Documente Academic
Documente Profesional
Documente Cultură
ABC of Wound Healing PDF
Încărcat de
MrJPhaetonTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
ABC of Wound Healing PDF
Încărcat de
MrJPhaetonDrepturi de autor:
Formate disponibile
Practice
ABC of wound healing This is the first in a series of 12 articles
Wound assessment
Joseph E Grey, Stuart Enoch, Keith G Harding
Most wounds, of whatever aetiology, heal without difficulty.
Some wounds, however, are subject to factors that impede
healing, although these do not prevent healing if the wounds
are managed appropriately. A minority of wounds will become
chronic and non-healing. In these cases the ultimate goal is to
control the symptoms and prevent complications, rather than
healing the wound.
Causes of ulceration
x Vascular (venous, arterial, lymphatic, vasculitis)
x Neuropathic (for example, diabetes, spina bifida, leprosy)
x Metabolic (for example, diabetes, gout)
x Connective tissue disease (for example, rheumatoid arthritis,
scleroderma, systemic lupus erythematosus)
x Pyoderma gangrenosum (often reflection of systemic disorder)
x Haematological disease (red blood cell disorders (for example,
Wounds are not just skin deep, and accurate assessment is an essential part
sickle cell disease); white blood cell disorders (for example, of treatment
leukaemia); platelet disorders (for example, thrombocytosis))
x Dysproteinaemias (for example, cryoglobulinaemia, amyloidosis)
x Immunodeficiency (for example, HIV, immunosuppressive therapy)
x Neoplastic (for example, basal cell carcinoma, squamous cell
carcinoma, metastatic disease)
x Infectious (bacterial, fungal, viral)
x Panniculitis (for example, necrobiosis lipoidica) Local and systemic factors that impede wound healing
x Traumatic (for example, pressure ulcer, radiation damage) Local factors Systemic factors
x Iatrogenic (for example, drugs) x Inadequate blood x Advancing age and general immobility
x Factitious (self harm, dermatitis artefacta) supply x Obesity
x Others (for example, sarcoidosis) x Increased skin tension x Smoking
x Poor surgical x Malnutrition
apposition x Deficiency of vitamins and trace elements
x Wound dehiscence x Systemic malignancy and terminal illness
x Poor venous drainage x Shock of any cause
It is important that the normal processes of developing a x Presence of foreign x Chemotherapy and radiotherapy
diagnostic hypothesis are followed before trying to treat the body and foreign x Immunosuppressant drugs,
wound. A detailed clinical history should include information body reactions corticosteroids, anticoagulants
on the duration of ulcer, previous ulceration, history of trauma, x Continued presence x Inherited neutrophil disorders, such as
family history of ulceration, ulcer characteristics (site, pain, of micro-organisms leucocyte adhesion deficiency
x Infection x Impaired macrophage activity
odour, and exudate or discharge), limb temperature, underlying
x Excess local mobility, (malacoplakia)
medical conditions (for example, diabetes mellitus, peripheral such as over a joint
vascular disease, ischaemic heart disease, cerebrovascular
accident, neuropathy, connective tissue diseases (such as
rheumatoid arthritis), varicose veins, deep venous thrombosis),
previous venous or arterial surgery, smoking, medications, and
allergies to drugs and dressings. Appropriate investigations
should be carried out.
Some complications of chronic wounds
x Sinus formation
x Fistula
x Unrecognised malignancy
x Malignant transformation in the ulcer bed (Marjolins ulcer)
x Osteomyelitis
x Contractures and deformity in surrounding joints
x Systemic amyloidosis
x Heterotopic calcification Areas of abnormal pressure
x Colonisation by multiple drug resistant pathogens, leading to distribution in the diabetic foot.
antibiotic resistance Plantar ulcers are most commonly
x Anaemia seen under the hallux, on the first
x Septicaemia and fifth metatarsal heads, and under
the heel
BMJ VOLUME 332 4 FEBRUARY 2006 bmj.com 285
Practice
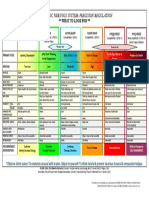
Assessing wounds Laboratory investigations before treating a wound
Size of wound Investigation Rationale
The size of the wound should be assessed at first presentation Haemoglobin Anaemia may delay healing
and regularly thereafter. The outline of the wound margin White cell count Infection
should be traced on to transparent acetate sheets and the Platelet count Thrombocytopenia
surface area estimated: in wounds that are approximately Erythrocyte sedimentation rate; Non-specific markers of infection
circular, multiply the longest diameter in one plane by the C reactive protein and inflammation; useful in
longest diameter in the plane at right angles; in irregularly diagnosis and monitoring
shaped wounds, add up the number of squares contained within treatment of infectious or
inflammatory ulceration
the margin of the outline of the wound from an acetate grid
Urea and creatinine High urea impairs wound healing.
tracing. These methods are the simplest, but it should be
Renal function important when
recognised that they are not precise. However, they do provide using antibiotics
a means by which progress over time to wound closure can be Albumin Protein loss delays healing
identified. Patient positioning, body curvature, or tapering of Glucose, haemoglobin A1C Diabetes mellitus
the limbs will affect the accuracy of these techniques. Markers of autoimmune disease Indicative of rheumatoid disease,
(such as rheumatoid factor, systemic lupus erythematosus, and
antinuclear antibodies, other connective tissue disorders
anticardiolipin antibodies, lupus
anticoagulant)
Cryoglobulins, cryofibrinogens, Haematological disease
prothrombin time, partial
thromboplastin time
Deficiency or defect of Vascular thrombosis
antithrombin III, protein C,
Tracing a wound for measurement and measuring a wound
protein S, factor V Leiden
Haemoglobinopathy screen Sickle cell anaemia, thalassaemia
HIV status Kaposis sarcoma
Edge of wound
Serum protein electrophoresis; Myeloma
Although not diagnostic, examination of the edge of the wound Bence-Jones proteins
may help to identify its aetiology in the context of the history of Urine analysis Useful in connective tissue disease
the wound. For example, venous leg ulcers generally have gently Wound swab Not routine; all ulcers colonised
sloping edges, arterial ulcers often appear well demarcated and (not the same as infection); swab
punched out, and rolled or everted edges should raise the only when clinical signs of infection
suspicion of malignancy. A biopsy should be taken of any
suspicious wound.
Wound edge characteristics
Edges Type of ulcer
Sloping Venous ulcer
Punched out Arterial or vasculitic ulcer
Rolled Basal cell carcinoma
Everted Squamous cell carcinoma
Left: Basal cell carcinoma with rolled edges. Right: Lymphoma
Undermining Tuberculosis, syphilis presenting as groin ulceration
Purple Vasculitic (such as pyoderma
gangrenosum) Site of wound and type of ulcer
Site Type of ulcer
Gaiter area of the leg Venous ulcer
Site of wound Sacrum, greater trochanter, heel Pressure ulcer
The site of the wound may aid diagnosis; diabetic foot ulcers Dorsum of the foot Arterial or vasculitic ulcer
often arise in areas of abnormal pressure distribution arising Shin Necrobiosis lipoidica
from disordered foot architecture. Venous ulceration occurs Lateral malleolus Venous, arterial, or pressure ulcer
mostly in the gaiter area of the leg (see next article in this or hydroxyurea induced ulceration
series). Non-healing ulcers, sometimes in unusual sites, should Plantar and lateral aspect of foot Diabetic ulcer
prompt consideration of malignancy. and toes
Sun exposed areas Basal cell carcinoma; squamous cell
Wound bed carcinoma
Healthy granulation tissue is pink in colour and is an indicator
of healing. Unhealthy granulation is dark red in colour, often
bleeds on contact, and may indicate the presence of wound
infection. Such wounds should be cultured and treated in the
light of microbiological results. Excess granulation or
overgranulation may also be associated with infection or
non-healing wounds. These often respond to simple cautery
Left: Healthy granulation tissue in a hidradenitis
with silver nitrate or with topically applied steroid preparations. suppurativa excision wound. Right: Unhealthy
Chronic wounds may be covered by white or yellow shiny granulation tissue in a venous leg ulcer
286 BMJ VOLUME 332 4 FEBRUARY 2006 bmj.com
Practice
fibrinous tissue (see next article in this series). This tissue is
Bone at the base of a wound may suggest a protracted
avascular, and healing will proceed only when it is removed.
healing time and the possibility of underlying
This can be done with a scalpel at the bedside. osteomyelitis
The type of tissue at the base of the wound will provide
useful information relating to expectation of total healing time
and the risk of complicationsfor example, bone at the base
may suggest osteomyelitis and delayed or non-healing.
Necrotic tissue, slough, and eschar
The wound bed may be covered with necrotic tissue (non-viable
tissue due to reduced blood supply), slough (dead tissue, usually
cream or yellow in colour), or eschar (dry, black, hard necrotic
tissue). Such tissue impedes healing. Necrotic tissue and slough
may be quantified as excessive (+++), moderate (++), minimal (+),
or absent ().
Since necrotic tissue can also harbour pathogenic
organisms, removal of such tissue helps to prevent wound
infection. Necrotic tissue and slough should be debrided with a
scalpel so that the wound bed can be accurately assessed and
facilitate healing. Eschar may be adherent to the wound bed,
making debridement with a scalpel difficult. Further
debridement, as part of wound management, may be required
using other techniques. Top: Necrotic tissue (black areas) in a pressure ulcer. Bottom: Slough at the
base of a pressure ulcer. Right: Eschar covering a heel pressure ulcer
Types of debridement
SharpAt the bedside (using scalpel or curette)
SurgicalIn the operating theatre
AutolyticFacilitation of the bodys own mechanism of debridement
with appropriate dressings
BiologicalLarval (maggot) therapy
EnzymaticNot widely used; pawpaw (papaya) or banana skin used in
developing countries
MechanicalWet-to-dry dressings (not widely used in the UK)
Left: Digital examination of a wound. Right: Examining a wound with a
probe
Depth
Accurate methods for measuring wound depth are not practical
or available in routine clinical practice. However, approximate
measurements of greatest depth should be taken to assess
wound progress. Undermining of the edge of the wound must
be identified by digital examination or use of a probe. The
depth and extent of sinuses and fistulas should be identified.
Undermining areas and sinuses should be packed with an
appropriate dressing to facilitate healing. Undermining wounds
and sinuses with narrow necks that are difficult to dress may be
amenable to be laid open at the bedside to facilitate drainage
and dressing. Wounds associated with multiple sinuses or
fistulas should be referred for specialist surgical intervention. Fistula in a diabetic foot
ulcer
Surrounding skin
Cellulitis associated with wounds should be treated with
systemic antibiotics. Eczematous changes may need treatment
with potent topical steroid preparations. Maceration of the
surrounding skin is often a sign of inability of the dressing to
control the wound exudate, which may respond to more
frequent dressing changes or change in dressing type. Callus
surrounding and sometimes covering neuropathic foot ulcers
(for example, in diabetic patients) must be debrided to (a)
visualise the wound, (b) eliminate potential source of infection,
and (c) remove areas close to the wound subject to abnormal
pressure that would otherwise cause enlargement of the wound.
This can be done at the bedside.
Infection
All open wounds are colonised. Bacteriological culture is Maceration of the skin
indicated only if clinical signs of infection are present or if surrounding a diabetic foot ulcer
BMJ VOLUME 332 4 FEBRUARY 2006 bmj.com 287
Practice
infection control issues (such as methicillin resistant
Wound exudate
staphylococcus aureus (MRSA)) need to be considered. The
classic signs of infection are heat, redness, swelling, and pain. x Wound exudate may be serous, serosanguinous, or sanguinous
x The quantity of exudate is usually classified as heavy (+++ (dressing
Additional signs of wound infection include increased exudate,
soaked)), medium (++ (dressing wet)), or minimal (+ (dressing dry))
delayed healing, contact bleeding, odour, and abnormal x Excessive exudate may be due to wound infection or gross oedema
granulation tissue. Treatment with antimicrobials should be in the wound area and may complicate wound healing
guided by microbiological results and local resistance patterns. x The exudate should be controlled with the use of dressings
appropriate for the level of exudate and any infection treated
x Barrier films applied to the surrounding skin help to prevent
Pain
further maceration (see the ninth article in the series)
Pain is a characteristic feature of many healing and non-healing x The oedematous leg should be raised when the patient is seated
wounds. Pain can be caused by both nociceptive and
neuropathic stimuli. Intermittent pain is often related to
dressing removal or recent application of new dressings and
may necessitate the use of analgesia before the dressing is The causes of malodorous wounds include infection
and the presence of necrotic tissue. Infection should be
changed. Constant pain may arise as a result of the underlying
treated with antibiotics. Odour associated with necrotic
condition, such as ischaemia, neuropathy, tissue oedema, tissue may be reduced by removal of the necrotic tissue
chronic tissue damage (for example, lipodermatosclerosis), or use of agents impregnated with antiseptics or
infection, or scarring (for example, atrophie blanche). The charcoal . Treatment with topical metronidazole and use
nature and type of pain should be identified and treated of odour absorbing dressings may help to reduce odour
appropriately. Pain assessment tools can help to assess the from fungating malignant wounds. Larval therapy may
nature and severity of pain. With recalcitrant pain, or pain that also be helpful in the debridement of malodorous tissue
is difficult to control, consider referral to a local pain team.
Clinical features of non-healing wounds
Non-healing wounds x Absence of healthy
granulation tissue
x
x
Lack of adequate blood supply
Failure of re-epithelialisation
Non-healing wounds have traditionally been defined as those x Presence of necrotic and x Cyclical or persistent pain
unhealthy tissue in the x Recurrent breakdown of wound
that fail to progress through an orderly sequence of repair in a
wound bed x Clinical or subclinical infection
timely fashion. Such wounds are sometimes thought of as being x Excess exudate and slough
caused by neglect, incompetence, misdiagnosis, or
inappropriate treatment strategies. However, some wounds are
resistant to all efforts of treatment aimed at healing, and
alternative end points should be considered; measures aimed
at improving the quality of life will be paramount in these
instances.
Quality of life
Several studies have shown that patients with non-healing
wounds have a decreased quality of life. Reasons for this include
the frequency and regularity of dressing changes, which affect
daily routine; a feeling of continued fatigue due to lack of sleep;
restricted mobility; pain; odour; wound infection; and the Overgranulation may be a sign of infection or
physical and psychological effects of polypharmacy. The loss of non-healing
independence associated with functional decline can lead to
changes, sometimes subtle, in overall health and wellbeing.
These changes include altered eating habits, depression, social Further reading
isolation, and a gradual reduction in activity levels. Many x Lazarus GS, Cooper DM, Knighton DR, Margolis DJ, Pecoraro RE,
patients with non-healing wounds complain of difficulties with Rodeheaver G, et al. Definitions and guidelines for assessment of
wounds and evaluation of healing. Arch Dermatol 1994;130:489-93.
emotions, finances, physical health, daily activities, friendships, x Izadi K, Ganchi P. Chronic wounds. Clin Plast Surg 2005;32:209-22.
and leisure pursuits. x Falanga V, Phillips TJ, Harding KG, Moy RL, Peerson LJ, eds. Text
Quality of life is not always related to healing of the wound. atlas of wound management. London: Martin Dunitz, 2000.
It may be clear from the outset that wounds in some patients
will be unlikely to heal. In such patients control of symptoms
Stuart Enoch is a research fellow of the Royal College of Surgeons of
and signs outlined aboveparticularly odour, exudate, and England and is based at the Wound Healing Research Unit, Cardiff
painmay improve the individuals quality of life. Additionally, University.
optimal chronic wound management will lead to a reduction in The ABC of wound healing is edited by Joseph E Grey
the frequency of dressing changes, further enhancing quality of (joseph.grey@cardiffandvale.wales.nhs.uk), consultant physician,
life. In a minority of instances, seemingly drastic measures University Hospital of Wales, Cardiff and Vale NHS Trust, Cardiff, and
such as amputation in a person with chronic leg ulceration honorary consultant in wound healing at the Wound Healing
Research Unit, Cardiff University, and by Keith G Harding, director of
may need to be considered when the quality of life is severely the Wound Healing Research Unit, Cardiff University, and professor
affected by the non-healing wound and its complications. of rehabilitation medicine (wound healing) at Cardiff and Vale NHS
Trust. The series will be published as a book in summer 2006.
The drawing on page 285 is adapted from one provided by Wendy Tyrrell,
School of Health and Social Sciences, University of Wales Institute, Cardiff. Competing interests: KGHs unit receives income from many commercial
companies for research and education, and for advice. It does not support
BMJ 2006;332:2858 one companys products over another.
288 BMJ VOLUME 332 4 FEBRUARY 2006 bmj.com
S-ar putea să vă placă și
- Diabetes Foot CareDocument2 paginiDiabetes Foot CareseramulambaÎncă nu există evaluări
- Splenic Trauma WSES Classification and GuidelinesDocument27 paginiSplenic Trauma WSES Classification and GuidelinespgmzÎncă nu există evaluări
- Advances in Cattle WelfareDe la EverandAdvances in Cattle WelfareCassandra TuckerÎncă nu există evaluări
- Hemolytic AnemiaDocument18 paginiHemolytic AnemiaAdisurya NugrahaÎncă nu există evaluări
- Internal MedicineDocument161 paginiInternal Medicinemain.genevive.diligÎncă nu există evaluări
- Colageno en OsteoartritisDocument12 paginiColageno en Osteoartritisluisarenas0Încă nu există evaluări
- Major Tropical Diseases - Prof. Dr. Sugeng JuwonoDocument48 paginiMajor Tropical Diseases - Prof. Dr. Sugeng JuwonosittihajarÎncă nu există evaluări
- Acute Pancreatitis: in The ClinicDocument16 paginiAcute Pancreatitis: in The ClinicdeltanueveÎncă nu există evaluări
- Iatrogenic Biliary InjuriesDocument15 paginiIatrogenic Biliary InjuriessolysanÎncă nu există evaluări
- Diffi Cult To Treat Asthma: Sandhya Khurana Fernando Holguin EditorsDocument339 paginiDiffi Cult To Treat Asthma: Sandhya Khurana Fernando Holguin Editorsneumologia.intervencionÎncă nu există evaluări
- Strategies To Deal With Uncertainty in Medicine 20Document2 paginiStrategies To Deal With Uncertainty in Medicine 20Emilio AssisÎncă nu există evaluări
- SOGP AnaemiaDocument16 paginiSOGP AnaemiaMuhammad Farrukh ul IslamÎncă nu există evaluări
- Approach To Joint PainDocument37 paginiApproach To Joint PainMuhammad MakkiÎncă nu există evaluări
- Hematological Disorders in Geriatric PatientsDocument18 paginiHematological Disorders in Geriatric PatientsAndre HawkÎncă nu există evaluări
- Initial Management of Trauma in Adults - UpToDateDocument37 paginiInitial Management of Trauma in Adults - UpToDateAlberto Kenyo Riofrio PalaciosÎncă nu există evaluări
- Acute Kidney InjuryDocument15 paginiAcute Kidney InjuryManish VijayÎncă nu există evaluări
- MSK Notes ImportantDocument25 paginiMSK Notes ImportantkexonlagodÎncă nu există evaluări
- Guidelines SBO (Small Bowel Obstruction)Document14 paginiGuidelines SBO (Small Bowel Obstruction)Ghege GuntaranÎncă nu există evaluări
- Management of Diabetic FootDocument13 paginiManagement of Diabetic FootHabib Bakri Mamat At-TaranjaniÎncă nu există evaluări
- Diabetic Foot Infections: by Scott Bergman, Pharm.D., BCPS-AQ ID and Punit J. Shah, Pharm.D., BCPSDocument20 paginiDiabetic Foot Infections: by Scott Bergman, Pharm.D., BCPS-AQ ID and Punit J. Shah, Pharm.D., BCPSPrashant LokhandeÎncă nu există evaluări
- Viral Hepatitis PDFDocument4 paginiViral Hepatitis PDFNina BracyÎncă nu există evaluări
- JNC 8Document40 paginiJNC 8Nadira Wulandari100% (1)
- Fellowship in Critical Care MedicineDocument12 paginiFellowship in Critical Care MedicinerajiÎncă nu există evaluări
- E Learning Geriatric Oncology An IntroductionDocument65 paginiE Learning Geriatric Oncology An IntroductionHarold JeffersonÎncă nu există evaluări
- Draft CPG OA PDFDocument52 paginiDraft CPG OA PDFRam NishaÎncă nu există evaluări
- Medex Exam Writeups PageDocument9 paginiMedex Exam Writeups Pageaahmad87Încă nu există evaluări
- Emergency Ortho BCS 2017Document80 paginiEmergency Ortho BCS 2017Priza RazunipÎncă nu există evaluări
- Chronic Hepatitis B Infection A ReviewDocument12 paginiChronic Hepatitis B Infection A ReviewMr. LÎncă nu există evaluări
- Fome - Impact of The Illness in A FamilyDocument29 paginiFome - Impact of The Illness in A FamilyMuhammad Gilang DwiputraÎncă nu există evaluări
- Inborn Errors of Metabolism - Basics For Students (Iver Andreas Norbergs Kopi Som Er I Konflikt 2016-01-24)Document4 paginiInborn Errors of Metabolism - Basics For Students (Iver Andreas Norbergs Kopi Som Er I Konflikt 2016-01-24)Wen Jie LauÎncă nu există evaluări
- Geriatric PharmacologyDocument77 paginiGeriatric PharmacologyKhirsna PasajolÎncă nu există evaluări
- Etika Hub DR - PasienDocument23 paginiEtika Hub DR - PasienyonetsaniÎncă nu există evaluări
- Test 33: Surgery - Rheumatology/Orthopedics & SportsDocument8 paginiTest 33: Surgery - Rheumatology/Orthopedics & Sportskabal321Încă nu există evaluări
- Oral Manifestations of Systemic DiseasesDocument14 paginiOral Manifestations of Systemic Diseasesshygal1981Încă nu există evaluări
- Diagnosis of Systemic Lupus ErythematosusDocument6 paginiDiagnosis of Systemic Lupus ErythematosusMuhammad Akhram ResmanaÎncă nu există evaluări
- Diabetic Foot Ulcer Assessment and Management Algorithm - 0Document11 paginiDiabetic Foot Ulcer Assessment and Management Algorithm - 0Herlan BelaÎncă nu există evaluări
- Surgery NeurologyDocument9 paginiSurgery Neurologyaam_tabishÎncă nu există evaluări
- Technologies Designed To Help Improve Patients OutcomeDocument53 paginiTechnologies Designed To Help Improve Patients OutcomeHarby Ongbay AbellanosaÎncă nu există evaluări
- Acute Medicine BlueprintDocument1 paginăAcute Medicine BlueprintKo KhiÎncă nu există evaluări
- Diabetic Foot Case PresentationDocument58 paginiDiabetic Foot Case PresentationZH. omg sarÎncă nu există evaluări
- Oncologic Emergencies Critical CareDocument11 paginiOncologic Emergencies Critical CareWlad PaCa100% (1)
- Diabetic Foot InfectionsDocument52 paginiDiabetic Foot Infectionsshivakumar52Încă nu există evaluări
- H&P GuideDocument7 paginiH&P GuideTBWPÎncă nu există evaluări
- Antimicrobial Prophylaxis For Prevention of Surgical Site Infection in AdultsDocument59 paginiAntimicrobial Prophylaxis For Prevention of Surgical Site Infection in Adultsbolohan biatriceÎncă nu există evaluări
- Hemodialysis Emergencies: Core Curriculum 2021.Document14 paginiHemodialysis Emergencies: Core Curriculum 2021.Tariq ZayanÎncă nu există evaluări
- Evaluation of Headache in AdultsDocument21 paginiEvaluation of Headache in AdultsMaicon RamosÎncă nu există evaluări
- Miller's Anesthesia, 8th Edition: Anesthesiology April 2016Document3 paginiMiller's Anesthesia, 8th Edition: Anesthesiology April 2016Sabbir AhammedÎncă nu există evaluări
- V Polycystic Ovarysyndrome: EpidemiologyDocument13 paginiV Polycystic Ovarysyndrome: Epidemiologyrolla_hiraÎncă nu există evaluări
- WC BPR - Prevention and Management of Diabetic Foot Ulcers 1573r4e FinalDocument68 paginiWC BPR - Prevention and Management of Diabetic Foot Ulcers 1573r4e FinalArumDesiPratiwiÎncă nu există evaluări
- 15-Tropical Medicine & Infectious DiseaseDocument2 pagini15-Tropical Medicine & Infectious DiseaseIbrahimFikryÎncă nu există evaluări
- Venous ThromboembolismDocument49 paginiVenous Thromboembolismadamu mohammadÎncă nu există evaluări
- Case-Based Pace, ICDs, and CRT Volume 1Document234 paginiCase-Based Pace, ICDs, and CRT Volume 1oxequlalisÎncă nu există evaluări
- Murmur EvaluationDocument4 paginiMurmur EvaluationManjunath GeminiÎncă nu există evaluări
- #9 Ie 8 PDFDocument8 pagini#9 Ie 8 PDFOmar BasimÎncă nu există evaluări
- Hipercalcemia JamaDocument13 paginiHipercalcemia JamaSebastián Camilo Duque100% (1)
- Non Operative Fracture Management: Splint and CastDocument78 paginiNon Operative Fracture Management: Splint and CastSaeda AhmedÎncă nu există evaluări
- Dermatology For The NonDermDocument7 paginiDermatology For The NonDermDanielleÎncă nu există evaluări
- Wound DressingsDocument6 paginiWound DressingsMrJPhaetonÎncă nu există evaluări
- VaricocelectomyDocument10 paginiVaricocelectomyMrJPhaetonÎncă nu există evaluări
- Jan Apelqvist Ed Negative Pressure Wound Therapy Future PerspectivesDocument4 paginiJan Apelqvist Ed Negative Pressure Wound Therapy Future PerspectivesMrJPhaetonÎncă nu există evaluări
- WOUNDS January2014Document12 paginiWOUNDS January2014MrJPhaetonÎncă nu există evaluări
- Examen de InglesDocument4 paginiExamen de InglesMrJPhaetonÎncă nu există evaluări
- Simplifying Venous Leg Ulcer ManagementDocument28 paginiSimplifying Venous Leg Ulcer ManagementMrJPhaetonÎncă nu există evaluări
- 1 s2.0 S0022399915004870 Main PDFDocument7 pagini1 s2.0 S0022399915004870 Main PDFMrJPhaetonÎncă nu există evaluări
- Our Survival of SoulDocument463 paginiOur Survival of SoulAnonymous Mq8EkiAyhM100% (2)
- Konsep Filosofi, Konsep Holistik GadarDocument30 paginiKonsep Filosofi, Konsep Holistik GadarWinda GanggurÎncă nu există evaluări
- Mediclaim 2009 AutumnDocument46 paginiMediclaim 2009 AutumngopalpaulÎncă nu există evaluări
- Seal of Good Local Governance For Barangay (SGLGB)Document2 paginiSeal of Good Local Governance For Barangay (SGLGB)Ponciano AlveroÎncă nu există evaluări
- Shaukat Khanum Memorial Cancer Hospital & Research CentreDocument2 paginiShaukat Khanum Memorial Cancer Hospital & Research CentreMa BeÎncă nu există evaluări
- Ansdell G Elefant C. Pavlicevic M. Stige B. (2010) - Where Music Helps CommunityDocument4 paginiAnsdell G Elefant C. Pavlicevic M. Stige B. (2010) - Where Music Helps CommunityNati de la BarraÎncă nu există evaluări
- SP - Sindy MilaDocument2 paginiSP - Sindy MilaSindy MelindaÎncă nu există evaluări
- Blood Result Interpretation BookletDocument129 paginiBlood Result Interpretation BookletsithumÎncă nu există evaluări
- Reducing Negativity in A WorkplaceDocument12 paginiReducing Negativity in A WorkplaceAna Jane Morales CasaclangÎncă nu există evaluări
- AyurvedaDocument32 paginiAyurvedaRajeswari RanganathanÎncă nu există evaluări
- ICNCDRS Blindness Registry FormDocument4 paginiICNCDRS Blindness Registry FormAprilAngeliRobleÎncă nu există evaluări
- CCAC MSW City Action Plan Cebu City, PhilippinesDocument6 paginiCCAC MSW City Action Plan Cebu City, Philippinesca1Încă nu există evaluări
- Murli Deora v. Union of India (Banning of Smoking in Public Places)Document2 paginiMurli Deora v. Union of India (Banning of Smoking in Public Places)Prerna SinghÎncă nu există evaluări
- Fundamentals of Nursing Part 1Document8 paginiFundamentals of Nursing Part 1Evergreen Verds100% (1)
- 2017-02-23 Calvert County TimesDocument24 pagini2017-02-23 Calvert County TimesSouthern Maryland OnlineÎncă nu există evaluări
- Sistema NervosoDocument1 paginăSistema NervosoPerisson Dantas100% (2)
- Karyotype WorksheetDocument4 paginiKaryotype WorksheetKellieM.8406Încă nu există evaluări
- MEM05052A Apply Safe Welding Practices - Learner GuideDocument14 paginiMEM05052A Apply Safe Welding Practices - Learner Guidequestionbank.com.au100% (1)
- Validated HPTLC Method For Assay of Prednisolone in Tablets and Comparison With Pharmacopeial MethodsDocument4 paginiValidated HPTLC Method For Assay of Prednisolone in Tablets and Comparison With Pharmacopeial MethodsSyifa KhairunnisaÎncă nu există evaluări
- Transport OshDocument260 paginiTransport OshAnlugosiÎncă nu există evaluări
- Project PrimaryDocument7 paginiProject PrimaryLisanwork HonseboÎncă nu există evaluări
- Is Iso 10555 1 1995Document21 paginiIs Iso 10555 1 1995Hemant SharmaÎncă nu există evaluări
- Medical Equipment Quality Assurance (Tobey Clark, U Vermont)Document151 paginiMedical Equipment Quality Assurance (Tobey Clark, U Vermont)MelissaBarriosUrcia100% (2)
- LCSW Additional CourseworkDocument8 paginiLCSW Additional Courseworkiuhvgsvcf100% (2)
- Form g11Document23 paginiForm g11Armely NiedoÎncă nu există evaluări
- HPA 14 Assignemnt Due November 16thDocument5 paginiHPA 14 Assignemnt Due November 16thcÎncă nu există evaluări
- Applying 5S ProceduresDocument70 paginiApplying 5S ProceduresSanta Best100% (3)
- PDFDocument278 paginiPDFmahesh babu100% (1)
- Paintball City Waiver FormDocument1 paginăPaintball City Waiver FormAndrew HalsteadÎncă nu există evaluări
- 2 BiotechnologyDocument5 pagini2 BiotechnologyJannah BuenavistaÎncă nu există evaluări
- The Obesity Code: Unlocking the Secrets of Weight LossDe la EverandThe Obesity Code: Unlocking the Secrets of Weight LossEvaluare: 4 din 5 stele4/5 (6)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDe la EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsÎncă nu există evaluări
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe la EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeEvaluare: 2 din 5 stele2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe la EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityEvaluare: 4 din 5 stele4/5 (24)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDe la EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDe la EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisEvaluare: 4.5 din 5 stele4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedEvaluare: 5 din 5 stele5/5 (80)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDe la EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDEvaluare: 5 din 5 stele5/5 (1)
- Self-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!De la EverandSelf-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!Evaluare: 5 din 5 stele5/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDe la EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsEvaluare: 5 din 5 stele5/5 (1)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDe la EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisEvaluare: 4 din 5 stele4/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.De la EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Evaluare: 4.5 din 5 stele4.5/5 (110)
- Gut: the new and revised Sunday Times bestsellerDe la EverandGut: the new and revised Sunday Times bestsellerEvaluare: 4 din 5 stele4/5 (392)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDe la EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityEvaluare: 4 din 5 stele4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDe la EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsEvaluare: 4.5 din 5 stele4.5/5 (169)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDe la EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryEvaluare: 4 din 5 stele4/5 (44)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDe la EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessEvaluare: 4.5 din 5 stele4.5/5 (328)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDe la EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsEvaluare: 3.5 din 5 stele3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDe la EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisEvaluare: 3.5 din 5 stele3.5/5 (2)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningDe la EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningEvaluare: 4 din 5 stele4/5 (3)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)De la EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Evaluare: 4 din 5 stele4/5 (378)
- To Explain the World: The Discovery of Modern ScienceDe la EverandTo Explain the World: The Discovery of Modern ScienceEvaluare: 3.5 din 5 stele3.5/5 (51)
- The Marshmallow Test: Mastering Self-ControlDe la EverandThe Marshmallow Test: Mastering Self-ControlEvaluare: 4.5 din 5 stele4.5/5 (58)