Documente Academic
Documente Profesional
Documente Cultură
Guidelines For Management of Stable Ischemic Heart Disease
Încărcat de
tjelongTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Guidelines For Management of Stable Ischemic Heart Disease
Încărcat de
tjelongDrepturi de autor:
Formate disponibile
Journal of the American College of Cardiology Vol. 60, No.
24, 2012
2012 by the American College of Cardiology Foundation and the American Heart Association, Inc. ISSN 0735-1097/$36.00
Published by Elsevier Inc. http://dx.doi.org/10.1016/j.jacc.2012.07.012
PRACTICE GUIDELINE
2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline
for the Diagnosis and Management of Patients With
Stable Ischemic Heart Disease: Executive Summary
A Report of the American College of Cardiology Foundation/American Heart Association Task Force on
Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery,
Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions,
and Society of Thoracic Surgeons
Writing Stephan D. Fihn, MD, MPH, Chair Michael J. Mack, MD*#
Committee Julius M. Gardin, MD, Vice Chair* Mark A. Munger, PHARMD*
Members*
Richard L. Prager, MD#
Jonathan Abrams, MD Joseph F. Sabik, MD***
Kathleen Berra, MSN, ANP* Leslee J. Shaw, PHD*
James C. Blankenship, MD* Joanna D. Sikkema, MSN, ANP-BC*
Apostolos P. Dallas, MD* Craig R. Smith, JR, MD**
Pamela S. Douglas, MD* Sidney C. Smith, JR, MD*
JoAnne M. Foody, MD* John A. Spertus, MD, MPH*
Thomas C. Gerber, MD, PHD Sankey V. Williams, MD*
Alan L. Hinderliter, MD
Spencer B. King III, MD* *Writing committee members are required to recuse themselves from
Paul D. Kligfield, MD voting on sections to which their specific relationship could apply; see
Appendix 1 for detailed information. ACP Representative. ACCF/
Harlan M. Krumholz, MD AHA Representative. PCNA Representative. SCAI Representative.
Raymond Y. K. Kwong, MD Critical care nursing expertise. #STS Representative. **AATS Repre-
sentative. ACCF/AHA Task Force on Practice Guidelines Liaison.
Michael J. Lim, MD*
ACCF/AHA Task Force on Performance Measures Liaison.
Jane A. Linderbaum, MS, CNP-BC
Full-text guideline available at: J Am Coll Cardiol 2012;60:e44 164; doi:10.1016/ Williams SV. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the
j.jacc.2012.07.013. diagnosis and management of patients with stable ischemic heart disease: a report of
The writing committee gratefully acknowledges the memory of James T. Dove, the American College of Cardiology Foundation/American Heart Association Task
MD, who died during the development of this document but contributed immensely Force on Practice Guidelines, and the American College of Physicians, American
to our understanding of stable ischemic heart disease. Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association,
This document was approved by the American College of Cardiology Foun- Society for Cardiovascular Angiography and Interventions, and Society of Thoracic
dation Board of Trustees, American Heart Association Science Advisory and Surgeons. J Am Coll Cardiol 2012;60:2564 603.
Coordinating Committee, American College of Physicians, American Association This article is copublished in Circulation.
for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Copies: This document is available on the World Wide Web sites of the American
Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons College of Cardiology (www.cardiosource.org) and American Heart Association
in July 2012. (my.americanheart.org). For copies of this document, please contact Elsevier Inc.
The American College of Cardiology Foundation requests that this document be Reprint Department, fax (212) 633-3820, e-mail reprints@elsevier.com.
cited as follows: Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas Permissions: Modification, alteration, enhancement and/or distribution of this
AP, Douglas PS, Foody JM, Gerber TC, Hinderliter AL, King SB III, Kligfield PD, document are not permitted without the express permission of the American College
Krumholz HM, Kwong RYK, Lim MJ, Linderbaum JA, Mack MJ, Munger MA, of Cardiology Foundation. Please contact Elseviers permission department:
Prager RL, Sabik JF, Shaw LJ, Sikkema JD, Smith CR Jr, Smith SC Jr, Spertus JA, healthpermissions@elsevier.com/.
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2565
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
ACCF/AHA Jeffrey L. Anderson, MD, FACC, FAHA, Steven M. Ettinger, MD, FACC
Task Force Chair Robert A. Guyton, MD, FACC
Members
Jonathan L. Halperin, MD, FACC, FAHA, Judith S. Hochman, MD, FACC, FAHA
Chair-Elect Sharon Ann Hunt, MD, FACC, FAHA
Alice K. Jacobs, MD, FACC, FAHA, Richard J. Kovacs, MD, FACC, FAHA
Immediate Past Chair 2009 2011 Frederick G. Kushner, MD, FACC, FAHA
Sidney C. Smith, Jr, MD, FACC, FAHA, Bruce W. Lytle, MD, FACC, FAHA
Past Chair 2006 2008 Rick A. Nishimura, MD, FACC, FAHA
E. Magnus Ohman, MD, FACC
Cynthia D. Adams, MSN, APRN-BC, Richard L. Page, MD, FACC, FAHA
FAHA Barbara Riegel, DNSC, RN, FAHA
Nancy M. Albert, PHD, CCNS, CCRN, William G. Stevenson, MD, FACC, FAHA
FAHA Lynn G. Tarkington, RN
Ralph G. Brindis, MD, MPH, MACC Clyde W. Yancy, MD, FACC, FAHA
Christopher E. Buller, MD, FACC
Former Task Force member during this writing effort.
Mark A. Creager, MD, FACC, FAHA
David DeMets, PHD
3.1.1. Resting Imaging to Assess Cardiac Structure
TABLE OF CONTENTS and Function . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2574
3.1.2. Stress Testing and Advanced Imaging in Patients
Preamble . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2566
With Known SIHD Who Require Noninvasive
Testing for Risk Assessment . . . . . . . . . . . . . . . . . . .2575
1. Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2568 3.1.2.1. RISK ASSESSMENT IN PATIENTS ABLE
TO EXERCISE . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2575
1.1. Methodology and Evidence Overview . . . . . . . . . . . .2568 3.1.2.2. RISK ASSESSMENT IN PATIENTS UNABLE TO
1.2. Organization of the Writing Committee . . . . . . . . . .2569 EXERCISE . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2576
3.1.2.3. RISK ASSESSMENT REGARDLESS OF
1.3. Document Review and Approval . . . . . . . . . . . . . . . . . .2569
PATIENTS ABILITY TO EXERCISE . . . . . . . . . . . . . . . . .2577
1.4. Scope of the Guideline . . . . . . . . . . . . . . . . . . . . . . . . . . . .2569
1.5. General Approach and Overlap With Other 3.2. Coronary Angiography . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2578
Guidelines or Statements . . . . . . . . . . . . . . . . . . . . . . . . .2571 3.2.1. Coronary Angiography as an Initial Testing
1.6. Magnitude of the Problem. . . . . . . . . . . . . . . . . . . . . . . . .2571 Strategy to Assess Risk . . . . . . . . . . . . . . . . . . . . . . . . .2578
1.7. Organization of the Guideline . . . . . . . . . . . . . . . . . . . . .2571 3.2.2. Coronary Angiography to Assess Risk After
1.8. Vital Importance of Involvement by an Initial Workup With Noninvasive Testing . . . . .2578
Informed Patient: Recommendation. . . . . . . . . . . . . .2572
4. Treatment: Recommendations . . . . . . . . . . . . . . . . . . . . . . .2579
2. Diagnosis of SIHD: Recommendations . . . . . . . . . . . . .2572
4.1. Patient Education . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2579
2.1. Clinical Evaluation of Patients With Chest
4.2. Guideline-Directed Medical Therapy . . . . . . . . . . . . . .2580
Pain . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2572
4.2.1. Risk Factor Modification . . . . . . . . . . . . . . . . . . . . . . .2580
2.1.1. Clinical Evaluation in the Initial Diagnosis of 4.2.1.1. LIPID MANAGEMENT . . . . . . . . . . . . . . . . . . . . . . . . . .2580
SIHD in Patients With Chest Pain . . . . . . . . . . . .2572 4.2.1.2. BLOOD PRESSURE MANAGEMENT . . . . . . . . . . . . . . . .2580
2.1.2. Electrocardiography . . . . . . . . . . . . . . . . . . . . . . . . . . . .2572 4.2.1.3. DIABETES MANAGEMENT . . . . . . . . . . . . . . . . . . . . . .2580
2.1.2.1. RESTING ELECTROCARDIOGRAPHY
4.2.1.4. PHYSICAL ACTIVITY . . . . . . . . . . . . . . . . . . . . . . . . . . .2580
TO ASSESS RISK . . . . . . . . . . . . . . . . . . . . . . . . . . . .2572
2.1.3. Stress Testing and Advanced Imaging for 4.2.1.5. WEIGHT MANAGEMENT . . . . . . . . . . . . . . . . . . . . . . . .2580
Initial Diagnosis in Patients With Suspected 4.2.1.6. SMOKING CESSATION COUNSELING. . . . . . . . . . . . . . .2580
SIHD Who Require Noninvasive Testing . . . . . .2572 4.2.1.7. MANAGEMENT OF PSYCHOLOGICAL FACTORS . . . . . . .2581
2.1.3.1. ABLE TO EXERCISE . . . . . . . . . . . . . . . . . . . . . . . . . . .2572 4.2.1.8. ALCOHOL CONSUMPTION . . . . . . . . . . . . . . . . . . . . . .2581
2.1.3.2. UNABLE TO EXERCISE . . . . . . . . . . . . . . . . . . . . . . . . .2572 4.2.1.9. AVOIDING EXPOSURE TO AIR POLLUTION . . . . . . . . . .2581
2.1.3.3. OTHER . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2574 4.2.2. Additional Medical Therapy to Prevent MI
and Death . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2581
3. Risk Assessment: Recommendations . . . . . . . . . . . . . .2574 4.2.2.1. ANTIPLATELET THERAPY . . . . . . . . . . . . . . . . . . . . . . .2581
4.2.2.2. BETA-BLOCKER THERAPY . . . . . . . . . . . . . . . . . . . . . .2581
3.1. Advanced Testing: Resting and 4.2.2.3. RENIN-ANGIOTENSIN-ALDOSTERONE BLOCKER
Stress Noninvasive Testing . . . . . . . . . . . . . . . . . . . . . . .2574 THERAPY . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2581
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2566 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
4.2.2.4. INFLUENZA VACCINATION . . . . . . . . . . . . . . . . . . . . . .2581 jointly produced guidelines in the area of cardiovascular
4.2.2.5. ADDITIONAL THERAPY TO REDUCE RISK OF MI
AND DEATH . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2581
disease since 1980. The ACCF/AHA Task Force on
4.2.3. Medical Therapy for Relief of Symptoms . . . . . .2581 Practice Guidelines (Task Force), charged with developing,
4.2.3.1. USE OF ANTI-ISCHEMIC MEDICATIONS . . . . . . . . . . . . .2581 updating, and revising practice guidelines for cardiovascular
4.2.4. Alternative Therapies for Relief of Symptoms in
diseases and procedures, directs and oversees this effort. Writ-
Patients With Refractory Angina . . . . . . . . . . . . . . .2582
ing committees are charged with regularly reviewing and
5. CAD Revascularization: Recommendations . . . . . . . .2582 evaluating all available evidence to develop balanced, patient-
centric recommendations for clinical practice.
5.1. Heart Team Approach to Revascularization
Decisions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2582 Experts in the subject under consideration are selected by
5.2. Revascularization to Improve Survival . . . . . . . . . . .2582
the ACCF and AHA to examine subject-specific data and
write guidelines in partnership with representatives from
5.3. Revascularization to Improve Symptoms . . . . . . . .2584
other medical organizations and specialty groups. Writing
5.4. Dual Antiplatelet Therapy Compliance and
Stent Thrombosis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2585 committees are asked to perform a literature review; weigh
the strength of evidence for or against particular tests,
5.5. Hybrid Coronary Revascularization . . . . . . . . . . . . . . .2585
treatments, or procedures; and include estimates of ex-
6. Patient Follow-Up: Monitoring of Symptoms pected outcomes where such data exist. Patient-specific
and Antianginal Therapy: Recommendations . . . . . .2585
modifiers, comorbidities, and issues of patient preference
that may influence the choice of tests or therapies are consid-
6.1. Clinical Evaluation, Echocardiography During
Routine, Periodic Follow-Up . . . . . . . . . . . . . . . . . . . . . . .2585 ered. When available, information from studies on cost is
6.2. Noninvasive Testing in Known SIHD . . . . . . . . . . . . . .2586 considered, but data on efficacy and outcomes constitute the
6.2.1. Follow-Up Noninvasive Testing in Patients With primary basis for the recommendations contained herein.
Known SIHD: New, Recurrent or Worsening In analyzing the data and developing recommendations
Symptoms, Not Consistent With Unstable and supporting text, the writing committee uses evidence-
Angina . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2586
6.2.1.1. PATIENTS ABLE TO EXERCISE . . . . . . . . . . . . . . . . . . .2586 based methodologies developed by the Task Force (1). The
6.2.1.2. PATIENTS UNABLE TO EXERCISE . . . . . . . . . . . . . . . . .2586 Class of Recommendation (COR) is an estimate of the size
6.2.1.3. IRRESPECTIVE OF ABILITY TO EXERCISE . . . . . . . . . . .2587 of the treatment effect, with consideration given to risks
6.2.2. Noninvasive Testing in Known
versus benefits in addition to evidence and/or agreement
SIHDAsymptomatic (or Stable Symptoms) . .2587
that a given treatment or procedure is or is not useful/
effective or in some situations may cause harm. The Level of
Appendix 1. Author Relationships With Industry Evidence (LOE) is an estimate of the certainty or precision
and Other Entities (Relevant) . . . . . . . . . . . . . . . . . . . . . . . . . . . .2599 of the treatment effect. The writing committee reviews and
ranks evidence supporting each recommendation, with the
Appendix 2. Reviewer Relationships With Industry weight of evidence ranked as LOE A, B, or C according to
and Other Entities (Relevant) . . . . . . . . . . . . . . . . . . . . . . . . . . . .2601
specific definitions that are included in Table 1. Studies are
identified as observational, retrospective, prospective, or
randomized as appropriate. For certain conditions for which
Preamble inadequate data are available, recommendations are based
on expert consensus and clinical experience and are ranked
The medical profession should play a central role in evalu- as LOE C. When recommendations at LOE C are sup-
ating the evidence related to drugs, devices, and procedures ported by historical clinical data, appropriate references
for the detection, management, and prevention of disease. (including clinical reviews) are cited if available. For issues
When properly applied, expert analysis of available data on for which sparse data are available, a survey of current
the benefits and risks of these therapies and procedures can practice among the clinicians on the writing committee is
improve the quality of care, optimize patient outcomes, and the basis for LOE C recommendations, and no references
favorably affect costs by focusing resources on the most are cited. The schema for COR and LOE is summarized in
effective strategies. An organized and directed approach to a Table 1, which also provides suggested phrases for writing
thorough review of evidence has resulted in the production recommendations within each COR. A new addition to this
of clinical practice guidelines that assist physicians in select- methodology is separation of the Class III recommendations to
ing the best management strategy for an individual patient. delineate whether the recommendation is determined to be of
Moreover, clinical practice guidelines can provide a foun- no benefit or is associated with harm to the patient. In
dation for other applications, such as performance measures, addition, in view of the increasing number of comparative
appropriate use criteria, and both quality improvement and effectiveness studies, comparator verbs and suggested phrases
clinical decision support tools. for writing recommendations for the comparative effectiveness
The American College of Cardiology Foundation of one treatment or strategy versus another have been added for
(ACCF) and the American Heart Association (AHA) have COR I and IIa, LOE A or B only.
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2567
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
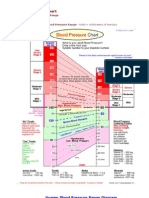
Table 1. Applying Classification of Recommendations and Level of Evidence
A recommendation with Level of Evidence B or C does not imply that the recommendation is weak. Many important clinical questions addressed in the guidelines do not lend themselves to clinical trials.
Although randomized trials are unavailable, there may be a very clear clinical consensus that a particular test or therapy is useful or effective.
Data available from clinical trials or registries about the usefulness/efficacy in different subpopulations, such as sex, age, history of diabetes, history of prior myocardial infarction, history of heart
failure, and prior aspirin use. For comparative effectiveness recommendations (Class I and IIa; Level of Evidence A and B only), studies that support the use of comparator verbs should involve direct
comparisons of the treatments or strategies being evaluated.
In view of the advances in medical therapy across the populations on the treatment effect and relevance to the
spectrum of cardiovascular diseases, the Task Force has ACCF/AHA target population to determine whether the
designated the term guideline-directed medical therapy findings should inform a specific recommendation.
(GDMT) to represent optimal medical therapy as defined by The ACCF/AHA practice guidelines are intended to assist
ACCF/AHA guideline-recommended therapies (primarily healthcare providers in clinical decision making by describing a
Class I). This new term, GDMT, will be used herein and range of generally acceptable approaches to the diagnosis,
throughout all future guidelines. management, and prevention of specific diseases or conditions.
Because the ACCF/AHA practice guidelines address The guidelines attempt to define practices that meet the needs
patient populations (and healthcare providers) residing in of most patients in most circumstances. The ultimate judg-
North America, drugs that are not currently available in ment about care of a particular patient must be made by the
North America are discussed in the text without a specific healthcare provider and patient in light of all the circumstances
COR. For studies performed in large numbers of subjects presented by that patient. As a result, situations may arise in
outside North America, each writing committee reviews the which deviations from these guidelines might be appropriate.
potential influence of different practice patterns and patient Clinical decision making should involve consideration of the
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2568 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
quality and availability of expertise in the area where care is ation for Thoracic Surgery (AATS), Preventive Cardiovascular
provided. When these guidelines are used as the basis for Nurses Association (PCNA), Society for Cardiovascular An-
regulatory or payer decisions, the goal should be improvement giography and Interventions (SCAI), and Society of Thoracic
in quality of care. The Task Force recognizes that situations Surgeons (STS), without commercial support. Writing commit-
arise in which additional data are needed to inform patient care tee members volunteered their time for this activity.
more effectively; these areas will be identified within each The recommendations in this guideline are considered
respective guideline when appropriate. current until they are superseded by a focused update or the
Prescribed courses of treatment in accordance with full-text guideline is revised. The reader is encouraged to
these recommendations are effective only if followed. consult the full-text guideline (2) for additional guidance
Because lack of patient understanding and adherence may and details about stable ischemic heart disease since the
adversely affect outcomes, physicians and other health- Executive Summary contains only the recommendations.
care providers should make every effort to engage the Guidelines are official policy of both the ACCF and AHA.
patients active participation in prescribed medical regi-
mens and lifestyles. In addition, patients should be Jeffrey L. Anderson, MD, FACC, FAHA
informed of the risks, benefits, and alternatives to a Chair, ACCF/AHA Task Force on Practice Guidelines
particular treatment and should be involved in shared
decision making whenever feasible, particularly for COR IIa 1. Introduction
and IIb, for which the benefit-to-risk ratio may be lower.
The Task Force makes every effort to avoid actual,
1.1. Methodology and Evidence Overview
potential, or perceived conflicts of interest that may arise as
a result of industry relationships or personal interests among The recommendations listed in this document are, when-
the members of the writing committee. All writing com- ever possible, evidence based. An extensive evidence review
mittee members and peer reviewers of this guideline were was conducted as the document was compiled through
required to disclose all such current healthcare-related December 2008. Repeated literature searches were per-
relationships, as well as those existing 24 months (from formed by the guideline development staff and writing
2005) before initiation of the writing effort. The writing committee members as new issues were considered. When
committee chair may not have any relevant relationships available, current and credible meta-analyses were used
with industry or other entities (RWI); however, RWI are instead of conducting a systematic review of all primary
permitted for the vice chair position. In December 2009, the literature. New clinical trials published in peer-reviewed
ACCF and AHA implemented a new policy that requires a journals and articles through December 2011 were also
minimum of 50% of the writing committee have no relevant reviewed and incorporated when relevant. Furthermore,
RWI; in addition, the disclosure term was changed to 12 because of the extended development time period for this
months before writing committee initiation. The present guideline, peer review comments indicated that the sections
guideline was developed during the transition in RWI focused on imaging technologies required additional updat-
policy and occurred over an extended period of time. In the ing, which occurred during 2011. Therefore, the evidence
interest of transparency, we provide full information on review for the imaging sections includes published literature
RWI existing over the entire period of guideline develop- through December 2011.
ment, including delineation of relationships that expired Searches were limited to studies, reviews, and other
more than 24 months before the guideline was finalized. evidence in human subjects and published in English.
This information is included in Appendix 1. These state- Key search words included, but were not limited to:
ments are reviewed by the Task Force and all members accuracy, angina, asymptomatic patients, cardiac magnetic
during each conference call and meeting of the writing resonance (CMR), cardiac rehabilitation, chest pain, chronic
committee and are updated as changes occur. All guideline angina, chronic coronary occlusions, chronic ischemic heart
recommendations require a confidential vote by the writing disease (IHD), chronic total occlusion, connective tissue
committee and must be approved by a consensus of the disease, coronary artery bypass graft (CABG) versus medical
voting members. Members who recused themselves from therapy, coronary artery disease (CAD) and exercise, coro-
voting are indicated in the list of writing committee mem- nary calcium scanning, cardiac/coronary computed tomogra-
bers, and section recusals are noted in Appendix 1. Authors phy angiography (CCTA), CMR angiography, CMR imag-
and peer reviewers RWI pertinent to this guideline are ing, coronary stenosis, death, depression, detection of CAD in
disclosed in Appendixes 1 and 2, respectively. Comprehen- symptomatic patients, diabetes, diagnosis, dobutamine stress
sive disclosure information for the Task Force is also echocardiography, echocardiography, elderly, electrocardio-
available online at http://www.cardiosource.org/ACC/ gram (ECG) and chronic stable angina, emergency depart-
About-ACC/Who-We-Are/Leadership/Guidelines-and- ment, ethnic, exercise, exercise stress testing, follow-up test-
Documents-Task-Forces.aspx. The work of the writing ing, gender, glycemic control, hypertension, intravascular
committee is supported exclusively by the ACCF, AHA, ultrasound, fractional flow reserve, invasive coronary an-
American College of Physicians (ACP), American Associ- giography, kidney disease, low-density lipoprotein lowering,
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2569
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
magnetic resonance imaging (MRI), medication adherence, Lastly, the imaging sections were also peer reviewed separately,
minority groups, mortality, myocardial infarction (MI), after an update to that evidence base.
noninvasive testing and mortality, nuclear myocardial per- This document was approved for publication by the
fusion, nutrition, obesity, outcomes, patient follow-up, pa- governing bodies of the ACCF, AHA, ACP, AATS,
tient education, prognosis, proximal left anterior descending PCNA, SCAI, and STS.
(LAD) disease, physical activity, reoperation, risk stratifica-
tion, smoking, stable ischemic heart disease (SIHD), stable 1.4. Scope of the Guideline
angina and reoperation, stable angina and revasculariza- These guidelines are intended to apply to adult patients with
tion, stress echocardiography, radionuclide stress testing, stable known or suspected IHD, including new-onset chest
stenting versus CABG, unprotected left main, weight reduc- pain (i.e., low-risk unstable angina [UA]), or to adult
tion, and women. patients with stable pain syndromes (Figure 1). Patients
1.2. Organization of the Writing Committee who have ischemic equivalents, such as dyspnea or arm
The writing committee was composed of physicians, car- pain with exertion, are included in the latter group. Many
diovascular interventionalists, surgeons, general internists, patients with IHD can become asymptomatic with appro-
imagers, nurses, and pharmacists. The writing committee priate therapy. Accordingly, the follow-up sections of this
included representatives from the ACP, AATS, PCNA, guideline pertain to patients who were previously symptom-
SCAI, and STS. atic, including those who have undergone percutaneous
coronary intervention (PCI) or CABG.
1.3. Document Review and Approval This guideline also addresses the initial diagnostic approach
This document was reviewed by 2 external reviewers nom- to patients who present with symptoms that suggest
inated by both the ACCF and the AHA; 2 reviewers IHD, such as anginal-type chest pain, but who are not
nominated by the ACP, AATS, PCNA, SCAI, and STS; known to have IHD. In this circumstance, it is essential
and 19 content reviewers, including representatives from the that the practitioner ascertain whether such symptoms
ACCF Imaging Council, ACCF Interventional Scientific represent the initial clinical recognition of chronic stable
Council, and the AHA Council on Clinical Cardiology. All angina, reflecting gradual progression of obstructive CAD or
reviewer RWI information was collected and distributed to an increase in supply/demand mismatch precipitated by a
the writing committee and is published in this document change in activity or concurrent illness (such as anemia or
(Appendix 2). Because extensive peer review comments re- infection), or whether they represent an acute coronary
sulted in substantial revision, the guideline was subjected to a syndrome (ACS), most likely due to an unstable plaque
second peer review by all official and organizational reviewers. causing acute thrombosis. For patients with newly diagnosed
Noninvasive Asymptomatic
Testing
(SIHD)
*Features of low risk unstable angina:
Age, 70 y
Exertional pain lasting <20 min.
Pain not rapidly accelerating
Normal or unchanged ECG
No elevation of cardiac markers
Stable Angina
Asymptomatic New Onset
or Low-Risk
Persons Chest Pain
UA* Patients
(SIHD; UA/NSTEMI; STEMI)
Without (SIHD; PCI/CABG) with
Known IHD Known IHD
(CV Risk)
Noncardiac Acute Coronary
Chest Pain Syndromes
(UA/NSTEMI; STEMI;
PCI/CABG)
Sudden Cardiac Death
(VA-SCD)
Figure 1. Spectrum of IHD
Guidelines relevant to the spectrum of IHD are in parentheses.
CABG indicates coronary artery bypass graft; CV, cardiovascular; ECG, electrocardiogram; IHD, ischemic heart disease; PCI, percutaneous coronary intervention; SCD, sudden
cardiac death; SIHD, stable ischemic heart disease; STEMI, ST-elevation myocardial infarction; UA, unstable angina; UA/NSTEMI, unstable angina/nonST-elevation myocar-
dial infarction; and VA, ventricular arrhythmia.
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2570 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
stable angina, this guideline should be used. For patients with Additionally, this guideline addresses the approach to
acute MI, the reader is referred to the ACCF/AHA guidelines asymptomatic patients with SIHD that has been diagnosed
for the management of patients with ST-elevation MI (3,4), solely on the basis of an abnormal screening study, rather than
and for patients with UA, the reader is referred to the on the basis of clinical symptoms or events such as anginal
ACCF/AHA Guidelines for the Management of Patients symptoms or ACS. Multiple ACCF/AHA guidelines and
With Unstable Angina/NonST-Elevation Myocardial In- scientific statements have discouraged the use of ambulatory
farction (5,5a). There are, however, patients with UA who can monitoring, treadmill testing, stress echocardiography, stress
be categorized as low risk and are addressed in this guideline myocardial perfusion imaging (MPI), and computed tomog-
(Table 2). raphy scoring of coronary calcium or coronary angiography as
A key premise of this guideline is that once a diagnosis of routine screening tests in asymptomatic individuals.
IHD is established, it is necessary in most patients to assess When patients with documented IHD develop recurrent
their risk of subsequent complications, such as acute myo- chest pain, the symptoms still could be attributable to
cardial infarction or death. Because the approach to diag- another condition. Such patients are included in this guide-
nosis of suspected IHD and the assessment of risk in a line if there is sufficient suspicion that their heart disease is
patient with known IHD are conceptually different and are a likely source of symptoms to warrant cardiac evaluation.
based on different literature, these issues are addressed Just as in the case of patients with new-onset chest pain, if
separately. A clinician might, however, select a procedure for the pain seems to be cardiac in origin, the clinician must
a patient with a moderate to high pretest likelihood of IHD to determine whether such recurrent or worsening pain is
provide information for both diagnosis and risk assessment, consistent with ACS or simply represents symptoms more
whereas in a patient with a low likelihood of IHD, it could be consistent with chronic stable angina that do not require
sensible to select a test simply for diagnostic purposes without emergent attention.
regard to risk assessment. The purpose of this dichotomy is to The approach to screening and management of asymp-
promote the sensible application of appropriate testing rather tomatic patients who are at risk for IHD but who are not
than routine use of the most expensive or complex tests known to have IHD is beyond the scope of this guideline,
whether warranted or not. but it is addressed in the ACCF/AHA Guideline for
Table 2. Short-Term Risk of Death or Nonfatal MI in Patients With UA/NSTEMI
High Risk Intermediate Risk Low Risk
No high- or intermediate-risk
At least 1 of the following features must No high-risk features are present, but patient features are present, but patient
Feature be present: must have 1 of the following: may have any of the following:
History Accelerating tempo of ischemic symptoms Prior MI, peripheral or cerebrovascular disease, N/A
in preceding 48 h or CABG
Prior aspirin use
Characteristics of pain Prolonged ongoing (20 min) rest pain Prolonged (20 min) rest angina, now resolved, Increased angina frequency, severity,
with moderate or high likelihood of CAD or duration
Rest angina (20 min) or relieved with rest or Angina provoked at a lower
sublingual NTG threshold
Nocturnal angina New-onset angina with onset 2 wk to
New-onset or progressive CCS Class III or IV 2 mo before presentation
angina in previous 2 wk without prolonged
(20 min) rest pain but with intermediate or
high likelihood of CAD
Clinical findings Pulmonary edema, most likely due to Age 70 y N/A
ischemia
New or worsening mitral regurgitation
murmur
S3 or new/worsening rales
Hypotension, bradycardia, or tachycardia
Age 75 y
ECG Angina at rest with transient ST-segment T-wave changes Normal or unchanged ECG
changes 0.5 mm Pathological Q waves or resting ST-depression
Bundle-branch block, new or presumed new 1 mm in multiple lead groups (anterior,
Sustained ventricular tachycardia inferior, lateral)
Cardiac markers Elevated cardiac TnT, TnI, or CK-MB Slightly elevated cardiac TnT, TnI, or CK-MB Normal
(i.e., TnT or TnI 0.1 ng/mL) (i.e., TnT 0.01 but 0.1 ng/mL)
Estimation of the short-term risks of death and nonfatal cardiac ischemic events in UA or NSTEMI is a complex multivariable problem that cannot be fully specified in a table such as this. Therefore,
the table is meant to offer general guidance and illustration rather than rigid algorithms.
CABG indicates coronary artery bypass graft; CAD, coronary artery disease; CCS, Canadian Cardiovascular Society; CK-MB, creatine kinase-MB fraction; ECG, electrocardiogram; MI, myocardial
infarction; NTG, nitroglycerin; N/A, not available; TnI, troponin I; TnT, troponin T; and UA/NSTEMI, unstable angina/nonST-elevation myocardial infarction.
Modified from Braunwald et al. (7).
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2571
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
Assessment of Cardiovascular Risk in Asymptomatic age, approximately 23% of men and 15% of women have
Adults (6). Similarly, the present guideline does not prevalent IHD, and these figures rise to 33% and 22%
apply to patients with chest pain symptoms early after among men and women 80 years of age, respectively (27).
revascularization, that is, within 6 months of revascular- Although the survival rate of patients with IHD has been
ization. steadily improving (28), it was still responsible for nearly
1.5. General Approach and Overlap With
380,000 deaths in the United States in 2010, with an
Other Guidelines or Statements
age-adjusted mortality rate of 113 per 100,000 population
(29). Although IHD is widely known to be the number 1
This guideline overlaps with numerous clinical practice cause of death in men, this is also the case for women,
guidelines published by the ACCF/AHA Task Force on among whom this condition accounts for 27% of deaths
Practice Guidelines; the National Heart, Lung, and Blood (compared with 22% due to cancer) (30). IHD also accounts
Institute; and the ACP (Table 3). To maintain consistency, for the vast majority of the mortality and morbidity of
the writing committee worked with members of other cardiac disease. Each year, 1.5 million patients have an
committees to harmonize recommendations and eliminate MI. Many more are hospitalized for UA and evaluation and
discrepancies. treatment of stable chest pain syndromes. Patients who have
This document recommends a combination of lifestyle had ACS, such as acute MI, remain at risk for recurrent
modifications and medications that constitute GDMT. events even if they have no, or limited, symptoms, and they
Recommendations for risk reduction are consistent with the should be considered to have SIHD.
AHA/ACCF Secondary Prevention and Risk Reduction In approximately 50% of patients, angina pectoris is the
Therapy for Patients With Coronary and Other Vascular initial manifestation of IHD (27). The incidence of angina
Disease: 2011 Update (8). Recommendations related to rises continuously with age in women, whereas the inci-
revascularization are the result of collaboration discussions dence of angina in men peaks between 55 and 65 years of
among several writing committees, including those address- age before declining (27). It has been estimated that there
ing SIHD, PCI, CABG, and unstable angina/nonST- are 30 patients with stable angina for every patient hospi-
elevation MI. To the fullest extent possible, these guidelines
talized with infarction, and symptoms in many of these
are consistent with the appropriate use criteria documents
patients are poorly controlled (3133). The direct and
for imaging testing, diagnostic catheterization, and coronary
indirect costs of caring for patients with IHD are estimated
revascularization that are also sponsored by the ACCF
to exceed $150 billion in the United States.
(9 14).
1.6. Magnitude of the Problem 1.7. Organization of the Guideline
It is estimated that 1 in 3 adults in the United States (about The overarching framework adopted in this guideline re-
71 million) has some form of cardiovascular disease, includ- flects the complementary goals of treating patients with
ing 13 million with CAD and nearly 9 million with known SIHD, alleviating or improving symptoms, and
angina pectoris (26,27). Among persons 60 to 79 years of prolonging life. This guideline is divided into 4 basic
Table 3. Associated Guidelines and Statements
Publication
Document Reference(s) Organization Year
Guidelines
Chronic Stable Angina: 2007 Focused Update (15) ACCF/AHA 2007
Valvular Heart Disease (16) ACCF/AHA 2008
Heart Failure: 2009 Update (17) ACCF/AHA 2009
STEMI (3,4,18) ACCF/AHA 2009
Assessment of Cardiovascular Risk in Asymptomatic Adults (6) ACCF/AHA 2010
Coronary Artery Bypass Graft Surgery (19) ACCF/AHA 2011
Percutaneous Coronary Intervention (20) ACCF/AHA/SCAI 2011
Secondary Prevention and Risk Reduction Therapy for Patients With Coronary and (8) AHA/ACCF 2011
Other Atherosclerotic Vascular Disease
UA/NSTEMI: 2007 and 2012 Updates (5,5a) ACCF/AHA 2012
Statements
NCEP ATP III Implications of Recent Clinical Trials (22,23) NHLBI 2004
National Hypertension Education Program (JNC VII) (24) NHLBI 2004
Referral, Enrollment, and Delivery of Cardiac Rehabilitation/Secondary Prevention Programs at (25) AHA 2011
Clinical Centers and Beyond: A Presidential Advisory From the AHA
ACCF indicates American College of Cardiology Foundation; AHA, American Heart Association; ATP III, Adult Treatment Panel 3; JNC VII, The Seventh Report of the Joint National Committee on
Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; NHLBI, National Heart, Lung and Blood Institute; and SCAI, Society for Cardiovascular Angiography and Interventions.
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2572 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
sections summarizing the approaches to diagnosis, risk the patient has an interpretable ECG and at least moderate physical
assessment, treatment, and follow-up summarized in 5 functioning or no disabling comorbidity. (Level of Evidence: C)
algorithms: diagnosis (Figure 2), risk assessment (Figure 3), 2. Exercise stress with nuclear MPI or echocardiography is reasonable
GDMT (Figure 4), and revascularization (Figures 5 and 6). for patients with an intermediate to high pretest probability of
In clinical practice, steps delineated in the algorithms often obstructive IHD who have an interpretable ECG and at least moder-
overlap. An essential principle that transcends all recommen- ate physical functioning or no disabling comorbidity (4353). (Level
dations in this guideline is that of informing and involving of Evidence: B)
patients in all decisions that affect them, directly or indirectly, 3. Pharmacological stress with CMR can be useful for patients with an
as summarized in the following recommendation: intermediate to high pretest probability of obstructive IHD who have
an uninterpretable ECG and at least moderate physical functioning
1.8. Vital Importance of Involvement by an or no disabling comorbidity (50,54,55). (Level of Evidence: B)
Informed Patient: Recommendation
CLASS IIb
CLASS I
1. CCTA might be reasonable for patients with an intermediate pretest
1. Choices about diagnostic and therapeutic options should be made
probability of IHD who have at least moderate physical functioning
through a process of shared decision making involving the patient
or no disabling comorbidity (5563). (Level of Evidence: B)
and provider, with the provider explaining information about risks,
benefits, and costs to the patient. (Level of Evidence: C) 2. For patients with a low pretest probability of obstructive IHD who do
require testing, standard exercise stress echocardiography might be
reasonable, provided the patient has an interpretable ECG and at
2. Diagnosis of SIHD: Recommendations
least moderate physical functioning or no disabling comorbidity.
(Level of Evidence: C)
2.1. Clinical Evaluation of Patients With Chest Pain
CLASS III: No Benefit
2.1.1. Clinical Evaluation in the Initial Diagnosis of 1. Pharmacological stress with nuclear MPI, echocardiography, or
SIHD in Patients With Chest Pain CMR is not recommended for patients who have an interpretable
CLASS I ECG and at least moderate physical functioning or no disabling
1. Patients with chest pain should receive a thorough history and comorbidity (52,64,65). (Level of Evidence: C)
physical examination to assess the probability of IHD before addi- 2. Exercise stress with nuclear MPI is not recommended as an initial
tional testing (34). (Level of Evidence: C) test in low-risk patients who have an interpretable ECG and at least
2. Patients who present with acute angina should be categorized as moderate physical functioning or no disabling comorbidity. (Level of
stable or unstable; patients with UA should be further categorized as Evidence: C)
being at high, moderate, or low risk (5,5a). (Level of Evidence: C)
2.1.3.2. UNABLE TO EXERCISE
2.1.2. Electrocardiography
CLASS I
2.1.2.1. RESTING ELECTROCARDIOGRAPHY TO ASSESS RISK
1. Pharmacological stress with nuclear MPI or echocardiography is
CLASS I recommended for patients with an intermediate to high pretest
1. A resting ECG is recommended in patients without an obvious, probability of IHD who are incapable of at least moderate physical
noncardiac cause of chest pain (3638). (Level of Evidence: B) functioning or have disabling comorbidity (43,46,47,4953). (Level
2.1.3. Stress Testing and Advanced Imaging for Initial of Evidence: B)
Diagnosis in Patients With Suspected SIHD Who CLASS IIa
Require Noninvasive Testing 1. Pharmacological stress echocardiography is reasonable for patients
See Table 4 for a summary of recommendations from this with a low pretest probability of IHD who require testing and are
section. incapable of at least moderate physical functioning or have dis-
abling comorbidity. (Level of Evidence: C)
2.1.3.1. ABLE TO EXERCISE 2. CCTA is reasonable for patients with a low to intermediate pretest
CLASS I probability of IHD who are incapable of at least moderate physical
1. Standard exercise ECG testing is recommended for patients with an functioning or have disabling comorbidity (5563). (Level of Evi-
intermediate pretest probability of IHD who have an interpretable dence: B)
ECG and at least moderate physical functioning or no disabling 3. Pharmacological stress CMR is reasonable for patients with an
comorbidity (3942). (Level of Evidence: A) intermediate to high pretest probability of IHD who are incapable of
2. Exercise stress with nuclear MPI or echocardiography is recom- at least moderate physical functioning or have disabling comorbid-
mended for patients with an intermediate to high pretest probability ity (50,54,55,6669). (Level of Evidence: B)
of IHD who have an uninterpretable ECG and at least moderate
physical functioning or no disabling comorbidity (4353). (Level of CLASS III: No Benefit
Evidence: B) 1. Standard exercise ECG testing is not recommended for patients who
CLASS IIa have an uninterpretable ECG or are incapable of at least moderate
1. For patients with a low pretest probability of obstructive IHD who do physical functioning or have disabling comorbidity (4353,58).
require testing, standard exercise ECG testing can be useful, provided (Level of Evidence: C)
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2573
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
Figure 2. Diagnosis of Patients with Suspected IHD
Colors correspond to the class of recommendations in the ACCF/AHA Table 1. The algorithms do not represent a comprehensive list of recommendations (see full guideline
text [2] for all recommendations). See Table 2 for short-term risk of death or nonfatal MI in patients with UA/NSTEMI. CCTA is reasonable only for patients with intermedi-
ate probability of IHD. CCTA indicates computed coronary tomography angiography; CMR, cardiac magnetic resonance; ECG, electrocardiogram; Echo, echocardiography; IHD,
ischemic heart disease; MI, myocardial infarction; MPI, myocardial perfusion imaging; Pharm, pharmacological; UA, unstable angina; and UA/NSTEMI, unstable angina/non
ST-elevation myocardial infarction.
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2574 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
Figure 3. Algorithm for Risk Assessment of Patients With SIHD*
*Colors correspond to the class of recommendations in the ACCF/AHA Table 1. The algorithms do not represent a comprehensive list of recommendations (see full guideline
text [2] for all recommendations). CCTA indicates coronary computed tomography angiography; CMR, cardiac magnetic resonance; ECG, electrocardiogram; Echo, echocardi-
ography; LBBB, left bundle-branch block; MPI, myocardial perfusion imaging; and Pharm, pharmacological.
2.1.3.3. OTHER 3. Risk Assessment: Recommendations
CLASS IIa
1. CCTA is reasonable for patients with an intermediate pretest prob-
ability of IHD who a) have continued symptoms with prior normal 3.1. Advanced Testing: Resting and
test findings, or b) have inconclusive results from prior exercise or Stress Noninvasive Testing
pharmacological stress testing, or c) are unable to undergo stress
3.1.1. Resting Imaging to Assess Cardiac
with nuclear MPI or echocardiography (70). (Level of Evidence: C)
Structure and Function
CLASS IIb
1. For patients with a low to intermediate pretest probability of ob- CLASS I
structive IHD, noncontrast cardiac computed tomography to deter- 1. Assessment of resting left ventricular (LV) systolic and diastolic
mine the coronary artery calcium score may be considered (71). ventricular function and evaluation for abnormalities of myocar-
(Level of Evidence: C) dium, heart valves, or pericardium are recommended with the use
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2575
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
Figure 4. Algorithm for Guideline-Directed Medical Therapy for Patients With SIHD*
*Colors correspond to the class of recommendations in the ACCF/AHA Table 1. The algorithms do not represent a comprehensive list of recommendations (see full guideline
text [2] for all recommendations). The use of bile acid sequestrant is relatively contraindicated when triglycerides are 200 mg/dL and is contraindicated when triglycer-
ides are 500 mg/dL. Dietary supplement niacin must not be used as a substitute for prescription niacin.ACCF indicates American College of Cardiology Foundation; ACEI,
angiotensin-converting enzyme inhibitor; AHA, American Heart Association; ARB, angiotensin-receptor blocker; ASA, aspirin, ATP III, Adult Treatment Panel 3; BP, blood pres-
sure; CCB, calcium channel blocker; CKD, chronic kidney disease; HDL-C, high-density lipoprotein cholesterol, JNC VII, Seventh Report of the Joint National Committee on
Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; LDL-C, low-density lipoprotein cholesterol; LV, left ventricular; MI, myocardial infarction; NHLBI,
National Heart, Lung, and Blood Institute; and NTG, nitroglycerin.
of Doppler echocardiography in patients with known or suspected 2. Routine reassessment (1 year) of LV function with technologies
IHD and a prior MI, pathological Q waves, symptoms or signs such as echocardiography radionuclide imaging, CMR, or cardiac
suggestive of heart failure, complex ventricular arrhythmias, or an computed tomography is not recommended in patients with no
undiagnosed heart murmur (17,36,37,72,73). (Level of Evidence: B) change in clinical status and for whom no change in therapy is
contemplated. (Level of Evidence: C)
CLASS IIb
1. Assessment of cardiac structure and function with resting echocar- 3.1.2. Stress Testing and Advanced Imaging in
diography may be considered in patients with hypertension or Patients With Known SIHD Who Require
diabetes mellitus and an abnormal ECG. (Level of Evidence: C) Noninvasive Testing for Risk Assessment
2. Measurement of LV function with radionuclide imaging may be
considered in patients with a prior MI or pathological Q waves,
See Table 5 for a summary of recommendations from this
provided there is no need to evaluate symptoms or signs suggestive
section.
of heart failure, complex ventricular arrhythmias, or an undiagnosed 3.1.2.1. RISK ASSESSMENT IN PATIENTS ABLE TO EXERCISE
heart murmur. (Level of Evidence: C)
CLASS I
CLASS III: No Benefit 1. Standard exercise ECG testing is recommended for risk assess-
1. Echocardiography, radionuclide imaging, CMR, and cardiac com- ment in patients with SIHD who are able to exercise to an
puted tomography are not recommended for routine assessment of adequate workload and have an interpretable ECG (41,45,7482).
LV function in patients with a normal ECG, no history of MI, no (Level of Evidence: B)
symptoms or signs suggestive of heart failure, and no complex 2. The addition of either nuclear MPI or echocardiography to stan-
ventricular arrhythmias. (Level of Evidence: C) dard exercise ECG testing is recommended for risk assessment in
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2576 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
Figure 5. Algorithm for Revascularization to Improve Survival of Patients With SIHD*
*Colors correspond to the class of recommendations in the ACCF/AHA Table 1. The algorithms do not represent a comprehensive list of recommendations (see full guideline
text [2] for all recommendations).
patients with SIHD who are able to exercise to an adequate CLASS III: No Benefit
workload but have an uninterpretable ECG not due to left bundle- 1. Pharmacological stress imaging (nuclear MPI, echocardiography, or
branch block or ventricular pacing (8387,117119). (Level of CMR) or CCTA is not recommended for risk assessment in patients
Evidence: B) with SIHD who are able to exercise to an adequate workload and
have an interpretable ECG. (Level of Evidence: C)
CLASS IIa
1. The addition of either nuclear MPI or echocardiography to standard 3.1.2.2. RISK ASSESSMENT IN PATIENTS UNABLE TO EXERCISE
exercise ECG testing is reasonable for risk assessment in patients
with SIHD who are able to exercise to an adequate workload and CLASS I
have an interpretable ECG (8897). (Level of Evidence: B) 1. Pharmacological stress with either nuclear MPI or echocardiogra-
2. CMR with pharmacological stress is reasonable for risk assessment phy is recommended for risk assessment in patients with SIHD who
in patients with SIHD who are able to exercise to an adequate are unable to exercise to an adequate workload regardless of
workload but have an uninterpretable ECG (97102). (Level of interpretability of ECG (8386,105108). (Level of Evidence: B)
Evidence: B)
CLASS IIa
CLASS IIb 1. Pharmacological stress CMR is reasonable for risk assessment in
1. CCTA may be reasonable for risk assessment in patients with SIHD patients with SIHD who are unable to exercise to an adequate
who are able to exercise to an adequate workload but have an workload regardless of interpretability of ECG (98102,109). (Level
uninterpretable ECG (103,104). (Level of Evidence: B) of Evidence: B)
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2577
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
Figure 6. Algorithm for Revascularization to Improve Symptoms of Patients With SIHD*
*Colors correspond to the class of recommendations in the ACCF/AHA Table 1. The algorithms do not represent a comprehensive list of recommendations (see full guideline
text [2] for all recommendations). CABG indicates coronary artery bypass graft; and PCI, percutaneous coronary intervention.
2. CCTA can be useful as a first-line test for risk assessment in patients larization of known coronary stenosis of unclear physiological sig-
with SIHD who are unable to exercise to an adequate workload nificance (84,96,111,112). (Level of Evidence: B)
regardless of interpretability of ECG (104). (Level of Evidence: C) CLASS IIa
1. CCTA can be useful for risk assessment in patients with SIHD who have an
indeterminate result from functional testing (104). (Level of Evidence: C)
3.1.2.3. RISK ASSESSMENT REGARDLESS OF PATIENTS ABILITY TO EXERCISE
CLASS IIb
CLASS I 1. CCTA might be considered for risk assessment in patients with SIHD
1. Pharmacological stress with either nuclear MPI or echocardiogra- unable to undergo stress imaging or as an alternative to invasive
phy is recommended for risk assessment in patients with SIHD who coronary angiography when functional testing indicates a moderate- to
have left bundle-branch block on ECG, regardless of ability to high-risk result and knowledge of angiographic coronary anatomy is
exercise to an adequate workload (105108,110). (Level of Evi- unknown. (Level of Evidence: C)
dence: B) CLASS III: No Benefit
2. Either exercise or pharmacological stress with imaging (nuclear 1. A request to perform either a) more than 1 stress imaging study or b) a
MPI, echocardiography, or CMR) is recommended for risk assess- stress imaging study and a CCTA at the same time is not recommended
ment in patients with SIHD who are being considered for revascu- for risk assessment in patients with SIHD. (Level of Evidence: C)
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2578 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
Table 4. Stress Testing and Advanced Imaging for Initial Diagnosis in Patients With Suspected SIHD
Who Require Noninvasive Testing
Exercise ECG
Status Interpretable Pretest Probability of IHD
Test Able Unable Yes No Low Intermediate High COR LOE References
Patients able to exercise*
Exercise ECG X X X I A (3942)
Exercise with nuclear MPI or Echo X X X X I B (4353)
Exercise ECG X X X IIa C N/A
Exercise with nuclear MPI or Echo X X X X IIa B (4353)
Pharmacological stress CMR X X X X IIa B (50,54,55)
CCTA X Any X IIb B (5563)
Exercise Echo X X X IIb C N/A
Pharmacological stress with nuclear X X Any III: No Benefit C (52,64,65)
MPI, Echo, or CMR
Exercise stress with nuclear MPI X X X III: No Benefit C N/A
Patients unable to exercise
Pharmacological stress with nuclear X Any X X I B (43,46,47,4953)
MPI or Echo
Pharmacological stress Echo X Any X IIa C N/A
CCTA X Any X X IIa B (5563)
Pharmacological stress CMR X Any X X IIa B (50,54,55,6669)
Exercise ECG X X Any III: No Benefit C (4353,58)
Other
CCTA Any Any X IIa C (70)
If patient has any of the following:
a) Continued symptoms with prior
normal test, or
b) Inconclusive exercise or
pharmacological stress, or
c) Unable to undergo stress with MPI
or Echo
CAC score Any Any X IIb C (71)
*Patients are candidates for exercise testing if they are capable of performing at least moderate physical functioning (i.e., moderate household, yard, or recreational work and most activities of daily
living) and have no disabling comorbidity. Patients should be able to achieve 85% of age-predicted maximum heart rate.
CAC indicates coronary artery calcium; CCTA, cardiac computed tomography angiography; CMR, cardiac magnetic resonance imaging; COR, class of recommendation; ECG, electrocardiogram; Echo,
echocardiography; IHD, ischemic heart disease; LOE, level of evidence; MPI, myocardial perfusion imaging; N/A, not available, and SIHD, stable ischemic heart disease.
3.2. Coronary Angiography CLASS IIa
1. Coronary angiography is reasonable to further assess risk in pa-
3.2.1. Coronary Angiography as an Initial Testing tients with SIHD who have depressed LV function (ejection fraction
Strategy to Assess Risk 50%) and moderate risk criteria on noninvasive testing with
demonstrable ischemia (137139). (Level of Evidence: C)
CLASS I
2. Coronary angiography is reasonable to further assess risk in pa-
1. Patients with SIHD who have survived sudden cardiac death or
tients with SIHD and inconclusive prognostic information after
potentially life-threatening ventricular arrhythmia should undergo
noninvasive testing or in patients for whom noninvasive testing is
coronary angiography to assess cardiac risk (121123). (Level of
contraindicated or inadequate. (Level of Evidence: C)
Evidence: B)
3. Coronary angiography for risk assessment is reasonable for
2. Patients with SIHD who develop symptoms and signs of heart failure
patients with SIHD who have unsatisfactory quality of life due to
should be evaluated to determine whether coronary angiography
angina, have preserved LV function (ejection fraction 50%), and
should be performed for risk assessment (124127). (Level of
have intermediate risk criteria on noninvasive testing (140,141).
Evidence: B)
(Level of Evidence: C)
3.2.2. Coronary Angiography to Assess Risk After CLASS III: No Benefit
Initial Workup With Noninvasive Testing 1.
Coronary angiography for risk assessment is not recommended in
CLASS I patients with SIHD who elect not to undergo revascularization or
1. Coronary arteriography is recommended for patients with SIHD who are not candidates for revascularization because of comorbidi-
whose clinical characteristics and results of noninvasive testing ties or individual preferences (140,141). (Level of Evidence: B)
indicate a high likelihood of severe IHD and when the benefits are 2. Coronary angiography is not recommended to further assess risk in
deemed to exceed risk (38,72,128136). (Level of Evidence: C) patients with SIHD who have preserved LV function (ejection frac-
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2579
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
Table 5. Using Stress Testing and Advanced Imaging for Patients With Known SIHD Who Require Noninvasive Testing for Risk
Assessment
Exercise ECG
Status Interpretable
Test Able Unable Yes No COR LOE References Additional Considerations
Patients able to exercise*
Exercise ECG X X I B (41,45,7482)
Exercise with nuclear MPI or X X I B (8387,117119) Abnormalities other than LBBB or
Echo ventricular pacing
Exercise with nuclear MPI or X X IIa B (8897)
Echo
Pharmacological stress CMR X X IIa B (97102)
CCTA X X IIb B (103,104)
Pharmacological stress X X III: No Benefit C N/A
imaging (nuclear MPI, Echo,
CMR) or CCTA
Patients unable to exercise
Pharmacological stress with X Any I B (8386,105108)
nuclear MPI or Echo
Pharmacological stress CMR X Any IIa B (98102,109)
CCTA X Any IIa C (104) Without prior stress test
Regardless of patients ability to exercise
Pharmacological stress with Any X I B (105108,110) LBBB present
nuclear MPI or Echo
Exercise/pharmacological Any Any I B (84,96,111,112) Known coronary stenosis of unclear
stress with nuclear MPI, physiological significance being
Echo, or CMR considered for revascularization
CCTA Any Any IIa C N/A Indeterminate result from
functional testing
CCTA Any Any IIb C N/A Unable to undergo stress imaging
or as alternative to coronary
catheterization when functional
testing indicates moderate to
high risk and angiographic
coronary anatomy is unknown
Requests to perform multiple Any Any III: No Benefit C N/A
cardiac imaging or stress
studies at the same time
CCTA indicates cardiac computed tomography angiography; CMR, cardiac magnetic resonance imaging; COR, class of recommendation; ECG, electrocardiogram; Echo, echocardiography; LBBB, left
bundle-branch block; LOE, level of evidence; MPI, myocardial perfusion imaging; and N/A, not available.
*Patients are candidates for exercise testing if they are capable of performing at least moderate physical functioning (i.e., moderate household, yard, or recreational work and most activities of daily
living) and have no disabling comorbidity. Patients should be able to achieve 85% of age-predicted maximum heart rate.
tion 50%) and low-risk criteria on noninvasive testing (140,141). b. an explanation of medication management and cardiovascular
(Level of Evidence: B) risk reduction strategies in a manner that respects the patients
3. Coronary angiography is not recommended to assess risk in pa- level of understanding, reading comprehension, and ethnicity
tients who are at low risk according to clinical criteria and who have (8,145149) (Level of Evidence: B);
not undergone noninvasive risk testing. (Level of Evidence: C) c. a comprehensive review of all therapeutic options (8,146149)
4. Coronary angiography is not recommended to assess risk in asymp- (Level of Evidence: B);
tomatic patients with no evidence of ischemia on noninvasive d. a description of appropriate levels of exercise, with encourage-
testing. (Level of Evidence: C) ment to maintain recommended levels of daily physical activity
(8,150153) (Level of Evidence: C);
4. Treatment: Recommendations e. introduction to self-monitoring skills (150,152,153) (Level of
Evidence: C); and
f. information on how to recognize worsening cardiovascular symp-
4.1. Patient Education
toms and take appropriate action. (Level of Evidence: C)
CLASS I
1. Patients with SIHD should have an individualized education plan to 2. Patients with SIHD should be educated about the following lifestyle
optimize care and promote wellness, including: elements that could influence prognosis: weight control, mainte-
a. education on the importance of medication adherence for man- nance of a body mass index of 18.5 to 24.9 kg/m2, and mainte-
aging symptoms and retarding disease progression (142144) nance of a waist circumference less than 102 cm (40 inches) in
(Level of Evidence: C); men and less than 88 cm (35 inches) in women (less for certain
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2580 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
racial groups) (8,145,154157); lipid management (23); blood ers, with addition of other drugs, such as thiazide diuretics or
pressure control (24,158); smoking cessation and avoidance of expo- calcium channel blockers, if needed to achieve a goal blood pres-
sure to secondhand smoke (8,159,160); and individualized medical, sure of less than 140/90 mm Hg (203,204). (Level of Evidence: B)
nutrition, and lifestyle changes for patients with diabetes mellitus to
4.2.1.3. DIABETES MANAGEMENT
supplement diabetes treatment goals and education (161). (Level of
Evidence: C) CLASS IIa
1. For selected individual patients, such as those with a short duration
CLASS IIa of diabetes mellitus and a long life expectancy, a goal hemoglobin
1. It is reasonable to educate patients with SIHD about
A1c of 7% or less is reasonable (205207). (Level of Evidence: B)
a. adherence to a diet that is low in saturated fat, cholesterol, and
2. A goal hemoglobin A1c between 7% and 9% is reasonable for
trans fat; high in fresh fruits, whole grains, and vegetables; and
certain patients according to age, history of hypoglycemia, presence
reduced in sodium intake, with cultural and ethnic preferences
of microvascular or macrovascular complications, or presence of
incorporated (8,23,24,162,163) (Level of Evidence: B);
coexisting medical conditions (208,209). (Level of Evidence: C)
b. common symptoms of stress and depression to minimize stress-
related angina symptoms (164) (Level of Evidence: C); CLASS IIb
c. comprehensive behavioral approaches for the management of 1. Initiation of pharmacotherapy interventions to achieve target hemoglo-
stress and depression (165168) (Level of Evidence: C); and bin A1c might be reasonable (161,210219). (Level of Evidence: A)
d. evaluation and treatment of major depressive disorder when CLASS III: Harm
indicated (142,165,167,169,170,173175). (Level of Evi- 1. Therapy with rosiglitazone should not be initiated in patients with
dence: B) SIHD (220,221). (Level of Evidence: C)
4.2. Guideline-Directed Medical Therapy 4.2.1.4. PHYSICAL ACTIVITY
4.2.1. Risk Factor Modification CLASS I
1. For all patients, the clinician should encourage 30 to 60 minutes of
4.2.1.1. LIPID MANAGEMENT moderate-intensity aerobic activity, such as brisk walking, at least 5
days and preferably 7 days per week, supplemented by an increase
CLASS I
1. Lifestyle modifications, including daily physical activity and weight in daily lifestyle activities (e.g., walking breaks at work, gardening,
management, are strongly recommended for all patients with SIHD household work) to improve cardiorespiratory fitness and move
(23,176). (Level of Evidence: B) patients out of the least-fit, least-active, high-risk cohort (bottom
2. Dietary therapy for all patients should include reduced intake of 20%) (222224). (Level of Evidence: B)
saturated fats (to 7% of total calories), trans fatty acids (to 1% 2. For all patients, risk assessment with a physical activity history
of total calories), and cholesterol (to 200 mg/d) (23,177180). and/or an exercise test is recommended to guide prognosis and
(Level of Evidence: B) prescription (225228). (Level of Evidence: B)
3. In addition to therapeutic lifestyle changes, a moderate or high dose 3. Medically supervised programs (cardiac rehabilitation) and physician-
of a statin therapy should be prescribed, in the absence of contra- directed, home-based programs are recommended for at-risk patients
indications or documented adverse effects (23,163,181183). at first diagnosis (222,229, 230). (Level of Evidence: A)
(Level of Evidence: A) CLASS IIa
1. It is reasonable for the clinician to recommend complementary
CLASS IIa
resistance training at least 2 days per week (231,232). (Level of
1. For patients who do not tolerate statins, low-density lipoprotein-
Evidence: C)
cholesterollowering therapy with bile acid sequestrants,* niacin,
or both is reasonable (184,186,187). (Level of Evidence: B) 4.2.1.5. WEIGHT MANAGEMENT
4.2.1.2. BLOOD PRESSURE MANAGEMENT CLASS I
1. Body mass index and/or waist circumference should be assessed at
CLASS I every visit, and the clinician should consistently encourage weight
1. All patients should be counseled about the need for lifestyle modi- maintenance or reduction through an appropriate balance of life-
fication: weight control; increased physical activity; alcohol moder- style physical activity, structured exercise, caloric intake, and formal
ation; sodium reduction; and emphasis on increased consumption behavioral programs when indicated to maintain or achieve a body
of fresh fruits, vegetables, and low-fat dairy products (24,188196). mass index between 18.5 and 24.9 kg/m2 and a waist circumfer-
(Level of Evidence: B) ence less than 102 cm (40 inches) in men and less than 88 cm (35
2. In patients with SIHD with blood pressure 140/90 mm Hg or inches) in women (less for certain racial groups) (154,233241).
higher, antihypertensive drug therapy should be instituted in (Level of Evidence: B)
addition to or after a trial of lifestyle modifications (197202). 2. The initial goal of weight loss therapy should be to reduce body weight
(Level of Evidence: A) by approximately 5% to 10% from baseline. With success, further
3. The specific medications used for treatment of high blood pressure weight loss can be attempted if indicated. (Level of Evidence: C)
should be based on specific patient characteristics and may include
angiotensin-converting enzyme (ACE) inhibitors and/or beta block- 4.2.1.6. SMOKING CESSATION COUNSELING
*The use of bile acid sequestrant is relatively contraindicated when triglycerides are CLASS I
200 mg/dL and is contraindicated when triglycerides are 500 mg/dL. 1. Smoking cessation and avoidance of exposure to environmental
Dietary supplement niacin must not be used as a substitute for prescription niacin. tobacco smoke at work and home should be encouraged for all
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2581
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
patients with SIHD. Follow-up, referral to special programs, and CLASS IIb
pharmacotherapy are recommended, as is a stepwise strategy for 1. Beta blockers may be considered as chronic therapy for all other
smoking cessation (Ask, Advise, Assess, Assist, Arrange, Avoid) patients with coronary or other vascular disease. (Level of Evidence: C)
(242244). (Level of Evidence: B)
4.2.2.3. RENIN-ANGIOTENSIN-ALDOSTERONE BLOCKER THERAPY
4.2.1.7. MANAGEMENT OF PSYCHOLOGICAL FACTORS CLASS I
1. ACE inhibitors should be prescribed in all patients with SIHD who
CLASS IIa
1. It is reasonable to consider screening SIHD patients for depression also have hypertension, diabetes mellitus, LV ejection fraction 40%
and to refer or treat when indicated (162,165,169,245248). (Level or less, or chronic kidney disease, unless contraindicated (113
of Evidence: B) 116,120). (Level of Evidence: A)
2. Angiotensin-receptor blockers are recommended for patients with
CLASS IIb SIHD who have hypertension, diabetes mellitus, LV systolic dysfunc-
1. Treatment of depression has not been shown to improve cardiovas- tion, or chronic kidney disease and have indications for, but are
cular disease outcomes but might be reasonable for its other intolerant of, ACE inhibitors (272274). (Level of Evidence: A)
clinical benefits (165,173,249). (Level of Evidence: C)
CLASS IIa
4.2.1.8. ALCOHOL CONSUMPTION 1. Treatment with an ACE inhibitor is reasonable in patients with both
SIHD and other vascular disease (275,276). (Level of Evidence: B)
CLASS IIb 2. It is reasonable to use angiotensin-receptor blockers in other pa-
1. In patients with SIHD who use alcohol, it might be reasonable for
tients who are ACE inhibitor intolerant (277). (Level of Evidence: C)
nonpregnant women to have 1 drink (4 ounces of wine, 12 ounces
of beer, or 1 ounce of spirits) a day and for men to have 1 or 2 drinks 4.2.2.4. INFLUENZA VACCINATION
a day, unless alcohol is contraindicated (such as in patients with a
CLASS I
history of alcohol abuse or dependence or with liver disease)
1. An annual influenza vaccine is recommended for patients with SIHD
(250252). (Level of Evidence: C)
(278282). (Level of Evidence: B)
4.2.1.9. AVOIDING EXPOSURE TO AIR POLLUTION
4.2.2.5. ADDITIONAL THERAPY TO REDUCE RISK OF MI AND DEATH
CLASS IIa
CLASS III: No Benefit
1. It is reasonable for patients with SIHD to avoid exposure to in- 1. Estrogen therapy is not recommended in postmenopausal women
creased air pollution to reduce the risk of cardiovascular events with SIHD with the intent of reducing cardiovascular risk or improv-
(253256). (Level of Evidence: C) ing clinical outcomes (283286). (Level of Evidence: A)
4.2.2. Additional Medical Therapy to 2. Vitamin C, vitamin E, and beta-carotene supplementation are not
recommended with the intent of reducing cardiovascular risk or
Prevent MI and Death
improving clinical outcomes in patients with SIHD (181,287291).
4.2.2.1. ANTIPLATELET THERAPY (Level of Evidence: A)
3. Treatment of elevated homocysteine with folate or vitamins B6 and
CLASS I
B12 is not recommended with the intent of reducing cardiovascular
1. Treatment with aspirin 75 to 162 mg daily should be continued
risk or improving clinical outcomes in patients with SIHD (292295).
indefinitely in the absence of contraindications in patients with SIHD
(Level of Evidence: A)
(257,258). (Level of Evidence: A)
4. Chelation therapy is not recommended with the intent of improving
2. Treatment with clopidogrel is reasonable when aspirin is contrain-
symptoms or reducing cardiovascular risk in patients with SIHD
dicated in patients with SIHD (259). (Level of Evidence: B)
(296299). (Level of Evidence: C)
CLASS IIb 5. Treatment with garlic, coenzyme Q10, selenium, or chromium is not
1. Treatment with aspirin 75 to 162 mg daily and clopidogrel 75 mg recommended with the intent of reducing cardiovascular risk or
daily might be reasonable in certain high-risk patients with SIHD improving clinical outcomes in patients with SIHD. (Level of Evi-
(260). (Level of Evidence: B) dence: C)
CLASS III: No Benefit 4.2.3. Medical Therapy for Relief of Symptoms
1. Dipyridamole is not recommended as antiplatelet therapy for pa-
tients with SIHD (261263). (Level of Evidence: B) 4.2.3.1. USE OF ANTI-ISCHEMIC MEDICATIONS
CLASS I
4.2.2.2. BETA-BLOCKER THERAPY
1. Beta blockers should be prescribed as initial therapy for relief of
CLASS I symptoms in patients with SIHD (264,300,301). (Level of Evidence: B)
1. Beta-blocker therapy should be started and continued for 3 years in 2. Calcium channel blockers or long-acting nitrates should be pre-
all patients with normal LV function after MI or ACS (264266). scribed for relief of symptoms when beta blockers are contraindi-
(Level of Evidence: B) cated or cause unacceptable side effects in patients with SIHD
2. Beta-blocker therapy should be used in all patients with LV systolic (302304). (Level of Evidence: B)
dysfunction (ejection fraction 40%) with heart failure or prior MI, 3. Calcium channel blockers or long-acting nitrates, in combination
unless contraindicated. (Use should be limited to carvedilol, meto- with beta blockers, should be prescribed for relief of symptoms
prolol succinate, or bisoprolol, which have been shown to reduce when initial treatment with beta blockers is unsuccessful in patients
risk of death.) (267271) (Level of Evidence: A) with SIHD (304). (Level of Evidence: B)
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2582 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
4. Sublingual nitroglycerin or nitroglycerin spray is recommended for CLASS IIa
immediate relief of angina in patients with SIHD (305307). (Level 1. PCI to improve survival is reasonable as an alternative to CABG in
of Evidence: B) selected stable patients with significant (50% diameter stenosis)
unprotected left main CAD with: 1) anatomic conditions associated
CLASS IIa with a low risk of PCI procedural complications and a high likelihood
1. Treatment with a long-acting nondihydropyridine calcium channel of good long-term outcome (e.g., a low SYNTAX score [22], ostial
blocker (verapamil or diltiazem) instead of a beta blocker as initial or trunk left main CAD); and 2) clinical characteristics that predict a
therapy for relief of symptoms is reasonable in patients with SIHD significantly increased risk of adverse surgical outcomes (e.g.,
(304). (Level of Evidence: B) STS-predicted risk of operative mortality 5%) (322,324,325,335
2. Ranolazine can be useful when prescribed as a substitute for beta 353). (Level of Evidence: B)
blockers for relief of symptoms in patients with SIHD if initial 2. PCI to improve survival is reasonable in patients with unstable
treatment with beta blockers leads to unacceptable side effects or angina/nonST-elevation MI when an unprotected left main coro-
is ineffective or if initial treatment with beta blockers is contraindi- nary artery is the culprit lesion and the patient is not a candidate for
cated (308). (Level of Evidence: B) CABG (325,340,342344,349352,354). (Level of Evidence: B)
3. Ranolazine in combination with beta blockers can be useful when 3. PCI to improve survival is reasonable in patients with acute ST-
prescribed for relief of symptoms when initial treatment with beta elevation MI when an unprotected left main coronary artery is the
blockers is not successful in patients with SIHD (309,310). (Level of culprit lesion, distal coronary flow is less than TIMI (Thrombolysis In
Evidence: A) Myocardial Infarction) grade 3, and PCI can be performed more
rapidly and safely than CABG (337,355,356). (Level of Evidence: C)
4.2.4. Alternative Therapies for Relief of Symptoms in
Patients With Refractory Angina CLASS IIb
1. PCI to improve survival may be reasonable as an alternative to
CLASS IIb CABG in selected stable patients with significant (50% diameter
1. Enhanced external counterpulsation may be considered for relief of
stenosis) unprotected left main CAD with: a) anatomic conditions
refractory angina in patients with SIHD (311). (Level of Evidence: B)
associated with a low to intermediate risk of PCI procedural com-
2. Spinal cord stimulation may be considered for relief of refractory
plications and an intermediate to high likelihood of good long-term
angina in patients with SIHD (312,313). (Level of Evidence: C)
outcome (e.g., lowintermediate SYNTAX score of 33, bifurcation
3. Transmyocardial revascularization may be considered for relief of
left main CAD); and b) clinical characteristics that predict an
refractory angina in patients with SIHD (314316). (Level of Evi-
increased risk of adverse surgical outcomes (e.g., moderate
dence: B)
severe chronic obstructive pulmonary disease, disability from
CLASS III: No Benefit
previous stroke, or previous cardiac surgery; STS-predicted risk of
1. Acupuncture should not be used for the purpose of improving operative mortality 2%) (322,324,325,335353,357). (Level
symptoms or reducing cardiovascular risk in patients with SIHD of Evidence: B)
(317,318). (Level of Evidence: C)
CLASS III: Harm
1. PCI to improve survival should not be performed in stable
5. CAD Revascularization: patients with significant (50% diameter stenosis) unprotected
Recommendations left main CAD who have unfavorable anatomy for PCI and who
are good candidates for CABG (322,324,325,328336). (Level of
Evidence: B)
Table 6 and Table 7 provide summaries of recommenda-
tions from this section. NonLeft Main CAD Revascularization
CLASS I
5.1. Heart Team Approach to 1. CABG to improve survival is beneficial in patients with significant
Revascularization Decisions (70% diameter) stenoses in 3 major coronary arteries (with or
CLASS I
without involvement of the proximal LAD artery) or in the proxi-
1. A Heart Team approach to revascularization is recommended in mal LAD artery plus 1 other major coronary artery (125,330,334,
patients with unprotected left main or complex CAD (319321). 358360). (Level of Evidence: B)
(Level of Evidence: C) 2. CABG or PCI to improve survival is beneficial in survivors of sudden
cardiac death with presumed ischemia-mediated ventricular tachy-
CLASS IIa cardia caused by significant (70% diameter) stenosis in a major
1. Calculation of the STS and SYNTAX scores is reasonable in patients coronary artery. (CABG Level of Evidence: B [122,378,379]; PCI
with unprotected left main and complex CAD (321327). (Level of Level of Evidence: C [378])
Evidence: B)
CLASS IIa
5.2. Revascularization to Improve Survival 1. CABG to improve survival is reasonable in patients with signifi-
cant (70% diameter) stenoses in 2 major coronary arteries with
Left Main CAD Revascularization
severe or extensive myocardial ischemia (e.g., high-risk criteria
CLASS I on stress testing, abnormal intracoronary hemodynamic evalua-
1. CABG to improve survival is recommended for patients with signif- tion, or 20% perfusion defect by myocardial perfusion stress
icant (50% diameter stenosis) left main coronary artery stenosis imaging) or target vessels supplying a large area of viable
(328334). (Level of Evidence: B) myocardium (363366). (Level of Evidence: B)
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2583
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
Table 6. Revascularization to Improve Survival Compared With Medical Therapy
Anatomic Setting COR LOE References
UPLM or complex CAD
CABG and PCI IHeart Team approach recommended C (319321)
CABG and PCI IIaCalculation of STS and SYNTAX scores B (321327)
UPLM*
CABG I B (328334)
PCI IIaFor SIHD when both of the following are present: B (322,324,325,335353)
Anatomic conditions associated with a low risk of PCI procedural
complications and a high likelihood of good long-term outcome (e.g., a low
SYNTAX score of 22, ostial or trunk left main CAD)
Clinical characteristics that predict a significantly increased risk of adverse
surgical outcomes (e.g., STS-predicted risk of operative mortality 5%)
IIaFor UA/NSTEMI if not a CABG candidate B (325,340,342344,349352,354)
IIaFor STEMI when distal coronary flow is TIMI flow grade 3 and PCI can be C (337,355,356)
performed more rapidly and safely than CABG
IIbFor SIHD when both of the following are present: B (322,324,325,335353,357)
Anatomic conditions associated with a low to intermediate risk of PCI
procedural complications and an intermediate to high likelihood of good long-
term outcome (e.g., low-intermediate SYNTAX score of 33, bifurcation left
main CAD)
Clinical characteristics that predict an increased risk of adverse surgical
outcomes (e.g., moderatesevere COPD, disability from prior stroke, or prior
cardiac surgery; STS-predicted operative mortality 2%)
III: HarmFor SIHD in patients (versus performing CABG) with unfavorable B (322,324,325,328336)
anatomy for PCI and who are good candidates for CABG
3-vessel disease with or without proximal LAD artery disease*
CABG I B (125,330,334,358360)
IIaIt is reasonable to choose CABG over PCI in patients with complex 3-vessel B (336,353,360362)
CAD (e.g., SYNTAX score 22) who are good candidates for CABG.
PCI IIbOf uncertain benefit B (140,330,353,358,360)
2-vessel disease with proximal LAD artery disease*
CABG I B (125,330,334,358360)
PCI IIbOf uncertain benefit B (140,330,358,360)
2-vessel disease without proximal LAD artery disease*
CABG IIaWith extensive ischemia B (363366)
IIbOf uncertain benefit without extensive ischemia C (360)
PCI IIbOf uncertain benefit B (140,330,358,360)
1-vessel proximal LAD artery disease
CABG IIaWith LIMA for long-term benefit B (334,360,367,368)
PCI IIbOf uncertain benefit B (140,330,358,360)
1-vessel disease without proximal LAD artery involvement
CABG III: Harm B (141,334,358,363, 364,369372)
PCI III: Harm B (141,334,358,363,364, 369372)
LV dysfunction
CABG IIaEF 35% to 50% B (139,334,373376)
CABG IIbEF 35% without significant left main CAD B (127,139,334,373377)
PCI Insufficient data N/A
Survivors of sudden cardiac death with presumed ischemia-mediated VT
CABG I B (122,378,379)
PCI I C (378)
No anatomic or physiological criteria for revascularization
CABG III: Harm B (141,334,358,363, 364,369372)
PCI III: Harm B (141,334,358,363,364,369372)
*In patients with multivessel disease who also have diabetes mellitus, it is reasonable to choose CABG (with LIMA) over PCI (365,380,381,381386) (Class IIa; LOE: B).
CABG indicates coronary artery bypass graft; CAD, coronary artery disease; COPD, chronic obstructive pulmonary disease; COR, class of recommendation; EF, ejection fraction; LAD, left anterior
descending; LIMA, left internal mammary artery; LOE, level of evidence; LV, left ventricular; N/A, not available; PCI, percutaneous coronary intervention; SIHD, stable ischemic heart disease; STEMI,
ST-elevation myocardial infarction; STS, Society of Thoracic Surgeons; SYNTAX, Synergy between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery; TIMI, Thrombolysis In Myocardial
Infarction; UA/NSTEMI, unstable angina/nonST-elevation myocardial infarction; UPLM, unprotected left main disease; and VT, ventricular tachycardia.
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2584 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
Table 7. Revascularization to Improve Symptoms With Significant Anatomic (>50% Left Main or >70% NonLeft Main CAD) or
Physiological (FFR <0.80) Coronary Artery Stenoses
Clinical Setting COR LOE References
1 significant stenoses amenable to revascularization and 1CABG A (140,387396)
unacceptable angina despite GDMT 1PCI
1 significant stenoses and unacceptable angina in whom GDMT IIaCABG C N/A
cannot be implemented because of medication contraindications, IIaPCI C N/A
adverse effects, or patient preferences
Previous CABG with 1 significant stenoses associated with IIaPCI C (397400)
ischemia and unacceptable angina despite GDMT IIbCABG C (401)
Complex 3-vessel CAD (e.g., SYNTAX score >22) with or without IIaCABG preferred over PCI B (353,360362)
involvement of the proximal LAD artery and a good candidate for
CABG
Viable ischemic myocardium that is perfused by coronary arteries that IIbTMR as an adjunct to CABG B (402406)
are not amenable to grafting
No anatomic or physiological criteria for revascularization III: HarmCABG C N/A
III: HarmPCI C N/A
CABG indicates coronary artery bypass graft; CAD, coronary artery disease; COR, class of recommendation; FFR, fractional flow reserve; GDMT, guideline-directed medical therapy; LOE, level of evidence;
N/A, not available; PCI, percutaneous coronary intervention; SYNTAX, Synergy between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery; and TMR, transmyocardial revascularization.
2. CABG to improve survival is reasonable in patients with mildmoderate stenosis, fractional flow reserve 0.80, no or only mild ischemia
LV systolic dysfunction (ejection fraction 35% to 50%) and significant on noninvasive testing), involve only the left circumflex or right
(70% diameter stenosis) multivessel CAD or proximal LAD coronary coronary artery, or subtend only a small area of viable myocar-
artery stenosis, when viable myocardium is present in the region of dium (141,334,358,363,364,369372). (Level of Evidence: B)
intended revascularization (139,334,373376). (Level of Evidence: B)
3. CABG with a left internal mammary artery graft to improve survival
5.3. Revascularization to Improve Symptoms
is reasonable in patients with significant (70% diameter) stenosis CLASS I
in the proximal LAD artery and evidence of extensive ischemia 1. CABG or PCI to improve symptoms is beneficial in patients with 1 or
(334,360,367,368). (Level of Evidence: B) more significant (70% diameter) coronary artery stenoses ame-
4. It is reasonable to choose CABG over PCI to improve survival in nable to revascularization and unacceptable angina despite GDMT
patients with complex 3-vessel CAD (e.g., SYNTAX score 22), with (140,387393,395,396,412). (Level of Evidence: A)
or without involvement of the proximal LAD artery who are good
CLASS IIa
candidates for CABG (336,353,360362). (Level of Evidence: B) 1. CABG or PCI to improve symptoms is reasonable in patients with 1
5. CABG is probably recommended in preference to PCI to improve or more significant (70% diameter) coronary artery stenoses and
survival in patients with multivessel CAD and diabetes mellitus, unacceptable angina for whom GDMT cannot be implemented
particularly if a left internal mammary artery graft can be anasto- because of medication contraindications, adverse effects, or patient
mosed to the LAD artery (365,380,381386). (Level of Evidence: B) preferences. (Level of Evidence: C)
2. PCI to improve symptoms is reasonable in patients with previous
CLASS IIb
1. The usefulness of CABG to improve survival is uncertain in patients CABG, 1 or more significant (70% diameter) coronary artery
with significant (70%) diameter stenoses in 2 major coronary stenoses associated with ischemia, and unacceptable angina de-
arteries not involving the proximal LAD artery and without extensive spite GDMT (397,399,400). (Level of Evidence: C)
ischemia (360). (Level of Evidence: C) 3. It is reasonable to choose CABG over PCI to improve symptoms in
2. The usefulness of PCI to improve survival is uncertain in patients patients with complex 3-vessel CAD (e.g., SYNTAX score 22), with or
with 2- or 3-vessel CAD (with or without involvement of the proximal without involvement of the proximal LAD artery, who are good candi-
LAD artery) or 1-vessel proximal LAD disease (140,330,358,360). dates for CABG (325,336,353,360362). (Level of Evidence: B)
(Level of Evidence: B) CLASS IIb
3. CABG might be considered with the primary or sole intent of 1. CABG to improve symptoms might be reasonable for patients with
improving survival in patients with SIHD with severe LV systolic previous CABG, 1 or more significant (70% diameter) coronary
dysfunction (ejection fraction 35%) whether or not viable myocar- artery stenoses not amenable to PCI, and unacceptable angina
dium is present (127,139,334,373377). (Level of Evidence: B) despite GDMT (401). (Level of Evidence: C)
4. The usefulness of CABG or PCI to improve survival is uncertain in 2. Transmyocardial revascularization performed as an adjunct to
patients with previous CABG and extensive anterior wall ischemia CABG to improve symptoms may be reasonable in patients with
on noninvasive testing (397401,408411). (Level of Evidence: B) viable ischemic myocardium that is perfused by arteries that are not
amenable to grafting (402406). (Level of Evidence: B)
CLASS III: Harm
1. CABG or PCI should not be performed with the primary or sole CLASS III: Harm
intent to improve survival in patients with SIHD with 1 or more 1. CABG or PCI to improve symptoms should not be performed in
coronary stenoses that are not anatomically or functionally patients who do not meet anatomic (50% diameter left main or
significant (e.g., 70% diameter nonleft main coronary artery 70% nonleft main stenosis diameter) or physiological (e.g.,
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2585
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
abnormal fractional flow reserve) criteria for revascularization. c. Unfavorable LAD artery for PCI (i.e., excessive vessel tortuosity or
(Level of Evidence: C) chronic total occlusion).
CLASS IIb
5.4. Dual Antiplatelet Therapy Compliance and 1. Hybrid coronary revascularization (defined as the planned com-
Stent Thrombosis bination of left internal mammary arterytoLAD artery grafting
and PCI of 1 non-LAD coronary arteries) may be reasonable as
CLASS III: Harm an alternative to multivessel PCI or CABG in an attempt to
1. PCI with coronary stenting (bare-metal stent or drug-eluting stent) improve the overall riskbenefit ratio of the procedures. (Level of
should not be performed if the patient is not likely to be able to Evidence: C)
tolerate and comply with dual antiplatelet therapy for the appropri-
ate duration of treatment based on the type of stent implanted 6. Patient Follow-Up: Monitoring of
(414417). (Level of Evidence: B)
Symptoms and Antianginal Therapy:
Recommendations
5.5. Hybrid Coronary Revascularization
CLASS IIa
6.1. Clinical Evaluation, Echocardiography During
1. Hybrid coronary revascularization (defined as the planned combina- Routine, Periodic Follow-Up
tion of left internal mammary arterytoLAD artery grafting and PCI CLASS I
of 1 non-LAD coronary arteries) is reasonable in patients with 1 or 1. Patients with SIHD should receive periodic follow-up, at least annu-
more of the following (418424) (Level of Evidence: B): ally, that includes all of the following (Level of Evidence: C):
a. Limitations to traditional CABG, such as heavily calcified proxi- a. Assessment of symptoms and clinical function;
mal aorta or poor target vessels for CABG (but amenable to PCI); b. Surveillance for complications of SIHD, including heart failure
b. Lack of suitable graft conduits; and arrhythmias;
Table 8. Follow-Up Noninvasive Testing in Patients With Known SIHD: New, Recurrent, or Worsening Symptoms
Not Consistent With UA
Exercise ECG
Status Interpretable
Test Able Unable Yes No COR LOE References Additional Considerations
Patients able to exercise*
Exercise ECG X X I B (3942)
Exercise with nuclear MPI or X X I B (69,95,96,102,
Echo 141,364,
426435)
Exercise with nuclear MPI or X Any IIa B (436,437) Prior requirement for imaging with
Echo exercise
Known or at high risk for multivessel
disease
Pharmacological stress X X III: No Benefit C (438)
nuclear MPI/Echo/CMR
Patients unable to exercise
Pharmacological stress X Any I B (43,46,47,4953)
nuclear MPI or Echo
Pharmacological stress CMR X Any IIa B (98,99,101)
Exercise ECG X X III: No Benefit C N/A
Irrespective of ability to exercise
CCTA Any Any IIb B (439443) Patency of CABG or coronary stent 3 mm
diameter
CCTA Any Any IIb B (55,58,439) In the absence of known moderate or
severe calcification and intent to assess
coronary stent 3 mm in diameter
CCTA Any Any III: No Benefit B (439443) Known moderate or severe native coronary
calcification or assessment of coronary
stent 3 mm in diameter in patients
who have new or worsening symptoms
not consistent with UA
*Patients are candidates for exercise testing if they are capable of performing at least moderate physical functioning (i.e., moderate household, yard, or recreational work and most activities of daily
living) and have no disabling comorbidity. Patients should be able to achieve 85% of age-predicted maximum heart rate.
CABG indicates coronary artery bypass graft surgery; CCTA, cardiac computed tomography angiography; CMR, cardiac magnetic resonance; COR, class of recommendation; ECG, electrocardiogram;
Echo, echocardiography; LOE, level of evidence; MPI, myocardial perfusion imaging; N/A, not available; SIHD, stable ischemic heart disease; and UA, unstable angina.
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2586 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
c. Monitoring of cardiac risk factors; and 6.2.1.1. PATIENTS ABLE TO EXERCISE
d. Assessment of the adequacy of and adherence to recommended
CLASS I
lifestyle changes and medical therapy. 1. Standard exercise ECG testing is recommended in patients with
known SIHD who have new or worsening symptoms not consistent
2. Assessment of LV ejection fraction and segmental wall motion by
with UA and who have a) at least moderate physical functioning and
echocardiography or radionuclide imaging is recommended in pa-
no disabling comorbidity and b) an interpretable ECG (3942).
tients with new or worsening heart failure or evidence of intervening
(Level of Evidence: B)
MI by history or ECG. (Level of Evidence: C)
2. Exercise with nuclear MPI or echocardiography is recommended in
CLASS IIb patients with known SIHD who have new or worsening symptoms
1. Periodic screening for important comorbidities that are prevalent in not consistent with UA and who have a) at least moderate physical
patients with SIHD, including diabetes mellitus, depression, and functioning or no disabling comorbidity but b) an uninterpretable
chronic kidney disease might be reasonable. (Level of Evidence: C) ECG (69,95,96,102,141,364,426435). (Level of Evidence: B)
2. A resting 12-lead ECG at 1-year or longer intervals between studies CLASS IIa
in patients with stable symptoms might be reasonable. (Level of 1. Exercise with nuclear MPI or echocardiography is reasonable in
Evidence: C) patients with known SIHD who have new or worsening symptoms
not consistent with UA and who have a) at least moderate physical
CLASS III: No Benefit
functioning and no disabling comorbidity, b) previously required
1. Measurement of LV function with a technology such as echocardi-
imaging with exercise stress, or c) known multivessel disease or
ography or radionuclide imaging is not recommended for routine
high risk for multivessel disease (436,437). (Level of Evidence: B)
periodic reassessment of patients who have not had a change in
clinical status or who are at low risk of adverse cardiovascular CLASS III: No Benefit
events (425). (Level of Evidence: C) 1. Pharmacological stress imaging with nuclear MPI, echocardiogra-
phy, or CMR is not recommended in patients with known SIHD who
have new or worsening symptoms not consistent with UA and who
6.2. Noninvasive Testing in Known SIHD
are capable of at least moderate physical functioning or have no
6.2.1. Follow-Up Noninvasive Testing in Patients disabling comorbidity (438). (Level of Evidence: C)
With Known SIHD: New, Recurrent, or Worsening
6.2.1.2. PATIENTS UNABLE TO EXERCISE
Symptoms Not Consistent With Unstable Angina
CLASS I
See Table 8 for a summary of recommendations from this 1. Pharmacological stress imaging with nuclear MPI or echocardiog-
section. raphy is recommended in patients with known SIHD who have new
Table 9. Noninvasive Testing in Known SIHD: Asymptomatic (or Stable Symptoms)
ECG
Exercise Status Interpretable
Pretest Probability of Additional
Test Able* Unable Yes No Ischemia COR LOE References Considerations
Exercise or pharmacological X X Prior evidence of silent IIa C (10,13,20) a) Unable to exercise to
stress with nuclear MPI, ischemia or high risk adequate workload
Echo, or CMR at 2-y for recurrent cardiac or
intervals event. Meets criteria b) Uninterpretable ECG
listed in additional or
considerations. c) History of incomplete
coronary
revascularization
Exercise ECG at 1-y X X Any IIb C N/A a) Prior evidence of
intervals silent ischemia OR
b) At high risk for
recurrent cardiac
event
Exercise ECG X X No prior evidence of silent IIb C N/A For annual surveillance
ischemia and not at
high risk of recurrent
cardiac event.
Exercise or pharmacological Any Any Any III: No C (10,13,20) a) 5-y intervals after
stress with nuclear MPI, Benefit CABG, or
Echo, or CMR or CCTA b) 2-y intervals after
PCI
*Patients are candidates for exercise testing if they are capable of performing at least moderate physical functioning (i.e., moderate household, yard, or recreational work and most activities of daily
living) and have no disabling comorbidity. Patients should be able to achieve 85% of age-predicted maximum heart rate.
CABG indicates coronary artery bypass graft surgery; CCTA, cardiac computed tomography angiography; CMR, coronary magnetic resonance; COR, class of recommendation; CCTA, computed
tomography angiography; CMR, cardiac magnetic resonance; ECG, electrocardiogram; Echo, echocardiography; LOE, level of evidence; MPI, myocardial perfusion imaging; N/A, not available; PCI,
percutaneous coronary intervention; and SIHD, stable ischemic heart disease.
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2587
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
or worsening symptoms not consistent with UA and who are inca- cardiac event, the usefulness of annual surveillance exercise ECG
pable of at least moderate physical functioning or have disabling testing is not well established. (Level of Evidence: C)
comorbidity (43,46,47,4953). (Level of Evidence: B)
CLASS III: No Benefit
1. Nuclear MPI, echocardiography, or CMR, with either exercise or
CLASS IIa
1. Pharmacological stress imaging with CMR is reasonable in patients pharmacological stress or CCTA, is not recommended for follow-up
with known SIHD who have new or worsening symptoms not con- assessment in patients with SIHD, if performed more frequently
sistent with UA and who are incapable of at least moderate physical than at a) 5-year intervals after CABG or b) 2-year intervals after PCI
functioning or have disabling comorbidity (98,99,101). (Level of (10,13,20). (Level of Evidence: C)
Evidence: B)
Presidents and Staff
CLASS III: No Benefit
1. Standard exercise ECG testing should not be performed in patients
with known SIHD who have new or worsening symptoms not con- American College of Cardiology Foundation
sistent with UA and who a) are incapable of at least moderate William A. Zoghbi, MD, FACC, President
physical functioning or have disabling comorbidity or b) have an Thomas E. Arend, Jr, Esq, CAE, Interim Chief Staff Officer
uninterpretable ECG. (Level of Evidence: C) William J. Oetgen, MD, MBA, FACC, Senior Vice
President, Science and Quality
6.2.1.3. IRRESPECTIVE OF ABILITY TO EXERCISE
Charlene L. May, Senior Director, Science and Clinical Policy
CLASS IIb Erin A. Barrett, MPS, Senior Specialist, Science and Clinical
1. CCTA for assessment of patency of CABG or of coronary stents 3 Policy
mm or larger in diameter might be reasonable in patients with
known SIHD who have new or worsening symptoms not consistent American College of Cardiology Foundation/
with UA, irrespective of ability to exercise (439443). (Level of American Heart Association
Evidence: B) Lisa Bradfield, CAE, Director, Science and Clinical Policy
2. CCTA might be reasonable in patients with known SIHD who have Maria Koinis, Specialist, Science and Clinical Policy
new or worsening symptoms not consistent with UA, irrespective of Sue Keller, BSN, MPH, Senior Specialist, Evidence-Based
ability to exercise, in the absence of known moderate or severe Medicine
calcification or if the CCTA is intended to assess coronary stents less
than 3 mm in diameter (55,58,439). (Level of Evidence: B) American Heart Association
Gordon F. Tomaselli, MD, FAHA, President
CLASS III: No Benefit Nancy Brown, Chief Executive Officer
1. CCTA should not be performed for assessment of native coronary
Rose Marie Robertson, MD, FAHA, Chief Science Officer
arteries with known moderate or severe calcification or with coro-
nary stents less than 3 mm in diameter in patients with known SIHD
Gayle R. Whitman, PhD, RN, FAHA, FAAN, Senior Vice
who have new or worsening symptoms not consistent with UA,
President, Office of Science Operations
irrespective of ability to exercise (439443). (Level of Evidence: B) Judy L. Bezanson, DSN, RN, CNS-MS, FAHA, Science
and Medicine Advisor, Office of Science Operations
6.2.2. Noninvasive Testing in Known SIHD
Asymptomatic (or Stable Symptoms) REFERENCES
See Table 9 for a summary of recommendations from this 1. ACCF/AHA Task Force on Practice Guidelines. Methodology
section. Manual and Policies From the ACCF/AHA Task Force on Practice
Guidelines. 2012. Available at: http://assets.cardiosource.com/
CLASS IIa Methodology_Manual_for_ACC_AHA_Writing_Committees.pdf
1. Nuclear MPI, echocardiography, or CMR with either exercise or and http://my.americanheart.org/idc/groups/ahamah-public/@wcm/
@sop/documents/downloadable/ucm_319826.pdf. Accessed May 16,
pharmacological stress can be useful for follow-up assessment 2012.
at 2-year or longer intervals in patients with SIHD with prior 2. Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/
evidence of silent ischemia or who are at high risk for a recurrent AATS/PCNA/SCAI/STS guideline for the diagnosis and manage-
cardiac event and a) are unable to exercise to an adequate ment of patients with stable ischemic heart disease: a report of the
American College of Cardiology Foundation/American Heart Asso-
workload, b) have an uninterpretable ECG, or c) have a history of ciation Task Force on Practice Guidelines, and the American College
incomplete coronary revascularization (10,13,20). (Level of Evi- of Physicians, American Association for Thoracic Surgery, Preventive
dence: C) Cardiovascular Nurses Association, Society for Cardiovascular An-
giography and Interventions, and Society of Thoracic Surgeons. J Am
CLASS IIb Coll Cardiol. 2012.60:e44 e164. doi:10.1016/j.jacc.2012.07.013.
1. Standard exercise ECG testing performed at 1-year or longer inter- 3. Antman EM, Hand M, Armstrong PW, et al. 2007 focused update
of the ACC/AHA 2004 guidelines for the management of patients
vals might be considered for follow-up assessment in patients with
with ST-elevation myocardial infarction: a report of the American
SIHD who have had prior evidence of silent ischemia or are at high College of Cardiology/American Heart Association Task Force on
risk for a recurrent cardiac event and are able to exercise to an Practice Guidelines. J Am Coll Cardiol. 2008;51:210 47.
adequate workload and have an interpretable ECG. (Level of Evi- 4. Kushner FG, Hand M, Smith SC Jr., et al. 2009 focused updates:
ACC/AHA guidelines for the management of patients with ST-
dence: C)
elevation myocardial infarction (updating the 2004 guideline and
2. In patients who have no new or worsening symptoms or no prior 2007 focused update) and ACC/AHA/SCAI guidelines on percuta-
evidence of silent ischemia and are not at high risk for a recurrent neous coronary intervention (updating the 2005 guideline and 2007
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2588 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
focused update): a report of the American College of Cardiology for Cardiovascular Magnetic Resonance. J Am Coll Cardiol.
Foundation/American Heart Association Task Force on Practice 2011;57:1126 66.
Guidelines. J Am Coll Cardiol. 2009;54:2205 41. 14. Antman EM, Peterson ED. Tools for guiding clinical practice from
5. Jneid H, Anderson JL, Wright RS, et al. 2012 ACCF/AHA focused the american heart association and the american college of cardiology:
update of the guideline for the management of patients with unstable what are they and how should clinicians use them? Circulation.
angina/nonST-elevation myocardial infarction (updating the 2007 2009;119:1180 5.
guideline and replacing the 2011 focused update): a report of the 15. Fraker TD Jr., Fihn SD, Gibbons RJ, et al. 2007 chronic angina
American College of Cardiology Foundation/American Heart Asso- focused update of the ACC/AHA 2002 guidelines for the manage-
ciation Task Force on Practice Guidelines. J Am Coll Cardiol. ment of patients with chronic stable angina: a report of the American
2012;60:645 681. College of Cardiology/American Heart Association Task Force on
5a.Wright RS, Anderson JL, Adams CD, et al. 2011 ACCF/AHA Practice Guidelines Writing Group to Develop the Focused Update
focused update incorporated into the ACC/AHA 2007 guidelines for of the 2002 Guidelines for the Management of Patients with Chronic
the management of patients with unstable angina/nonST-elevation Stable Angina. J Am Coll Cardiol. 2007;50:2264 74.
myocardial infarction: a report of the American College of Cardiology 16. Bonow RO, Carabello BA, Chatterjee K, et al. 2008 focused update
Foundation/American Heart Association Task Force on Practice incorporated into the ACC/AHA 2006 guidelines for the manage-
Guidelines. J Am Coll Cardiol. 2011;57:e215367. ment of patients with valvular heart disease: a report of the American
6. Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA College of Cardiology/American Heart Association Task Force on
guideline for assessment of cardiovascular risk in asymptomatic Practice Guidelines (Writing Committee to Revise the 1998 Guide-
adults: a report of the American College of Cardiology Foundation/ lines for the Management of Patients with Valvular Heart Disease).
American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2008;52:e1142.
J Am Coll Cardiol. 2010;56:e50 103. 17. Hunt SA, Abraham WT, Chin MH, et al. 2009 focused update
7. Braunwald E, Mark D, Jones R, et al. Unstable Angina: Diagnosis incorporated into the ACC/AHA 2005 guidelines for the diagnosis
and Management. Clinical Practice Guideline Number 10. Rockville, and management of heart failure in adults: a report of the American
MD: Agency for Healthcare Policy and Research and the National College of Cardiology Foundation/American Heart Association Task
Heart, Lung, and Blood Institue, Public Health Service, U.S. Force on Practice Guidelines: developed in collaboration with the
Department of Health and Human Services: 1994. International Society for Heart and Lung Transplantation. J Am Coll
8. Smith SC Jr., Benjamin EJ, Bonow RO, et al. AHA/ACCF secondary Cardiol. 2009;53:e190.
prevention and risk reduction therapy for patients with coronary and 18. Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guide-
other atherosclerotic vascular disease: 2011 update: a guideline from the lines for the management of patients with ST-elevation myocardial
American Heart Association and American College of Cardiology infarction; A report of the American College of Cardiology/
Foundation. J Am Coll Cardiol. 2011;58:2432 46. American Heart Association Task Force on Practice Guidelines
9. Patel MR, Spertus JA, Brindis RG, et al. ACCF proposed method (Committee to Revise the 1999 Guidelines for the Management of
for evaluating the appropriateness of cardiovascular imaging. J Am patients with acute myocardial infarction). J Am Coll Cardiol.
Coll Cardiol. 2005;46:1606 13.
2004;44:E1E211.
10. Hendel RC, Berman DS, Di Carli MF, et al. ACCF/ASNC/ACR/
19. Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA
AHA/ASE/SCCT/SCMR/SNM 2009 appropriate use criteria for
Guideline for Coronary Artery Bypass Graft Surgery. A report of the
cardiac radionuclide imaging: a report of the American College of
American College of Cardiology Foundation/American Heart Asso-
Cardiology Foundation Appropriate Use Criteria Task Force, the
ciation Task Force on Practice Guidelines. J Am Coll Cardiol.
American Society of Nuclear Cardiology, the American College of
2011;58:123210.
Radiology, the American Heart Association, the American Society of
20. Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/
Echocardiography, the Society of Cardiovascular Computed Tomog-
SCAI Guideline for Percutaneous Coronary Intervention. A report of
raphy, the Society for Cardiovascular Magnetic Resonance, and the
Society of Nuclear Medicine. J Am Coll Cardiol. 2009;53:220129. the American College of Cardiology Foundation/American Heart
11. Hendel RC, Patel MR, Kramer CM, et al. ACCF/ACR/SCCT/ Association Task Force on Practice Guidelines and the Society for
SCMR/ASNC/NASCI/SCAI/SIR 2006 appropriateness criteria for Cardiovascular Angiography and Interventions. J Am Coll Cardiol.
cardiac computed tomography and cardiac magnetic resonance im- 2011;58:44 122.
aging: a report of the American College of Cardiology Foundation 21. Deleted in proof.
Quality Strategic Directions Committee Appropriateness Criteria 22. Grundy SM, Cleeman JI, Merz CNB, et al. Implications of recent
Working Group, American College of Radiology, Society of Cardio- clinical trials for the National Cholesterol Education Program Adult
vascular Computed Tomography, Society for Cardiovascular Mag- Treatment Panel III guidelines. Circulation. 2004;110:22739.
netic Resonance, American Society of Nuclear Cardiology, North 23. Third Report of the National Cholesterol Education Program
American Society for Cardiac Imaging, Society for Cardiovascular (NCEP) Expert Panel on Detection, Evaluation, and Treatment of
Angiography and Interventions, and Society of Interventional Radi- High Blood Cholesterol in Adults (Adult Treatment Panel III) final
ology. J Am Coll Cardiol. 2006;48:147597. report. Circulation. 2002;106:3143 421.
12. Taylor AJ, Cerqueira M, Hodgson JM, et al. ACCF/SCCT/ACR/ 24. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the
AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use cri- Joint National Committee on Prevention, Detection, Evaluation, and
teria for cardiac computed tomography: a report of the American Treatment of High Blood Pressure. Hypertension. 2003;42:1206 52.
College of Cardiology Foundation Appropriate Use Criteria Task 25. Balady GJ, Ades PA, Bittner VA, et al. Referral, Enrollment, and
Force, the Society of Cardiovascular Computed Tomography, the Delivery of Cardiac Rehabilitation/Secondary Prevention Programs
American College of Radiology, the American Heart Association, at Clinical Centers and Beyond: A Presidential Advisory From the
the American Society of Echocardiography, the American Society of American Heart Association. Circulation. 2011;124:2951 60.
Nuclear Cardiology, the North American Society for Cardiovascular 26. Mensah GA, Brown DW. An overview of cardiovascular disease
Imaging, the Society for Cardiovascular Angiography and Interven- burden in the United States. Health Aff (Millwood). 2007;26:38 48.
tions, and the Society for Cardiovascular Magnetic Resonance. J Am 27. Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and
Coll Cardiol. 2010;56:1864 94. stroke statistics2010 update: a report from the American Heart
13. Douglas PS, Garcia MJ, Haines DE, et al. ACCF/ASE/AHA/ Association. Circulation. 2010;121:e46 215.
ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 appropri- 28. Ford ES, Capewell S. Coronary heart disease mortality among young
ate use criteria for echocardiography: a report of the American adults in the U.S. from 1980 through 2002: concealed leveling of
College of Cardiology Foundation Appropriate Use Criteria Task mortality rates. J Am Coll Cardiol. 2007;50:2128 32.
Force, American Society of Echocardiography, American Heart 29. Murphy SL, Xu JQ, Kochanek KD. Deaths: Preliminary Data for
Association, American Society of Nuclear Cardiology, Heart Failure 2010. National Vital Statistics Reports. 2012;60.
Society of America, Heart Rhythm Society, Society for Cardiovas- 30. National Heart, Lung, and Blood Institute. Incidence and Preva-
cular Angiography and Interventions, Society of Critical Care Med- lence: 2006 Chart Book on Cardiovascular and Lung Diseases.
icine, Society of Cardiovascular Computed Tomography, and Society Bethesda, MD: National Institutes of Health. 2006. Available at:
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2589
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
http://www.nhlbi.nih.gov/resources/docs/06_ip_chtbk.pdf. Accessed detection of coronary artery disease: a meta-analysis. J Am Coll
January 6, 2012. Cardiol. 2007;50:134353.
31. Rumsfeld JS, Magid DJ, Plomondon ME, et al. Health-related 51. Picano E, Molinaro S, Pasanisi E. The diagnostic accuracy of
quality of life after percutaneous coronary intervention versus coro- pharmacological stress echocardiography for the assessment of
nary bypass surgery in high-risk patients with medically refractory coronary artery disease: a meta-analysis. Cardiovasc Ultrasound.
ischemia. J Am Coll Cardiol. 2003;41:1732 8. 2008;6:30. Published online 2008 June 19, doi:10.1186/1476-
32. Rumsfeld JS, MaWhinney S, McCarthy M Jr., et al. Health-related 7120-6-30.
quality of life as a predictor of mortality following coronary artery 52. Underwood SR, Shaw LJ, Anagnostopoulos C, et al. Myocardial
bypass graft surgery. Participants of the Department of Veterans perfusion scintigraphy and cost effectiveness of diagnosis and man-
Affairs Cooperative Study Group on Processes, Structures, and agement of coronary heart disease. Heart. 2004;90 Suppl 5:v34 v36.
Outcomes of Care in Cardiac Surgery. JAMA. 1999;281:1298 303. 53. Underwood SR, Anagnostopoulos C, Cerqueira M, et al. Myocardial
33. Wiest FC, Bryson CL, Burman M, et al. Suboptimal pharmacother- perfusion scintigraphy: the evidence. Eur J Nucl Med Mol Imaging.
apeutic management of chronic stable angina in the primary care 2004;31:26191.
setting. Am J Med. 2004;117:234 41. 54. Hamon M, Fau G, Nee G, et al. Meta-analysis of the diagnostic
34. Diamond GA, Forrester JS. Analysis of probability as an aid in the performance of stress perfusion cardiovascular magnetic resonance for
clinical diagnosis of coronary-artery disease. N Engl J Med. 1979; detection of coronary artery disease. J Cardiovasc Magn Reson.
300:1350 8. 2010;12:29.
35. Deleted in proof. 55. Schuetz GM, Zacharopoulou NM, Schlattmann P, et al. Meta-
36. Daly CA, De Stavola B, Sendon JLL, et al. Predicting prognosis in analysis: noninvasive coronary angiography using computed tomog-
stable anginaresults from the Euro heart survey of stable angina: raphy versus magnetic resonance imaging. Ann Intern Med. 2010;
prospective observational study. BMJ. 2006;332:2627. 152:16777.
37. Daly C, Norrie J, Murdoch DL, et al. The value of routine 56. Budoff MJ, Dowe D, Jollis JG, et al. Diagnostic performance of
non-invasive tests to predict clinical outcome in stable angina. Eur 64-multidetector row coronary computed tomographic angiography
Heart J. 2003;24:532 40. for evaluation of coronary artery stenosis in individuals without
38. Hammermeister KE, DeRouen TA, Dodge HT. Variables predictive known coronary artery disease: results from the prospective multi-
of survival in patients with coronary disease. Selection by univariate center ACCURACY (Assessment by Coronary Computed Tomo-
and multivariate analyses from the clinical, electrocardiographic, graphic Angiography of Individuals Undergoing Invasive Coronary
exercise, arteriographic, and quantitative angiographic evaluations. Angiography) trial. J Am Coll Cardiol. 2008;52:1724 32.
Circulation. 1979;59:42130. 57. Hamon M, Biondi-Zoccai GG, Malagutti P, et al. Diagnostic
39. Gianrossi R, Detrano R, Mulvihill D, et al. Exercise-induced ST performance of multislice spiral computed tomography of coronary
depression in the diagnosis of coronary artery disease. A meta- arteries as compared with conventional invasive coronary angiogra-
analysis. Circulation. 1989;80:8798. phy: a meta-analysis. J Am Coll Cardiol. 2006;48:1896 910.
58. Janne dOthee B, Siebert U, Cury R, et al. A systematic review on
40. Kwok Y, Kim C, Grady D, et al. Meta-analysis of exercise testing to
diagnostic accuracy of CT-based detection of significant coronary
detect coronary artery disease in women. Am J Cardiol. 1999;83:
artery disease. Eur J Radiol. 2008;65:449 61.
660 6.
59. Meijboom WB, Meijs MF, Schuijf JD, et al. Diagnostic accuracy
41. Sabharwal NK, Stoykova B, Taneja AK, et al. A randomized trial
of 64-slice computed tomography coronary angiography: a pro-
of exercise treadmill ECG versus stress SPECT myocardial
spective, multicenter, multivendor study. J Am Coll Cardiol.
perfusion imaging as an initial diagnostic strategy in stable
2008;52:2135 44.
patients with chest pain and suspected CAD: cost analysis. J Nucl
60. Miller JM, Rochitte CE, Dewey M, et al. Diagnostic performance of
Cardiol. 2007;14:174 86.
coronary angiography by 64-row CT. N Engl J Med. 2008;359:
42. Shaw LJ, Mieres JH, Hendel RH, et al. Comparative Effectiveness of 2324 36.
exercise electrocardiography with or without myocardial perfusion 61. Schuijf JD, Bax JJ, Shaw LJ, et al. Meta-analysis of comparative
single photon emission computed tomography in women with diagnostic performance of magnetic resonance imaging and multislice
suspected coronary artery disease: results from the What Is the computed tomography for noninvasive coronary angiography. Am
Optimal Method for Ischemia Evaluation in Women (WOMEN) Heart J. 2006;151:404 11.
trial. Circulation. 2011;124:1239 49. 62. Stein PD, Beemath A, Kayali F, et al. Multidetector computed
43. Biagini E, Shaw LJ, Poldermans D, et al. Accuracy of non-invasive tomography for the diagnosis of coronary artery disease: a systematic
techniques for diagnosis of coronary artery disease and prediction of review. Am J Med. 2006;119:20316.
cardiac events in patients with left bundle branch block: a meta- 63. Sun Z, Jiang W. Diagnostic value of multislice computed tomogra-
analysis. Eur J Nucl Med Mol Imaging. 2006;33:144251. phy angiography in coronary artery disease: a meta-analysis. Eur J
44. Fleischmann KE, Hunink MG, Kuntz KM, et al. Exercise echocar- Radiol. 2006;60:279 86.
diography or exercise SPECT imaging? A meta-analysis of diagnostic 64. Underwood SR, Godman B, Salyani S, et al. Economics of myocar-
test performance. JAMA. 1998;280:91320. dial perfusion imaging in Europethe EMPIRE Study. Eur Heart J.
45. Garber AM, Solomon NA. Cost-effectiveness of alternative test 1999;20:157 66.
strategies for the diagnosis of coronary artery disease. Ann Intern 65. Nucifora G, Schuijf JD, van Werkhoven JM, et al. Relationship
Med. 1999;130:719 28. between obstructive coronary artery disease and abnormal stress
46. Geleijnse ML, Krenning BJ, Soliman OI, et al. Dobutamine stress testing in patients with paroxysmal or persistent atrial fibrillation. Int
echocardiography for the detection of coronary artery disease in J Cardiovasc Imaging. 2011;27:777 85.
women. Am J Cardiol. 2007;99:714 7. 66. Greenwood JP, Maredia N, Younger JF, et al. Cardiovascular
47. Imran MB, Palinkas A, Picano E. Head-to-head comparison of magnetic resonance and single-photon emission computed tomogra-
dipyridamole echocardiography and stress perfusion scintigraphy for phy for diagnosis of coronary heart disease (CE-MARC): a prospec-
the detection of coronary artery disease: a meta-analysis. Comparison tive trial. Lancet. 2012;379:453 60.
between stress echo and scintigraphy. Int J Cardiovasc Imaging. 67. Hundley WG, Hamilton CA, Thomas MS, et al. Utility of fast cine
2003;19:23 8. magnetic resonance imaging and display for the detection of myo-
48. Mahajan N, Polavaram L, Vankayala H, et al. Diagnostic accuracy of cardial ischemia in patients not well suited for second harmonic stress
myocardial perfusion imaging and stress echocardiography for the echocardiography. Circulation. 1999;100:1697702.
diagnosis of left main and triple vessel coronary artery disease: a 68. Nagel E, Lehmkuhl HB, Bocksch W, et al. Noninvasive diagnosis of
comparative meta-analysis. Heart. 2010;96:956 66. ischemia-induced wall motion abnormalities with the use of high-
49. Marcassa C, Bax JJ, Bengel F, et al. Clinical value, cost-effectiveness, dose dobutamine stress MRI: comparison with dobutamine stress
and safety of myocardial perfusion scintigraphy: a position statement. echocardiography. Circulation. 1999;99:76370.
Eur Heart J. 2008;29:557 63. 69. Schwitter J, Wacker CM, van Rossum AC, et al. MR-IMPACT:
50. Nandalur KR, Dwamena BA, Choudhri AF, et al. Diagnostic comparison of perfusion-cardiac magnetic resonance with single-
performance of stress cardiac magnetic resonance imaging in the photon emission computed tomography for the detection of coronary
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2590 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
artery disease in a multicentre, multivendor, randomized trial. Eur patients with normal exercise electrocardiographic testing. J Am Coll
Heart J. 2008;29:480 9. Cardiol. 2009;53:198190.
70. de Azevedo CF, Hadlich MS, Bezerra SG, et al. Prognostic value of 89. Navare SM, Mather JF, Shaw LJ, et al. Comparison of risk
CT angiography in patients with inconclusive functional stress tests. stratification with pharmacologic and exercise stress myocardial
J Am Coll Cardiol Img. 2011;4:740 51. perfusion imaging: a meta-analysis. J Nucl Cardiol. 2004;11:551 61.
71. Sarwar A, Shaw LJ, Shapiro MD, et al. Diagnostic and prognostic 90. Gebker R, Jahnke C, Manka R, et al. The role of dobutamine stress
value of absence of coronary artery calcification. J Am Coll Cardiol cardiovascular magnetic resonance in the clinical management of
Img. 2009;2:675 88. patients with suspected and known coronary artery disease. J Cardio-
72. Mock MB, Ringqvist I, Fisher LD, et al. Survival of medically treated vasc Magn Reson. 2011;13:46.
patients in the Coronary Artery Surgery Study (CASS) registry. 91. Peteiro J, Bouzas-Mosquera A, Broullon FJ, et al. Prognostic value of
Circulation. 1982;66:562 8. peak and post-exercise treadmill exercise echocardiography in pa-
73. Vitarelli A, Tiukinhoy S, Di Luzio S, et al. The role of echocardi- tients with known or suspected coronary artery disease. Eur Heart J.
ography in the diagnosis and management of heart failure. Heart Fail 2010;31:18795.
Rev. 2003;8:1819. 92. Yao SS, Wever-Pinzon O, Zhang X, et al. Prognostic value of stress
74. Christian TF, Miller TD, Bailey KR, et al. Exercise tomographic echocardiogram in patients with angiographically significant coronary
thallium201 imaging in patients with severe coronary artery disease artery disease. Am J Cardiol. 2012;109:153 8.
and normal electrocardiograms. Ann Intern Med. 1994;121:82532. 93. Shaw LJ, Cerqueira MD BM. For the BARI 2D Investigators.
75. Gibbons RJ, Zinsmeister AR, Miller TD, et al. Supine exercise Impact of left ventricular function and the extend of ischemia and
electrocardiography compared with exercise radionuclide angiography scar by stress myocardial perfusion imaging on prognosis and thera-
in noninvasive identification of severe coronary artery disease. Ann peutic risk reduction in diabetic patients with coronary artery disease:
Intern Med. 1990;112:7439. results from the bypass angioplasty revascularization investigation 2
76. Hachamovitch R, Hayes SW, Friedman JD, et al. Stress myocardial diabetes (BARI 2D) trial. J Nucl Cardiol. 2012;In Press.
perfusion single-photon emission computed tomography is clinically 94. Hachamovitch R, Rozanski A, Shaw LJ, et al. Impact of ischaemia
effective and cost effective in risk stratification of patients with a high and scar on the therapeutic benefit derived from myocardial revascu-
likelihood of coronary artery disease (CAD) but no known CAD. larization vs. medical therapy among patients undergoing stress-rest
J Am Coll Cardiol. 2004;43:200 8. myocardial perfusion scintigraphy. Eur Heart J. 2011;32:101224.
77. Kuntz KM, Fleischmann KE, Hunink MG, et al. Cost-effectiveness 95. Shaw LJ, Min JK, Hachamovitch R, et al. Nomograms for estimating
of diagnostic strategies for patients with chest pain. Ann Intern Med. coronary artery disease prognosis with gated stress myocardial perfu-
1999;130:709 18. sion SPECT. J Nucl Cardiol. 2012;19:4352.
78. Ladenheim ML, Kotler TS, Pollock BH, et al. Incremental prog- 96. Doesch C, Seeger A, Doering J, et al. Risk stratification by adenosine
nostic power of clinical history, exercise electrocardiography and stress cardiac magnetic resonance in patients with coronary artery
myocardial perfusion scintigraphy in suspected coronary artery dis- stenoses of intermediate angiographic severity. J Am Coll Cardiol
Img. 2009;2:424 33.
ease. Am J Cardiol. 1987;59:270 7.
97. Jahnke C, Nagel E, Gebker R, et al. Prognostic value of cardiac
79. Lorenzoni R, Cortigiani L, Magnani M, et al. Cost-effectiveness
magnetic resonance stress tests: adenosine stress perfusion and
analysis of noninvasive strategies to evaluate patients with chest pain.
dobutamine stress wall motion imaging. Circulation. 2007;115:
J Am Soc Echocardiogr. 2003;16:128791.
1769 76.
80. Mattera JA, Arain SA, Sinusas AJ, et al. Exercise testing with
98. Bingham SE, Hachamovitch R. Incremental prognostic significance
myocardial perfusion imaging in patients with normal baseline
of combined cardiac magnetic resonance imaging, adenosine stress
electrocardiograms: cost savings with a stepwise diagnostic strategy.
perfusion, delayed enhancement, and left ventricular function over
J Nucl Cardiol. 1998;5:498 506.
preimaging information for the prediction of adverse events. Circu-
81. Mowatt G, Vale L, Brazzelli M, et al. Systematic review of the lation. 2011;123:1509 18.
effectiveness and cost-effectiveness, and economic evaluation, of 99. Coelho-Filho OR, Seabra LF, Mongeon F-P. Stress myocardial
myocardial perfusion scintigraphy for the diagnosis and management perfusion imaging by CMR provides strong prognostic value to
of angina and myocardial infarction. Health Technol Assess. 2004; cardiac events regardless of patients sex. J Am Coll Cardiol Img.
8:iii207. 2011;4:850 61.
82. Nallamothu N, Ghods M, Heo J, et al. Comparison of thallium201 100. Kelle S, Chiribiri A, Vierecke J, et al. Long-term prognostic value
single-photon emission computed tomography and electrocardio- of dobutamine stress CMR. J Am Coll Cardiol Img. 2011;4:161
graphic response during exercise in patients with normal rest elec- 72.
trocardiographic results. J Am Coll Cardiol. 1995;25:830 6. 101. Korosoglou G, Elhmidi Y, Steen H, et al. Prognostic value of
83. Gibbons RJ, Abrams J, Chatterjee K, et al. ACC/AHA 2002 high-dose dobutamine stress magnetic resonance imaging in 1,493
guideline update for the management of patients with chronic stable consecutive patients: assessment of myocardial wall motion and
angina--summary article: a report of the American College of perfusion. J Am Coll Cardiol. 2010;56:122534.
Cardiology/American Heart Association Task Force on practice 102. Steel K, Broderick R, Gandla V, et al. Complementary prognostic
guidelines (Committee on the Management of Patients With values of stress myocardial perfusion and late gadolinium enhancement
Chronic Stable Angina). J Am Coll Cardiol. 2003;41:159 68. imaging by cardiac magnetic resonance in patients with known or
84. Johansen A, Hoilund-Carlsen PF, Vach W, et al. Prognostic value of suspected coronary artery disease. Circulation. 2009;120:1390 400.
myocardial perfusion imaging in patients with known or suspected 103. Chow BJW, Wells GA, Chen L, et al. Prognostic value of 64-slice
stable angina pectoris: evaluation in a setting in which myocardial cardiac computed tomography severity of coronary artery disease,
perfusion imaging did not influence the choice of treatment. Clin coronary atherosclerosis, and left ventricular ejection fraction. J Am
Physiol Funct Imaging. 2006;26:288 95. Coll Cardiol. 2010;55:101728.
85. Leischik R, Dworrak B, Littwitz H, et al. Prognostic significance of 104. Min JK, Dunning A, Lin FY, et al. Age- and Sex-Related Differ-
exercise stress echocardiography in 3329 outpatients (5-year longitu- ences in All-Cause Mortality Risk Based on Coronary Computed
dinal study). Int J Cardiol. 2007;119:297305. Tomography Angiography Findings Results From the International
86. Nagao T, Chikamori T, Hida S, et al. Quantitative gated single- Multicenter CONFIRM (Coronary CT Angiography Evaluation for
photon emission computed tomography with (99m)Tc sestamibi Clinical Outcomes: An International Multicenter Registry) of 23,854
predicts major cardiac events in elderly patients with known or Patients Without Known Coronary Artery Disease. J Am Coll
suspected coronary artery disease: the QGS-Prognostic Value in the Cardiol. 2011;58:849 60.
Elderly (Q-PROVE) Study. Circ J. 2007;71:1029 34. 105. America YGCJ, Bax JJ, Boersma E, et al. Prognostic value of gated
87. Wagdy HM, Hodge D, Christian TF, et al. Prognostic value of SPECT in patients with left bundle branch block. J Nucl Cardiol.
vasodilator myocardial perfusion imaging in patients with left bundle- 2007;14:75 81.
branch block. Circulation. 1998;97:156370. 106. Gil VM, Almeida M, Ventosa A, et al. Prognosis in patients with left
88. Bouzas-Mosquera A, Peteiro J, Alvarez-Garcia N, et al. Prediction of bundle branch block and normal dipyridamole thallium201 scintig-
mortality and major cardiac events by exercise echocardiography in raphy. J Nucl Cardiol. 1998;5:414 7.
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2591
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
107. Nallamothu N, Bagheri B, Acio ER, et al. Prognostic value of stress Surgery Study (CASS) registry. J Thorac Cardiovasc Surg.
myocardial perfusion single photon emission computed tomography 1989;97:48795.
imaging in patients with left ventricular bundle branch block. J Nucl 126. Myers WO, Gersh BJ, Fisher LD, et al. Medical versus early
Cardiol. 1997;4:48793. surgical therapy in patients with triple-vessel disease and mild
108. Nigam A, Humen DP. Prognostic value of myocardial perfusion angina pectoris: a CASS registry study of survival. Ann Thorac
imaging with exercise and/or dipyridamole hyperemia in patients Surg. 1987;44:471 86.
with preexisting left bundle branch block. J Nucl Med. 1998;39: 127. Bonow RO, Maurer G, Lee KL, et al. Myocardial Viability and
579 81. Survival in Ischemic Left Ventricular Dysfunction. N Engl J Med.
109. Pilz G, Jeske A, Klos M, et al. Prognostic value of normal adenosine- 2011;364:161725.
stress cardiac magnetic resonance imaging. Am J Cardiol. 2008;101: 128. Brunelli C, Cristofani R, LAbbate A. Long-term survival in medi-
1408 12. cally treated patients with ischaemic heart disease and prognostic
110. Tandogan I, Yetkin E, Yanik A, et al. Comparison of thallium201 importance of clinical and electrocardiographic data (the Italian CNR
exercise SPECT and dobutamine stress echocardiography for diag- Multicentre Prospective Study OD1). Eur Heart J. 1989;10:292303.
nosis of coronary artery disease in patients with left bundle branch 129. Chuah SC, Pellikka PA, Roger VL, et al. Role of dobutamine stress
block. Int J Cardiovasc Imaging. 2001;17:339 45. echocardiography in predicting outcome in 860 patients with known
111. Hacker M, Jakobs T, Hack N, et al. Combined use of 64-slice or suspected coronary artery disease. Circulation. 1998;97:1474 80.
computed tomography angiography and gated myocardial perfusion 130. Hachamovitch R, Berman DS, Shaw LJ, et al. Incremental prognos-
SPECT for the detection of functionally relevant coronary artery tic value of myocardial perfusion single photon emission computed
stenoses. First results in a clinical setting concerning patients with tomography for the prediction of cardiac death: differential stratifi-
stable angina. Nuklearmedizin. 2007;46:29 35. cation for risk of cardiac death and myocardial infarction. Circulation.
112. Yao SS, Bangalore S, Chaudhry FA. Prognostic implications of stress 1998;97:535 43.
echocardiography and impact on patient outcomes: an effective 131. Harris PJ, Harrell FE Jr., Lee KL, et al. Survival in medically treated
gatekeeper for coronary angiography and revascularization. J Am Soc coronary artery disease. Circulation. 1979;60:1259 69.
Echocardiogr. 2010;23:8329. 132. Ladenheim ML, Pollock BH, Rozanski A, et al. Extent and severity
113. Braunwald E, Domanski MJ, Fowler SE, et al. Angiotensin- of myocardial hypoperfusion as predictors of prognosis in patients
converting-enzyme inhibition in stable coronary artery disease. with suspected coronary artery disease. J Am Coll Cardiol. 1986;7:
N Engl J Med. 2004;351:2058 68. 464 71.
114. Fox KM. Efficacy of perindopril in reduction of cardiovascular events 133. Mark DB, Hlatky MA, Harrell FE Jr., et al. Exercise treadmill score
among patients with stable coronary artery disease: randomised, for predicting prognosis in coronary artery disease. Ann Intern Med.
double-blind, placebo-controlled, multicentre trial (the EUROPA 1987;106:793 800.
study). Lancet. 2003;362:782 8. 134. Marwick TH, Mehta R, Arheart K, et al. Use of exercise echocar-
115. Garg R, Yusuf S. Overview of randomized trials of angiotensin- diography for prognostic evaluation of patients with known or
converting enzyme inhibitors on mortality and morbidity in patients suspected coronary artery disease. J Am Coll Cardiol. 1997;30:8390.
with heart failure. Collaborative Group on ACE Inhibitor Trials.
135. Morrow K, Morris CK, Froelicher VF, et al. Prediction of cardio-
JAMA. 1995;273:1450 6.
vascular death in men undergoing noninvasive evaluation for coronary
116. Kunz R, Friedrich C, Wolbers M, et al. Meta-analysis: effect of
artery disease. Ann Intern Med. 1993;118:689 95.
monotherapy and combination therapy with inhibitors of the renin
136. Stratmann HG, Williams GA, Wittry MD, et al. Exercise techne-
angiotensin system on proteinuria in renal disease. Ann Intern Med.
tium99m sestamibi tomography for cardiac risk stratification of
2008;148:30 48.
patients with stable chest pain. Circulation. 1994;89:61522.
117. McCully RB, Roger VL, Mahoney DW, et al. Outcome after
137. Miller TD, Christian TF, Taliercio CP, et al. Impaired left ventric-
abnormal exercise echocardiography for patients with good exercise
ular function, one- or two-vessel coronary artery disease, and severe
capacity: prognostic importance of the extent and severity of exercise-
related left ventricular dysfunction. J Am Coll Cardiol. 2002;39: ischemia: outcome with medical therapy versus revascularization.
134552. Mayo Clin Proc. 1994;69:626 31.
118. Metz LD, Beattie M, Hom R, et al. The prognostic value of normal 138. Emond M, Mock MB, Davis KB, et al. Long-term survival of
exercise myocardial perfusion imaging and exercise echocardiography: medically treated patients in the Coronary Artery Surgery Study
a meta-analysis. J Am Coll Cardiol. 2007;49:22737. (CASS) Registry. Circulation. 1994;90:264557.
119. Shaw LJ, Hendel R, Borges-Neto S, et al. Prognostic value of normal 139. Alderman EL, Fisher LD, Litwin P, et al. Results of coronary artery
exercise and adenosine (99m)Tc-tetrofosmin SPECT imaging: re- surgery in patients with poor left ventricular function (CASS).
sults from the multicenter registry of 4,728 patients. J Nucl Med. Circulation. 1983;68:78595.
2003;44:134 9. 140. Boden WE, ORourke RA, Teo KK, et al. Optimal medical therapy
120. Yusuf S, Sleight P, Pogue J, et al. Effects of an angiotensin- with or without PCI for stable coronary disease. N Engl J Med.
converting-enzyme inhibitor, ramipril, on cardiovascular events in 2007;356:150316.
high-risk patients. The Heart Outcomes Prevention Evaluation 141. Shaw LJ, Berman DS, Maron DJ, et al. Optimal medical therapy
Study Investigators. N Engl J Med. 2000;342:14553. with or without percutaneous coronary intervention to reduce isch-
121. Survivors of out-of-hospital cardiac arrest with apparently normal emic burden: results from the Clinical Outcomes Utilizing Revascu-
heart. Need for definition and standardized clinical evaluation. larization and Aggressive Drug Evaluation (COURAGE) trial nu-
Consensus statement of the Joint Steering Committees of the clear substudy. Circulation. 2008;117:128391.
Unexplained Cardiac Arrest Registry of Europe and of the Idiopathic 142. McGillion M, Watt-Watson J, LeFort S, et al. Positive shifts in the
Ventricular Fibrillation Registry of the United States. Circulation. perceived meaning of cardiac pain following a psychoeducation
1997;95:26572. program for chronic stable angina. Can J Nurs Res. 2007;39:48 65.
122. Every NR, Fahrenbruch CE, Hallstrom AP, et al. Influence of 143. Muszbek N, Brixner D, Benedict A, et al. The economic conse-
coronary bypass surgery on subsequent outcome of patients resusci- quences of noncompliance in cardiovascular disease and related
tated from out of hospital cardiac arrest. J Am Coll Cardiol. conditions: a literature review. Int J Clin Pract. 2008;62:338 51.
1992;19:14359. 144. Rao SV, Schulman KA, Curtis LH, et al. Socioeconomic status and
123. Spaulding CM, Joly LM, Rosenberg A, et al. Immediate coronary outcome following acute myocardial infarction in elderly patients.
angiography in survivors of out-of-hospital cardiac arrest. N Engl Arch Intern Med. 2004;164:1128 33.
J Med. 1997;336:1629 33. 145. Mosca L, Benjamin EJ, Berra K, et al. Effectiveness-based guidelines
124. Califf RM, Harrell FE Jr., Lee KL, et al. The evolution of medical for the prevention of cardiovascular disease in women-2011 update:
and surgical therapy for coronary artery disease. A 15-year perspec- a guideline from the American Heart Association. Circulation.
tive. JAMA. 1989;261:2077 86. 2011;123:1243 62.
125. Myers WO, Schaff HV, Gersh BJ, et al. Improved survival of 146. Joint Commission. The Joint Commission announces the 2008
surgically treated patients with triple vessel coronary artery disease National Patient Safety Goals and Requirements. Jt Comm Perspect.
and severe angina pectoris. A report from the Coronary Artery 2007;27:1, 9 1,22.
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2592 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
147. Miller NH, Taylor C. Lifestyle Management for Patients with 166. Carney RM, Freedland KE, Eisen SA, et al. Major depression and
Coronary Heart Disease. (Current Issues in Cardiac Rehabilitation, medication adherence in elderly patients with coronary artery disease.
Monograph No. 2.). 1st ed. Champaign, IL: Human Kinetics; 1995. Health Psychol. 1995;14:88 90.
148. DeBusk RF, Miller NH, Superko HR, et al. A case-management 167. Rees K, Bennett P, West R, et al. Psychological interventions for
system for coronary risk factor modification after acute myocardial coronary heart disease. Cochrane Database Syst Rev. 2004;
infarction. Ann Intern Med. 1994;120:7219. CD002902.
149. Haskell WL, Alderman EL, Fair JM, et al. Effects of intensive 168. Ziegelstein RC, Fauerbach JA, Stevens SS, et al. Patients with
multiple risk factor reduction on coronary atherosclerosis and clinical depression are less likely to follow recommendations to reduce cardiac
cardiac events in men and women with coronary artery disease. The risk during recovery from a myocardial infarction. Arch Intern Med.
Stanford Coronary Risk Intervention Project (SCRIP). Circulation. 2000;160:1818 23.
1994;89:97590. 169. Lesperance F, Frasure-Smith N, Koszycki D, et al. Effects of citalopram
150. Lichtenstein AH, Appel LJ, Brands M, et al. Diet and lifestyle and interpersonal psychotherapy on depression in patients with coronary
recommendations revision 2006: a scientific statement from the artery disease: the Canadian Cardiac Randomized Evaluation of Anti-
American Heart Association Nutrition Committee. Circulation. depressant and Psychotherapy Efficacy (CREATE) trial. JAMA. 2007;
2006;114:8296. 297:36779.
151. Thompson PD, Buchner D, Pina IL, et al. Exercise and physical 170. McManus D, Pipkin SS, Whooley MA. Screening for depression in
activity in the prevention and treatment of atherosclerotic cardiovas- patients with coronary heart disease (data from the Heart and Soul
cular disease: a statement from the Council on Clinical Cardiology Study). Am J Cardiol. 2005;96:1076 81.
(Subcommittee on Exercise, Rehabilitation, and Prevention) and 171. Deleted in proof.
the Council on Nutrition, Physical Activity, and Metabolism 172. Deleted in proof.
(Subcommittee on Physical Activity). Circulation. 2003;107: 173. Glassman AH, OConnor CM, Califf RM, et al. Sertraline treatment
3109 16. of major depression in patients with acute MI or unstable angina.
152. Thompson PD, Franklin BA, Balady GJ, et al. Exercise and acute JAMA. 2002;288:7019.
cardiovascular events placing the risks into perspective: a scientific 174. Whooley MA. Depression and cardiovascular disease: healing the
statement from the American Heart Association Council on Nutri- broken-hearted. JAMA. 2006;295:2874 81.
tion, Physical Activity, and Metabolism and the Council on Clinical 175. Lichtman JH, Bigger JT Jr., Blumenthal JA, et al. Depression and
Cardiology. Circulation. 2007;115:2358 68. Coronary Heart Disease. Recommendations for Screening, Referral,
153. Artinian NT, Fletcher GF, Mozaffarian D, et al. Interventions to and Treatment. A Science Advisory From the American Heart
promote physical activity and dietary lifestyle changes for cardiovas- Association Prevention Committee of the Council on Cardiovascular
cular risk factor reduction in adults: a scientific statement from the Nursing, Council on Clinical Cardiology, Council on Epidemiology
American Heart Association. Circulation. 2010;122:406 41. and Prevention, and Interdisciplinary Council on Quality of Care and
154. National Institutes of Health, National Heart Lung and Blood Outcomes Research. Circulation. 2008;118:1768 75.
176. Dattilo AM, Kris-Etherton PM. Effects of weight reduction on
Institute. Clinical guidelines on the identification, evaluation, and
blood lipids and lipoproteins: a meta-analysis. Am J Clin Nutr.
treatment of overweight and obesity in adults: the evidence report.
1992;56:320 8.
http://www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.pdf. 1998.
177. Ginsberg HN, Kris-Etherton P, Dennis B, et al. Effects of reducing
Accessed January 6, 2012.
dietary saturated fatty acids on plasma lipids and lipoproteins in
155. Oka R, Kobayashi J, Yagi K, et al. Reassessment of the cutoff values
healthy subjects: the DELTA Study, protocol 1. Arterioscler
of waist circumference and visceral fat area for identifying Japanese
Thromb Vasc Biol. 1998;18:4419.
subjects at risk for the metabolic syndrome. Diabetes Res Clin Pract.
178. Schaefer EJ, Lamon-Fava S, Ausman LM, et al. Individual variability
2008;79:474 81.
in lipoprotein cholesterol response to National Cholesterol Education
156. Tan CE, Ma S, Wai D, et al. Can we apply the National Cholesterol
Program Step 2 diets. Am J Clin Nutr. 1997;65:82330.
Education Program Adult Treatment Panel definition of the meta- 179. Schaefer EJ, Lichtenstein AH, Lamon-Fava S, et al. Efficacy of a
bolic syndrome to Asians? Diabetes Care. 2004;27:1182 6. National Cholesterol Education Program Step 2 diet in normolipi-
157. Buse JB, Ginsberg HN, Bakris GL, et al. Primary prevention of demic and hypercholesterolemic middle-aged and elderly men and
cardiovascular diseases in people with diabetes mellitus: a scientific women. Arterioscler Thromb Vasc Biol. 1995;15:1079 85.
statement from the American Heart Association and the American 180. Yu-Poth S, Zhao G, Etherton T, et al. Effects of the National
Diabetes Association. Circulation. 2007;115:114 26. Cholesterol Education Programs Step I and Step II dietary inter-
158. Bosworth HB, Olsen MK, Dudley T, et al. The Take Control of vention programs on cardiovascular disease risk factors: a meta-
Your Blood pressure (TCYB) study: study design and methodology. analysis. Am J Clin Nutr. 1999;69:632 46.
Contemp Clin Trials. 2007;28:33 47. 181. MRC-BHF Heart Protection Study of cholesterol lowering with
159. The 2004 United States Surgeon Generals Report: The Health simvastatin in 20,536 high-risk individuals: a randomised placebo-
Consequences of Smoking. N S W Public Health Bull. 2004;15:107. controlled trial. Lancet. 2002;360:722.
160. Critchley JA, Capewell S. Mortality risk reduction associated with 182. LaRosa JC, Grundy SM, Waters DD, et al. Intensive lipid lowering
smoking cessation in patients with coronary heart disease: a system- with atorvastatin in patients with stable coronary disease. N Engl
atic review. JAMA. 2003;290:86 97. J Med. 2005;352:142535.
161. Standards of medical care in diabetes2011. Diabetes Care. 2011;34 183. Pedersen TR, Faergeman O, Kastelein JJ, et al. High-dose atorva-
Suppl 1:S11S61. statin vs usual-dose simvastatin for secondary prevention after myo-
162. Appel LJ, Champagne CM, Harsha DW, et al. Effects of compre- cardial infarction: the IDEAL study: a randomized controlled trial.
hensive lifestyle modification on blood pressure control: main results JAMA. 2005;294:2437 45.
of the PREMIER clinical trial. JAMA. 2003;289:208393. 184. The Lipid Research Clinics Coronary Primary Prevention Trial
163. Baigent C, Blackwell L, Emberson J, et al. Efficacy and safety of more results. I. Reduction in incidence of coronary heart disease. JAMA.
intensive lowering of LDL cholesterol: a meta-analysis of data from 1984;251:351 64.
170,000 participants in 26 randomised trials. Lancet. 2010;376: 185. Deleted in proof.
1670 81. 186. Canner PL, Berge KG, Wenger NK, et al. Fifteen year mortality in
164. Frattaroli J, Weidner G, Merritt-Worden TA, et al. Angina pectoris Coronary Drug Project patients: long-term benefit with niacin. J Am
and atherosclerotic risk factors in the multisite cardiac lifestyle Coll Cardiol. 1986;8:124555.
intervention program. Am J Cardiol. 2008;101:911 8. 187. Brown BG, Zhao XQ, Chait A, et al. Simvastatin and niacin,
165. Berkman LF, Blumenthal J, Burg M, et al. Effects of treating antioxidant vitamins, or the combination for the prevention of
depression and low perceived social support on clinical events after coronary disease. N Engl J Med. 2001;345:158392.
myocardial infarction: the Enhancing Recovery in Coronary Heart 188. Effects of weight loss and sodium reduction intervention on blood
Disease Patients (ENRICHD) Randomized Trial. JAMA. 2003;289: pressure and hypertension incidence in overweight people with
3106 16. high-normal blood pressure. The Trials of Hypertension Prevention,
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2593
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
phase II. The Trials of Hypertension Prevention Collaborative 210. Nathan DM, Cleary PA, Backlund JY, et al. Intensive diabetes
Research Group. Arch Intern Med. 1997;157:657 67. treatment and cardiovascular disease in patients with type 1 diabetes.
189. Stevens VJ, Corrigan SA, Obarzanek E, et al. Weight loss interven- N Engl J Med. 2005;353:264353.
tion in phase 1 of the Trials of Hypertension Prevention. The TOHP 211. Effect of intensive blood-glucose control with metformin on compli-
Collaborative Research Group. Arch Intern Med. 1993;153:849 58. cations in overweight patients with type 2 diabetes (UKPDS 34). UK
190. Whelton PK, Appel LJ, Espeland MA, et al. Sodium reduction and Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352:
weight loss in the treatment of hypertension in older persons: a 854 65.
randomized controlled trial of nonpharmacologic interventions in the 212. Dormandy JA, Charbonnel B, Eckland DJ, et al. Secondary preven-
elderly (TONE). TONE Collaborative Research Group. JAMA. tion of macrovascular events in patients with type 2 diabetes in the
1998;279:839 46. PROactive Study (PROspective pioglitAzone Clinical Trial In ma-
191. Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects croVascular Events): a randomised controlled trial. Lancet. 2005;366:
of dietary patterns on blood pressure. DASH Collaborative Research 1279 89.
Group. N Engl J Med. 1997;336:111724. 213. Skyler JS, Bergenstal R, Bonow RO, et al. Intensive glycemic control
192. Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure and the prevention of cardiovascular events: implications of the
of reduced dietary sodium and the Dietary Approaches to Stop ACCORD, ADVANCE, and VA diabetes trials: a position state-
Hypertension (DASH) diet. DASH-Sodium Collaborative Research ment of the American Diabetes Association and a scientific statement
Group. N Engl J Med. 2001;344:310. of the American College of Cardiology Foundation and the Ameri-
193. MacGregor GA, Markandu ND, Sagnella GA, et al. Double-blind can Heart Association. Circulation. 2009;119:3517.
study of three sodium intakes and long-term effects of sodium 214. Kelly TN, Bazzano LA, Fonseca VA, et al. Systematic review:
restriction in essential hypertension. Lancet. 1989;2:1244 7. glucose control and cardiovascular disease in type 2 diabetes. Ann
194. Whelton SP, Chin A, Xin X, et al. Effect of aerobic exercise on blood Intern Med. 2009;151:394 403.
pressure: a meta-analysis of randomized, controlled trials. Ann Intern 215. Selvin E, Bolen S, Yeh HC, et al. Cardiovascular outcomes in trials
Med. 2002;136:493503. of oral diabetes medications: a systematic review. Arch Intern Med.
195. Xin X, He J, Frontini MG, et al. Effects of alcohol reduction on 2008;168:2070 80.
blood pressure: a meta-analysis of randomized controlled trials. 216. Turnbull FM, Abraira C, Anderson RJ, et al. Intensive glucose
Hypertension. 2001;38:11127. control and macrovascular outcomes in type 2 diabetes. Diabetologia.
196. Appel LJ, Frohlich ED, Hall JE, et al. The importance of 2009;52:2288 98.
population-wide sodium reduction as a means to prevent cardiovas- 217. Ray KK, Seshasai SR, Wijesuriya S, et al. Effect of intensive control
cular disease and stroke: a call to action from the American Heart of glucose on cardiovascular outcomes and death in patients with
Association. Circulation. 2011;123:1138 43. diabetes mellitus: a meta-analysis of randomised controlled trials.
197. Medical Research Council trial of treatment of hypertension in Lancet. 2009;373:176572.
older adults: principal results. MRC Working Party. BMJ. 1992; 218. Currie CJ, Peters JR, Tynan A, et al. Survival as a function of
304:40512. HbA(1c) in people with type 2 diabetes: a retrospective cohort study.
198. Prevention of stroke by antihypertensive drug treatment in older
Lancet. 2010;375:4819.
persons with isolated systolic hypertension. Final results of the
219. Holman RR, Paul SK, Bethel MA, et al. 10-year follow-up of
Systolic Hypertension in the Elderly Program (SHEP). SHEP
intensive glucose control in type 2 diabetes. N Engl J Med. 2008;
Cooperative Research Group. JAMA. 1991;265:3255 64.
359:1577 89.
199. MRC trial of treatment of mild hypertension: principal results.
220. Loke YK, Kwok CS, Singh S. Comparative cardiovascular effects of
Medical Research Council Working Party. Br Med J (Clin Res Ed).
thiazolidinediones: systematic review and meta-analysis of observa-
1985;291:97104.
tional studies. BMJ. 2011;342:1309.
200. Effect of stepped care treatment on the incidence of myocardial
221. Woodcock J. Center for Drug Evaluation and Research. Decision on
infarction and angina pectoris. 5-Year findings of the hypertension
detection and follow-up program. Hypertension. 1984;6:I198-I206. continued marketing of rosiglitazone (Avandia, Avandamet,
201. The effect of treatment on mortality in mild hypertension: results of Avandaryl) [Report NDA 021071]. 2010. Available at: http://
the hypertension detection and follow-up program. N Engl J Med. www.fda.gov/downloads/Drugs/DrugSafety/PostmarketDrugSafety
1982;307:976 80. InformationforPatientsandProviders/UCM226959.pdf. Accessed
202. Five-year findings of the hypertension detection and follow-up January 15, 2011.
program. I. Reduction in mortality of persons with high blood 222. Taylor RS, Brown A, Ebrahim S, et al. Exercise-based rehabilitation
pressure, including mild hypertension. Hypertension Detection and for patients with coronary heart disease: systematic review and
Follow-up Program Cooperative Group. JAMA. 1979;242:256271. meta-analysis of randomized controlled trials. Am J Med. 2004;116:
203. Major outcomes in high-risk hypertensive patients randomized to 68292.
angiotensin-converting enzyme inhibitor or calcium channel blocker 223. Haskell WL, Lee IM, Pate RR, et al. Physical activity and public
vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to health: updated recommendation for adults from the American
Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288:298197. College of Sports Medicine and the American Heart Association.
204. Turnbull F. Effects of different blood-pressure-lowering regimens on Circulation. 2007;116:108193.
major cardiovascular events: results of prospectively-designed over- 224. US Department of Health and Human Services. 2008 Physical
views of randomised trials. Lancet. 2003;362:152735. Activity Guidelines for Americans. Washington, DC: 2008.
205. The effect of intensive treatment of diabetes on the development and 225. Ken-Dror G, Lerman Y, Segev S, et al. [Development of a Hebrew
progression of long-term complications in insulin-dependent diabetes questionnaire to be used in epidemiological studies to assess physical
mellitus. The Diabetes Control and Complications Trial Research fitnessvalidation against sub maximal stress test and predicted
Group. N Engl J Med. 1993;329:977 86. VO2max]. Harefuah. 2004;143:566 72, 623.
206. Intensive blood-glucose control with sulphonylureas or insulin com- 226. Cardinal BJ. Predicting cardiorespiratory fitness without exercise
pared with conventional treatment and risk of complications in testing in epidemiologic studies: a concurrent validity study. J
patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Epidemiol. 1996;6:315.
Study (UKPDS) Group. Lancet. 1998;352:83753. 227. Nowak Z, Plewa M, Skowron M, et al. Paffenbarger Physical Activity
207. Patel A, MacMahon S, Chalmers J, et al. Intensive Blood Glucose Questionnaire as an additional tool in clinical assessment of patients
Control and Vascular Outcomes in Patients with Type 2 Diabetes. with coronary artery disease treated with angioplasty. Kardiol Pol.
N Engl J Med. 2008;358:2560 72. 2010;68:329.
208. Dluhy RG, McMahon GT. Intensive Glycemic Control in the 228. Jurca R, Jackson AS, LaMonte MJ, et al. Assessing cardiorespiratory
ACCORD and ADVANCE Trials. N Engl J Med. 2008;358: fitness without performing exercise testing. Am J Prev Med. 2005;
2630 3. 29:18593.
209. Duckworth W, Abraira C, Moritz T, et al. Glucose Control and 229. Taylor RS, Dalal H, Jolly K, et al. Home-based versus centre-based
Vascular Complications in Veterans with Type 2 Diabetes. N Engl cardiac rehabilitation. Cochrane Database of Systematic Reviews
J Med. 2009;360:129 39. CD007130. 2010. Accessed January 6, 2012.
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2594 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
230. Clark AM, Haykowsky M, Kryworuchko J, et al. A meta-analysis of 252. Muntwyler J, Hennekens CH, Buring JE, et al. Mortality and light
randomized control trials of home-based secondary prevention pro- to moderate alcohol consumption after myocardial infarction. Lancet.
grams for coronary artery disease. Eur J Cardiovasc Prev Rehabil. 1998;352:18825.
2010;17:26170. 253. Pope CA III, Burnett RT, Thurston GD, et al. Cardiovascular
231. McCartney N, McKelvie RS, Haslam DR, et al. Usefulness of mortality and long-term exposure to particulate air pollution: epide-
weightlifting training in improving strength and maximal power miological evidence of general pathophysiological pathways of dis-
output in coronary artery disease. Am J Cardiol. 1991;67:939 45. ease. Circulation. 2004;109:717.
232. Beniamini Y, Rubenstein JJ, Faigenbaum AD, et al. High-intensity 254. Pope CA III, Muhlestein JB, May HT, et al. Ischemic heart disease
strength training of patients enrolled in an outpatient cardiac reha- events triggered by short-term exposure to fine particulate air pollu-
bilitation program. J Cardiopulm Rehabil. 1999;19:8 17. tion. Circulation. 2006;114:2443 8.
233. Bogers RP, Bemelmans WJ, Hoogenveen RT, et al. Association of 255. Pope CA III. Mortality effects of longer term exposures to fine
overweight with increased risk of coronary heart disease partly particulate air pollution: review of recent epidemiological evidence.
independent of blood pressure and cholesterol levels: a meta-analysis Inhal Toxicol. 2007;19 Suppl 1:33 8.
of 21 cohort studies including more than 300 000 persons. Arch 256. Brook RD, Rajagopalan S, Pope CA III, et al. Particulate matter air
Intern Med. 2007;167:1720 8. pollution and cardiovascular disease: An update to the scientific
234. Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and manage- statement from the American Heart Association. Circulation. 2010;
ment of the metabolic syndrome: an American Heart Association/ 121:233178.
National Heart, Lung, and Blood Institute Scientific Statement. 257. Collaborative meta-analysis of randomised trials of antiplatelet ther-
Circulation. 2005;112:273552. apy for prevention of death, myocardial infarction, and stroke in high
235. Klein S, Burke LE, Bray GA, et al. Clinical implications of obesity risk patients. BMJ. 2002;324:71 86.
with specific focus on cardiovascular disease: a statement for profes- 258. Juul-Moller S, Edvardsson N, Jahnmatz B, et al. Double-blind trial
sionals from the American Heart Association Council on Nutrition, of aspirin in primary prevention of myocardial infarction in patients
Physical Activity, and Metabolism. Circulation. 2004;110:2952 67. with stable chronic angina pectoris. The Swedish Angina Pectoris
236. Calle EE, Thun MJ, Petrelli JM, et al. Body-mass index and Aspirin Trial (SAPAT) Group. Lancet. 1992;340:14215.
mortality in a prospective cohort of U.S. adults. N Engl J Med. 259. A randomised, blinded, trial of clopidogrel versus aspirin in patients
1999;341:1097105. at risk of ischaemic events (CAPRIE). CAPRIE Steering Commit-
237. Jensen MK, Chiuve SE, Rimm EB, et al. Obesity, behavioral lifestyle tee. Lancet. 1996;348:1329 39.
factors, and risk of acute coronary events. Circulation. 2008;117: 260. Bhatt DL, Flather MD, Hacke W, et al. Patients with prior
30629. myocardial infarction, stroke, or symptomatic peripheral arterial
238. Arnlov J, Ingelsson E, Sundstrom J, et al. Impact of body mass index disease in the CHARISMA trial. J Am Coll Cardiol. 2007;49:
and the metabolic syndrome on the risk of cardiovascular disease and 1982 8.
death in middle-aged men. Circulation. 2010;121:230 6. 261. Hirsh J, Dalen JE, Fuster V, et al. Aspirin and other platelet-active
drugs. The relationship among dose, effectiveness, and side effects.
239. Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular
Chest. 1995;108:247S57S.
disease: risk factor, paradox, and impact of weight loss. J Am Coll
262. Balsano F, Rizzon P, Violi F, et al. Antiplatelet treatment with
Cardiol. 2009;53:192532.
ticlopidine in unstable angina. A controlled multicenter clinical trial.
240. Gruberg L, Weissman NJ, Waksman R, et al. The impact of obesity
The Studio della Ticlopidina nellAngina Instabile Group. Circula-
on the short-term and long-term outcomes after percutaneous coro-
tion. 1990;82:1726.
nary intervention: the obesity paradox? J Am Coll Cardiol. 2002;39:
263. The Persantine-aspirin reinfarction study. The Persantine-aspirin
578 84.
Reinfarction Study (PARIS) research group. Circulation. 1980;62:
241. Jacobs EJ, Newton CC, Wang Y, et al. Waist circumference and
V85 8.
all-cause mortality in a large US cohort. Arch Intern Med. 2010;170:
264. Kernis SJ, Harjai KJ, Stone GW, et al. Does beta-blocker therapy
1293301. improve clinical outcomes of acute myocardial infarction after suc-
242. Critchley J, Capewell S. Smoking cessation for the secondary pre- cessful primary angioplasty? J Am Coll Cardiol. 2004;43:17739.
vention of coronary heart disease. Cochrane Database Syst Rev. 265. de Peuter OR, Lussana F, Peters RJ, et al. A systematic review of
2003;CD003041. selective and non-selective beta blockers for prevention of vascular
243. Rigotti NA. Helping smokers with cardiac disease to abstain from events in patients with acute coronary syndrome or heart failure. Neth
tobacco after a stay in hospital. CMAJ. 2009;180:1283 4. J Med. 2009;67:284 94.
244. Smith PM, Burgess E. Smoking cessation initiated during hospital 266. Freemantle N, Cleland J, Young P, et al. beta Blockade after
stay for patients with coronary artery disease: a randomized controlled myocardial infarction: systematic review and meta regression analysis.
trial. CMAJ. 2009;180:1297303. BMJ. 1999;318:1730 7.
245. Ruo B, Rumsfeld JS, Hlatky MA, et al. Depressive symptoms and 267. Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on
health-related quality of life: the Heart and Soul Study. JAMA. morbidity and mortality in patients with chronic heart failure. U.S.
2003;290:21521. Carvedilol Heart Failure Study Group. N Engl J Med. 1996;334:
246. Honig A, Kuyper AM, Schene AH, et al. Treatment of post- 1349 55.
myocardial infarction depressive disorder: a randomized, placebo- 268. Tepper D. Frontiers in congestive heart failure: Effect of Metoprolol
controlled trial with mirtazapine. Psychosom Med. 2007;69:606 13. CR/XL in chronic heart failure: Metoprolol CR/XL Randomised
247. DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor Intervention Trial in Congestive Heart Failure (MERIT-HF). Con-
for noncompliance with medical treatment: meta-analysis of the gest Heart Fail. 1999;5:184 5.
effects of anxiety and depression on patient adherence. Arch Intern 269. Leizorovicz A, Lechat P, Cucherat M, et al. Bisoprolol for the
Med. 2000;160:21017. treatment of chronic heart failure: a meta-analysis on individual data
248. Yoshinaga K, Chow BJ, Williams K, et al. What is the prognostic of two placebo-controlled studiesCIBIS and CIBIS II. Cardiac
value of myocardial perfusion imaging using rubidium 82 positron Insufficiency Bisoprolol Study. Am Heart J. 2002;143:3017.
emission tomography? J Am Coll Cardiol. 2006;48:1029 39. 270. Poole-Wilson PA, Swedberg K, Cleland JG, et al. Comparison of
249. Taylor CB, Youngblood ME, Catellier D, et al. Effects of antide- carvedilol and metoprolol on clinical outcomes in patients with
pressant medication on morbidity and mortality in depressed patients chronic heart failure in the Carvedilol Or Metoprolol European Trial
after myocardial infarction. Arch Gen Psychiatry. 2005;62:792 8. (COMET): randomised controlled trial. Lancet. 2003;362:713.
250. Di Castelnuovo A., Rotondo S, Iacoviello L, et al. Meta-analysis of 271. Domanski MJ, Krause-Steinrauf H, Massie BM, et al. A comparative
wine and beer consumption in relation to vascular risk. Circulation. analysis of the results from 4 trials of beta-blocker therapy for heart
2002;105:2836 44. failure: BEST, CIBIS-II, MERIT-HF, and COPERNICUS. J Card
251. Mukamal KJ, Maclure M, Muller JE, et al. Prior alcohol consump- Fail. 2003;9:354 63.
tion and mortality following acute myocardial infarction. JAMA. 272. McMurray JJ, Ostergren J, Swedberg K, et al. Effects of candesartan
2001;285:196570. in patients with chronic heart failure and reduced left-ventricular
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2595
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
systolic function taking angiotensin-converting-enzyme inhibitors: 293. Bonaa KH, Njolstad I, Ueland PM, et al. Homocysteine lowering
the CHARM-Added trial. Lancet. 2003;362:76771. and cardiovascular events after acute myocardial infarction. N Engl
273. Nissen SE, Tuzcu EM, Libby P, et al. Effect of antihypertensive J Med. 2006;354:1578 88.
agents on cardiovascular events in patients with coronary disease and 294. Lonn E, Yusuf S, Arnold MJ, et al. Homocysteine lowering with folic
normal blood pressure: the CAMELOT study: a randomized con- acid and B vitamins in vascular disease. N Engl J Med. 2006;354:
trolled trial. JAMA. 2004;292:221725. 156777.
274. Julius S, Weber MA, Kjeldsen SE, et al. The Valsartan Antihyper- 295. Toole JF, Malinow MR, Chambless LE, et al. Lowering homocys-
tensive Long-Term Use Evaluation (VALUE) trial: outcomes in teine in patients with ischemic stroke to prevent recurrent stroke,
patients receiving monotherapy. Hypertension. 2006;48:38591. myocardial infarction, and death: the Vitamin Intervention for Stroke
275. Danchin N, Cucherat M, Thuillez C, et al. Angiotensin-converting Prevention (VISP) randomized controlled trial. JAMA. 2004;291:
enzyme inhibitors in patients with coronary artery disease and 56575.
absence of heart failure or left ventricular systolic dysfunction: an 296. Guldager B, Jelnes R, Jorgensen SJ, et al. EDTA treatment of
overview of long-term randomized controlled trials. Arch Intern intermittent claudication--a double-blind, placebo-controlled study.
Med. 2006;166:78796. J Intern Med. 1992;231:2617.
276. Al-Mallah MH, Tleyjeh IM, bdel-Latif AA, et al. Angiotensin- 297. van Rij AM, Solomon C, Packer SG, et al. Chelation therapy for
converting enzyme inhibitors in coronary artery disease and preserved intermittent claudication. A double-blind, randomized, controlled
left ventricular systolic function: a systematic review and meta- trial. Circulation. 1994;90:1194 9.
analysis of randomized controlled trials. J Am Coll Cardiol. 2006;47:
298. Sloth-Nielsen J, Guldager B, Mouritzen C, et al. Arteriographic
1576 83.
findings in EDTA chelation therapy on peripheral arteriosclerosis.
277. Pitt B, ONeill B, Feldman R, et al. The QUinapril Ischemic Event
Am J Surg. 1991;162:1225.
Trial (QUIET): evaluation of chronic ACE inhibitor therapy in
299. Knudtson ML, Wyse DG, Galbraith PD, et al. Chelation therapy for
patients with ischemic heart disease and preserved left ventricular
function. Am J Cardiol. 2001;87:1058 63. ischemic heart disease: a randomized controlled trial. JAMA. 2002;
278. H5N1 avian influenza: first steps towards development of a human 287:481 6.
vaccine. Wkly Epidemiol Rec. 2005;80:277 8. 300. Frishman WH, Heiman M, Soberman J, et al. Comparison of
279. Davis MM, Taubert K, Benin AL, et al. Influenza vaccination as celiprolol and propranolol in stable angina pectoris. Celiprolol Inter-
secondary prevention for cardiovascular disease: a science advisory national Angina Study Group. Am J Cardiol. 1991;67:66570.
from the American Heart Association/American College of Cardi- 301. Narahara KA. Double-blind comparison of once daily betaxolol
ology. J Am Coll Cardiol. 2006;48:1498 502. versus propranolol four times daily in stable angina pectoris. Betaxolol
280. de Diego C, Vila-Corcoles A, Ochoa O, et al. Effects of annual Investigators Group. Am J Cardiol. 1990;65:577 82.
influenza vaccination on winter mortality in elderly people with 302. Boberg J, Larsen FF, Pehrsson SK. The effects of beta blockade with
chronic heart disease. Eur Heart J. 2008;30:209 16. (epanolol) and without (atenolol) intrinsic sympathomimetic activity
281. Couch RB, Winokur P, Brady R, et al. Safety and immunogenicity of in stable angina pectoris. The Visacor Study Group. Clin Cardiol.
a high dosage trivalent influenza vaccine among elderly subjects. 1992;15:5915.
Vaccine. 2007;25:7656 63. 303. Ryden L. Efficacy of epanolol versus metoprolol in angina pectoris:
282. Keitel WA, Atmar RL, Cate TR, et al. Safety of high doses of report from a Swedish multicentre study of exercise tolerance. J Intern
influenza vaccine and effect on antibody responses in elderly persons. Med. 1992;231:711.
Arch Intern Med. 2006;166:11217. 304. Heidenreich PA, McDonald KM, Hastie T, et al. Meta-analysis of
283. Hulley S, Grady D, Bush T, et al. Randomized trial of estrogen plus trials comparing beta-blockers, calcium antagonists, and nitrates for
progestin for secondary prevention of coronary heart disease in stable angina. JAMA. 1999;281:192736.
postmenopausal women. Heart and Estrogen/progestin Replacement 305. Abrams J. Clinical practice. Chronic stable angina. N Engl J Med.
Study (HERS) Research Group. JAMA. 1998;280:60513. 2005;352:2524 33.
284. Anderson GL, Limacher M, Assaf AR, et al. Effects of conjugated 306. Wight LJ, VandenBurg MJ, Potter CE, et al. A large scale compar-
equine estrogen in postmenopausal women with hysterectomy: the ative study in general practice with nitroglycerin spray and tablet
Womens Health Initiative randomized controlled trial. JAMA. formulations in elderly patients with angina pectoris. Eur J Clin
2004;291:170112. Pharmacol. 1992;42:3412.
285. Manson JE, Hsia J, Johnson KC, et al. Estrogen plus progestin and 307. VandenBurg MJ, Wight LJ, Griffiths GK, et al. Sublingual nitro-
the risk of coronary heart disease. N Engl J Med. 2003;349:52334. glycerin or spray in the treatment of angina. Br J Clin Pract.
286. Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of 1986;40:524 7.
estrogen plus progestin in healthy postmenopausal women: principal 308. Rousseau MF, Pouleur H, Cocco G, et al. Comparative efficacy of
results From the Womens Health Initiative randomized controlled ranolazine versus atenolol for chronic angina pectoris. Am J Cardiol.
trial. JAMA. 2002;288:32133. 2005;95:311 6.
287. Dietary supplementation with n3 polyunsaturated fatty acids and 309. Chaitman BR, Pepine CJ, Parker JO, et al. Effects of ranolazine with
vitamin E after myocardial infarction: results of the GISSI-
atenolol, amlodipine, or diltiazem on exercise tolerance and angina
Prevenzione trial. Gruppo Italiano per lo Studio della Sopravvivenza
frequency in patients with severe chronic angina: a randomized
nellInfarto miocardico. Lancet. 1999;354:44755.
controlled trial. JAMA. 2004;291:309 16.
288. de Gaetano G. Low-dose aspirin and vitamin E in people at
310. Stone PH, Gratsiansky NA, Blokhin A, et al. Antianginal efficacy of
cardiovascular risk: a randomised trial in general practice. Collabor-
ative Group of the Primary Prevention Project. Lancet. 2001;357: ranolazine when added to treatment with amlodipine: the ERICA
89 95. (Efficacy of Ranolazine in Chronic Angina) trial. J Am Coll Cardiol.
289. Stephens NG, Parsons A, Schofield PM, et al. Randomised con- 2006;48:566 75.
trolled trial of vitamin E in patients with coronary disease: Cam- 311. Arora RR, Chou TM, Jain D, et al. The multicenter study of
bridge Heart Antioxidant Study (CHAOS). Lancet. 1996;347: enhanced external counterpulsation (MUST-EECP): effect of EECP
781 6. on exercise-induced myocardial ischemia and anginal episodes. J Am
290. Yusuf S, Dagenais G, Pogue J, et al. Vitamin E supplementation and Coll Cardiol. 1999;33:1833 40.
cardiovascular events in high-risk patients. The Heart Outcomes 312. Mannheimer C, Eliasson T, Augustinsson LE, et al. Electrical
Prevention Evaluation Study Investigators. N Engl J Med. 2000;342: stimulation versus coronary artery bypass surgery in severe angina
154 60. pectoris: the ESBY study. Circulation. 1998;97:1157 63.
291. Bjelakovic G, Nikolova D, Gluud LL, et al. Mortality in randomized 313. Hautvast RW, DeJongste MJ, Staal MJ, et al. Spinal cord stimulation
trials of antioxidant supplements for primary and secondary preven- in chronic intractable angina pectoris: a randomized, controlled
tion: systematic review and meta-analysis. JAMA. 2007;297:84257. efficacy study. Am Heart J. 1998;136:1114 20.
292. Bazzano LA, Reynolds K, Holder KN, et al. Effect of folic acid 314. van der Sloot JA, Huikeshoven M, Tukkie R, et al. Transmyocardial
supplementation on risk of cardiovascular diseases: a meta-analysis of revascularization using an XeCl excimer laser: results of a randomized
randomized controlled trials. JAMA. 2006;296:2720 6. trial. Ann Thorac Surg. 2004;78:875 81.
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2596 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
315. Guleserian KJ, Maniar HS, Camillo CJ, et al. Quality of life and trials by the Coronary Artery Bypass Graft Surgery Trialists
survival after transmyocardial laser revascularization with the holmi- Collaboration. Lancet. 1994;344:56370.
um:YAG laser. Ann Thorac Surg. 2003;75:18427. 335. Capodanno D, Caggegi A, Miano M, et al. Global Risk Classifica-
316. Myers J, Oesterle SN, Jones J, et al. Do transmyocardial and tion and Clinical SYNTAX (Synergy between Percutaneous Coro-
percutaneous laser revascularization induce silent ischemia? An as- nary Intervention with TAXUS and Cardiac Surgery) Score in
sessment by exercise testing. Am Heart J. 2002;143:10527. Patients Undergoing Percutaneous or Surgical Left Main Revascu-
317. Ballegaard S, Pedersen F, Pietersen A, et al. Effects of acupuncture in larization. J Am Coll Cardiol Intv. 2011;4:28797.
moderate, stable angina pectoris: a controlled study. J Intern Med. 336. Hannan EL, Wu C, Walford G, et al. Drug-eluting stents vs.
1990;227:2530. coronary-artery bypass grafting in multivessel coronary disease.
318. Ballegaard S, Jensen G, Pedersen F, et al. Acupuncture in severe, N Engl J Med. 2008;358:331 41.
stable angina pectoris: a randomized trial. Acta Med Scand. 1986; 337. Ellis SG, Tamai H, Nobuyoshi M, et al. Contemporary percutaneous
220:30713. treatment of unprotected left main coronary stenoses: initial results
319. Feit F, Brooks MM, Sopko G, et al. Long-term clinical outcome in from a multicenter registry analysis 1994 1996. Circulation. 1997;
the Bypass Angioplasty Revascularization Investigation Registry: 96:386772.
comparison with the randomized trial. BARI Investigators. Circula- 338. Biondi-Zoccai GG, Lotrionte M, Moretti C, et al. A collaborative
tion. 2000;101:2795 802. systematic review and meta-analysis on 1278 patients undergoing
320. King SB III, Barnhart HX, Kosinski AS, et al. Angioplasty or surgery percutaneous drug-eluting stenting for unprotected left main coro-
for multivessel coronary artery disease: comparison of eligible registry nary artery disease. Am Heart J. 2008;155:274 83.
and randomized patients in the EAST trial and influence of treat- 339. Boudriot E, Thiele H, Walther T, et al. Randomized comparison of
ment selection on outcomes. Emory Angioplasty versus Surgery Trial percutaneous coronary intervention with sirolimus-eluting stents
Investigators. Am J Cardiol. 1997;79:14539. versus coronary artery bypass grafting in unprotected left main stem
321. Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous stenosis. J Am Coll Cardiol. 2011;57:538 45.
coronary intervention versus coronary-artery bypass grafting for 340. Brener SJ, Galla JM, Bryant R III, et al. Comparison of percuta-
severe coronary artery disease. N Engl J Med. 2009;360:96172. neous versus surgical revascularization of severe unprotected left
322. Chakravarty T, Buch MH, Naik H, et al. Predictive accuracy of main coronary stenosis in matched patients. Am J Cardiol.
SYNTAX score for predicting long-term outcomes of unprotected 2008;101:169 72.
left main coronary artery revascularization. Am J Cardiol. 2011;107: 341. Buszman PE, Kiesz SR, Bochenek A, et al. Acute and late outcomes
360 6. of unprotected left main stenting in comparison with surgical
323. Grover FL, Shroyer AL, Hammermeister K, et al. A decades revascularization. J Am Coll Cardiol. 2008;51:538 45.
experience with quality improvement in cardiac surgery using the 342. Chieffo A, Magni V, Latib A, et al. 5-year outcomes following
Veterans Affairs and Society of Thoracic Surgeons national databases. percutaneous coronary intervention with drug-eluting stent implan-
Ann Surg. 2001;234:464 72. tation versus coronary artery bypass graft for unprotected left main
coronary artery lesions the milan experience. J Am Coll Cardiol Intv.
324. Kim YH, Park DW, Kim WJ, et al. Validation of SYNTAX
2010;3:595 601.
(Synergy between PCI with Taxus and Cardiac Surgery) score for
343. Chieffo A, Morici N, Maisano F, et al. Percutaneous treatment with
prediction of outcomes after unprotected left main coronary revascu-
drug-eluting stent implantation versus bypass surgery for unprotected
larization. J Am Coll Cardiol Intv. 2010;3:61223.
left main stenosis: a single-center experience. Circulation. 2006;113:
325. Morice MC, Serruys PW, Kappetein AP, et al. Outcomes in
25427.
patients with de novo left main disease treated with either
344. Lee MS, Kapoor N, Jamal F, et al. Comparison of coronary artery
percutaneous coronary intervention using paclitaxel-eluting stents
bypass surgery with percutaneous coronary intervention with drug-
or coronary artery bypass graft treatment in the Synergy Between
eluting stents for unprotected left main coronary artery disease. J Am
Percutaneous Coronary Intervention with TAXUS and Cardiac Coll Cardiol. 2006;47:864 70.
Surgery (SYNTAX) trial. Circulation. 2010;121:264553. 345. Makikallio TH, Niemela M, Kervinen K, et al. Coronary angioplasty
326. Shahian DM, OBrien SM, Filardo G, et al. The Society of Thoracic in drug eluting stent era for the treatment of unprotected left main
Surgeons 2008 cardiac surgery risk models: part 1 coronary artery stenosis compared to coronary artery bypass grafting. Ann Med.
bypass grafting surgery. Ann Thorac Surg. 2009;88:S222. 2008;40:437 43.
327. Shahian DM, OBrien SM, Normand SL, et al. Association of 346. Naik H, White AJ, Chakravarty T, et al. A meta-analysis of 3,773
hospital coronary artery bypass volume with processes of care, patients treated with percutaneous coronary intervention or surgery
mortality, morbidity, and the Society of Thoracic Surgeons composite for unprotected left main coronary artery stenosis. J Am Coll Cardiol
quality score. J Thorac Cardiovasc Surg. 2010;139:273 82. Intv. 2009;2:739 47.
328. Caracciolo EA, Davis KB, Sopko G, et al. Comparison of surgical 347. Palmerini T, Marzocchi A, Marrozzini C, et al. Comparison between
and medical group survival in patients with left main coronary artery coronary angioplasty and coronary artery bypass surgery for the
disease. Long-term CASS experience. Circulation. 1995;91:232534. treatment of unprotected left main coronary artery stenosis (the
329. Chaitman BR, Bourassa MG, Davis K, et al. Angiographic preva- Bologna Registry). Am J Cardiol. 2006;98:54 9.
lence of high-risk coronary artery disease in patient subsets (CASS). 348. Park DW, Seung KB, Kim YH, et al. Long-term safety and efficacy
Circulation. 1981;64:360 7. of stenting versus coronary artery bypass grafting for unprotected left
330. Dzavik V, Ghali WA, Norris C, et al. Long-term survival in 11,661 main coronary artery disease: 5-year results from the MAIN-
patients with multivessel coronary artery disease in the era of stenting: COMPARE (Revascularization for Unprotected Left Main Coro-
a report from the Alberta Provincial Project for Outcome Assessment nary Artery Stenosis: Comparison of Percutaneous Coronary Angio-
in Coronary Heart Disease (APPROACH) Investigators. Am plasty Versus Surgical Revascularization) registry. J Am Coll Cardiol.
Heart J. 2001;142:119 26. 2010;56:11724.
331. Takaro T, Hultgren HN, Lipton MJ, et al. The VA cooperative 349. Rodes-Cabau J, Deblois J, Bertrand OF, et al. Nonrandomized
randomized study of surgery for coronary arterial occlusive disease II. comparison of coronary artery bypass surgery and percutaneous
Subgroup with significant left main lesions. Circulation. 1976;54: coronary intervention for the treatment of unprotected left main
III107III117. coronary artery disease in octogenarians. Circulation. 2008;118:
332. Takaro T, Peduzzi P, Detre KM, et al. Survival in subgroups of 2374 81.
patients with left main coronary artery disease. Veterans Adminis- 350. Sanmartin M, Baz JA, Claro R, et al. Comparison of drug-eluting
tration Cooperative Study of Surgery for Coronary Arterial Occlusive stents versus surgery for unprotected left main coronary artery disease.
Disease. Circulation. 1982;66:14 22. Am J Cardiol. 2007;100:970 3.
333. Taylor HA, Deumite NJ, Chaitman BR, et al. Asymptomatic left 351. Seung KB, Park DW, Kim YH, et al. Stents versus coronary-artery
main coronary artery disease in the Coronary Artery Surgery Study bypass grafting for left main coronary artery disease. N Engl J Med.
(CASS) registry. Circulation. 1989;79:11719. 2008;358:178192.
334. Yusuf S, Zucker D, Peduzzi P, et al. Effect of coronary artery bypass 352. White A, Kedia G, Mirocha J, et al. Comparison of coronary artery
graft surgery on survival: overview of 10-year results from randomised bypass surgery and percutaneous drug-eluting stent implantation for
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2597
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
treatment of left main coronary artery stenosis. J Am Coll Cardiol rience from the Duke Cardiovascular Disease Databank). Am J
Card Inter. 2008;1:236 45. Cardiol. 2002;90:1017.
353. Kappetein AP, Feldman TE, Mack MJ, et al. Comparison of 374. Phillips HR, OConnor CM, Rogers J. Revascularization for heart
coronary bypass surgery with drug-eluting stenting for the treatment failure. Am Heart J. 2007;153:6573.
of left main and/or three-vessel disease: 3-year follow-up of the 375. Tarakji KG, Brunken R, McCarthy PM, et al. Myocardial viability
SYNTAX trial. Eur Heart J. 2011;32:212534. testing and the effect of early intervention in patients with advanced
354. Montalescot G, Brieger D, Eagle KA, et al. Unprotected left main left ventricular systolic dysfunction. Circulation. 2006;113:230 7.
revascularization in patients with acute coronary syndromes. Eur 376. Tsuyuki RT, Shrive FM, Galbraith PD, et al. Revascularization in
Heart J. 2009;30:2308 17. patients with heart failure. CMAJ. 2006;175:3615.
355. Lee MS, Tseng CH, Barker CM, et al. Outcome after surgery and 377. Velazquez EJ, Lee KL, Deja MA, et al. Coronary-Artery Bypass
percutaneous intervention for cardiogenic shock and left main dis- Surgery in Patients with Left Ventricular Dysfunction. N Engl
ease. Ann Thorac Surg. 2008;86:29 34. J Med. 2011;364:160716.
356. Lee MS, Bokhoor P, Park SJ, et al. Unprotected left main coronary 378. Borger van der Burg AE, Bax JJ, Boersma E, et al. Impact of
disease and ST-segment elevation myocardial infarction: a contem- percutaneous coronary intervention or coronary artery bypass grafting
porary review and argument for percutaneous coronary intervention. on outcome after nonfatal cardiac arrest outside the hospital. Am J
J Am Coll Cardiol Intv. 2010;3:7915. Cardiol. 2003;91:7859.
357. Park SJ, Kim YH, Park DW, et al. Randomized Trial of Stents versus 379. Kaiser GA, Ghahramani A, Bolooki H, et al. Role of coronary artery
Bypass Surgery for Left Main Coronary Artery Disease. N Engl surgery in patients surviving unexpected cardiac arrest. Surgery.
J Med. 2011;364:1718 27. 1975;78:749 54.
358. Jones RH, Kesler K, Phillips HR III, et al. Long-term survival 380. The BARI Investigators. Influence of diabetes on 5-year mortality
benefits of coronary artery bypass grafting and percutaneous translu- and morbidity in a randomized trial comparing CABG and PTCA in
minal angioplasty in patients with coronary artery disease. J Thorac patients with multivessel disease: the Bypass Angioplasty Revascu-
Cardiovasc Surg. 1996;111:101325. larization Investigation (BARI). Circulation. 1997;96:17619.
359. Varnauskas E. Twelve-year follow-up of survival in the randomized 381. Hueb W, Lopes NH, Gersh BJ, et al. Five-year follow-up of the
European Coronary Surgery Study. N Engl J Med. 1988;319:3327. Medicine, Angioplasty, or Surgery Study (MASS II): a randomized
360. Smith PK, Califf RM, Tuttle RH, et al. Selection of surgical or controlled clinical trial of 3 therapeutic strategies for multivessel
percutaneous coronary intervention provides differential longevity coronary artery disease. Circulation. 2007;115:10829.
benefit. Ann Thorac Surg. 2006;82:1420 8. 382. Banning AP, Westaby S, Morice MC, et al. Diabetic and nondia-
361. Brener SJ, Lytle BW, Casserly IP, et al. Propensity analysis of betic patients with left main and/or 3-vessel coronary artery disease:
long-term survival after surgical or percutaneous revascularization in comparison of outcomes with cardiac surgery and paclitaxel-eluting
patients with multivessel coronary artery disease and high-risk fea- stents. J Am Coll Cardiol. 2010;55:106775.
tures. Circulation. 2004;109:2290 5. 383. Hoffman SN, TenBrook JA, Wolf MP, et al. A meta-analysis of
362. Hannan EL, Racz MJ, Walford G, et al. Long-term outcomes of randomized controlled trials comparing coronary artery bypass graft
coronary-artery bypass grafting versus stent implantation. N Engl with percutaneous transluminal coronary angioplasty: one- to eight-
J Med. 2005;352:2174 83. year outcomes. J Am Coll Cardiol. 2003;41:1293304.
363. Di Carli MF, Maddahi J, Rokhsar S, et al. Long-term survival of 384. Malenka DJ, Leavitt BJ, Hearne MJ, et al. Comparing long-term
patients with coronary artery disease and left ventricular dysfunction: survival of patients with multivessel coronary disease after CABG or
implications for the role of myocardial viability assessment in man- PCI: analysis of BARI-like patients in northern New England.
agement decisions. J Thorac Cardiovasc Surg. 1998;116:9971004. Circulation. 2005;112:I371I376.
364. Hachamovitch R, Hayes SW, Friedman JD, et al. Comparison of the 385. Niles NW, McGrath PD, Malenka D, et al. Survival of patients with
short-term survival benefit associated with revascularization com- diabetes and multivessel coronary artery disease after surgical or
pared with medical therapy in patients with no prior coronary artery percutaneous coronary revascularization: results of a large regional
disease undergoing stress myocardial perfusion single photon emis- prospective study. Northern New England Cardiovascular Disease
sion computed tomography. Circulation. 2003;107:2900 7. Study Group. J Am Coll Cardiol. 2001;37:1008 15.
365. Sorajja P, Chareonthaitawee P, Rajagopalan N, et al. Improved 386. Weintraub WS, Stein B, Kosinski A, et al. Outcome of coronary
survival in asymptomatic diabetic patients with high-risk SPECT bypass surgery versus coronary angioplasty in diabetic patients with
imaging treated with coronary artery bypass grafting. Circulation. multivessel coronary artery disease. J Am Coll Cardiol. 1998;31:
2005;112:I311I316. 10 9.
366. Davies RF, Goldberg AD, Forman S, et al. Asymptomatic Cardiac 387. Benzer W, Hofer S, Oldridge NB. Health-related quality of life in
Ischemia Pilot (ACIP) study two-year follow-up: outcomes of patients with coronary artery disease after different treatments for
patients randomized to initial strategies of medical therapy versus angina in routine clinical practice. Herz. 2003;28:421 8.
revascularization. Circulation. 1997;95:2037 43. 388. Bonaros N, Schachner T, Ohlinger A, et al. Assessment of health-
367. Cameron A, Davis KB, Green G, et al. Coronary bypass surgery with related quality of life after coronary revascularization. Heart Surg
internal-thoracic-artery grafts effects on survival over a 15-year Forum. 2005;8:E380 E385.
period. N Engl J Med. 1996;334:216 9. 389. Bucher HC, Hengstler P, Schindler C, et al. Percutaneous translu-
368. Loop FD, Lytle BW, Cosgrove DM, et al. Influence of the minal coronary angioplasty versus medical treatment for non-acute
internal-mammary-artery graft on 10-year survival and other cardiac coronary heart disease: meta-analysis of randomised controlled trials.
events. N Engl J Med. 1986;314:1 6. BMJ. 2000;321:737.
369. Cashin WL, Sanmarco ME, Nessim SA, et al. Accelerated progres- 390. Favarato ME, Hueb W, Boden WE, et al. Quality of life in patients
sion of atherosclerosis in coronary vessels with minimal lesions that with symptomatic multivessel coronary artery disease: a comparative
are bypassed. N Engl J Med. 1984;824 8. post hoc analyses of medical, angioplasty or surgical strategies-MASS
370. Pijls NH, de BB, Peels K, et al. Measurement of fractional flow II trial. Int J Cardiol. 2007;116:364 70.
reserve to assess the functional severity of coronary-artery stenoses. 391. Hueb W, Lopes N, Gersh BJ, et al. Ten-year follow-up survival of
N Engl J Med. 1996;334:1703 8. the Medicine, Angioplasty, or Surgery Study (MASS II): a random-
371. Tonino PA, de BB, Pijls NH, et al. Fractional flow reserve versus ized controlled clinical trial of 3 therapeutic strategies for multivessel
angiography for guiding percutaneous coronary intervention. N Engl coronary artery disease. Circulation. 2010;122:949 57.
J Med. 2009;360:21324. 392. Pocock SJ, Henderson RA, Seed P, et al. Quality of life, employment
372. Sawada S, Bapat A, Vaz D, et al. Incremental value of myocardial status, and anginal symptoms after coronary angioplasty or bypass
viability for prediction of long-term prognosis in surgically revascu- surgery. 3-year follow-up in the Randomized Intervention Treatment
larized patients with left ventricular dysfunction. J Am Coll Cardiol. of Angina (RITA) Trial. Circulation. 1996;94:135 42.
2003;42:2099 105. 393. Pocock SJ, Henderson RA, Clayton T, et al. Quality of life after
373. OConnor CM, Velazquez EJ, Gardner LH, et al. Comparison of coronary angioplasty or continued medical treatment for angina:
coronary artery bypass grafting versus medical therapy on long-term three-year follow-up in the RITA2 trial. Randomized Intervention
outcome in patients with ischemic cardiomyopathy (a 25-year expe- Treatment of Angina. J Am Coll Cardiol. 2000;35:90714.
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2598 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
394. Trial of invasive versus medical therapy in elderly patients with artery stents: a science advisory from the American Heart
chronic symptomatic coronary-artery disease (TIME): a randomised Association, American College of Cardiology, Society for Cardiovas-
trial. Lancet. 2001;358:9517. cular Angiography and Interventions, American College of Surgeons,
395. Weintraub WS, Spertus JA, Kolm P, et al. Effect of PCI on quality and American Dental Association, with representation from the
of life in patients with stable coronary disease. N Engl J Med. American College of Physicians. Circulation. 2007;115:813 8.
2008;359:677 87. 415. Leon MB, Baim DS, Popma JJ, et al. A clinical trial comparing three
396. Wijeysundera HC, Nallamothu BK, Krumholz HM, et al. Meta- antithrombotic-drug regimens after coronary-artery stenting. Stent
analysis: effects of percutaneous coronary intervention versus medical Anticoagulation Restenosis Study Investigators. N Engl J Med.
therapy on angina relief. Ann Intern Med. 2010;152:370 9. 1998;339:166571.
397. Gurfinkel EP, Perez de la Hoz R, Brito VM, et al. Invasive vs 416. Mauri L, Hsieh WH, Massaro JM, et al. Stent thrombosis in
non-invasive treatment in acute coronary syndromes and prior bypass randomized clinical trials of drug-eluting stents. N Engl J Med.
surgery. Int J Cardiol. 2007;119:6572. 2007;356:1020 9.
398. Morrison DA, Sethi G, Sacks J, et al. Percutaneous coronary 417. McFadden EP, Stabile E, Regar E, et al. Late thrombosis in
intervention versus coronary artery bypass graft surgery for patients drug-eluting coronary stents after discontinuation of antiplatelet
with medically refractory myocardial ischemia and risk factors for therapy. Lancet. 2004;364:1519 21.
adverse outcomes with bypass: a multicenter, randomized trial. 418. Bonatti J, Schachner T, Bonaros N, et al. Simultaneous hybrid
Investigators of the Department of Veterans Affairs Cooperative coronary revascularization using totally endoscopic left internal mam-
Study #385, the Angina With Extremely Serious Operative Mortality mary artery bypass grafting and placement of rapamycin eluting stents
Evaluation (AWESOME). J Am Coll Cardiol. 2001;38:1439. in the same interventional session. The COMBINATION pilot
399. Subramanian S, Sabik JF, Houghtaling PL, et al. Decision-making study. Cardiology. 2008;110:925.
for patients with patent left internal thoracic artery grafts to left 419. Gilard M, Bezon E, Cornily JC, et al. Same-day combined percuta-
anterior descending. Ann Thorac Surg. 2009;87:1392 8. neous coronary intervention and coronary artery surgery. Cardiology.
400. Pfautsch P, Frantz E, Ellmer A, et al. [Long-term outcome of 2007;108:3637.
therapy of recurrent myocardial ischemia after surgical revasculariza- 420. Holzhey DM, Jacobs S, Mochalski M, et al. Minimally invasive
tion]. Z Kardiol. 1999;88:489 97. hybrid coronary artery revascularization. Ann Thorac Surg. 2008;86:
401. Weintraub WS, Jones EL, Morris DC, et al. Outcome of reoperative 1856 60.
coronary bypass surgery versus coronary angioplasty after previous 421. Kon ZN, Brown EN, Tran R, et al. Simultaneous hybrid coronary
bypass surgery. Circulation. 1997;95:868 77. revascularization reduces postoperative morbidity compared with
402. Aaberge L, Nordstrand K, Dragsund M, et al. Transmyocardial results from conventional off-pump coronary artery bypass. J Thorac
revascularization with CO2 laser in patients with refractory angina Cardiovasc Surg. 2008;135:36775.
pectoris. Clinical results from the Norwegian randomized trial. J Am 422. Reicher B, Poston RS, Mehra MR, et al. Simultaneous hybrid
Coll Cardiol. 2000;35:1170 7. percutaneous coronary intervention and minimally invasive surgical
403. Allen KB, Dowling RD, DelRossi AJ, et al. Transmyocardial laser bypass grafting: feasibility, safety, and clinical outcomes. Am Heart J.
revascularization combined with coronary artery bypass grafting: a
2008;155:6617.
multicenter, blinded, prospective, randomized, controlled trial.
423. Vassiliades TA Jr., Douglas JS, Morris DC, et al. Integrated coronary
J Thorac Cardiovasc Surg. 2000;119:540 9.
revascularization with drug-eluting stents: immediate and seven-
404. Burkhoff D, Schmidt S, Schulman SP, et al. Transmyocardial laser
month outcome. J Thorac Cardiovasc Surg. 2006;131:956 62.
revascularisation compared with continued medical therapy for treat-
424. Zhao DX, Leacche M, Balaguer JM, et al. Routine intraoperative
ment of refractory angina pectoris: a prospective randomised trial.
completion angiography after coronary artery bypass grafting and
ATLANTIC Investigators. Angina Treatments-Lasers and Normal
1-stop hybrid revascularization results from a fully integrated hybrid
Therapies in Comparison. Lancet. 1999;354:88590.
catheterization laboratory/operating room. J Am Coll Cardiol. 2009;
405. Schofield PM, Sharples LD, Caine N, et al. Transmyocardial laser
revascularisation in patients with refractory angina: a randomised 53:232 41.
controlled trial. Lancet. 1999;353:519 24. 425. Hachamovitch R, Berman DS, Kiat H, et al. Value of stress
406. Stamou SC, Boyce SW, Cooke RH, et al. One-year outcome after myocardial perfusion single photon emission computed tomography
combined coronary artery bypass grafting and transmyocardial laser in patients with normal resting electrocardiograms: an evaluation of
revascularization for refractory angina pectoris. Am J Cardiol. 2002; incremental prognostic value and cost-effectiveness. Circulation.
89:1365 8. 2002;105:8239.
407. Deleted in proof. 426. Yao SS, Qureshi E, Sherrid MV, et al. Practical applications in stress
408. Brener SJ, Lytle BW, Casserly IP, et al. Predictors of revasculariza- echocardiography: risk stratification and prognosis in patients with
tion method and long-term outcome of percutaneous coronary known or suspected ischemic heart disease. J Am Coll Cardiol.
intervention or repeat coronary bypass surgery in patients with 2003;42:1084 90.
multivessel coronary disease and previous coronary bypass surgery. 427. Shaw LJ, Hachamovitch R, Heller GV, et al. Noninvasive strategies
Eur Heart J. 2006;27:413 8. for the estimation of cardiac risk in stable chest pain patients. The
409. Lytle BW, Loop FD, Taylor PC, et al. The effect of coronary Economics of Noninvasive Diagnosis (END) Study Group. Am J
reoperation on the survival of patients with stenoses in saphenous Cardiol. 2000;86:17.
vein bypass grafts to coronary arteries. J Thorac Cardiovasc Surg. 428. Shaw LJ, Hendel RC, Cerquiera M, et al. Ethnic differences in the
1993;105:60512. prognostic value of stress technetium99m tetrofosmin gated single-
410. Sergeant P, Blackstone E, Meyns B, et al. First cardiological or photon emission computed tomography myocardial perfusion imag-
cardiosurgical reintervention for ischemic heart disease after primary ing. J Am Coll Cardiol. 2005;45:1494 504.
coronary artery bypass grafting. Eur J Cardiothorac Surg. 1998;14: 429. Sawada SG, Safadi A, Gaitonde RS, et al. Stress-induced wall
480 7. motion abnormalities with low-dose dobutamine infusion indicate
411. Stephan WJ, OKeefe JH Jr., Piehler JM, et al. Coronary angio- the presence of severe disease and vulnerable myocardium. Echocar-
plasty versus repeat coronary artery bypass grafting for patients diography. 2007;24:739 44.
with previous bypass surgery. J Am Coll Cardiol. 1996;28: 430. Lauer MS, Lytle B, Pashkow F, et al. Prediction of death and
1140 6. myocardial infarction by screening with exercise-thallium testing
412. Abizaid A, Costa MA, Centemero M, et al. Clinical and economic after coronary-artery-bypass grafting. Lancet. 1998;351:61522.
impact of diabetes mellitus on percutaneous and surgical treatment of 431. Hachamovitch R, Hayes SW, Friedman JD, et al. A prognostic score
multivessel coronary disease patients: insights from the Arterial for prediction of cardiac mortality risk after adenosine stress myocar-
Revascularization Therapy Study (ARTS) trial. Circulation. 2001; dial perfusion scintigraphy. J Am Coll Cardiol. 2005;45:7229.
104:533 8. 432. Gehi AK, Ali S, Na B, et al. Inducible ischemia and the risk of
413. Deleted in proof. recurrent cardiovascular events in outpatients with stable coronary
414. Grines CL, Bonow RO, Casey DE Jr., et al. Prevention of premature heart disease: the heart and soul study. Arch Intern Med. 2008;168:
discontinuation of dual antiplatelet therapy in patients with coronary 1423 8.
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2599
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
433. Calnon DA, McGrath PD, Doss AL, et al. Prognostic value of and double-vessel disease. Findings from the Angioplasty Compared
dobutamine stress technetium99m-sestamibi single-photon emis- to Medicine (ACME) Study. J Am Coll Cardiol. 1997;30:1256 63.
sion computed tomography myocardial perfusion imaging: stratifica- 439. Mowatt G, Cook JA, Hillis GS, et al. 64-Slice computed
tion of a high-risk population. J Am Coll Cardiol. 2001;38:15117. tomography angiography in the diagnosis and assessment of
434. Bodi V, Sanchis J, Lopez-Lereu MP, et al. Prognostic value of coronary artery disease: systematic review and meta-analysis.
dipyridamole stress cardiovascular magnetic resonance imaging in Heart. 2008;94:1386 93.
patients with known or suspected coronary artery disease. J Am Coll 440. Jones CM, Athanasiou T, Dunne N, et al. Multi-detector computed
Cardiol. 2007;50:1174 9. tomography in coronary artery bypass graft assessment: a meta-
435. Berman DS, Hachamovitch R, Kiat H, et al. Incremental value of analysis. Ann Thorac Surg. 2007;83:341 8.
prognostic testing in patients with known or suspected ischemic heart 441. Hamon M, Lepage O, Malagutti P, et al. Diagnostic performance of
16- and 64-section spiral CT for coronary artery bypass graft
disease: a basis for optimal utilization of exercise technetium99m
assessment: meta-analysis. Radiology. 2008;247:679 86.
sestamibi myocardial perfusion single-photon emission computed
442. Carrabba N, Schuijf JD, de Graaf FR, et al. Diagnostic accuracy of
tomography. J Am Coll Cardiol. 1995;26:639 47.
64-slice computed tomography coronary angiography for the detec-
436. Chatziioannou SN, Moore WH, Ford PV, et al. Prognostic value of tion of in-stent restenosis: a meta-analysis. J Nucl Cardiol. 2010;17:
myocardial perfusion imaging in patients with high exercise tolerance. 470 8.
Circulation. 1999;99:86772. 443. Sun Z, Almutairi AM. Diagnostic accuracy of 64 multislice CT
437. Peteiro J, Monserrrat L, Pineiro M, et al. Comparison of exercise angiography in the assessment of coronary in-stent restenosis: a
echocardiography and the Duke treadmill score for risk stratification meta-analysis. Eur J Radiol. 2010;73:266 73.
in patients with known or suspected coronary artery disease and
normal resting electrocardiogram. Am Heart J. 2006;151:1324 10. Key Words: ACCF/AHA Practice Guidelines y cardiovascular
438. Parisi AF, Hartigan PM, Folland ED. Evaluation of exercise thal- diagnostic techniques y coronary artery disease y coronary stenosis y
lium scintigraphy versus exercise electrocardiography in predicting minimally invasive surgical procedures y myocardial ischemia y
survival outcomes and morbid cardiac events in patients with single- myocardial revascularization y prognosis y risk factors y stable angina.
APPENDIX 1. AUTHOR RELATIONSHIPS WITH INDUSTRY AND OTHER ENTITIES (RELEVANT):
2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS GUIDELINES FOR THE DIAGNOSIS AND MANAGEMENT OF
PATIENTS WITH STABLE ISCHEMIC HEART DISEASE
Institutional,
Ownership/ Organizational, or Voting
Committee Partnership/ Other Financial Expert Recusals by
Member Employment Consultant Speakers Bureau Principal Personal Research Benefit Witness Section*
Stephan D. Veterans Health None None None None None None None
Fihn (Chair) Administration
Director, Office of
Analytics and
Business Intelligence;
University of Washington
Professor of Medicine
and of Health Services;
Head,
Division of General
Internal Medicine
Julius M. Hackensack University Arena Bristol-Myers Squibb None Merck (Expired Dec. None None 4.4.1.1
Gardin (Vice Medical Center Pharmaceuticals (Expired Dec. 2009) 2009) 4.4.1.2
Chair) Professor and (Expired Dec. 2008) CV Therapeutics 4.4.1.3
Chairman, AstraZeneca (Expired Dec. 2007) 4.4.1.5
Department of (Expired Dec. 2009) Pfizer (Expired Dec. 4.4.2.1
Internal Medicine Bristol-Myers Squibb 2009) 4.4.2.2
(Expired Dec. 2009) Takeda (Expired 4.4.2.3
CV Therapeutics Dec. 2007) 4.4.3.1
(Expired Dec. 2007) 4.4.4
Pfizer (Expired Dec.
2009)
Sanofi-aventis
(Expired 2009)
Takeda (Expired
Dec. 2007)
Jonathan University of New None None None None None None None
Abrams Mexico, Office of
CMEProfessor of
Medicine (Cardiology)
Kathleen Berra Stanford Prevention Boehringer Sanofi-aventis None Kai Pharmaceuticals PCNABoard None 4.4.1.1
Research Center Ingelheim Member 4.4.1.2
Clinical Trial Director CV Therapeutics 4.4.2.1
Gilead Sciences 4.4.2.2
Novartis 4.4.2.3
Pfizer 4.4.3.1
James C. Geisinger Medical None Sanofi-aventis None Abiomed None None 4.4.2.1
Blankenship CenterDirector AstraZeneca
Cardiology; Director Boston Scientific
Cardiac Conor Medsystems
Catheterization Kai Pharmaceutical
Laboratory Novartis
Schering-Plough
The Medicines
Company
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2600 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
Institutional,
Ownership/ Organizational, or Voting
Committee Partnership/ Other Financial Expert Recusals by
Member Employment Consultant Speakers Bureau Principal Personal Research Benefit Witness Section*
Apostolos P. Carilion Roanoke None None GlaxoSmithKline None None None 4.4.1.2
Dallas Memorial Hospital Johnson & 4.4.1.2
Director of Johnson 4.4.1.3
Continuing Medical Novartis 4.4.1.6
Education Sanofi-aventis 4.4.2.1
4.4.2.2
4.4.2.3
4.4.3.1
Pamela S. Duke University Medical None None None Novartis None None 4.4.1.1
Douglas CenterUrsula Geller 4.4.1.2
Professor of 4.4.1.3
Research in 4.4.2.3
Cardiovascular
Diseases
JoAnne M. Harvard Medical School Abbott None None None None None 2.2.2.2
Foody Associate Professor; Amarin 2.2.3.3
Brigham and Gilead 3.2.2.6
Womens/Faulkner Merck 4.4.1.1
Hospitals Novartis 4.4.1.2
Pfizer 4.4.1.3
Sanofi-aventis 4.4.3.1.4
Thomas C. Mayo ClinicRadiology, None None None None None None None
Gerber Professor of
Medicine
Alan L. University of North None None None None None None None
Hinderliter Carolina: Division of
CardiologyAssociate
Professor
Spencer B. Saint Josephs Heart Medtronic (Expired None None None Merck (DSMB) None 4.4.2.1
King III and Vascular June 2007) Wyeth 4.4.2.2
InstitutePresident; Pharmaceuticals 4.4.2.3
Saint Josephs (DSMB) 4.4.3.1
Health
SystemExecutive
Director Academic
Affairs
Paul D. Cornell Medical Cardiac Science None None None None None 2.2.1
Kligfield CenterProfessor of GE Healthcare 2.2.4.2
Medicine MDS Pharma 2.2.4.3
Services 3.2.2
Mortara Instrument 6.1
Philips Medical
Systems
Harlan M. Yale University School None None None None None None None
Krumholz of MedicineHarold
H. Hines, Jr.
Professor of
Medicine and
Epidemiology and
Public Health
Raymond Y.K. Brigham & Womens None None None None None None None
Kwong Hospital Medicine,
Cardiovascular
DivisionInstructor
of Medicine
Michael J. Lim St. Louis University Bristol-Myers Squibb None None None None None 4.4.1.1
Associate Professor Cordis 4.4.1.2
of Medicine; Division Sanofi-aventis 4.4.1.3
of Cardiology, Interim Schering-Plough 4.4.2.1.1
Director; J. Gerard 4.4.2.3
Mudd Cardiac
Catheterization
Laboratory, Director
Jane A. Mayo ClinicAssistant None None None None None None None
Linderbaum Professor of
Medicine
Michael J. The Heart Hospital None None None None None None None
Mack Baylor
PlanoDirector
Mark A. University of Utah None Gilead None Novartis None None 4.4.3.1
Munger College of
Pharmacy
Professor
Pharmacotherapy
and Internal
Medicine; Associate
Dean, Academic
Affairs
Richard L. University of Michigan None None None None None None None
Prager Hospitals and Health
CentersProfessor
of Surgery, Section of
Cardiac Surgery
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2601
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
Institutional,
Ownership/ Organizational, or Voting
Committee Partnership/ Other Financial Expert Recusals by
Member Employment Consultant Speakers Bureau Principal Personal Research Benefit Witness Section*
Joseph F. Cleveland Clinic Medtronic None None None None None 4.4.1.3
Sabik Foundation Novo Nordisk
Professor of Surgery
Leslee J. Shaw Emory University School None None None Bracco Diagnostics None None 3.2.2.6
of Medicine
Professor of
Medicine
Joanna D. University of Miami None AstraZeneca None None None None 4.4.1.1
Sikkema School of Nursing 4.4.1.2
Craig R. Smith, Columbia University None None None None None None None
Jr Chairman,
Department of
Surgery
Sidney C. Center for Eli Lilly (Expired July AstraZeneca None GlaxoSmithKline None None 4.4.2.1
Smith, Jr Cardiovascular 2007) (Expired Nov. 2009) (DSMB) (Expired March
Science and Sanofi-aventis Bayer (Expired Oct. 2009)
MedicineProfessor (Expired Sept. 2009)
of Medicine; Director 2009) Fornier (Expired May
2009)
Sanofi-aventis
(Expired Nov. 2009)
John A. MidAmerica Heart Gilead None None BMS/sanofi-aventis None None 4.4.1.1
Spertus Institute of St. Lukes Cordis 4.4.1.2
HospitalDirector, Eli Lilly 4.4.1.3
Outcomes Research; Johnson & Johnson 4.4.3.1
University of Roche Diagnostics 6.3.1
MissouriKansas
City
Sankey V. Hospital of the None None Johnson & None None None 4.4.1.1
Williams University of Johnson 4.4.1.2
Pennsylvania Merck 4.4.1.3
Solomon Katz 4.4.1.5
Professor of General 4.4.1.6
Medicine, Division of 4.4.2.1
General Internal 4.4.2.2
Medicine 4.4.2.3
This table represents the relationships of committee members with industry and other entities that were reported by authors to be relevant to this document. These relationships were reviewed and
updated in conjunction with all meetings and conference calls of the writing committee during the document development process. The table does not necessarily reflect relationships with industry at
the time of publication. A person is deemed to have a significant interest in a business if the interest represents ownership of 5% of the voting stock or share of the business entity, or ownership
of $10,000 of the fair market value of the business entity; or if funds received by the person from the business entity exceed 5% of the persons gross income for the previous year. A relationship
is considered to be modest if it is less than significant under the preceding definition. Relationships in this table are modest unless otherwise noted.
The current guideline was developed during the transition in RWI policy and occurred over an extended period of time. In the interest of transparency, we provide full information on RWI existing over the
entire period of guideline development, including delineation of relationships that expired 24 months before the guideline was finalized.
*Writing committee members are required to recuse from voting on sections to which their specific relationships with industry and other entities could apply. Section numbers apply to the full-text
guideline. Significant relationship. No financial benefit.
CV indicates cardiovascular; DSMB, data safety and monitoring board; and SAQ, Seattle Angina Questionnaire.
APPENDIX 2. REVIEWER RELATIONSHIPS WITH INDUSTRY AND OTHER ENTITIES (RELEVANT):
2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS GUIDELINES FOR THE DIAGNOSIS AND MANAGEMENT OF
PATIENTS WITH STABLE ISCHEMIC HEART DISEASE
Institutional,
Ownership/ Organizational, or
Partnership/ Other Financial
Reviewer Representation Consultant Speaker Principal Research Benefit Expert Witness
Ralph G. Brindis Official ReviewerACCF None None None None None None
Board of Trustees
Timothy D. Official ReviewerAHA CV Therapeutics None None Baxter* None None
Henry Sanofi-aventis CV Therapeutics*
Judith S. Official Reviewer Eli Lilly None None Johnson & Johnson
Hochman ACCF/AHA Task GlaxoSmithKline Merck
Force on Practice
Guidelines
Robert H. Jones Official ReviewerSTS None None None None None None
Janet B. Long Official ReviewerPCNA None AstraZeneca None None None None
Bruce W. Lytle Official ReviewerAATS None None None None None None
Douglass A. Official ReviewerSCAI None None None None None None
Morrison
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
2602 Fihn et al. JACC Vol. 60, No. 24, 2012
Stable Ischemic Heart Disease: Executive Summary December 18, 2012:2564603
Institutional,
Ownership/ Organizational, or
Partnership/ Other Financial
Reviewer Representation Consultant Speaker Principal Research Benefit Expert Witness
E. Magnus Official ReviewerAHA Abiomed CV Therapeutics* Inovise* Bristol-Myers None None
Ohman Datascope The Medicines Squibb*
Inovise* Company* Daiichi-Sankyo*
Liposcience Eli Lilly*
The Medicines The Medicines
Company Company*
Response Millennium
Biomedical Pharmaceuticals*
Sanofi-aventis*
Schering-Plough*
Douglas K. Official ReviewerACP GE Healthcare* None None None None None
Owens
Paul Poirier Official ReviewerACCF None None None None None None
Board of Governors
Amir Qaseem Official ReviewerACP None None None None None None
Joyce L. Ross Official ReviewerPCNA Kaneka America Abbott None None None None
AstraZeneca*
Bristol-Myers
Squibb
Oscient
Pfizer
Sanofi-aventis
Timothy A. Official ReviewerSCAI None The Medicines None St. Jude Medical None None
Sanborn Company (DSMB)
Merck
Jeffrey L. Content Reviewer BMS/sanofi-aventis None None None None None
Anderson ACCF/AHA Task Daiichi-Sankyo
Force on Practice Eli Lilly
Guidelines
William E. Content Reviewer Abbott Medicure Pharma None None None None
Boden CV Therapeutics/
Gilead*
Sanofi-aventis
Schering-Plough
Matthew Budoff Content Reviewer None None None None None None
ACCF Imaging
Council
Kim A. Eagle Content Reviewer None None None None None None
Gordon A. Ewy Content Reviewer None None None None None None
Victor Ferrari Content Reviewer None None None None None None
ACCF Imaging
Council
Raymond J. Content Reviewer Cardiovascular None None Velomedix* None None
Gibbons Clinical Studies
Lantheus Medical
Imaging
Medscape
Molecular Insight
TherOx
Linda Gillam Content Reviewer Abbott Vascular None None None Core Lab None
ACCF Imaging Edwards Services
Council Lifesciences
Robert A. Content Reviewer None None None Edwards None None
Guyton ACCF/AHA Task Lifesciences
Force on Practice
Guidelines
L. David Hillis Content Reviewer None None None None None None
David R. Content Reviewer None None None None None None
Holmes ACCF Interventional
Scientific Council
Hani Jneid Content Reviewer None None None None None None
AHA Council on
Clinical Cardiology
Sanjay Kaul Content Reviewer None None None None None None
Howard C. Content Reviewer None None Positron None None None
Lewin ACCF Imaging Imaging
Council Partners
Todd D. Miller Content Reviewer The Medicines None None Kai Pharmaceuticals None None
AHA Council on Company King
Clinical Cardiology TherOx Pharmaceuticals
Lantheus Medical
Imaging
Molecular Insight
Pharmaceuticals
L. Kristin Newby Content Reviewer Adolor Daiichi-Sankyo None AstraZeneca None None
AHA Council on Biovascular BG Medicine
Clinical Cardiology CV Therapeutics Carvio Dx*
Inverness Medical GlaxoSmithKline*
Johnson & Johnson Medicare*
Novartis Millennium
Roche Diagnostics Pharmaceuticals
Schering-Plough*
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
JACC Vol. 60, No. 24, 2012 Fihn et al. 2603
December 18, 2012:2564603 Stable Ischemic Heart Disease: Executive Summary
Institutional,
Ownership/ Organizational, or
Partnership/ Other Financial
Reviewer Representation Consultant Speaker Principal Research Benefit Expert Witness
Elizabeth Ross Content Reviewer None None None None None None
William S. Content Reviewer AstraZeneca* None None Abbott* None 2004; Defendant;
Weintraub Bayer* AstraZeneca* Aprotinin
Bristol-Myers Bristol-Myers 2008; Defendant;
Squibb Squibb* Quetiapine
Cardionet Otsuka* 2008; Defendant;
Eli Lilly Sanofi-aventis* Celebrex
Pfizer*
Sanofi-aventis
Shionogi
This table represents the relationships of reviewers with industry and other entities that were disclosed at the time of peer review. It does not necessarily reflect relationships with industry at the time
of publication. A person is deemed to have a significant interest in a business if the interest represents ownership of 5% of the voting stock or share of the business entity, or ownership of >$10,000
of the fair market value of the business entity; or if funds received by the person from the business entity exceed 5% of the persons gross income for the previous year. A relationship is considered
to be modest if it is less than significant under the preceding definition. Relationships noted in this table are modest unless otherwise noted.
*Significant relationship.
AATS indicates American Association for Thoracic Surgery; ACCF, American College of Cardiology Foundation; ACP, American College of Physicans; AHA, American Heart Association; NIH, National
Institutes of Health; PCNA, Preventive Cardiovascular Nurses Association; SCAI, Society for Cardiovascular Interventions and Angiography; and STS, Society of Thoracic Surgeons.
Downloaded From: http://content.onlinejacc.org/ on 03/08/2013
S-ar putea să vă placă și
- Crash Cart Comp. 2018Document1 paginăCrash Cart Comp. 2018Roxenette Gil Pangilinan RNÎncă nu există evaluări
- Perioperative Management of Anticoagulant andDocument14 paginiPerioperative Management of Anticoagulant andIlija Kosić100% (2)
- RACGP - Bones and JointsDocument31 paginiRACGP - Bones and JointstjelongÎncă nu există evaluări
- Blood Pressure ChartDocument5 paginiBlood Pressure Chartmahajan1963100% (1)
- 2013 Imagen Cardiaca en Falla CardiacaDocument25 pagini2013 Imagen Cardiaca en Falla CardiacaCarlos DiazÎncă nu există evaluări
- Interpretación TroponinaDocument37 paginiInterpretación TroponinaSteven WalkerÎncă nu există evaluări
- Cateterismo Cardiaco Consenso Americano 2012Document85 paginiCateterismo Cardiaco Consenso Americano 2012Jorge Alejandro Sepulveda GallegoÎncă nu există evaluări
- Management of Patients With Peripheral Artery Disease (Compilation of 2005 and 2011 ACCF/AHA Guideline Recommendations)Document16 paginiManagement of Patients With Peripheral Artery Disease (Compilation of 2005 and 2011 ACCF/AHA Guideline Recommendations)Nurul Azmi Rosmala PutriÎncă nu există evaluări
- J Jacc 2022 08 004Document171 paginiJ Jacc 2022 08 004Sur AJÎncă nu există evaluări
- Acc:aha Hypertension Guideline 2017Document56 paginiAcc:aha Hypertension Guideline 2017Nicoleta Popa-FoteaÎncă nu există evaluări
- Acc Aha Ventricular Aritmia SCD 2017 PDFDocument130 paginiAcc Aha Ventricular Aritmia SCD 2017 PDFJuwita PratiwiÎncă nu există evaluări
- Manejo Da SCADocument51 paginiManejo Da SCAaj2713Încă nu există evaluări
- S76 FullDocument28 paginiS76 FullAAÎncă nu există evaluări
- Guias de Revascularizacion CoronariaDocument19 paginiGuias de Revascularizacion CoronariaoscarpalaciosÎncă nu există evaluări
- 2018 AHA/ACC Guideline For The Management of Adults With Congenital Heart DiseaseDocument171 pagini2018 AHA/ACC Guideline For The Management of Adults With Congenital Heart DiseaseDr-Mohammed Farid KadhimÎncă nu există evaluări
- Adults With Congeital Heart disease-AHA 2018 PDFDocument175 paginiAdults With Congeital Heart disease-AHA 2018 PDFDanissa Fidia PuteriÎncă nu există evaluări
- ACC AHA 2013 Guideline On The Assessment of Cardiovascular RiskDocument25 paginiACC AHA 2013 Guideline On The Assessment of Cardiovascular RiskAbdul AzisÎncă nu există evaluări
- 2018 AHA Guidelines For Management of Blood CholesterolDocument66 pagini2018 AHA Guidelines For Management of Blood CholesterolsarumaxÎncă nu există evaluări
- 2018 Guideline On The Management of Blood CholesterolDocument42 pagini2018 Guideline On The Management of Blood CholesterolkarenÎncă nu există evaluări
- American GuidelinesDocument37 paginiAmerican GuidelinesElena RMÎncă nu există evaluări
- CIR 0b013e3182742c84Document27 paginiCIR 0b013e3182742c84tonklasi123Încă nu există evaluări
- CIR 0b013e3182742cf6 FullDocument88 paginiCIR 0b013e3182742cf6 FullKussetya AnggaÎncă nu există evaluări
- Acc-Aha Practice GuidelineDocument12 paginiAcc-Aha Practice GuidelineShofa ShofiatunnisaÎncă nu există evaluări
- ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 Appropriate Use Criteria for Coronary RevascularizationDocument30 paginiACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 Appropriate Use Criteria for Coronary RevascularizationFahmi RaziÎncă nu există evaluări
- AHA Performance Measures For Adults With Coronary Artery Desease and HipertensionDocument28 paginiAHA Performance Measures For Adults With Coronary Artery Desease and HipertensionPaty Alatorre IcazaÎncă nu există evaluări
- 2011 Uso Apropiado de EcoDocument41 pagini2011 Uso Apropiado de EcoRobertoÎncă nu există evaluări
- 2018 AHA Guidelines BradicardiaDocument106 pagini2018 AHA Guidelines BradicardiaArio Richard NinaÎncă nu există evaluări
- 570 Full PDFDocument22 pagini570 Full PDFSyilla PriscilliaÎncă nu există evaluări
- 2013 AHA/ACC Guideline On Lifestyle Management To Reduce Cardiovascular RiskDocument24 pagini2013 AHA/ACC Guideline On Lifestyle Management To Reduce Cardiovascular RiskMiguel VillamilÎncă nu există evaluări
- 2013 Lifestyle ManagementDocument24 pagini2013 Lifestyle ManagementAnn DahngÎncă nu există evaluări
- Aha PDFDocument151 paginiAha PDFYassef Helicoidal AntunezÎncă nu există evaluări
- 2015 ACC AHA HRS Guideline For The Management of Adult Patients With Supraventricular TachycardiaDocument89 pagini2015 ACC AHA HRS Guideline For The Management of Adult Patients With Supraventricular TachycardiaMoises Torres AlvarezÎncă nu există evaluări
- 2015 ACC/AHA/HRS Guideline For The Management of Adult Patients With Supraventricular TachycardiaDocument89 pagini2015 ACC/AHA/HRS Guideline For The Management of Adult Patients With Supraventricular TachycardiaKevin EsquivelÎncă nu există evaluări
- Angina Cronica Estable 2014 JACCDocument21 paginiAngina Cronica Estable 2014 JACCGustavo Reyes QuezadaÎncă nu există evaluări
- 2014 AHA/ACC/HRS Guideline For The Management of Patients With Atrial Fibrillation: Executive SummaryDocument35 pagini2014 AHA/ACC/HRS Guideline For The Management of Patients With Atrial Fibrillation: Executive SummaryLUIS ANGEL RUIZ ZAMORAÎncă nu există evaluări
- GuidelineDocument83 paginiGuidelineSyilla PriscilliaÎncă nu există evaluări
- 2008 Device-Based Therapy of Cardiac Rhythm AbnormalitiesDocument62 pagini2008 Device-Based Therapy of Cardiac Rhythm AbnormalitiesRafi UllahÎncă nu există evaluări
- 2018 Aha/Acc/Aacvpr/Aapa/ Abc/Acpm/Ada/Ags/Apha/Aspc/ NLA/PCNA Guideline On The Management of Blood CholesterolDocument66 pagini2018 Aha/Acc/Aacvpr/Aapa/ Abc/Acpm/Ada/Ags/Apha/Aspc/ NLA/PCNA Guideline On The Management of Blood CholesterolTom BiusoÎncă nu există evaluări
- J Jacc 2020 11 018Document173 paginiJ Jacc 2020 11 018Ashvanee sharmaÎncă nu există evaluări
- 2016 Acc PadDocument92 pagini2016 Acc PadiqbalaminÎncă nu există evaluări
- Acc Aha 2017Document129 paginiAcc Aha 2017nancy graceÎncă nu există evaluări
- Ecocardigrafia en EmergenciaDocument26 paginiEcocardigrafia en EmergenciaIvana Bravo OsorioÎncă nu există evaluări
- 2021 Aha/Acc/Ase/Chest/Saem/ SCCT/SCMR Guideline For The Evaluation and Diagnosis of Chest Pain: Executive SummaryDocument44 pagini2021 Aha/Acc/Ase/Chest/Saem/ SCCT/SCMR Guideline For The Evaluation and Diagnosis of Chest Pain: Executive SummaryernestoÎncă nu există evaluări
- Management TOF in AdultDocument103 paginiManagement TOF in AdultBagus Budi SantosoÎncă nu există evaluări
- J Jacc 2021 07 052Document44 paginiJ Jacc 2021 07 052andrew timanta brahmanaÎncă nu există evaluări
- J Jacc 2018 10 038Document29 paginiJ Jacc 2018 10 038totya91Încă nu există evaluări
- Guias de Manejo Dislipidemia Aha 2018Document120 paginiGuias de Manejo Dislipidemia Aha 2018Maria Fernanda CoralÎncă nu există evaluări
- 2016 AHA/ACC Guideline On The Management of Patients With Lower Extremity Peripheral Artery DiseaseDocument56 pagini2016 AHA/ACC Guideline On The Management of Patients With Lower Extremity Peripheral Artery DiseaseSilvana-Elena HojdaÎncă nu există evaluări
- Guia de ICC ACC 2022 PDFDocument159 paginiGuia de ICC ACC 2022 PDFMauricio villota taquezÎncă nu există evaluări
- 2017 ACC - AHA - HRS Directrices para La Evaluación y Manejo de Los Pacientes Con SyncopeDocument109 pagini2017 ACC - AHA - HRS Directrices para La Evaluación y Manejo de Los Pacientes Con SyncopePaty Alatorre IcazaÎncă nu există evaluări
- Accepted Manuscript: Journal of The American College of CardiologyDocument47 paginiAccepted Manuscript: Journal of The American College of CardiologyRyan RepvblikanÎncă nu există evaluări
- 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Top 10 Take-Home MessagesDocument24 pagini2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Top 10 Take-Home MessagesAna RuizÎncă nu există evaluări
- J Jacc 2023 03 410Document23 paginiJ Jacc 2023 03 410Luis David Sanchez MayoÎncă nu există evaluări
- 2015 ACC/AHA/HRS Guideline For The Management of Adult Patients With Supraventricular TachycardiaDocument69 pagini2015 ACC/AHA/HRS Guideline For The Management of Adult Patients With Supraventricular TachycardiaAfek ProductionÎncă nu există evaluări
- CPG AfDocument49 paginiCPG AfjickÎncă nu există evaluări
- 2018 ACC-AHA-HRS Guideline On The Evaluation and Management of Patients With Bradicardia y Trastornos de La Conduccion CardiacaDocument181 pagini2018 ACC-AHA-HRS Guideline On The Evaluation and Management of Patients With Bradicardia y Trastornos de La Conduccion CardiacaDra. Maclo Salido R1MFÎncă nu există evaluări
- 2019 ACC AHA Guidelines For Primary Prevention of CV DiseaseDocument39 pagini2019 ACC AHA Guidelines For Primary Prevention of CV DiseaseArdel RomeroÎncă nu există evaluări
- Aha 2014 NsteacDocument83 paginiAha 2014 NsteaccindyÎncă nu există evaluări
- NT StemiDocument241 paginiNT StemiRholter Dave LeeÎncă nu există evaluări
- Aha 2014Document123 paginiAha 2014Nereida AceitunoÎncă nu există evaluări
- 2021 ACC/AHA/SCAI Guidelines On Coronary Artery RevascularizationDocument109 pagini2021 ACC/AHA/SCAI Guidelines On Coronary Artery Revascularizationalexandan100% (1)
- Specific Heart Muscle DiseaseDe la EverandSpecific Heart Muscle DiseaseCecil SymonsÎncă nu există evaluări
- Vital Directions for Health & Health Care: An Initiative of the National Academy of MedicineDe la EverandVital Directions for Health & Health Care: An Initiative of the National Academy of MedicineÎncă nu există evaluări
- Gota NEJMDocument11 paginiGota NEJMPerejiloÎncă nu există evaluări
- Circadian Rhythm NEJMDocument12 paginiCircadian Rhythm NEJMtjelongÎncă nu există evaluări
- 4 5931499803149076504 PDFDocument126 pagini4 5931499803149076504 PDFCristianAltunaSotomayorÎncă nu există evaluări
- Lee Kuan Yew, Founding PM of Singapore, Dies at 91Document13 paginiLee Kuan Yew, Founding PM of Singapore, Dies at 91H.S.Încă nu există evaluări
- Diabetes y Enfermedades CardiovascularesDocument69 paginiDiabetes y Enfermedades CardiovascularesSMIBA MedicinaÎncă nu există evaluări
- Chinese Kinship Terms (Oxford Dictionary)Document1 paginăChinese Kinship Terms (Oxford Dictionary)tjelongÎncă nu există evaluări
- ESC Guidelines CardiomyopathiesDocument124 paginiESC Guidelines CardiomyopathiesSergio Mora CanelaÎncă nu există evaluări
- Autoimmune Encephalitis Review (Lancet 2016)Document14 paginiAutoimmune Encephalitis Review (Lancet 2016)tjelongÎncă nu există evaluări
- 2019 ESC Guidelines For The Diagnosis and Management of Chronic Coronary SyndromeDocument71 pagini2019 ESC Guidelines For The Diagnosis and Management of Chronic Coronary SyndromeOber SánchezÎncă nu există evaluări
- NEJM Notable Articles Of2016 PDFDocument55 paginiNEJM Notable Articles Of2016 PDFmatteoÎncă nu există evaluări
- Accelerated Idioventricular RhythymDocument4 paginiAccelerated Idioventricular RhythymtjelongÎncă nu există evaluări
- NVDPA Managment Guideline Quick Reference Guide PDFDocument8 paginiNVDPA Managment Guideline Quick Reference Guide PDFtjelongÎncă nu există evaluări
- Nejmoa 070829Document14 paginiNejmoa 070829farracholidia_867630Încă nu există evaluări
- Absolute CVD ManagementDocument124 paginiAbsolute CVD ManagementtjelongÎncă nu există evaluări
- Medical Management of Chronic Stable Angina (Australian Guideline)Document8 paginiMedical Management of Chronic Stable Angina (Australian Guideline)tjelongÎncă nu există evaluări
- Physician Burnout The Root of The Problem and The Path To SolutionsDocument52 paginiPhysician Burnout The Root of The Problem and The Path To SolutionstjelongÎncă nu există evaluări
- Medical Management of Chronic Stable Angina (Australian Guideline)Document8 paginiMedical Management of Chronic Stable Angina (Australian Guideline)tjelongÎncă nu există evaluări
- Changing Landscape of Nursing Homes in SingaporeDocument7 paginiChanging Landscape of Nursing Homes in SingaporetjelongÎncă nu există evaluări
- Austin Evidence Based CVDocument2 paginiAustin Evidence Based CVtjelongÎncă nu există evaluări
- Diabetes ManagementDocument200 paginiDiabetes ManagementPritam DugarÎncă nu există evaluări
- The Day You Gave Us o Lord Has EndedDocument1 paginăThe Day You Gave Us o Lord Has EndedtjelongÎncă nu există evaluări
- Changing Landscape of Nursing Homes in SingaporeDocument7 paginiChanging Landscape of Nursing Homes in SingaporetjelongÎncă nu există evaluări
- Praise To The Lord The AlmightyDocument1 paginăPraise To The Lord The AlmightytjelongÎncă nu există evaluări
- FeverDocument2 paginiFevertjelongÎncă nu există evaluări
- The Importance of Being Continent Control of VoidingDocument11 paginiThe Importance of Being Continent Control of VoidingtjelongÎncă nu există evaluări
- Contraception - Is It Always Wrong (Grisez)Document33 paginiContraception - Is It Always Wrong (Grisez)tjelongÎncă nu există evaluări
- Health Status of Manitobans ReportDocument78 paginiHealth Status of Manitobans ReportCityNewsTorontoÎncă nu există evaluări
- Tube+Aftercare+Tear Off+Sheets+PDFDocument8 paginiTube+Aftercare+Tear Off+Sheets+PDFNikola StojsicÎncă nu există evaluări
- 4.2 Endo - Nisha GargDocument556 pagini4.2 Endo - Nisha GargSrishti SrivastavaÎncă nu există evaluări
- Lifestyle ModificationDocument48 paginiLifestyle ModificationPGI MANALILI MARIA DIANAÎncă nu există evaluări
- Psychological Impact of COVID-19 in Grade 12 HUMSSDocument18 paginiPsychological Impact of COVID-19 in Grade 12 HUMSSPsyche AnithaÎncă nu există evaluări
- Presented by Animesh Amal: Brand Plan On Salbutamol + Ambroxol + GuaifenesinDocument36 paginiPresented by Animesh Amal: Brand Plan On Salbutamol + Ambroxol + GuaifenesinAnonymous 75aETJ8OÎncă nu există evaluări
- What's in A Name? - The Kew AsylumDocument9 paginiWhat's in A Name? - The Kew AsylumIsabelle FarlieÎncă nu există evaluări
- Epidemiology & Health Information: NU1103 Tara Brookes @tarapb8Document40 paginiEpidemiology & Health Information: NU1103 Tara Brookes @tarapb8smartisaacÎncă nu există evaluări
- NABH 5 STD April 2020Document120 paginiNABH 5 STD April 2020kapil100% (7)
- Responsibility, Authority and Accountability of EHS/ERT TeamDocument1 paginăResponsibility, Authority and Accountability of EHS/ERT Teamsuraj rawatÎncă nu există evaluări
- FKIK DikonversiDocument119 paginiFKIK DikonversiIera TajudinÎncă nu există evaluări
- Pathogens: A 2021 Update On Syphilis: Taking Stock From Pathogenesis To VaccinesDocument14 paginiPathogens: A 2021 Update On Syphilis: Taking Stock From Pathogenesis To Vaccinesgupro tahiÎncă nu există evaluări
- What We Need From You: Please Return Page 2 Via Fax To (512) 738-8397Document2 paginiWhat We Need From You: Please Return Page 2 Via Fax To (512) 738-8397Tàrár ŁàráibÎncă nu există evaluări
- Final HICC Manual AIIMSDocument35 paginiFinal HICC Manual AIIMSNaMakÎncă nu există evaluări
- NCM 210 LECT - Primary Health CareDocument7 paginiNCM 210 LECT - Primary Health CareLYRIZZA LEA BHEA DESIATAÎncă nu există evaluări
- Letter From TGA DR Leonie Hunt To Balmoral Naval Hospital DR George Blackwood, 19 July 2000 PDFDocument3 paginiLetter From TGA DR Leonie Hunt To Balmoral Naval Hospital DR George Blackwood, 19 July 2000 PDFHenry BelotÎncă nu există evaluări
- Rundown 2nd Annual Plastic Surgery in Daily PracticeDocument2 paginiRundown 2nd Annual Plastic Surgery in Daily PracticeIzar AzwarÎncă nu există evaluări
- Medical and Dental Clearance.1 2017Document2 paginiMedical and Dental Clearance.1 2017cristina tamonteÎncă nu există evaluări
- PHE Complete Immunisation Schedule Jan2020 PDFDocument2 paginiPHE Complete Immunisation Schedule Jan2020 PDFJyotirmaya RajaÎncă nu există evaluări
- Certificate 2Document1 paginăCertificate 2api-339742296Încă nu există evaluări
- Markel H - The Stethoscope and The Art of Listening 2006Document3 paginiMarkel H - The Stethoscope and The Art of Listening 2006GeorgianaRamonaÎncă nu există evaluări
- MalariaDocument38 paginiMalariaMehroze FatimaÎncă nu există evaluări
- God is Our Refuge in Times of TroubleDocument3 paginiGod is Our Refuge in Times of TroubleMarcelo piñaÎncă nu există evaluări
- OSCE GuideDocument184 paginiOSCE GuideKesavaa VasuthavenÎncă nu există evaluări
- Pulp Therapy For Primary and Immature Permanent Teeth: Latest RevisionDocument9 paginiPulp Therapy For Primary and Immature Permanent Teeth: Latest RevisionGhufran KhalilÎncă nu există evaluări
- BBBFDocument3 paginiBBBFSkAliHassanÎncă nu există evaluări
- Post Dural Puncture HeadacheDocument7 paginiPost Dural Puncture Headachedrsaurav86623Încă nu există evaluări
- Exams NAC Guideline Rating ScaleDocument2 paginiExams NAC Guideline Rating ScaleM.Dalani100% (1)