Documente Academic
Documente Profesional
Documente Cultură
Ophthalmia Neonatorum
Încărcat de
Yhanna UlfianiTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Ophthalmia Neonatorum
Încărcat de
Yhanna UlfianiDrepturi de autor:
Formate disponibile
POSITION STATEMENT
Preventing ophthalmia neonatorum
Dorothy L Moore, Noni E MacDonald; Canadian Paediatric Society, Infectious Diseases and Immunization Committee
Infectious Diseases and Immunization Committee
Paediatr Child Health 2015;20(2):93-96
Posted: Mar 6 2015
diatric Societys Infectious Diseases and Immunization
Abstract Committee.[1] This update is indicated because in
The use of silver nitrate as prophylaxis for neonatal Canada, the epidemiology and antibiotic susceptibility
ophthalmia was instituted in the late 1800s to pre of Neisseria gonorrhoeae, as well as the availability of
vent the devastating effects of neonatal ocular in products for prophylaxis, have all changed, raising
fection with Neisseria gonorrhoeae. At that time concerns about the utility of the previously recom
during the preantibiotic era many countries made mended strategy.
such prophylaxis mandatory by law. Today, neona
tal gonococcal ophthalmia is rare in Canada, but Neonatal ophthalmia, a relatively common illness, is
ocular prophylaxis for this condition remains defined as conjunctivitis occurring within the first four
mandatory in some provinces/territories. Silver ni weeks of life.[2] Originally, this term only referred to
trate drops are no longer available and ery cases caused by N gonorrhoeae, but the term current
thromycin, the only ophthalmic antibiotic eye oint ly encompasses any conjunctivitis in this age group. N
ment currently available for use in newborns, is of gonorrhoeae now accounts for <1% of reported cases
questionable efficacy. Ocular prophylaxis is not ef of neonatal ophthalmia in the United States, while that
fective in preventing chlamydial conjunctivitis. Ap due to Chlamydia trachomatis ranges from 2% to 40%.
plying medication to the eyes of newborns may re Other bacteria such as Staphylococcus species, Strep
sult in mild eye irritation and has been perceived by tococcus species, Haemophilus species and other
some parents as interfering with mother-infant Gram- negative bacterial species account for 30% to
bonding. Physicians caring for newborns should ad 50% of cases.[2] Much less commonly, neonatal con
vocate for rescinding mandatory ocular prophylaxis junctivitis is caused by viral infections (herpes simplex,
laws. More effective means of preventing oph adenovirus, enteroviruses). Infectious conjunctivitis
thalmia neonatorum include screening all pregnant must be distinguished from eye discharge secondary
women for gonorrhea and chlamydia infection, and to blocked tear ducts and from conjunctivitis due to ex
treatment and follow-up of those found to be infect posure to chemical or other irritants.
ed. Mothers who were not screened should be test
ed at delivery. Infants of mothers with untreated In most instances, neonatal ophthalmia is a mild ill
gonococcal infection at delivery should receive cef ness. The exception is ophthalmia due to infection with
triaxone. Infants exposed to chlamydia at delivery N gonorrhoeae.[2] Without preventive measures, gono
should be followed closely for signs of infection. coccal ophthalmia occurs in 30% to 50% of infants ex
posed during delivery[3]-[5] and may progress quickly to
Key Words: Chlamydia; Gonococcus; Neonatal corneal ulceration, perforation of the globe and perma
ophthalmia; Prophylaxis; Screening in pregnancy; nent visual impairment.[6] Infants at increased risk for
STIs gonococcal ophthalmia are those whose mothers are
at risk for sexually transmitted infections (STIs).[7]
Historically, the purpose of prophylaxis for neonatal
ophthalmia was to prevent devastating neonatal eye
infection due to N gonorrhoeae. Silver nitrate prophy
The present statement replaces a statement on neona laxis against N gonorrhoeae ophthalmia neonatorum,
tal ophthalmia published in 2002 by the Canadian Pae first used by Dr Carl Cred in 1880,[6] was a significant
preventive medicine triumph at a time when there was
INFECTIOUS DISEASES AND IMMUNIZATION COMMITTEE, CANADIAN PAEDIATRIC SOCIETY | 1
no effective treatment available for gonorrhea. Never infants born to untreated mothers has been used in the
theless, silver nitrate was not a perfect agent because past but has not been recommended since the associ
it caused transient chemical conjunctivitis in 50% to ation between erythromycin and pyloric stenosis was
90% of infants.[8] Also, some parents were concerned recognized.[27] Routine prenatal screening for C tra
that the practice could interfere with mother-infant chomatis and treatment of identified infections during
bonding.[9] Silver nitrate eye drops are no longer avail pregnancy is the preferred option for preventing
able in Canada. Tetracycline and erythromycin oint neonatal conjunctivitis and other infections in new
ments have been considered to be acceptable alterna borns caused by this organism. Close clinical follow-up
tives for preventing gonococcal ophthalmia.[2][10] How of exposed infants is recommended.[2][28] The Public
ever, N gonorrhoeae strains isolated in Canada in Health Agency of Canada recommends testing con
2012 showed considerable resistance to these agents, junctival and nasopharyngeal secretions of sympto
with tetracycline at 30% and erythromycin at 23%.[11] matic infants and treating those who show positive re
Whether this resistance can be overcome by the high sults.[28]
local antibiotic levels achieved by topical application is
unknown, and there are no recent studies of the effica A recent meta-analysis concluded that evidence from
cy of ophthalmia prophylaxis with these agents. randomized and quasirandomized trials regarding the
efficacy of prophylactic agents used to prevent gono
In Canada, erythromycin has been the only antibiotic coccal and chlamydia conjunctivitis was not of high
eye ointment available for use in neonates since tetra quality. Moreover, all of the agents reviewed had clini
cycline ophthalmic ointment became unavailable. Povi cally significant failure rates.[18]
done-iodine has been considered for prophylaxis,[12]
but this agent may not be effective[13][14] and has been Rates of neonatal ophthalmia caused by N gonor
associated with a 5% rate of chemical conjunctivitis.[15] rhoeae and C trachomatis declined significantly in
Gentamicin ointment was used for newborn ocular pro North America through the 1980s due to the de
phylaxis during a shortage of erythromycin ointment in creased prevalence of these infections in the general
the United States in 2009, but resulted in reports of se population, and the institution of routine prenatal
vere ocular reactions.[16][17] Other ophthalmic antibiotic screening and treatment of these STIs in pregnancy.[18]
[19] In the United States in 2002, the rate of neonatal
preparations have not been evaluated in newborns.
Therefore, it is questionable whether universal ocular ophthalmia was 8.5 per 100,000 births.[18] National sur
prophylaxis for neonatal gonococcal ophthalmia re veillance of neonatal ophthalmia was discontinued in
mains an effective option in Canada. Of note, universal Canada in 2000 because of low incidence.[29] Current
ocular prophylaxis was abandoned decades ago in rates of infection can be estimated from reported cas
several high-income countries including Denmark, Nor es of chlamydia and gonorrhea in infants <1 year of
way, Sweden and the United Kingdom. One study from age, for whom the average national rate between 2000
the United Kingdom showed that this change did not and 2011 was six per 100,000 for chlamydia infection
increase the rate of blindness due to gonococcal oph and 0.5 per 100,000 for gonorrhea.[30] In Ontario, the
thalmia.[18] However, the Canadian Medical Protective combined rate of chlamydia and gonococcal oph
Association established that in 2013, neonatal ocular thalmia in 2004 was 4.5 per 100,000.[18] There were no
prophylaxis was required by law in Alberta, British Co reported cases of neonatal gonococcal ophthalmia in
lumbia, Ontario, Prince Edward Island and Quebec. In Alberta between 2005 and 2013, but rates of chlamydi
British Columbia, prophylaxis may be waived if a par al ophthalmia ranged from 0 to 12.2 per 100,000 per
ent makes a written request. In New Brunswick, the year, with a reported rate of 7.5 per 100,000 in 2013.
[31] In areas of the world where prenatal screening and
law requiring prophylaxis was repealed in 2009. No
current legislation was found for the remaining treatment are not available and prevalence of gono
provinces and territories.[19][20] coccal infections is high, vision loss from neonatal
gonococcal ophthalmia continues to occur and ocular
Infants born to women with untreated chlamydia infec prophylaxis with silver nitrate continues to be an impor
tion at delivery have a 50% risk of acquiring chlamydia, tant and cost-effective intervention.[4][32]
a 30% to 50% risk of developing neonatal conjunctivitis
and a 10% to 20% risk of developing chlamydia pneu If ocular prophylaxis must be given to comply with
monia.[21] Topical ocular prophylaxis does not prevent provincial/territorial regulations, 0.5% erythromycin
transmission from mother to infant, does not reliably base can be used and may be effective in some cases,
prevent neonatal conjunctivitis and does not prevent depending on the antibiotic sensitivity of circulating
pneumonia.[10][22]-[26] Oral erythromycin prophylaxis of strains. Povidone-iodine or gentamicin ointment should
2 | PREVENTING OPHTHALMIA NEONATORUM
not be used because of high rates of adverse topical trimester.[2][7][28][33] Rescreening for N gonorrhoeae,
effects.[2][7] To prevent potential cross-contamination, C trachomatis and other STIs should be considered
single-use tubes of erythromycin are used. Before ad in the third trimester for women who are not in a
ministration, each eyelid is wiped gently with sterile stable monogamous relationship.
cotton to remove foreign matter and to permit ade
quate eversion of the lower lid. A line of antibiotic oint Processes should be in place to ensure communi
ment, sufficiently long to cover the entire lower con cation between physicians and others caring for a
junctival area, is placed in each lower conjunctival sac, woman during pregnancy, and those who will care
taking care to prevent injury to the eye or the eyelid for her newborn. Information regarding maternal
from the tip of the tube. The closed eyelids are mas STI screening, treatment and risk factors is crucial
saged gently to help spread the ointment. After 1 min, to the well-being of the newborn, and must be
excess ointment is gently wiped from the eyelids and available to all health care providers caring for the
surrounding skin with sterile cotton. newborn at and following delivery.
Pregnant women who were not screened during
Recommendations pregnancy should be screened for N gonorrhoeae
To prevent neonatal ophthalmia caused by N gonor and C trachomatis at delivery, using the most rapid
rhoeae and C trachomatis, the Canadian Paediatric tests available.[7][28]
Society recommends the following:
Managing newborns exposed to N gonorrhoeae:
Neonatal ocular prophylaxis:
A system should be established to ensure that all
Neonatal ocular prophylaxis with erythromycin, the infants born to mothers found to have untreated N
only agent currently available in Canada for this gonorrhoeae infection at delivery are treated.
purpose, may no longer be useful and, therefore,
should not be routinely recommended.
Paediatricians and other physicians caring for new
borns, along with midwives and other health care
providers, should become familiar with local legal
requirements concerning ocular prophylaxis.
Paediatricians and other physicians caring for new
borns should advocate to rescind ocular prophylax
is regulations in jurisdictions in which this is still
legally mandated.
Jurisdictions in which ocular prophylaxis is still
mandated should assess their current rates of
neonatal ophthalmia and consider other, more ef
fective preventive strategies, as outlined below.
Screening and treatment of pregnant women:
All pregnant women should be screened for N gon
orrhoeae and C trachomatis infections at the first
prenatal visit.
Those who are infected should be treated during
pregnancy, tested after treatment to ensure thera
peutic success and tested again in the third
trimester or, failing that, at time of delivery. Their
partners should also be treated. Women who test
negative but are at risk for acquiring infection later
in pregnancy should be screened again in the third
INFECTIOUS DISEASES AND IMMUNIZATION COMMITTEE, CANADIAN PAEDIATRIC SOCIETY | 3
If the mothers test results are not available at dis Acknowledgements
charge, a plan must be in place to ensure that she
This statement has been reviewed by the Community
can be contacted promptly if the results are posi
Paediatrics and Fetus and Newborn Committees of the
tive. The mother must also be advised to watch her
Canadian Paediatric Society, as well as by the Public
infant for eye discharge in the first week of life and
Health Agency of Canadas Canadian STI Guidelines
told whom to contact immediately if this symptom
Expert Working Group and representatives from the
develops, or if the child is unwell in any way. When
Society of Obstetricians and Gynaecologists of Cana
there is doubt about maternal compliance with this
da.
recommendation and the mother is considered to
be at risk for gonococcal infection, administering
one dose of ceftriaxone should be considered for References
the infant before discharge. 1. Canadian Paediatric Society, Infectious Diseases and
Immunization Committee. Recommendations for the
Infants born to women with untreated N gonor prevention of neonatal ophthalmia. Paediatr Child
rhoeae infection at the time of delivery, including Health 2002;7(7):480-3.
those born by Caesarian section,[34] should be test 2. American Academy of Pediatrics. Prevention of neonatal
ophthalmia. In: Pickering LK, Baker CJ, Kimberlin DW,
ed and treated immediately without waiting for test
Long SS, eds. Red Book: 2012 Report of the Committee
results.[28] on Infectious Diseases, 29th ed. Elk Grove Village, IL.
Infants exposed to N gonorrhoeae who appear American Academy of Pediatrics, 2012:880-2.
to be healthy at birth, both term and preterm, 3. Laga M, Plummer FA, Nzanze H, et al. Epidemiology of
should have a conjunctival culture for N gonor ophthalmia neonatorum in Kenya. Lancet 1986;2(8516):
rhoeae and receive a single dose of ceftriaxone 1145-9.
(50 mg/kg to a maximum of 125 mg) intra 4. Galega FP, Heymann DL, Nasah BT. Gonococcal oph
venously or intramuscularly. The preferred dilu thalmia neonatorum: The case for prophylaxis in tropical
ent for intramuscular ceftriaxone is 1% lidocaine Africa. Bull World Health Organ 1984;62(1):95-8
5. Davidson HH, Hill JH, Eastman NJ. Penicillin in the pro
without epinephrine (0.45 mL/125 mg). This in
phylaxis of ophthalmia neonatorum. J Am Med Assoc
tervention is both safe and effective. Biliary sta 1951;145(14):1052-5.
sis from ceftriaxone is not considered to be a 6. Forbes GB, Forbes GM. Silver nitrate and the eye of the
risk with a single dose. (Ceftriaxone is con newborn. Creds contribution to preventive medicine.
traindicated in newborns receiving intravenous Am J Dis Child 1971;121(1):1-3.
calcium. A single dose of cefotaxime [100 mg/kg 7. U.S. Centers for Disease Control and Prevention. Sexu
given intravenously or intramuscularly] is an ac ally transmitted diseases treatment guidelines, 2010.
ceptable alternative.) MMWR 2010;59(No. RR-12): http://www.cdc.gov/std/
treatment/2010/default.htm (Accessed November 27,
If the exposed infant is unwell in any way, blood 2014).
and cerebrospinal fluid cultures should also be 8. Nishida H, Risenberg HM. Silver nitrate ophthalmic solu
performed. Infants with established gonococcal tion and chemical conjunctivities. Pediatrics 1975;56(3):
368-73.
disease require additional investigation and
9. Butterheld PM, Emdh RN, Svejda MJ. Does the early
therapy in consultation with a specialist in pae application of silver nitrate impair maternal attachment?
diatric infectious diseases.[2][7][28] Pediatrics 1981;67(5):737-8.
10. Laga M, Plummer FA, Piot P, et al. Prophylaxis of gono
Managing newborns exposed to C trachomatis: coccal and chlamydial ophthalmia neonatorum. A com
parison of silver nitrate and tetracycline. N Engl J Med
Infants born either vaginally or by Caesarian sec 1988;318(11):653-7.
tion to mothers with an untreated chlamydia infec 11. Public Health Agency of Canada, National Microbiology
tion should be closely monitored for symptoms (eg, Laboratory. National surveillance of antimicrobial sus
conjunctivitis, pneumonitis) and treated if infection ceptibilities of Neisseria gonorrhoeae. Annual Summary
occurs.[2][7][28] Routine cultures should not be per 2012: http://publications.gc.ca/collections/collec
tion_2014/aspc-phac/HP57-3-2012-eng.pdf (Accessed
formed on asymptomatic infants.
November 27, 2014).
Prophylaxis of exposed newborns is not recom 12. Isenberg SJ, Apt L, Wood M. A controlled trial of povi
mended because of the association of macrolides done-iodine as prophylaxis against ophthalmia neonato
rum. N Engl J Med 1995;332(9):562-6.
with pyloric stenosis, but may be considered when 13. Ali Z, Khadije D, Elahe A, Mohammad M, Fateme Z,
infant follow-up cannot be guaranteed.[7][28] Narges Z. Prophylaxis of ophthalmia neonatorum com
4 | PREVENTING OPHTHALMIA NEONATORUM
parison of betadine, erythromycin and no prophylaxis. J ing for newborns exposed to Chlamydia trachomatis.
Trop Pediatr 2007; 53(6):388-92. Arch Pediatr Adolesc Med 2003;157(6):565-71.
14. Ramirez-Ortiz MA, Rodriguez-Almaraz M, Ochoa-Dia 28. Public Health Agency of Canada, Centre for Communi
zlopez H, Diaz-Prieto P, Rodriguez-Surez RS. Ran cable Diseases and Infection Control. Canadian guide
domised equivalency trial comparing 2.5% povidone-io lines on sexually transmitted infections: The evergreen
dine drops and ophthalmic chloramphenicol for prevent edition. Updated January 2010: http://www.phac-
ing neonatal conjunctivitis in a trachoma endemic area aspc.gc.ca/std-mts/sti-its/guide-lignesdir-eng.php (Ac
in southern Mexico. Br J Ophthalmol 2007;91(11): cessed November 27, 2014).
1430-4. 29. Public Health Agency of Canada. Notifiable Diseases
15. David M, Rumelt S, Weintraub Z. Efficacy comparison On-Line. Gonococcal ophthalmia neonatorum. Number
between povidone iodine 2.5% and tretracycline 1% in of Reported Cases, Canada, 1990 to 1999. Accessed
prevention of ophthalmia neonatorum. Ophthalmology November 27, 2014.
2011;118(7):1454-8. 30. Public Health Agency of Canada. Notifiable Diseases
16. Binenbaum G, Bruno CJ, Forbes BJ, et al. Periocular ul On-Line: http://dsol-smed.phac-aspc.gc.ca/dsol-smed/
cerative dermatitis associated with gentamicin ointment ndis/charts.php?c=gb (Accessed November 27, 2014).
prophylaxis in newborns. J Pediatr 2010;156(2):320-1. 31. Alberta Health Services, Centralized STI Services, Feb
17. Nathawad R, Mendez H, Ahmad A, et al. Severe ocular ruary 2014, personal communication.
reactions after neonatal ocular prophylaxis with gentam 32. Laga M, Meheus A, Piot P. Epidemiology and control of
icin ophthalmic ointment. Pediatr Infect Dis J 2011;30(2): gonococcal ophthalmia neonatorum. Bull World Health
175-6. Organ 1989;67(5):471-8.
18. Darling EK, McDonald H. A meta-analysis of the efficacy 33. Public Health Agency of Canada. Canadian guidelines
of ocular prophylactic agents used for the prevention of on sexually transmitted infections. Supplementary state
gonococcal and chlamydial ophthalmia neonatorum. J ment for recommendations related to the diagnosis,
Midwifery Womens Health 2010;55(4):319-27. management, and follow-up of pregnant women. March
19. Gray J. Executive Director, Canadian Medical Protective 2014: http://www.phac-aspc.gc.ca/std-mts/sti-its/cgsti-ld
Agency. June 2013. Personal communication. cits/preg-ence-eng.php (Accessed November 27, 2014).
20. Wong T. Director, Professional Guidelines and Public 34. Diener B. Cesarean section complicated by gonococcal
Health Practice Division, Centre for Communicable Dis ophthalmia neonatorum. J Fam Pract 1981;13(5):
eases and Infection Control, Public Health Agency of 739-44.
Canada. June 2013, Personal communication.
21. Hammerschlag MR. Chlamydial and gonococcal infec CPS INFECTIOUS DISEASES AND IMMUNIZATION
tions in infants and children. Clin Infect Dis COMMITTEE
2011;53(Suppl 3):S99-102. Members: Natalie A Bridger MD; Jane C Finlay MD
22. Rettig PJ, Patamasucon P, Siegal JD. Postnatal prophy (past member); Susanna Martin MD (Board Represen-
laxis of chlamydial conjunctivitis. JAMA 1981;246(20):
tative); Jane C McDonald MD; Heather Onyett MD;
2321-2.
23. Bell TA, Sandstrm KI, Gravett MG, et al. Comparison of Joan L Robinson MD (Chair); Marina I Salvadori MD
ophthalmic silver nitrate solution and erythromycin oint (past member); Otto G Vanderkooi MD
ment for prevention of natally acquired Chlamydia tra Liaisons: Upton D Allen MBBS, Canadian Pediatric
chomatis. Sex Transm Dis 1987;14(4):195-200. AIDS Research Group; Michael Brady MD, Committee
24. Chen JY. Prophylaxis of ophthalmia neonatorum: Com on Infectious Diseases, American Academy of Pedi-
parison of silver nitrate, tetracycline, erythromycin and atrics; Charles PS Hui MD, Committee to Advise on
no prophylaxis. Pediatr Infect Dis J 1992;11(12): Tropical Medicine and Travel (CATMAT), Public Health
1026-30. Agency of Canada; Nicole Le Saux MD, Immunization
25. Hammerschlag MR, Cummings C, Roblin PM, Williams
TH, Delke I. Efficacy of neonatal ocular prophylaxis for
Monitoring Program, ACTive (IMPACT); Dorothy L
the prevention of chlamydial and gonococcal conjunctivi Moore MD, National Advisory Committee on Immu-
tis. N Engl J Med 1989;320(12):769-72. nization (NACI); Nancy Scott-Thomas MD, College of
26. Black-Payne C, Bocchini JA Jr, Cedotal C. Failure of Family Physicians of Canada; John S Spika MD, Pub-
erythromycin ointment for postnatal ocular prophylaxis lic Health Agency of Canada
of chlamydial conjunctivitis. Pediatr Infect Dis J Consultant: Noni E MacDonald MD
1989;8(8):491-5. Principal authors: Dorothy L Moore MD, Noni E Mac-
27. Rosenman MB, Mahon BE, Downs SM, Kleiman MB. Donald MD
Oral erythromycin prophylaxis vs watchful waiting in car
Also available at www.cps.ca/en
Canadian Paediatric Society 2017
The Canadian Paediatric Society gives permission to print single copies of this document from our website. Disclaimer: The recommendations in this position statement do not indicate an
For permission to reprint or reproduce multiple copies, please see our copyright policy. INFECTIOUS DISEASES AND IMMUNIZATION COMMITTEE,
exclusive course ofCANADIAN PAEDIATRIC
treatment or procedure SOCIETY
to be followed. | 5 taking in
Variations,
to account individual circumstances, may be appropriate. Internet addresses
are current at time of publication.
S-ar putea să vă placă și
- Problems with the Power: Dystocia Causes and Nursing ManagementDocument3 paginiProblems with the Power: Dystocia Causes and Nursing ManagementJP Porras Ali100% (1)
- Live Preterm Baby Delivered NSDDocument13 paginiLive Preterm Baby Delivered NSDKristine Anne SorianoÎncă nu există evaluări
- Maternal and Child Health Nursing: Acute Conditions of the NewbornDocument70 paginiMaternal and Child Health Nursing: Acute Conditions of the NewbornSam PothÎncă nu există evaluări
- Transient Tachypnea of NewbornsDocument16 paginiTransient Tachypnea of NewbornsSelena Marie0% (1)
- SDL - 4.pdf AnotherDocument3 paginiSDL - 4.pdf AnotherJose Troy NgoaÎncă nu există evaluări
- Pneumonia in Children: Symptoms, Causes, TreatmentDocument4 paginiPneumonia in Children: Symptoms, Causes, TreatmentkuterinbatÎncă nu există evaluări
- 6-Health Problems Common in PreschoolerDocument36 pagini6-Health Problems Common in PreschoolerPam Lala100% (2)
- PolyhydramniosDocument2 paginiPolyhydramniosNathaniel RemandabanÎncă nu există evaluări
- NCM 107 FINALS Growth and DevelopmentDocument5 paginiNCM 107 FINALS Growth and DevelopmentDWIGHT LESTER O. MANGILAÎncă nu există evaluări
- Newborn Care: Establish Respiration and Maintain Clear AirwayDocument10 paginiNewborn Care: Establish Respiration and Maintain Clear Airwaysneb1392Încă nu există evaluări
- The High-Risk Pregnant Client:: NCM 109 Handout # 1Document3 paginiThe High-Risk Pregnant Client:: NCM 109 Handout # 1ApRil Anne BalanonÎncă nu există evaluări
- Compiled By: Lorie Noval Paclipan, MPH, RN: Newborn Screening in The PhilippinesDocument94 paginiCompiled By: Lorie Noval Paclipan, MPH, RN: Newborn Screening in The PhilippinesRovenick SinggaÎncă nu există evaluări
- Intrauterine Growth RestrictionDocument5 paginiIntrauterine Growth RestrictionColleen MercadoÎncă nu există evaluări
- Pregnancy Induced Hypertension Case StudyDocument4 paginiPregnancy Induced Hypertension Case StudyMae Arra Lecobu-anÎncă nu există evaluări
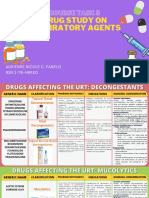
- Respiratory Drug Study GuideDocument23 paginiRespiratory Drug Study GuideAdrienne Nicole PaneloÎncă nu există evaluări
- HANDOUT Chapter 11 Promoting Fetal and Maternal HealthDocument7 paginiHANDOUT Chapter 11 Promoting Fetal and Maternal HealthClouiseÎncă nu există evaluări
- Episiotomy Wound Haematoma: Recognition, Management and Healing Assessment by REEDA Scale in Postpartum PeriodDocument4 paginiEpisiotomy Wound Haematoma: Recognition, Management and Healing Assessment by REEDA Scale in Postpartum PeriodIOSRjournalÎncă nu există evaluări
- MCH BulletsDocument13 paginiMCH BulletsPatziedawn GonzalvoÎncă nu există evaluări
- Transient Tachypnea of The NewbornDocument2 paginiTransient Tachypnea of The Newbornjulesubayubay5428Încă nu există evaluări
- Idiopathic Thrombocytopenic Purpura: Overview With Report of A CaseDocument4 paginiIdiopathic Thrombocytopenic Purpura: Overview With Report of A CaseHernan GonzalezÎncă nu există evaluări
- Child's Abdominal Pain Admitting ConferenceDocument24 paginiChild's Abdominal Pain Admitting ConferenceRaul MangrobangÎncă nu există evaluări
- Chapter 025 PSDocument10 paginiChapter 025 PSSalea Fleur TaverronÎncă nu există evaluări
- The Expanded Program On ImmunizationDocument4 paginiThe Expanded Program On Immunizationapi-3745792100% (3)
- Infant of Diabetic MotherDocument14 paginiInfant of Diabetic MothersreekalaÎncă nu există evaluări
- Abortion and Ectopic PregnancyDocument3 paginiAbortion and Ectopic PregnancyJefelson Eu Palaña NahidÎncă nu există evaluări
- Pathophysiology of Abortion Case Study (Vizconde, Ehreiz Raiden C. BSN2-A)Document4 paginiPathophysiology of Abortion Case Study (Vizconde, Ehreiz Raiden C. BSN2-A)Raiden VizcondeÎncă nu există evaluări
- Newborn Journal PDFDocument8 paginiNewborn Journal PDFRose Ann ManalastasÎncă nu există evaluări
- Fluid Volume Deficit and Excess: Types, Causes, Signs and Nursing ManagementDocument32 paginiFluid Volume Deficit and Excess: Types, Causes, Signs and Nursing ManagementAcohCChaoÎncă nu există evaluări
- HypertensionDocument6 paginiHypertensionTj Kevin P-DoctorÎncă nu există evaluări
- HES 032 BSN - Lab Comprehensive ExamDocument40 paginiHES 032 BSN - Lab Comprehensive ExamDIAZ, GIANNA D.Încă nu există evaluări
- Obstetric Nursing Care PlanDocument12 paginiObstetric Nursing Care PlanJass Mira Bueno100% (1)
- PPH Introduction 1Document95 paginiPPH Introduction 1regine maeÎncă nu există evaluări
- Pre and Post PregnancyDocument23 paginiPre and Post PregnancyJitendra ChaudharyÎncă nu există evaluări
- Treating Pneumonia in Children Under 5Document38 paginiTreating Pneumonia in Children Under 5Arjumand AliÎncă nu există evaluări
- Ectopic Pregnancy - PathophysiologyDocument1 paginăEctopic Pregnancy - PathophysiologyMarimiel PagulayanÎncă nu există evaluări
- 8. Care of Child With GI Dysfunction (1) ءءءءDocument44 pagini8. Care of Child With GI Dysfunction (1) ءءءءNuhaÎncă nu există evaluări
- Pharmacologic management of bleomycinDocument1 paginăPharmacologic management of bleomycinKim ApuradoÎncă nu există evaluări
- Idiopathic Thrombocytopenic Purpura (ITP)Document7 paginiIdiopathic Thrombocytopenic Purpura (ITP)Rizqka PertiwiÎncă nu există evaluări
- Nursing Assessment, Planning, Implementation and EvaluationDocument2 paginiNursing Assessment, Planning, Implementation and EvaluationDiana MuañaÎncă nu există evaluări
- Idiophatic Thrombocytopenic Purpura (ITP) in PregnancyDocument27 paginiIdiophatic Thrombocytopenic Purpura (ITP) in PregnancyAdietya Bima PrakasaÎncă nu există evaluări
- Chapter 19: Nutritional Needs of A NewbornDocument13 paginiChapter 19: Nutritional Needs of A NewbornAlyssaGrandeMontimorÎncă nu există evaluări
- Unit VIII PRESUMPTIVE SIGNS AND SYMPTOMS OF PREGNANCYDocument5 paginiUnit VIII PRESUMPTIVE SIGNS AND SYMPTOMS OF PREGNANCYNancy100% (1)
- Pregnancy Induced Hypertension PihDocument17 paginiPregnancy Induced Hypertension PihRose DeymÎncă nu există evaluări
- Neonatal Jaundice Case Study: Early Diagnosis and Treatment Prevents Brain DamageDocument6 paginiNeonatal Jaundice Case Study: Early Diagnosis and Treatment Prevents Brain DamagemuzamirÎncă nu există evaluări
- Epilepsy in Pregnancy JatuDocument57 paginiEpilepsy in Pregnancy Jatuninjahattori1Încă nu există evaluări
- Case Simulation 118Document4 paginiCase Simulation 118Rica AvendañoÎncă nu există evaluări
- Case Study, Chapter 42, Management of Patients With Musculoskeletal TraumaDocument2 paginiCase Study, Chapter 42, Management of Patients With Musculoskeletal TraumaAhmad BaolayyanÎncă nu există evaluări
- Obstetric Case Study CesarianDocument16 paginiObstetric Case Study CesarianRazan NasereddineÎncă nu există evaluări
- The Expanded Program On ImmunizationDocument5 paginiThe Expanded Program On ImmunizationLovelyn B. OliverosÎncă nu există evaluări
- Spontaneous AbortionDocument17 paginiSpontaneous Abortionanon_985338331Încă nu există evaluări
- The Child With Hematologic DisordersDocument149 paginiThe Child With Hematologic DisordersNics FranciscoÎncă nu există evaluări
- Midterms-NCM-109-Pedia-Lec-Dean (Repaired)Document28 paginiMidterms-NCM-109-Pedia-Lec-Dean (Repaired)Drannel FajardoÎncă nu există evaluări
- Eclampsia Nursing Case AnalysisDocument38 paginiEclampsia Nursing Case AnalysisMary Justine Nuyad-AfricaÎncă nu există evaluări
- Cemonc: Esmas, Lexi MCN 2 Le 1 1Document8 paginiCemonc: Esmas, Lexi MCN 2 Le 1 1EmpieÎncă nu există evaluări
- Uterine Atony: Group 3Document23 paginiUterine Atony: Group 3Trisha Mae MarquezÎncă nu există evaluări
- 1 - Presentation - Management of Preclamplsia, Mild and ModerateDocument22 pagini1 - Presentation - Management of Preclamplsia, Mild and ModeratesharonÎncă nu există evaluări
- Acute Management of Burns in ChildrenDocument52 paginiAcute Management of Burns in ChildrenJonie Vince SañosaÎncă nu există evaluări
- MCN Test DrillsDocument20 paginiMCN Test DrillsFamily PlanningÎncă nu există evaluări
- Transient Tachypnea of the Newborn (TTNDocument6 paginiTransient Tachypnea of the Newborn (TTNWivan Havilian DjohanÎncă nu există evaluări
- Personal Treatment PneumoniaDocument19 paginiPersonal Treatment PneumoniaYhanna UlfianiÎncă nu există evaluări
- Funding Plan for Practice Facilities ProgramDocument7 paginiFunding Plan for Practice Facilities ProgramYhanna UlfianiÎncă nu există evaluări
- Funding Plan for Practice Facilities ProgramDocument7 paginiFunding Plan for Practice Facilities ProgramYhanna UlfianiÎncă nu există evaluări
- Chapter 4. Developing Your Practice Facilitation Approach: Create A Key-Driver Model For Your PF InterventionDocument15 paginiChapter 4. Developing Your Practice Facilitation Approach: Create A Key-Driver Model For Your PF InterventionYhanna UlfianiÎncă nu există evaluări
- Developing and Running A Primary Care Practice Facilitation ProgramDocument139 paginiDeveloping and Running A Primary Care Practice Facilitation ProgramYhanna Ulfiani100% (1)
- Thoracic Outlet Syndrome: The ProblemDocument6 paginiThoracic Outlet Syndrome: The ProblemDavid SugiartoÎncă nu există evaluări
- Personal Treatment PneumoniaDocument19 paginiPersonal Treatment PneumoniaYhanna UlfianiÎncă nu există evaluări
- Chapter 3. Funding Your Practice Facilitation ProgramDocument10 paginiChapter 3. Funding Your Practice Facilitation ProgramYhanna UlfianiÎncă nu există evaluări
- Kehamilan MolaDocument88 paginiKehamilan MolaYhanna UlfianiÎncă nu există evaluări
- Mapping Konsep Ovary CystDocument1 paginăMapping Konsep Ovary CystYhanna UlfianiÎncă nu există evaluări
- RCOG Guidelines - Gestational Trophoblastic DiseaseDocument12 paginiRCOG Guidelines - Gestational Trophoblastic Diseasemob3100% (1)
- Neonatal KonjunctivitisDocument5 paginiNeonatal KonjunctivitisYhanna UlfianiÎncă nu există evaluări
- Multiple Cyst Lung StudyDocument11 paginiMultiple Cyst Lung StudyYhanna UlfianiÎncă nu există evaluări
- ProoksidanDocument11 paginiProoksidanYhanna UlfianiÎncă nu există evaluări
- PCOS Algorithm 5 From Evidence Based Guidelines PDFDocument1 paginăPCOS Algorithm 5 From Evidence Based Guidelines PDFYhanna UlfianiÎncă nu există evaluări
- BPHDocument1 paginăBPHYhanna UlfianiÎncă nu există evaluări
- PCOS Algorithm 5 From Evidence Based Guidelines PDFDocument1 paginăPCOS Algorithm 5 From Evidence Based Guidelines PDFYhanna UlfianiÎncă nu există evaluări
- Kimmel Et Al-1995-Developmental Dynamics PDFDocument58 paginiKimmel Et Al-1995-Developmental Dynamics PDFallisonmperezÎncă nu există evaluări
- Sept2011 Algorithms PDFDocument16 paginiSept2011 Algorithms PDFYhanna UlfianiÎncă nu există evaluări
- Neck MassesDocument7 paginiNeck MassesSaad AbdullahÎncă nu există evaluări
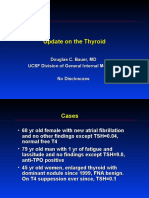
- Follikular TiroidDocument9 paginiFollikular TiroidYhanna UlfianiÎncă nu există evaluări
- Radioiodine Is Indicated For The Treatment of HyperDocument3 paginiRadioiodine Is Indicated For The Treatment of HyperYhanna UlfianiÎncă nu există evaluări
- 2-Update On The Thyroid. Doug Bauer, MDDocument41 pagini2-Update On The Thyroid. Doug Bauer, MDYhanna UlfianiÎncă nu există evaluări
- Diagnostic Imaging - Appendiceal Intussusception Into Cecum - 2013-06-04Document7 paginiDiagnostic Imaging - Appendiceal Intussusception Into Cecum - 2013-06-04Yhanna UlfianiÎncă nu există evaluări
- Diagnostic Imaging - Appendiceal Intussusception Into Cecum - 2013-06-04Document7 paginiDiagnostic Imaging - Appendiceal Intussusception Into Cecum - 2013-06-04Yhanna UlfianiÎncă nu există evaluări
- Recent Antihypertension Drugs in Preeclampsia PDFDocument31 paginiRecent Antihypertension Drugs in Preeclampsia PDFYhanna UlfianiÎncă nu există evaluări
- Zebrafish AssayDocument8 paginiZebrafish AssayYhanna UlfianiÎncă nu există evaluări
- Dizziness Diagnosis ApproachDocument1 paginăDizziness Diagnosis ApproachYhanna UlfianiÎncă nu există evaluări
- Konsep Ovary CystDocument1 paginăKonsep Ovary CystYhanna UlfianiÎncă nu există evaluări
- Hand Trauma: Illustrated Surgical Guide of Core Procedures: Dariush NikkhahDocument1 paginăHand Trauma: Illustrated Surgical Guide of Core Procedures: Dariush NikkhahMastoid AntrumÎncă nu există evaluări
- Summary of Product Characteristics: 4.1 Therapeutic IndicationsDocument3 paginiSummary of Product Characteristics: 4.1 Therapeutic IndicationsasdwasdÎncă nu există evaluări
- Nurse Patient Ratio PDFDocument7 paginiNurse Patient Ratio PDFSafrina WaldiniÎncă nu există evaluări
- Ssa 3368Document14 paginiSsa 3368JonOstiguyÎncă nu există evaluări
- Covid Vaccination Vs MortalityDocument7 paginiCovid Vaccination Vs MortalityashilÎncă nu există evaluări
- Values of Participating in Physical ActivityDocument10 paginiValues of Participating in Physical ActivityHana Landingin100% (1)
- !!!!!! Black StainsDocument7 pagini!!!!!! Black StainsGhimpu DanielaÎncă nu există evaluări
- 11-Rely Too Much On DoctorsDocument3 pagini11-Rely Too Much On DoctorsThu TrangÎncă nu există evaluări
- DentalCertificate DULDULAODocument5 paginiDentalCertificate DULDULAORolan Domingo GalamayÎncă nu există evaluări
- P.Chitra Resume PDFDocument2 paginiP.Chitra Resume PDFSam rajÎncă nu există evaluări
- Grade 10-Health-Quarter 1 Lesson 3Document40 paginiGrade 10-Health-Quarter 1 Lesson 3eric manuevo100% (1)
- SHN ObjectivesDocument3 paginiSHN Objectivescherie_92989Încă nu există evaluări
- Psychosocial Considerations For Children and Adolescents Living With Rare DiseasesDocument206 paginiPsychosocial Considerations For Children and Adolescents Living With Rare DiseasesAtif AvdovićÎncă nu există evaluări
- Administering Intramuscular Injection StepsDocument3 paginiAdministering Intramuscular Injection StepsJela Jane ArcalÎncă nu există evaluări
- Example: Family Medicine Structured Reference LetterDocument3 paginiExample: Family Medicine Structured Reference LetterHayder Al-TukmachiÎncă nu există evaluări
- Miliaria Pustulosa (Infetrop)Document11 paginiMiliaria Pustulosa (Infetrop)Muhammad mukramÎncă nu există evaluări
- RFID Technology in Outpatient Logistics: An Analysis of Its Potential and AcceptanceDocument92 paginiRFID Technology in Outpatient Logistics: An Analysis of Its Potential and AcceptanceBurak Onurlu100% (1)
- Centre for Innovations in Public Systems - Health Automation in RajasthanDocument4 paginiCentre for Innovations in Public Systems - Health Automation in RajasthanDurgeshTiwariÎncă nu există evaluări
- Nursing InformaticsDocument50 paginiNursing InformaticsAlec AnonÎncă nu există evaluări
- 3 Tracking Treatment Success With VEPDocument1 pagină3 Tracking Treatment Success With VEPANDREC CORPORATIONÎncă nu există evaluări
- Pep 2021 - October QuestionsDocument4 paginiPep 2021 - October QuestionsCynthia ObiÎncă nu există evaluări
- OphthalmologyDocument69 paginiOphthalmologyjatavÎncă nu există evaluări
- Full Version in PDF (Pashto/Dari & English) : DVD University Author Name of The Book No I. P.C.BDocument4 paginiFull Version in PDF (Pashto/Dari & English) : DVD University Author Name of The Book No I. P.C.BDrMohib Habibzai100% (1)
- Guide to Implementing Medicine Use EvaluationsDocument26 paginiGuide to Implementing Medicine Use EvaluationsmrboredguyÎncă nu există evaluări
- (Medicine and Biomedical Sciences in Modern History) Ornella Moscucci (Auth.) - Gender and Cancer in England, 1860-1948-Palgrave Macmillan UK (2016)Document347 pagini(Medicine and Biomedical Sciences in Modern History) Ornella Moscucci (Auth.) - Gender and Cancer in England, 1860-1948-Palgrave Macmillan UK (2016)Federico AnticapitalistaÎncă nu există evaluări
- Gcu Nrs410 Week 4 Assignment Benchmark Nursing Process Approach To Care Latest 2019 JulyDocument3 paginiGcu Nrs410 Week 4 Assignment Benchmark Nursing Process Approach To Care Latest 2019 JulyDoreenÎncă nu există evaluări
- KG College of Nursing VisitDocument7 paginiKG College of Nursing VisitShubha JeniferÎncă nu există evaluări
- Department of Education: Republic of The PhilippinesDocument11 paginiDepartment of Education: Republic of The PhilippinesRogen VigilÎncă nu există evaluări
- Decision Trees and Markov Chains List of Suggested Problems To DoDocument5 paginiDecision Trees and Markov Chains List of Suggested Problems To Dosolo docs0% (1)
- The State of The Worlds Children 2009Document168 paginiThe State of The Worlds Children 2009UNICEF SverigeÎncă nu există evaluări