Documente Academic
Documente Profesional
Documente Cultură
Monitoring For Depth of Anesthesia: A Review: Reviews
Încărcat de
Lestari Chye PouedanTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Monitoring For Depth of Anesthesia: A Review: Reviews
Încărcat de
Lestari Chye PouedanDrepturi de autor:
Formate disponibile
www.sciedu.ca/jbgc Journal of Biomedical Graphics and Computing, December 2012, Vol. 2, No.
REVIEWS
Monitoring for depth of anesthesia: a review
Amornyotin Somchai
Department of Anesthesiology and Siriraj GI Endoscopy Center, Faculty of Medicine Siriraj Hospital, Mahidol University,
Bangkok, Thailand.
Correspondence: Somchai Amornyotin. Address: Department of Anesthesiology and Siriraj GI Endoscopy Center,
Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok 10700, Thailand. Telephone: 662-419-7990. Fax:
662-411-3256. Email: sisam@mahidol.ac.th.
Received: May 27, 2012 Accepted: July 16, 2012 Published: December 1, 2012
DOI: 10.5430/jbgc.v2n2p119 URL: http://dx.doi.org/10.5430/jbgc.v2n2p119
Abstract
Monitoring depth of anesthesia is a newer advance in the monitoring of anesthesia. Accurate assessment of the depth of
anesthesia contributes to tailoring drug administration to the individual patient. Its increasing use may help to prevent
awareness or excessive anesthetic depth and to improve the patients outcomes. Awareness experiences frighten the
patients and can leave a lifetime of residual emotional and psychological problems. To date, no monitoring system has
been found to measure the depth of anesthesia reliably for all patients and all anesthetic agents. In this review, the author
critically analyzes the use of a number of the depth of anesthesia monitors including the traditional techniques and the
modern techniques.
Key words
Monitoring, Depth of anesthesia, Sedation
1 Introduction
Many surgical procedures would not be possible without anesthesia or sedation. The goals of anesthesia or sedation are a
reversible loss of consciousness with a lack of movement, a lack of awareness or recall, and unresponsiveness to painful
stimuli. Inadequate anesthesia or sedation may lead to intraoperative awareness with recall or to prolonged recovery and
increased risk of postoperative complications for the patients. Important signs of inadequate anesthesia, signs which
develop in response to stress or painful stimuli, are patient movement, increased breathing or blood pressure and increased
heart rate [1]. Failure to adjust the anesthetic requirements to individual variations in patient drug requirements and to the
intensity of pain stimulation during surgical procedures will also lead to over dosage or under dosage with anesthesia or
sedation.
2 Depth of sedation/anesthesia
Minimal sedation (anxiolysis) is a drug-induced state during which patients respond normally to verbal commands.
Although cognitive function and physical coordination may be impaired, airway reflexes and ventilatory and
cardiovascular functions are unaffected.
Published by Sciedu Press 119
www.sciedu.ca/jbgc Journal of Biomedical Graphics and Computing, December 2012, Vol. 2, No. 2
Moderate sedation (conscious sedation) is a drug-induced depression of consciousness during which patients respond
purposefully to verbal commands, either alone or accompanied by light tactile stimulation. No interventions are required
to maintain a patent airway, and spontaneous ventilation is adequate. Cardiovascular function is usually maintained.
Deep sedation is a drug-induced depression of consciousness during which patients can not be easily aroused but respond
purposefully following repeated or painful stimulation. The ability to independently maintain ventilatory function may be
impaired. Patients may require assistance in maintaining a patent airway, and spontaneous ventilation may be inadequate.
Cardiovascular function is usually maintained.
General anesthesia is a drug-induced loss of consciousness during which patients are not arousable, even by painful
stimulation. The ability to independently maintain ventilatory function is often impaired. Patients often require assistance
in maintaining a patent airway, and positive pressure ventilation may be required because of depressed spontaneous
ventilation or drug-induced depression of neuromuscular function. Cardiovascular function may be impaired.
3 Monitoring for depth of anesthesia
The transition from a state of wakefulness to a state of general anesthesia is accompanied by profound changes in the
brains spontaneous electrical activity recorded from electrodes placed on the scalp (electroencephalogram or EEG). The
clinical monitoring is simple and is commonly used by the variety of physicians. Only the advances in computer hardware
and signal processing algorithms have enabled the processing of EEG signals.
4 Clinical monitoring
Continuous monitoring of patient undergoing anesthesia or sedation is very important for ensuring the safety of the
procedure, and is of paramount importance in order to obtain a correct level of sedation in surgical patients. The physicians
need to monitor and evaluate the patients status and the depth of anesthesia or sedation throughout the procedure. Clinical
scoring systems are simple and inexpensive. In addition, clinical observation of the sedated patients can provide an early
warning for potentially dangerous problems. The clinical monitoring used to assess intraoperative consciousness are
checking for movement, response to verbal command, eyelash reflex, pupillary responses, tearing and pattern of
respiration.
4.1 Clinical signs
The most commonly used scoring system is Evanss score [2]. This score assesses autonomic activity related to systolic
blood pressure, heart rate, sweating and tears. This system is simple and not requiring specialized equipment. However,
these parameters are not specific and the scores can vary widely among individuals. ASA task force members on practice
advisory for intraoperative awareness and brain function monitoring have been recommended physicians should be used
these clinical signs to assess intraoperative consciousness [3]. Additionally, conventional monitoring systems including
electrocardiogram, noninvasive blood pressure, capnography and end tidal anesthetic analyzer are valuable and should be
used to help assessment of these clinical signs.
4.2 Skin conductance
Measuring skin resistance level and changes in the resistance of the skin is a simple and noninvasive method for evaluating
the sympathetic nerve activity. The measurement of skin conductance is a quantification of the clinical sign of sweat
production. Skin conductance is initially low and increases as anesthetic depth is increased. There has a correlation
between electrical skin impedance, predicted plasma concentrations of propofol and the MOAAS scale [4]. The individual
variability of the measurement values constitutes a problem in the interpretation of skin resistance measurements. In
addition, several factors affecting sweating can reduce the accuracy of this monitoring.
120 ISSN 1925-4008 E-ISSN 1925-4016
www.sciedu.ca/jbgc Journal of Biomedical Graphics and Computing, December 2012, Vol. 2, No. 2
4.3 Isolated forearm technique
Isolated forearm technique is a method detecting awareness during clinical practice. The tourniquet is applied to the
patients upper arm before administration of the muscle relaxant, and is inflated above systolic blood pressure to exclude
its effect. Movement of the arm indicated wakefulness or light anesthesia, although not necessarily explicit awareness.
However, the incidence of movement with this technique can vary with the choice of anesthetic drugs [5]. Other limitations
of this technique are the limited time available before the patients are unable to move their arms, level of
sedation/anesthesia needed to prevent the movement of patients arm, and the nonspecific response may be misinterpreted.
4.4 Heart rate variability
Clinically, the beat to beat variability of heart rate may provide information which would be useful for monitoring depth of
anesthesia. Three components of the heart rate variability are low, medium and high frequency fluctuations. Heart rate
increases during inspiration and decreases during expiration through the parasympathetic reflex. This is called as the
respiratory sinus arrhythmia (RSA). The reduction of the RSA is observed during anesthesia together with increase during
recovery. Some monitors use the heart rate variability at respiratory frequency or RSA as a method assessing anesthetic
depth [6]. However, the vagal tone depends on an intact of autonomic nervous system and healthy myocardial conducting
system. Additionally, several factors influencing the heart rate variability in the perioperative setting are conduction
abnormalities, autonomic neuropathy and sepsis as well as some medications such as beta-blockers and atropine.
4.5 Ramsay scale
The Ramsay scale was developed in 1970 in order to promote adequate sedation in intensive care units. It is internationally
one of the most frequently cited sedation assessment tools. The Ramsay scale mainly involves a positive approach to the
patient, designed to cause minimal disturbance to sleep. The level of sedation in mechanically ventilated patients is most
often assessed with the Ramsay scale. This sedation scale divides into six score responses [7].
1 Anxious, agitated, restless
2 Cooperative, tranquil, oriented
3 Drowsy, response to verbal command
4 Asleep, brisk response to light glabellar tap and loud auditory stimulus
5 Asleep, sluggish response to light glabellar tap and loud auditory stimulus
6 No response to stimulus
To date, the reliability of the Ramsay scale remains controversial. Many studies show that there are insufficient evidences
to support the reliability of the Ramsay sedation scale as a measure of sedation assessment [8, 9]. In contrast, several studies
demonstrate that the inter-observer reliability of the level of sedation measurements, performed in daily clinical practice
within a large team of physicians, proved to be almost perfect [10, 11]. However, the Ramsay scale is largely outdated and
has been superseded by more appropriate, practical scoring tools.
4.6 Modified observer assessment of alertness/sedation scale MOAA/S)
The Modified Observer Assessment of Alertness/Sedation scale (MOAA/S) is a six-point scale ranging from 5 to 0. It
entails a positive action that involves eliciting a response to increasingly intense stimuli[12]. Patients are considered to have
loss of consciousness at the transition between level 3 and level 2.
5 Responds readily to name spoken in normal tone
4 Lethargic response to name spoken in normal tone
Published by Sciedu Press 121
www.sciedu.ca/jbgc Journal of Biomedical Graphics and Computing, December 2012, Vol. 2, No. 2
3 Response only after name is called loudly and/or repeatedly
2 Response only after mild prodding or shaking
1 Response only after painful trapezius squeeze
0 No response after painful trapezius squeeze
To date, the author also uses the MOAA/S for sedation for various gastrointestinal endoscopic procedures [13-15].
Generally, the MOAA/S and the Ramsay scale are not interchangeable with the definitions of the levels of sedation. There
is evidence of a correlation between the MOAA/S score and the Bispectral (BIS) measurement in several studies [16]. The
monitoring of stress response during surgery is important, because prolonged surgical stress can lead to increased
morbidity and delayed postoperative recovery [17]. An appropriate depth of sedation is routinely adjusted by titration of
sedative concentration. Generally, the changes in heart rate and arterial blood pressure were used as signs of increased
nociception during sedation but their specificity and sensitivity is not very high [18].
5 Anesthetic depth monitoring tools
Because of clinical scoring systems are often inadequate in evaluating the patients level of consciousness, many
instrumental tools of anesthetic depth monitoring have been proposed, and particularly the direct evaluation of the central
nervous system actions of anesthetic drugs. The monitor that would enable objective, reproducible and continuous
measurement of anesthetic depth has lead to the development of EEG or AEP (auditory evoked potentials) based
monitors[1, 19].
6 Factors that interfere EEG measurements
The quality of EEG records is mainly influenced by internal or external sources of electromagnetic waves. Numerous
sources of interference can mislead EEG measurements. The common sources of interference are the electrical activity of
head muscles [20], cardiac pacemaker [21], hot air blanket systems [22] and the electrocoagulation needles [23]. The EEG
activity is also influenced by anesthetic agents. However, ketamine does not change the BIS index even when patients are
unconscious[24]. Ketamine has no effects on AEP [25]. The effects of nitrous oxide on EEG or BIS value are varied and
therefore unpredictable [24, 26, 27]. So, the current EEG or AEP-based anesthetic monitoring devices are not able to reliably
assess the patients depth of anesthesia when ketamine or nitrous oxide is used.
Physiological conditions, such as age [28], race [29], gender [30], low body temperature [31], acid-base imbalances [32], low
blood glucose [33] or cerebral ischemia [26] also have a significant effect on patient can influence the EEG. The changes in
the patients age or general health may require adjustment of anesthetic agents. This variability in drug concentration is
caused by variability of physiological effects of drugs on the differences in pharmacodynamics and pharmacokinetics.
Neuromuscular blocking agents have the effects on muscle electrical activity and indirectly on the signal quality of EEG
measurement [34]. AEP are the responses of the auditory pathway to sound stimuli. An AEP is calculated by repeatedly
applying an auditory stimulus to the patient and averaging EEG periods that immediately follow each stimulus[6].
Compared to the raw EEG, AEP is less sensitive to artifacts. However, there still have no direct measure of consciousness
available in clinical practice and thus no gold standard against which to test EEG or AEP derived indices of anesthetic
depth [35].
122 ISSN 1925-4008 E-ISSN 1925-4016
www.sciedu.ca/jbgc Journal of Biomedical Graphics and Computing, December 2012, Vol. 2, No. 2
7 Commercial monitoring tools
The anesthetic depth monitoring technology is promising and used widely, nevertheless to date no health authority has so
far recommended that such monitors should be compulsory during general anesthesia or sedation, but should be
considered only on an individual basis. To date, there have many commercial monitoring tools.
7.1 Bispectral Index Monitor
The Bispectral index (BIS) was first introduced in 1992 by Aspect Medical Systems. The main component of the BIS
monitor is the bispectral analysis, which evaluates the phase relations from a single channel EEG signal measured from the
patients forehead. Recently, the BIS is developed to ease EEG interpretation. It gives the level of sedation as a constant
read-out from the device after analysis of single channel EEG findings. The BIS has been reported to be more precise in
measurement of the depth of anesthesia. Among instrumental tools for anesthetic depth monitoring, BIS monitor is now
widely used due to its reliability and applicability. In addition, the BIS monitoring is a noninvasive method of assessing
patients level of consciousness. The BIS scale ranges from 0 to 100 (0, no cortical activity or coma; 40-60, unconscious,
general anesthesia; 60-70, deep sedation with low probability of explicit recall; 70-95, light to moderate sedation; 95-100,
awake). BIS monitor has been employed to monitor the depth of anesthesia [36] and sedation in intensive care unit
patients [37]. Additionally, BIS monitor is also the anesthetic depth monitoring that has been routinely used in pediatric
anesthesia [38, 39].
Generally, the BIS or alternative EEG-based monitoring of anesthetic depth might be useful in preventing oversedation
and in reducing propofol dosages during the maintenance phase of the procedure [40]. However, the previous observational
study of BIS during nurse-administered propofol sedation (NAPS) found that the BIS scores lagged substantially behind
actual sedation scores during both induction of sedation and recovery[41]. Additionally, several studies also demonstrated
that BIS did not lead to reduction in mean propofol dose or recovery time when used as an adjunct to NAPS for
colonoscopy, or when used as the primary target for sedation. No clinically important role for BIS monitoring as an
adjunct to NAPS has yet been established [42, 43].
7.2 Narcotrend monitor
The Narcotrend monitor is produced by Monitor Technik, Hannover Medical School and was introduced in the year 2000.
It performs a computerized analysis of the raw EEG. Narcotrend monitor has two recording modes; the one channel mode
as the standard for the assessment of the depth of hypnosis during anesthesia or sedation, and the two channel mode for
comparison of signals from the two hemispheres of the brain. After accounting for the artifacts, a multivariate statistical
algorithm is used for analysis which results in a six-stage classification from A (awake) to F (general anesthesia/coma) and
14 substages [44]. Additionally, the Narcotrend would have less problems with EMG interference than the BIS monitor[45].
This is most likely due to the fact that the Narcotrend modulates the index value with artifact surrogate analysis. The
Narcotrend-guided sedation demonstrated lower hemodynamic changes and fewer complications compared with the
clinical assessment-guided sedation for endoscopic retrograde cholangiopancreatography procedure. However, the
Narcotrend and clinical assessment-guided deep sedation showed comparable propofol dosage and recovery time [46].
7.3 AEP Monitor/ 2
The first commercial monitor based on AEP was introduced by Danmeter in 2001. After further research, the same
company introduced the new version of the monitor. The AEP Monitor/2 (Danmeter A/S, Odense, Denmark) features an
auditory evoked potential (AEP) and EEG-derived hybrid index of the patients hypnotic state. This monitor uses
autoregressive models with exogenous input (ARX) to detect the AEP. The ARX was used because the method enables
fast responses of the monitor [47]. Like other successful monitors the new version of the index also calculates the
AEP-ARX-Index (AAI index), which is a dimensionless number. The AAI index can be displayed on two scales; either
from 0 to 100, or from 0 to 60.
Published by Sciedu Press 123
www.sciedu.ca/jbgc Journal of Biomedical Graphics and Computing, December 2012, Vol. 2, No. 2
Because the EMG is propagated in the same frequency band, the AAI can be influenced by the EMG artifacts. The
decision how the AAI is constructed from AEP and EEG analyses is made by the weighting function, which is based on the
signal to noise ratio. All of the above parameters must be monitored simultaneously in order to ensure optimal
sedation/anesthesia of the patient during general anesthesia[48, 49]. Several studies have compared AAI with BIS and
revealed that the AAI was more sensitive in monitoring depth of anesthesia and in predicting recovery to
consciousness [50, 51].
7.4 PSA 4000 Monitor
The Patient State Analyzer 4000 (PSA) was developed by the Physiometrix, North Billerica, MA and launched in 2001 in
the USA. The PSA monitor calculates the value of the index from four EEG channels. The acquired signals are
pre-processed and an artifact removal algorithm is applied. The Patient State Index (PSI) uses a set of features that best
describe the variances, which are related to the EEG. The development of the PSI algorithm was based on three databases
of EEG records, which were used for development of artifact detection and removal algorithms, classification algorithms
and finally a third database was used for calibrating the index [52]. The PSI is a dimensionless number from 100 (awake)
to 0 (isoelectricity).
7.5 Cerebral State Monitor
The Cerebral State Monitor (CSM) was introduced by the Danmeter Company in 2004.The ability of CSM for separation
of consciousness and unconsciousness was comparable to other commercially available EEG-based devices[53]. Although,
CSM has a simpler algorithm in comparison to Narcotrend and PSI, it is the slowest to respond to a change in sedation. The
study of Hoymork et al. showed that the CSM was a satisfactory alternative to BIS for monitoring hypnotic effect in 87%
of non-paralyzed patients. In 13% of the patients, CSI displayed values indicating an awaked state despite clinical sleep,
all correctly identified with the BIS. However, their study was done with the very first version of the CSM, while the BIS
monitor has undergone several revisions [54].
7.6 Entropy Module
Another way of using EEG data is for the calculation of entropy, which is a measure of the irregularity, complexity or
predictability characteristics of the data [55]. The Entropy Module was introduced in 2003 by the Datex-Ohmeda Company.
The increasing depth of anesthesia causes increase in regularity of the EEG, which can then be inferred by the entropy and
used to estimate the depth of anesthesia.
Two features of this monitor are state entropy (SE) and response entropy (RE). Both are dimensionless numbers between
91-0 and 100-0, respectively. The SE includes information only from EEG, and the RE includes the EMG activity and can
be therefore used as a surrogate parameter. The Entropy monitor is also the anesthetic depth monitor that has been
routinely used in pediatric anesthesia [38, 39].
8 The response time of DGA monitors
One of the most important parameters of the anesthetic depth monitor is its response time to a rapid change in the level of
sedation/anesthesia. The response time is between 30-100 seconds for the transition between EEG suppression and the
awaked state for BIS, Narcotrend and CSM [56]. However, the response time is not constant and is dependent upon the
depth of anesthesia. The time delays of the tested indices may limit their value in prevention of recall of intraoperative
events. Furthermore, different latencies for decreasing and increasing values may indicate a limitation of these monitors
for the pharmacodynamic studies [57].
124 ISSN 1925-4008 E-ISSN 1925-4016
www.sciedu.ca/jbgc Journal of Biomedical Graphics and Computing, December 2012, Vol. 2, No. 2
9 Conclusions
One of the objectives of anesthesia is to ensure adequate depth of anesthesia to prevent the patients awareness. All
available monitors are no predictors whether the depth of anesthesia is sufficient for the painful surgical stimulus. The
anesthetic personnel must consider any technique for monitoring of the depth of anesthesia as an individual help in
improving care for their patients. Recent advances in the introduction of EEG-based monitors have made important
contributions towards understanding of the fundamental changes in brain activity brought about by anesthetic agents. The
development of these monitors, which directly measures the state of consciousness, would also enable a safe and
cost-effective anesthetic procedure.
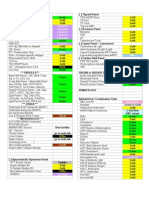
Table. Comparison of anesthetic depth monitors
AEP
BIS Narcotrend PSA 4000 CSM Entropy
Monitor/2
First introduced 1992 2000 2001 2001 2004 2003
Aspect
Datex-Oh
Produced by Medical Monitor Technik Danmeter Physiometrix Danmeter
meda
System
Time delay
Awake to deep 61 sec 26 sec No data No data 55 sec No data
anesthesia
Deep anesthesia to 63 sec 90 sec No data No data 106 sec No data
awake
Electromagnetic
Moderate Moderate No data No data Moderate High
interference
Correlation with Needed more
Yes Yes Yes Yes Yes
clinical signs studies
References
[1] Myles PS. Prevention of awareness during anesthesia. Best Pract Res Clin Anesthesiol. 2007; 21: 345-355.
http://dx.doi.org/10.1016/j.bpa.2007.04.004
[2] Evans JM, Davies WL. Monitoring anesthesia. Clin Anesth. 1984; 2: 243-262.
[3] Anonymous. Practice advisory for intraoperative awareness and brain function monitoring. A report by the American Society of
Anesthesiologists Task Force on intraoperative awareness. Anesthesiology. 2006; 104: 847-864. PMid:16571982
[4] Winterhaltera M, Munted S, Taschenbreckerc P, et al. Skin impedance correlates to sedation grade, plasma propofol concentrations and
bispectral index during a target-controlled infusion of propofol. Eur J Anaesthesiol. 2009; 26: 589-596. PMid:19455042
http://dx.doi.org/10.1097/EJA.0b013e328329b149
[5] Russell IF. Comparison of wakefulness with two anesthetic regimens: total IV balanced anesthesia. Br J Anaesth.1986; 58: 965.
PMid:3756056 http://dx.doi.org/10.1093/bja/58.9.965
[6] Sinha PK, Koshy T. Monitoring devices for measuring the depth of anesthesia-an overview. Indian J Anesth. 2007; 51: 365-381.
[7] Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974; 2: 656-659.
PMid:4835444 http://dx.doi.org/10.1136/bmj.2.5920.656
[8] Olson DW, Lynn M, Thoyre SM, Graffagnino C. The limited reliability of the Ramsay scale. Neurocritical Care. 2007; 7: 227-231.
PMid:17896083 http://dx.doi.org/10.1007/s12028-007-0069-x
[9] Nemethy M, Paroli L, Williams-Russo P, et al. Assessing sedation with regional anesthesia: inter-rater agreement on a Modified Wilson
Sedation scale. Anesth Analg. 2002; 94: 725-728.
[10] Van Dishoeck AM, Van der Hooft T, Simoons ML, et al. Reliable assessment of sedation level in routine clinical practice by adding an
instruction to the Ramsay scale. Eur J Cardiovasc Nurs. 2009; 8: 125-128. PMid:19056319
http://dx.doi.org/10.1016/j.ejcnurse.2008.10.004
[11] Mottahedian TE, Tadrissi SD, Mohammad YA, Ebadi A, Mirhashemi S. Validity and reliability of Ramsay sedation scale in intensive care
unit adult patients. Iranian J Crit Care Nursing. 2010; 3: 39-44.
Published by Sciedu Press 125
www.sciedu.ca/jbgc Journal of Biomedical Graphics and Computing, December 2012, Vol. 2, No. 2
[12] Chernik DA, Gillings D, Laine H, et al. Validity and reliability of the observers assessment of alertness/sedation scale: study with
intravenous midazolam. J Clin Psychopharmacol. 1990; 10: 244-251. PMid:2286697
[13] Amornyotin S, Srikureja W, Pausawasdi N, Prakanrattana U, Kachintorn U. Intravenous sedation for gastrointestinal endoscopy in very
elderly patients of Thailand. Asian Biomed. 2011; 5: 485-491.
[14] Amornyotin S, Kachintorn U, Chalayonnawin W, Kongphlay S. Propofol-based deep sedation for endoscopic retrograde
cholangiopancreatography procedure in sick elderly patients in a developing country. Ther Clin Risk Manag. 2011; 7: 251-255.
PMid:21753887 http://dx.doi.org/10.2147/TCRM.S21519
[15] Amornyotin S, Kongphlay S. Esophagogastroduodenoscopy procedure in sick pediatric patients: a comparison between deep sedation and
general anesthesia technique. J Anesth Clin Res. 2012; 3: 185.
[16] Punjasawadwong Y, Boonjeungmonkol N, Phongchiewboon A. Bispectral index for improving anesthetic delivery and post-operative
recovery. Cochrane Database Syst Rev. 2007; 4: CD003843. PMid:17943802
[17] Hahnenkamp K, Herroeder S, Hollmann MW. Regional anesthesia, local anesthetics and the surgical stress response. Best Pract Res Clin
Anesthesiol. 2004; 18: 509-527. http://dx.doi.org/10.1016/j.bpa.2004.01.004
[18] Luginbuhl M, Ypparila-WoltersH, Rufenacht M, Petersen-Felix S, Korhonen I. Heart rate variability does not discriminate between
different levels of hemodynamic responsiveness during surgical anesthesia. Br J Anesth. 2007; 98: 728-736. PMid:17468493
http://dx.doi.org/10.1093/bja/aem085
[19] Bruhn J, Myles PS, Sneyd R, Struys MM. Depth of anesthesia monitoring: What's available, what's validated and what's next? Br J Anesth.
2006; 97: 85-94. PMid:16751211 http://dx.doi.org/10.1093/bja/ael120
[20] Renna M, Wigmore T, Mofeez A, Gillbe C. Biasing effect of the electromyogram on BIS: a controlled study during high-dose fentanyl
induction. J Clin Monit Comput. 2002; 17: 377-381. PMid:12885182 http://dx.doi.org/10.1023/A:1024210405543
[21] Vretzakis G, Dragoumanis C, Ferdi H, Papagiannopoulou P. Influence of an external pacemaker on bispectral index. Eur J Anaesthesiol.
2005; 22: 70-72. PMid:15816579
[22] Hemmerling TM, Fortier JD. Falsely increased bispectral index values in a series of patients undergoing cardiac surgery using
forced-air-warming therapy of the head. Anesth Analg. 2002; 95: 322-323. PMid:12145044
[23] Gomez LM, Anadon MP, Salvador M, Aldaz M, Raigoso O, Senandez MJ. Increase of bispectral index values due to electrical interference
by the RF 2000 radiofrequency generator during ablation of hepatic metastases. Rev Esp Anestesiol Reanim. 2002; 49: 218-219.
PMid:14606384
[24] Hirota K. Special cases: ketamine, nitrous oxide and xenon. Best Pract Res Clin Anesthesiol. 2006; 20: 69-79.
http://dx.doi.org/10.1016/j.bpa.2005.08.014
[25] Vereecke HE, Struys MM, Mortier EP. A comparison of bispectral index and ARX-derived auditory evoked potential index in measuring
the clinical interaction between ketamine and propofol anesthesia. Anaesthesia. 2003; 58: 957-961. PMid:12969037
http://dx.doi.org/10.1046/j.1365-2044.2003.03403.x
[26] Hirota K, Kubota T, Ishihara H, Matsuki A. The effects of nitrous oxide and ketamine on the bispectral index and 95% spectral edge
frequency during propofol-fentanyl anesthesia. Eur J Anaesthesiol. 1999; 16: 779-783. PMid:10713872
[27] Puri GO. Paradoxical changes in bispectral index during nitrous oxide administration. Br J Anesth. 2001; 86: 141-142. PMid:11575394
http://dx.doi.org/10.1093/bja/86.1.141
[28] Schultz A, Grouven U, Zander I, Beger FA, Siedenberg M, Schultz B. Age-related effects in the EEG during propofol anesthesia. Acta
Anaesthesiol Scand. 2004; 48: 27-34. PMid:14674970 http://dx.doi.org/10.1111/j.1399-6576.2004.00258.x
[29] Ortolani O, Conti A, Ngumi ZW, et al. Ethnic differences in propofol and fentanyl response: a comparison among Caucasians, Kenyan
Africans and Brazilians. Eur J Anaesthesiol. 2004; 21: 314-319.
[30] Kodaka M, Johansen JW, Sebel PS. The influence of gender on loss of consciousness with sevoflurane or propofol. Anesth Analg. 2005;
101: 377-381. http://dx.doi.org/10.1213/01.ANE.0000154534.71371.4F
[31] Schmidlin D, Hager P, Schmid ER. Monitoring level of sedation with bispectral EEG analysis: comparison between hypothermic and
normothermic cardiopulmonary bypass. Br J Anaesth. 2001; 86: 769-776. PMid:11573582 http://dx.doi.org/10.1093/bja/86.6.769
[32] Turnbull D, Furlonger A, Andrzejowski J. The influence of changes in end-tidal carbondioxide upon the Bispectral index. Anaesthesia.
2008; 63: 458-462. PMid:18412642 http://dx.doi.org/10.1111/j.1365-2044.2007.05399.x
[33] Vivien B, Langeron O, Riou B. Increase in bispectral index (BIS) while correcting a severe hypoglycemia. Anesth Analg. 2002; 95:
1824-1825. http://dx.doi.org/10.1097/00000539-200212000-00082
[34] Messner M, Beese U, Romstock J, Dinkel M, Tschaikowsky K. The bispectral index declines during neuromuscular block in fully awake
persons. Anesth Analg. 2003; 97: 488-491. http://dx.doi.org/10.1213/01.ANE.0000072741.78244.C0
[35] Palanca BJ, Mashour GA, Avidan MS. Processed electroencephalogram in depth of anesthesia monitoring. Curr Opin Anesthesiol. 2009;
22: 553-559. PMid:19652597 http://dx.doi.org/10.1097/ACO.0b013e3283304032
[36] Johansen JW, Sebel PS. Development and clinical application of electroencephalographic bispectrum monitoring. Anesthesiology. 2000;
93: 1336-1344. PMid:11046224 http://dx.doi.org/10.1097/00000542-200011000-00029
[37] Consales G, Chelazzi C, Rinaldi S, De Gaudio AR. Bispectral index compared to Ramsay score for sedation monitoring in intensive care
units. Minerva Anestesiol. 2006; 72: 329-336. PMid:16675941
126 ISSN 1925-4008 E-ISSN 1925-4016
www.sciedu.ca/jbgc Journal of Biomedical Graphics and Computing, December 2012, Vol. 2, No. 2
[38] Powers KS, Nazarian EB, Tapyrik SA, et al. Bispectral index as a guide for titration of propofol during procedural sedation among
children. Pediatrics. 2005; 115: 1666-1674. PMid:15930231 http://dx.doi.org/10.1542/peds.2004-1979
[39] Klockars JG, Hiller A, Ranta S, et al. Spectral entropy as a measure of hypnosis in children. Anesthesiology. 2006; 104: 708-717.
PMid:16571966 http://dx.doi.org/10.1097/00000542-200604000-00015
[40] Wehrmann T, Grotkamp J, Stergiou N, et al. Electroencephalogram monitoring facilitates sedation with propofol for routine ERCP: a
randomized controlled trial. Gastrointest Endosc. 2002; 56:817-824. http://dx.doi.org/10.1016/S0016-5107(02)70353-2
[41] Chen SC, Rex DK. An initial investigation of bispectral monitoring as an adjunct to nurse-administered propofol sedation for colonoscopy.
Am J Gastroenterol. 2004; 99: 1081-1086. PMid:15180729 http://dx.doi.org/10.1111/j.1572-0241.2004.03279.x
[42] Drake LM, Chen SC, Rex DK. Efficacy of Bispectral monitoring as an adjunct to nurse-administered propofol sedation for colonoscopy: a
randomized controlled trial. Am J Gastroenterol. 2006; 101: 2003-2007. PMid:16968506
http://dx.doi.org/10.1111/j.1572-0241.2006.00806.x
[43] DeWitt JM. Bispectral index monitoring for nurse-administered propofol sedation during upper endoscopic ultrasound: a prospective,
randomized controlled trial. Dig Dis Sci. 2008; 53: 2739-2745. PMid:18274899 http://dx.doi.org/10.1007/s10620-008-0198-x
[44] Kreuer S, Biedler A, Larsen R, Altmann S, Wilhelm W. Narcotrend monitoring allows faster emergence and a reduction of drug
consumption in propofol-remifentanil anesthesia. Anesthesiology. 2003; 99: 34-41. PMid:12826839
http://dx.doi.org/10.1097/00000542-200307000-00009
[45] Panousis P, Heller AR, Burghardt M, Bleyl JU, Koch T. The effects ofelectromyographic activity on the accuracy of the Narcotrend
monitor compared with the Bispectral index during combined anesthesia. Anaesthesia. 2007; 62: 868-874. PMid:17697211
http://dx.doi.org/10.1111/j.1365-2044.2007.05145.x
[46] Amornyotin S, Chalayonnawin W, Kongphlay S. Deep sedation for endoscopic retrograde cholangiopancreatography: a comparison
between clinical assessment and NarcotrendTM monitoring. Med Devices: Evid Res. 2011; 4: 43-49. PMid:22915929
http://dx.doi.org/10.2147/MDER.S17236
[47] Weber F, Zimmermann M, Bein T. The impact of acoustic stimulation on the AEP Monitor/2 derived composite auditory evoked potential
index under awake and anesthetized conditions. Anesth Analg. 2005; 101: 435-439.
http://dx.doi.org/10.1213/01.ANE.0000158470.34024.EF
[48] Plourde G. Auditory evoked potentials. Best Pract Res Clin Anesthesiol. 2006; 20: 129-139. http://dx.doi.org/10.1016/j.bpa.2005.07.012
[49] Horn B, Pilge S, Kochs EF, Stockmanns G, Hock A, Schneider G. A combination of electroencephalogram and auditory evoked potentials
separates different levels of anesthesia in volunteers. Anesth Analg. 2009; 108: 1512-1521.
http://dx.doi.org/10.1213/ane.0b013e3181a04d4c
[50] Gajraj RJ, Doi M, Mantzaridis H, Kenny GNC. Comparison of bispectral EEG analysis and auditory evoked potentials for monitoring
depth of anesthesia during propofol anesthesia. Br J Anaesth. 1999; 82: 672-678. PMid:10536541 http://dx.doi.org/10.1093/bja/82.5.672
[51] Nishiyama T, Hanaoka K. The A-line ARX index may be a more sensitive detector of arousal than the bispectral index during
propofol-fentanyl-nitrous oxide anesthesia: a preliminary investigation. Can J Anesth. 2004; 51: 539-544. PMid:15197114
http://dx.doi.org/10.1007/BF03018394
[52] Drover DR, Lemmens HJ, Pierce ET, et al. Patient state index. Anesthesiology. 2002; 97: 82-89. PMid:12131107
http://dx.doi.org/10.1097/00000542-200207000-00012
[53] Pilge S, Blum J, Kochs EF, Schoniger SA, Kreuzer M, Schneider G. Does the Cerebral State Index separate consciousness from
unconsciousness? Anesth Analg. 2011; 113: 1403-1410. http://dx.doi.org/10.1213/ANE.0b013e31823007cd
[54] Hoymork SC, Hval K, Jensen EW, Raeder J. Can the Cerebral State Monitor replace the Bispectral index in monitoring hypnotic effect
during propofol/remifentanil anesthesia? Acta Anaesthesiol Scand. 2007; 51: 210-216. PMid:17330331
http://dx.doi.org/10.1111/j.1399-6576.2006.01213.x
[55] Bruhn J, Lehmann LE, Ropcke H, et al. Shannon entropy applied to the measurement of the electroencephalographic effects of desflurane.
Anesthesiology. 2001; 95: 30-55. PMid:11465580 http://dx.doi.org/10.1097/00000542-200107000-00010
[56] Zanner R, Pilge S, Kochs EF, Kreuzer M, Schneider G. Time delay ofelectroencephalogram index calculation: analysis of cerebral state,
bispectral, and Narcotrend indices using perioperatively recorded electroencephalographic signals. Br J Anaesth. 2009; 103: 394-399.
PMid:19648154 http://dx.doi.org/10.1093/bja/aep198
[57] Pilge S, Zanner R, Schneider G, et al. Time delay of index calculation: analysis of cerebral state, bispectral, and Narcotrend indices.
Anesthesiology. 2006; 104: 488-494. PMid:16508396 http://dx.doi.org/10.1097/00000542-200603000-00016
Published by Sciedu Press 127
S-ar putea să vă placă și
- Awareness During AnesthesiaDocument40 paginiAwareness During Anesthesiadr_nkhan3415Încă nu există evaluări
- DR Makam Sri Harsha ThesisDocument33 paginiDR Makam Sri Harsha ThesissumitÎncă nu există evaluări
- Diagnostics Assessment Programme Depth of Anaesthesia Monitors (E-Entropy, BIS and Narcotrend) Final ScopeDocument15 paginiDiagnostics Assessment Programme Depth of Anaesthesia Monitors (E-Entropy, BIS and Narcotrend) Final ScopeMinaz PatelÎncă nu există evaluări
- Advances in Awareness Monitoring TechnologiesDocument6 paginiAdvances in Awareness Monitoring TechnologiesEdwin SanchezÎncă nu există evaluări
- PRACTICE Advisories Are Systematically Developed Reports That Are Intended To AssistDocument4 paginiPRACTICE Advisories Are Systematically Developed Reports That Are Intended To AssistFadhillawatie MaanaiyaÎncă nu există evaluări
- 1-Definitions:: Quality Management UNIT - 2010Document11 pagini1-Definitions:: Quality Management UNIT - 2010EsamÎncă nu există evaluări
- Nihms-1579274 PDFDocument23 paginiNihms-1579274 PDFAhmed ElshewiÎncă nu există evaluări
- Update On Multimodality MonitoDocument8 paginiUpdate On Multimodality MonitoConstanza Andrea Saldivia Blanco(RedSalud Magallanes)Încă nu există evaluări
- Neurologic Monitoring in MedicalDocument5 paginiNeurologic Monitoring in MedicalMark Russel Sean LealÎncă nu există evaluări
- Sedation Vacation in The ICU: Sandeep Sharma Dominic J. Valentino IIIDocument8 paginiSedation Vacation in The ICU: Sandeep Sharma Dominic J. Valentino IIIFebri Yudha Adhi KurniawanÎncă nu există evaluări
- RCCM 200204-270ccDocument5 paginiRCCM 200204-270ccJunior BarretoÎncă nu există evaluări
- Sedatives in Neurocritical Care 2019 Curr Opin Crit CareDocument8 paginiSedatives in Neurocritical Care 2019 Curr Opin Crit CareCAMILO ERNESTO DAZA PERDOMOÎncă nu există evaluări
- Neuro in The ICUDocument4 paginiNeuro in The ICUEduardo GarciaÎncă nu există evaluări
- Procedural Sedation AnalgesiaDocument24 paginiProcedural Sedation Analgesiabenitez1228Încă nu există evaluări
- Moderate Sedation Provider PacketDocument55 paginiModerate Sedation Provider PacketAhmed ElshewiÎncă nu există evaluări
- Sedation, Delirium, and Cognitive Function After Criticall IlnessDocument14 paginiSedation, Delirium, and Cognitive Function After Criticall IlnessPsiquiatría CESAMEÎncă nu există evaluări
- Monitored Anaesthesia Care (MAC)Document6 paginiMonitored Anaesthesia Care (MAC)Kamrul HassanÎncă nu există evaluări
- ASA Guidelines For Sedation and AnalgesiaDocument14 paginiASA Guidelines For Sedation and AnalgesiamichaelÎncă nu există evaluări
- 290 Residual Neuromuscular BlockadeDocument8 pagini290 Residual Neuromuscular BlockadeTias Diah100% (1)
- Hongliang Mao Short and Long Term Response of VagusDocument16 paginiHongliang Mao Short and Long Term Response of VagusArbey Aponte PuertoÎncă nu există evaluări
- Pe 2 3 36Document6 paginiPe 2 3 36Oslo SaputraÎncă nu există evaluări
- ICU ProtocolsDocument35 paginiICU ProtocolsJohn Reynolds100% (6)
- Anesthesia Barash Key Points Chapter 1-9Document8 paginiAnesthesia Barash Key Points Chapter 1-9Jed MostajoÎncă nu există evaluări
- MirasolDocument7 paginiMirasolJan Chrispian MirasolÎncă nu există evaluări
- Good Morning EveryoneDocument6 paginiGood Morning EveryoneRichlle CortesÎncă nu există evaluări
- Delirium in The Intensive Care UnitDocument9 paginiDelirium in The Intensive Care Uniton miniÎncă nu există evaluări
- Haemodynamic Monitoring & Manipulation: an easy learning guideDe la EverandHaemodynamic Monitoring & Manipulation: an easy learning guideÎncă nu există evaluări
- HshsjneDocument5 paginiHshsjneyunia habsariÎncă nu există evaluări
- The Effect of Foot Reflexive Massage On The Physiological Indexes of Cerebrovascular Accident (CVA) PatientsDocument7 paginiThe Effect of Foot Reflexive Massage On The Physiological Indexes of Cerebrovascular Accident (CVA) PatientsYusra DelfinÎncă nu există evaluări
- Upper Airway Stimulation For Obstructive Sleep Apnea: Durability of The Treatment Effect at 18 MonthsDocument9 paginiUpper Airway Stimulation For Obstructive Sleep Apnea: Durability of The Treatment Effect at 18 MonthsHamzeh AlsalhiÎncă nu există evaluări
- Tham 2010Document13 paginiTham 2010Santosa TandiÎncă nu există evaluări
- Stereoelectroencephalography Versus Subdural ElectrodeDocument9 paginiStereoelectroencephalography Versus Subdural ElectrodedhruvaÎncă nu există evaluări
- Anestesia 1Document22 paginiAnestesia 1Carlos MÎncă nu există evaluări
- Sem6 - Acute Non-Traumatic WeaknessDocument20 paginiSem6 - Acute Non-Traumatic WeaknessJenifer PerezÎncă nu există evaluări
- South Erland 2016Document38 paginiSouth Erland 2016jennyfilgueira001Încă nu există evaluări
- Ni Hms 666511Document13 paginiNi Hms 666511Sean JamesÎncă nu există evaluări
- Neurological Complications of Surgery and AnaesthesiaDocument14 paginiNeurological Complications of Surgery and Anaesthesiarian rantungÎncă nu există evaluări
- 2018 08 AbstractsDocument33 pagini2018 08 AbstractsAchyut Giridhar DasÎncă nu există evaluări
- MCQ Anaesthesia QuestionsDocument8 paginiMCQ Anaesthesia QuestionsOanamikaela VaidaÎncă nu există evaluări
- Targeted Treatment of Severe Head InjuryDocument4 paginiTargeted Treatment of Severe Head InjuryAstari RahayuningtyasÎncă nu există evaluări
- DeliriumDocument15 paginiDeliriumRobin gruÎncă nu există evaluări
- Merge Merge Merge MergeDocument3 paginiMerge Merge Merge MergeJade CentinoÎncă nu există evaluări
- PTJ 1006Document9 paginiPTJ 1006sundar_kumar0Încă nu există evaluări
- iCU Delirium-A Diagnostic and Therapeutic Challenge in The Intensive Care UnitDocument13 paginiiCU Delirium-A Diagnostic and Therapeutic Challenge in The Intensive Care UnitTai rascunhos TaiÎncă nu există evaluări
- Neorologycal PhysioterapyDocument4 paginiNeorologycal PhysioterapyDiana-Silva RestyeÎncă nu există evaluări
- Sleep Hypoventilation in Neuromuscular and Chest Wall DisordersDocument15 paginiSleep Hypoventilation in Neuromuscular and Chest Wall Disorderssavvy_as_98-1Încă nu există evaluări
- Tambahan Nonvolatile AnastesiDocument6 paginiTambahan Nonvolatile AnastesiNaina Shin HyeÎncă nu există evaluări
- Practice Advisory For Intraoperative Awareness and Brain Function MonitoringDocument18 paginiPractice Advisory For Intraoperative Awareness and Brain Function MonitoringBig TexÎncă nu există evaluări
- Rapid Focused Neurological Assessment in The Emergency Department and ICUDocument16 paginiRapid Focused Neurological Assessment in The Emergency Department and ICUAnnie RicoÎncă nu există evaluări
- Medico Legal Aspects of Severe Traumatic Brain InjuryDocument17 paginiMedico Legal Aspects of Severe Traumatic Brain InjuryIrv CantorÎncă nu există evaluări
- Direct Accuracy Performance Comparison of Cerebral Oximeter Devices - AANA Journal CoursesDocument8 paginiDirect Accuracy Performance Comparison of Cerebral Oximeter Devices - AANA Journal CoursesRaluca LÎncă nu există evaluări
- Perioperative Management of Neurological ConditionsDocument8 paginiPerioperative Management of Neurological ConditionsDra Claudia AranedaÎncă nu există evaluări
- Procedural Sedation in Children - Preparation - UpToDateDocument26 paginiProcedural Sedation in Children - Preparation - UpToDaterogelio cruzÎncă nu există evaluări
- Herni Suprapti DR MkesDocument52 paginiHerni Suprapti DR MkesHerry HermawanÎncă nu există evaluări
- Procedural Sedation in Adults Outside The Operating Room - UpToDateDocument32 paginiProcedural Sedation in Adults Outside The Operating Room - UpToDatehatsuneÎncă nu există evaluări
- Clinical Practice Guidelines For Physical Therapy in Patients With Intermittent ClaudicationDocument51 paginiClinical Practice Guidelines For Physical Therapy in Patients With Intermittent ClaudicationsilkofosÎncă nu există evaluări
- Principles of Monitoring Postoperative Patients: Oleh: Meity Sarah 2012610108Document8 paginiPrinciples of Monitoring Postoperative Patients: Oleh: Meity Sarah 2012610108Jefry ArieÎncă nu există evaluări
- Physiotherapy Interventions For A Traumatic Brain Injury Patient: A Case StudyDocument5 paginiPhysiotherapy Interventions For A Traumatic Brain Injury Patient: A Case StudymunaazizahÎncă nu există evaluări
- Sedation and Anesthesia in GI Endoscopy 2008Document12 paginiSedation and Anesthesia in GI Endoscopy 2008Siva SankarÎncă nu există evaluări
- Jurnal App PDFDocument6 paginiJurnal App PDFInggriht Senny BondangÎncă nu există evaluări
- N % Cases Valid 20 100.0 Excluded 0 .0 Total 20 100.0 A. Listwise Deletion Based On All Variables in The ProcedureDocument1 paginăN % Cases Valid 20 100.0 Excluded 0 .0 Total 20 100.0 A. Listwise Deletion Based On All Variables in The ProcedureLestari Chye PouedanÎncă nu există evaluări
- Bab IDocument3 paginiBab ILestari Chye PouedanÎncă nu există evaluări
- Seminar On EltDocument15 paginiSeminar On EltLestari Chye PouedanÎncă nu există evaluări
- Jurnal App PDFDocument4 paginiJurnal App PDFBrinaÎncă nu există evaluări
- Monitored Anesthesia Care An OverviewDocument3 paginiMonitored Anesthesia Care An OverviewLestari Chye PouedanÎncă nu există evaluări
- Diabetic Foot Guidelines 2006Document68 paginiDiabetic Foot Guidelines 2006Elizabeth BrugesÎncă nu există evaluări
- Arm 39 735Document10 paginiArm 39 735Lestari Chye PouedanÎncă nu există evaluări
- C01110916 PDFDocument8 paginiC01110916 PDFLestari Chye PouedanÎncă nu există evaluări
- Akut Kolangitis PDFDocument5 paginiAkut Kolangitis PDFDhen Mas PrimanaÎncă nu există evaluări
- Acute Calculous Cholecystitis: Clinical PracticeDocument8 paginiAcute Calculous Cholecystitis: Clinical PracticeLestari Chye PouedanÎncă nu există evaluări
- IndianJAnaesth575472-2540068 070320Document9 paginiIndianJAnaesth575472-2540068 070320Lestari Chye PouedanÎncă nu există evaluări
- Acute Appendicitis - Evidence Based ManagementDocument4 paginiAcute Appendicitis - Evidence Based ManagementAlex Toman Fernando SaragihÎncă nu există evaluări
- Clayton, 2009Document7 paginiClayton, 2009Anggie AnggriyanaÎncă nu există evaluări
- Volume N Occupation Study Occupationl Asthma National 45allasp1Document4 paginiVolume N Occupation Study Occupationl Asthma National 45allasp1Lestari Chye PouedanÎncă nu există evaluări
- Judul EsterDocument1 paginăJudul EsterLestari Chye PouedanÎncă nu există evaluări
- Clayton, 2009Document7 paginiClayton, 2009Anggie AnggriyanaÎncă nu există evaluări
- Judul Thesis MurinyDocument1 paginăJudul Thesis MurinyLestari Chye PouedanÎncă nu există evaluări
- Summary JejeDocument1 paginăSummary JejeLestari Chye PouedanÎncă nu există evaluări
- MuriniDocument8 paginiMuriniLestari Chye PouedanÎncă nu există evaluări
- Jurnal JOCM Work Related AsmaDocument10 paginiJurnal JOCM Work Related AsmahazaziÎncă nu există evaluări
- Monitored Anesthesia Care An OverviewDocument3 paginiMonitored Anesthesia Care An OverviewLestari Chye PouedanÎncă nu există evaluări
- Volume N Occupation Study Occupationl Asthma National 45allasp1Document4 paginiVolume N Occupation Study Occupationl Asthma National 45allasp1Lestari Chye PouedanÎncă nu există evaluări
- SummarysabethDocument2 paginiSummarysabethLestari Chye PouedanÎncă nu există evaluări
- Management of The Traumatized AirwayDocument8 paginiManagement of The Traumatized AirwayAnonymous h0DxuJTÎncă nu există evaluări
- Trauma Airway Management GuidelinesDocument6 paginiTrauma Airway Management GuidelinesLestari Chye PouedanÎncă nu există evaluări
- Airway Adjuncts Fact and SkillDocument4 paginiAirway Adjuncts Fact and Skillfpanaguiton13Încă nu există evaluări
- Geudels Chart Final WEBDocument12 paginiGeudels Chart Final WEBLestari Chye PouedanÎncă nu există evaluări
- AirwaysDocument2 paginiAirwaysLestari Chye PouedanÎncă nu există evaluări
- Phenylephrine HydrochlorideDocument5 paginiPhenylephrine HydrochlorideRoger Jr PumarenÎncă nu există evaluări
- DRUGSDocument4 paginiDRUGSHoney Grace L LemorenasÎncă nu există evaluări
- Strengthening Quality Midwifery Education For 2030 - Who Unfpa Unicef 20Document4 paginiStrengthening Quality Midwifery Education For 2030 - Who Unfpa Unicef 20Sheilla Tania MarcelinaÎncă nu există evaluări
- Form 5 Chemistry Folio - MedicineDocument37 paginiForm 5 Chemistry Folio - MedicineHeon50% (2)
- Selected Instructional Course LecturesDocument27 paginiSelected Instructional Course LecturesAhmad ShakirÎncă nu există evaluări
- BestDocument25 paginiBestAlejandro Lopez OsorioÎncă nu există evaluări
- Fullsize SBAR Report SheetDocument1 paginăFullsize SBAR Report SheetShane LambertÎncă nu există evaluări
- Nicotiana Tabacum: Topic: Created byDocument20 paginiNicotiana Tabacum: Topic: Created byfurqan baigÎncă nu există evaluări
- AscarisDocument16 paginiAscarisRommy Kurniawan DeskyÎncă nu există evaluări
- MBB 1 Handout 1 and What About BiotechnologyDocument4 paginiMBB 1 Handout 1 and What About BiotechnologyMariah Shanice BasaÎncă nu există evaluări
- Teaching Experience Log All - Sarah WedeDocument2 paginiTeaching Experience Log All - Sarah Wedeapi-647779956Încă nu există evaluări
- NCM 106 IntroductionDocument126 paginiNCM 106 IntroductionYra JhaneÎncă nu există evaluări
- Reflective Functioning: A ReviewDocument11 paginiReflective Functioning: A ReviewNeilermind100% (1)
- Lavender Lavender Lavender Lavender Lavender Lavender: UrineDocument3 paginiLavender Lavender Lavender Lavender Lavender Lavender: UrineJonathan A. Sarmiento67% (6)
- Physical Injuries of Oral CavityDocument57 paginiPhysical Injuries of Oral Cavitygud4nothing50% (2)
- Hepatitis in Children: DR Hamza BawumiaDocument36 paginiHepatitis in Children: DR Hamza BawumiaHamza BawumiaÎncă nu există evaluări
- 544 Prophetic MedicineDocument6 pagini544 Prophetic MedicineMohd HasanÎncă nu există evaluări
- Guia UnimaxDocument2.063 paginiGuia UnimaxClarineMontezzanaÎncă nu există evaluări
- Mary Oliver - US History Final ProjectDocument6 paginiMary Oliver - US History Final ProjectMary OliverÎncă nu există evaluări
- 13 Rekapan Amprahan Ranap Jan 2019Document242 pagini13 Rekapan Amprahan Ranap Jan 2019sisca yolizaÎncă nu există evaluări
- Paneer Do DaDocument7 paginiPaneer Do Darockingtwo07Încă nu există evaluări
- MSDS Refrigerant R407CDocument8 paginiMSDS Refrigerant R407Chambali bimatamaÎncă nu există evaluări
- Music TherapyDocument7 paginiMusic Therapyzakir2012Încă nu există evaluări
- Inhibidores de La ECADocument16 paginiInhibidores de La ECAFarmaFMÎncă nu există evaluări
- Moretsu Shain (Fanatical Workers) and Yoi Kigyo Senshi (Good Corporate Soldiers)Document7 paginiMoretsu Shain (Fanatical Workers) and Yoi Kigyo Senshi (Good Corporate Soldiers)Erwin Alvih Taufik HidayatÎncă nu există evaluări
- Ineffective Health MaintenanceDocument6 paginiIneffective Health MaintenanceRYAN SAPLADÎncă nu există evaluări
- Paediatric Clerking SheetDocument5 paginiPaediatric Clerking SheetIamTinesh100% (2)
- MDMA PowerpointDocument16 paginiMDMA Powerpointapi-26938624Încă nu există evaluări
- Antifungal Susceptibility Pattern Against Dermatophytic Strains Isolated From Humans in Anambra State, NigeriaDocument8 paginiAntifungal Susceptibility Pattern Against Dermatophytic Strains Isolated From Humans in Anambra State, NigeriaIJAERS JOURNALÎncă nu există evaluări
- NCP Ineffective Airway Clearance Related To Lung Impairment PNEUMOTHORAXDocument5 paginiNCP Ineffective Airway Clearance Related To Lung Impairment PNEUMOTHORAXMa. Elaine Carla Tating0% (2)