Documente Academic
Documente Profesional
Documente Cultură
Am J Crit Care 2010 Jacobowski 421 30
Încărcat de
Beny HermawanDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Am J Crit Care 2010 Jacobowski 421 30
Încărcat de
Beny HermawanDrepturi de autor:
Formate disponibile
Families in Critical Care
C OMMUNICATION IN
CRITICAL CARE: FAMILY
ROUNDS IN THE INTENSIVE
CARE UNIT
By Natalie L. Jacobowski, BA, Timothy D. Girard, MD, MSCI, John A. Mulder,
MD, and E. Wesley Ely, MD, MPH
Background Communication with family members of
patients in intensive care units is challenging and fraught
with dissatisfaction.
Objectives We hypothesized that family attendance at struc-
tured interdisciplinary family rounds would enhance commu-
nication and facilitate end-of-life planning (when appropriate).
Methods The study was conducted in the 26-bed medical
intensive care unit of a tertiary care, academic medical center
from April through October 2006. Starting in July 2006, families
were invited to attend daily interdisciplinary rounds where
the medical team discussed the plan for care. Family members
were surveyed at least 1 month after the patient’s stay in the
unit, completing the validated “Family Satisfaction in the
ICU” tool before and after implementation of family rounds.
Results Of 227 patients enrolled, 187 patients survived and 40
died. Among families of survivors, participation in family rounds
was associated with higher family satisfaction regarding fre-
quency of communication with physicians (P = .004) and sup-
port during decision making (P = .005). Participation decreased
satisfaction regarding time for decision making (P = .02).
Overall satisfaction scores did not differ between families who
attended rounds and families who did not. For families of
patients who died, participation in family rounds did not sig-
nificantly change satisfaction.
Conclusions In the context of this pilot study of family rounds,
certain elements of satisfaction were improved, but not over-
all satisfaction. The findings indicate that structured interdisci-
plinary family rounds can improve some families’ satisfaction,
whereas some families feel rushed to make decisions. More
work is needed to optimize communication between staff in
the intensive care unit and patients’ families, families’ compre-
hension, and the effects on staff workload. (American Journal
©2010 American Association of Critical-Care Nurses of Critical Care. 2010;19:421-430)
doi: 10.4037/ajcc2010656
www.ajcconline.org AJCC AMERICAN JOURNAL OF CRITICAL CARE, September 2010, Volume 19, No. 5 421
Downloaded from http://ajcc.aacnjournals.org/ by AACN on January 5, 2018
C
omprehensive state-of-the-art care of patients in intensive care units (ICUs)
involves not only excellent medical treatment but also optimal communication
and interaction with the health care team. Family members, who frequently
must act as the surrogates for ICU patients, experience marked distress in situa-
tions characterized by poor communication and interpersonal interactions.1-6
For many patients and their families, this need for communication and interaction becomes
especially important when the transition from anticipation of cure to the realization of non-
survivability must be negotiated in the ICU, making the ICU team responsible for providing
a quality end-of-life experience for the patient and the patient’s family members.7
Although much attention has been given to the often is lacking.3,20 Failure to comprehend a diagno-
family conference separate from rounds,5,8-11 commu- sis, prognosis, or treatment occurs in 35% to 50%
nication may also be enhanced through routine of family members.21,22 Improved comprehension is
incorporation of families into daily interdisciplinary thought to be a base from which overall satisfaction
ICU rounds. Studies in pediatric12-14 and trauma15,16 can arise,1 making this deficit in understanding a
patients have suggested a beneficial significant impediment to optimal care. Thus, a
effect of including patients’ families “family rounds” approach, with nurses inviting and
Studies have in interdisciplinary rounds, and bringing the family into daily rounds, might facili-
suggested a exploration of the related practice of tate the earliest possible and most regular form of
bedside rounds shows the practice communication for all patients, not just those for
beneficial effect to be positively received by patients whom problems arise, such as the need for end-of-
of including as well.17,18 Studies of families’ experi- life discussions. On the other hand, such an
ences with end-of-life care in the approach of hearing the actual medical discussions
patients’ families ICU indicate a need for better com- on rounds could increase family members’ fear,
in interdisciplinary munication, as communication
deficits may contribute to family
confusion, and doubts about care.
We conducted this pilot investigation to explore
rounds. anxiety and depression,1,3,5,6 increased the effect of consistent, early communication through
risk of contradictory information the addition of a family component to interdiscipli-
from multiple physicians,19 and potential family nary rounds in the medical ICU, a setting in which
mistrust of physicians.5 Families desire more fre- this type of communication intervention has rarely
quent communication with nurses and physicians,6 been reported. This intervention will be referred to
and access to and comprehension of information as “family rounds” to focus on this 1 aspect of inter-
disciplinary rounds. While constructing this study,
we noted the importance of including both families
About the Authors
Natalie L Jacobowski is a medical student at the Vander- of patients who survive their ICU stay and families
bilt University School of Medicine, Nashville, Tennessee. of patients who die during or shortly after an ICU
John A. Mulder is an assistant professor in the Department stay in the study. The needs of surviving patients
of Family Medicine at the Michigan State University
College of Human Medicine and the medical director and their families for communication can be neg-
for palliative care services for Spectrum Health in Grand lected because of the focus on communication in
Rapids, Michigan. Timothy D. Girard is an assistant pro- the end-of-life setting.23 We hypothesized that
fessor and E. Wesley Ely is a professor in the Division of
Allergy, Pulmonary, and Critical Care Medicine and the implementation of family rounds would enhance
Center for Health Services Research in the Department communication and facilitate end-of-life planning
of Medicine at Vanderbilt University School of Medicine. (when appropriate) between families and the med-
Dr Girard is also a staff physician and Dr Ely is the asso-
ciate director for research in the Geriatric Research, ical team, leading to improved family satisfaction,
Education, and Clinical Center at the Department of Vet- especially with aspects of communication.
erans Affairs Medical Center, Tennessee Valley Healthcare
System, in Nashville.
Materials and Methods
Corresponding author: Natalie L. Jacobowski, BA, Vander- Study Design
bilt School of Medicine, 6th floor Medical Center East #6109,
Vanderbilt University Medical Center, Nashville, TN We conducted a before-after study during which
37232-8300 (e-mail: natalie.jacobowski@vanderbilt.edu). family satisfaction in the ICU was assessed before and
422 AJCC AMERICAN JOURNAL OF CRITICAL CARE, September 2010, Volume 19, No. 5 www.ajcconline.org
Downloaded from http://ajcc.aacnjournals.org/ by AACN on January 5, 2018
after implementation of a family rounds component of 1 to 5, with higher values indicating increased
of interdisciplinary rounds. satisfaction. In keeping with prior studies, responses
were converted to a score of 0 to 100 per question.25
Population of Patients The mean score for the 13 questions and 10 ques-
Two study investigators (N.J., A.D.) conducted tions provided the total score for
phone interviews with family members designated as each subdomain. The mean of
primary contacts for all patients admitted for longer these 2 subscores provided the
As many as 50% of
than 24 hours to the Vanderbilt University Medical total score. family members do
Center medical ICU, a 26-bed unit, before and after
the implementation of family rounds on July 7, 2006. Family Rounds Process not understand a
The study period included April 24, 2006, through The structure of family rounds diagnosis, progno-
October 31, 2006. Patients without a primary con- as a family communication com-
tact or whose primary contact did not understand ponent of daily interdisciplinary sis, or a treatment.
English sufficiently to complete the survey were rounds was developed through
excluded. Family members of patients enrolled multiple discussions with the physicians and nurses
before implementation of family rounds comprised of the ICU, with the following format settled upon.
the baseline group. Family members who attended Family rounds were added to the existing structure
rounds after implementation of family rounds com- of interdisciplinary rounds in the medical ICU,
prised the family rounds group. Upon admission to which occurred before regular visiting hours and
the ICU, patients’ families received a letter describing consisted of (1) nurses’ presentation of vital signs
the study and the phone surveys. For patients dis- and relevant events from the previous 24 hours, (2)
charged from the unit, surveys were completed within interns’ presentation of 24-hour events, assessment,
1 month following discharge. For patients who died and plan, complementing information provided by
in the unit, surveys were completed between 3 and the nurse, (3) upper level residents’ and fellows’
5 months following the death, allowing for a griev- refinement of 24-hour goals and treatment plan,
ing period for the families. At the time of the phone and (4) teaching provided by the attending physi-
call, the purpose of the survey was described again, cian to the treatment team. Two additional steps,
families were informed that the survey was voluntary which we define as family rounds, were added: (5)
and anonymous, and verbal consent was obtained. the attending physician provided a summary for the
Only 1 respondent was interviewed per patient, and family using understandable, lay language and (6)
no patient included in the baseline group was read- the family was offered an opportunity to ask ques-
mitted during the family rounds period. This study tions of the team. To limit extension of the time of
was reviewed by the institutional review board at rounds, each patient was allowed up to 2 family
Vanderbilt University and granted expedited review members at the bedside and if questions exceeded a
and approval with verbal consent obtained at the few minutes, the team invited the family to meet
time of interview. with them again after rounds for further discussion.
More extended family conferences
Survey Development and Administration did not occur for every patient,
The previously refined and validated Family but the standard medical ICU
The physician pro-
Satisfaction in the ICU (FS-ICU) survey24 was used procedure was to arrange such vided a summary for
in this study. The survey consisted of 2 subdo- conferences as needed because of
mains: care and decision making, which consisted complexity of illness or to facilitate
the family that used
of 13 and 10 questions, respectively. The Cronbach decision making. lay language, and
α coefficients for the 2 subscales were 0.92 and Families received an explana-
0.88, respectively, and the 2 subscales showed good tory letter and verbal explanation families were able
correlation with each other (Spearman ρ = 0.73, P < from the nurse upon admission, to ask questions.
.001), supporting their combination into a single orienting them to these procedures
scale with a Cronbach α coefficient of 0.94. The as well. It was essential that the nurses embraced
survey’s validity was demonstrated by a significant the concept of family rounds, as they would be the
correlation with results of the previously estab- ones helping bring families in and out of the ICU
lished Family-Quality of Death and Dying survey. in the morning and also would have the most fre-
Respondents rated their satisfaction with multiple quent interactions with families, which meant that
aspects of the patient’s care in the ICU and the the nurses were a primary influence to encourage
respondent’s experience during that time on a scale their patients’ families to attend family rounds.
www.ajcconline.org AJCC AMERICAN JOURNAL OF CRITICAL CARE, September 2010, Volume 19, No. 5 423
Downloaded from http://ajcc.aacnjournals.org/ by AACN on January 5, 2018
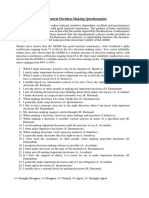
Table 1
Items related to communication on the Family
Satisfaction in the Intensive Care Unit (ICU) survey
summary scores. Because responses on individual
How often nurses communicated to you about your family member’s survey items were strongly skewed (ie, most respon-
condition. dents rated their experiences “good” or “excellent”),
How often doctors communicated to you about your family member’s we also reduced each item to a dichotomous vari-
condition. able representing the highest level of satisfaction
(eg, “excellent” or “very supported”) versus less than
Willingness of ICU staff to answer your questions.
the highest level of satisfaction and compared these
How well ICU staff provided you with explanations that you understood.
variables using the χ2 test.
The honesty of information provided to you about your family member’s To explore potential interactions between the
condition. effect of family rounds and patients’ survival in the
How well ICU staff informed you what was happening to your family ICU, we included interaction terms in proportional
member and why things were being done. odds logistic regression models with individual FS-
The consistency of information provided to you about your family mem- ICU items as the dependent variables. In keeping
ber’s condition. with authoritative recommendations on the topic,26,27
Did you feel included in the decision-making process? no adjustments were made to our results to account
for multiple comparisons. Although this lack of
Did you feel supported during the decision-making process?
adjustment may increase the likelihood of a type I
When making decisions, did you have adequate time to have your con-
error, our approach of not making such adjustments
cerns addressed and questions answered?
avoids an unnecessary inflation of type II errors.
STATA version 10.0 (StataCorp, College Station, Texas),
Data Entry and Statistical Analysis and SPSS version 15 (SPSS Inc, Chicago, Illinois)
For this pilot study, sample size was determined were used for data analysis, and a 2-sided 5% sig-
by available resources. Thus, we sought to enroll all nificance level was used for all statistical inferences.
eligible patients during the specified period of study.
Because our goal for this study was to assess the Results
efficacy of family rounds as a source of improved Demographics and Clinical Characteristics
satisfaction via better communication, we focused Among 402 families of survivors for whom
our analysis on specific items in the FS-ICU that we contact information was available, 234 respondents
deemed most relevant (Table 1). These questions (58%) completed the survey; among 67 families of
had a primary focus on communication with mem- deceased patients for whom contact information
bers of the ICU team, understanding and decision was available, 44 respondents (66%) completed the
making by family members, and frequency of con- survey. After we eliminated those who did not attend
tact with the ICU team. Although any family rounds despite this intervention’s avail-
The number of less specific to this study, the sum-
mative scores for decision making
ability at the time of their family member’s ICU
admission, 227 survey interviews of family members
families feeling and overall satisfaction were evalu- remained to be analyzed. Of these families, 187
ated as well, in keeping with prior were of patients discharged from the ICU and 40
“very supported” research.25 We also stratified all were of patients who died in the ICU. The break-
improved after analyses according to whether the down of those interviews is shown in Figures 1 and
patient survived to ICU discharge or 2. For patients who survived and those who died in
attending family died in the ICU, because we hypoth- the ICU, survey respondents during the baseline
rounds. esized that family members of phase were similar to respondents who attended
patients who died would have differ- family rounds, without significant differences in age,
ent interactions with ICU staff than would families race, or relationship to the patient (Table 2). Patients
of patients who survived, and therefore the effect of enrolled during the 2 study periods were similar
family rounds on satisfaction may differ according except that patients who survived during the family
to survival status of the patient. rounds phase had longer stays in the ICU than did
Baseline characteristics are presented by using patients who survived before implementation of
median and interquartile range for continuous vari- family rounds.
ables and proportions for categorical variables. We
used χ2 tests to compare categorical variables between Follow-Up Family Evaluations: Surviving Patients’
the study groups, and the Wilcoxon-Mann-Whitney Families
2-sample rank-sum test to compare continuous vari- When families of surviving patients were asked
ables, including individual items on the FS-ICU and to rate “How often doctors communicated to you
424 AJCC AMERICAN JOURNAL OF CRITICAL CARE, September 2010, Volume 19, No. 5 www.ajcconline.org
Downloaded from http://ajcc.aacnjournals.org/ by AACN on January 5, 2018
223 patients
about your family member’s condition,” the number admitted >24 hours
of families who rated this central aspect of communi-
cation as “excellent” improved significantly (P = .004)
after the implementation of family rounds (Table 3).
Families also were asked about the support they 191 patients 32 patients died in the
received via the question: “Did you feel supported discharged intensive care unit
during the decision-making process?” The number
of families who reported feeling “very supported,”
the top value on the Likert scale, improved signifi-
cantly (P = .005) after families had the opportunity 52 without contact 5 without contact
information information
to attend family rounds. In contrast, the percentage
41 refused 9 refused
of family members who responded that they had
“more than enough time to have concerns addressed
and questions answered” during decision making
declined after implementation of family rounds 98 families surveyed 18 families surveyed
(P = .02). When all potential responses to this item
were compared before and after family rounds, results Figure 1 Flowchart shows the numbers of surveys conducted dur-
of the Wilcoxon rank-sum test indicated no signifi- ing the baseline phase, with detailed listing of whether the family
cant difference between groups (P = .19). All other was associated with a patient who had been discharged alive
items were rated similarly before and after implemen- from the intensive care unit or was associated with a patient who
died in the unit (designated as end-of-life).
tation of family rounds.
Follow-Up Family Evaluations: Deceased Patients’
Families
Among families of patients who died in the ICU, 403 patients
none of the FS-ICU items pertaining to communica- admitted >24 hours
tion were rated significantly better by respondents
who participated in family rounds than by families
who did not (Table 3). Families of deceased patients
who were in the family rounds group tended to report 344 patients 59 patients died in the
the highest level of satisfaction regarding “How discharged intensive care unit
often nurses communicated to you about your fam-
ily member’s condition” more often than did fami-
lies of deceased patients who did not participate in
81 without contact 19 without contact
family rounds (P = .11). Similarly, the number of
information information
family members of deceased patients who reported 127 refused 14 refused
the highest level of satisfaction regarding “willingness
of ICU staff to answer your questions” increased
after implementation of family rounds (P = .18).
136 families surveyed 26 families surveyed
89 at family rounds 22 at family rounds
Overall Measures of Satisfaction and Interactions 47 did not attend* 4 did not attend*
Neither the decision-making subscore nor the
total FS-ICU score differed significantly between
respondents who attended family rounds and Figure 2 Flowchart shows the numbers of surveys conducted after
implementation of family rounds, during the intervention phase,
respondents from before implementation of family with detailed listing of whether the family was associated with a
rounds (Table 3). Additionally, no significant inter- patient who had been discharged alive from the intensive care unit
actions were noted between the effect of family or was associated with a patient who died in the unit (designated as
rounds on family satisfaction and patients’ survival end-of-life) and whether the family attended family rounds.
in the ICU. *Families who did not attend family rounds despite the opportunity to do so were
excluded from all analyses.
Discussion
In this pilot before-after study, a family rounds family satisfaction but did result in significant
component during interdisciplinary rounds in the improvements in some aspects of family satisfaction
medical ICU did not affect the global measure of related to communication. Specifically, families of
www.ajcconline.org AJCC AMERICAN JOURNAL OF CRITICAL CARE, September 2010, Volume 19, No. 5 425
Downloaded from http://ajcc.aacnjournals.org/ by AACN on January 5, 2018
Table 2
Demographics and clinical characteristics
Patient survived Patient died
Baseline Family rounds Baseline Family rounds
Characteristics (n = 98) (n = 89) P value (n = 18) (n = 22) P value
Patient
Age, median [interquartile range], y 57 [46-66] 55 [37-66] .45 62 [51-68] 56 [49-71] .94
Female, % 49 42 .31 56 50 .73
Race, % .61 .97
White 79 85 82 82
Black 12 10 18 18
Other 9 5 0 0
Admission diagnosis, % .11 .36
Cardiovascular 11 8 17 9
Respiratory 21 33 50 27
Neurological 11 16 6 9
Sepsis 14 10 0 18
Gastroenterological 12 18 6 9
Other 31 15 21 28
Days in intensive care unit, median 3 [2-5] 4 [3-8] .001 4 [2-6] 4 [3-9] .46
[interquartile range]
Full code status, % 97 93 .33 65 76 .23
Respondent
Age, y, % .41 .23
≥80 0 1 0 4
60-79 30 21 47 18
40-59 53 57 35 55
20-39 16 20 18 23
<20 1 1
Female, % 69 80 .10 61 77 .27
Race, % .56 .97
White 79 87 82 82
Black 13 10 18 18
Other 8 3
Relationship to patient, % .66 .33
Spouse/partner 49 49 72 50
Child 28 23 11 36
Parent 11 17 6 5
Other 12 11 11 9
discharged patients reported an increased frequency the scheduled opportunity to receive information
of communication. Additionally, although family and answers to questions. Past studies also have
rounds had been conceived as an efficient use of revealed a link between family satisfaction and psy-
time for both families and the medical team, the chological health.1,3,5,6 Hospitalization of a loved one
results indicated that more families perceived the in the ICU is a very stressful event for family mem-
time for decision making as inadequate after imple- bers, with nearly 3 out of every 4 family members
mentation of family rounds. struggling with anxiety and 1 in 3 showing signs of
Other researchers have evaluated patients’ per- depression.6,28 A proactive approach to bereavement
spectives of similar interventions such as bedside and implementation of a proactive communication
case presentations that brought the patient and fam- strategy leads to decreases in the frequency of post-
ily into the midst of rounds. Most patients preferred traumatic stress disorder, anxiety, and depressive
such bedside presentations.17,18 Studies of family symptoms.5 In our family rounds pilot study, this com-
inclusion in ICU rounds are limited,15,16 but the results munication began at admission, congruent with the
available indicate that patients’ families appreciated reported increased satisfaction with communication
426 AJCC AMERICAN JOURNAL OF CRITICAL CARE, September 2010, Volume 19, No. 5 www.ajcconline.org
Downloaded from http://ajcc.aacnjournals.org/ by AACN on January 5, 2018
Table 3
Effect of family rounds on family satisfaction
Patient survived Patient died
Historical Family rounds Historical Family rounds
Outcome (n = 98) (n = 89) P value (n = 18) (n = 22) P value
Individual items, % excellenta
Frequency of nurse communication 64 57 .30 33 59 .11
Frequency of physician communication 38 60 .004 50 43 .66
Willingness to answer questions 55 59 .58 33 55 .18
Understandable explanations 54 54 .98 39 41 .90
Honesty of information 61 58 .74 53 48 .74
Informative regarding treatment 56 56 .95 39 52 .40
Consistency of information 51 53 .81 33 55 .18
Included in decision making 66 76 .12 77 82 .71
Supported in decision making 49 69 .005 61 73 .44
Adequate time for questions 40 23 .02 39 41 .90
Summary scores, median
[interquartile range]
Decision-making subscore 83 [65-93] 85 [74-93] .67 75 [63-88] 78 [73-90] .18
Total survey score 85 [70-95] 88 [75-95] .65 74 [62-92] 82 [72-94] .26
a “% excellent” indicates the proportion of respondents who gave the survey item the highest rating, that is, expressed the highest level of satisfaction.
when prognostic information is provided within a format and a frequently updated picture of their
shorter time interval.29 By addressing some of these loved one’s condition.13,15 These rounds also helped
key components of family satisfaction, family rounds prepare families for more in-depth discussions that
could minimize psychological distress in the stress- were sometimes necessary later in the day to meet
ful ICU environment (especially if family members their reported need for more time in decision mak-
who feel rushed by such an approach are encour- ing than might be possible during rounds. However,
aged to have family conferences later in the day to the effect of family rounds on knowledge and com-
allow more time for decision making). Simultane- prehension was not studied in this investigation
ously, subsequent studies of family inclusion should beyond families’ summary statements about access
consider the potential for families to feel intimidated to and satisfaction with information. As comprehen-
or overwhelmed in the setting of daily rounds and sion is a central aspect of good communication, it
should explore family comfort in that setting and warrants more extensive attention in future studies.
any potential effects on families’ levels of stress and Studies of families of patients with end-of-life
anxiety. This important balance must be explored experiences have documented a need for informa-
in future research. tion early and often,7,22 and inadequacies of infor-
This pilot study highlights that family satisfac- mation and communication may impede removal
tion with communication may hinge on receipt of of life support, leading to a prolonged dying process
adequate knowledge to improve family members’ and longer stays for patients.32 Interdisciplinary inclu-
comprehension and aid in surrogate decision mak- sion of the ICU medical care team during family
ing.1,5,20,21,25,28,30,31 Inadequate comprehension is reported rounds may reduce communication obstacles by
in 30% to 50% of patients’ families,21,22,28 a statistic fostering more cohesive care with better integration
that we felt necessitated that the structure of family of palliative care,33 yet the pace of these rounds and
rounds include having the physician provide the the inclusion of medical terminology amid the dis-
families with a 1- or 2-minute summary in lay lan- cussions between doctors and nurses could also
guage. Family rounds initiated brief, structured, and increase communication problems.
consistent communication within the first 24 hours Our study included only English-speaking
of admission, providing families a realistic, real-time patients. This necessitates further study of the
www.ajcconline.org AJCC AMERICAN JOURNAL OF CRITICAL CARE, September 2010, Volume 19, No. 5 427
Downloaded from http://ajcc.aacnjournals.org/ by AACN on January 5, 2018
application of family rounds with non–English- limited sensitivity to detect a difference from before
speaking families as alterations in translation during to after implementation of family rounds. Addition-
interpreted interactions can adversely affect commu- ally, the study size—determined by restricted
nication, complicating both the transmission of resources and time available to conduct this pilot
knowledge and emotional support.34 study—was small, especially regarding patients with
In addition to examining the success end-of-life experiences, and the small number of
Families of dis- of content transmission in these participants may have impaired our ability to observe
charged patients conversations, studies of patient- overall changes in satisfaction. The study did not
physician relationships have shown have enough power to assess for differences between
reported an that styles of interpersonal commu- family members of living versus deceased patients.
increased frequency nication influence satisfaction.35,36 The refusal rate of families in study participa-
Studies in the ICU also have made tion warrants exploration. High baseline levels of
of communication. apparent a need to improve the satisfaction may point to a selection bias because
quality of communication.9,10 Future family members without contact information or
research also should evaluate the influence of the who refused to participate most likely are different
style and nature of the communication itself on sat- from families who responded to the survey, and the
isfaction of patients’ families. families who responded may represent a population
From the perspective of the ICU nurses, 2 of the most likely to attend and benefit from family
most significant obstacles to providing end-of-life rounds, even though demographically attendees
care are multiple physicians with discordant opin- and nonattendees were not significantly different.
ions about the plan of care and multiple family Because Vanderbilt University Medical Center serves
members contacting the staff instead of communi- a diverse population, other factors probably influ-
cating with 1 designated team member.19 From the enced family members’ ability and willingness to
perspective of the ICU care team, attention to com- attend family rounds, such as socioeconomic status,
munication and palliative care can lead to improved availability to be at the hospital at the time of rounds,
nurse-assessed quality of death in the ICU.37 In the geographic factors (many patients and their families
case of end-of-life care, nurses experienced distress live hours away from the hospital), and comfort
and decreased satisfaction with quality of care when and experience with the medical system. The rate of
they perceived care to be overly aggressive given the nonattendance is a limitation of this study, so these
patient’s expected prognosis,38,39 and the Critical Care factors should be explored.
Medicine Task Force 2004-2005 identified poor Attention also should be given to the level of
communication as a major source of stress for staff.40 nurse engagement in family rounds and nurse-
Although those issues were not explored formally in perceived barriers to successful family rounds, because
our study, family rounds may be a forum to address the level of family participation may depend on
these issues, providing components of suggested how well families are informed about and encour-
interventions,41 including a systemic framework to aged to attend family rounds by the bedside nurse
support integration of palliative care and attitudinal with whom they interact during the day.
change regarding communication Other limitations of this study should be dis-
Family rounds given the increased, regular interac- cussed. This was a single-center study, so future
tion with patients’ families. multicenter work is needed to assess the effects of
did not affect the Why did this study not show family rounds in other settings. Although no other
global measure of global improvements in satisfaction major changes were noted in our routine ICU prac-
among patients’ family members? tices during the course of the study, it is possible
family satisfaction. Several important factors must be that improvements in satisfaction were confounded
considered when addressing this by unmeasured factors such as time spent in further
intriguing question. As seen in other studies using communications during the rest of the day. In future
the FS-ICU,4,25,31,42 family members in the baseline work, particular attention should be given to the
group reported high satisfaction in general, thus time nurses and physicians spend communicating
improvements in satisfaction with family rounds medical updates to patients’ families as well as the
could have been difficult to detect because the high effect on nursing work flow and productivity during
baseline ratings may have caused a ceiling effect. the day. Different ICU team members differ with
Combined with the limited number of questions respect to their reactions to family rounds,38,43 neces-
on the FS-ICU that targeted aspects likely to be sitating exploration of the effects of family rounds
affected by family rounds, our study most likely had on all members of the team.
428 AJCC AMERICAN JOURNAL OF CRITICAL CARE, September 2010, Volume 19, No. 5 www.ajcconline.org
Downloaded from http://ajcc.aacnjournals.org/ by AACN on January 5, 2018
Conclusions 2. Azoulay E, Pochard F, Chevret S, et al. Meeting the needs
of intensive care unit patient families: a multicenter study.
ICU patients’ and families’ satisfaction and com- Am J Respir Crit Care Med. 2001;163(1):135-139.
prehension of the course of critical illness increas- 3. Azoulay E, Sprung CL. Family-physician interactions in the
intensive care unit. Crit Care Med. 2004;32(11):2323-2328.
ingly are recognized as relevant measures of outcome 4. Heyland D, Cook D, Rocker G, et al. Decision-making in the
and benchmarks of high-quality ICU care. Family ICU: perspectives of the substitute decision-maker. Inten-
sive Care Med. 2003;29(1):75-82.
members participate in decision making, represent- 5. Lautrette A, Darmon M, Megarbane B, et al. A communica-
ing the voice of the patient, and suffer significant tion strategy and brochure for relatives of patients dying in
the ICU. N Engl J Med. 2007;356(5):469-478.
distress when inadequately educated and supported 6. Pochard F, Darmon M, Fassier T, et al. Symptoms of anxiety
during a loved one’s ICU care. In this pilot investi- and depression in family members of intensive care unit
patients before discharge or death: a prospective multicen-
gation, including a family component in daily inter- ter study. J Crit Care. 2005;20:90-96.
disciplinary rounds appeared to be a potential means 7. Mosenthal AC. Palliative care in the surgical ICU. Surg Clin
North Am. 2005;85:303-313.
by which to improve some elements of satisfaction, 8. Azoulay E. The end-of-life family conference: communication
including support during decision making and fre- empowers. Am J Respir Crit Care Med. 2005;171(8):803-804.
9. Curtis JR, Engelberg RA, Wenrich MD, et al. Studying com-
quency of communication with physicians. Yet, an munication about end-of-life care during the ICU family
important minority of respondents reported inade- conference: developing a framework. J Crit Care. 2002;17(3):
147-160.
quate time for decision making. 10. Curtis JR, Engelberg RA, Wenrich MD, et al. Missed oppor-
Global satisfaction was not changed by the tunities during family conferences about end-of-life care in
the intensive care unit. Am J Respir Crit Care Med. 2005;171:
implementation of family rounds in this study, and 844-849.
concern was raised about a potential negative per- 11. White DB, Engelberg RA, Wenrich MD, Lo B, Curtis JR.
Prognostication during physician-family discussions about
ception regarding having adequate time for decision limiting life support in intensive care units. Crit Care Med.
making. A need remains to explore further the impact 2007;2007(35):442-448.
12. Latta L, Dick R, Parry C, Tamura G. Parental responses to
of family rounds on family members’ psychological involvement in rounds on a pediatric inpatient unit at a
outcomes, family rounds’ ability to affect family teaching hospital: a qualitative study. Acad Med. 2008;83(3):
292-297.
members’ comprehension and knowledge, the use 13. Lewis C, Knopf D, Chastain-Lorber K, et al. Patient, parent,
and effects of physicians’ differing communication and physician perspectives on pediatric oncology rounds.
J Pediatr. 1988;112(3):378-384.
styles and approaches, factors influencing family 14. Muething SE, Kotagal UR, Schoettker PJ, Gonzalez del Rey
attendance at family rounds, and the effect of fam- J, DeWitt TG. Family-centered bedside rounds: a new
approach to patient care and teaching. Pediatrics. 2007;119:
ily rounds on an ICU team’s workload. 829-832.
15. Mangram A, Mccauley T, Villarreal D, et al. Families’ percep-
tion of the value of timed daily “family rounds” in a trauma
ACKNOWLEDGMENTS
ICU. Am Surg. 2005;71(10):886-891.
We thank the director of the medical intensive care unit, 16. Schiller WR, Anderson BF. Family as a member of the trauma
Art Wheeler, MD, and the nurse manager of the medical rounds: a strategy for maximized communication. J Trauma
intensive care unit, Julie Foss, RN, MSN, for their support Nurs. 2003;10(4):93-99.
in the implementation of this research. Additionally, we 17. Lehmann LL, Brancati FL, Chen M-C, Roter D, Dobs AS. The
thank Andrea Dugas, MD, for her assistance in conducting effect of bedside case presentations on patients’ perceptions
phone surveys of family members. of their medical care. N Engl J Med. 1997;336(16):1150-1155.
18. Wang-Cheng R, Barnsas G, Sigmann P, Riendl P, Young M.
Bedside case presentations: why patients like them but
FINANCIAL DISCLOSURES
learners don’t. J Gen Intern Med. 1989;4(4):284-287.
During the course of this research, Dr Girard was sup- 19. Beckstrand RL, Kirchhoff KT. Providing end-of-life care to
ported in part by the National Institutes of Health patients: critical care nurses’ perceived obstacles and sup-
(AG034257), the Hartford Geriatrics Health Outcomes portive behaviors. Am J Crit Care. 2005;14(5):395-403.
Research Scholars Award Program, the Vanderbilt Physi- 20. Azoulay E, Pochard F. Communication with family members
cian Scientist Development Program, and the Veterans of patients dying in the intensive care unit. Curr Opin Crit
Affairs Tennessee Valley Geriatrics Research, Education Care. 2003;9:545-550.
and Clinical Center. Dr Ely was supported in part by the 21. Azoulay E, Chevret S, Leleu G, et al. Half the families of
intensive care unit patients experience inadequate commu-
National Institutes of Health (AG027472) and the Veter-
nication with physicians. Crit Care Med. 2000;28(8):3116-3117.
ans Affairs Tennessee Valley Geriatrics Research, Educa- 22. Azoulay E, Pochard F, Chevret S, Arich C, et al. Family par-
tion and Clinical Center. ticipation in care to the critically ill: opinions of families
and staff. Intensive Care Med. 2003;29:1498-1504.
23. Curtis JR, White DB. Practical guidelines for evidence-
based ICU family conferences. Chest. 2008;134:835-843.
eLetters
24. Wall RJ, Engelberg RA, Downey L, Heyland D, Curtis JR.
Now that you’ve read the article, create or contribute to an
Refinement, scoring, and validation of the Family Satisfac-
online discussion on this topic. Visit www.ajcconline.org
tion in the ICU (FS-ICU) survey. Crit Care Med. 2007;35(1):
and click “Respond to This Article” in either the full-text or
271-279.
PDF view of the article.
25. Heyland D, Rocker G, Dodeck P, et al. Family satisfaction
with care in the intensive care unit: results of a multiple
center study. Crit Care Med. 2002;30(7):1413-1418.
26. Perneger T. What’s wrong with Bonferroni adjustments.
REFERENCES BMJ. 1998;316(7139):1236-1238.
1. Azoulay E, Pochard F, Chevret S, et al. Impact of a family 27. Rothman K. No adjustments are needed for multiple com-
information leaflet on effectiveness of information provided parisons. Epidemiology. 1990;1(1):43-46.
to family members of intensive care unit patients. Am J 28. Azoulay E, Pochard F, Chevret S, et al. Half the family mem-
Respir Crit Care Med. 2002;165:438-442. bers of intensive care unit patients do not want to share in
www.ajcconline.org AJCC AMERICAN JOURNAL OF CRITICAL CARE, September 2010, Volume 19, No. 5 429
Downloaded from http://ajcc.aacnjournals.org/ by AACN on January 5, 2018
the decision-making process: a study in 78 French intensive 37. Curtis JR, Treecy PD, Nielsen EL, et al. Integrating palliative
care units. Crit Care Med. 2004;32(9):1832-1838. and critical care: evaluation of a quality-improvement inter-
29. LeClaire M, Oakes J, Weinert C. Communication of prognos- vention. Am J Respir Crit Care Med. 2008;178:269-275.
tic information for critically ill patients. Chest. 2005;128(3): 38. Hamric AB, Blackhall LJ. Nurse-physician perspectives on
1728-1735. the care of dying patients in intensive care units: collabora-
30. Cohen S, Sprung CL, Sjokvist P, et al. Communication in tion, moral distress, and ethical climate. Crit Care Med.
end-of-life decisions in European intensive care units. 2007;35(2):422-429.
Intensive Care Med. 2005;31:1215-1221. 39. Ho KM. The involvement of intensive care nurses in end-of-
31. Heyland D, Rocker G, O’Callaghan C, Dodeck P, Cook D. life decisions: a nationwide survey. Intensive Care Med.
Dying in the ICU: perspectives of family members. Chest. 2005;31:668-673.
2003;124(1):392-397. 40. Davidson JE, Powers K, Hedayat KM, et al. Clinical practice
32. Gerstel E, Engelberg RA, Koepsell T, Curtis JR. Duration of guidelines for support of the family in the patient-centered
withdrawal of life support in the intensive care unit and intensive care unit: American College of Critical Care Medi-
association with family satisfaction. Am J Respir Crit Care cine task force. Crit Care Med. 2007;35(2):605-622.
Med. 2008;178:798-804. 41. Treece PD, Engelberg RA, Shannon SE, et al. Integrating
33. Curtis JR. Caring for patients with critical illness and their palliative and critical care: description of an intervention.
families: the value of an integrated team. Respir Care. 2008; Crit Care Med. 2008;34(11 suppl):2380-2387.
53(4):480-487. 42. Gries CJ, Curtis JR, Wall RJ, Engelberg RA. Family member
34. Pham K, Thornton J, Engelberg RA, Jackson J, Curtis JR. satisfaction with end-of-life decision making in the ICU.
Alterations during medical interpretation of ICU family con- Chest. 2008;133:704-712.
ference that interfere with or enhance communication. 43. Levy CR, Ely EW, Payne K, et al. Quality of death and dying
Chest. 2008;134(1):106-116. in two medical ICUs: perceptions of family and clinicians.
35. Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, Chest. 2005;127(5):1775-1783.
and partnership in the patient-physician relationship. JAMA.
1999;282(6):583-589.
36. Napoles AMN, Gregorich SE, Santoyo-Olsson J, O’Brien H,
To purchase electronic or print reprints, contact The
Stewart AL. Interpersonal processes of care and patient InnoVision Group, 101 Columbia, Aliso Viejo, CA 92656.
satisfaction: do associations differ by race, ethnicity, and Phone, (800) 899-1712 or (949) 362-2050 (ext 532); fax,
language? Health Serv Res. 2009;44(4):1326-1344. (949) 362-2049; e-mail, reprints@aacn.org.
430 AJCC AMERICAN JOURNAL OF CRITICAL CARE, September 2010, Volume 19, No. 5 www.ajcconline.org
Downloaded from http://ajcc.aacnjournals.org/ by AACN on January 5, 2018
Communication in Critical Care: Family Rounds in the Intensive Care Unit
Natalie L. Jacobowski, Timothy D. Girard, John A. Mulder and E. Wesley Ely
Am J Crit Care 2010;19 421-430 10.4037/ajcc2010656
©2010 American Association of Critical-Care Nurses
Published online http://ajcc.aacnjournals.org/
Personal use only. For copyright permission information:
http://ajcc.aacnjournals.org/cgi/external_ref?link_type=PERMISSIONDIRECT
Subscription Information
http://ajcc.aacnjournals.org/subscriptions/
Information for authors
http://ajcc.aacnjournals.org/misc/ifora.xhtml
Submit a manuscript
http://www.editorialmanager.com/ajcc
Email alerts
http://ajcc.aacnjournals.org/subscriptions/etoc.xhtml
The American Journal of Critical Care is an official peer-reviewed journal of the American Association of Critical-Care Nurses
(AACN) published bimonthly by AACN, 101 Columbia, Aliso Viejo, CA 92656. Telephone: (800) 899-1712, (949) 362-2050, ext.
532. Fax: (949) 362-2049. Copyright ©2016 by AACN. All rights reserved.
Downloaded from http://ajcc.aacnjournals.org/ by AACN on January 5, 2018
S-ar putea să vă placă și
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Bookshelf NBK153098Document238 paginiBookshelf NBK153098Beny HermawanÎncă nu există evaluări
- Jurnal 16Document166 paginiJurnal 16Beny HermawanÎncă nu există evaluări
- Jurnal 9Document312 paginiJurnal 9Beny HermawanÎncă nu există evaluări
- Jurnal 12Document142 paginiJurnal 12Beny HermawanÎncă nu există evaluări
- Jurnal 9Document312 paginiJurnal 9Beny HermawanÎncă nu există evaluări
- The Effect of An Emergency Department Dedicated Midtrack Area On Patient FlowDocument6 paginiThe Effect of An Emergency Department Dedicated Midtrack Area On Patient FlowBeny HermawanÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Homeroom Guidance Learner'S Development Assessment: School Year 2020 - 2021 KindergartenDocument3 paginiHomeroom Guidance Learner'S Development Assessment: School Year 2020 - 2021 KindergartenRouselle Umagat Rara100% (1)
- NLR - Vol 8 - No-2Document330 paginiNLR - Vol 8 - No-2Ankit AmanÎncă nu există evaluări
- EDUC 213 - Final 5Document8 paginiEDUC 213 - Final 5Fe Canoy100% (2)
- Valuing Vs Recognizing EmployeesDocument5 paginiValuing Vs Recognizing EmployeesSush BiswasÎncă nu există evaluări
- Career Development WorkbookDocument15 paginiCareer Development WorkbookDheeraj BahlÎncă nu există evaluări
- Financial Literacy and Financial Behavior of Management Undergraduates of Sri LankaDocument6 paginiFinancial Literacy and Financial Behavior of Management Undergraduates of Sri LankaRod SisonÎncă nu există evaluări
- Enrichment Activity MAS RELEVANT COSTINGDocument3 paginiEnrichment Activity MAS RELEVANT COSTINGarlyn ajero100% (1)
- Unit 17. ULC - Assignment - 17BMDocument19 paginiUnit 17. ULC - Assignment - 17BMMinh LợiÎncă nu există evaluări
- Ogl 481 Pro-Seminar I Pca-Human Resource Frame Worksheet 2Document2 paginiOgl 481 Pro-Seminar I Pca-Human Resource Frame Worksheet 2api-545456362Încă nu există evaluări
- Homeroom ReportDocument15 paginiHomeroom ReportReese Arvy MurchanteÎncă nu există evaluări
- 4th SemDocument70 pagini4th SemSandeep KumarÎncă nu există evaluări
- Business EthicsDocument12 paginiBusiness EthicsGil DelgadoÎncă nu există evaluări
- Principles of Management: Assignment ONDocument5 paginiPrinciples of Management: Assignment ONshivaniÎncă nu există evaluări
- Cognitive Biases of Investors and Financial Risk ToleranceDocument6 paginiCognitive Biases of Investors and Financial Risk TolerancelaluaÎncă nu există evaluări
- Organizational Structure Redesign For An Aviation Services Company - A PaperDocument24 paginiOrganizational Structure Redesign For An Aviation Services Company - A PapernanditaÎncă nu există evaluări
- Pmqa 3Document3 paginiPmqa 3YoushÎncă nu există evaluări
- 9.decision TheoryDocument51 pagini9.decision Theorysrishti bhatejaÎncă nu există evaluări
- GDMS FinalDocument1 paginăGDMS FinalJoysri RoyÎncă nu există evaluări
- A Systematic Problem Solving & Decision Making Method: Kepner Tregoe Problem AnalysisDocument16 paginiA Systematic Problem Solving & Decision Making Method: Kepner Tregoe Problem AnalysisRahul_regal100% (1)
- Land Evaluation ASLE DefinitionsDocument13 paginiLand Evaluation ASLE DefinitionsKani ManikandanÎncă nu există evaluări
- ST - Scholasticas College Tacloban: Basic Education DepartmentDocument13 paginiST - Scholasticas College Tacloban: Basic Education DepartmentThereseÎncă nu există evaluări
- IE 405 ProblemSet 4 Solutions SharedDocument3 paginiIE 405 ProblemSet 4 Solutions SharedHasan AydınÎncă nu există evaluări
- Brainstorming and NGTDocument21 paginiBrainstorming and NGTkabbirhossainÎncă nu există evaluări
- Critical Success Factors For Creating SuperbDocument14 paginiCritical Success Factors For Creating Superbali al-palaganiÎncă nu există evaluări
- ql7 STRDocument41 paginiql7 STRDanish ButtÎncă nu există evaluări
- Orlove 1980 - Ecological AnthropologyDocument40 paginiOrlove 1980 - Ecological AnthropologyJona Mae VictorianoÎncă nu există evaluări
- Planning Function of Management PPMDocument6 paginiPlanning Function of Management PPMCalvince OumaÎncă nu există evaluări
- AIand HRMframeworkDocument21 paginiAIand HRMframeworkJohn AstliÎncă nu există evaluări
- Book Review Built To ServeDocument16 paginiBook Review Built To ServegajamaniÎncă nu există evaluări
- Rapid Risk Assessment of Acute Public Health EventsDocument44 paginiRapid Risk Assessment of Acute Public Health EventsdinahajjarÎncă nu există evaluări