Documente Academic
Documente Profesional
Documente Cultură
BiliSummary - Newborn Nursery at LPCH - Stanford University School of Medici
Încărcat de
Mohammed Usman IbrahimDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
BiliSummary - Newborn Nursery at LPCH - Stanford University School of Medici
Încărcat de
Mohammed Usman IbrahimDrepturi de autor:
Formate disponibile
BiliSummary - Newborn Nursery at LPCH - Stanford University School of Medicine
Bilirubin Screening and Management of
Hyperbilirubinemia
This document does not represent a comprehensive review of relevant information or
recommendations included in the Clinical Practice Guideline released by the AAP Subcommittee of
Pediatrics. It is only meant to be a quick summary/reference of useful points coupled with our
approach to bilirubin screening at LPCH. For the complete guideline visit the AAP link below.
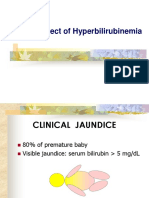
The Pathophysiology of Hyperbilirubinemia
Guidelines for Phototherapy
The LPCH Approach to Screening
AAP Clinical Practice Guideline
Bilirubin Basics:
Bilirubin is derived from proteins that contain heme
Biggest source is breakdown of from red blood cells
Heme is broken down to biliverdin, which is reduced to bilirubin (in the process, CO is
produced)
Measurement of exhaled CO is an indication of ongoing hemolysis
Major Risk Factors for Developing Hyperbilirubinemia:
Predischarge TSB in High Risk zone on Bhutani nomogram
Jaundice observed in the first 24 hours
ABO incompatibility with positive direct Coombs, other known helmolytic disease
Gestational age 35-36 weeks
Previous sibling received phototherapy
Cephalohematoma or significant bruising
Exclusive breastfeeding, especially if not nursing well and excessive weight loss
East Asian race
Use of Nomograms and Guidelines:
http://newborns.stanford.edu/BiliSummary.html[9/6/2010 6:50:18 AM]
BiliSummary - Newborn Nursery at LPCH - Stanford University School of Medicine
Nomograms help assess risk for developing hyperbilirubinemia and help arrange
appropriate follow-up
There is now good data and an accepted nomogram for assessing risk based on bilirubin
level (Bhutani, 1999)
Clinical Guidelines for screening and management are available from the AAP (July 2004)
Early jaundice (age < 24h) still has a broad differential and requires workup, despite the
ease of initiating management with phototherapy
Bilirubin Screening:
Screening policies that are widely used do not have good evidence for predicting
hyperbilirubinemia (eg. screening babies of all O+ moms)
Total Serum Bilirubin is inexpensive (<$2) and thus has a good cost/benefit ratio
Technology will ultimately allow us to determine ongoing hemolysis with exhaled CO
back to top
Guidelines for Initiating Phototherapy . . .
. . . IF INFANT IS "LOW RISK"
>38 WEEKS AND OTHERWISE WELL
Age 24 hours 48 hours 72 hours 96 hours
TSB 12 mg/dl 15 mg/dl 18 mg/dl 20 mg/dl
. . . IF INFANT IS "MEDIUM RISK"
>38 WEEKS WITH RISK FACTOR (see below) OR 35 - 37 WEEKS AND WELL
Age 24 hours 48 hours 72 hours 96 hours
TSB 10 mg/dl 13 mg/dl 15 mg/dl 17 mg/dl
. . . IF INFANT IS "HIGH RISK"
35-37 WEEKS WITH RISK FACTOR (see below)
Age 24 hours 48 hours 72 hours 96 hours
TSB 8 mg/dl 11 mg/dl 13 mg/dl 15 mg/dl
http://newborns.stanford.edu/BiliSummary.html[9/6/2010 6:50:18 AM]
BiliSummary - Newborn Nursery at LPCH - Stanford University School of Medicine
RISK FACTORS THAT IMPACT
PHOTOTHERAPY RECOMENDATIONS
ISOIMMUNE HEMOLYTIC DISEASE
G6PD DEFICIENCY
ASPHYXIA
LETHARGY
TEMPERATURE INSTABILITY
SEPSIS
ACIDOSIS
ALBUMIN <3 g/dL
BiliTool provides a free, user friendly, interactive way to match patient bili
levels to the Bhutani nomogram and phototherapy guidelines.
back to top
the LPCH approach. . .
http://newborns.stanford.edu/BiliSummary.html[9/6/2010 6:50:18 AM]
BiliSummary - Newborn Nursery at LPCH - Stanford University School of Medicine
ABurgos, reviewed 5-06
http://newborns.stanford.edu/BiliSummary.html[9/6/2010 6:50:18 AM]
S-ar putea să vă placă și
- Chem41 Postlabexpt.n0.3Document36 paginiChem41 Postlabexpt.n0.3HJakansjakkaÎncă nu există evaluări
- Jaundice An Emergency Department Approach To Diagnosis and ManagementDocument24 paginiJaundice An Emergency Department Approach To Diagnosis and ManagementAmali FikriahÎncă nu există evaluări
- Inv PedDocument21 paginiInv PedGoha BashaÎncă nu există evaluări
- Neonatal Jaundice Disease Infographics by SlidesgoDocument42 paginiNeonatal Jaundice Disease Infographics by Slidesgoshahedshaderma15Încă nu există evaluări
- Phototherapy 2Document8 paginiPhototherapy 2Dyah Putri PermatasariÎncă nu există evaluări
- Inservices PhototherapyDocument11 paginiInservices PhototherapySweta ManandharÎncă nu există evaluări
- PhototherapyDocument8 paginiPhototherapyNylia AtibiÎncă nu există evaluări
- Review For Pediajc OsoeDocument9 paginiReview For Pediajc OsoeAlloy Trixia BaguioÎncă nu există evaluări
- Bilirubin Less Than 35 WeeksDocument8 paginiBilirubin Less Than 35 WeeksDesmiyati AdoeÎncă nu există evaluări
- Neonatal JaundiceDocument23 paginiNeonatal JaundiceAsad M AminÎncă nu există evaluări
- HyperbilirubinemiaDocument48 paginiHyperbilirubinemiaVirna CuntapayÎncă nu există evaluări
- Mahapedicon 2005Document3 paginiMahapedicon 2005noelmendonsaÎncă nu există evaluări
- NNJ by DR MadhuDocument59 paginiNNJ by DR MadhuNabrazz SthaÎncă nu există evaluări
- HyperbiliruminemiaDocument36 paginiHyperbiliruminemiamurugesh69Încă nu există evaluări
- 04 NNJDocument39 pagini04 NNJKiramatÎncă nu există evaluări
- 2 Jaundice in The NBDocument33 pagini2 Jaundice in The NBCheru DugaseÎncă nu există evaluări
- QR Management of Neonatal Jaundice (Second Edition) PDFDocument8 paginiQR Management of Neonatal Jaundice (Second Edition) PDFOlayinka AwofoduÎncă nu există evaluări
- JaundiceDocument41 paginiJaundicesavina hasbianiÎncă nu există evaluări
- Neonatal Jaundice: Carolyn Joy Mendoza-Capisnon Geraldine Marie SalvoDocument46 paginiNeonatal Jaundice: Carolyn Joy Mendoza-Capisnon Geraldine Marie SalvoCarolyn CapisnonÎncă nu există evaluări
- Mosby Phototherapy 1Document12 paginiMosby Phototherapy 1غيداء الذويبيÎncă nu există evaluări
- Approach To Neonatal HyperbilirubinemiaDocument34 paginiApproach To Neonatal HyperbilirubinemiaNilesh HatzadeÎncă nu există evaluări
- PhototherapyDocument11 paginiPhototherapySweta ManandharÎncă nu există evaluări
- Neonatal HyperbilirubinemiaDocument50 paginiNeonatal HyperbilirubinemiaTommy AkromaÎncă nu există evaluări
- Neonatal Jaundice PDFDocument10 paginiNeonatal Jaundice PDFibanggÎncă nu există evaluări
- Neonatal Jaundice Lecture,,By DR Kassahun GirmaDocument25 paginiNeonatal Jaundice Lecture,,By DR Kassahun GirmaKassahun Girma GelawÎncă nu există evaluări
- Neonatal Jaundice Clinical Practice GuidelineDocument35 paginiNeonatal Jaundice Clinical Practice GuidelineprinsepejesseÎncă nu există evaluări
- Neonatal JaundiceDocument3 paginiNeonatal Jaundicedrraj07Încă nu există evaluări
- Hyperbilirubinemia Practice ToolDocument4 paginiHyperbilirubinemia Practice Toolphilipb010288Încă nu există evaluări
- 01 - GLM - JM - 105 - Product Presentation - FinalDocument68 pagini01 - GLM - JM - 105 - Product Presentation - Finalrahim iqbalÎncă nu există evaluări
- Referat HiperbilirubinemiaDocument27 paginiReferat HiperbilirubinemiasarahfajriaÎncă nu există evaluări
- Christopher Aseervatham Neonatal Jaundice DiscussionDocument7 paginiChristopher Aseervatham Neonatal Jaundice DiscussionChristopher AlÎncă nu există evaluări
- Bilirubin o MetersDocument9 paginiBilirubin o MetersLia OktarinaÎncă nu există evaluări
- Diagnosis and Management of Neonatal Hyperbilirubinemia in Term and Late Preterm InfantsDocument40 paginiDiagnosis and Management of Neonatal Hyperbilirubinemia in Term and Late Preterm InfantsFerinaTarizaIIÎncă nu există evaluări
- Neonatal HyperbilirubinemiaDocument51 paginiNeonatal HyperbilirubinemiaJaya Prabha0% (1)
- Approach To Neonatal HyperbilirubinemiaDocument34 paginiApproach To Neonatal HyperbilirubinemiaNilesh HatzadeÎncă nu există evaluări
- Recent - Neonatal JaundiceDocument30 paginiRecent - Neonatal JaundiceBibek DasÎncă nu există evaluări
- Clinical Aspect of HyperbilirubinemiaDocument39 paginiClinical Aspect of HyperbilirubinemiaAfdelina RizkyÎncă nu există evaluări
- Blood Group and Mechanism of IncompabilityDocument5 paginiBlood Group and Mechanism of IncompabilityshaveimernÎncă nu există evaluări
- Ikterus PDFDocument4 paginiIkterus PDFRibut NingsihÎncă nu există evaluări
- Neonatal JaundiceDocument46 paginiNeonatal JaundiceEricson KipronoÎncă nu există evaluări
- HYPERBILIRUBINEMIADocument30 paginiHYPERBILIRUBINEMIAAlexisRoyE100% (1)
- Neonatal JaundiveDocument15 paginiNeonatal JaundiveCarolyn CapisnonÎncă nu există evaluări
- JaundiceDocument25 paginiJaundiceIke RilleraÎncă nu există evaluări
- 113 JMSCRDocument12 pagini113 JMSCRRiki AntoÎncă nu există evaluări
- Juan DiceDocument12 paginiJuan DiceSutirtha RoyÎncă nu există evaluări
- Management of Hyperbilirubinemia in The Newborn PeriodDocument3 paginiManagement of Hyperbilirubinemia in The Newborn PeriodVineet GuptaÎncă nu există evaluări
- Approach To Neonatal JaundiceDocument36 paginiApproach To Neonatal JaundiceDrMubashir ShaikhÎncă nu există evaluări
- Referat Hiperbil ZDocument26 paginiReferat Hiperbil ZAzando Rizki PutraÎncă nu există evaluări
- Neonatal JaundiceDocument65 paginiNeonatal JaundiceAditi BanerjeeÎncă nu există evaluări
- NNF RecommendationDocument15 paginiNNF RecommendationSuman MondalÎncă nu există evaluări
- Neonatal Jaundice Pathway PDFDocument35 paginiNeonatal Jaundice Pathway PDFarjunaquellÎncă nu există evaluări
- Konsensus HiperbilirubinemiaDocument8 paginiKonsensus Hiperbilirubinemiaanggi6Încă nu există evaluări
- Pertanyaan Jurnal ReadingDocument5 paginiPertanyaan Jurnal ReadingMohammad AlmuhaiminÎncă nu există evaluări
- Hyper Bilirubin Emi ADocument16 paginiHyper Bilirubin Emi ANichole Audrey SaavedraÎncă nu există evaluări
- Ideal Medical Management For HyperbilirubinemiaDocument3 paginiIdeal Medical Management For HyperbilirubinemiaClaring CiprianoÎncă nu există evaluări
- Neonatal Jaundice: Addisu AnDocument38 paginiNeonatal Jaundice: Addisu AnAbiy AliyeÎncă nu există evaluări
- Neonatal Jaundice Cme 3Document56 paginiNeonatal Jaundice Cme 3Arief NorddinÎncă nu există evaluări
- Management of Neonatal Jaundice - Depkes MalaysiaDocument5 paginiManagement of Neonatal Jaundice - Depkes MalaysiaRohmantuah_Tra_1826Încă nu există evaluări
- JaundiceDocument11 paginiJaundiceHusna Mat IsaÎncă nu există evaluări
- PathophysiologyDocument6 paginiPathophysiologyPrei BaltazarÎncă nu există evaluări
- Alert Medical Series: Internal Medicine Alert I, II, IIIDe la EverandAlert Medical Series: Internal Medicine Alert I, II, IIIÎncă nu există evaluări
- Aspirin Antiplatelet Agents During Operative Coronary RevascDocument8 paginiAspirin Antiplatelet Agents During Operative Coronary RevascMohammed Usman IbrahimÎncă nu există evaluări
- Diagnosis and Management of Foodborne Illnesses - A Primer For Physicians 2Document2 paginiDiagnosis and Management of Foodborne Illnesses - A Primer For Physicians 2Mohammed Usman IbrahimÎncă nu există evaluări
- Gen Surgery Straub 07 08Document5 paginiGen Surgery Straub 07 08Mohammed Usman IbrahimÎncă nu există evaluări
- Family MedicineDocument156 paginiFamily MedicinedtriggÎncă nu există evaluări
- Chemical Examination of UrineDocument17 paginiChemical Examination of Urinekaran kambojÎncă nu există evaluări
- Physiology Lec 1Document6 paginiPhysiology Lec 1Hussein AlaÎncă nu există evaluări
- BilirrubinemiaDocument17 paginiBilirrubinemiadanielamonsalvetkÎncă nu există evaluări
- Jaundice: Seminar Under The Guidance Of-Dr. Shiva NarangDocument47 paginiJaundice: Seminar Under The Guidance Of-Dr. Shiva NarangMiguel MansillaÎncă nu există evaluări
- Neonatal JaundiceDocument15 paginiNeonatal JaundiceSharan SekhonÎncă nu există evaluări
- Metabolisme Porfirin 2013Document47 paginiMetabolisme Porfirin 2013Indra ToshiwayÎncă nu există evaluări
- UW Peds Notes - @pedunculatedDocument179 paginiUW Peds Notes - @pedunculatedMarion Sanchez100% (6)
- Assessmentof The Fundamentalaccuracyof The Jendrassik-Gr# (243) F Total and Direct BilirubinassaysDocument6 paginiAssessmentof The Fundamentalaccuracyof The Jendrassik-Gr# (243) F Total and Direct Bilirubinassayssri309Încă nu există evaluări
- Liver MCQDocument14 paginiLiver MCQMohammad Ra'fat Rostom86% (7)
- 1 ThesisDocument70 pagini1 ThesisSuresh L100% (1)
- Assessment of Liver FunctionDocument14 paginiAssessment of Liver FunctionAaron Jed Tan PaulinoÎncă nu există evaluări
- Interference of Bilirubin in Creatinine Value Measurement by Jaffe Kinetic MethodDocument4 paginiInterference of Bilirubin in Creatinine Value Measurement by Jaffe Kinetic MethodSourav MondalÎncă nu există evaluări
- BLOODDocument175 paginiBLOODJohn JimsÎncă nu există evaluări
- 1 Wordsology-1Document200 pagini1 Wordsology-1sehapaldai4Încă nu există evaluări
- Liver Function TestDocument50 paginiLiver Function TestJhannÎncă nu există evaluări
- Hyperbilirubinemia: West Visayas State University College of Medicine Neonatal Intensive Care UnitDocument49 paginiHyperbilirubinemia: West Visayas State University College of Medicine Neonatal Intensive Care UnitDonna LabaniegoÎncă nu există evaluări
- Jbo 028 067001Document14 paginiJbo 028 067001Neethu GeorgeÎncă nu există evaluări
- Jurnal Zinc HiperbilirubinemiaDocument5 paginiJurnal Zinc HiperbilirubinemiaAbdurrohman IzzuddinÎncă nu există evaluări
- Neonatal Jaundice DR - MaslianiDocument58 paginiNeonatal Jaundice DR - MaslianiHengky HanggaraÎncă nu există evaluări
- A Comprehensive: Health Analysis ReportDocument18 paginiA Comprehensive: Health Analysis ReportTanmay BhattÎncă nu există evaluări
- MHRS 48 Medical Examination FormDocument6 paginiMHRS 48 Medical Examination FormImroz AhmedÎncă nu există evaluări
- Reference Range and Normal ValuesDocument13 paginiReference Range and Normal ValuesMs Tahniat RehmanÎncă nu există evaluări
- #10 - NCM109 (Pedia) - TransesDocument70 pagini#10 - NCM109 (Pedia) - TransesJaimie BanaagÎncă nu există evaluări
- Pooled Mcqs For Gre/Gat/Subject Discipline: (Pathology)Document61 paginiPooled Mcqs For Gre/Gat/Subject Discipline: (Pathology)Faizan AliÎncă nu există evaluări
- Liver Disease by Rehana MamDocument20 paginiLiver Disease by Rehana Mamraisameh23Încă nu există evaluări
- Phototherapy 2022Document7 paginiPhototherapy 2022António BragaÎncă nu există evaluări
- Bilirubin: Clinical SignificanceDocument14 paginiBilirubin: Clinical SignificanceLyka PapaÎncă nu există evaluări