Documente Academic
Documente Profesional
Documente Cultură
Toxicology: Membrane Transporter Mediated Drug Interactions
Încărcat de
AlexThomas.aTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Toxicology: Membrane Transporter Mediated Drug Interactions
Încărcat de
AlexThomas.aDrepturi de autor:
Formate disponibile
1
TOXICOLOGY
NEWSLETTER
“The art of healing comes from nature, not from the physician.
Therefore, the physician must start from nature, with an open
mind.”
-Paracelsus (1493-1541)
January 2018
Membrane Transporter Mediated Drug Interactions
Abstract: Carrier proteins bind specific solutes and transfer them across
the lipid bilayer by undergoing conformational changes that expose the
solute-binding site sequentially on one side of the membrane and then on
the other. Some carrier proteins simply transport a single solute
“downhill,” whereas others can act as pumps to transport a solute “uphill”
against its electrochemical gradient, using energy provided by ATP
hydrolysis, by a downhill flow of another solute (such as Na+ or H+), or by
light to drive the requisite series of conformational changes in an orderly
manner. Carrier proteins belong to a small number of families. Each family
comprises proteins of similar amino acid sequence that are thought to have
evolved from a common ancestral protein and to operate by a similar
mechanism. Membrane transporters can have clinically relevant effects on
the pharmacokinetics and pharmacodynamics of a drug in various organs
and tissues by controlling its absorption, distribution, and elimination. In
contrast to drug metabolizing enzymes that are largely expressed in the
liver and small intestines, transporters are expressed in tissues throughout
the human body and govern the access of endogenous and exogenous
substances to various sites in the body. Transporters, in concert with
metabolizing enzymes, can govern a drug’s disposition and
pharmacological action. Conversely, a drug can also modulate transporter
expression or activity, resulting in altered disposition of endogenous (e.g.,
creatinine, glucose) or exogenous substances.
Key words: Carrier proteins, electrochemical gradient, membrane
transporters, metabolizing enzymes.
Membrane Transporter Mediated Drug Interactions
2
INTRODUCTION
A membrane transport protein (or simply transporter) is a membrane protein
involved in the movement of ions, small molecules, or macromolecules, such
as another protein, across a biological membrane. The process by which a
carrier protein transfers a solute molecule across the lipid bilayer resembles an
enzyme-substrate reaction, and in many ways carriers behave like enzymes. In
contrast to ordinary enzyme-substrate reactions, however, the transported
solute is not covalently modified by the carrier protein, but instead is delivered
unchanged to the other side of the membrane.
Each type of carrier protein has one or more specific binding sites for its solute
(substrate). It transfers the solute across the lipid bilayer by undergoing
reversible conformational changes that alternately expose the solute-binding
site first on one side of the membrane and then on the other. When the carrier
is saturated (that is, when all solute-binding sites are occupied), the rate of
transport is maximal. This rate, referred to as Vmax, is characteristic of the
specific carrier and reflects the rate with which the carrier can flip between its
two conformational states. In addition, each transporter protein has a
characteristic binding constant for its solute, Km, equal to the concentration of
solute when the transport rate is half its maximum value. As with enzymes, the
binding of solute can be blocked specifically by either competitive inhibitors
(which compete for the same binding site and may or may not be transported
by the carrier) or noncompetitive inhibitors (which bind elsewhere and
specifically alter the structure of the carrier).
Some carrier proteins simply transport a single solute from one side of the
membrane to the other at a rate determined by Vmax and Km; they are called
uniporters. Others, with more complex kinetics, function as coupled carriers, in
which the transfer of one solute strictly depends on the transport of a second.
Coupled transport involves either the simultaneous transfer of a second solute
in the same direction, performed by symporters, or the transfer of a second
solute in the opposite direction, performed by antiporters.
Membrane Transporter Mediated Drug Interactions
3
Membrane transporters can have clinically relevant effects on the
pharmacokinetics and pharmacodynamics of a drug in various organs and
tissues by controlling its absorption, distribution, and elimination. In contrast
to drug metabolizing enzymes that are largely expressed in the liver and small
intestines, transporters are expressed in tissues throughout the human body and
govern the access of endogenous and exogenous substances to various sites in
the body. Transporters, in concert with metabolizing enzymes, can govern a
drug’s disposition and pharmacological action. Conversely, a drug can also
modulate transporter expression or activity, resulting in altered disposition of
endogenous (e.g., creatinine, glucose) or exogenous substances.
Several transporters interact with drugs in clinical use, for example:
• P-glycoprotein {P-gp or Multi-Drug Resistance 1 (MDR1) protein}
• Breast Cancer Resistance Protein (BCRP)
• Organic Anion Transporting Polypeptide 1B1/1B3 (OATP1B1/OATP1B3)
• Organic Anion Transporter 1/3 (OAT1/OAT3)
• Multidrug and Toxin Extrusion (MATE) proteins
• Organic Cation Transporter 2 (OCT2)
Understanding whether the drug is a substrate or perpetrator (i.e., inhibitor or
inducer) of these key transporters can explain some clinical consequences,
such as increased toxicity or altered efficacy, that result from altered tissue
distribution of a drug that is a substrate of a transporter.
For example, if the intended population is likely to use statins, the sponsor
should examine the potential of the investigational drug to interact with
OATP1B1/1B3 before clinical studies in patients. If in vitro experiments
indicate a low potential for an interaction between the transporter and
investigational drug, subjects taking statins may be included in clinical studies
to better represent the intended patient population.
Membrane Transporter Mediated Drug Interactions
4
A. Determining if the Investigational Drug is a Substrate of the
Transporters P-gp and BCRP
P-gp and BCRP are expressed in various tissues including the
gastrointestinal tract, liver, kidney, and brain. Thus, both transporters have
the potential to impact the oral bioavailability, the tissue distribution, and
the hepatic and renal elimination of substrates.
P-gp and BCRP are not expected to impact the oral bioavailability of
highly permeable and highly soluble drugs. In vitro assessment of these drugs
as P-gp or BCRP substrates is not suggested unless there are potential safety
concerns with the drug distributing into tissues (e.g., the kidney and brain).
The following results suggest that an investigational drug is an in vitro P-gp
substrate:
a. A net flux ratio (or efflux ratio (ER)) of ≥ 2 for an investigational drug
in cells that express P-gp (e.g., Caco-2 cells or other cells over
expressing P-gp)
A flux that is inhibited by at least one known P-gp inhibitor at a concentration
of at least 10 times its Ki (e.g., the ER decreases to < 50% of the ER in the
absence of inhibitor or the flux reduced to unity).
When using Caco-2 cells that express multiple efflux transporters, the sponsor
should use more than one P-gp inhibitor to determine the specificity of the
efflux. One may consider using a net flux ratio cutoff other than 2 or a specific
relative ratio to positive controls.
If in vitro studies indicate that a drug is a P-gp substrate, the sponsor should
consider whether to conduct an in vivo study based on the drug’s safety
margin, therapeutic index, and likely concomitant medications that are known
P-gp inhibitors in the indicated patient population.
If in vitro studies indicate that a drug is a BCRP substrate, then one should
Membrane Transporter Mediated Drug Interactions
5
consider whether to conduct an in vivo study based on the drug’s safety
margin, therapeutic index, and likely concomitant medications that are known
BCRP inhibitors in the indicated patient population.
B. Determining if the Investigational Drug is a Substrate of the Hepatic
Transporters OATP1B1 and OATP1B3
OATP1B1 and OATP1B3 are key uptake transporters expressed on the
sinusoidal membrane of hepatocytes and play a key role in the hepatic uptake
of various drugs.
If in vitro studies or human/animal absorption, distribution, metabolism,
and/or excretion (ADME) data suggest that an investigational drug’s hepatic
uptake or elimination is significant (i.e., the drug’s clearance through hepatic
metabolism or biliary secretion is ≥ 25% of the total drug’s clearance), or the
drug’s uptake into the liver is clinically important (e.g., for biotransformation
or to exert a pharmacological effect), the sponsor should evaluate the
investigational drug in vitro to determine whether it is a substrate for the
hepatic uptake transporters OATP1B1 and OATP1B3.
An investigational drug is considered an in vitro substrate for OATP1B1 or
OATP1B3 if: (1) the uptake of the drug in OATP1B1- or OATP1B3-
transfected cells is ≥ 2-fold of the drug’s uptake in empty vector-transfected
cells; and (2) a known inhibitor (e.g., rifampin) can decrease the drug’s uptake
to ≤ 50% at a concentration at least 10 times that of the Ki or IC50.
If in vitro studies indicate that a drug is an OATP1B1 or OATP1B3 substrate,
the sponsor should consider whether to conduct an in vivo study based on the
drug’s safety margin, therapeutic index, and likely co-medications that are
known OATP1B1 or OATP1B3 inhibitors in the indicated patient populations.
Membrane Transporter Mediated Drug Interactions
6
C. Determining if the Investigational Drug is a Substrate of the Renal
Transporters OAT, OCT, and MATE
OAT1, OAT3, and OCT2 are renal transporters expressed on the basolateral
membrane of the renal proximal tubule. MATE1 and MATE2-K are expressed
on the brush border membrane. All of the aforementioned renal transporters
can play a role in the active renal secretion of investigational drugs.
If the investigational drug’s ADME data suggest that active renal secretion is
significant for a drug (i.e., active secretion of the parent drug by the kidney is
≥ 25% of the total clearance), then one should evaluate the drug in vitro to
determine whether it is a substrate of OAT1/3, OCT2 and MATE1 and
MATE2-K.
The investigational drug is an in vitro substrate for the renal transporters if: (1)
the ratio of the investigational drug’s uptake in the cells expressing the
transporter versus the drug’s uptake in control cells (or cells containing an
empty vector) is ≥ 2; and (2) a known inhibitor of the transporter decreases the
drug’s uptake to ≤ 50% at a concentration at least 10 times its Ki or IC50.
If in vitro studies indicate that a drug is a substrate of one or more of the renal
transporters, one should consider whether to conduct an in vivo study based on
the drug’s safety margin, therapeutic index, and likely concomitant
medications that are known inhibitors of these renal transporters in the
indicated patient populations.
D. Determining if the Investigational Drug is an Inhibitor of a
Transporter
The investigator should conduct in vitro studies to evaluate whether an
investigational drug is an inhibitor of P-gp, BCRP, OATP1B1, OATP1B3,
OCT2, MATEs (MATE-1, MATE-2K), OAT1, and OAT3.
Membrane Transporter Mediated Drug Interactions
7
a. P-gp and BCRP: The investigator should conduct studies to determine
if an investigational drug inhibits the net flux of a known P-gp or
BCRP substrate in Caco-2, P-gp- or BCRP-over expressed cells and
determine the drug’s inhibition potency (i.e., IC50 or Ki). The
investigational drug has the potential to inhibit P-gp or BCRP in vivo if
the investigational drug is administered orally, and the Igut /IC50 ≥10
where Igut = dose of inhibitor/250 mL.
b. ATP1B1 and OATP1B3: The investigator should conduct studies to
determine the inhibition potency (i.e., IC50 or Ki) of the investigational
drug on the uptake of a known OATP1B1 orOATP1B3 substrate in
cells over expressing the relevant transporter. Because some
knownOATP1B1/3 inhibitors demonstrate time-dependent inhibition,
the sponsor should determineIC50 values following pre-incubation
with the investigational drug for a minimum of 30 minutes. The
investigational drug has the potential to inhibit OATP1B1/3 in vivo if
the R value is > 1.1.
c. OAT, OCT, and MATE: The investigator should conduct studies to
determine the inhibition potency (i.e., IC50 or Ki) of the investigational
drug on the uptake of a known substrate for renal transporters (i.e.,
OAT1, OAT3, OCT2, MATE1, and MATE2K) in cells over expressing
these transporters. The investigational drug has the potential to inhibit
these transporters in vivo if themaximal unbound plasma concentration
of the interactingdrug (Imax,u) IC50 value is ≥ 0.1 for
OAT1/OAT3/OCT2 or the Imax,u/IC50 value is ≥ 0.02 for MATEs.
Creatinine is also a substrate for OCT2, MATEs, and OAT2. Elevated
serum creatinine levels is observed in clinical studies could be due to
inhibition of these transporters by the investigational drug.
Membrane Transporter Mediated Drug Interactions
8
E. Determining if the Investigational Drug is an Inducer of a Transporter
Certain transporters such as P-gp are induced through mechanisms similar to
those for CYP enzymes (e.g., by activation of specific nuclear receptors).
Because of these similarities, information from CYP3A induction studies can
inform P-gp induction studies. However, in vitro methods to evaluate the
induction of P-gp and other transporters are not well established at this time.
F. Evaluation Of The Drug-Drug Interaction (DDI) Potential of
Metabolites
The investigator should evaluate the DDI potential of an investigational drug’s
metabolites for their impact on the drug’s safety and efficacy using a risk-
based assessment that considers safety margins, likely concomitant
medications, and therapeutic indications. A metabolite with significant plasma
exposure or pharmacological activities may need to be evaluated for its DDI
potential as a substrate or as an inhibitor of metabolizing enzymes. In vitro
studies normally use a synthesized or purified metabolite standard or radio
labeled drug. Published data have shown that some Phase II metabolites can be
better substrates (more polar than the parent) or inhibitors of various
transporters leading to a higher chance of DDIs than the parent drug.
Therefore, the DDI potential of a metabolite as a substrate or a perpetrator of
major drug transporters should be assessed on a case-by-case basis. The same
principles and strategies mentioned above for parent drug should be applied
where applicable.
a. Metabolite as an Inhibitor
If in vitro assessments suggest that the parent drug inhibits major CYP
enzymes and transporters and in vivo DDI studies are warranted, in
vitro assessments of metabolites as enzyme or transporter inhibitors
may not be needed because the in vivo inhibition potential of
metabolites would be evaluated in vivo along with the parent drug,
unless clinically relevant exposures of the metabolite cannot be
adequately represented in the in vivo DDI study. However, if in vitro
Membrane Transporter Mediated Drug Interactions
9
assessments suggest that the parent drug alone will not inhibit major
CYP enzymes or transporters, in vivo DDIs caused by metabolites may
still be possible. In this situation, the investigator should evaluate the in
vitro inhibition potential of a metabolite on CYP enzymes taking into
account the following factors:
i. the systemic exposure of the metabolite relative to the parent
drug;
ii. any structural alerts, such as Quantitative Structure-Activity
Relationship
The sponsor should conduct an in vitro inhibition study of the metabolite if a
metabolite is less polar than the parent drug and the AUC of metabolite ≥ 25%
× the AUC parent (i.e.,AUC metabolite ≥ 0.25 × AUC parent).One should
conduct an in vitro inhibition study of the metabolite if a metabolite is more
polar than the parent drug, and the AUC of metabolite ≥ 100% × AUC parent
(i.e., AUC metabolite ≥ AUC parent).
The investigator should conduct an in vitro inhibition study of the metabolite
on CYP enzymes if a metabolite with a structural alert for TDI has an AUC
metabolite ≥ 25% × the AUC parent and an AUC metabolite ≥ 10% × the
AUC of the total drugs.
Evaluating Transporter-Mediated Drug Interactions In Vitro
In vitro transporter assays can determine whether an investigational drug is a
substrate or inhibitor of a particular transporter. Coupled with appropriate in
vitro-to-in vivo extrapolation methods, these assays can determine if the
sponsor should conduct an in vivo drug interaction study. The investigator
should choose an in vitro test system that is suitable for a specific transporter,
such as a membrane vesicle system, a polarized cell-based bidirectional assay
for efflux transporters, or a cell-based assay for uptake transporters. Table
below summarizes examples of in vitro systems to investigate potential
transporter-mediated drug interactions with an investigational drug as either a
Membrane Transporter Mediated Drug Interactions
10
substrate or an inhibitor of a specific transporter.
Examples of In Vitro Systems to Investigate Transporter-Mediated Drug
Interactions
Transporter In Vitro Systems
ABC Transporters
Caco-2 cells, commercial or in-house
membrane vesicles, knock-out/down
BCRP, P-gp
cells, transfected cells (MDCK, LLC-
PK1, etc.)
Solute Carrier (SLC) Transporters
Hepatocytes, transfected cells (CHO,
OATPs
HEK293, MDCK, etc.)
Transfected cells (CHO, HEK293,
OATs, OCTs
MDCK, etc.)
Commercial or in-house membrane
MATEs* vesicles, transfected cells (CHO,
HEK293, MDCK)
CHO: Chinese hamster ovary cell; HEK293: human embryonic kidney 293 cell;
LLC-PK1: Lewis-lung cancer porcine kidney 1 cell; MDCK: Madin-Darby canine
kidney cell.
Author Editor
Dr. K.S. Rao, M.V.Sc., Ph.D., DABT Alex Thomas, M. Pharm.
Mobile: +91-733-783-0074 Mobile: +91-974-545-0045
Email toxrao@gmail.com Email: alexthomas.a@gmail.com
Membrane Transporter Mediated Drug Interactions
S-ar putea să vă placă și
- A Dictionary of Terms Used in Drug MetabolismDocument7 paginiA Dictionary of Terms Used in Drug MetabolismOksana KamenetskaÎncă nu există evaluări
- Comparative Pharmacology of The H AntihistaminesDocument10 paginiComparative Pharmacology of The H Antihistaminesostosjesus4824Încă nu există evaluări
- Factors Affecting Drug Abosrtion and DistributionDocument5 paginiFactors Affecting Drug Abosrtion and DistributionBruno Adriel ZamoraÎncă nu există evaluări
- Drug Absorption MechanismDocument20 paginiDrug Absorption MechanismhabibieÎncă nu există evaluări
- PHARMACODYNAMICSDocument19 paginiPHARMACODYNAMICSshifa100% (1)
- Assignment On Pharmacokinetic Drug Interaction: Teerthanker Mahaveer UniversityDocument8 paginiAssignment On Pharmacokinetic Drug Interaction: Teerthanker Mahaveer Universityt24008882Încă nu există evaluări
- Chapter 5Document22 paginiChapter 5diah apriliaÎncă nu există evaluări
- WHO definition of health, drugs, pharmacology basicsDocument13 paginiWHO definition of health, drugs, pharmacology basics54momoÎncă nu există evaluări
- The Role of Transporters On Drug Therapy: NgatidjanDocument8 paginiThe Role of Transporters On Drug Therapy: NgatidjanMuhIrsalJumadilÎncă nu există evaluări
- Factors Contributing To Variability in Drug Pharmacokinetics. 11. Drug DistributionDocument9 paginiFactors Contributing To Variability in Drug Pharmacokinetics. 11. Drug DistributionStella WatkinsÎncă nu există evaluări
- Factors Contributing To Variability in Drug Pharmacokinetics. 11. Drug DistributionDocument9 paginiFactors Contributing To Variability in Drug Pharmacokinetics. 11. Drug DistributionStella WatkinsÎncă nu există evaluări
- Sheet PDFDocument316 paginiSheet PDFMarina WorldÎncă nu există evaluări
- General PharmacologyDocument149 paginiGeneral PharmacologyAbebe TilahunÎncă nu există evaluări
- The Journal of Clinical Pharma - 2016 - Patel - Importance of Hepatic Transporters in Clinical Disposition of Drugs andDocument17 paginiThe Journal of Clinical Pharma - 2016 - Patel - Importance of Hepatic Transporters in Clinical Disposition of Drugs andgabriel.nathan.kaufmanÎncă nu există evaluări
- 1 IntroductionDocument68 pagini1 Introductiondona donneÎncă nu există evaluări
- Basic pharmacology concepts and principlesDocument59 paginiBasic pharmacology concepts and principlesYoueel IbrahemÎncă nu există evaluări
- Drug Interaction Linked To Drug TransporterDocument25 paginiDrug Interaction Linked To Drug TransporterPrarthna Yadav100% (1)
- Mechanism of Protein Binding of Drug To ReceptorsDocument7 paginiMechanism of Protein Binding of Drug To ReceptorsZubiya SiddiquiÎncă nu există evaluări
- General 2012 Final PDFDocument25 paginiGeneral 2012 Final PDFMohd Haizaq FarhanÎncă nu există evaluări
- المعلومات بالداخل موثوق بها لنها مراجعه و معتمده من Certified from Pharmacists_coffee magazineDocument20 paginiالمعلومات بالداخل موثوق بها لنها مراجعه و معتمده من Certified from Pharmacists_coffee magazineMedhat EyadaÎncă nu există evaluări
- Biopharmaceutics &pharmakinetics: Subject Code-604t Unit - 1Document27 paginiBiopharmaceutics &pharmakinetics: Subject Code-604t Unit - 1Babbu Singh GurjarÎncă nu există evaluări
- Biopharmaceutics and Clinical PharmacokineticsDocument302 paginiBiopharmaceutics and Clinical PharmacokineticsBalisa MosisaÎncă nu există evaluări
- BiopharmaceuticsDocument52 paginiBiopharmaceuticsDharma ShantiniÎncă nu există evaluări
- Drug Distribution Factors and ModelingDocument27 paginiDrug Distribution Factors and ModelingLailaturrahmi LailaturrahmiÎncă nu există evaluări
- General Pharmacology) 343 (Document28 paginiGeneral Pharmacology) 343 (ALNAKI100% (1)
- Grup 4 Passage of Drugs Across Biology MembraneDocument24 paginiGrup 4 Passage of Drugs Across Biology MembraneIndiy Heny SaLindriÎncă nu există evaluări
- General PharmacologyDocument76 paginiGeneral PharmacologyMiyuru HasarangaÎncă nu există evaluări
- Applying QSP and Multiscale Models to Improve Drug DevelopmentDocument20 paginiApplying QSP and Multiscale Models to Improve Drug Developmentmr samoÎncă nu există evaluări
- Makalah KBM Kel 3Document32 paginiMakalah KBM Kel 3Novia RozadiÎncă nu există evaluări
- DMD 106 010793 PDFDocument6 paginiDMD 106 010793 PDFTetteh JudeÎncă nu există evaluări
- PharmacokineticsDocument2 paginiPharmacokineticsMihaela Toma100% (1)
- 4 DerlemeDocument6 pagini4 DerlemeŞahin ŞahinÎncă nu există evaluări
- Pharmaco KineticsDocument14 paginiPharmaco KineticsMariusNeicuÎncă nu există evaluări
- 5 Evaluation of PermeabilityDocument38 pagini5 Evaluation of PermeabilityEduardMartinezÎncă nu există evaluări
- Drug AbsorptionDocument30 paginiDrug AbsorptionShiva KantÎncă nu există evaluări
- Pharmaco DynamicsDocument7 paginiPharmaco DynamicsDavid NicholasÎncă nu există evaluări
- Chapter 5 DDS Clarion LCDocument15 paginiChapter 5 DDS Clarion LCclyde clarionÎncă nu există evaluări
- Modul: Pharmacodynamics I. DescriptionDocument9 paginiModul: Pharmacodynamics I. DescriptionEli Ezer SimangunsongÎncă nu există evaluări
- Pharmacokinetics PDFDocument14 paginiPharmacokinetics PDFLea PesiganÎncă nu există evaluări
- What The Body Does To A Drug: PharmacokineticsDocument14 paginiWhat The Body Does To A Drug: PharmacokineticsSabrina JonesÎncă nu există evaluări
- 01 Basic Principles in PharmacologyDocument51 pagini01 Basic Principles in PharmacologyMicah Monte0% (1)
- Neusci 404 Notes Exam 1Document19 paginiNeusci 404 Notes Exam 1api-545982271Încă nu există evaluări
- Clinical Pharmacokinetics in Liver DiseaseDocument25 paginiClinical Pharmacokinetics in Liver Diseasedarlington D. y ayimÎncă nu există evaluări
- Pengantar Farmakologi Untuk Mahasiswa FarmasiDocument74 paginiPengantar Farmakologi Untuk Mahasiswa FarmasiHanifÎncă nu există evaluări
- J Natl Cancer Inst Monogr 2001 Lee 41 4Document4 paginiJ Natl Cancer Inst Monogr 2001 Lee 41 4Ashish SarafÎncă nu există evaluări
- Clinical PharmacologDocument81 paginiClinical PharmacologSHILOTAÎncă nu există evaluări
- Pharmacokinetics: Pharmacokinetics (In Greek: "Pharmacon" Meaning Drug and "Kinetikos" MeaningDocument5 paginiPharmacokinetics: Pharmacokinetics (In Greek: "Pharmacon" Meaning Drug and "Kinetikos" Meaning0921pyÎncă nu există evaluări
- Pharmacology Is A Biomedical Discipline That Studies The Effects of Drugs in A Human Body, From The WholeDocument18 paginiPharmacology Is A Biomedical Discipline That Studies The Effects of Drugs in A Human Body, From The WholeNudžejma KadrićÎncă nu există evaluări
- Materi 3 - Sifat FisikokimiaDocument61 paginiMateri 3 - Sifat Fisikokimiaashley vechtersbaasÎncă nu există evaluări
- Biopharmaceutics Absorption FactorsDocument130 paginiBiopharmaceutics Absorption FactorsMinal NadeemÎncă nu există evaluări
- Principles of Pharmacology - Chapter 3Document5 paginiPrinciples of Pharmacology - Chapter 3lalee704Încă nu există evaluări
- Factors Affecting Drug Absorption and DistributionDocument3 paginiFactors Affecting Drug Absorption and DistributionEster VillacampaÎncă nu există evaluări
- Ceutics CAT 2Document9 paginiCeutics CAT 2Ria KitlerÎncă nu există evaluări
- Principles of Pharmacokinetics (PKDocument25 paginiPrinciples of Pharmacokinetics (PKSimonÎncă nu există evaluări
- I IntroductionDocument31 paginiI IntroductionOsama adel Mohamed SmadiÎncă nu există evaluări
- Drug Receptor TheoryDocument9 paginiDrug Receptor TheoryFish YanÎncă nu există evaluări
- Pharmaco KineticsDocument427 paginiPharmaco KineticsMehrdad AvestaÎncă nu există evaluări
- Drug Metabolism in DiseasesDe la EverandDrug Metabolism in DiseasesWen XieÎncă nu există evaluări
- Pharmacology in Drug Discovery: Understanding Drug ResponseDe la EverandPharmacology in Drug Discovery: Understanding Drug ResponseÎncă nu există evaluări
- Pharmacology- The Molecular Dance: Understanding Drug Interactions: Harmony and Chaos: The Symphony of Drug InteractionsDe la EverandPharmacology- The Molecular Dance: Understanding Drug Interactions: Harmony and Chaos: The Symphony of Drug InteractionsÎncă nu există evaluări
- Peri Implant Health: Mauricio G. Araujo - Jan LindheDocument7 paginiPeri Implant Health: Mauricio G. Araujo - Jan LindheCristian CulcitchiÎncă nu există evaluări
- Defense Mechanisms of the GingivaDocument249 paginiDefense Mechanisms of the GingivaAssssssÎncă nu există evaluări
- Nursing Care Plan AmoebiasisDocument2 paginiNursing Care Plan Amoebiasisderic97% (35)
- Chapter 1 The Foundations of BiochemistryDocument5 paginiChapter 1 The Foundations of BiochemistryghurapÎncă nu există evaluări
- Teachers' Health Examination Card (CS Form 86)Document4 paginiTeachers' Health Examination Card (CS Form 86)Maria Angellie S. Bellido - EramisÎncă nu există evaluări
- Endocrine Physiology Lecture 2Document9 paginiEndocrine Physiology Lecture 2Tofunmi Kunle-KunbiÎncă nu există evaluări
- IndianJOralSci5278-1137123 030931Document5 paginiIndianJOralSci5278-1137123 030931Maqbul AlamÎncă nu există evaluări
- Cell Biology Test - 70 Possible Points: Prokaryotic and Eukaryotic Cells (2 Points Per Question)Document3 paginiCell Biology Test - 70 Possible Points: Prokaryotic and Eukaryotic Cells (2 Points Per Question)Vienne MonroidÎncă nu există evaluări
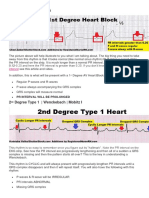
- Understanding 1st, 2nd and 3rd Degree Heart BlocksDocument3 paginiUnderstanding 1st, 2nd and 3rd Degree Heart BlockslhenÎncă nu există evaluări
- Nursing DictionaryDocument353 paginiNursing DictionaryEmmanuel BoadÎncă nu există evaluări
- NCP-Case Presentation (CHF)Document4 paginiNCP-Case Presentation (CHF)Jessamine EnriquezÎncă nu există evaluări
- Ebook PDF Developmental Biology 12th Edition PDFDocument41 paginiEbook PDF Developmental Biology 12th Edition PDFjanet.dicks248100% (36)
- Burn Patient Management - Clinical Practice GuidelinesDocument47 paginiBurn Patient Management - Clinical Practice GuidelinesAna PÎncă nu există evaluări
- Language and BrainDocument23 paginiLanguage and Brainalbino100% (1)
- Pathology of Neurodegenerative DiseasesDocument22 paginiPathology of Neurodegenerative DiseasesKarel GuevaraÎncă nu există evaluări
- The TongueDocument21 paginiThe Tonguemanojchouhan2014Încă nu există evaluări
- Physiology Objectives DetailedDocument35 paginiPhysiology Objectives DetailedSOOOS94Încă nu există evaluări
- BTL Ultrasound 5000 - User ManualDocument16 paginiBTL Ultrasound 5000 - User ManualAlexaÎncă nu există evaluări
- 12 White Blood Cell Counting Techniques in BirdsDocument5 pagini12 White Blood Cell Counting Techniques in BirdsPablo LópezÎncă nu există evaluări
- 11.transportation in Plants & AnimalsDocument51 pagini11.transportation in Plants & AnimalsReshma ModhiaÎncă nu există evaluări
- Week 006 Animal-Immune-SystemDocument13 paginiWeek 006 Animal-Immune-SystemMark Lorens StaanaÎncă nu există evaluări
- 3B Arm Model - M11Document28 pagini3B Arm Model - M11rswongym449Încă nu există evaluări
- Neurology Crossword Puzzle Answer KeyDocument1 paginăNeurology Crossword Puzzle Answer KeyRavinaAhujaÎncă nu există evaluări
- PTC MCQDocument7 paginiPTC MCQYevan HarryBrata0% (1)
- Skeletal System of FishesDocument18 paginiSkeletal System of FishesYousaf AnwarÎncă nu există evaluări
- Autopsy Report: DECEDENT: John AndersonDocument5 paginiAutopsy Report: DECEDENT: John AndersonjilliankadÎncă nu există evaluări
- Brain Herniation SyndromeDocument28 paginiBrain Herniation SyndromeSarahScandy100% (4)
- Assessment of HearingDocument51 paginiAssessment of HearingSwetha PasupuletiÎncă nu există evaluări
- Haemodialysis CatheterDocument10 paginiHaemodialysis CatheterRizqi AhmadÎncă nu există evaluări
- Acute and Chronic PyelonephritisDocument7 paginiAcute and Chronic PyelonephritisMatthew Ryan100% (1)