Documente Academic
Documente Profesional
Documente Cultură
Bleeding Disorders
Încărcat de
Laurence RoiDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Bleeding Disorders
Încărcat de
Laurence RoiDrepturi de autor:
Formate disponibile
BLEEDING DISORDERS Coagulation Cascade
HEMOSTASIS
A complex process which is well regulated that maintains blood in a fluid, clot-free
state in normal blood vessels
An active process that clots blood in areas of blood vessel injury and limits the clot
size only to the areas of injury
Clot is lysed by the fibrinolytic system to restore normal blood flow
Main components:
o Blood vessels
o Platelets
o Coagulation proteins
o Anticoagulant problems
o Fibrinolytic system
Three mechanisms:
o Vascular spasm – damaged blood vessels constrict
o Platelet plug formation – platelets adhere to damaged endothelium to form
platelet plug (primary hemostasis) and then degranulate
o Blood coagulation – clots form upon the conversion of fibrinogen to fibrin, and
its addition to the platelet plug (secondary hemostasis)
Following and injury to blood vessels…
Fibrinolysis
Local Vasoconstriction
(a) The coagulation cascade, which favors clot formation, is initiated in vivo by tissue factor and
factor VIIa (FVIIa) and leads to the conversion of prothrombin to thrombin by the prothrombinase
complex (FXa and FVa). Subsequent cleavage of fibrinogen by thrombin, along with the
aggregation of platelets, can result in formation of a thrombus. The fibrin clot is further stabilized
by FXIII, which is also activated by thrombin, and the clotting process is magnified by other
positive-feedback loops (not shown). (b) Plasmin-mediated fibrinolysis, resulting in fibrin
degradation products and clot lysis, occurs following the conversion of plasminogen to plasmin by
tissue-type plasminogen activator (tPA). Plasminogen activator inhibitor 1 (PAI-1) rapidly inhibits
tPA. a-2-Antiplasmin (a-2-AP) inactivates plasmin by forming a 1:1 inhibitory complex with
circulating plasmin. Thrombin-activatable fibrinolysis inhibitor (TAFI) cleaves the C-terminal lysine
residues of fibrin, preventing the co-activation of plasminogen by fibrin
Primary Hemostasis (Platelet plug formation) Natural anticoagulants
o Antithrombin III (AT-III)
- Inhibits factor Xa and thrombin
- Inhibits IXa, XIa, XIIa
o Protein C and S
- Activated by thrombin-thrombomodulin complex
- Degrade factor Va and VIIIa
o Tissue Factor pathway Inhibitor (TFPI) – inactivates Xa by VIIa and Tissue factor
The Hemostatic Balance: Hemorrhage = Thrombosis
Abnormalities of Hemostasis
PEDIA: BLEEDING DISORDERS (Dr. Lucero) RMB x PRIMORIS Page 1 of 7
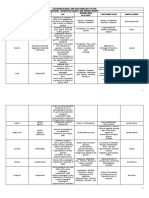
Practical Approach: LABORATORY EVALUATION
Evaluation of a child with bleeding o Screening Tests:
1. Comprehensive medical history, including bleeding history CBC
2. Family History Peripheral Blood Smear
3. Detailed Physical Examination Bleeding Time
4. Selected Laboratory Tests Prothrombin Time
Bleeding History must consider: Activated Partial Thromboplastin Time
o Age PT aPTT Platelet Count Defect:
o Sex
o Clinical Presentation vWD, F VIII, IX, XI deficiency, acquired
Normal Prolonged Normal
o Past History autoantibody anti-against F VIII
o Family history Severe vitamin K deficiency, Liver
Prolonged Prolonged Normal
MEDICAL HISTORY disease, Excessive coagulation
o Type of Bleeding Prolonged Normal Normal Excessive coumarin, Congenital FVII
- Epistaxis? deficiency
- Gum bleeding? Normal Normal Normal vWD, Platelet Function defect
- Menorrhagia? – Excessive uterine bleeding occurring at the expected intervals of the
Platelet Disorder, Von Willebrand,
menstrual periods. Petechiae, Ecchymosis +/- mucous
Disease, Hereditary Telangiectasia,
- Bruising? membrane bleeding
Pinpoint flat round red spots under the skin surface caused by intradermal
Dysfibrinogenemia
hemorrhage (bleeding into the skin) THROMBOCYTOPENIA (Other screening tests normal)
Petechiae
Contain red blood that has leaked from the capillaries into the skin Large Platelets Normal Size Platelets
Tiny (< 3 millimeters in diameter) and do not blanch when pressed upon
ITP
Hemorrhage (bleeding) into the surface of the skin.
HUS Acute leukemia
> 3 millimeters in diameter.
Purpura The appearance of an individual area of purpura varies with the duration of TTP Aplastic Anemia
the lesions. Early purpura is red and becomes darker, then purple, and brown- NAITP
yellow as it fades.
Nonraised skin discoloration caused by the escape of blood into the tissues Manifestation Defect
Ecchymosis from ruptured blood vessels.
Vasculitic Henoch Schonlein Purpura
Can occur in mucous membranes (for example, in the mouth)
A localized swelling that is filled with blood caused by a break in the wall of a Hematoma Coagulopathy, Hemophilia A or B
Hematoma blood vessel. Confluent purpura, Ischemic Disseminated Intravascular
Palpable necrosis Coagulopathy
Clotting factor
Clinical Characteristics Platelet Disorders
deficiency VON WILLEBRAND DISEASE
Site of bleeding Skin, mucous Most common inherited bleeding disorder with qualitative &/or quantitative defects
Deep in soft tissues of multimeric, glycoprotein, Von Willebrand Factor
membranes (gingivae,
nares, GI and GUT)
(joints, muscles) Autosomal inheritance
o Autosomal dominant (Types 1, 2)
Bleeding after minor cuts YES Not usually
o Autosomal recessive (Type 3)
Petechiae Present Absent
Ecchymosis Small, Superficial Large, Palpable Males = Females
Von Willebrand Factor (vWF):
Hemarthrosis, muscle
Rare Common o Adherence of platelets to damage endothelium
hematomas
o Carrier protein for plasma Factor VIII
Bleeding after surgery Intermediate, mild Delayed, Severe
o Stored in the endothelial cells and in platelet Weibel-Palade bodies
o Response to hemostatic challenge
Types:
Surgery: Circumcision, tonsillectomy, Tooth extraction
Type 1 vWD Type 2 vWD Type 3 vWD
Phlebotomy
Immunization/ Intramuscular injection Most common variant Most severe type,
Childbirth (60-80%) Quantitative defects
*Absence of bleeding during surgery affecting the mucosal surfaces rules out a vWF structurally Qualitative defects of vWF completely absent
congenital bleeding disorder. normal, reduced in vWF Plasma vWF and FVIII
o Underlying Medical conditions with known associations with hemostatatic concentration levels <10 units/dl
defects (<30IU/dl)
Liver disease Mild to moderate Subtypes: 2A, 2B, 2N, ICH, Major epistaxis,
Renal Failure quantitative defects 2M, Platelet-type Joint bleed and
Connective Tissue Disorder Pseudo menorrhagia
Malabsorption Syndrome Autosomal dominant Autosomal dominant Autosomal recessive
Vitamin K deficiency Treatment:
Malignancies – Leukemia DDAVP vWF replacement vWF replacement
o Medications that can affect: (Desmopressin) therapy therapy
PLATELET FUNCTION PLATELET COUNT CLOTTING FACTORS platelet Type (Psuedo)
Aspirin Quinidine Anticoagulants: vWD = Platelet
NSAIDs – Naproxen, Ibuprofen, Penicillin Warfarin, transfusion
Phenylbutazone, Piroxicam Anticonvulsants Heparin, LMW Signs & Symptoms:
Ticlopidine Quinine heparin o Epistaxis
Antibiotics: Sulfonamides Antimetabolites: L- o Ecchymosis
PCN – Carbenicillin, Pen G, Digoxin asparginase o Menorrhagia
Ampicillin, Ticarcillin, Nafcillin, Heparin o Post-traumatic. Post-surgical Bleed
Azlocillin Mezlocillin o Post dental extraction
Cephalosphorin – Moxalactam, o CNS bleed
Cefotaxime Laboratory Evaluation
Nitrofurantoin o Screening Tests:
Volume expanders: Dextran, BT prolonged
Hodroethyl starch aPTT prolonged
Heparin PT normal
Fibrinolytic agents Platelet count normal
o Cannot be ruled out on the basis of a normal BT and aPTT
o No reliable screening tests
o Suboptimal sensitivity and specificity
PEDIA: BLEEDING DISORDERS (Dr. Lucero) RMB x PRIMORIS Page 2 of 7
Accurate diagnosis requires the following measurements: Clinical Features:
1. VWF: Ag o Hemarthroses – Hallmark of hemophilia
2. VWF: Rco o Easy bruising
3. VWF: Rco / VWF: Ag o Intramuscular hematomas
4. F VIII:C o Bleeding from minor traumatic lacerations
5. VWF: multimer analysis o Life-threatening bleeding from vital structures (CNS, Upper airways, GI, or
Iliopsoas hemorrhage)
HEMOPHILIA Laboratory Tests:
Inherited, X-linked recessive, lifelong disorder o aPTT – always prolonged (2-3x) in severe hemophilia
Affects males almost exclusively - slightly prolonged or may be normal in mild/moderate hemophilia
Hemophilia A – Factor VII deficiency o Confirmatory: Factor VIII, IX assay
- Classic Hemophilia - FVIII/FIX levels – below the normal range
- More common Severity based on patient’s circulating FVIII/FIX
Hemophilia B – Factor IX deficiency Spontaneous bleeding
- Christmas Disease Recurrent hemarrthrosis
Most serious congenital coagulation factor deficiency SEVERE <1%
Serious hemorrhages into vital organs
X-linked recessive Replacement needed several times per month
↓ blood levels of procoagulant FVIII or FIX Less frequent bleeding
1:5,000-6,000 live male births MODERATE 1-5% Trauma, surgery or dental work
Hemophilia A = 85%; Hemophilia B = 10-15% Occasional hematomas or hemarrthrosis
No apparent racial predilection Infrequent bleeding
6 to <50%
High rate of spontaneous mutation (~30%) MILD Disease undiagnosed for years
6-25%
Inheritance Pattern: Bleeds after severe trauma or surgery
X-linked recessive, expressed primarily in males with defective gene Lower Limit of FVIII & FIX in normal individual ~50%
Symptomatic Carriers: Hemostatic level for FVIII >30-40%; FIX >25-30%
o Factor level: 30-50% Differences: Von Willebrand Disease and Hemophilia
o Daughter of a maternal carrier and a hemophilic father Characteristics Von Willebrand Disease Hemophilia
Symptoms Bruising Joint bleeding
Mucosal Bleeding Muscle bleeding
(epistaxis, menorrhagia)
Sexual Distribution Males = Females Males
Frequency 1:200 to 1:500 1:6000 males
AbN protein vWF Factor VIII
Inhibitor freq Rare 14-25% of patients
Bleeding time Often abnormal Usually normal
PTT Normal or ↑ Prolonged
Factor VIII Borderline or ↓ ↓ or Absent
vWF Ag ↓ or Absent Normal or ↑
vWF R:Co ↓ or Abnormal Normal or ↑
vWF multimers Normal or Abnormal Normal
Treatment
1. Factor replacement therapy – mainstay of TX
- Degree of correction depends on the site & nature of bleeding episode
o Factor VIII or IX concentrates
o Cryoprecipitate – rich in factor VIII, vWF, fibrinogen and FXIII
Hemophilia Inheritance – Father with Hemophilia and Mother Who is Not a Carrier o FFP – contains all clotting factors
2. Ancillary TX
o DDAVP (Stimate) – ↑ FVIII levels 2.5 – 6 fold by releasing endogenously
produced FVIII in mild hemophiliac
o Antifibrinolytic agent – prevents activation of plasminogen to plasmin
Ex: Epsiolon aminocaproic acid, Trenexamic acid
Inhibitor Formation to Hemophilia – Inhibitor alloantibodies, IgG, against factor VIII
or IX that blocks the clotting activity
o 25-35% in Hemophilia A (Hemophilia A>B)
o Severe cases treated; Less common in mild and moderate cases
o Appearance unpredictable
o Clinical Features:
Failure of standard replacement therapy to stop muscle bleed &
hemarthroses
First sign of an inhibitor
Hemophilia Inheritance – Carrier Mother and Father without Hemophilia Decline in half of transfused factor concentrate
Treatment Guidelines in Hemophilia
o Factor VIII – Half life: 8-12 hours
Minor Bleed: 15-25 IU/kg
Major Bleed: 40 – 100 IU/kg
Expected response: 1IU/kg = 2% rise
Dose of Factor VIII = % desired (rise in FVIII) x body wt (kg) x 0.5
o Factor IX – Half life: 12-24 hours
Minor Bleed: 15-22 IU/kg
Major Bleed: 40 – 100 IU/kg
Expected response: 1IU/kg = 1.0-1.5% rise
Dose of Factor VIII = % desired (rise in FIX) x body wt (kg) x 1.4
o Childhood immunization:
Avoid IM injections unless administered under factor cover
Venipuncture of superficial veins – safe press on area >5 minutes
Apply ice
Femoral or jugular venipunctures should not be attempted
PEDIA: BLEEDING DISORDERS (Dr. Lucero) RMB x PRIMORIS Page 3 of 7
Treatment for Inhibitors in Hemophilia LABS: marked prolongation of PT and PTT, prolonged thrombin time,
o Desensitization Program – to saturate the antibody and permit the body to unmeasurable fibrinogen level (diagnostic). In addition to the quantitative
develop tolerance deficiency
- High dose factor VIII or IX concentrate, continuous infusion Dysfibrinogenemia – dysfunctional fibrinogens; Rarely present with thrombosis
o Alternative Approaches: TX: Human fibrinogen concentrate, FFP or cryoprecipitate
a. Activated Prothrombin Complex Concentrate o Fibrinogen t1/2 = 2-4 days
- Activated PCC: Feiba, Atuplex o Hemostatic level of fibrinogen is >60 mg/Dl
- Activation of Factor X o 1 cryoprecipitate = 100-150 mg of fibrinogen
- Dose: 75 IU/kg q12hrs Inhibited by high doses of heparin reptilase time = Prolonged = confirms that
b. Recombinant Factor VIIa functional levels of fibrinogen are low and that heparin is not present.
- Activates Factor X that bypasses Factor VIII
- Dependent steps
PROTHROMBIN (FACTOR II) DEFICIENCY
- Dose: 90 IU/kg q2hrs CAUSE:
c. Immunosuppression o ↓↓Prothrombin level (hypoprothrombinemia) OR
- Cyclophosphamide, Azathioprine o Functionally abnormal prothrombin (dysprothrombinemia)
- IVIG, Cyclosphorin A LABS: Prolonged PT and PTT. Factor II / prothrombin assays: markedly reduced
d. Plasmapheresis CMX: Mucocutaneous bleeding in infancy and posttraumatic bleeding later
Comprehensive Care for Hemophilia TX: FFP / Prothrombin complex concentrates
o State-of-the-Art approach to Hemophilia RX: o Prothrombin t1/2 = 3.5 days
- Coordinated care plan for the patient o 1 IU/kg of prothrombin will increase the plasma activity by 1%
- Family education/prevention/treatment COMBINE DEFICIENCIES OF FACTOR V AND VIII
o Patient is evaluated by a multidisciplinary team: Occurs secondary to the absence of an intracellular transport protein
- Hematologist, Orthopedist, Nurse, Dietician, Infectious disease specialist, Paradoxical deficiency of 2 factors in chromosome 1 & X chromosome.
Social worker, Physical therapist, Dentist, Occupational Therapist, Milder Bleeding symptoms
Psychologist and Genetic counselor
TX: FFP – replace both factors V and VIII.
FACTOR XI DEFICIENCY (HEMOPHILIA C) FACTOR XIII DEFICIENCY – FIBRIN STABILIZING FACTOR
Autosomal, Mild to Moderate bleeding Responsible for the crosslinking of fibrin to stabilize the fibrin clot
Bleeding not correlated with amount of Factor XI CMX: Trauma 1 day and then have a bruise or hematoma the next day.
Bleeding: major surgery o Mild bruising
Chronic joint bleed – rare o Delayed separation of the umbilical stump beyond 4 wk in neonates
PTT prolonged o Poor wound healing
Factor XI assay o Recurrent spontaneous abortions in women
Dental extraction: antifibrinolytic (aminocaproic acid) LABS: normal screening tests, clot dissolves in the presence of 5M urea
FFP – used for replacement therapy TX: Heat-treated, lyophilized concentrate of coagulation factor XIII – treat
bleeding episodes or for prophylaxis.
OTHER COAGULATION FACTOR DEFICIENCIES o Factor XIII t1/2 = 5-7 days
FACTOR VII DEFICIENCY o hemostatic level = 2-3% activity
Rare autosomal bleeding disorder
Usually detected only in the homozygous state. DEFICIENCIES OF CONTACT FACTORS (NONBLEEDING DISORDERS)
CMX: Mild to severe with hemarthroses, spontaneous intracranial hemorrhage, Factor XII, Prekalikrein, HMWK (High Molecular Wt Kininogen)
and mucocutaneous bleeding, especially nosebleeds and menorrhagia PTT – prolonged, no bleeding
LBAS: Markedly prolonged PT but normal PTT, ↓↓↓Factor VII assays No need for Treatment – even with major surgery
TX: Recombinant factor VIIa
o Factor VII plasma t1/2 = 2-4 hr HEMORRHAGIC DISEASE OF THE NEWBORN
CLASSIC HDN
FACTOR V DEFICIENCY (PARAHEMOPHILIA)
Accentuate and prolongation of deficiency of Vit. K dependent factors: II, VII, IX,
Autosomal recessive, mild to moderate bleeding disorder
and X
CMX:
Onset: 2-7 days
o Hemarthroses – rare
Bleeding: GIT, ENT-mucosal, ICH, Post circumcision
o Mucocutaneous bleeding and hematomas – most common symptoms.
Risk Factors: Vit K deficiency, Breastfeeding
o Severe menorrhagia in women
HDN more common among breastfed babies since human milk has less Vit K –
LABS: Prolonged PTT and PT, Factor V assays: ↓
ranges from 1-4cg/L. (1.5ug/L) that cow’s milk (6-12ug/L)
TX: FFP is the only currently available therapeutic product that contains factor V.
LATE ONSET VITAMIN K DEFICIENCY BLEEDING IN THE NEWBORN
o Factor V is lost rapidly from stored FFP
This usually occurs between age 2-12 weeks; however late-onset vitamin K
o Infusion rate: 10 mL/kg every 12 hr
deficiency can be seen as long as 6 months after birth
Acquired antibody to factor V – negative family history of bleeding; does not
This disease is most common in breastfed infants who did not receive vitamin K
bleed because the factor V in platelets prevents excessive bleeding.
prophylaxis at birth
FACTOR X DEFICIENCY Lab: ↑PT, ↑PTT in severe cases
Rare: 1/1,000,000 autosomal disorder with variable severity Prevention: Vitamin K administration (IM, PO)
o Mild deficiency = Mucocutaneous and posttraumatic bleeding TX: Vit K, FFP
o Severe deficiency = Spontaneous hemarthroses and intracranial hemorrhages. POST NEONATAL VITAMIN K DEFICENCY
Quantitative deficiency or a dysfunctional molecule. Vitamin K Deficiency Bleeding:
LABS: Prolongation of both PT and PTT o Vit K dependent clotting factors II, VII, IX, X
TX: FFP or prothrombin complex concentrate o Lack of oral intake of vitamin K
o Factor X plasma t1/2 = 30 hr o Long term use of Broad-spectrum antibiotics – alter GUT flora
o 1 unit/kg will increase the plasma level of factor X by 1% o Liver Disease
Systemic amyloidosis – may be associated with factor X deficiency, owing to the o Malabsorption of Vitamin K: Biliary atresia, Cystic Fibrosis
adsorption of factor X on the amyloid protein. Transfusion therapy often is not Prophylaxis:
successful because of the rapid clearance of factor X. o Oral Vitamin K
- Children: 2-3 mg/24hr
FIBRINOGEN DEFICIENCY (FACTOR I)
- Adolescents/Adults: 5-10 mg/24hr
Congenital afibrinogenemia
o Parenteral Vitamin K: 1-2mg, IV
Rare AR disorder inwhich there is an absence of fibrinogen
CMX:
o Do not bleed as frequently, rarely have hemarthroses.
o Neonatal period: GI hemorrhage or hematomas after vaginal delivery
PEDIA: BLEEDING DISORDERS (Dr. Lucero) RMB x PRIMORIS Page 4 of 7
HENOCH-SCHONLEIN PURPURA THROMBOPHILIA OR HYPERCOAGULABILITY
Also known as anaphylactoid purpura Abnormality in the system of coagulation
Common vasculitis of small vessels with cutaneous and systemic complications Genetic vs. Acquired Defects
Most common cause of nonthrombocytopenic purpura in children Inherited: Unprovoked thrombolytic events in children
Etiology: Unknown Family History of Thrombosis
Clinical Features: Prothrombotic risk factors:
1. Palpable cutaneous purpura – dependent areas of the body or in areas of o Lower extremity casting/ prolonged immobility
greater tissue distensibility o Sedentary lifestyle
2. Arthritis – in 2/3 of patients; localized to the knees and ankles concomitant o Dehydration, Obesity, Smoking
with edema o Estrogen based contraceptives
3. Visceral involvement Inherited Thrombotic Disorders:
a. GIT – colicky abdominal pain; >1/2 occult heme (+) stools a. Deficiency or Qualitative Abnormalities of Inhibitors of activated coagulation
b. Kidneys – 25-30% with nephritis or nephrosis factors
b. Impaired Clot lysis
c. Metabolic Defect
d. Abnormality of coagulation zymogen or cofactor
Common Inherited Thrombophilias:
o Factor V Leiden mutation
o Prothrombin 20210 mutation
o Antithrombin Deficiency
o Protein S deficiency
o Hyperhomocystinemia
o Elevated Factor VIII
INHERITED THROMBOTIC DISORDERS
FACTOR V LEIDEN MUTATION
Most common inherited risk factor for thrombosis
Factor Va becomes resistant to inactivation by activated protein C, also known as
“Activated Protein C Resistance”
Heterozygous state: 5-7 fold increase for venous thrombosis
Homozygous state: relative risk of 80-100 fold
PROTHROMBIN GENE MUTATION G20210A
Increased levels of prothrombin messenger RNA
Relative risk 2-3 fold
PROTEIN C, S AND ANTITHROMBIN III DEFICIENCY
Deficiency of naturally occurring anticoagulants
Rare but stronger risk for thrombosis
Heterozygous state: Do not often present during childhood
Homozygous state: Present as pupura fulminans
NEONATAL PURPURA FULMINANS
Due to homozygous state deficiency of AT, Protein C,S
Life threatening clinical entity
o Rapidly spreading purpuric skin lesions
o Necrotic purpura of the skin
o Thrombosis of major vessels
o Cerebral thrombosis, Opthalmic thrombosis
Definitive DX of Vasculitis: Biopsy of cutaneous site showing leukocytoclastic angitis o DIC
–when presentation is typical Treatment: FFP, Protein C and AT concentrates
Treatment:
o Symptomatic
HOMOCYSTINURIA
o Steroids for intestinal symptoms An inborn error of metabolism
o Hydrostatic reduction or resection of intussusceptions when necessary Deficiency of cystathione -synthase, resulting to an increase in homocysteine
>100umol/L
DISSEMINATED INTRAVASCULAR COAGULOPATHY Associated with venous and arterial thrombosis
Consumption of coagulation factors, platelets and anticoagulant proteins ELEVATED FVIII (>150 IU/dl)
Widespread intravascular deposition of fibrin Ischemia, Necrosis, a generalized Regulated by genetic and environmental factors
hemorrhagic state and Microangipathic Hemolytic Anemia Increased risk for thrombosis
Life threatening pathologic process: Hypoxia, Acidosis, Tissue necrosis, Shock and Acute phase reactant – increase transiently during inflammation
Endothelial damage mat trigger DIC
Secondary event associated with septic shock, incompatible blood transfusion, Giant THROMBOTIC DISORDERS IN CHILDREN
Hemangioma, Malignancy (APL), Purpura fulminans, Snakebite, Ricketsial Infection VENOUS THROMBOEMBOLISM (VTE)
Clinical Manifestations: Central Venous Catheter (CVC) – single most important risk factor
o Bleeding frequently occur in sites of venipunctures/ Surgical incision 90% neonatal VTE; 60% childhood VTE
o Petechiae and Ecchymosis Damage endothelial lining, Blood flow disruption
o Tissue necrosis/infarction of skin, Subcutaneous tissues, or Kidney
Acquired Risk Factors: Trauma, Infection, Vasculitis, Medications
Lab Findings: Hypercoagulable states:
o Consumption of Factors II, V, VIII, Fibrinogen, Platelets
o Prematurity
o Prolongation of PT, aPTT, Thrombin Time
o Congenital heart diseases
o Thrombocytopenia
o Pregnancy, Malignancy
o PBS: RBCs are fragmented, helmet-shaped, burr cells (Schistocytes)
o Nephrotic Syndrome
o FDPs, D-dimers – more specific for activation of coagulation and fibrinolysis
o Antiphospholipid Syndrome
Treatment:
o Treat the underlying cause (trigger)
o Restore normal hemostasis by correcting shock, acidosis, hypoxia
o Blood components for replacement: Platelets, FFP, cryoprecipitate
PEDIA: BLEEDING DISORDERS (Dr. Lucero) RMB x PRIMORIS Page 5 of 7
CLINICAL MANIFESTATIONS (THROMBOSIS) PLATELETS
Extremity Deep Vein Thrombosis Non-nucleated cellular fragments produced by megakaryocytes
- Pain, swelling, discoloration Thrombopoietin (TPO) – growth factor for platelet production
- History of current or recent CVC in that extremity Life span of platelets: 10-14 days
Pulmonary Embolism Normal platelet count: 150 – 450 x 109/L
- Shortness of breath, pleuritic chest pain, cough, hemoptysis, fever Platelets play multiple hemostatic roles
- Massive: hypotension, right heart failure o Platelet adhesion: vWF
Cerebral Sinovenous Thrombosis (CSVT) o Platelet aggregation: Agonists – ADP, ATP, Collagen, Ristocetin, Epinephrine,
- Neonates: Seizure Arachidonic acid, Thrombin
- Children: Headahce, vomiting, seizures, focal signs
- Concurrent sinusitis, Mastoiditis PLATELET DISORDERS
Renal Vein Thrombosis (RVT) I. Platelet Function Defects (inherited/ Acquired)
- Most common spontaneous TE in neonates II. Platelet Disorders with Thrombocytopenia
- Hematuria, abdominal mass, and/or thrombocytopenia
PLATELET FUNCTION DISORDERS
- Infants of Diabetic Mothers – increased risk
Most inborn platelet pathologies predispose to hemorrhage
- 25% bilateral
Rare conditions
Peripheral Arterial Thrombosis
- Neonates: Umbilical catheters Laboratory Findings:
o Bleeding Time (platelet-vessel wall interaction) – prolonged
- Cardiac defects: Cardiac catherization
o PFA – 100 (platelet adhesion/aggregation) – prolonged
- Extremities: Cold, Pale, Blue, Poor/absent pulses
o Platelet aggregometer
Stroke
o Normal platelet count
- Acute Ischemic Stroke: Hemiparesis, Loss of consciousness, Seizures
- Intracranial arteries – Sickle Cell Disease, Vasculopathy, Traumatic arterial CONGENITAL PLATELET DEFECTS
dissection Glanzmann’s Thrombasthenia – deficient GP IIb-IIIa
- Venous thrombi – Congenital heart disease (patent foramen ovale) o Fibrinogen receptor on the platelets
Rapidly Progressive Thrombosis Bernard-Soulier Syndrome – abnormal glycoprotein Ib-IX-V complex
- Rare complication of APS, Heparin-induced thrombocytopenia with o VWF receptor on platelets
thrombosis, thrombotic thrombocytopenic purpura (while on antithrombotic Gray Platelet Syndrome – deficient alpha granules
therapy) Delta Storage Pool Deficiency – deficient dense granules
- Multiple organ dysfunction, Elevated D-dimer levels Von Willebrand disease – deficiency or abnormal vWF
- Treatment: anticoagulation, direct thrombin inhibitor, fondaparinux followed
ACQUIRED DEFECTS
by prolongated warfarin therapy
Liver Disease
DIAGNOSIS Kidney Disease (Uremia)
Ultrasound with Doppler Flow – Upper/Lower Extremity VTE Drug-induced (Aspirin) – Valproic acid, High dose Penicillin
Spiral CT – diagnose PE
CT and MR Venography PLATELET DISORDERS (THROMBOCYTOPENIA)
Brain MRI with Venography (MRV) – cerebral sinovenous thrombosis and acute Causes:
ishemic stroke o Decreased production – congenital or acquired
Laboratory Findings: o Sequestration of platelets by an enlarged spleen
o CBC, PT, aPTT o Increased destruction – immune or nonimmune
o D-dimer
I. DECREASED PRODUCTION OF PLATELETS
o Renal & Hepatic Fucntion tests
A. Congenital Causes:
o Work-up for APS – lupus anticoagulant, anticardiolipin, -glycoprotein
Congenital Amegakaryocytic Thrombocytopenia
antibodies
Thrombocytopenia Absent Radius (TAR)
o Thrombophilia Testing – inherited risk factors
Wiskott-Aldrich Syndrome
TREATMENT: B. Acquired causes:
Therapeutic options: Anticoagulation, Thrombolysis, Surgery, Observation Infiltrative: Leukemia, Histiocytosis, Lymphoma
a. Anticoagulation Aplastic Anemia
Goal: reduce the risk of embolism, stop clot extension, prevent recurrence Myelodysplastic Syndrome (MDS)
Anticoagulants: catalyzes action of Antithrombin (AT) Drug/Radiation-induced
o Therapeutic heparin dose – aPTT 1.5 – 2.5x (upper limit of normal)
Nutirtional: Folate, Vitamin B12
Unfractioned Heparin (uFH): 75-100 u/kg (bolus); 20-28 U/kg (continuous
infusion) II. SEQUESTRATION OF PLATELETS
Low Molecular Weight Heparin (Enoxaparin) Hypersplenism (Massive Splenomegaly)
o <2 months old: 1.5mg/kg, every 12 hrs, subcutaneous o Pancytopenia
o >2 months old: 1 mg/kg, every 12 hrs, subcutaneous Etiology:
o Monitoring: Anti-Xa activity (4 hrs after 2nd or 3rd dose) = 0.5 to 1 IU/ml o Infectious
o Caution for patients with renal insufficiency, avoided in renal failure o Inflammatory
Warfarin – oral anticoagulant o Infiltrative
o MOA: Decrease concentration of Vitamin K dependent factors II, VII, IX, X, o Neoplastic
Protein C,S o Obstructive
o Dose: 0.1-0.2 mg/kg, orally o Hemolytic
o PT – monitoring using International Normalized Ratio (INR)
o VTE: INR 2.0 -3.0 III. PLATELET DESTRUCTION
Direct Thrombin or Factor Xa Inhbitors A. IMMUNE:
b. Thrombolytic Therapy – hasten thrombus resolution (tissue plasminogen Acute and Chronic ITP, HIV-associated
activator) Autoimmune disorders: SLE
Thromboprophylaxis Antiphospholipid Antibody Syndrome
Antiplatelet Therapy Neonatal Immune Thrombocytopenia
Drug-induced Immune Thrombocytopenia
Post-transfusion purpura, Post-transplant pupura
B. NONIMMUNE:
Infections: Viral, Bacterial, Protozoan
Thrombotic Microangiopathic Disorders: HUS, TTP
DIC, Kasabach-Merirtt Syndrome, Drug-induced
Congenital Heart Disease
PEDIA: BLEEDING DISORDERS (Dr. Lucero) RMB x PRIMORIS Page 6 of 7
IMMUNE THROMBOCYTOPENIC PURPURA NON-IMMUNE THROMBOCYTOPENIA
Most common cause of acute thrombocytopenia in an otherwise well child HEMOLYTIC UREMIC SYNDROME
1/20,000 Acute disease of infancy & early childhood following acute gastroenteritis,
Antibody coated platelets are recognized by Fc receptor on the splenic E.coli0157:H7 (Verotoxin)
macrophages, thus are ingested and destroyed Hemolytic anemia, Thrombocytopenia, Acute renal failure
RBC morphology: Helmet cells, Spherocytes, Schistocytes, Burr cells
D-dimers: increased
Urinalysis: Proteins, RBCs, Casts
Treatments: Fluid therapy, Prompt dialysis, Plasmapheresis: HUS with neurologic
complications
Etiology: Unknown
o Antecedent viral infection in 1-4 wks (50-65%) THROMBOTIC THROMBOCYTOPENIC PURPURA
o Autoantibodies against platelet surface – a1 1b-3 and GP1b Rare
o EBV-related ITP: Short duration, follows course of Infectious Mononucleosis Pentad: Fever, Microangiopathic hemolytic anemia, Thrombocytopenia, Abnormal
o HIV-associated ITP: Chronic renal function, CNS changes
o Helicobacter pylori Clinically similar to HUS
o Following vaccinations Congenital, Adults (usually), Adolescents (occasional)
Clinical Features: Etiology:
o Generally well-looking, unless with serious bleeding (CNS, intraabdominal) o Antibody-mediated deficiency of metalloproteinase (ADAMTS-13)
Platelet Count <10,000 o Cleaves HMW multimers of VWF
o Normal PE except for mucocutaneous bleeding o Thrombotic microangiopathy
o Splenomegaly, Lymphadenopathy, Bone pain, Pallor – Rare Laboratory findings:
o (UK) Severity of Bleeding: No symptoms, Mild, Moderate and Severe o Microangiopathic hemolytic anemia (PBS: abnormal RBCs – schistocytes,
o 70-80% spontaneous remission w/in 6 months spherocytes, helmet cells)
o 10-25% develop chronic ITP o Reticulocytosis, Thrombocytopenia
Acute ITP (80%) – complete resolution of platelet CT in 6 months o Coagulation studies – non-diagnostic
Chronic ITP (20%) – persistence of thrombocytopenia > 12 months o BUN: creatinine – elevated
o Monitor for SLE (ANA) Treatment:
Lab findings: o Plasmapheresis
o Thrombocytopenia <20 x 109/L o Rituximab, Corticosteroids, Splenectomy (refractory)
o Platelet size – normal to large platelets
o Normal WBC, RBC
o BMA: increased megakaryocytes, normal granulocytes, Erythroid
Indications for bone marrow aspiration:
1. Abnormal WBC count or differential count
2. Unexplained anemia
3. Findings suggestive of BM disease
Coombs (+) = IT w/ AIHA = Evans Syndrome
In adolescents with new onset ITP, ANA test should be done to evaluate for SLE
Management:
o Major bleedings are rare if the platelet counts are >10,000
o Treatment goal for ITP is to get safe platelet levels and prevent bleeding
o American Society of Hematology hives the following guidelines for treatment of
ITP:
Don’t treat if: Platelet count >50,000 and patient is Asymptomatic
Consider treatment if: Platelet count >50,000 and there is mucus
membrane bleeding
Definitely treat if: Platelet count <50,000
IVIG or Glucocorticoid:
- Platelet counts <20,000/ul + Significant mucosal membrane bleeding
- Platelet counts <10,000/ul & Minor purpura
- Treatment: Corticosteroids, IVIG, anti-D, Rituximab, Monitoring of
platelet count
PEDIA: BLEEDING DISORDERS (Dr. Lucero) RMB x PRIMORIS Page 7 of 7
S-ar putea să vă placă și
- Browmans Capsule: Respiratory System: Mesophrenic DuctDocument2 paginiBrowmans Capsule: Respiratory System: Mesophrenic DuctLaurence RoiÎncă nu există evaluări
- Parts of A CellDocument1 paginăParts of A CellLaurence RoiÎncă nu există evaluări
- ImtDocument2 paginiImtLaurence RoiÎncă nu există evaluări
- Animal DiversityDocument2 paginiAnimal DiversityLaurence RoiÎncă nu există evaluări
- SynapseDocument3 paginiSynapseLaurence RoiÎncă nu există evaluări
- Animal DiversityDocument2 paginiAnimal DiversityLaurence RoiÎncă nu există evaluări
- Way of PhiloDocument1 paginăWay of PhiloLaurence RoiÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Barangay Anti-Smoking OrdinanceDocument4 paginiBarangay Anti-Smoking Ordinancejacquelyn samson100% (1)
- Med 1 Block 2 - Wet Lab NotesDocument36 paginiMed 1 Block 2 - Wet Lab NotesluckyÎncă nu există evaluări
- Phet Natural SelectionDocument6 paginiPhet Natural Selectionapi-315485944Încă nu există evaluări
- Colposcopic Findings Prepubertal Assessed For Sexual Abuse: Genital GirlsDocument5 paginiColposcopic Findings Prepubertal Assessed For Sexual Abuse: Genital GirlsSusi PuspitaÎncă nu există evaluări
- Alex Cox Death 911 Call TranscriptDocument10 paginiAlex Cox Death 911 Call Transcripttmiller696733% (3)
- The Concept of NeuropsychiatryDocument10 paginiThe Concept of NeuropsychiatryOscar Adrian Carmona NietoÎncă nu există evaluări
- Antihypertensive Drugs - Classification and SynthesisDocument14 paginiAntihypertensive Drugs - Classification and SynthesisCường NguyễnÎncă nu există evaluări
- Salivation PDFDocument5 paginiSalivation PDFmehdi mafakheri100% (1)
- Borderline Personality Disorder, Bipolar Disorder, Depression, Attention ... Narcissistic Personality Disorder, Diferential Diagnostic, KernbergDocument23 paginiBorderline Personality Disorder, Bipolar Disorder, Depression, Attention ... Narcissistic Personality Disorder, Diferential Diagnostic, KernbergjuaromerÎncă nu există evaluări
- The Race Myth (Excerpted)Document30 paginiThe Race Myth (Excerpted)Wayne Owen Richards100% (1)
- Protein Synthesis: The Protein-Making ProcessDocument21 paginiProtein Synthesis: The Protein-Making ProcessLanie De la Torre100% (1)
- Warehouse EssayDocument8 paginiWarehouse Essayafibojmbjifexj100% (2)
- Section 5 - Students WorksheetDocument4 paginiSection 5 - Students WorksheetEsraa AhmedÎncă nu există evaluări
- A 55-Year-Old Woman With Shock and Labile Blood PressureDocument11 paginiA 55-Year-Old Woman With Shock and Labile Blood PressureMr. LÎncă nu există evaluări
- GASTROINTESTINAL DRUGS FOR ULCERS AND REFLUXDocument11 paginiGASTROINTESTINAL DRUGS FOR ULCERS AND REFLUXRhealyn LegaspiÎncă nu există evaluări
- GugulipidDocument7 paginiGugulipidManish WadhwaniÎncă nu există evaluări
- Nutrition During InfancyDocument4 paginiNutrition During InfancyMaryHope100% (1)
- Pteridophytes MorphologyDocument79 paginiPteridophytes MorphologyBoopathiAyyanarMÎncă nu există evaluări
- Pain Scales and Assessment UnhasDocument93 paginiPain Scales and Assessment Unhashaphahap0% (1)
- 2020 Pickaway County Fair ReportDocument9 pagini2020 Pickaway County Fair ReportWSYX/WTTEÎncă nu există evaluări
- Nursing Care Plan Neonatal PneumoniaDocument2 paginiNursing Care Plan Neonatal Pneumoniaderic93% (41)
- Nur 097 Sas 1 3Document9 paginiNur 097 Sas 1 3gekkonoojiÎncă nu există evaluări
- Test-11 (Current Affair-2)Document86 paginiTest-11 (Current Affair-2)Pavansaikumar DasariÎncă nu există evaluări
- Rundown Iomu 071019 - 08.10 PDFDocument13 paginiRundown Iomu 071019 - 08.10 PDFEfi OctavianyÎncă nu există evaluări
- CHAPTER II Open BurningDocument6 paginiCHAPTER II Open Burningjedric_14100% (1)
- 5388 Tech ManualDocument198 pagini5388 Tech ManualMichal SzymanskiÎncă nu există evaluări
- FCA (SA) Part I Past PapersDocument72 paginiFCA (SA) Part I Past PapersmatentenÎncă nu există evaluări
- Yes, aside from the educational SMS intervention, the groups were treated equally as they both received routine trainingDocument54 paginiYes, aside from the educational SMS intervention, the groups were treated equally as they both received routine trainingYogiÎncă nu există evaluări
- CU DFScience Notes Bacteria General Dairy Micro 06 10 PDFDocument10 paginiCU DFScience Notes Bacteria General Dairy Micro 06 10 PDFjoel osortoÎncă nu există evaluări
- Basic Life Support Field GuideDocument56 paginiBasic Life Support Field GuidelmaoheartsÎncă nu există evaluări