveness
and topical nasal cromoglicate) [11].
based upon skin prick test results.
Specialist centres can provide Immunotherapy for patients who
have had optimal medical treatment yet symptom control has been Method
either minimal or non-existent, there is impact on quality of life and no
contra-indications to immunotherapy. Immunotherapy treatment itself The MSNOT-20 questionnaire is a validated, disease specific
has lasting benefits for the first few years after treatment though this questionnaire (Appendix 1) which can identify rhinitis, its associated
will diminish over time [12]. impact on quality of life and disease response to treatment in the adult
population, its modified version has similar proven qualities in the
Study aim paediatric population of 11-16 year olds [3,13]. It consists of three
sections; section one comprises of demographic details, section two is
The primary aims of this study is to analyse the effect of the disease specific section and section three is the quality of life
combination nasal spray (azelastine hydrochloride and fluticasone section. In the disease specific section, patients would describe the
severity of their symptoms based on a Likert 1 to 5 scale with 5 being
Otolaryngol (Sunnyvale), an open access journal Volume 7 Issue 1 1000294
ISSN:2161-119X
Citation: Sami AS, Ahmed AS, Ahmed N (2017) Response to Combination Intranasal Corticosteroid and Intranasal Antihistamine in Allergic
Rhinitis, A Questionnaire Based Study in ENT Outpatients. Otolaryngol (Sunnyvale) 7: 294. doi:10.4172/2161-119X.1000294
Page 3 of 7
quantified as bad as it can be. The related questions are grouped changes in each subgroup before and after treatment delineated in
together into subgroups, each of which is composed of the following Figures 4a-4e. There was a greater than 50% decrease in symptomology
questions from this section: post treatment with all subgroups showing improvement, though the
improvement was greatest in the nasal subgroup.
Nasal: questions 1, 2, 3, 19
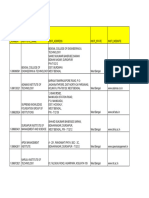
Paranasal: 5, 6, 7, 8, 9, 10-can be further split into the below for Mean before Mean after
treatment treatment
further analysis (Standard (Standard
Subgroup Deviation) Deviation) p value
Sinus: 5, 6, 10
Ear: 7, 8, 9 Nasal 15.69 (4.04) 6.08 (2.43) <0.01
Sleep: 11, 12, 13,14 Paranasal 9.40 (5.54) 3.56 (2.95) <0.01
Social: 15, 16, 17 Sleep 6.29 (6.82) 2.44 (3.93) <0.01
Emotional: 18, 20 Social 4.10 (5.15) 1.90 (3.14) <0.01
Inclusion criteria: Patients being referred from their GP to the ENT
Emotional 1.83 (2.36) 0.83 (1.36) <0.01
and Allergy department at Royal National Throat, Nose and Ear
hospital, London due to nasal and sinus symptoms. These patients
showed no response to optimal primary care treatment along the Table 1: Representing total subgroup mean and standard deviation for
Figure 1 algorithm (which begins with monotherapy agents) or each subgroup before and after treatment with p value quoted.
practice-specific guidelines. Participants were enrolled in two four-
month periods, February-May 2014 and February-May 2016.
Exclusion criteria: Patients with nasal polyposis.
At first clinical contact patients had a full clinical assessment,
completed the MSNOT-20 questionnaire and, if relevant, had skin
prick test.
Subsequent management plan including pharmaceutical option was
discussed; if eligible and clinically appropriate (using treatment
guidelines and clinical experience), treatment was advised with the
aforementioned combination nasal spray and, following informed
consent, initiated as per manufacturers guidelines; 1 spray in each
nostril twice a day in those over 12 years (at the time of the study).
Where needed, a patient information leaflet and clinical demonstration
of the correct technique when using a nasal spray was carried out.
Figure 2: MSNOT-20 score before and after treatment for each
As this particular brand combination was initially not available at
subject, n=48, p<0.01.
the index hospital a GP prescription was provided. After four weeks,
patients were asked to repeat section two of the MSNOT-20
questionnaire again, results were sent back to the researchers. Data was
then collated and statistical analysis was carried out.
Results
In total, 48 candidates (24 males, 24 females) were eligible for
inclusion into the study, age range 20-69 with just under 2/3rd (65%)
being in the 20-44 age group. There was no statistically significant
difference in symptom severity between males and females and
between those with a positive family history compared to those
without.
Before and after treatment comparisons
The sum of the symptom severity patients reported for each of the
twenty questions were calculated to produce the MSNOT-20 score and Figure 3: Mean of MSNOT-20 scores before and after treatment,
is represented in Figure 2 for each subject. All patients had significant blue box representing the mean with black lines representing
improvement in their overall symptom severity. standard deviation, numerical values shown at the bottom of the
graph, n=48, p<0.01.
The mean and standard deviations were calculated for before and
after treatment responses and shown in Figure 3. Similar calculation
was then carried out for all five subgroups as shown in Table 1 with the
Otolaryngol (Sunnyvale), an open access journal Volume 7 Issue 1 1000294
ISSN:2161-119X
Citation: Sami AS, Ahmed AS, Ahmed N (2017) Response to Combination Intranasal Corticosteroid and Intranasal Antihistamine in Allergic
Rhinitis, A Questionnaire Based Study in ENT Outpatients. Otolaryngol (Sunnyvale) 7: 294. doi:10.4172/2161-119X.1000294
Page 4 of 7
Figure 4: a) Nasal subgroup histogram of change in score following treatment, p<0.01, b) Paranasal subgroup histogram of change in score
following treatment, p<0.01, c) Sleep subgroup histogram of change in score following treatment, p<0.01, d) Social subgroup histogram of
change in score following treatment, p<0.01, e) Emotional subgroup histogram of change in score following treatment, p<0.01.
Key symptoms 2nd Need to blow nose
Figure 5 represents the mean responses to each question before and 3rd Sneezing
after treatment, showing the improvement in all symptoms post 4th Runny nose
treatment whilst also showing what the most severe symptoms patients
presented with were (below, in descending order), this order remained 5th Post nasal discharge
the same post treatment. The questionnaire asked patients to report the top five symptoms
1st Blocked nose they felt were most important to them in terms of impact on their
health. All responses to this were collated and the top 5 symptoms
Otolaryngol (Sunnyvale), an open access journal Volume 7 Issue 1 1000294
ISSN:2161-119X
Citation: Sami AS, Ahmed AS, Ahmed N (2017) Response to Combination Intranasal Corticosteroid and Intranasal Antihistamine in Allergic
Rhinitis, A Questionnaire Based Study in ENT Outpatients. Otolaryngol (Sunnyvale) 7: 294. doi:10.4172/2161-119X.1000294
Page 5 of 7
patients perceived to be of greatest importance to them were the same MSNOT-20 Nasal Nasal
as the above list. score MSNOT-20 subgroup Subgroup
Allergen before score after before after
Seasonal
Allergen
Grass pollen 41 16.54 15.89 6.19
Tree Pollen 45.29 17.82 17.71 7.12
Perennial
Allergen
House dust mite 41.41 16.9 14.66 5.79
Mould 51.4 16.8 14.8 4
Aspergillus 30.33 14.67 14 5.67
Cat 48.44 19.5 16.81 6.81
Figure 5: Mean responses to all questions in disease specific section Dog 49.08 19.92 15.85 5.85
before and after treatment, n=48, p<0.01.
Table 2: MSNOT-20 before and after treatment and Nasal subgroup
before and after treatment split by individual allergen (as confirmed by
Subgroup Correlation skin prick test), n=48, p<0.01.
Spearmans Rank Correlation Coefficient test was used to determine
correlations between the subgroup as defined in the Method section. Discussion
The strength of the correlation is represented by the R value; a score of
greater than 0.30 is considered a positive, an R score of greater 0.50 Summary
considered moderately strong positive correlation whilst a score over
There was improvement in overall symptom severity and in all
0.70 in strength is considered a strongly positive correlation [14].
subgroups following treatment in patients with seasonal Allergic
The MSNOT-20 correlates strongest with the sleep subgroup Rhinitis and perennial Allergic Rhinitis who had failed community
(R=0.90, p<0.05) followed by social (0.85, p<0.05), paranasal (0.78, treatment and been referred to secondary care. It can take
p<0.05) and emotional (0.76, p<0.05) approximately 6 weeks from GP referral to presentation at clinic; our
Paranasal subgroup correlates positively with sleep (0.62, p<0.05) results showed that patients had a high burden of symptoms at
followed by social (0.52, p<0.05) and emotional subgroups (0.46, presentation to clinic indicating inadequacy of initial treatment and
p<0.05) unlikelihood of symptom resolution independent of our interventions.
In subgroup analysis, the biggest improvement post treatment was
Skin prick test results and correlation with overall score seen in the nasal subgroup, followed by the paranasal subgroup
The breakdown of the skin prick test results for the entire cohort showing the effective beneficial relief this local agent is able to achieve.
(n=48) are shown below: Though it is a case that all subgroups improved this was small (but
significant) in the emotional subgroup indicating the variety of
House dust mite: n=29 individuals positive on skin prick testing different causes of impairment in this domain and importance of
Grass pollen: n=37 individuals positive on skin prick testing assessing the impact of treatment based on the overall response.
Tree pollen: n=17 individuals positive on skin prick testing
This study also demonstrated the widespread impact that this
Mould: n=5 individuals positive on skin prick testing condition has; as seen by the fact that some of the strongest correlation
Aspergillus: n=3 individuals positive on skin prick testing noted with a high MSNOT-20 score (i.e., most symptomatic) is with
Cat: n=16 individuals positive on skin prick testing the sleep and social subgroups. This study also represents the dominant
Dog: n=13 individuals positive on skin prick testing role of paranasal symptoms in Allergic Rhinitis, which also responded
to the treatment provided here. Paranasal subgroup itself correlated
Table 2 shows the improvement in MSNOT-20 score and Nasal with sleep and social subgroups as well as the emotional subgroup.
subgroup score before and after treatment and has been split by
seasonal (grass or tree pollen in this study) and perennial (allergens This study has shown that the MSNOT-20 is able to detect
present all year round, this study included house dust mite, mould, objectively the most severe symptoms of the patient (among others)
aspergillus, cat and dog) allergens. The results show that the total and correlate this with what the patients perceive to be their most
MSNOT-20 was reduced by two and a half times through the troublesome symptoms, ensuring this very important aspect of
treatment in the seasonal allergens, this was also similar in the nasal management is noted as early as possible. In this study, Blocked nose
score. A considerable improvement in MSNOT-20 score and Nasal was the most severe symptom both objectively and as perceived by the
subgroup was also noted for perennial allergens. patient as most impacting on their health, this is decreased by more
than two-and-a-half times through this intranasal effective treatment
in patients who had initially failed treatment through their GP.
Otolaryngol (Sunnyvale), an open access journal Volume 7 Issue 1 1000294
ISSN:2161-119X
Citation: Sami AS, Ahmed AS, Ahmed N (2017) Response to Combination Intranasal Corticosteroid and Intranasal Antihistamine in Allergic
Rhinitis, A Questionnaire Based Study in ENT Outpatients. Otolaryngol (Sunnyvale) 7: 294. doi:10.4172/2161-119X.1000294
Page 6 of 7
The majority of our patients were within the young working age Conflict of Interest
group which is likely to have impact on occupation, among others,
however Section 3 of the MSNOT-20 questionnaire which addresses A.S.S has received fees from Meda Pharmaceuticals. Meda
this was not reviewed in this analysis, as were data on ethnicity, Pharmaceuticals had no role in study design, collection, analysis,
housing, smoking due to incomplete results available allowing for interpretation of data, writing the report or decision to submit for
scope to further look into this. publication.
Skin prick testing revealed our cohort had sensitisation to multiple
Funding
allergens, which is not uncommon in clinical practise. One study of
200 patients with medically unresponsive chronic or recurrent A.S.S received fees from Meda Pharmaceuticals.
rhinosinusitis revealed that 52% of these had multiple allergy
sensitivities however this did not appear to determine the severity of References
sinus disease as seen on imaging, mitigating impact on clinical severity
[15]. 1. Baena-Cagnani CE, Canonica GW, Helal MZ, Gmez RM, Compalati E,
et al. (2015) The international survey on the management of allergic
rhinitis by physicians and patients (ISMAR). World Allergy Organ J 8: 1.
Strength and limitations
2. Sami AS, Scadding G (2013) Management of allergic rhinitis in schools.
This study was able to elicit large improvements in the key domains British Journal of School Nursing 8: 119-123.
of nasal and overall symptomatology, with improvements in all 3. Sami AS, Malik M, Amjad M, Howarth P (2013) Rhinitis, sinusitis and
domains noted in patients with proven Allergic Rhinitis, this was in ocular disease2092. The MSNOT-20 questionnaire: Repeatability and
disease analysis of rhinitis/rhinosinusitis. World Allergy Organ J 6: 1.
spite of the relatively limited sample size. A larger sample size may also
allow us to explore the role of family history and symptom severity, to 4. Bousquet J, Khaltaev N, Cruz A, Denburg J, Fokkens W, et al. (2008)
Allergic rhinitis and its impact on asthma (ARIA) 2008. Allergy 63:
correlate with current research identifying genetic factors, notably 8-160.
genes involved in epithelial barrier/regulatory function, which may be
5. Kariyawasam HH, Scadding GK (2010) Seasonal allergic rhinitis:
involved in allergic rhinitis [16]. It was also difficult to carry out Fluticasone propionate and fluticasone furoate therapy evaluated. J
comprehensive analyses on some aspects e.g. Section 3 of the Asthma Allergy 3: 19-28.
questionnaire due to some incomplete data. 6. Canonica GW, Bousquet J, Mullol J, Scadding GK, Virchow JC (2007) A
survey of the burden of allergic rhinitis in Europe. Allergy 85: 17-25.
Comparison with existing literature 7. Meltzer EO, Gross GN, Katial R, Storms WW (2012) Allergic rhinitis
substantially impacts patient quality of life: Findings from the Nasal
Treatment of Allergic Rhinitis is a combination of lifestyle changes Allergy Survey Assessing Limitations. J Fam Pract 61: S5-S10.
(by reducing exposure to the allergens) and medical therapy including 8. Smith HE, Hogger C, Lallemant C, Crook D, Frew AJ (2009) Is structured
nasal irrigation. One meta-analysis (n=2,267) showed that intranasal allergy history sufficient when assessing patients with asthma and rhinitis
corticosteroids in patients with Allergic Rhinitis provides significantly in general practice? J Allergy Clin Immunol 123: 646-650.
greater relief of nasal congestion than oral antihistamines [17]. 9. Bousquet P, Chinn S, Janson C, Kogevinas M, Burney P, et al. (2007).
Geographical variation in the prevalence of positive skin tests to
It is combination therapy which has proven to not only improve environmental aeroallergens in the European Community Respiratory
symptomatology but also be found to be more convenient and effective Health Survey I. Allergy 62: 301-309.
when used by patients [18,19]. 10. Baena-Cagnani CE, Gmez RM (2009) Is the prevalence of allergy
continuously increasing? Allergy frontiers: Epigenetics, allergens and risk
Implications for research and/or practice factors. Springer, pp: 17-31.
11. Ghouri N, Hippisley-Cox J, Newton J, Sheikh A (2008) Trends in the
Primary care setting has an increasing demand of medications used epidemiology and prescribing of medication for allergic rhinitis in
in Allergic Rhinitis [11]. This combination therapy has proven to be England. J R Soc Med 101: 466-472.
effective at decreasing disease burden and relief from its associated 12. Walker SM, Durham SR, Till SJ, Roberts G, Corrigan CJ, et al. (2011)
impact on sleep, social and emotional domains. Its effects have been Immunotherapy for allergic rhinitis. Clin Exp Allergy 41: 1177-1200.
proven in a cohort of patients with confirmed Allergic Rhinitis who 13. Sami AS, Scadding GK (2014) Rhinosinusitis in secondary school
had initially failed treatment at the primary care level and as such is a children-part 2: Main project analysis of MSNOT-20 Young Persons
viable option available to the community setting. Questionnaire (MSYPQ). Rhinology 52: 225-230.
14. Mukaka MM (2012) Statistics corner: A guide to appropriate use of
Future research into correlation of familial and demographic correlation coefficient in medical research. Malawi Med J 24: 69-71.
variables on disease and severity with a more comprehensive 15. Emanuel IA, Shah SB (2000) Chronic rhinosinusitis: allergy and sinus
assessment of financial and occupational complications of this very computed tomography relationships. Otolaryngol Head Neck Surg 123:
prevalent disease are warranted. 687-691.
16. Portelli MA, Hodge E, Sayers I (2015) Genetic risk factors for the
Conclusion development of allergic disease identified by genome-wide association.
Clin Exp Allergy 45: 21-31.
There was significant improvement in Allergic Rhinitis symptoms 17. Nathan RA (2008) The pathophysiology, clinical impact, and
with all five subgroups having improvements in symptomatology. The management of nasal congestion in allergic rhinitis. Clin Ther 30:
nasal subgroup in particular responded well in patients with both 573-586.
seasonal allergens and perennial allergens. This treatment has been 18. Carr W, Bernstein J, Lieberman P, Meltzer E, Bachert C, et al. (2012) A
effective where subjects had previously failed community therapy. novel intranasal therapy of azelastine with fluticasone for the treatment of
allergic rhinitis. J Allergy Clin Immunol 129: 1282-1289.
Otolaryngol (Sunnyvale), an open access journal Volume 7 Issue 1 1000294
ISSN:2161-119X
Citation: Sami AS, Ahmed AS, Ahmed N (2017) Response to Combination Intranasal Corticosteroid and Intranasal Antihistamine in Allergic
Rhinitis, A Questionnaire Based Study in ENT Outpatients. Otolaryngol (Sunnyvale) 7: 294. doi:10.4172/2161-119X.1000294
Page 7 of 7
19. Meltzer EO, LaForce C, Ratner P, Price D, Ginsberg D, et al. (2012) randomized, double-blind, placebo-controlled trial of efficacy and safety.
MP29-02 (a novel intranasal formulation of azelastine hydrochloride and Allergy Asthma Proc 33: 324-332.
fluticasone propionate) in the treatment of seasonal allergic rhinitis: A
Otolaryngol (Sunnyvale), an open access journal Volume 7 Issue 1 1000294
ISSN:2161-119X
S-ar putea să vă placă și
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Apexi Powerfc Instruction ManualDocument15 paginiApexi Powerfc Instruction ManualEminence Imports0% (2)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Workbook Group TheoryDocument62 paginiWorkbook Group TheoryLi NguyenÎncă nu există evaluări
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Catify To Satisfy - Simple Solutions For Creating A Cat-Friendly Home (PDFDrive)Document315 paginiCatify To Satisfy - Simple Solutions For Creating A Cat-Friendly Home (PDFDrive)Paz Libros100% (2)
- Configuring BGP On Cisco Routers Lab Guide 3.2Document106 paginiConfiguring BGP On Cisco Routers Lab Guide 3.2skuzurov67% (3)
- Executive Summary-P-5 181.450 To 222Document14 paginiExecutive Summary-P-5 181.450 To 222sat palÎncă nu există evaluări
- Desktop 9 QA Prep Guide PDFDocument15 paginiDesktop 9 QA Prep Guide PDFPikine LebelgeÎncă nu există evaluări
- Case Study 2Document5 paginiCase Study 2api-247285537100% (1)
- WBDocument59 paginiWBsahil.singhÎncă nu există evaluări
- Iguana Joe's Lawsuit - September 11, 2014Document14 paginiIguana Joe's Lawsuit - September 11, 2014cindy_georgeÎncă nu există evaluări
- Patrick Meyer Reliability Understanding Statistics 2010Document160 paginiPatrick Meyer Reliability Understanding Statistics 2010jcgueinj100% (1)
- Comparison Between CompetitorsDocument2 paginiComparison Between Competitorsritesh singhÎncă nu există evaluări
- Physics Education Thesis TopicsDocument4 paginiPhysics Education Thesis TopicsPaperWriterServicesCanada100% (2)
- Book 1518450482Document14 paginiBook 1518450482rajer13Încă nu există evaluări
- Reported SpeechDocument6 paginiReported SpeechRizal rindawunaÎncă nu există evaluări
- Cooperative Learning: Complied By: ANGELICA T. ORDINEZADocument16 paginiCooperative Learning: Complied By: ANGELICA T. ORDINEZAAlexis Kaye GullaÎncă nu există evaluări
- Lesson 3 - ReviewerDocument6 paginiLesson 3 - ReviewerAdrian MarananÎncă nu există evaluări
- Algoritm BackTracking EnglezaDocument6 paginiAlgoritm BackTracking Englezaionutz_67Încă nu există evaluări
- Fertilization Guide For CoconutsDocument2 paginiFertilization Guide For CoconutsTrade goalÎncă nu există evaluări
- Student Exploration: Inclined Plane - Simple MachineDocument9 paginiStudent Exploration: Inclined Plane - Simple MachineLuka MkrtichyanÎncă nu există evaluări
- Pityriasis VersicolorDocument10 paginiPityriasis Versicolorketty putriÎncă nu există evaluări
- Hướng Dẫn Chấm: Ngày thi: 27 tháng 7 năm 2019 Thời gian làm bài: 180 phút (không kể thời gian giao đề) HDC gồm có 4 trangDocument4 paginiHướng Dẫn Chấm: Ngày thi: 27 tháng 7 năm 2019 Thời gian làm bài: 180 phút (không kể thời gian giao đề) HDC gồm có 4 trangHưng Quân VõÎncă nu există evaluări
- An Evaluation of MGNREGA in SikkimDocument7 paginiAn Evaluation of MGNREGA in SikkimBittu SubbaÎncă nu există evaluări
- Progressive Muscle RelaxationDocument4 paginiProgressive Muscle RelaxationEstéphany Rodrigues ZanonatoÎncă nu există evaluări
- Eloy-Stock English Full PDFDocument0 paginiEloy-Stock English Full PDFR.s. WartsÎncă nu există evaluări
- Determination Rules SAP SDDocument2 paginiDetermination Rules SAP SDkssumanthÎncă nu există evaluări
- LSCM Course OutlineDocument13 paginiLSCM Course OutlineDeep SachetiÎncă nu există evaluări
- SSP 237 d1Document32 paginiSSP 237 d1leullÎncă nu există evaluări
- SachinDocument3 paginiSachinMahendraÎncă nu există evaluări
- Chapter 2Document13 paginiChapter 2Kumkumo Kussia KossaÎncă nu există evaluări
- Rajiv Gandhi University of Health Sciences, Bengaluru, KarnatakaDocument9 paginiRajiv Gandhi University of Health Sciences, Bengaluru, KarnatakaNavin ChandarÎncă nu există evaluări