Documente Academic
Documente Profesional
Documente Cultură
Timing of Initiation of Antiretrovirals Among Patients With HIV Requiring Tuberculosis Treatment
Încărcat de
AgieDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Timing of Initiation of Antiretrovirals Among Patients With HIV Requiring Tuberculosis Treatment
Încărcat de
AgieDrepturi de autor:
Formate disponibile
Timing of initiation of antiretrovirals among patients with
HIV requiring tuberculosis treatment.
There is now clear evidence that providing antiretroviral therapy to HIV-infected adults during
tuberculosis treatment, rather than waiting until completion of tuberculosis therapy, reduces
mortality, particularly among those with advanced HIV disease. In one randomized controlled
clinical trial among HIV-infected adults in South Africa, initiating antiretroviral therapy during
tuberculosis therapy rather than waiting until tuberculosis treatment was completed reduced the
hazard of all-cause mortality by 56% and was beneficial regardless of CD4 count.3 Subsequent
clinical trials evaluating the optimal timing of initiation of antiretroviral therapy during tuberculosis
treatment were conducted.4-7 Results from these trials, all of which were conducted in high
prevalence/low resource settings, indicated that earlier initiation of ART significantly reduced
mortality in persons with (non-meningitis) HIV-TB and CD4 cell count below 50/mm3. Based on
the results of these trials, the Department of Health and Human Services and Infectious Diseases
Society of America now recommend that antiretroviral treatment be started two weeks after
initiation of tuberculosis treatment for most patients with CD4 counts less than 50
cells/mm3.8Challenges of co-treatment of HIV and tuberculosis.
Concurrent treatment of tuberculosis and HIV is complicated by
the adherence challenges of polypharmacy,
overlapping side effect profiles of antituberculosis and antiretroviral drugs,
immune reconstitution inflammatory syndrome, and
drug-drug interactions.9
The focus of this document is the drug-drug interaction between rifamycin antibiotics (rifampin,
rifabutin, and rifapentine) and four classes of antiretroviral drugs: protease inhibitors, non-nucleoside
reverse-transcriptase inhibitors (NNRTI), CCR5-receptor antagonists, and integrase inhibitors.10, 11 Only
two of the currently available antiretroviral drug classes, the nucleoside/nucleotide analogues (NRTI)
[with the exception of zidovudine 12, 13] and the entry inhibitor enfuvirtide (given parenterally)14 are free
of clinically-significant interactions with the rifamycins. Although serum concentrations of the NRTI
zidovudine are diminished by co-administration of rifamycins, no dose adjustment is recommended as
the relationship between zidovudine plasma concentrations and efficacy is unclear.
Objectives of these guidelines.
The purpose of these guidelines is to provide the clinician with updated recommendations for
managing the drug-drug interactions that occur when using antiretroviral therapy during tuberculosis
treatment. (Table 1) Changes from previous versions of these guidelines include:
a summary of data from clinical trials regarding timing of initiation of antiretroviral therapy among
patients with tuberculosis;
drug interaction data for new antiretroviral drugs; and
changes in dosing guidelines for rifabutin when co-administered with protease inhibitors,
for nevirapine when co-administered with rifampin, and
for raltegravir when co-administered with rifampin.
more detailed recommendations regarding co-treatment of tuberculosis and HIV among children
and pregnant women
We include pharmacokinetic data as well as data about immunologic response and virologic
suppression (where available) for antiretroviral drugs that are licensed and available for use in the
United States when administered in combination with antituberculosis drugs.
Methodology for Preparation of these
Guidelines
These guidelines were developed by the HIV-TB Drug Interaction Guideline Development Group
(hereafter, Guideline Development Group). The Guideline Development Group consisted of experts
in tuberculosis and HIV treatment and pharmacokinetics from CDC and other institutions (see
listing of the Guideline Development Group at the end of this document on page 15). Members of
the Guideline Development Group were selected by the chair and co-chairs. They sought to include
as members some persons who had participated in preparation and review of the prior version of
these guidelines. Particular effort was made to include staff from the U.S. National Institutes of
Health (NIH), in order to coordinate these recommendations with those of the Federally-approved
HIV/AIDS medical practice guidelines available online at http://www.aidsinfo.nih.gov/. No
members of the Guideline Development Group were deemed to have substantial competing interests
related to the recommendations in these guidelines. Guideline Development Group member
competing interests are listed on page 16.
A literature search was conducted to extract articles that met the following inclusion criteria: clinical
studies involving healthy volunteers or patients with HIV or HIV/TB co-infection with relevant PK, safety,
or HIV (viral load suppression, change in CD4 count) endpoints. Our search strategy was as follows: (1)
between March 2011 and May 2012 we searched in Pubmed and Embase for English and French articles
published from 1990 to 2012. We used as MeSH terms tuberculosis, HIV, and the names of the
drugs being evaluated. (2) After articles were extracted and selected, we hand-searched references at
the end of include
S-ar putea să vă placă și
- Lichen Simplex Chronicus Is Induced by Rubbing and Scratching Secondary To ItchDocument1 paginăLichen Simplex Chronicus Is Induced by Rubbing and Scratching Secondary To ItchAgieÎncă nu există evaluări
- NMBDocument3 paginiNMBAgieÎncă nu există evaluări
- Giant Cell Fibroma of The Gingiva: A Case Report and Review of LiteratureDocument4 paginiGiant Cell Fibroma of The Gingiva: A Case Report and Review of LiteratureAgieÎncă nu există evaluări
- Jaga shift perawat dan dokter di rumah sakitDocument7 paginiJaga shift perawat dan dokter di rumah sakitAgieÎncă nu există evaluări
- Jaga shift perawat dan dokter di rumah sakitDocument7 paginiJaga shift perawat dan dokter di rumah sakitAgieÎncă nu există evaluări
- Jaga shift perawat dan dokter di rumah sakitDocument7 paginiJaga shift perawat dan dokter di rumah sakitAgieÎncă nu există evaluări
- Jaga shift perawat dan dokter di rumah sakitDocument7 paginiJaga shift perawat dan dokter di rumah sakitAgieÎncă nu există evaluări
- Jaga shift perawat dan dokter di rumah sakitDocument7 paginiJaga shift perawat dan dokter di rumah sakitAgieÎncă nu există evaluări
- MR 31 1Document10 paginiMR 31 1AgieÎncă nu există evaluări
- Jaga shift perawat dan dokter di rumah sakitDocument7 paginiJaga shift perawat dan dokter di rumah sakitAgieÎncă nu există evaluări
- Jaga shift perawat dan dokter di rumah sakitDocument7 paginiJaga shift perawat dan dokter di rumah sakitAgieÎncă nu există evaluări
- MR 31 1Document10 paginiMR 31 1AgieÎncă nu există evaluări
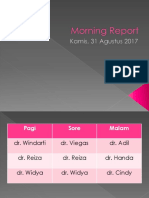
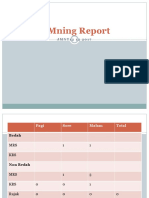
- Morning Report: Kamis, 31 Agustus 2017Document10 paginiMorning Report: Kamis, 31 Agustus 2017AgieÎncă nu există evaluări
- Jaga shift perawat dan dokter di rumah sakitDocument7 paginiJaga shift perawat dan dokter di rumah sakitAgieÎncă nu există evaluări
- Jaga shift perawat dan dokter di rumah sakitDocument7 paginiJaga shift perawat dan dokter di rumah sakitAgieÎncă nu există evaluări
- MR 31 1Document10 paginiMR 31 1AgieÎncă nu există evaluări
- MR 17 Sept 17Document7 paginiMR 17 Sept 17AgieÎncă nu există evaluări
- MR 3 9 17Document8 paginiMR 3 9 17AgieÎncă nu există evaluări
- MBDocument11 paginiMBAgieÎncă nu există evaluări
- MR 1lopDocument6 paginiMR 1lopAgieÎncă nu există evaluări
- Dengue FeverDocument1 paginăDengue FeverAgieÎncă nu există evaluări
- MRMNBDocument6 paginiMRMNBAgieÎncă nu există evaluări
- MRED 17 s12Document6 paginiMRED 17 s12AgieÎncă nu există evaluări
- Morning Report: Kamis, 31 Agustus 2017Document10 paginiMorning Report: Kamis, 31 Agustus 2017AgieÎncă nu există evaluări
- Mmning Report: J M N T 1 2 1 2 2 0 1 7Document6 paginiMmning Report: J M N T 1 2 1 2 2 0 1 7AgieÎncă nu există evaluări
- Morning Report: Jumat, 1 Desember 2017Document6 paginiMorning Report: Jumat, 1 Desember 2017AgieÎncă nu există evaluări
- Morning Report: Minggu, 3 September 2017Document8 paginiMorning Report: Minggu, 3 September 2017AgieÎncă nu există evaluări
- MR 3 9 17Document8 paginiMR 3 9 17AgieÎncă nu există evaluări
- MMDocument8 paginiMMAgieÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Liugong 938 Wheel Loader Parts ManualDocument20 paginiLiugong 938 Wheel Loader Parts Manualjonathan100% (49)
- Automated Crime Reporting SystemDocument101 paginiAutomated Crime Reporting SystemDeepak Kumar60% (10)
- UntitledDocument21 paginiUntitledRoberto RamosÎncă nu există evaluări
- Math 2 Curriculum GuideDocument19 paginiMath 2 Curriculum GuideMichelle Villanueva Jalando-onÎncă nu există evaluări
- ECE 4400 Performance Analysis Local Computer Networks HomeworkDocument2 paginiECE 4400 Performance Analysis Local Computer Networks HomeworkNguyen Phi HungÎncă nu există evaluări
- 4MB0 02R Que 20160609 PDFDocument32 pagini4MB0 02R Que 20160609 PDFakashÎncă nu există evaluări
- GEd 105 Midterm ReviewerDocument17 paginiGEd 105 Midterm ReviewerAndryl MedallionÎncă nu există evaluări
- Financial Reporting Statement Analysis Project Report: Name of The Company: Tata SteelDocument35 paginiFinancial Reporting Statement Analysis Project Report: Name of The Company: Tata SteelRagava KarthiÎncă nu există evaluări
- Asian Games African Games: Beach VolleyballDocument5 paginiAsian Games African Games: Beach VolleyballJessan Ybañez JoreÎncă nu există evaluări
- Painter CardDocument1 paginăPainter CardPraveen RANAÎncă nu există evaluări
- Vsip - Info - Ga16de Ecu Pinout PDF FreeDocument4 paginiVsip - Info - Ga16de Ecu Pinout PDF FreeCameron VeldmanÎncă nu există evaluări
- IntegrityDocument5 paginiIntegrityPritam Kumar100% (1)
- Valentine Gifting - Accessories EditionDocument25 paginiValentine Gifting - Accessories EditionPriyanath PaulÎncă nu există evaluări
- Utilization of Wood WasteDocument14 paginiUtilization of Wood WasteSalman ShahzadÎncă nu există evaluări
- OJT Form 03 Performance EvaluationDocument2 paginiOJT Form 03 Performance EvaluationResshille Ann T. SalleyÎncă nu există evaluări
- Osprey, Men-At-Arms #008 The Black Watch (1971) (-) OCR 8.12Document48 paginiOsprey, Men-At-Arms #008 The Black Watch (1971) (-) OCR 8.12mancini100% (4)
- DOW™ HDPE 05962B: High Density Polyethylene ResinDocument3 paginiDOW™ HDPE 05962B: High Density Polyethylene ResinFredo NLÎncă nu există evaluări
- Description MicroscopeDocument4 paginiDescription MicroscopeRanma SaotomeÎncă nu există evaluări
- 60Hz Axial-Fan Centrifugal-Fan AC EN (2009) PDFDocument136 pagini60Hz Axial-Fan Centrifugal-Fan AC EN (2009) PDFRodrigo GonçalvesÎncă nu există evaluări
- Adjutant-Introuvable BASIC VERSIONDocument7 paginiAdjutant-Introuvable BASIC VERSIONfurrypdfÎncă nu există evaluări
- Lake Isle of Innisfree Lesson Plan BV ZGDocument4 paginiLake Isle of Innisfree Lesson Plan BV ZGapi-266111651100% (1)
- Compabloc Manual NewestDocument36 paginiCompabloc Manual NewestAnonymous nw5AXJqjdÎncă nu există evaluări
- Big Band EraDocument248 paginiBig Band Erashiloh32575% (4)
- HIS 101 Home Work 2Document10 paginiHIS 101 Home Work 2Nabil HussainÎncă nu există evaluări
- Case Analysis of CriminologyDocument12 paginiCase Analysis of CriminologyinderpreetÎncă nu există evaluări
- Ips 350:400:450:500:600 07:05 PDFDocument124 paginiIps 350:400:450:500:600 07:05 PDFRandall PettersonÎncă nu există evaluări
- Padmavati Gora BadalDocument63 paginiPadmavati Gora BadalLalit MishraÎncă nu există evaluări
- Community Development A Critical Approach PDFDocument2 paginiCommunity Development A Critical Approach PDFNatasha50% (2)
- As 2710-1984 Screw Gauges - VerificationDocument7 paginiAs 2710-1984 Screw Gauges - VerificationSAI Global - APACÎncă nu există evaluări
- Johnson 1999Document20 paginiJohnson 1999Linh Hoàng PhươngÎncă nu există evaluări