Documente Academic
Documente Profesional
Documente Cultură
Assessing Dehydration Chart Msword 485697997
Încărcat de
Aqila MumtazTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Assessing Dehydration Chart Msword 485697997
Încărcat de
Aqila MumtazDrepturi de autor:
Formate disponibile
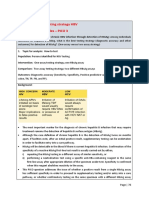
Assessing dehydration in children under 5 years
Use this table to detect clinical dehydration and shock during remote and face-to-face assessments
Adapted from Diarrhoea and vomiting in children (NICE clinical guideline 84). The quick reference guide and full guidance are available from: www.nice.org.uk/CG84
Increasing severity of dehydration
No clinically Clinical dehydration Clinical shock
detectable
dehydration
Signs (face-to-face assessface-to-(remoteSympto
Appears well Appears to be unwell or
ms
deteriorating
Alert and responsive Altered responsiveness (for Decreased level of
example, irritable, lethargic) consciousness
and
Normal urine output Decreased urine output
Skin colour unchanged Skin colour unchanged Pale or mottled skin
ments) face
Warm extremities Warm extremities Cold extremities
Alert and responsive Altered responsiveness (for Decreased level of
example, irritable, lethargic) consciousness
assessments)
Skin colour unchanged Skin colour unchanged Pale or mottled skin
Warm extremities Warm extremities Cold extremities
Eyes not sunken Sunken eyes
Moist mucous Dry mucous membranes
membranes (except (except for mouth breather')
after a drink)
Normal heart rate Tachycardia Tachycardia
Normal breathing Tachypnoea Tachypnoea
pattern
Normal peripheral Normal peripheral pulses Weak peripheral pulses
pulses
Normal capillary refill Normal capillary refill time Prolonged capillary refill
time time
Normal skin turgor Reduced skin turgor
Normal blood pressure Normal blood pressure Hypotension
Interpret symptoms and signs taking into account risk factors for dehydration (see box 1). More numerous and more pronounced symptoms and signs of clinical
(decompensated
dehydration indicate greater severity. For clinical shock, one or more of the symptoms shock)
and/or signs listed would be present. Dashes () indicate that these clinical features
do not specifically indicate shock. Symptoms and signs with red flags ( ) may help to identify children at increased risk of progression to shock. If in doubt, manage as if
there are symptoms and/or signs with red flags.
Assessing dehydration in children under 5 years
Use this table to detect clinical dehydration and shock during remote and face-to-face assessments
Adapted from Diarrhoea and vomiting in children (NICE clinical guideline 84). The quick reference guide and full guidance are available from: www.nice.org.uk/CG84
Box 1 At increased risk of dehydration: more in the past 24 hours
Children younger than 1 year, especially children who have not been offered or have
those younger than 6 months not been able to tolerate supplementary
infants who were of low birth weight fluids before presentation
children who have passed six or more infants who have stopped breastfeeding
diarrhoeal stools in the past 24 hours during the illness
children who have vomited three times or children with signs of malnutrition.
Suspect hypernatraemic dehydration if there are any of the following:
jittery movements
increased muscle tone
hyperreflexia
convulsions
drowsiness or coma.
Laboratory investigations:
Do not routinely perform blood biochemistry.
Measure plasma sodium, potassium, urea, creatinine and glucose
concentrations if:
intravenous fluid therapy is required or
there are symptoms or signs suggesting hypernatraemia.
Measure venous blood acidbase status and chloride concentration if shock is
suspected or confirmed.
Interpret symptoms and signs taking into account risk factors for dehydration (see box 1). More numerous and more pronounced symptoms and signs of clinical
dehydration indicate greater severity. For clinical shock, one or more of the symptoms and/or signs listed would be present. Dashes () indicate that these clinical features
do not specifically indicate shock. Symptoms and signs with red flags ( ) may help to identify children at increased risk of progression to shock. If in doubt, manage as if
there are symptoms and/or signs with red flags.
S-ar putea să vă placă și
- HBV Easl-CpgDocument48 paginiHBV Easl-CpgAqila MumtazÎncă nu există evaluări
- 4.5. How To Test - Testing Strategy HBV Decision-Making Tables - PICO 3Document10 pagini4.5. How To Test - Testing Strategy HBV Decision-Making Tables - PICO 3Aqila MumtazÎncă nu există evaluări
- Lung CaDocument1 paginăLung CaAqila MumtazÎncă nu există evaluări
- Weight Percentiles CalculatorDocument1 paginăWeight Percentiles CalculatorAqila MumtazÎncă nu există evaluări
- Manual CBC 1 3: - Wbcs - Platelets Count - PCV or HCT - Retics Count - HB Estimation 3 3 4 5 6Document25 paginiManual CBC 1 3: - Wbcs - Platelets Count - PCV or HCT - Retics Count - HB Estimation 3 3 4 5 6Aqila MumtazÎncă nu există evaluări
- Approach of TraumaDocument45 paginiApproach of TraumaAqila MumtazÎncă nu există evaluări
- Weight Percentiles CalculatorDocument1 paginăWeight Percentiles CalculatorAqila MumtazÎncă nu există evaluări
- Ethics Approval2013 - NewDocument8 paginiEthics Approval2013 - NewAqila MumtazÎncă nu există evaluări
- DKA Study GroupDocument24 paginiDKA Study GroupAqila MumtazÎncă nu există evaluări
- Diabetic Foot UlcerDocument3 paginiDiabetic Foot UlcerAqila MumtazÎncă nu există evaluări
- Treatment and Management of AstrocytomaDocument2 paginiTreatment and Management of AstrocytomaAqila MumtazÎncă nu există evaluări
- Hyperglycemic Hyperosmolar StateDocument17 paginiHyperglycemic Hyperosmolar StateAqila Mumtaz50% (2)
- Assignments 2016: M T W T F S SDocument12 paginiAssignments 2016: M T W T F S SAqila MumtazÎncă nu există evaluări
- HO OnG NotesDocument38 paginiHO OnG NotesAqila MumtazÎncă nu există evaluări
- Ray DiagramsDocument3 paginiRay DiagramsAqila MumtazÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Pediatric Case 5: Eva Madison (Core) : Guided Reflection QuestionsDocument3 paginiPediatric Case 5: Eva Madison (Core) : Guided Reflection QuestionsDai Nguyen100% (3)
- Revised Ramadan HandoutDocument2 paginiRevised Ramadan Handoutapi-570986190Încă nu există evaluări
- IV Fluid Cheat SheetsDocument8 paginiIV Fluid Cheat SheetsNhietz SeraÎncă nu există evaluări
- Heat Stress Monitoring Plan Rev 1 EnglishDocument10 paginiHeat Stress Monitoring Plan Rev 1 EnglishBogdan RaduÎncă nu există evaluări
- SCADDDocument4 paginiSCADDRajiv Kabad0% (1)
- Cues Nursing Diagnosis Goal Nursing Interventions Rationale EvaluationDocument3 paginiCues Nursing Diagnosis Goal Nursing Interventions Rationale EvaluationVher SisonÎncă nu există evaluări
- XcaretDocument9 paginiXcaretmubarek abdurohemanÎncă nu există evaluări
- MalariaDocument30 paginiMalariaNipul MondolÎncă nu există evaluări
- Hope 3 Q2 M9Document16 paginiHope 3 Q2 M9lalatina best grillÎncă nu există evaluări
- American Family Physician - February 1, 2019 - Gastroenteritis in ChildrenDocument17 paginiAmerican Family Physician - February 1, 2019 - Gastroenteritis in ChildrenDaniel PuertasÎncă nu există evaluări
- CPR AED First Aid Certification Course National CPR FoundationDocument24 paginiCPR AED First Aid Certification Course National CPR FoundationHarjot Singh GandhiÎncă nu există evaluări
- Cues Objectives Interventions Rationale Evaluation: Nursing Care Plan 1Document7 paginiCues Objectives Interventions Rationale Evaluation: Nursing Care Plan 1JP2001Încă nu există evaluări
- Dolores WellbeingDocument1 paginăDolores Wellbeingcharles estradaÎncă nu există evaluări
- Working Environmental HazardsDocument5 paginiWorking Environmental HazardsSri100% (1)
- Fluid Balance Monitoring PosterDocument1 paginăFluid Balance Monitoring PosterSania oktaÎncă nu există evaluări
- 02 Handout 1Document5 pagini02 Handout 1Mickle LapitanÎncă nu există evaluări
- DENGUE CPG Final Manuscript v.12.2024Document211 paginiDENGUE CPG Final Manuscript v.12.2024shrwn.y.goÎncă nu există evaluări
- Heat Stress PresentationDocument54 paginiHeat Stress Presentationkhan40100% (2)
- PICU Protocol FINALDocument120 paginiPICU Protocol FINALwalaa mousaÎncă nu există evaluări
- Fluid and Electrolyte BalanceDocument52 paginiFluid and Electrolyte BalanceFrancis Appau100% (1)
- Nursing Care Plan Cues Nursing Diagnosis Objectives Nursing Intervention Rationale EvaluationDocument6 paginiNursing Care Plan Cues Nursing Diagnosis Objectives Nursing Intervention Rationale EvaluationMae AzoresÎncă nu există evaluări
- (SỐ 11-20) DE THI HSG ANH 9 CAP TINH +FILE NGHE+ DAP ANDocument89 pagini(SỐ 11-20) DE THI HSG ANH 9 CAP TINH +FILE NGHE+ DAP ANVy 's Khánh100% (1)
- Fluid Volume Deficit (Dehydration) Nursing Care Plan - NurseslabsDocument17 paginiFluid Volume Deficit (Dehydration) Nursing Care Plan - NurseslabsA.Încă nu există evaluări
- DiarroheaDocument44 paginiDiarroheaRashmi SharmaÎncă nu există evaluări
- Nursing Diagnosis Nursing Interventions Rationale: IndependentDocument2 paginiNursing Diagnosis Nursing Interventions Rationale: IndependentJessica SurmiedaÎncă nu există evaluări
- USAtoday Final PDFDocument4 paginiUSAtoday Final PDFparapencarituhanÎncă nu există evaluări
- NCP CKDDocument9 paginiNCP CKDDanica Salinas100% (1)
- Acute GastroenteritisDocument19 paginiAcute GastroenteritisJoy Jarin100% (1)
- Hope Quarter 2 (Week 1-2)Document3 paginiHope Quarter 2 (Week 1-2)Patrick OliverosÎncă nu există evaluări
- Cholera: Causes Risks Factors Symptoms Diagnosis and Treatment Complications PreventionDocument5 paginiCholera: Causes Risks Factors Symptoms Diagnosis and Treatment Complications Preventionsubham kumarÎncă nu există evaluări