Documente Academic
Documente Profesional
Documente Cultură
Pcap - Pathophysiology
Încărcat de
Ayla MarTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Pcap - Pathophysiology
Încărcat de
Ayla MarDrepturi de autor:
Formate disponibile
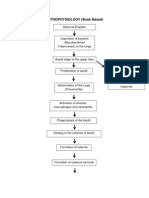
PATHOPHYSIOLOGY
WRITTEN
Pediatric Community Acquired Pneumonia (CAP) is most commonly caused by
aspiration or inhalation of microorganisms (Streptococcus pneumoniae) through the
nasopharynx or oropharynx. Due to failure of primary defense, a microorganism invades
the lower respiratory tract wherein there is a release of antibodies by the activation of B-
cell. Antigen- antibodies have 2 reactions which its complex adheres to the mucosal
lining of the lower respiratory tract and initiation in the immune system. When antibody
adheres to the mucosal lining of lower respiratory tract, it irritates the mucosa that
increases the mucus production and it accumulates the mucus which causes a
productive cough.
In initiation of the immune system, there will be a vasodilation and increased
blood flow leads to vaso-congestion that increases the hydrostatic pressure of the
plasma and capillary permeability. When this happens, there will be an escape of
plasma which causes edema, escape of RBC, Serum and fibrin which forms exudates,
and a transportation of the phagocyting cells. Edema and Exudate formation may
initiate a narrowing of airway and filling of the bronchi and alveoli. Narrowed airway
causes use of accessory muscles and increased respiration where asymmetrical chest
expansion noted. Accumulation of exudates can lead to consolidation and decreased
lung inflation.
Transportation of phagocyting cells may manifest a fever or hyperthermia. The
phagocytes will engulf the antigen and infects a cell. When the cell was being infected, it
will be detected by the T-cell and destroy the antigen. This T-cell is an effector cell that
was strengthens by the regulatory T-cell. The effector and regulatory cell will synthesize
and release a cytokines. There will be altered temperature maintenance in the
hypothalamus that causes a fever.
To be able to treat Pneumonia, vaccination is the primary mode of prevention,
antibiotics are essential, vasodilators. Other medications and oxygen must be readily
given to the patient to easily ease his/her complication. If left untreated, pneumonic
consolidation, septicemia, empyema, lung abscess and pleural effusion may occur
within the lungs; and in rare cases, respiratory failure, and hypoxia and soon, death may
occur if becomes severe.
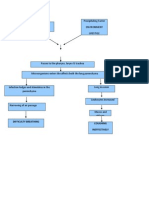
DIAGRAM
Precipitating factors:
Predisposing factor:
- Environment
- Age
- Previous diagnosis of
Respiratory Infections
- Immuno-compromised
Inhalation of Microorganism
Failure of Defense
Invasion of the Lower
Respiratory Tract
Activation of B-cells
Release of Antibodies
Antigen-Antibody Reaction
Antigen Antibody Complex Initiation of Immune system
adheres to the mucosal lining
of the lower respiratory tract
Vasodilation and increased blood
flow
Mucosal irritation
Vaso-congestion
Increase Mucus production
Increase plasma Hydrostatic Pressure
Accumulation of mucus Increase capillary permeability
Productive Cough
Escape of Plasma Escape of RBC, Serum Transportation of
and Fibrin phagocyting cells
Edema
Exudate formation Engulfing the Antigen
Narrowing of airways
Filling of Bronchi and Cell becomes infected
Alveoli
Use of accessory
muscles Detection of the
Consolidation of lung infected cell by the
T-cells
Increased Respiration
Decreased lung
inflation Effector T-cells
Asymmetrical chest destroys antigen
expansion
Regulatory T-cell
strengthen act of
effector cell
Altered Temperature Effector and
Regulating Regulatory cells
Fever
maintenance in the synthesize and
Hypothalamus release cytokines
Vaccination is the primary mode of Immune system will weaken
prevention
Pneumonic consolidation,
Antibiotics, vasodilators and other septicemia, empyema, lung
medications must be given to the
abscess and pleural effusion may
patient immediately.
occur within the lungs.
Oxygen would be given to assist
in breathing. Respiratory failure, hypoxia and
soon, death may occur if it
becomes severe.
S-ar putea să vă placă și
- HMO Proposal For Individual F-1Document10 paginiHMO Proposal For Individual F-1DesÎncă nu există evaluări
- DSM 5 Mood DisorderDocument9 paginiDSM 5 Mood DisorderErlin IrawatiÎncă nu există evaluări
- 1.pathophysiology of MeningitisDocument1 pagină1.pathophysiology of Meningitisshielamaygo05100% (1)
- Acute Medicine (Medical Masterclass)Document163 paginiAcute Medicine (Medical Masterclass)Chris Jardine Li100% (1)
- Final Case Study PCAPDocument71 paginiFinal Case Study PCAPGabriel Lorenz S. ParongÎncă nu există evaluări
- Pathophysiology of Pediatric Community Acquired PneumoniaDocument2 paginiPathophysiology of Pediatric Community Acquired PneumoniaKeij AranetaÎncă nu există evaluări
- Patho PneumoniaDocument2 paginiPatho Pneumoniaailyne_galicia100% (2)
- PCAP Pediatric Community Acquired Pneumonia PATHOPHYSIOLOGYDocument2 paginiPCAP Pediatric Community Acquired Pneumonia PATHOPHYSIOLOGYCHRISTIE MONTANO0% (3)
- Pcap PathophysiologyDocument3 paginiPcap PathophysiologyZandra Lyn AlundayÎncă nu există evaluări
- Community-Acquired Pneumonia PathophysiologyDocument2 paginiCommunity-Acquired Pneumonia PathophysiologyFrancis Adrian83% (12)
- UMTC PCAP - C Case StudyDocument17 paginiUMTC PCAP - C Case StudyMary Ann Credo Manlangit100% (2)
- General Surgery Board Exam QuestionsDocument6 paginiGeneral Surgery Board Exam Questionschristinejoan100% (1)
- CASE STUDY: Bronchial Asthma in Acute Exacerbation: EtiologyDocument35 paginiCASE STUDY: Bronchial Asthma in Acute Exacerbation: EtiologyMishiel Castillo100% (1)
- Pathophysiology of Neonatal Sepsis Secondary To Neonatal PneumoniaDocument4 paginiPathophysiology of Neonatal Sepsis Secondary To Neonatal Pneumoniapaul andrew laranjo asuncion80% (5)
- Community Acquired Pneumonia, A Case StudyDocument26 paginiCommunity Acquired Pneumonia, A Case StudyMenggay SanDiego57% (7)
- Pathophysiology PneumoniaDocument2 paginiPathophysiology PneumoniaSheila Mae Escalante67% (3)
- Curriculum Vitae: Dr. Muh - Ilyas, SP - PD, KP, SP.P (K), FINASIMDocument51 paginiCurriculum Vitae: Dr. Muh - Ilyas, SP - PD, KP, SP.P (K), FINASIMMuhammad ZakkiÎncă nu există evaluări
- PCAP-c Group A NiggasDocument39 paginiPCAP-c Group A NiggasJenny YenÎncă nu există evaluări
- Pathophysiology Dengue 2Document4 paginiPathophysiology Dengue 2KatherineÎncă nu există evaluări
- Community Acquired Pneumonia PathophysiologyDocument3 paginiCommunity Acquired Pneumonia Pathophysiologyjordan aguilar67% (3)
- Multiple Organ Dysfunction Syndrome: HistoryDocument6 paginiMultiple Organ Dysfunction Syndrome: HistoryJasmine BaduaÎncă nu există evaluări
- A Case of PCAP-C (Individual INP)Document44 paginiA Case of PCAP-C (Individual INP)Preiane PayladoÎncă nu există evaluări
- Bronchial Asthma in Acute Exacerbation BAIAE Pathophysiology Schematic DiagramDocument3 paginiBronchial Asthma in Acute Exacerbation BAIAE Pathophysiology Schematic DiagramVictor Angelo VeraÎncă nu există evaluări
- Pathophysiology of TuberculosisDocument3 paginiPathophysiology of TuberculosisMonica Marie Morales86% (14)
- Pathophysiology Community Aquired Pneumonia and AnemiaDocument3 paginiPathophysiology Community Aquired Pneumonia and Anemiapa3kmedina100% (2)
- Munity Acquired Pneumonia PathoDocument1 paginăMunity Acquired Pneumonia PathoJohanna Elaine Tandoc100% (1)
- Pathophysiology of PneumoniaDocument2 paginiPathophysiology of PneumoniaJeffrey Ramos100% (1)
- Pathophysiology Copd-ChfDocument2 paginiPathophysiology Copd-ChfZaira Batalo100% (2)
- Pathophysiology of PneumoniaDocument2 paginiPathophysiology of PneumoniaMaria Cristina100% (1)
- Pcap PathoDocument2 paginiPcap PathoDiana Jean Abad Dacumos69% (13)
- CS5 (AGE) Acute Gastroenteritis NCPDocument2 paginiCS5 (AGE) Acute Gastroenteritis NCPAudrie Allyson GabalesÎncă nu există evaluări
- IX: Pathophysiology: Predisposing Factor Precipitating FactorsDocument2 paginiIX: Pathophysiology: Predisposing Factor Precipitating FactorsCandace AlcarazÎncă nu există evaluări
- Pathophysiology and Concept Map Guide: Pneumoniae, Chlamydia Pneumoniae and Staphylococcus AureusDocument2 paginiPathophysiology and Concept Map Guide: Pneumoniae, Chlamydia Pneumoniae and Staphylococcus AureusSharl Bea EsmeraldaÎncă nu există evaluări
- Community Acquired Pneumonia. FinalDocument48 paginiCommunity Acquired Pneumonia. FinalHampson Malekano100% (2)
- DRUG STUDY: Fenofibrate - TricorDocument2 paginiDRUG STUDY: Fenofibrate - TricorYum CÎncă nu există evaluări
- Pcap PathophysiologyDocument3 paginiPcap PathophysiologyAko Gle C Mariz80% (10)
- Presentation onCAP MRDocument92 paginiPresentation onCAP MRrouche100% (10)
- CAP - Patho DiagramDocument5 paginiCAP - Patho DiagramAzai Rhea Malate63% (8)
- Case Study - AGE With Some DHNDocument19 paginiCase Study - AGE With Some DHNJessica Mae Abaquita-javierÎncă nu există evaluări
- PneumoniaDocument1 paginăPneumoniaAyen FornollesÎncă nu există evaluări
- Case Study PCAPDocument32 paginiCase Study PCAPJohn Paul Andrade100% (1)
- Case Study of Community Acquired PneumoniaDocument14 paginiCase Study of Community Acquired PneumoniaRachelÎncă nu există evaluări
- Acute GastroenteritisDocument10 paginiAcute GastroenteritisRhajeeb SugalaÎncă nu există evaluări
- Pathophysiology of Acute GastroenteritisDocument1 paginăPathophysiology of Acute GastroenteritisAlliah Grejie AnneÎncă nu există evaluări
- Pathophysiology TBDocument2 paginiPathophysiology TBJhen DeguzmanÎncă nu există evaluări
- Case Study of Acute GastritisDocument12 paginiCase Study of Acute Gastritisstudent_01960% (5)
- Bronchitis PathophysiologyDocument1 paginăBronchitis PathophysiologyFerry Reyes0% (1)
- Pathophysiology of PTB (Myrc)Document2 paginiPathophysiology of PTB (Myrc)Rj MagpayoÎncă nu există evaluări
- Pcap Pathophysiology PDFDocument3 paginiPcap Pathophysiology PDFMikaela RamosÎncă nu există evaluări
- Age - Weather: Aspiration of Secretions Containing MicrobesDocument4 paginiAge - Weather: Aspiration of Secretions Containing Microbeslouie john abilaÎncă nu există evaluări
- Pathophysiology Dengue Hemorrhagic FeverDocument1 paginăPathophysiology Dengue Hemorrhagic FeverShiella Heart Malana100% (1)
- AGE PathophysiologyDocument2 paginiAGE Pathophysiologyjosephcanlas67% (3)
- Pathophysiology of PneumoniaDocument1 paginăPathophysiology of Pneumoniaoxidalaj97% (31)
- Patho Pleural EffusionDocument2 paginiPatho Pleural EffusionJess Prodigo50% (2)
- Amoebiasis PathophysiologyDocument3 paginiAmoebiasis PathophysiologyApril CornejoÎncă nu există evaluări
- Cap MRDocument4 paginiCap MRKit BarcelonaÎncă nu există evaluări
- Pathophysiology of PneumoniaDocument4 paginiPathophysiology of PneumoniamatrixtrinityÎncă nu există evaluări
- Patient Based PathophysiologyDocument2 paginiPatient Based PathophysiologyDeinielle Magdangal RomeroÎncă nu există evaluări
- Pneumonia Pathophysiology (Book Based) : Non-Modifiable: ModifiableDocument2 paginiPneumonia Pathophysiology (Book Based) : Non-Modifiable: ModifiableYVETTE CLAIRE BORRESÎncă nu există evaluări
- (PULMO) - Asthma PDFDocument5 pagini(PULMO) - Asthma PDFKeith LajotÎncă nu există evaluări
- Isabela State University: Republic of The Philippines San Fabian, Echague, Isabela Activity 2 Medical-Surgical NursingDocument9 paginiIsabela State University: Republic of The Philippines San Fabian, Echague, Isabela Activity 2 Medical-Surgical Nursingpinoy HubÎncă nu există evaluări
- Asthma 2009:: Latest in Diagnostic and Treatment Options Wendy L. Wright, MS, APRN, BC, FAANPDocument84 paginiAsthma 2009:: Latest in Diagnostic and Treatment Options Wendy L. Wright, MS, APRN, BC, FAANPmuthia saniÎncă nu există evaluări
- Asthma Pathophysiology: Ixsy Ramirez, MD, MPH Pediatric Pulmonology University of Michigan, C.S. Mott Children's HospitalDocument21 paginiAsthma Pathophysiology: Ixsy Ramirez, MD, MPH Pediatric Pulmonology University of Michigan, C.S. Mott Children's HospitalAru VermaÎncă nu există evaluări
- 50 DiseasesDocument44 pagini50 DiseasesJewenson SalvadorÎncă nu există evaluări
- Group 3 BSN3D CapDocument6 paginiGroup 3 BSN3D CapJingky AnquillanoÎncă nu există evaluări
- Chronic Obstructive Pulmonary Disease: Iman Galal, MDDocument60 paginiChronic Obstructive Pulmonary Disease: Iman Galal, MDYan Sheng HoÎncă nu există evaluări
- Asthma Mechanisms: Key PointsDocument6 paginiAsthma Mechanisms: Key PointsAfrian RahmandaÎncă nu există evaluări
- Pathophysiology of Chronic Renal Failure PDFDocument4 paginiPathophysiology of Chronic Renal Failure PDFDewa Made Rendy SanjayaÎncă nu există evaluări
- Airway Management: Lecture By: Dr. Ayesha Latif (PT)Document32 paginiAirway Management: Lecture By: Dr. Ayesha Latif (PT)Ayesha LatifÎncă nu există evaluări
- KumeDocument28 paginiKumeGrace Clemenia-GrefaldiaÎncă nu există evaluări
- Applications of Next Generation SequencinginhematologyDocument6 paginiApplications of Next Generation SequencinginhematologyAbhishek SharmaÎncă nu există evaluări
- Kumpulan Tugas: Disusun Oleh: Revi Adestika 2008730105Document1 paginăKumpulan Tugas: Disusun Oleh: Revi Adestika 2008730105Revi AdestikaÎncă nu există evaluări
- RANITIDINEDocument2 paginiRANITIDINEChoox PriiÎncă nu există evaluări
- First Page PDFDocument1 paginăFirst Page PDFEricaÎncă nu există evaluări
- 71 Bed Bug Information HLDocument1 pagină71 Bed Bug Information HLMatthew SelfÎncă nu există evaluări
- PED025 SAS Lesson 5Document7 paginiPED025 SAS Lesson 5Sheena Mae PoÎncă nu există evaluări
- UDID What Medical Doctors May Need To KnowDocument37 paginiUDID What Medical Doctors May Need To KnowdrhareeshÎncă nu există evaluări
- Jonathan C. Lubag Unintentional Injuries Q3M1 W1-3Document26 paginiJonathan C. Lubag Unintentional Injuries Q3M1 W1-3Jonathan LubagÎncă nu există evaluări
- An Introduction To The Mckenzie Method: Treating Your Own BackDocument24 paginiAn Introduction To The Mckenzie Method: Treating Your Own BackR HariÎncă nu există evaluări
- Microbiology CaseDocument3 paginiMicrobiology Caseclower112100% (2)
- Use of CoQ10 To Treat MalignanciesDocument2 paginiUse of CoQ10 To Treat MalignanciesTUartistÎncă nu există evaluări
- Norovirus Public Health Fact SheetDocument2 paginiNorovirus Public Health Fact SheetClickon DetroitÎncă nu există evaluări
- Ovarian Cancer: A. IntroductionDocument10 paginiOvarian Cancer: A. IntroductionBer AnneÎncă nu există evaluări
- Is Vaginal Delivery or Caesarean Section The Safer Mode of Delivery in Patients With Adult Congenital Heart DiseaseDocument7 paginiIs Vaginal Delivery or Caesarean Section The Safer Mode of Delivery in Patients With Adult Congenital Heart DiseaseNathania TjuwatjaÎncă nu există evaluări
- Acute Painful ScrotumDocument15 paginiAcute Painful ScrotumthinkercolÎncă nu există evaluări
- Pregnancy Induced Urinary Tract Changes Urinary Tract InfectionsDocument5 paginiPregnancy Induced Urinary Tract Changes Urinary Tract InfectionsDilausan B MolukÎncă nu există evaluări
- Casali 2009Document6 paginiCasali 2009Giancarlo Maruri MunarettoÎncă nu există evaluări
- GES 107 - Introduction To HIV&AIDSDocument39 paginiGES 107 - Introduction To HIV&AIDSSafiyah IzuagieÎncă nu există evaluări
- HemorrhoidsDocument26 paginiHemorrhoidsWaqar ZahirÎncă nu există evaluări
- Microbiology MB QuestionsDocument13 paginiMicrobiology MB QuestionsRashmi Ranjan100% (1)