Documente Academic
Documente Profesional
Documente Cultură
Decreased Intracranial Pressure With Optimal Head Elevation of 30 or 45 Degrees in Traumatic Brain Injury Patients (Literatur Review)
Încărcat de
Theresia Avila Kurnia0 evaluări0% au considerat acest document util (0 voturi)
158 vizualizări4 paginintracranial Pressure With Optimal Head Elevation of 30 or 45 Degrees in Traumatic Brain Injury Patients %28literatur Review%29
Titlu original
Decreased Intracranial Pressure With Optimal Head Elevation of 30 or 45 Degrees in Traumatic Brain Injury Patients %28literatur Review%29
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentntracranial Pressure With Optimal Head Elevation of 30 or 45 Degrees in Traumatic Brain Injury Patients %28literatur Review%29
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
158 vizualizări4 paginiDecreased Intracranial Pressure With Optimal Head Elevation of 30 or 45 Degrees in Traumatic Brain Injury Patients (Literatur Review)
Încărcat de
Theresia Avila Kurniantracranial Pressure With Optimal Head Elevation of 30 or 45 Degrees in Traumatic Brain Injury Patients %28literatur Review%29
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 4
DECREASED INTRACRANIAL PRESSURE WITH OPTIMAL
HEAD ELEVATION OF 30 OR 45 DEGREES IN TRAUMATIC
BRAIN INJURY PATIENTS (LITERATUR REVIEW)
Heni Maryati*
*Lecture of Pemkab Jombang Institute of Health Science Departement of Medical Surgical
and Critical Care Nursing Jombang Indonesia
Email: zahra.zubir@yahoo.com
ABSTRACT
Introduction: Intracranial pressure (ICP) can be elevated in traumatic brain injury. Raised ICP is a lift
threatening conditions. Unless recognized and treated early to reduce cerebral perfusion pressure (CPP)
and progress to brain herniation and death. Management of elevated ICP is, in part, dependent on the
underlying cause. The purpose of this literature review was to find a management of a noninvasive
physical intervention procedural for decreasing intracranial pressure for brain injury and reduce the
duration of treatment invasive. Method: Systematic searches were undertaken using Medline database,
PubMed and Cochrane, restricted from 2011 to 2016. There 12 articles included by searching through
the appropriate key word topic, but only 5 articles were selected based on the inclusion criteria. Results:
Medical options for treating elevated ICP include head of bed elevation, IV mannitol, hypertonic saline,
transient hyperventilation, barbiturates. A head elevation of 30 or 45 degrees is optimal for decreasing
intracranial pressure. Discussion: Head elevations of 30 or 45 degrees is optimal a conventional nursing
of a noninvasive physical intervention procedure for decreasing intracranial pressure for brain injured.
Is the most effective management that showed simple, inexpensive treatment procedure and can be
applied in variety ages today, independent nursing intervention without side effect. Recommended in
clinical practice, intensive care unit staff members need to cautiously perform head elevation of 30 or
45 degrees its physiologic effect and potential hazard.
Key words: management intracranial pressure, head elevation, traumatic brain injury patients
INTRODUCTION elevated ICP6.. Intracranial pressure (ICP) can
Traumatic brain injury (TBI) and its be elevated in traumatic brain injury.
complications are the leading of mortality and Management of elevated ICP is, in
morbidity. In the US alone over 2,300 deaths, part, dependent on the underlying cause.
42,000 hospitalizations, and 404,000 Medical options for treating elevated ICP
Emergency Department visits occurs annually include head of bed elevation, IV mannitol,
among children 0 -14 years old related to TBI. hypertonic saline, transient hyperventilation,
Mortality with severe TBI is often the result of barbiturates, and if ICP remains refractory,
a refractory increase in intracranial pressure sedation, endotracheal intubation, mechanical
(ICP). Therefore prevention and management of ventilation, and neuromuscular paralysis.
raised ICP is increasingly recognized as central Surgical options include CSF drainage if
to current neuro-critical care. Increased ICP is hydrocephalus is present and decompression of
an important caused of secondary brain injury in a surgical lesion, such as an intracranial
TBI and both degree and duration of high ICP is hematoma/ large infarct or tumor, if the
associated with poor outcomes. Sustained patients condition is deemed salvageable3. The
increased to 20 mmHg for >5 min may need purpose of this literature review was to find a
treatment. Though the efficacy of treatment method and technique of a noninvasive physical
based on ICP monitoring has been questioned intervention procedural for decreasing
intracranial pressure (ICP). Increased intracranial pressure for brain injury, reduce the
intracranial pressure (ICP) is associated with duration of treatment invasive, and reduce the
worse outcome after traumatic brain injury cost of treatment. Head elevation a conventional
(TBI). The current guidelines and management nursing procedure for brain injured individuals
strategies are aimed at maintaining adequate with intracranial hypertension. It is performed
cerebral perfusion pressure and treating with the intent of reducing intracranial pressure
(ICP) by means of a noninvasive physical
intervention. Head up position may have than at 10 and 15 degrees. Patients with
beneficial effect on intracranial pressure (ICP) increased intracranial pressure significantly
via changes in mean arterial pressure (MAP), air benefitted from a head elevation of 10, 15, 30
way pressure, central venous pressure and and 45 degrees compared with 0 degrees. A
cerebral spinal fluid displacement. However, in head elevation of 30 or 45 degrees is optimal for
some circumstances head up position may decreasing intracranial pressure4. According to
decrease MAP with in turn will result in a research Agbeko RS, et al (2012) that in severe
paradoxical rise in ICP trough auto regulation pediatric traumatic brain injury, the relations
the degree of head elevation has to be titrated by ship between change in head of the bead and
evaluating the most adequate cerebral perfusion change in intracranial pressure was negative and
pressure (CPP) for each patient by means of linier. The lowest intracranial pressure was
trans cranial. A change in head position can lead usually, but not always, achieved at highest
to a change in intracranial pressure, however, head 0f the bed angles depend, in parts, on the
there a conflicting data regarding the optimal subjects height.
degree of elevation that decreases intracranial The other therapies to reduce elevated
pressure in post craniotomy patients. Patients intracranial pressure if ICP not remains
with increased intracranial pressure refractory used osmotic agents, such as
significantly benefitted from a head elevation of mannitol, hypertonic saline and the other
10, 15,30 and 45 degrees compared with 0 therapies, such as hyperventilation and
degrees. A head elevation of 30 or 45 degrees is barbiturates. Recording the research Scalfani, et
optimal for decreasing intracranial pressure. al (2012) that in cerebral blood flow (CBF) is
Recommended in clinical practice, intensive reduce after severe traumatic brain injury (TBI)
care unit staff members need to cautiously with considerable regional variation osmotic
perform head elevation of 30 - 45 degrees with agents are used to reduce elevated intracranial
a thorough understanding of its physiologic pressure (ICP). In 8 patients with acute TBI, we
effect and potential hazard4. measured regional CBF with positron emission
tomography before and 1 hour after
METHOD administration of equi osmolar 20% mannitol (1
A literature review revealed that ml/kg) or 23,4 % hypertonic saline (0,686
studies have been conducted in a range of ml/kg) in regions with focal injury and baseline
countries by using a variety of management to hypo perfusion CBF < 25 ml per 100 gr/min.
screen leaners decrease intracranial pressure for Result that osmotic therapy reduce the number
traumatic brain injury patients. It was of hypo-perfuse brain regions by 40% (p ,
conventional nursing of a noninvasive physical 0,001) 5. Recording the research Mangat HS
intervention procedure for decreasing (2012) that in hyperosmolar agents are
intracranial pressure for brain injured reduce the commonly used as an initial treatment for the
duration of treatment invasive, and reduce the management of raised intracranial pressure
cost of treatment. (ICP) after several traumatic brain injury (TBI).
A head elevation of 30 or 45 degrees They have an excellent adverse effect profile
is optimal for decreasing intracranial pressure. compared to other therapies, such as
Is the most effective management that showed hyperventilation and barbiturates, which carry
simple, inexpensive treatment procedure and the risk of reducing cerebral perfusion.
can be applied in variety ages today, The hyperosmolar agent mannitol has
independent nursing intervention without side been used for several decades to reduce raised
effect. It was conventional nursing of a ICP, and there is accumulating evidence from
noninvasive physical intervention procedure for pilot studies suggesting beneficial effects of
decreasing intracranial pressure for brain hypertonic saline (HTS) for similar purposes. In
injured. According to research J. Adv Nurs ideal therapeutic agent for ICP reduction should
(2015) that a changes in head position can lead reduce ICP while maintaining cerebral
to a change intracranial pressure. Compared perfusion (pressure). While mannitol can cause
with a degree 10,15,30 and 45 degrees of head dehydration over time, HTS helps maintain
elevation resulted in lower intracranial pressure. normovolemia and cerebral perfusion, a finding
Intracranial pressure at 30 degrees was not that has led to a large amount of pilot data being
significantly different in comparison to 45 published o benefits of HTS, albeit in small
degrees of head elevation and was lower that cohorts. Prophylactic therapy is not
recommended with mannitol, although it may 45 degrees is optimal for decreasing
be beneficial with HTS. To date, no large intracranial pressure. Is the most effective
clinical trial has been performed to directly management that showed simple, inexpensive
compare the two agents. The best current treatment procedure and can be applied in
evidence suggest that mannitol is effective in variety ages today, independent nursing
reducing ICP in the management of traumatic intervention without side effect. It was
intracranial hypertension and carries mortality conventional nursing of a noninvasive physical
benefit compared to barbiturates. Current intervention procedure for decreasing
evidence regarding the use of HTS in severe intracranial pressure for brain injured.
TBI is limited to smaller studies, which a benefit The other therapies to reduce elevated
in ICP reduction and perhaps mortality7. intracranial pressure used osmotic agents, such
According to research Mangat HS,et al (2015) as mannitol, hypertonic saline and the other
that a Hypertonic saline (HTS) given as bolus therapies, such as hyperventilation and
therapy was more effective than mannitol in barbiturates. Mannitol can cause dehydration
lowering the cumulative and daily ICP burdens over time, HTS helps maintain normovolemia
after severe TBI. Patients in the HTS group had and cerebral perfusion. Prophylactic therapy is
significantly lower number of ICU days. not recommended with mannitol, although it
may be beneficial with HTS. To date, no large
RESULTS clinical trial has been performed to directly
Systematic searches were undertaken compare the two agents. The best current
using Medline database, Pubmed and Cochrane evidence suggest that mannitol is effective in
, restricted from 2011 to 2016. There 7 articles reducing ICP in the management of traumatic
included by searching through the appropriate intracranial hypertension and carries mortality
key word topic, but only 3 articles were benefit compared to barbiturates.
selected based on the inclusion criteria.
Management of raised ICP includes care air CONCLUSION AND
way, ventilation and oxygenation, adequate RECOMMENDATION
sedation and analgesia, neutral neck position, Head elevations of 30 or 45 degrees is
head end elevation 30 or 45 degrees and short optimal a conventional nursing of a noninvasive
term hyperventilation, and hyperosmolar physical intervention procedure for decreasing
therapy (manitol or hypertonic saline) , in intracranial pressure for brain injured. Is the
critically raised ICP barbitural coma, moderate most effective management that showed simple,
hypothermia and surgical decompression. inexpensive treatment procedure and can be
applied in variety ages today, independent
DISCUSSION nursing intervention without side effect.
Intracranial pressure (ICP) can be In clinical practice, intensive care unit
elevated in traumatic brain injury. Management staff members need to cautiously perform head
of elevated ICP is, in part, dependent on the elevation of 30 or 45 degrees its physiologic
underlying cause. Medical options for treating effect and potential hazard.
elevated ICP include head of bed elevation, IV
mannitol, hypertonic saline, transient REFERENCES
hyperventilation, barbiturates, and if ICP Agbeho RS, et al. (2012). Intracranial pressure
remains refractory, sedation, endotracheal and cerebral perfusion pressure responses
intubation, mechanical ventilation, and to head elevation change in pediatric
neuromuscular paralysis. Surgical options traumatic brain injury. Pediatr crit care
include CSF drainage if hydrocephalus is med Jan ; 13 (1) : e 39 - 47 .
present and decompression of a surgical lesion, Freeman WD. (2015). Neuro critical care.
such as an intracranial hematoma/ large infarct Management of intracranial pressure.
or tumor, if the patients condition is deemed Continuum (minea p min). Oct ; 2 (5) :
salvageable. Intracranial pressure (ICP) can be 1299 -323.doi.1212/ CON
elevated in traumatic brain injury. Raised ICP 0000000000000235
is a lift threatening conditions. Unless Freeman WO. (2015). Management of
recognized and treated early to reduce cerebral intracranial pressure. Continuum (minn
perfusion pressure (CPP) and progress to brain eap minn). Oct ; 21 (Neurocritical care ) :
herniation and death. A head elevation of 30 or 1299 323
_______ (2015). Systematic review of Scalfani MT, et al. (2012). Effect of osmotic
decreased intracranial pressure with agenrs on regional cerebral blood flow in
optimal head elevation in post traumatic brain injury. J. Crit care.
craniotomy patients. A Meta analysis. 71 Published online : Desember 16,2011.
(10) : 2237 46. Doi : 10.1111/ Doi : http:// dx. Doi.org / 10.1016 / J.J
jan.12679. E pub 2015 May 17 Crc. 2011.008
Mangan HS,et al. (2015). Hypertonic saline Vinay Kukreti, Hadi Mohseni, Bod and James
reduces cumulative and daily intracranial Drake. (2014). Management of raised
pressure burdens after severe traumatic intracranial pressure in children with
brain injury. J Neurosurg. 2015 Jan ; traumatic brain injury. J. Pediatr
122(1): 202 -10. Doi: Neurosci. Sept Dec, 9 (3) : 207 -215
10.3171/2014.10.JNS132545
S-ar putea să vă placă și
- Diaphragmatic HerniaDocument8 paginiDiaphragmatic HerniaAnonymous 9xHTwHYÎncă nu există evaluări
- Memory SkillsDocument70 paginiMemory SkillsAsiri Samanatha Elegoda100% (1)
- Sensory Processing and Autism Evidence Research Future Directions DR Roseann Schaaf PDFDocument59 paginiSensory Processing and Autism Evidence Research Future Directions DR Roseann Schaaf PDFKiyorÎncă nu există evaluări
- Enteral Nutrition in The Critically Ill Marik PDFDocument8 paginiEnteral Nutrition in The Critically Ill Marik PDFCami Cuevas VergaraÎncă nu există evaluări
- UNIT-5 Pharmacology of NeurosurgeryDocument12 paginiUNIT-5 Pharmacology of NeurosurgeryFaizan Mazhar100% (1)
- Guidelines For The Management of Severe Traumatic Brain Injury 4th EditionDocument62 paginiGuidelines For The Management of Severe Traumatic Brain Injury 4th EditionNailahRahmahÎncă nu există evaluări
- Nursing Care of The Patient With Neurological DisordersDocument89 paginiNursing Care of The Patient With Neurological DisordersRaveenmayiÎncă nu există evaluări
- gbs4 171105053149Document71 paginigbs4 171105053149Theresia Avila KurniaÎncă nu există evaluări
- AppendicitisDocument11 paginiAppendicitisbobtagubaÎncă nu există evaluări
- Reflexology - 5 Power PointsDocument6 paginiReflexology - 5 Power Pointsrickiti9100% (1)
- Traumatic Brain InjuryDocument23 paginiTraumatic Brain InjuryRisal WintokoÎncă nu există evaluări
- Thyroid Function TestDocument11 paginiThyroid Function TestBookmyscansÎncă nu există evaluări
- Increased ICPDocument7 paginiIncreased ICPK-La BreanneÎncă nu există evaluări
- Principles of Opioid Management: Symptom GuidelinesDocument45 paginiPrinciples of Opioid Management: Symptom GuidelinesTheresia Avila KurniaÎncă nu există evaluări
- Aubrey de Grey - SENSDocument57 paginiAubrey de Grey - SENSBruceKlein50% (2)
- CarePlans PDFDocument130 paginiCarePlans PDFTheresia Avila KurniaÎncă nu există evaluări
- Ishihara Colour Plates - 38 Set GuideDocument13 paginiIshihara Colour Plates - 38 Set Guidenelutza_popÎncă nu există evaluări
- Brain Injury Resuscitation 2009Document8 paginiBrain Injury Resuscitation 2009Dandy Azmi AzwirÎncă nu există evaluări
- Pathophysiology and Management of ICH and Brain Hypoxia After TBIDocument13 paginiPathophysiology and Management of ICH and Brain Hypoxia After TBIitalofgÎncă nu există evaluări
- Morning Case DiscussionDocument21 paginiMorning Case Discussionسلطان الحنبصيÎncă nu există evaluări
- Intracerebral Hemorrhage Medical TreatmentDocument3 paginiIntracerebral Hemorrhage Medical TreatmentDarrel Allan MandiasÎncă nu există evaluări
- Critical AppraisalDocument15 paginiCritical AppraisalRio HerawanÎncă nu există evaluări
- Critical Care of Patients With Acute Ischemic and Hemorrhagic StrokeDocument7 paginiCritical Care of Patients With Acute Ischemic and Hemorrhagic StrokeMary Jhane VillanuevaÎncă nu există evaluări
- Helbok 2018Document3 paginiHelbok 2018Julieta PereyraÎncă nu există evaluări
- New Therapies For Intracranial Hypertension: Review ArticleDocument10 paginiNew Therapies For Intracranial Hypertension: Review ArticleBeny RiliantoÎncă nu există evaluări
- Ebp Head Up 30Document9 paginiEbp Head Up 30La fazaÎncă nu există evaluări
- 12 JMSCRDocument6 pagini12 JMSCRArdianÎncă nu există evaluări
- JURNAL Sip 1Document30 paginiJURNAL Sip 1Irwan SabriÎncă nu există evaluări
- MannitolDocument10 paginiMannitolFenzy Septiana AnggrainiÎncă nu există evaluări
- Emergency Airway Management in The Patient With Elevated ICP UpToDateDocument16 paginiEmergency Airway Management in The Patient With Elevated ICP UpToDateJoyce CarolineÎncă nu există evaluări
- Bansal 2021 - Neutral Spinal Compress HRVDocument2 paginiBansal 2021 - Neutral Spinal Compress HRVdudekula salmaÎncă nu există evaluări
- Management of Raised Intracranial Pressure in Children With Traumatic Brain Injury - PMCDocument19 paginiManagement of Raised Intracranial Pressure in Children With Traumatic Brain Injury - PMChadi40canadaÎncă nu există evaluări
- Management of raised intracranial pressure in childrenDocument24 paginiManagement of raised intracranial pressure in childrenMita AmaliaÎncă nu există evaluări
- Nihms687466 PDFDocument14 paginiNihms687466 PDFyoiiiÎncă nu există evaluări
- Tiopentone Vs PentobarbitalDocument10 paginiTiopentone Vs PentobarbitalFrank PuchiÎncă nu există evaluări
- Effect of Early Physiotherapy On Intracranial PressureDocument6 paginiEffect of Early Physiotherapy On Intracranial Pressurebendot29Încă nu există evaluări
- Management of Moderate To Severe Traumatic Brain Injury 2022Document18 paginiManagement of Moderate To Severe Traumatic Brain Injury 2022Vladimir BasurtoÎncă nu există evaluări
- Guidelines For Management EspañolDocument14 paginiGuidelines For Management EspañolGrace KellyÎncă nu există evaluări
- Current Concepts and Advancements in TBIDocument3 paginiCurrent Concepts and Advancements in TBIMacros FitÎncă nu există evaluări
- Brainhypoxiaisassociatedwithshort Termoutcomeafterseveretraumaticbraininjuryindependentlyofi 2Document9 paginiBrainhypoxiaisassociatedwithshort Termoutcomeafterseveretraumaticbraininjuryindependentlyofi 2indahÎncă nu există evaluări
- Head Injury Management: Ahimbisibwe Alaphael Lecturer DR - JulietDocument33 paginiHead Injury Management: Ahimbisibwe Alaphael Lecturer DR - JulietNinaÎncă nu există evaluări
- Oddo 2009Document6 paginiOddo 2009rodolfo riosÎncă nu există evaluări
- Use of Hyperoncotic Human Albumin Solution in Severe Traumatic Brain Injury Revisited-A Narrative Review and Meta-AnalysisDocument10 paginiUse of Hyperoncotic Human Albumin Solution in Severe Traumatic Brain Injury Revisited-A Narrative Review and Meta-Analysisjose luis iribarrenÎncă nu există evaluări
- Managing Increased Intracranial PressureDocument13 paginiManaging Increased Intracranial PressureLudmila PirtacÎncă nu există evaluări
- Tugas Bu EltrikaDocument20 paginiTugas Bu EltrikaHervina22Încă nu există evaluări
- Intracranial Pressure: Presenter: NailaDocument26 paginiIntracranial Pressure: Presenter: NailaInam KhanÎncă nu există evaluări
- Cerebral Perfusion PressureDocument36 paginiCerebral Perfusion PressureAbdullah Shidqul AzmiÎncă nu există evaluări
- The Coagulation DefectDocument9 paginiThe Coagulation DefectTimotius Wira YudhaÎncă nu există evaluări
- B5W2 - Brainstem Herniation TreatmentDocument2 paginiB5W2 - Brainstem Herniation TreatmentCatherine MernaÎncă nu există evaluări
- Management of Acute Severe Traumatic Brain InjuryDocument19 paginiManagement of Acute Severe Traumatic Brain InjuryMustafa AadanÎncă nu există evaluări
- Evaluation and Management of Elevated Intracranial Pressure in Adults - UpToDateDocument41 paginiEvaluation and Management of Elevated Intracranial Pressure in Adults - UpToDateManuelEduardoSanchezSotoÎncă nu există evaluări
- 2.-Management of Moderate To Severe Traumatic Brain Injury An Update For The IntensivistDocument18 pagini2.-Management of Moderate To Severe Traumatic Brain Injury An Update For The IntensivistEllys Macías PeraltaÎncă nu există evaluări
- Hypertension: SMF Saraf Rsud Bangli Fakultas Kedokteran Universitas Islam Al-Azhar 2018Document49 paginiHypertension: SMF Saraf Rsud Bangli Fakultas Kedokteran Universitas Islam Al-Azhar 2018Muhammad HidayatullahÎncă nu există evaluări
- Title: Sildenafil in The The Management of Patients With SevereDocument2 paginiTitle: Sildenafil in The The Management of Patients With SevereAnca Oprea TighiliuÎncă nu există evaluări
- Surgical Management: SurgeryDocument5 paginiSurgical Management: SurgeryKarl Angelo MontanoÎncă nu există evaluări
- Increased Intracranial Pressure - StatPearls - NCBI BookshelfDocument5 paginiIncreased Intracranial Pressure - StatPearls - NCBI BookshelfWIWI HRÎncă nu există evaluări
- Stroke 2013 Qureshi S67 9Document4 paginiStroke 2013 Qureshi S67 9Herlinda Dwi NingrumÎncă nu există evaluări
- Ventilatory Strategies For Patients With Acute Brain InjuryDocument8 paginiVentilatory Strategies For Patients With Acute Brain InjuryKhalid Walid AhmadÎncă nu există evaluări
- Focused Management of Patients With Severe Acute Brain Injury and ARDSDocument12 paginiFocused Management of Patients With Severe Acute Brain Injury and ARDSPepeee:DÎncă nu există evaluări
- Management Head Injury in ICUDocument5 paginiManagement Head Injury in ICUIrma KusumaÎncă nu există evaluări
- JNNB 4 144Document4 paginiJNNB 4 144luciaÎncă nu există evaluări
- Wolfe-Management of Intracranial Pressure-Curr Neurol Neurosci Rep-2009Document9 paginiWolfe-Management of Intracranial Pressure-Curr Neurol Neurosci Rep-2009Beny RiliantoÎncă nu există evaluări
- Stroke BP 24 HrsDocument11 paginiStroke BP 24 HrsrodribeatsÎncă nu există evaluări
- Tadevosyan 2021Document26 paginiTadevosyan 2021W Antonio Rivera MartínezÎncă nu există evaluări
- Efficacy and Safety of Amlodipine Versus Captopril and Their Combination Inhypertensive Urgency A Randomized Controlled Trial 2329 9126 1000274Document7 paginiEfficacy and Safety of Amlodipine Versus Captopril and Their Combination Inhypertensive Urgency A Randomized Controlled Trial 2329 9126 1000274Laras OktavianiÎncă nu există evaluări
- Targeted Treatment of Severe Head Injury Based on Monitoring of Secondary InjuryDocument4 paginiTargeted Treatment of Severe Head Injury Based on Monitoring of Secondary InjuryAstari RahayuningtyasÎncă nu există evaluări
- Outcome Following Decompressive Craniectomy in Severe Head Injury - Rashid Hospital ExperienceDocument7 paginiOutcome Following Decompressive Craniectomy in Severe Head Injury - Rashid Hospital ExperienceSyafiq IshakÎncă nu există evaluări
- SSH en HTE. J Neuros 2012Document12 paginiSSH en HTE. J Neuros 2012Laura López Del Castillo LalydelcaÎncă nu există evaluări
- Traumatic Head InjuriesDocument50 paginiTraumatic Head InjuriesVasudha BuddyÎncă nu există evaluări
- Edema Cerebral UPTODATEDocument32 paginiEdema Cerebral UPTODATEChristian Andres Cruz PerezÎncă nu există evaluări
- Cerebral Herniation Syndromes and Intracranial HypertensionDe la EverandCerebral Herniation Syndromes and Intracranial HypertensionMatthew KoenigÎncă nu există evaluări
- Sudden Death: Advances in Diagnosis and TreatmentDe la EverandSudden Death: Advances in Diagnosis and TreatmentHaiyan ZhuÎncă nu există evaluări
- PsikososialDocument8 paginiPsikososialFatanahÎncă nu există evaluări
- Program PaliatifDocument10 paginiProgram PaliatifTheresia Avila KurniaÎncă nu există evaluări
- Status Gizi Ibu Saat Hamil, Berat Badan Lahir Bayi Dengan Stunting Pada BalitaDocument7 paginiStatus Gizi Ibu Saat Hamil, Berat Badan Lahir Bayi Dengan Stunting Pada BalitaDewa Ray Yunita SariÎncă nu există evaluări
- Jurnal Gizi Dan PanganDocument8 paginiJurnal Gizi Dan PanganUchiha Albert PardedeÎncă nu există evaluări
- Status Gizi Ibu Saat Hamil, Berat Badan Lahir Bayi Dengan Stunting Pada BalitaDocument7 paginiStatus Gizi Ibu Saat Hamil, Berat Badan Lahir Bayi Dengan Stunting Pada BalitaDewa Ray Yunita SariÎncă nu există evaluări
- Hasil Seleksi SNMPTN 2019 UnpadDocument41 paginiHasil Seleksi SNMPTN 2019 Unpadpkm pelindung hewanÎncă nu există evaluări
- 2520 4993 1 SMDocument8 pagini2520 4993 1 SMVeraÎncă nu există evaluări
- Disorders of Endocrine System: Prof. J. Hanáček, MD, PHDDocument66 paginiDisorders of Endocrine System: Prof. J. Hanáček, MD, PHDjerinthomasrajanÎncă nu există evaluări
- Lakip Yankes Tahun 2016Document1 paginăLakip Yankes Tahun 2016Theresia Avila KurniaÎncă nu există evaluări
- InfodatinDocument13 paginiInfodatinTheresia Avila KurniaÎncă nu există evaluări
- Principles of Anatomy and Physiology: The Endocrine SystemDocument84 paginiPrinciples of Anatomy and Physiology: The Endocrine SystemTheresia Avila KurniaÎncă nu există evaluări
- Who NMH NHD 14.5 EngDocument8 paginiWho NMH NHD 14.5 EngAsty PuthryyÎncă nu există evaluări
- Review: Factors Relating To Nurses' Caring Behaviors For Dying PatientsDocument13 paginiReview: Factors Relating To Nurses' Caring Behaviors For Dying PatientsFrederick BaldemoroÎncă nu există evaluări
- Rencana Anggaran 2016 PDFDocument27 paginiRencana Anggaran 2016 PDFLibriantyÎncă nu există evaluări
- 2520 4993 1 SMDocument8 pagini2520 4993 1 SMVeraÎncă nu există evaluări
- Journal of Career Assessment-2014-Chang PDFDocument14 paginiJournal of Career Assessment-2014-Chang PDFTheresia Avila KurniaÎncă nu există evaluări
- LiverpoolSedation ManagementDocument9 paginiLiverpoolSedation ManagementTheresia Avila KurniaÎncă nu există evaluări
- Guillain Barre SyndromeDocument2 paginiGuillain Barre SyndromeTheresia Avila KurniaÎncă nu există evaluări
- Guide To The Care of The Patient With PDFDocument41 paginiGuide To The Care of The Patient With PDFDaniel CainÎncă nu există evaluări
- Guillain Barre SyndromeDocument2 paginiGuillain Barre SyndromeTheresia Avila KurniaÎncă nu există evaluări
- Marketplace Provider Reimbursement ManualDocument270 paginiMarketplace Provider Reimbursement ManualTheresia Avila KurniaÎncă nu există evaluări
- 10 1016@j Resuscitation 2015 08 020Document6 pagini10 1016@j Resuscitation 2015 08 020Theresia Avila KurniaÎncă nu există evaluări
- Understanding Guillain-Barré Syndrome and Myasthenia GravisDocument31 paginiUnderstanding Guillain-Barré Syndrome and Myasthenia GravisTheresia Avila KurniaÎncă nu există evaluări
- Approach To The Infant or Child With Nausea and Vomiting - UpToDateDocument47 paginiApproach To The Infant or Child With Nausea and Vomiting - UpToDatemayteveronica1000Încă nu există evaluări
- PhysioEx Exercise 9 Activity 5Document3 paginiPhysioEx Exercise 9 Activity 5MARILYN MARIANA HERNANDEZ MENDOZAÎncă nu există evaluări
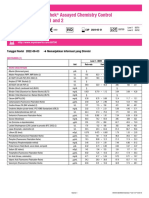
- Lyphochek Assayed Chemistry Control Levels 1 and 2: Tanggal Revisi 2022-06-03 Menunjukkan Informasi Yang DirevisiDocument2 paginiLyphochek Assayed Chemistry Control Levels 1 and 2: Tanggal Revisi 2022-06-03 Menunjukkan Informasi Yang DirevisiFahmiÎncă nu există evaluări
- Anatomy of The Left EyeDocument3 paginiAnatomy of The Left EyeJaessa FelicianoÎncă nu există evaluări
- Cambridge International General Certificate of Secondary EducationDocument16 paginiCambridge International General Certificate of Secondary EducationJeet JeetÎncă nu există evaluări
- Physical Exam of the Eye: Structures, Findings, DiagnosesDocument16 paginiPhysical Exam of the Eye: Structures, Findings, DiagnosesriveliÎncă nu există evaluări
- Surah Al An'aam (6:99) - Green Factory in PlantsDocument3 paginiSurah Al An'aam (6:99) - Green Factory in PlantsMuhammad Awais TahirÎncă nu există evaluări
- Imaging Modalities For Lung DiseasesDocument14 paginiImaging Modalities For Lung DiseasesYnaffit Alteza Untal100% (1)
- Feeding The Hemodinamically Unstable Patient A Critical Evolution of The EvidenceDocument9 paginiFeeding The Hemodinamically Unstable Patient A Critical Evolution of The EvidenceYanes NatanaelÎncă nu există evaluări
- Problems with Polyvagal TheoryDocument6 paginiProblems with Polyvagal TheoryCamilo IgnacioÎncă nu există evaluări
- Class X Biology Assignment Chapter 6 Life ProcessesDocument2 paginiClass X Biology Assignment Chapter 6 Life ProcessesVivek Nijhawan100% (1)
- Botany II PDFDocument7 paginiBotany II PDFMuhammad AmirÎncă nu există evaluări
- Macmillan Science Level 4 Pupil S Book Unit 1 PP 11 16Document6 paginiMacmillan Science Level 4 Pupil S Book Unit 1 PP 11 16reema2050reemaÎncă nu există evaluări
- Bipap A30 Specification / Part NumbersDocument2 paginiBipap A30 Specification / Part NumbersDejan ŽujovićÎncă nu există evaluări
- Jan 07 Old SNAB Unit 1 MSDocument10 paginiJan 07 Old SNAB Unit 1 MSCeleste FernandesÎncă nu există evaluări
- 10 Urinary BladderDocument32 pagini10 Urinary BladderMarera DomnicÎncă nu există evaluări
- A6. Karring T, Lang N, Löe H. The Role of Gingival Connective Tissue in Determining Epithelial Differentiation. J Perio Res 1975Document12 paginiA6. Karring T, Lang N, Löe H. The Role of Gingival Connective Tissue in Determining Epithelial Differentiation. J Perio Res 1975Daniel CubasÎncă nu există evaluări
- Company Most Recent Adposition (S) First Name Last Name Contact TypeDocument8 paginiCompany Most Recent Adposition (S) First Name Last Name Contact TypepaytencasÎncă nu există evaluări
- Photosynthesis WorksheetDocument3 paginiPhotosynthesis WorksheetByambazaya E100% (2)
- Somatic HybridizationDocument23 paginiSomatic HybridizationJan VivienelÎncă nu există evaluări
- Thesis Reza Salman Roghani PDFDocument76 paginiThesis Reza Salman Roghani PDFscoopyÎncă nu există evaluări
- Answer Guide For O Level Biology (5090/3) - Paper 3 Practical Test June 2001Document3 paginiAnswer Guide For O Level Biology (5090/3) - Paper 3 Practical Test June 2001MSHÎncă nu există evaluări
- Strain SprainDocument17 paginiStrain SprainPuterinugraha Wanca ApatyaÎncă nu există evaluări