Documente Academic
Documente Profesional
Documente Cultură
The Digestive System Part 1
Încărcat de
nadya wahyuDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
The Digestive System Part 1
Încărcat de
nadya wahyuDrepturi de autor:
Formate disponibile
Art & science If you would like to contribute to the Art & science
section, email gwen.clarke@rcnpublishing.co.uk
The synthesis of art and science is lived by the nurse in the nursing act
Josephine G Paterson
The digestive system: part 1
Johnstone C et al (2014) The digestive system: part 1.
Nursing Standard. 28, 24, 37-45. Date of submission: December 7 2012; date of acceptance: March 18 2013.
THE DIGESTIVE SYSTEM is the collective name
Abstract for the gastrointestinal tract or the alimentary canal
This article, which forms part of the life sciences series and is the and accessory organs associated with digestion
first of two articles on the digestive system, explores the structure (Figure 1). The gastrointestinal tract is a hollow
and function of the digestive system. It is important that nurses tube that is approximately 29 feet long in adults
understand how the digestive system works and its role in maintaining (Thibodeau and Patton 2008). It starts at the
health. The article describes the gross structure of the gastrointestinal mouth, passes through the thorax, abdomen
tract along with relevant physiology. It also outlines several disorders and pelvis, and terminates at the anus (Waugh
of the gastrointestinal tract and their treatment and nursing and Grant 2010). The accessory organs include
management. The second article will explain the liver, pancreas the teeth, tongue, salivary glands, and exocrine
and gall bladder and their digestive functions, and provides a brief pancreas, liver and gall bladder (Waugh and Grant
overview of the disorders of chronic liver disease, pancreatitis and 2010, Sherwood 2013, Tortora and Derrickson
gallstones. 2013) (Box 1).
The main function of the digestive system
Authors is to take food and fluids in from the external
environment and to prepare nutrients, water and
Carolyn Johnstone, Lecturer in nursing, School of Nursing electrolytes into components that can be taken into
and Midwifery, University of Dundee, Dundee, Scotland. the internal environment of the body (Sherwood
Charles Hendry, Retired, was senior lecturer, School of Nursing 2013), therefore providing raw materials and
and Midwifery, University of Dundee. energy sources for cell activity. The digestive
Alistair Farley, Retired, was lecturer in nursing, School of Nursing system is complex because it carries out many
and Midwifery, University of Dundee. functions to ensure food is available in a form
Ella McLafferty, Retired, was senior lecturer, School of Nursing that allows cells to use it.
and Midwifery, University of Dundee.
Correspondence to: c.c.johnstone@dundee.ac.uk
Layers of the gastrointestinal system
Keywords The gastrointestinal system has many specific
Crohns disease, digestive system and disorders, gastrointestinal functions; however, the gastrointestinal tract has
tract, large intestine, small intestine, ulcerative colitis four main layers (Figure 2) including:
Mucosa or mucous membrane (innermost layer).
Review Submucosa.
Muscularis externa (muscle layer).
All articles are subject to external double-blind peer review and Serosa (outermost layer).
checked for plagiarism using automated software. The mucosa is made up of three layers. The
innermost layer of the mucosa is epithelium,
Online which acts as a protective surface against scratches
Guidelines on writing for publication are available at and grazes, for example in the mouth and
www.nursing-standard.co.uk. For related articles visit the archive oesophagus. It is also adapted in other parts of the
and search using the keywords above. gastrointestinal tract, for example in the stomach
and small intestine, for secretion and absorption
(Waugh and Grant 2010). The second layer is the
NURSING STANDARD / RCN PUBLISHING february 12 :: vol 28 no 24 :: 2014 37
Art & science life sciences: 16
lamina propria that supports the epithelium and BOX 1
is a layer of connective tissue containing lymphoid
Components of the digestive system
tissue that protects the gut from intestinal bacteria
(Tortora and Derrickson 2013). The outermost Major components:
layer of the mucosa, the muscularis mucosa, is a Mouth.
thin smooth muscle layer. Pharynx.
Oesophagus.
The submucosa is a thick layer of connective
Stomach.
tissue that contains nerves, blood vessels and
Small intestine.
glands (Seeley et al 2007). This layer enables the Large intestine.
gastrointestinal tract to stretch to accommodate Rectum and anal canal.
food passing through it (Sherwood 2013). The Accessory organs:
nerves form plexuses controlled by the autonomic Teeth.
nervous system, and these networks of nerves are Tongue.
important for the control of secretions of the Three major pairs of salivary glands.
organs of the gastrointestinal tract (Tortora and Liver.
Derrickson 2013). Pancreas.
Gall bladder.
The muscularis externa is usually made up of
(Waugh and Grant 2010)
two layers of smooth muscle, an inner circular
layer and an outer longitudinal layer. The muscles
work together to produce propulsive and mixing The serosa is an outer layer of connective tissue
movements (Sherwood 2013). Movement and the that covers the digestive organs and prevents
production of secretions in the gastrointestinal friction between them by discharging a thin
tract are under the control of the autonomic serous fluid during peristaltic movement. The
nervous system through the myenteric plexus serosa is also called the visceral peritoneum and
found between the muscle layers (Tortora and covers the organs in the abdominal cavity, while
Derrickson 2009a). the parietal peritoneum lines the abdominal
wall (Tortora and Derrickson 2013). Within the
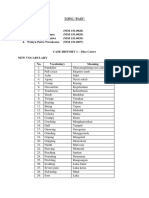
FIGURE 1 folds of the peritoneum, blood vessels, lymphatic
vessels and nerves supply the abdominal organs
Organs of the digestive system
(Tortora and Derrickson 2013). The omentum,
a fold of peritoneum that is described as a fatty
apron hanging over the abdominal organs
(Waugh and Grant 2010), contains many lymph
nodes that protect the gastrointestinal tract from
Soft palate
Hard palate infections and prevent them from spreading
Oropharynx outside the gastrointestinal tract (Tortora and
Tongue
Laryngopharynx Derrickson 2013). Throughout much of the
Larynx gastrointestinal tract, the serosa is continuous
Oesophagus with the mesentery, a double fold of peritoneum
that suspends the digestive organs from the inner
Diaphragm walls of the abdominal cavity (Sherwood 2013).
Stomach
Mouth
Pancreas The mouth or oral cavity consists of a roof, a floor
Liver
(behind stomach) and walls. The lips at the opening of the mouth
Gall bladder guide and keep food in the mouth (Sherwood
Transverse colon
2013). The tongue is composed of skeletal muscle
Duodenum Small intestine covered with mucous membrane and is attached
to the floor of the mouth by the frenulum. It
Ascending colon Descending colon
guides food during mastication, forming of
Sigmoid colon the bolus or small ball of food and swallowing
Caecum
Anus (deglutition), and is also important for taste and
speech. The tongue is covered by protrusions
Appendix
PETER LAMB
called papillae, some of which contain taste
Rectum
buds that when stimulated, create an enjoyable
subjective feeling of taste (Tortora and Derrickson
38 february 12 :: vol 28 no 24 :: 2014 NURSING STANDARD / RCN PUBLISHING
2013). The taste buds also stimulate the 99.5% water and 0.5% electrolytes and proteins
production of secretions from the salivary glands, (Tortora and Derrickson 2009b, Sherwood 2013).
stomach, pancreas and gall bladder in preparation Salivation, the process of producing saliva from
for the arrival of food in the digestive system the salivary glands, is controlled by the autonomic
(Sherwood 2013). The roof of the mouth contains nervous system (Tortora and Derrickson 2009b).
the hard and soft palates. Sections of the palatine Saliva has the following functions:
and maxillary bones of the skull form the hard It contains the enzyme salivary amylase that
palate, while the soft palate comprises muscle begins the process of carbohydrate digestion
lined with mucous membrane and is found at the in the mouth (Sherwood 2013). According to
back of the mouth (Thibodeau and Patton 2008). Tortora and Derrickson (2009b), this process
Originating from the free edge of the soft palate continues for approximately one hour until the
is the uvula, a conical muscular process. This gastric acids inactivate salivary amylase.
protects the nasopharynx during swallowing. It contains the enzyme lysozyme, which has
In the adult mouth, there are 32 permanent an antibacterial action and destroys bacteria in
teeth consisting of incisors, canines, premolars the mouth.
and molars. The incisors are chisel shaped and It washes away material that may act as a food
designed to cut into food. The canines have a source for bacteria and helps to keep the mouth
pointed surface and are designed to tear and shred and teeth clean.
food, while the premolars and molars are designed The thick mucus present in saliva aids
to crush and grind food. The molars can apply a swallowing by moistening and lubricating
crushing force of 200lb (Sherwood 2013). A bolus particles of food and decreasing friction as the
of food is created once food has been chewed. particles move through the oesophagus.
There are three major pairs of salivary glands Bicarbonate buffers in saliva neutralise acids
that release saliva into the oral cavity. The parotid in food so that dental caries are prevented
glands are the largest salivary glands and are found (Sherwood 2013).
in front of and under each ear. The submandibular
glands are located in the floor of the mouth and
the sublingual glands are located in the floor of Pharynx
the mouth in front of the submandibular glands The pharynx is formed of muscle and lined with a
(Waugh and Grant 2010). Approximately 1L of mucous membrane (Seeley et al 2007). The tonsils
saliva is produced daily by the salivary glands in the pharynx are made up of lymphoid tissue,
(Thibodeau and Patton 2008), consisting of which protect the body from infection (Sherwood
FIGURE 2
Layers of the gastrointestinal tract
Duct of gland outside the gastrointestinal Submucosa
tract (such as pancreas)
Lumen Gland
Mucosa-associated
lymphatic tissue
Submucosal plexus
Glands in submucosa
(plexus of Meissner)
Mucosa: Nerve
Epithelium
Lamina propria
Muscularis mucosae Artery
Muscularis: Vein
Circular muscle
Longitudinal muscle
Mesentery
Myenteric plexus
Serosa:
PETER LAMB
(plexus of Auerbach)
Areolar connective tissue
Epithelium
NURSING STANDARD / RCN PUBLISHING february 12 :: vol 28 no 24 :: 2014 39
Art & science life sciences: 16
2013). The pharynx consists of the nasopharynx, and is a passageway for food. At each end of the
oropharynx and laryngopharynx (Waugh and oesophagus there is a sphincter. At the pharyngeal
Grant 2010). end, the upper oesophageal sphincter is closed
The nasopharynx is essential in respiration; except while swallowing to avoid air passing into
however, the oropharynx and laryngopharynx are the oesophagus. The closed sphincter prevents
shared by the respiratory and digestive systems. the aspiration of food from the oesophagus into
Air enters the pharynx on its way to the lungs, the lungs. At the lower end of the oesophagus at
while food travels through the pharynx on its way the entrance into the stomach is the cardiac or
to the stomach. The bolus of food is voluntarily lower oesophageal sphincter that is closed except
moved from the mouth to the oropharynx by during swallowing. It inhibits food contents that
swallowing (Figure 3). Receptors in the pharynx are acidic from refluxing from the stomach into
act in response to the pressure from the bolus the oesophagus (Waugh and Grant 2010). The
by sending impulses to the swallowing centre oesophagus also has an upwards curve as it goes
in the medulla oblongata of the brain stem. The through the diaphragm, preventing food going
swallowing centre acts so that the soft palate rises back into the oesophagus once it has entered the
up to block the nasopharynx, stopping food and stomach (Waugh and Grant 2010). Mucus secreted
fluid from entering it, and the epiglottis moves from the mucosa of the oesophagus lubricates and
upwards and forwards so that the opening of the assists the movement of food (Seeley et al 2007).
larynx is closed and the bolus passes over it and on Food is moved through the oesophagus on a
into the laryngopharynx and then the oesophagus peristaltic wave started by the swallowing centre in
(Watson 2005). When the bolus enters the the medulla oblongata so that the bolus is pushed
pharynx, swallowing is under involuntary control from the top to bottom of the oesophagus towards
(Waugh and Grant 2010). The oropharyngeal the stomach. The lower oesophageal sphincter
stage of swallowing only lasts for approximately relaxes allowing the food to pass into the stomach.
one second while the bolus moves from the
oropharynx to the oesophagus (Sherwood 2013).
Stomach
The stomach, which is J-shaped, lies under the
Oesophagus diaphragm in the upper part of the abdominal
The oesophagus is a muscular tube, about 25cm cavity. It is divided into three parts: the fundus,
long with a diameter of 2cm, which starts at which lies near the lower oesophageal sphincter;
the laryngopharynx and ends at the stomach, the body, which is the middle part; and the
FIGURE 3
Swallowing
Nasopharynx
Hard palate
Bolus
Soft palate
Tongue
Uvula
Oropharynx
Epiglottis
Laryngopharynx
Larynx
PETER LAMB
Oesophagus
a) Position of structures before swallowing b) During the pharyngeal stage of swallowing
40 february 12 :: vol 28 no 24 :: 2014 NURSING STANDARD / RCN PUBLISHING
antrum, which is the lower part containing the the sphincter so that it opens and small amounts of
pyloric sphincter that controls the amount of chyme are pushed through into the small intestine.
food leaving the stomach and entering the small An estimated 2L of gastric secretions are
intestine (Sherwood 2013). The stomach looks produced daily (Waugh and Grant 2010). There
small when empty, with the capacity increasing are three phases involved in the regulation of
in response to ingesting a big meal. According gastric secretions: cephalic, gastric, and intestinal.
to Tortora and Derrickson (2009b), it can cope In the cephalic phase, the stomach is prepared
with up to 6.4L of food because of the presence for the intake of food stimulated by the sight,
of rugae or folds in the mucosa and submucosa of smell or taste of food. Gastric juices flow in
the stomach that flatten, enabling it to expand to response to stimulation of the vagus nerves in the
accommodate ingested food (Seeley et al 2007). parasympathetic pathways (Waugh and Grant
The experience of eating too much distends the 2010). Gastrin stimulates an increase in gastric
stomach, causing discomfort. The mucosal lining secretions (Seeley et al 2007), with salivary glands
of the stomach is formed from simple columnar also being stimulated causing excess salivation.
epithelium and contains many gastric pits, which The gastric phase is initiated by the presence of
are openings for the gastric glands. The gastric food in the stomach and at this time, most of the
glands under the surface of the mucosa are made gastric secretions are being mixed with food. Pepsin
up of specialised cells that secrete gastric juice into stimulates the production of additional gastrin,
the stomach and secrete water and mineral salts. and in turn additional gastric juices including
The specialised cells in the gastric glands include: hydrochloric acid (Seeley et al 2007). Once the pH
Goblet cells found on the inner surface of the in the pyloric antrum falls to about 1.5, gastrin
stomach, and lining the gastric glands, produce secretion ceases (Waugh and Grant 2010).
mucus to coat and protect the stomach lining The intestinal phase is responsible for stopping
from the effects of hydrochloric acid and pepsin. the production of gastric secretions and slowing
Parietal cells produce hydrochloric acid and the exit of chyme from the stomach thus preventing
intrinsic factor. Hydrochloric acid is responsible the duodenum from being overloaded (Tortora
for achieving a pH 2 within the stomach. The and Derrickson 2009b). The hormone secretin
pH in the stomach kills bacteria present in is released from the duodenal mucosa once the
ingested food. Intrinsic factor is required for the pH falls to 2 and stimulates the flow of alkaline
absorption of vitamin B12 in the small intestine pancreatic juice to neutralise the effects of the
and for the normal production of red blood acidic chyme. Cholecystokinin is released from the
cells. A shortage of intrinsic factor leads to intestinal glands when the chyme in the duodenum
pernicious anaemia. contains amino acids and fatty acids. It stimulates
G cells secrete the hormone gastrin, which is the release of pancreatic juice, causes the gall
involved in the regulation of gastric secretions bladder to contract and slows gastric emptying,
(Tortora and Derrickson 2009b). creating a feeling of fullness or satiety (Tortora and
Chief cells produce pepsinogen, the inactive Derrickson 2009a).
precursor of pepsin, an enzyme that digests
protein. Pepsin requires a pH 2 to work (Tortora
and Derrickson 2009a) and inactive pepsinogen Small intestine
is converted into the active pepsin by hydrochloric The small intestine is an estimated six metres long
acid. Pepsin breaks down polypeptide chains into and is divided into three parts: the duodenum,
smaller peptide fragments. which is attached to the pylorus and is 25cm long;
The muscle layer in the stomach differs from the jejunum, which is 2.5m long; and the ileum,
other muscle areas of the gastrointestinal tract. which is 3.5m long (Seeley et al 2008). The ileum
There are three layers of muscle in the stomach is attached to the large intestine at the ileocaecal
wall: the outer longitudinal, middle circular and sphincter (Waugh and Grant 2010). The small
inner oblique layers (Seeley et al 2007). This intestine has an important role in the absorption of
arrangement of muscles is important in digestion food, and the cells of the submucosa and mucosa
because they are responsible for the churning are designed to maximise absorption by increasing
action that takes place within the stomach. the surface area greatly through circular folds,
The contraction of these muscles mixes the food villi and microvilli (Seeley et al 2007). The circular
with gastric juice and assists in breaking down folds in the mucosa and submucosa promote
ingested food into chyme, which has a semi-solid mixing of chyme as it moves through the small
consistency. Peristaltic contractions of the intestine. The villi are about 0.5-1.5mm long and
stomach muscles also help to move food to the are finger-like projections on the mucosa. Each
pyloric sphincter, causing partial relaxation of villus contains a blood capillary network and
NURSING STANDARD / RCN PUBLISHING february 12 :: vol 28 no 24 :: 2014 41
Art & science life sciences: 16
a lacteal. Microvilli are hair-like projections of Between the ascending colon and the transverse
epithelial cells covering the villi. Microvilli produce colon there is a bend called the hepatic or right colic
digestive enzymes and absorb digested food. The flexure and between the transverse colon and the
products of carbohydrate and protein digestion descending colon there is another bend called the
from the gastrointestinal tract are absorbed into splenic or left colic flexure. The vermiform appendix
the blood capillaries from the microvilli (Tortora is found on the caecum and is a small tube that is
and Derrickson 2009b). The lacteals absorb closed at one end and contains the same layers as the
lipids from chyme. Also present in the intestinal rest of the colon, but more lymphoid tissue is present
epithelium are goblet cells that secrete mucus. (Waugh and Grant 2010).
Intestinal glands are situated at the base of Food residue enters the caecum from the ileum
the villi and secrete intestinal juice consisting of through the ileocaecal valve. The contents of the
mucus and water. The pH of the fluid is normally ileum enter through this valve, however they cannot
between 7.8 and 8.0 (Waugh and Grant 2010), and return into the ileum as the folds of tissue of this
these secretions help to protect the small intestine valve are forcibly closed when caecal contents try to
from the acidic effects of chyme and the activity move backwards (Sherwood 2013). This is a safety
of digestive enzymes. They also help to keep mechanism, preventing bacteria from the large
chyme in its liquid form to increase the likelihood intestine from entering the ileum. Once food matter
of digestion in the small intestine. The intestinal reaches the large intestine, it is no longer called
glands contain endocrine cells that secrete secretin chyme (Thibodeau and Patton 2008) and it takes on
and cholecystokinin. Groups of aggregated lymph the consistency and colour of faeces, as water and
nodules are found in the ileum called Peyers salts are absorbed.
patches and these protect the small intestine when There are 500 different species of bacteria found
microbes may be present (Seeley et al 2007). within the large intestine, and they are harmless to
When acidic chyme enters the small intestine, humans unless they are transferred to other parts
ducts in the middle third of the duodenum deliver of the body (Waugh and Grant 2010). The bacteria
pancreatic juice and bile from the liver. These cause the release of hydrogen, carbon dioxide and
and intestinal juice come into contact with the methane as a result of the bacterial fermentation of
contents of the small intestine and digestion of the unabsorbed nutrients, particularly carbohydrate.
nutrients is completed. The duodenal glands in the These gases form flatus in the large intestine
mucosa secrete alkaline mucus that helps with the (Tortora and Derrickson 2009b). Any proteins
neutralisation of the gastric acid in chyme (Tortora that are present are broken down into amino acids,
and Derrickson 2009b). and bilirubin is broken down into simple pigments
Stimulated by the presence of chyme, including stercobilin giving faeces a brown colour
segmentation contractions from smooth muscle (Tortora and Derrickson 2009b). Vitamin K is
in the intestinal wall move food along the small manufactured by bacteria in the large intestine,
intestine. Segmentation contractions occur when while B complex vitamins are also products of
contracted rings in the small intestine relax and the bacterial action. Once these vitamins have been
relaxed rings contract so that chyme is chopped produced in the large intestine, they are absorbed
and thoroughly mixed as it moves backwards into the bloodstream (Thibodeau and Patton 2008).
and forwards between the rings. Segmentation The contents of the large intestine take an
becomes more forceful after a meal (Sherwood estimated 18-24 hours to pass along its length
2013). As well as mixing chyme with digestive (Seeley et al 2007). Faecal matter is made up of
juices, segmentation ensures that as much of the water, cellulose fibre, microbes, epithelial cells lost
chyme as possible is in contact with the mucosa from the walls of the gastrointestinal tract, fatty
for absorption (Tortora and Derrickson 2009b). acids and mucus secreted from the epithelial lining
When the meal has been absorbed, peristaltic of the large intestine (Waugh and Grant 2010). It
contractions move the remains of the meal towards is important that faecal matter does not take too
the large intestine. long to travel through the large intestine because
increasing amounts of water will be absorbed the
longer the contents remain in the system resulting
Large intestine in constipation, whereas if bowel contents travel
The large intestine or colon is approximately 1.5m through too quickly, diarrhoea can occur because
long and continues from the end of the ileum to the less water is absorbed.
anus (Tortora and Derrickson 2009b). The large Arrangement of the muscle layers encourages
intestine is made up of the caecum, ascending colon, the movement of faecal contents through the
transverse colon, descending colon, sigmoid colon, large intestine. The outer longitudinal smooth
rectum and anal canal (Waugh and Grant 2010). muscle layer does not completely surround the
42 february 12 :: vol 28 no 24 :: 2014 NURSING STANDARD / RCN PUBLISHING
large intestine, but has three longitudinal bands There are two common symptoms. The first
of smooth muscle running the entire length of is heartburn, characterised by a burning pain
the intestine called taeniae coli. They stop at the behind the sternum that may radiate into the
junction between the sigmoid colon and the rectum jaw and around the ribs. The second symptom is
(Waugh and Grant 2010) and are shorter than the regurgitation or reflux of acid into the throat (Selby
underlying smooth muscle. Tonic contractions of 2010). Pain may occur before, during or after
the bands gather the colon into a series of pouches eating, and it may come in waves, may be constant
called haustra. During haustral churning, the walls and may worsen on lying down and cause nausea
contract and squeeze the contents into the next and vomiting.
haustrum; however, there is a significant increase GORD occurs when the acidic gastric contents
in movement of the large intestine after meals reflux into the oesophagus. Normally, the lower
(Tortora and Derrickson 2009b). Large areas of oesophageal sphincter is closed to the backflow
the transverse colon contract at the same time, of gastric contents, but the sphincter can weaken
propelling faeces along most of the length of the as a result of ageing, increased pressure from
large intestine and into the rectum within seconds. the stomach because of a high body mass index,
These contractions are called mass movements. and delay in stomach emptying caused by a high
The presence of faeces in the rectum causes fat diet(NHS Choices 2012b). Pain is caused
tension, leading to stimulation of stretch receptors by the reflux of gastric contents, which leads to
which trigger the defecation reflex (Seeley et al mucosal damage to the oesophagus as a result
2007). This reflex causes the internal anal of the acid nature of the stomach contents (Selby
sphincter to relax and the rectum and sigmoid 2010). Other symptoms may include hoarseness,
colon to contract forcibly. If the external anal chronic laryngitis, sore throat, feeling a lump in
sphincter also relaxes, then defecation takes place. the throat, asthma, chronic cough and dental
Defecation can be prevented because the external erosions (Sveen 2009). Dental erosions can occur
anal sphincter is made up of skeletal muscle and is when stomach contents reflux into the oral cavity.
under voluntary control (Tortora and Derrickson There seems to be a link between asthma and
2009b). Although distension of the rectum GORD, the exact reason for this is unknown,
produces the urge to defecate, if it is not but small amounts of stomach contents may be
appropriate at that time, the external sphincter can aspirated into the trachea causing inflammation
be voluntarily tightened so that defecation does not and inducing asthma (Sveen 2009).
take place until a more suitable time. During the Many people link their symptoms to overeating
process of defecation, the abdominal muscles and, therefore, they do not report their symptoms.
contract at the same time as a forcible expiration However, they may not sleep well and they
against a closed glottis, the Valsalva manoeuvre may avoid certain foods or activities that cause
occurs accompanying voluntary straining irritation or pain. Assessment of patients should
movements. This results in an increased intra- include a history of symptoms and other symptoms
abdominal pressure that helps to expel faeces should be checked for, including weight loss,
(Sherwood 2013). dysphagia, presence of any abnormal masses in the
abdomen, vomiting and iron deficiency anaemia,
because these are red flag symptoms requiring
Disorders of the digestive system further investigation (Fairclough and Silk 2009).
There are several disorders that may affect the There is no evidence to suggest that endoscopy
digestive system. This article focuses on is required if symptoms are benign although
gastro-oesophageal reflux disease and troublesome, and the National Institute for Health
inflammatory bowel disease. and Care Excellence (NICE) (2004) has produced
guidance on the need for endoscopy. This
Gastro-oesophageal reflux disease guidance is reinforced by a report for the Scottish
Gastro-oesophageal reflux disease is also known Intercollegiate Guidelines Network (SIGN) (2003).
as GORD or GERD, dyspepsia, indigestion and Management of patients with GORD includes a
heartburn (Stevens 2006). Many people in the review of medicines that can cause dyspepsia such
UK experience dyspepsia or reflux-like symptoms as non-steroidal anti-inflammatory drugs and
annually, but not all episodes will be reported to nitrates (NHS Choices 2012b). Advice should
a healthcare professional (NHS Choices 2012a). be given relating to lifestyle factors, including
GORD has been defined as a condition which adoption of healthy eating, weight reduction
develops when the reflux of stomach contents cause and smoking cessation. Drug therapy should
troublesome symptoms and/or complications include either a one or two-month supply of
(Richter 2007). a proton pump inhibitor (PPI) or testing for
NURSING STANDARD / RCN PUBLISHING february 12 :: vol 28 no 24 :: 2014 43
Art & science life sciences: 16
Helicobacter pylori and eradication therapy if it Low grade pyrexia.
is confirmed as being present (NICE 2004). PPIs Fever.
work by reducing the acidity produced in the Weight loss.
stomach (Wood 2011) and include omeprazole Loss of energy.
and esomeprazole. SIGN (2003) recommends Up to ten bloody diarrhoea episodes daily
non-invasive faecal antigen testing to identify (Pullen and Julian 2012).
the presence of H. pylori and if present, this can Development of a tender mass in the
be managed by a one-week course of a PPI and lower abdomen.
an antibiotic such as metronidazole. Antacids, Cramping in the right lower quadrant especially
alginates and anti-secretory medications may after a meal (Dettinger et al 2008).
also be useful (NHS Choices 2012b), and advice Diagnosis is confirmed by history, physical
should be provided on the avoidance of triggers. examination, endoscopy, colonoscopy, and
haematological, radiological and histological
Inflammatory bowel disease findings.
The two forms of inflammatory bowel disease are
Crohns disease and ulcerative colitis. The underlying Ulcerative colitis Ulcerative colitis affects the
cause of these conditions is unknown, but evidence mucosa of the large intestine only and is limited
suggests that inflammation is caused by bacteria to the colon and rectum, with continuous
(Pullen and Julian 2012). The risk factors for the inflammation. The colon is red and oedematous
disease include: and ulcers form on the mucosal lining, bleeding
Having a family history of inflammatory occurs and the lining becomes thickened,
bowel disease. causing narrowing of the lumen of the intestine
Age any age group can be affected by and shortening of the large intestine (Pullen and
inflammatory bowel disease, but there is an Julian 2012). The intestine can perforate and
increased risk between the ages of 15-35 abscesses can form, and these changes can
(Dettinger et al 2008) and 50-70 years influence the elasticity of the intestine and its
(Boirivant and Cossu 2012). absorption of water and nutrients. The signs
Urban areas the prevalence is higher than in and symptoms of ulcerative colitis include
rural areas (Dettinger et al 2008). (Boirivant and Cossu 2012):
Lifestyle and environmental factors, including Abdominal pain that is relieved with bowel
diet and exposure to industrial chemicals. movements.
Smoking has been linked to the development Bloody diarrhoea and rectal bleeding.
of Crohns disease (Pullen and Julian 2012). Passage of mucus or pus or both.
Although patients with Crohns disease and Rectal urgency.
ulcerative colitis follow a pattern of exacerbations Weight loss and fatigue.
and remissions (Bodger 2011), the effects on the Diagnosis is confirmed by history, endoscopy,
intestinal wall and, therefore, the presentation and barium enema and negative stool sample
management are different. for infections.
Nursing management of Crohns disease and
Crohns disease Crohns disease can arise anywhere ulcerative colitis Common to both conditions
along the gastrointestinal tract. However, it most is the need to carry out an assessment of the
commonly affects the terminal ileum. The lining frequency of bowel movements, overall nutritional
of the intestine develops ulcers, which is then and hydration status, and any signs of infection.
replaced with scar tissue, causing the wall of the Conservative management includes teaching
intestine to thicken and develop into fibrous tissue patients about appropriate dietary choices,
and causing a narrowing of the intestine lumen. adhering to drug regimens and ensuring they
The intestine becomes oedematous and skip lesions replace any fluid losses. If the patient requires
(Dettinger et al 2008), abscesses and fistulae may surgery, the nurse should provide emotional
form. These problems can lead to a bowel support to enable the individual to deal with any
perforation or obstruction as the lumen narrows changes to body image.
if left untreated. As a result of the damage to the Drug therapy aims to reduce inflammation
walls of the intestine, the ability of the intestine and provide symptom relief. The drugs used to
to absorb nutrients and fluids may be affected, treat Crohns disease and ulcerative colitis have
leading to malnutrition and weight loss (Pullen a number of different actions and include:
and Julian 2012). The signs and symptoms Aminosalicylates these are anti-inflammatory
of Crohns disease are dependent on where the drugs that act on the digestive system.
disease occurs and include: Mesalazine is used as a first-line treatment.
44 february 12 :: vol 28 no 24 :: 2014 NURSING STANDARD / RCN PUBLISHING
If mesalazine is not successful, a course of Conclusion
corticosteroids can be used in place of or along This article introduces the reader to the anatomy
with mesalazine, although corticosteroids and physiology of the digestive system, an
should not be administered for more than three understanding of which is essential to assisting
months because of their potential side effects patients with eating and drinking. Disorders of the
such as weight gain (Dettinger et al 2008), and digestive system are common and nurses in every
their ability to suppress the immune system. sphere of practice will encounter patients with
Immune modifiers, such as azathioprine, can be these conditions. By understanding the normal
used to reduce inflammation by suppressing the structure and function of the digestive system
immune response. the nurse is better able to respond to patients
Antibiotics, such as metronidazole, may be experiencing digestive dysfunction NS
necessary if there are any signs of infection
related to fistulae, abscesses or medications
that cause immunosuppression (Pullen and POINTS FOR PRACTICE
Julian 2012). In your area of clinical practice, reflect on how the activities of eating
Biological modifiers, such as infliximab, can be and drinking might impinge on a patients overall wellbeing?
used to induce remission of the condition. How can bacteria from the large intestine be transferred to other parts of
If conservative therapy is unsuccessful and/ the body? What advice should patients be given to prevent such transfer?
or there are complications, surgery may be What are the side effects of long-term use of corticosteroids?
necessary. In patients with ulcerative colitis, a
total colectomy is required and this will cure the
disease. Crohns disease is incurable, therefore GLOSSARY
the goals of surgery are to manage symptoms and Enzymes
decrease complications. Bowel surgery consists of Specialised protein molecules that act as catalysts. Catalysts speed up
the removal of the affected area and rejoining the specific chemical reactions without being changed or consumed during
the reaction process.
bowel. A temporary or permanent ileostomy may
Fistula
be performed, and patients need to be aware of
A passageway between two organs that do not normally connect.
watery stools, managing their ileostomy, replacing Plexus
fluids, and monitoring fluid intake and output A complex network of nerves.
(Dettinger et al 2008).
References
Bodger K (2011) Cost NHS Choices (2012a) Indigestion. Seeley RR, Stephens TD, Tate P (2008) International Student Version.
effectiveness of treatments tinyurl.com/9ua7z4n (Last Anatomy and Physiology. Eighth John Wiley and Sons, Hoboken NJ.
for inflammatory bowel disease. accessed: January 24 2014.) edition. McGraw Hill, Boston MA.
PharmacoEconomics. 29, 5, Tortora GJ, Derrickson BH
387-401. NHS Choices (2012b) Heartburn Selby M (2010) GORD and (2009b) Principles of Anatomy and
and Gastro-oesophageal Reflux dyspepsia. Practice Nurse. Physiology. Volume 2. Maintenance
Boirivant M, Cossu A (2012) Disease. tinyurl.com/o5nz23y 39, 9, 19-22. and Continuity of the Human Body.
Inflammatory bowel disease. (Last accessed: January 24 2014. 12th edition. John Wiley and Sons,
Oral Diseases. 18, 1, 1-15. Sherwood L (2013) Introduction Hoboken NJ.
Pullen RL, Julian MK (2012) Caring to Human Physiology. Eighth
Dettinger M, Matzke M, McKay K, for a patient with inflammatory edition. Brooks/Cole, Pacific Tortora GJ, Derrickson BH
Sizer R, Thoreson M, Wrobleski D bowel disease. Nursing Made Grove CA. (2013) Essentials of Anatomy
(2008) Crohns Disease and Incredibly Easy! 10, 4, 36-45. and Physiology. Ninth edition
ulcerative colitis. Journal of Stevens R (2006) Indigestion and International Student Version. John
Continuing Education in Nursing. Richter JE (2007) Heartburn. Update. 72, 3, 23-30. Wiley and Sons, Hoboken NJ.
39, 4, 151-152. Gastrooesophageal reflux
disease. Best Practice & Research: Sveen S (2009) Symptom check: Watson R (2005) Anatomy and
Fairclough PD, Silk BA (2009) Clinical Gastroenterology. 21, 4, is it GERD? Journal of Continuing Physiology for Nurses. 12th edition.
Gastro-intestinal disease. In Kumar P, 609-631. Education in Nursing. 40, 3, Elsevier, London.
Clark M (Eds) Kumar and Clarks 103-104.
Clinical Medicine. Seventh edition. Scottish Intercollegiate Guidelines Waugh A, Grant A (2010) Ross and
Saunders Elsevier, Edinburgh, Network (2003) Dyspepsia: A Thibodeau GA, Patton KT (2008) Wilson Anatomy and Physiology
241-318. National Clinical Guideline. No. 68. Structure & Function of the Body. in Health and Ilness. 11th edition.
SIGN, Edinburgh. 13th edition. Elsevier Mosby, Churchill Livingstone Elsevier,
National Institute for Health and St. Louis MO. Edinburgh.
Care Excellence (2004) Dyspepsia: Seeley RR, Stephens TD, Tate P
Managing Dyspepsia in Adults in (2007) Essentials of Anatomy and Tortora GJ, Derrickson BH Wood S (2011) Indigestion and
Primary Care. Clinical guideline Physiology. Sixth edition. McGraw (2009a) Essentials of Anatomy heartburn. Practice Nurse. 41, 15,
No. 17. NICE, London. Hill, Boston MA. and Physiology. Eighth edition 14-19.
NURSING STANDARD / RCN PUBLISHING february 12 :: vol 28 no 24 :: 2014 45
S-ar putea să vă placă și
- Diabetic Foot Care Behaviors: A Literature Review: Titis Kurniawan, Imas Rafiyah, Ardia Putra, Yanuar PrimandaDocument7 paginiDiabetic Foot Care Behaviors: A Literature Review: Titis Kurniawan, Imas Rafiyah, Ardia Putra, Yanuar Primandanadya wahyuÎncă nu există evaluări
- Efn GroupDocument1 paginăEfn Groupnadya wahyuÎncă nu există evaluări
- Nursing CommunicationDocument5 paginiNursing Communicationnadya wahyuÎncă nu există evaluări
- Safety and Preventing Accident: Providing General Giving Information Offering Self Giving InformationDocument3 paginiSafety and Preventing Accident: Providing General Giving Information Offering Self Giving Informationnadya wahyuÎncă nu există evaluări
- Personal Care-Cleansing and Dressing, Skin Care Case History-Mrs. Mcbride New Vocabulary and Difficult WordsDocument4 paginiPersonal Care-Cleansing and Dressing, Skin Care Case History-Mrs. Mcbride New Vocabulary and Difficult Wordsnadya wahyuÎncă nu există evaluări
- Topic PainDocument3 paginiTopic Painnadya wahyuÎncă nu există evaluări
- Wheel Chair Makes People Lazy and Not Trying Can Not Be Independent The Price of Cane Is Also Relatively Cheaper Than The Wheel ChairDocument1 paginăWheel Chair Makes People Lazy and Not Trying Can Not Be Independent The Price of Cane Is Also Relatively Cheaper Than The Wheel Chairnadya wahyuÎncă nu există evaluări
- Group 1 Group 2 Group 3Document2 paginiGroup 1 Group 2 Group 3nadya wahyuÎncă nu există evaluări
- Mencari "VOCABULARY" Yang Sulit Dan Di "TERJEMAHKAN" 2. Menentukan Kalimat "THERAPEUTIC COMMUNICATION TECHNIQUES"Document1 paginăMencari "VOCABULARY" Yang Sulit Dan Di "TERJEMAHKAN" 2. Menentukan Kalimat "THERAPEUTIC COMMUNICATION TECHNIQUES"nadya wahyuÎncă nu există evaluări
- Breathing Problems (Difficult Words)Document2 paginiBreathing Problems (Difficult Words)nadya wahyuÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- SalivaDocument84 paginiSalivaVidya SenthuÎncă nu există evaluări
- 518901689-Chemistry-Project-Class-XII-2021-22-Investigatory-Project AKDocument25 pagini518901689-Chemistry-Project-Class-XII-2021-22-Investigatory-Project AKayushkumar2945100% (2)
- Lab Report 12 Salivary AmylaseDocument5 paginiLab Report 12 Salivary Amylase3amabelle arevaloÎncă nu există evaluări
- Thi Thu Chuyen Nguyen Hue 357Document6 paginiThi Thu Chuyen Nguyen Hue 357Quang Nam HaÎncă nu există evaluări
- MCQ RRB NTPC Biology PDFDocument3 paginiMCQ RRB NTPC Biology PDFSiddharth PradhanÎncă nu există evaluări
- Dr. Smriti Gupta - ThesisDocument195 paginiDr. Smriti Gupta - ThesisKritika KejriwalÎncă nu există evaluări
- Explanation Text 2Document26 paginiExplanation Text 2Neltan Tibepril Tusev DuhaÎncă nu există evaluări
- Pharmacotherapy Casa Patient Focused Approach 10Th Edition Full ChapterDocument41 paginiPharmacotherapy Casa Patient Focused Approach 10Th Edition Full Chaptermuriel.moreno949100% (29)
- Beta Glucan For Children American Journal of Immunology 2013Document5 paginiBeta Glucan For Children American Journal of Immunology 2013MariaMaria2014Încă nu există evaluări
- Nto Uchenna Note On GI SecretionsDocument10 paginiNto Uchenna Note On GI SecretionsNwaoha Chibuzor AnthonyÎncă nu există evaluări
- Full Experiment Digestion Starch in HumanDocument10 paginiFull Experiment Digestion Starch in Humanfatin nadiaÎncă nu există evaluări
- Gastrointestinal PhysiologyDocument134 paginiGastrointestinal Physiologyapi-19916399100% (1)
- Salivary SecretionDocument23 paginiSalivary SecretionSamridhi SinghÎncă nu există evaluări
- Salivary Gland DisordersDocument241 paginiSalivary Gland DisordersDRPRIYA007Încă nu există evaluări
- Koa's Horticulture GuideDocument8 paginiKoa's Horticulture GuidePedro Santos CardosoÎncă nu există evaluări
- Dario Fo - La Storia Di Una Tigre - The TALE of A TIGER - Translated by Ed EmeryDocument22 paginiDario Fo - La Storia Di Una Tigre - The TALE of A TIGER - Translated by Ed EmeryAruna Premarathne100% (1)
- Ebf 303 Environmental and Animal PhysiologyDocument61 paginiEbf 303 Environmental and Animal PhysiologyAngela BrownÎncă nu există evaluări
- Artificial Saliva For Therapeutic Management of Xerostomia: A Structured ReviewDocument5 paginiArtificial Saliva For Therapeutic Management of Xerostomia: A Structured ReviewAlexander KevinÎncă nu există evaluări
- Comparative Human Salivary and Plasma Proteomes: Critical Reviews in Oral Biology & MedicineDocument8 paginiComparative Human Salivary and Plasma Proteomes: Critical Reviews in Oral Biology & MedicinerenattoÎncă nu există evaluări
- Chemistry ProjectDocument11 paginiChemistry ProjectSwarnabha BhattacharyyaÎncă nu există evaluări
- 10 1016@j Archoralbio 2019 104593 PDFDocument3 pagini10 1016@j Archoralbio 2019 104593 PDFSaeful RamadonÎncă nu există evaluări
- Salivary Gland Anat and Phys FinalDocument19 paginiSalivary Gland Anat and Phys FinalAteeq KhanÎncă nu există evaluări
- Oral Biologic Defenses in Tooth Demineralization and RemineralizationDocument14 paginiOral Biologic Defenses in Tooth Demineralization and RemineralizationWilson Fransiskus Chia GirsangÎncă nu există evaluări
- Proctor GB - The Physiology of Salivary Secretion. Periodontologi 200. 2016 Vol 70 11-25 PDFDocument15 paginiProctor GB - The Physiology of Salivary Secretion. Periodontologi 200. 2016 Vol 70 11-25 PDFyolandapmaÎncă nu există evaluări
- Sains Dalam Air Liur ManusiaDocument11 paginiSains Dalam Air Liur ManusiaacehhfzhÎncă nu există evaluări
- Sialometria ClinicaDocument4 paginiSialometria ClinicaDr. JharÎncă nu există evaluări
- Critical Review of Dietetics in AyurvedaDocument14 paginiCritical Review of Dietetics in AyurvedakavalapparaÎncă nu există evaluări
- Git Lec 1Document8 paginiGit Lec 1Kim Sa-buÎncă nu există evaluări
- The Functions of Human Saliva - A ReviewDocument12 paginiThe Functions of Human Saliva - A ReviewRaúl Ernesto Quispe CórdovaÎncă nu există evaluări
- Defence Mechanism of Gingiva PerioDocument58 paginiDefence Mechanism of Gingiva PerioFourthMolar.com100% (1)