Documente Academic
Documente Profesional
Documente Cultură
Critical Care Note PDF
Încărcat de
lml100%(1)100% au considerat acest document util (1 vot)
233 vizualizări10 paginiTitlu original
206039316-Critical-Care-Note.pdf
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
100%(1)100% au considerat acest document util (1 vot)
233 vizualizări10 paginiCritical Care Note PDF
Încărcat de
lmlDrepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 10
CARING FOR CRITICALLY ILL PATIENT Legal Relationships Nurses duty MYOCARDIAL INFARCTION (MI)
Nurse-employer Competent & able to
Role of a Critical Care Nurse follow policies and Definition:
Provide care direct to the patient. procedures. Irreversible myocardial necrosis due to sudden
Involve family members in patient’s care. Nurse-patient Give reasonable and decrease or total stop of coronary blood flow to a
Facilitate communication among healthcare careful care specific area of myocardium.
provider, patient, and family. Nurse-law Provide safe and
Provide appropriate intervention & actions. competent practice as Pathophysiology
Formulate patient care goals. defined by the standard Cholesterol deposited on
Ensure patient safety: artery wall forming plagues
Identify patient correctly and causes it to harden and
Patient Care Issues
narrows the lumen.
Improve communication among staffs. Consent must be voluntary and informed
Use medication safely. Person giving consent must be:
Prevent infection. Legally competent The plagues may rupture and
Identify patient safety risks Adult blood clot form on the surface of
Prevent mistakes in surgery. Mentally stable the plague.
Have capacity (reasoning)
ETHICAL & LEGAL ISSUES Patient can refuse treatment.
If patient is not for resuscitation, DNR order The clot blocks the blood
Autonomy should be documented by doctor. flow and causes MI.
Freedom to make decision without others The doctor should explain everything to the
interference. patient about diagnosis and treatment.
Critical care nurse act as patient advocate Oxygen delivery is affected and cause
before patient and family make decision: due to the thrombosis or spasm close
PATIENT & FAMILY EDUCATION
Provide information to the rupture plague
Clarify points Nurses responsibility
Reinforce information Assess patient & family learning needs. Clinical Manifestation
Provide support Education must be ongoing, interactive, and Chest pain squeezing in nature radiating to
consistent with the education level. left arm, jaw or upper back
Beneficence Reduce stress, anxiety, and fear first. Shortness of breath Nausea & vomiting
Promote wellbeing by considering harms and Focus on orientation of environment & Heartburn Sweating
benefits, leading to positive outcome. equipment, procedure explanation, and General malaise STEMI/ NSTEMI
immediate plan of care.
Non-maleficence Ensure patient is emotionally stable. Risk Factors
Prevent harm and correct harmful situation. Hyperlipidemia Diabetes
Learning Needs Smoking Male
Veracity Orientation of various care providers & Family history Obesity
Truth telling in information given. services available.
Important in requesting informed consent Orientation on environment (eg: call bell) Types of MI
because patient need to be aware about the Orientation on unit rutines and care plan
risks and benefits. (visiting hour, monitoring, daily weight) Anterior MI
Explanation on equipments, monitors &
•Occlusion of proximal left anterior
Fidelity associates alarms (eg: ventilator) descending artery
Requires loyalty, fairness, truthfulness, Explanation on procedures & expected
•ST-elevation in lead V1-V4
advocacy, and dedication outcomes.
•Most dangerous MI
Information on medication (name, indication,
Justice side effects) and reporting to nurse. Left Lateral MI
Refers to an equal and fair distribution of Immediate plan of care
resources, based on analysis of benefits and Transition to next level of care: transferring, •Occlusion of circumflex coronary artery
burdens of decision. staffs, environment •New Q waves & ST-elevation in leads I, aVL.
Discharge plan (medication, diet, activity) V 5, V 6
Elements in Code of Ethics Inferior MI
The professional code of ethics Successful Education
Values and relationship among members of the Attention •Occlusion of right coronary artery
profession and society. The information must be important to know. •Distiurb blood supply to SA & AV nodes,
The purpose of the profession Simple and Bundle of His (proximal part)
The need of profession to provide certain Use everyday language & avoid medical terms •High mortality if Rt ventricle affected.
duties formed between nursing and society Time
Right Ventricular MI
The standards of practice of the professional Be present when teaching.
Describe specifics of practice in variety of Reinforce •Occlusion of the proximal part of Rt
settings and subspecialties. Provide positive rewards to patient. coronary artery
•Can affect right ventricle and inferior wall
Steps in ethical decision making Special Consideration for:
Identify the health problem 1. Older adult Posterior MI
Define the ethical issue 2. Sedated or unconscious patient •Occlusion in Rt coronary artery or
Gather additional information 3. Illiterate patient circumflex artery
Outline the decision maker 4. Noncompliant patient •Tall R waves can be seen in leads V1, V2
Examine ethical & moral principles
Explore alternative options
Implement decisions
Evaluate & modify actions
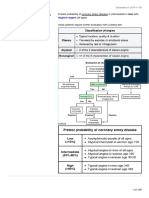
Diagnostic Test CORONARY ARTERY DISEASE (CAD) Types of Heart Failure
I. 12-lead ECG Left Ventricular Failure (LVF)
ST-segment (elevated/ not elevated) Definition: •Disturbance of contractility of left ventricle
If NSTEMI, necrosis is not full thickness Hardening of the coronary arteries, this may •Results in low CO, increase afterload &
Q wave present cause angina pectoris and lead to myocardial vascular resistance, and pulmonary edema
II. Cardiac enzyme or biomarkers infarction.
•Symptoms: Tachypnea, tachycardia, cough
CK-MB (rise 3-12 hrs, peak at 24 hrs,
Right Ventricular Failure (RVF)
remain elevated for 2-3 days) Clinical manifestation
•Disturbance of contractility of right
Trop-I (rise 3-12 hrs, peak at 24 hrs, remain Chest pain/discomfort at arms, jaw, neck
ventricle
elevated for 2-3 days) Shortness of breath Lightheaded
•Due to acute condition like pulmonary
Trop-T (rise 3-12 hrs, peak at 12-48 hrs, Sweating Nausea and vomiting
embolus and right ventricle infarction.
remain elevated 5-14 days)
•Symptoms: Peripheral edema, high CVP,
III. Chest X-ray Risk Factors weakness, jugular venous distention
Middle to old age Male Systolic Heart Failure
Treatment Family history Hyperlipidemia
a) Reopening of the coronary artery Obesity Hypertension •Abnormality of heart muscle that decrease
-Fibrinolytic therapy contractility during systolic & reduse
Smoking Diabetes
quantity of blood that can be pumped out.
-Percutaneous Catheter Intervention (PCI) Chronic Kidney disease Post-menopause
b)Anticoagulation •Symptoms: Dysnea, fluid overload,
exercise intolerance.
-IV Heparin bolus with fibrinolytic therapy
c) Pain control Diastolic Heart Failure
Types of angina
-SL Nitroglycerin 1 tab (0.04mg) every 5 mins •Abnormality in heart muscle making it
Stable Angina Unstable Angina
-IV Morphine 2-4mg unable to rest, stretch or fill during
• Cause by the same • Cause by change in diastolic.
-Non-coated Aspirin 162-325mg
precipitating pattern of stable •Ejection fraction may be normal or low.
-Oxygen therapy maintain >90%
factors each time angina
d)Dysrhythmias prevention Congestive Heart Failure
(eg: exercise)
-IV Amiodarone
• Pain reduce by rest • Pain need more •Determined by rapidity of syndrome
-Beta blocker reduce heart rate
and taking S/L GTN than rest & GTN. A develops, presents of compensatory
e) Glucose control mechanism & presence of fluid
medical
f) Prevention of ventricular remodelling accumulation.
emergency
-ACE inhibitor/ ARB reduce risk of heart failure •In acute, it is sudden onset with no
• Due to 75 blockage • Due to plague
of coronary artery. instability & can compensatory mechanism.
Complications of MI •In chronic HF, symptoms may be tolerable
cause MI
Related to electrical dysfunction with medication, diet & activity level.
New murmur
Bradycardia Management:
Bundle branch block Management: Medical
Heart block Accurate assessment of chest pain to Pulmonary Artery Catheter (PAC) to monitor
Related to contractility differentiate unstable & stable angina. left ventricle function
Heart failure Recognize myocardial ischemia by intensity of Administer diuretics & fluid restriction to
Pulmonary edema pain, vital signs, 12-lead ECG, and immediate prevent fluid overload.
Cardiogenic shock fibrinolytic & heparin administered or PCI are Serve Morphine to reduce anxiety &
performed to detect obstruction. facilitate peripheral dilatation
Nursing Management Relieve chest pain by giving oxygen,
Serve vasodilator (nitroglycerin) to reduce
Preventing complication nitroglycerin, analgesics, and aspirin.
preload & dilate coronary arteries.
-Manage and alleviate chest pain Maintain calm environment to reduce anxiety
Intra-aortic Balloon Pump (IABP) to support
-Assess and reduce anxiety Patient education:
inadequate CO and blood pressure.
-Monitor lab result (esp. K and Mg to prevent -Alert nurse for any chest pain or discomfort
Administer inotropic (dopamine) to increase
arrhythmia) -Avoid straining
contractility.
-Monitor ST-segment continuously -Risk factor modification
Administer ACEi to inhibit ventricular
-Monitor signs of arrhythmia -Identify signs & symptoms of angina
remodelling slows ventricular dilation.
-Monitor arterial oxygen saturation -Importance of medication
Administer Beta blocker (carvedilol) to
-Create plan for patient’s physical activity -When to call doctors/seek treatment
-Emotion & stress management reduce heart rate
-Assess signs of heart failure (pedal edema) Serve Digoxin to control Atrial Fibrillation
-Assess heart sound for new murmur. Permanent pacemaker
-Monitor patient for drug compliance HEART FAILURE
-Give stool softener to prevent straining.
Definition: Nursing
Patient education
-Eat variety of fruit and veggies, limit amount A condition in which the heart cannot pump Optimizing cardiopulmonary function
of fat & reduce salt intake. blood at a volume required to meet the body’s -Assess ECG for dysrhythmia due to Digoxin
-Stop smoking needs. toxicity and electrolyte imbalance.
-Do simple, regular exercise 20-30 mins a day -Assess respiration pattern & rate for
-Explain the medication’ Classification (based on symptoms & pt’s effort) pulmonary congestion
-Reduce anxiety by deep breathing. Class I Normal daily activity does not -Give oxygen if dyspnea
-Avoid sex for a few weeks. Consult the doctor. initiate symptoms. -Administer diuretic or vasodilator to reduce
Cardiac rehabilitation Class II Normal daily activity initiate preload and afterload
Phase I (admission till discharge)-inapatient symptoms, bit subside with rest. -Serve Morphine to decrease anxiety
Self care, exercise, diet, smoking Class III Minimal activity initiate symptoms. -Assist in intubation & mechanical
Phase II (After discharge and last for 4-8 weeks) No symptoms at rest. Ventilation
Level of activity, psychological, modify risk Class IV Any activity initiates symptoms -Daily weight in fluid management.
factors, and return to work. and also present at rest.
Phase III (Maintenance)- Follow-up.
Promote comfort and emotional support Clinical Manifestation: Tricuspid Valve Regurgitation
-Restrict activity and assist ADL during SOB Dyspnea Fatigue
-Put patient on bed rest Palpitation Orthopnea Definition:
-Prop up the bed for maximal lung expansion Paroxysmal nocturnal Pulmonary venous Backflow of blood from right ventricle into right
-Document signs of activity intolerance such dyspnea hypertension atrium during systole.
as dysnea, fatigue & tachycardia.
Monitor effects of pharmacological therapy Diagnostic test: Diagnostic test:
-Know the action, side effect & toxic level I. Chest X-ray: Left atrial enlargement and I. ECG: Incomplete right BBB
-Monitor hemodynamic status closely cardiomegaly II. Chest X-ray: Cardiomegaly
-Document correctly intake & output II. ECHO III. ECHO: Identify the presence & severity
Provide adequate nutritional intake
-Monitor closely for nausea & low appetite Treatment Treatment:
-Encourage small, frequent meal Acute Chronic Tricuspid valve annuloplasty
-Advice family members to provide tasty food IV Nitropruside to Medication to delay Tricuspid valve replacement.
from home which compatible with condition. reduce afterload surgery or
Provide patient education IV Nitroglycerin to preventing left Pulmonic Valve Disease
-Assess understanding of the disease & risk reduce pulmonary ventricular
factors of heart failure. pressures dysfunction Definition:
-Educate the importance of diet restriction Assess ventricular Stenosis- Narrowing of the pulmonic valve orifice
IABP to stabilize
-Educate importance of daily weight, fluid size, function & Regurgitation- Backflow of blood from pulmonary
vital signs
restriction & medication to control symptom severity every 6-12 artery into the right ventricle
Mitral valve repair/
-Educate importance of lifestyle changes like replacement month by ECHO.
smoking, weight loss & exercise Diagnostic test:
-Inform when to call or seek treatment I. ECG: Incomplete right BBB
Aortic Valve Stenosis
II. Chest X-ray: Prominent pulmonary artery
VALVULAR HEART DISEASE III. ECHO: Identify right ventricular hypertrophy
Definition:
IV. Catheterization: Comfirm the diagnosis
Narrowing of aortic valve orifice which impedes
Definition: the blood flow from heart to body.
Several disorders and diseases of the heart CARDIOMYOPATHY
valves, which are the tissue flaps that regulate Diagnostic test:
the flow of blood through the chambers of the Definition:
I. ECG: Abnormal pattern reflecting thickening
heart. A disease of heart muscle & associated with
of heart muscle
ventricular dysfunction.
II. Chest X-ray: Dilation of aorta above the valve
Mitral Valve Stenosis III. ECHO: Diagnose & evaluate the severity
Hypertropic Obstructive Cardiomyopathy
Definition: Treatment:
2
Narrowing of mitral valve orifice (<2cm ). The Definition:
Restriction from activity
thickened, calcified valve cannot open or close Excessive myocardial hypertrophy which the
6-12 month evaluation by ECHO to indicate
passively, obstructing flow of blood from left heart able to contract but unable to relax and
aortic valve replacement.
atrium to left ventricle. remain stiff in diastole.
Antibiotic prophylaxis given to avoid
endocarditis.
Clinical Manifestation Clinical manifestation:
Diuretics
Dyspnea Fatigue Supraventricular Ventricular
Chest pain Atrial Fibrillation tachycardia (SVT) Tachycardia (VT)
Aortic Valve Regurgitation
Syncope Shortness of breath
Diagnostic test: Fatigue Atrial Fibrillation
Definition:
I. Chest X-ray: Pulmonary congestion, Backflow of blood into the left ventricle during
enlargement of main arteries & Lt atrium. ventricular diastole. Diagnostic test:
II. ECG: Atrial fibrillation 1. Physical examination
III. ECHO: Valve leaflet thickening & restricted Treatment: 2. Chest X-ray
opening 3. ECHO
Aortic valve replacement
IV. Cardiac catheterization 4. Genetic testing
Tricuspid Valve Stenosis
Treatment: Treatment:
Diuretics & sodium restriction Definition: Beta blockers to reduce heart rate
Anti-arrhythmia to treat atrial fibrillation Narrowing of the tricuspid valve orifice results in Anti-arrhythmia
Anticoagulant to prevent thromboembolism increase pressure in right ventricle. Anti-coagulant
Beta blockers/CCB/digoxin to control HR Activity restriction to reduce sudden death
Antibiotic for prophylaxis of rheumatic fever Diagnostic test: Implantable cardioverter defibrillator
Percutaneous Balloon Vulvotomy I. ECG: Tall P wave in sinus rhythm Myectomy to improve blood flow from heart.
Mitral commissurotomy II. ECHO: To identify the presence & severity.
Mitral valve replacement Dilated Cardiomyopathy
Treatment:
Mitral Valve Regurgitation Sodium restriction Definition:
Diuretics Characterized as dilation of both ventricles
Definition: Tricuspid Valve Replacement without muscle hypertrophy.
Backflow of blood in left atrium with each
ventricular contraction due to rupture of chordae Types:
tendinae/ papillary muscle (emergency) or Ischemic Repeated MI/ myocardial injury
dilatation of left atrium to maintain CO. Familial Idiopathic /genetic
Clinical Manifestation: Monitoring: ELECTROCARDIOGRAM (ECG)
Low cardiac output Dyspnea Non invasive Invasive
Fatigue Orthopnea Consciousness level CO- Arterial line/ CVP 12 lead ECG consist of:
Liver enlargement Syncope Vital signs Ventilator a) 6 limb leads (I, II, III, aVR, aVL, aVF)
Oxygenation Urine output b) 6 chest leads (V1-V6)
Restrictive Cardiomyopathy Infection signs Arterial Blood Gases c) Standard speed of 25mm/second
Urine output Blood results d) Small box = 0.04 sec = 1 mm
Definition: Skin turgor ECHO/ TOE e) Large box = 0.20 sec = 5 mm
Characterized as ventricular wall rigidity due to Peripheral perfusion
myocardium scarring.
Treatment:
Clinical manifestation: Restoring blood volume and ensure
Shortness of Breath Edema oxygenation and blood pressure adequate.
Palpitation Disrhythmia -Normal Saline
-Hartmann Solution Crystalloids
Diagnostic test: -Dextrose solution
+ Physical examination -Albumin
+ ECG -Polygeline
-Gelatin Colloids
+ ECHO
+ MRI -Hetastarch
-Blood products
Treatment: Airway managed & initiate oxygen therapy
P wave Atrial contraction 0.08-0.10 sec
Diuretics Vasopressant to induce vasoconstriction
QRS Ventricular 0.06-0.10 sec
ACE inhibitor Use anti-shock trousers to concentrate blood complex contraction
Exercise restriction in vital organs (lungs, brain, heart)
T wave Ventricular relax -
Keep patient warm
PR AV node function 0.12-0.20 sec
SHOCK Antibiotics to prevent sepsis interval
Adrenaline to stimulate cardiac performance
Definition: Corticosteroid to reduce inflammation ST segment
A serious, life threatening medical condition Trendelenburg position to shunt blood back Measured from end of QRS complex to
where there is insufficient blood flow to meet to body’s core beginning of T wave.
tissues demand. Chest tube to treat pneumo/hemothorax Evaluate base on shape & location
Thrombolysis to reduce size of clot. Normally flat/isoelectric level
Stages of shock Pericardiocentesis to treat tamponade
Initial 1 mm above Myocardial ischemia
CARDIAC TAMPONADE 2 mm above Myocardial infarction/
•Hyperperfusion causes hypoxia. pericarditis
•Cellsperform anaerobic respiration leading Definition: 1 mm below Myocardial ischemia
to lactate & pyruvate build up causing Sudden accumulation of blood, fluid, clots, pus or
metabolic acidosis. gas in pericardial space resulting in compression QT interval
Compensatory of heart muscle & interfere systole & diastole. Indicates total time from onset of contraction
to relaxation.
•Hyerventilate to clear CO2 and improve pH. Clinical Manifestation: Shorten with fast HR, lengthen in slow HR
•Baroreceptors detect hypotension due to Tachycardia Difficulty in breathing Normal: <46 sec (women), <0.45 sec (male)
vasodilatation Hypotension Jugular vein distension Prolong indicates torsades de pointes,
•Adrenaline is released to increase BP. Shock Oliguria electrolyte imbalance, dysrhythmic treatment
•Renin-angitensin axis is activated and Restlessness Dyspnea
vasopresssin released to conserve fluid via Reading ECG
kidneys reducing urine output. Risk Factors: 1. P wave presence and have relation with QRS.
•Vessels in other organ also constrict to Blunt/ penetrating cardiac trauma 2. PR interval duration
divert blood to heart, lungs & kidneys. Post cardiac catheterization 3. QRS complex shape, width & duration
Anticoagulant therapy 4. QT segment length
Progressive (decompensating)
Myocardial Infarction 5. ST segment elevation.
•Vessel constriction causes blood remain in Acute pericarditis
capillaries. Methods in calculating heart rate
•Hydrostatic pressure increase and Management: i. No. of R-R intervals in 6 sec times 10
histamine released cause leakage of fluid Pericardiocentesis (Irregular rhythm)
and protein into surrounding tissue. -Aspirate fluid from pericardial by needle ii. No. of large boxes between QRS complex
•Blood concentration increase causing Subxiphoid pericardiostomy divided into 300
sludging of microcirculation. -Drain pericardial sac iii. No. of small boxes between QRS complex
•Vital organ compromised due to reduced Emergency thoracotomy divided into 1500
perfusion. -Pericardial sac evacuation
Fluid resuscitation *If HR>200 bpm or <30 bpm, emergency
Refractory
-Blood products, colloids, crystalloids measures are taken.
•Vital organ failed and brain death occured. Inotropic agent
•Death will occur imminently. -Increase myocardial contractility and CO
Airway
-Oxygen, intubation, mechanical ventilation
HEMODYNAMIC MONITORING ACUTE LUNG INJURY (ALI) PNEUMONIA
Definition: Definition: Definition:
Is the bedside measurement of the ever-changing A systemic process of pulmonary manifestation Acute inflammation of the lung parenchyma
pressure of blood flow through the cardiac, which cause multiple organ dysfunction
pulmonary & systemic vasculature via invasive syndromes. Severe ALI is known as Acute Community Acquired Hospital Acquired
catheters. Respiratory Distress Syndrome (ARDS). Pneumonia (CAP) Penumonia (HAP)
Pathogens Pathogens
Benefits: Clinical Manifestation: -Strep. Pneumoniae -Staph. Aureus
Improve patient outcome Exudative phase Fibroproliferative -Legionella sp. -Strep. Pneumoniae
Lower mortality rates phase -H. Influenzae -Pseudomonas
Better quality of life after critical illness * Tachypnea * Agitation -Staph. Aureus -Aceno. Baumannii
* Restlessness * Dyspnea -Mycoplasma pneu. -Klesiella sp.
Measurement: * Anxiety * Fatigue -Clamydia pneu. -Proteus sp.
Direct Indirect (calculation) * Use accessory * Use accessory -Pseudomonas -Serratia sp.
CVP Cardiac output muscles muscle excessively Risk factors Risk factors
Rt Ventricle Pressure Cardiac Index * Fine crackles Alcoholism Elderly
Pulmonary Artery P. Lt Ventricular COPD COPD
Ejection Fraction Risk factors: Diabetes Chronic illness
Lt Atrial Pressure Direct Indirect Malignancy Mecha. ventilation
Capillary Wedge P. Aspiration Sepsis Coronary disease Smoking
Drowning Trauma
Tools: Toxic inhalation Hypertransfusion Clinical manifestation:
Intra-Arterial Purpose Pulmonary CABG Dyspnea Uremia
Catheters (IAC) Measure MAP correctly contusion Severe pancreatitis Fever Thrombocytopenia
Draw blood for ABG Pneumonia Embolism Cough Hypoxemia
Monitor Arterial BP Oxygen toxicity Shock Coarse crackles Tachypnea
Insertion site Pathophysiology Diagnostic test
* Radial artery a. Chest X-ray
After direct/ indirect injury, inflammatory-
* Femoral artery b. Sputum culture
immune system is stimulated
* Dorsalis pedis c. Bronchoscopy
* Brachial artery Inflammatory mediators released from the d. Full Blood Count
* Axillary artery site e. Arterial Blood Gases
Central Venous Purpose
Access When peripheral site Causes neutrophils, macrophages & platelet Nursing management:
nor accessible accumulate in pulmonary artery. i. Optimize oxygenation & ventilation
Insertion site For fluid resuscitation -Oxygen therapy
Initiate humoral mediators that damage
* Subclavian vein CVP monitoring -Positioning
alveolar-capillary mambrane.
* Brachial vein Access for PAC -Secretion clearance
Jugular vein Monitor blood Alveolar collapse and cause increase work of -Bronchodilators
circulation breathing ii. Prevent infection spreading
Pulmonary Artery Purpose -Proper hand washing
Catheter (PAC) Measure pressure in -Administer antibiotic
Hypoxemia
both side of heart & iii. Provide comfort & emotional support
Insertion site pulmonary artery -Adequate rest
* Subclavian vein Measure CO Diagnostic test: -Perform procedures as needed
* Jugular vein Blood for mixed venous I. Arterial Blood Gases (ABG) -Explanation on procedures
* Femoral vein Fluid infusion -↓ PaCO2: Despite high oxygen demand iv. Prevent complications
* Brachial vein -↑ PaCO2: Hyperventilation, fatigue -Close monitoring
Nursing intervention -↓ pH: Respiratory acidosis -Aseptic technique
th
Tranducer at 4 ICS II. Chest X-ray
Zero transducer b4 PULMONARY EMBOLISM
read Management:
Supine/ Semi-fowlers Medical Nursing Definition:
Intra-aortic Purpose Mecha. Ventilation Optimizing Occurs when thrombotic embolus (clots) or non-
Balloon Pump Support in low CO & BP Low tidal volume oxygenation & embolus (fat, air, foreign bodies) stuck into the
(IABP) Post CABG (6ml/kg)- prevent ventilation pulmonary arterial system, disrupting blood flow
Barotrauma Preventing to the lungs.
Insertion site Signs of complications Pemissive desaturation Pathophysiology
* Femoral artery ↓ Peripheral pulses hypercapnia Promote When occluded, alveolar dead space ↑
↓ Urine output Increase CO2 secretion
Balloon migration slowly clearance ↑ work of breathing
↑ temperature/ WBC Oxygen therapy Positioning
↓ Hematocrit (bleed) Tissue perfusion Provide comfort & Hypercapnia & hypoxia causes
Adequate CO emotional support bronchoconstriction
Weaning: ↑ contractility Prevent
complications ↑ pulmonary vascular resistance
Hemodynamic stable Restrict fluid
No chest pain Diuretics ↑ right ventricular workload
Adequate urine output
Clinical manifestation: BASIC AIRWAY MANAGEMENT MECHANICAL VENTILATION
Tachycardia Hemoptysis
Tachypnea Cough Oxygen administration: Definition:
Dyspnea Crackles Types Amount/percentage A mode of assisted or controlled ventilation using
Anxiety Fever Nasal cannula 2-6 Lpm/25-50% mechanical devices that cycle automatically to
Face mask 6-10 Lpm/ 35-60% generate airway pressure.
Risk factors: Partial rebreather >10 Lpm/ >60%
Venous stasis (AF,↓ CO, immobility) Non rebreather >10Lpm/ 60-95% Types:
Injury to vessels (infection, incision) Demand valve 100 Lpm/ 100% i. Volume-cycled: Preset tidal volume
Polycythemia Venturi mask With reservoir 50% ii. Pressure-cycled: Preset pressure limit
Cardivascular disease (HF, cardiomyopathy) (15 Lpm) No reservoir >95% iii. Flow-cycled: Preset flow rate
Cancer iv. Time-cycled: Preset time factor
Trauma Intubation
Pregnancy Techniques Modes:
Head tilt, chin lift: Tongue may obstruct
Diagnostic test: Jaw thrust: For spinal injury patient Control Ventilation (CV)
Arterial Blood Gases (↓ PaCO2, ↓PaO2, ↑ pH) Body position
ECG (sinus tachycardia, BBB, AF) •Deliver preset volume/pressure despite own
Lateral position allow fluid drain out inspiratory effort
Chest X-ray (cardiomegaly, pleural effusion) Used when no spinal injury
Pulmonary angiogram •Used for apneic patient
If so, patient secured on a board first.
DVT studies
Airway adjunct Assist-Control Ventilation (ACV)
Oropharyngeal:
Management:
-For unconscious patient •Deliver breath in response to own effort &
Medical Nursing
-Measure from mouth to angle of when fail to breathe.
~ Fibrinolytic agents ~ Optimize ventilation
mandible •Used in spontaneous breathing with weaken
(streptokinase) & oxygenation
Nasopharygeal: respiratory muscle
~ Embolectomy ~ Monitor bleeding
-For conscious patient Synchronize Intermitten Mandatory
~ Anticoagulant ~ Provide comfort
-When oropharungeal airway not Ventilation (SIMV)
(heparin or warfarin) ~ Prevent
accessible
~ Inotropes complications •Ventilator breath are synchronize with own
-Measure from tip of nose to end of
~ Fluid ~ Health education effort
earlobe
Laryngeal mask: •Used in weaning from ventilation
PNEUMOTHORAX
-For unconscious patient
Pressure Support Ventilation (PSV)
-Not suitable if esophagus is injured
Definition:
-Must be remove after patient conscious
Accumulation of air between the parietal & •Preset pressure that augment own
-Does not prevent aspiration inspiratory effort & decrease work of
visceral pleura with lung collapse.
Tracheostomy: breathing
-For prolong ventilation •Used in weaning with SIMV mode
Types:
-When patient fail to be intubated
Spontaneous -Done in OT Positive End Expiratory Pressure (PEEP)
•A closed pneumothorax (no leak)
•Causes: Rupture of visceral layer due to Complications of intubation:
infection (primary), disease complication Laceration of gum, lip, vocal cord, pharynx •Used with CV, AC & SIMV to improve
(secondary) Broken teeth oxygenation by opening collapse alveoli.
•Symptoms happen during rest Vocal cord paralysis
Pneumothorax Constant Positive Airway Pressure (CPAP)
Traumatic
Esophageal intubation
•Can be opened (opening in chest wall) or ETT dislodgement •Similar to PEEP but used only with
closed spontaneously breathing patient.
•Causes: Penetrating injury (biopsy, Suctioning: •Maintain constant +ve pressure in airways.
thoracocentesis), fracture, PEEP, CPR Hyperventilate patient or apply high-
Independent Lung Ventilation (ILV)
Tension concentration of oxygen before suction
Use sterile apparatus
•Air enter pleura space when inhale and •Ventilate each lung separately. Requires 2
Maximum of 10 sec on each suction ventilator and sedation.
cannot escape because of flap-valve effect.
Be gentle
Life- threatening (↓ CO) •Used in unilateral lung disease/ different
Rotate the catheter when withdrawing it. disease process in each lung
•Causes: Trauma, infection, mechanical
Apply aseptic technique
ventilation
Use soft, flexible catheters High Frequency Ventilation (HFV)
Monitor for arrhythmia
Management:
Attach oxygen after suction •Deliver small gas amount at rapid rate (60-
1. Oxygen therapy
100 bpm). Require sedation
2. Analgesics
•Used in hemodynamic instability, in short-
3. Thoracocentesis
term procedure or risk of pneumothorax.
4. Chest tube
5. Thoracotomy- prevent recurrent Inverse Ratio Ventilation (IRV)
•I:E ratio reversed to allow longer inspiration.
Require sedation.
•Improve oxygenation in hypoxic patient with
PEEP. Keeps alveoli from collapse.
Settings: Physiological NON INVASIVE VENTILATION
Ventilator Modes used in delivering A. Respiratory
Modes positive pressure. -Barotrauma Definition:
Respiratory Number of breath ventilator -Atelectasis Delivery of mechanical ventilation with a nasal or
Rate delivers per minute -Infection (VAP) face mask.
(10-12/min) B. Cardiovascular
Tidal Volume delivered to patient -Decrease venous return and CO Advantages:
Volume during normal ventilator C. Gastrointestinal Prevent intubation
breath (7-10 ml/kg). Volume -Gastric ulceration Enhance alveolar ventilation
>10 ml/kg cause volutrauma. -Microaspiration ↓ work of breathing
Inspiratory A measure of preset D. Renal/ hepatic Improve gaseous exchange
flow respiratory volume: the more -Decrease urine output ↓ nosocomial infection
quantity of a flow, the more -Sodium & water retention Enhance patient comfort
quickly ventilator will submit -Decrease portal blood flow ↓ length of stay
mandatory respiratory volume E. Central Nervous System ↓ cost
(45-60 L/min) -Decrease cerebral perfusion following
excessive PEEP Indication
I:E ratio Ratio comparing time
AECOPD & respiratory failure
delivering O2 and time to
Drugs used in managing ventilated patient: Respiratory failure with hypercapnia
exhale (1:2).
a) Sedative/ analgesics Respiratory failure with acute hypoxemia
PEEP Positive pressure applied at
-Midazolam Asthma
end of expiration (3-5 cm H2O)
FiO2 Select delivery of O2 (21- -Morphine
-Propofol Methods:
100%). Should be the lowest 1. Continuous Positive Airway Pressure (CPAP)
level to prevent oxygen b) Neuromuscular Blocking Agent (NMBA)
-Suxamethonium o Air delivered via mask fit to patient’s face
toxicity. o Pump provide positive pressure
-Vecuronium
Inspiratory A control that adjust ventilator o Increase amount of air breathed in
-Atracurium
trigger response to patient o Not increase work of breathing
respiratory. o Patient breathe spontaneously
Care of Patient on Mechanical Ventilator
Check ventilator settings according to doctor’s o Usual range 5-15 cmH20
Criteria for starting mechanical ventilation: 2. Bilevel Positive Airway Pressure (BiPAP)
order every shift
i. Respiratory rate >35 or <5 breaths/minute o Provide higher positive pressure for
Make sure alarm are set
ii. Hypoxia: central cyanosis inspiration
Empty ventilator tubing when moisture collects.
iii. Hypercapnia o Enhance oxygenation & ventilation
Never empty the fluid back into the cascade
iv. Decreasing conscious level o Higher pressure is for inhalation (IPAP),
Ensure temperature of delivered air maintained
v. Significant chest trauma lower pressure for expiration (EPAP)
at body temperature
vi. Tidal volume <5ml/kg o When inhale, air flow in high pressure to
If on PEEP, observe peak airway pressure to
vii. Control ICP in head injury support inhalation.
determine the proper level
viii. Following cardiac arrest o Increase delivery of air with less breathing
Assess patient’s respiratory status every shift:
ix. Prolong major surgery workload.
Take vital signs 4 hourly
Check cuff pressure everyday to ensure tidal
Definition of weaning: Nursing management
volume
Gradual withdrawal of the mechanical ventilator Claustrophobia Assess for comfort
Provide mouth care every 2-4 hours
& reestablishment of spontaneous breathing Serve anxiolytic
Observe the need for suction every 2 hours
Provide tracheostomy care every shift. Pressure on Place hydrocolloid dressing
Criteria for weaning: face
Change tube tape as needed
a. Respiratory rate <25 per min Mucosal Apply lip balm or nasal
Check mouth for pressure sores.
b. Tidal volume 3-5 ml/kg dryness spray
Move the tube to opposite side of mouth every
c. pH >7.35 Stomach Insert nasogastric tube
24 hour to prevent ulcers
d. PaO2 >80 mmHg with FiO2 <0.5 distension
Maintain accurate intake & output records
e. PaCO2 35-45 mmHg Aspiration Check for nausea, abdo
Position patient every 2 hours to prevent
complication of immobility girth
Factors to consider before weaning Serve antiemetic
Plan nursing care to provide rest
-Resolution of underlying pathologic condition Corneal Ensure mask fit well
Include patient & family members in care
-Chest X-ray show good lung expansion irritation Apply eye drop
Provide materials for communication
-Acceptable ABG with ventilator support Hypoventilate Ensure mask fit well
Observe for gastrointestinal distress
-Sepsis under control
Administer medication as appropriate
-Awake with intact respiratory drive
Initiate relaxation technique
-Minimal inotropic support ARTERIAL BLOOD GASES (ABG)
Monitor for complication (barotraumas, ↓ CO)
-Good hydration with normal serum electrolyte
Monitor readiness to wean.
-Adequate nutrition & energy Interpreting ABG
-Intact gag & cough reflex before extubation 1. Partial pressure of Oxygen (PaO2)
2. pH level
Complications: 3. Partial pressure of Carbon Dioxide (PaCO2)
Mechanical- Equipment malfunction 4. Bicarbonate (HCO3)
a) Ventilator
Fail to cycle, Power failure
b) Circuit
Disconnection, Infection
c) Humidifier
Inadequate humidification, overheating
Estimation of burn size DIABETIC KETOACIDOSIS (DKA)
Disorder pH PaCO2 HCO3 I. Rule of nine
mmHg mEq/L Divides body part into 9% of TBSA each Definition:
Respiratory acidosis II. Lund & Browder chart A metabolic state resulting from a profound lack
Uncompensated < 7.35 > 45 normal Surface area is based on age of insulin, usually found in type I DM. Inability to
Partially < 7.35 > 45 > 26 III. Palmar method inhibit glucose production from the liver results
Compensated normal > 45 > 26 Use patient own hand, representing 11% of in hyperglycemia, which can be extreme and lead
Respiratory alkalosis TBSA to severe dehydration.
Uncompensated > 7.45 < 35 normal
Partially > 7.45 < 35 < 22 Degree of burns Pathophysiology
st
Compensated normal < 35 < 22 1 degree -Superficial burn Hyperglycemia (absolute deficit in
Metabolic acidosis -Causes pain, redness, swelling insulin)
Uncompensated < 7.35 normal < 22 -Heal within 3-5 days
nd
Partially < 7.35 < 35 < 22 2 degree -Partial thickness burn Inability of glucose to move into cells,
Compensated normal < 35 < 22 -Causes pain, swelling, blister increasing its level
Metabolic alkalosis -Heal within 10-14 days
Uncompensated > 7.45 normal > 26 rd
3 degree -Full thickness burn Fat from adipose tissue converted into
Partially > 7.45 > 45 > 26 -Causes black,char skin, numb free fatty acids (FFA)
Compensated normal > 45 > 26 -Heal within 30 days-months
Mixed
Alkalosis < 7.35 > 45 < 22 FFA converted to
Diagnosis test: glucose by liver
Acidosis > 7.45 < 35 > 26 Arterial Blood Gases
Carboxy Hb level
Causes: Coagulation studies Liver also convert
Respiratory ~ Fever Group Cross Match (GXM) glycogen into glucose
alkalosis ~ Trauma Urine analysis
~ CNS infection Worsen the
~ High altitude Management: hyperglycemia
~ Pneumothorax a) Resuscitative phase
~ Pregnancy -Adult (> 15%), children (>10%) Clinical Manifestations:
Respiratory ~ Airway obstruction -Fluid resuscitation (Ringer’s Lactate): Hyperglycemia Coma
acidosis ~ Pulmonary edema Parkland’s Formula ↑ ketone level Shortness of breath
~ Pneumonia (4 x BSA involved x body weight) Polydipsia Weakness
st
~ CNS depression -50% given in 1 8 hours, 50% nest 16 hours Polyuria Weight loss
~ Neuromuscular impairment b) Acute phase Polyphagia Abdominal pain
Metabolic ~ Volume depletion -Wound care Nausea & vomiting Dehydration
alkalosis ~ Bicarb administration -Open dressing: Apply topical agent with gauze
~ Diuretics -Close dressing: Use gauze to cover after apply Complication:
Metabolic ~ Diarrhea topical agents 1) Cerebral edema
acidosis ~ Renal insufficiency -Apply topical antimicrobial (Silver nitrate) -Brain swell due to water accumulation
~ Rapid saline administration c) Rehabilitation phase 2) Acute kidney failure
~ Starvation -Physiotherapy -Caused by severe dehydration
~ DKA -Psychiatry 3) Acute Respiratory Distress Syndrome
~ Lactic acidosis -Social worker -Lungs filled with fluid causing SOB
4) Hypoglycemia
BURNS Nursing care: -Insulin enter into cells and ↓ glucose level
Strict intake & output chart 5) Hypokalemia
Definition: Vital signs monitoring -Due to fluid & insulin used in treating DKA
Tissue damage caused by such agents as heat, Pain assessment, administer analgesics
chemicals, electricity, UV light or nuclear Nutrition (high protein, enteral feeding) HYPERGLYCEMIA HYPEROSMOLAR NON-
radiation. Leading cause of death is infection. KETOACIDOSIS SYNDROME (HHNS)
Types Causes Definition:
Thermal Hot water, flammable liquid, Hyperosmolarity & severe hyperglycemia
explosion, fire predominate with change of mental status due to
Electrical Massive electrical current insulin resistance. Occurs in type II DM.
Chemical Strong acid/ alkali, mustard gas
Radiation Exposure to UV light Pathophysiology
Classification of burn Deficit in insulin prevent glucose enter cells
Major 25% of TBSA
10% of TBSA full-thickness burn Glucose level ↑ & blood become
Deep burn (head, perineum) hyperosmolar
Inhalational injury
Chemical/high voltage burn Fluid drawn from the cell into vascular bed
Moderate 15-25% of TBSA Body try to eliminate excessive glucose by
Superficial partial thickness burn urinating
(head, perineum, limbs)
Suspected child abuse If patient do not consume enough water, it
Concomitant trauma may results in severe dehydration
Minor 15% of TBSA
Clinical manifestations: Brain * Hyperventilate TRAUMA CARE IN EMERGENCY
Hyperglycemia Polyuria herniation * Mannitol
Dehydration Weakness * Immediate CT brain Triaging
Excessive thirst Weight loss * Contact neurosurgeon Categorising the patient according to
Confusion Fatigue Thoracic * Adequate pain control treatment priority.
trauma * Adequate oxygenation A 24 hour basis by well trained Triage
Risk factors: * Chest wall stabilization Officers.
A. Poor DM control * Treat complication Triage criteria:
B. Non compliant to DM treatment Pneumothorax * Chest tube insertion Non-critical Walk-in & stable
C. Drink inadequate water * Needle thoracostomy Semi-critical Hemodynamically stable
D. Intravenous feeding- ↑ glucose * High flow oxygen but unable to walk
E. Peritoneal dialysis * Asherman chest seal Critical Critically ill, require
F. Diuretics Massive * Tube thoracostomy immediate treatment.
hemothorax drainage
Complication: * Thoracotomy Zone & facilities:
1) Shock * Adequate fluid volume Resuscitation Resuscitation bays
2) Coma Cardiac * Pericardiocentesis zone -Emergency treatment
3) Acute tubular necrosis temponade “golden hour”
4) Vascular thrombosis Aortic rupture * Maintain adequate volume -Activation of trauma team
5) Death * Angiogram Critical care bays
* Emergency endovascular -Observation & monitoring
Management for DKA and HHNS: stent graph Immediate Immediate bays
Medical Nursing Renal injury * CRIB Care zone -Active bays for incoming
* Fluid resuscitation * Administer fluid, * Sedation semicritical
* Administer insulin insulin, electrolyte * Observation (abd, girth) Observation bays
* Restore electrolyte * Monitor compliant * IV fluid (major injury) -Observation for semi-
* Patent airway to therapy * Antibiotic critical cases
* Enough ventilation * Prevent * Full laparotomy
-Duration stay <12 hours
& oxygenation complications GI injury * Debride devitalized tissue
Green zone Consultation room
* Close monitoring * Patient education * Anastomoses if required
-Minor treatment prior to be
* NGT suction
discharge
Patient education for DKA & HHNS: * IV fluids
-Eg: injection, dressing
a. Control blood sugar Pancreatic * External drainage
Asthma bay No waiting time
b. Consult doctor for blood sugar level target injury * Control hemorrhage
Liver injury * Close monitoring Emergency treatment
c. Drink a lot of water
* Blood transfusion One Stop Victims of domestic violence,
d. Take medication as ordered
* Laparotomy Crisis Centre rape, child abuse
e. Watch for signs & symptoms- Ketone in urine
Spleen injury * Close monitoring (OSCC) Registration done in the
* Assess for bleeding room by emergency staff
Comparison between DKA & HHNS
DKA HHNS * Splenectomy
Vertical Shear * Apply compression belt/ Stabilization & transport of critically ill patient:
In type I DM In type II DM
external fixator Indication Contraindication
Sudden onset Slow onset
* Peritoneal aspiration Diagnostic purpose Increase potential
↑ ketone level Normal level * Urine catheterization Therapeutic risk
Serum sodium low Serum sodium high * Suprapubic cystotomy purpose (surgery) Unstable/potential
Low bicarb level Normal level * Bed rest Specialized care patient
Urine ketone present No urine ketone Acetabular * Traction (ED to ICU)
fracture * Reduce dislocation
POLYTRAUMA * Operative reduction (if fail) Potential mishap:
Pelvic fracture * Massive fluid replacement Accidental extubation
Definition: * Immobilization Ventilator disconnect
Consecutive systemic reactions which may lead * Bleeding control ECG disconnect
to dysfunction or failure of remote organs and Fat embolism * Adequate oxygenation Monitor power failure
vital systems. * Stabilizing hemodynamic Vaso-active drug interruption
* DVT prophylaxis IV infiltration or disconnection
Trauma death: Second death peak occurs within * Early immobilization
minutes to several hours after injury. This period * Use corticosteroid & Elements:
is called “Golden Hour” characterized by: heparin reduce APO i. Communication
-Rapid transportation Hypothermia * Cover with warm blanket - Reason for transport
-Rapid assessment& stabilization * Warm IV fluid before infuse -Patient’s condition
-Rapid definitive care Shock * Oxygenation -Equipment needed
* Arrest bleeding -Notify receiving department before transfer
Conditions & its management: * Pneumatic antishock
Head injury * Airway, breathing, garment
circulation * Monitor vital signs, I/O,
* Neurological assessment; CVP, acid-base balance
GCS * Blood tranfusion
Obtain CT brain if comatose,
unequal pupils, GCS <13/15
ii. Equipments Muscle relaxant/paralytics
-Small size, light Indication For intubation
-Compatible In mechanical
-Safe to staff and patient ventilation
Monitors -Know how to operate Prevent increase in ICP
-Monitors ECG, ABP, ICP, Reduce lactic acidosis
SpO2, capnograph Common drugs
Ventilators -Different modes Depolarizing Eg: Succinylcholine
-High & low pressure alarms agents
-Electrically powered Non- Eg: Pancuronium,
-Have humidification system depolarizing Vecuronium, Atracurium
-Oxygen supply, backup
Medication -List of drugs to be used Vasopressors
& infusion -Aware of drug effects Indication Increase contraction (β1)
-Use plastic infusion bag Vasodilate vessels (β2)
-Test IV drip before infuse Bronchodilate (β2)
iii. Monitoring Vasoconstrict (α)
-Pulse, SpO2, BP, RR Common drugs
iv. Handling over (documentation) Dopamine + Increase mesenteric blood
-Indication for transport flow
-Patient status during transport + Risk of tachyarrhythmias
(Vital signs, level of consciousness) Dobutamine + Primarily β1
+ SVR may decrease
COMMON DRUGS IN ICU + Useful in Rt heart failure
+ Risk of tachyarrhythmias
Sedation Isoproteronol + Positive chronotrope
Indication Relieve pain + Increase HR & myocardial
Reduce anxiety & oxygen consumption
agitation + May worse ischemia
Provide amnesia PDE inhibitor
Reduce patient-ventilator * Milrinone + Positive inotrope &
dysynchrony * Amrinone vasodilator
Reduce respiratory + Little effect in HR
muscle oxygen + Used in CHF
consumption + Risk of tachyarrhythmia
Common drugs Adrenaline + Very potent agent
BDZ + No analgesic properties + Effect on metabolic rate
* Diazepam + Lipid soluble + Useful in anaphylaxis
* Lorazepam + Interact with propranolol + Risk of coronary ischemia,
* Midazolam renal vasoconstriction
Propofol + Respiratory & CVS Noradrenaline + Potent α agent
depression + Tend to spare brain & heart
+ Only in ventilated patient + Good in increasing SVR
Butyrophenones + Anti-psychotic tranquilizer + Can cause reflex
* Haloperidol + In agitated, delirious bradycardia
&psychotic patient Phenylephrine + Pure α agent
+ Patient can develop EPS + Cause minimal increase in
HR or contractility
Analgesics + Does not spare brain &
Indication Relieve pain heart
Common drugs Ephedrine + Release tissue stores of
Opiods adrenaline
* Morphine + Morphine- hypotension + Last longer & less potent
* Fentanyl + Fentanyl- expensive than adrenaline
Non-opiods Vasopressin + Useful in septic shock
* Ketamine + Ketamine can cause + To parallel HRT
* Ketorolac nightmares, hallucination Nitroglycerine + Venodilator at low dose
& bronchodilate + Arteriodilation at high dose
+ Ketorolac side effect’s + Short duration, rapid onset
increase in critically ill & + Risk of ↑ ICP, headache
can cause renal failure. Nitroprusside + Balanced vasodilator
+ Rapid onset
+ Used in HPT emergency,
severe CHF, aortic
dissection
+ Risk of CN poisoning, ↑ ICP
Labetolol + α1 & β blocker
+ Does not ↑ ICP
+ Used in HPT emergency,
aortic dissection
S-ar putea să vă placă și
- Chest Tubes: Reason For UseDocument15 paginiChest Tubes: Reason For UseJack Keurig100% (2)
- Hemodynamic Management Pocket Card PDFDocument8 paginiHemodynamic Management Pocket Card PDFjenn1722Încă nu există evaluări
- Common Cardiac MedicationsDocument1 paginăCommon Cardiac MedicationsPaige HardekopfÎncă nu există evaluări
- Cardiovascular MneumonicsDocument10 paginiCardiovascular MneumonicsKaly RieÎncă nu există evaluări
- CCRN Synergy and Exam StartegiesDocument12 paginiCCRN Synergy and Exam StartegiesMarcus, RN100% (2)
- The 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsDe la EverandThe 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsÎncă nu există evaluări
- CCRN-PCCN Review GastrointestinalDocument23 paginiCCRN-PCCN Review GastrointestinalGiovanni MictilÎncă nu există evaluări
- Ecg InterpretationDocument9 paginiEcg InterpretationEthan Rodriguez100% (3)
- TNCC Prep Packet Revised June 2016Document12 paginiTNCC Prep Packet Revised June 2016nurse2012100% (3)
- ICU Basic Critical Care For NursesDocument8 paginiICU Basic Critical Care For Nursesarv rskoÎncă nu există evaluări
- Answers MediDocument443 paginiAnswers MediAmine Younis100% (13)
- Chest Tube Explanation by AllnursesDocument3 paginiChest Tube Explanation by AllnursesYemaya84Încă nu există evaluări
- ICU Guideline: Temporary Cardiac PacingDocument8 paginiICU Guideline: Temporary Cardiac PacingistiÎncă nu există evaluări
- ECG Master Class-2Document138 paginiECG Master Class-2Shohag ID Center100% (1)
- CCRN Review Part 1: "Never Let What You Cannot Do Interfere With What You Can Do"Document160 paginiCCRN Review Part 1: "Never Let What You Cannot Do Interfere With What You Can Do"Paolo VegaÎncă nu există evaluări
- Boot Camp Hemodynamic MonitoringDocument37 paginiBoot Camp Hemodynamic MonitoringTinaHo100% (7)
- 2 ICU Nursing For NoviceDocument27 pagini2 ICU Nursing For NoviceChannelGÎncă nu există evaluări
- Icu NotesDocument47 paginiIcu NotesChryst Louise SaavedraÎncă nu există evaluări
- Critical Care Nursing Course MapDocument1 paginăCritical Care Nursing Course MapMelissa David0% (1)
- ABCDE Approach PDFDocument3 paginiABCDE Approach PDFJohn SmithÎncă nu există evaluări
- Myocardial Infarction Case Analysis: Symptoms, Causes, Diagnosis (MIDocument76 paginiMyocardial Infarction Case Analysis: Symptoms, Causes, Diagnosis (MIIpeÎncă nu există evaluări
- Basic EKG Dysrhythmia IdentificationDocument40 paginiBasic EKG Dysrhythmia IdentificationIlda Dhe Devis Spaho100% (1)
- Critical Care NursingDocument159 paginiCritical Care NursingJoy Jarin50% (2)
- FLASH CardsDocument3 paginiFLASH Cardsclarheena100% (2)
- Deadly PE Blood Clot Blocks Lung ArteriesDocument1 paginăDeadly PE Blood Clot Blocks Lung ArteriesTrisha VergaraÎncă nu există evaluări
- Cardiac Notes NursingDocument16 paginiCardiac Notes NursingYemaya8494% (17)
- Afib NCPDocument3 paginiAfib NCPGen RodriguezÎncă nu există evaluări
- Understanding 1st, 2nd and 3rd Degree Heart BlocksDocument3 paginiUnderstanding 1st, 2nd and 3rd Degree Heart BlockslhenÎncă nu există evaluări
- Critical Care Nursing Manuall IDocument90 paginiCritical Care Nursing Manuall ILesley Gonzalez75% (4)
- ECG Questions for MRCP/MRCPI ExamsDocument52 paginiECG Questions for MRCP/MRCPI ExamsHasan Mahmud100% (1)
- Drugs in PediatricsDocument18 paginiDrugs in PediatricsKarla Sanchez100% (5)
- Drugs in PediatricsDocument18 paginiDrugs in PediatricsKarla Sanchez100% (5)
- Drugs in PediatricsDocument18 paginiDrugs in PediatricsKarla Sanchez100% (5)
- Emergency Medical Procedures GuideDocument57 paginiEmergency Medical Procedures GuideDuane Liloc100% (1)
- 1700 Subject Wise by PLAB Zillas (Bookmarked)Document380 pagini1700 Subject Wise by PLAB Zillas (Bookmarked)hackchild100% (1)
- Emergency Room NursingDocument6 paginiEmergency Room Nursingsberry5220% (1)
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsDe la EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsÎncă nu există evaluări
- Surviving the ICU: A Toolkit for the Critical Care NurseDe la EverandSurviving the ICU: A Toolkit for the Critical Care NurseÎncă nu există evaluări
- CRITICAL CARE NURSE: Passbooks Study GuideDe la EverandCRITICAL CARE NURSE: Passbooks Study GuideÎncă nu există evaluări
- Concept Map 1Document5 paginiConcept Map 1api-396919069Încă nu există evaluări
- Anticoagulation Care GuideDocument13 paginiAnticoagulation Care GuideSadiah Hasyim AlweiniÎncă nu există evaluări
- Publication Requirement for Laws to Ensure Due ProcessDocument6 paginiPublication Requirement for Laws to Ensure Due ProcessElieÎncă nu există evaluări
- Case-Based Discussion: BY: DAFFA JOKO N W (30101507415) Advisor: Dr. Saugi Abduh, Sp. PD., KKV, FinasimDocument71 paginiCase-Based Discussion: BY: DAFFA JOKO N W (30101507415) Advisor: Dr. Saugi Abduh, Sp. PD., KKV, FinasimAmanullah RayenÎncă nu există evaluări
- Nursing School EKGDocument43 paginiNursing School EKGRob Dickerson100% (1)
- 209 Pope, B. CCRN-PCCN-CMC Review Cardiac Part 1Document14 pagini209 Pope, B. CCRN-PCCN-CMC Review Cardiac Part 1peanant100% (1)
- Myocardium - The heart muscle that surrounds the ventricles and atriaDocument19 paginiMyocardium - The heart muscle that surrounds the ventricles and atriaFilane AntonetteÎncă nu există evaluări
- Maternity Nursing Edited Royal PentagonDocument49 paginiMaternity Nursing Edited Royal PentagonRichard Ines Valino95% (38)
- CABG PathwayDocument5 paginiCABG PathwayHardyansyah Harisman100% (1)
- Week 2 Case StudyDocument8 paginiWeek 2 Case StudyMelissa Cerny100% (3)
- PDF - VeinsDocument3 paginiPDF - VeinsjulialeoÎncă nu există evaluări
- Catholic Vicar Apostolic of The Mountain Province v. CADocument2 paginiCatholic Vicar Apostolic of The Mountain Province v. CAlmlÎncă nu există evaluări
- 409 Pope, B. and Maillie, S. CCRN-PCCN Review Multisystem and Q and ADocument21 pagini409 Pope, B. and Maillie, S. CCRN-PCCN Review Multisystem and Q and Agliftan100% (2)
- Necrotizing Otitis 2022Document20 paginiNecrotizing Otitis 2022asmashÎncă nu există evaluări
- Inotropes in Critical Care UnitDocument48 paginiInotropes in Critical Care UnitKelvin Christopher Ker100% (1)
- Adult Cardiac Surgery - Nursing Care and ManagementDocument225 paginiAdult Cardiac Surgery - Nursing Care and ManagementOsama Elsayed AhmedÎncă nu există evaluări
- City of Manila v. Laguio-DigestDocument4 paginiCity of Manila v. Laguio-DigestCreshan Ellah Combate SolivenÎncă nu există evaluări
- Pope, B. CCRN-PCCN-CMC Review Endocrine and BehavioralDocument14 paginiPope, B. CCRN-PCCN-CMC Review Endocrine and BehavioralKeisha JenkinsÎncă nu există evaluări
- Arterial Lines Mark Hammerschmidt, RN FromDocument9 paginiArterial Lines Mark Hammerschmidt, RN FromMark Hammerschmidt100% (3)
- PLAB 1 MOCK TEST: 7th MARCH 2017Document35 paginiPLAB 1 MOCK TEST: 7th MARCH 2017Alena0% (1)
- Shock Types 141009102815 Conversion Gate01Document41 paginiShock Types 141009102815 Conversion Gate01Samjaisheel SamsonÎncă nu există evaluări
- ACS AMI FacilitatorDocument21 paginiACS AMI FacilitatorPaul Zantua57% (7)
- Cardio Oncology - Abstract Booklet - 2022Document62 paginiCardio Oncology - Abstract Booklet - 2022U of T MedicineÎncă nu există evaluări
- ACAQ Crit Care Nursing CurriculumDocument91 paginiACAQ Crit Care Nursing CurriculumAnne Julia Agustin100% (1)
- Proper Nursing Documentation WillDocument4 paginiProper Nursing Documentation Willbel_dawn019Încă nu există evaluări
- Top Nursing Actions for Chest Pain, Transfusions, Evisceration and MoreDocument4 paginiTop Nursing Actions for Chest Pain, Transfusions, Evisceration and MoreAnn ChenÎncă nu există evaluări
- Study Guide For Fluid and Electrolyte ImbalancesDocument5 paginiStudy Guide For Fluid and Electrolyte ImbalancesMandi Goetz HarmonÎncă nu există evaluări
- Arterial Lines in PACU: Presented by Autum Jacobs RN, BSNDocument34 paginiArterial Lines in PACU: Presented by Autum Jacobs RN, BSNinuko1212Încă nu există evaluări
- Arterial Line Monitoring GuideDocument13 paginiArterial Line Monitoring GuideberhanubedassaÎncă nu există evaluări
- IV Fluid CalculationDocument7 paginiIV Fluid Calculationemyjones0% (1)
- Reducing CLABSI Rates Through Proper Hand HygieneDocument1 paginăReducing CLABSI Rates Through Proper Hand HygieneMomina ArshadÎncă nu există evaluări
- Ekg Chart PDF 01Document5 paginiEkg Chart PDF 01YukiMaedaÎncă nu există evaluări
- Critical CareDocument40 paginiCritical Carenkuligowski100% (6)
- Emergency Nursing: A. General Information: Emergency Nurses Association (ENA)Document21 paginiEmergency Nursing: A. General Information: Emergency Nurses Association (ENA)Sarah Loraine100% (3)
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsDe la EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsÎncă nu există evaluări
- Republic v. Jaralve (Loo, Lissa Marie G.)Document2 paginiRepublic v. Jaralve (Loo, Lissa Marie G.)lmlÎncă nu există evaluări
- Crim - 05 Intod v. CA PDFDocument1 paginăCrim - 05 Intod v. CA PDFlmlÎncă nu există evaluări
- Palomo, Et Al. v. CA and Perfecto, Et Al. (Loo, Lissa Marie G.)Document2 paginiPalomo, Et Al. v. CA and Perfecto, Et Al. (Loo, Lissa Marie G.)lmlÎncă nu există evaluări
- 2011 Sapalo Copyright PDFDocument31 pagini2011 Sapalo Copyright PDFlmlÎncă nu există evaluări
- 132301-1989-Yaokasin v. Commissioner of CustomsDocument13 pagini132301-1989-Yaokasin v. Commissioner of CustomslmlÎncă nu există evaluări
- Mapa v. Insular GovernmentDocument1 paginăMapa v. Insular GovernmentlmlÎncă nu există evaluări
- Commissioner of Customs v. HypermixDocument8 paginiCommissioner of Customs v. HypermixJc IsidroÎncă nu există evaluări
- Bagatsing v. RamirezDocument6 paginiBagatsing v. RamirezUnis BautistaÎncă nu există evaluări
- Petitioners vs. VS.: en BancDocument14 paginiPetitioners vs. VS.: en BancAb CastilÎncă nu există evaluări
- 124079-1998-Municipality of para Aque v. V.M. RealtyDocument10 pagini124079-1998-Municipality of para Aque v. V.M. RealtyShawn LeeÎncă nu există evaluări
- de Leon vs. EsguerraDocument15 paginide Leon vs. EsguerraJordan ChavezÎncă nu există evaluări
- Petitioner Vs Vs Respondent The Solicitor General Senining Belciña & AtupDocument11 paginiPetitioner Vs Vs Respondent The Solicitor General Senining Belciña & AtupYanÎncă nu există evaluări
- People v. Que Po Lay (G.R. No. 6791 March 29, 1954)Document3 paginiPeople v. Que Po Lay (G.R. No. 6791 March 29, 1954)Hershey Delos SantosÎncă nu există evaluări
- 1.CD Control Program: Anopheles MosquitoDocument16 pagini1.CD Control Program: Anopheles MosquitoRachael Archy Engracia AdamasÎncă nu există evaluări
- QI:ourt: of Tbe IlbilippinesDocument8 paginiQI:ourt: of Tbe IlbilippinesAnonymous KgPX1oCfrÎncă nu există evaluări
- IV Cheatsheet Bgnocolor PDFDocument2 paginiIV Cheatsheet Bgnocolor PDFHermiie Joii Galang MaglaquiiÎncă nu există evaluări
- United States v. Nixon (1974) PDFDocument42 paginiUnited States v. Nixon (1974) PDFlmlÎncă nu există evaluări
- Void and Voidable MarriagesDocument6 paginiVoid and Voidable MarriageslmlÎncă nu există evaluări
- People vs. Que Po LayDocument2 paginiPeople vs. Que Po LayKatrina MontesÎncă nu există evaluări
- People v. Jaime Jose G.R. No. L-28232 - Forcible Abduction With Rape PDFDocument1 paginăPeople v. Jaime Jose G.R. No. L-28232 - Forcible Abduction With Rape PDFlmlÎncă nu există evaluări
- People v. Delmo - 130078-82 - October 4, 2002 - J. Quisumbing - en Banc PDFDocument1 paginăPeople v. Delmo - 130078-82 - October 4, 2002 - J. Quisumbing - en Banc PDFlmlÎncă nu există evaluări
- People v. Delmo - 130078-82 - October 4, 2002 - J. Quisumbing - en Banc PDFDocument1 paginăPeople v. Delmo - 130078-82 - October 4, 2002 - J. Quisumbing - en Banc PDFlmlÎncă nu există evaluări
- CONTRACTSDocument11 paginiCONTRACTSlmlÎncă nu există evaluări
- I Am Sharing 'Case Study NCM 118' With YouDocument6 paginiI Am Sharing 'Case Study NCM 118' With YouQusai BassamÎncă nu există evaluări
- Advanced Cardiovascular Life Support (Acls)Document45 paginiAdvanced Cardiovascular Life Support (Acls)Erinne DefrianiÎncă nu există evaluări
- Arrhythmias: Domina Petric, MDDocument22 paginiArrhythmias: Domina Petric, MDMwaba PeterÎncă nu există evaluări
- Chapter 125. CardioversionDocument21 paginiChapter 125. CardioversionZoe VelasquezÎncă nu există evaluări
- ECG EKG: BasicsDocument191 paginiECG EKG: BasicsSabio DenmenÎncă nu există evaluări
- Nejmcp 2023658Document9 paginiNejmcp 2023658bbraitsilvaÎncă nu există evaluări
- Alcoholic Cardiomyopathy - UpToDateDocument29 paginiAlcoholic Cardiomyopathy - UpToDateAnca StanÎncă nu există evaluări
- Amiodarone For Atrial FibrillationDocument7 paginiAmiodarone For Atrial FibrillationARÎncă nu există evaluări
- Acenocoumarol Drug Information, ProfessionalDocument47 paginiAcenocoumarol Drug Information, ProfessionalMoisés PonceÎncă nu există evaluări
- Cardioembolic StrokeDocument20 paginiCardioembolic StrokeEdwinda Desy Ratu100% (1)
- FebruaryDocument56 paginiFebruarypehuyÎncă nu există evaluări
- Cardioversion of Atrial Fibrillation in Obese Patients: Results From The Cardioversion-BMI Randomized Controlled TrialDocument22 paginiCardioversion of Atrial Fibrillation in Obese Patients: Results From The Cardioversion-BMI Randomized Controlled TrialAttilio Del RossoÎncă nu există evaluări
- (IM) End-Posting Examination Questions (G1)Document14 pagini(IM) End-Posting Examination Questions (G1)Hamud RashydÎncă nu există evaluări
- Catheter Ablation For Atrial Fibrillation: Original ArticleDocument7 paginiCatheter Ablation For Atrial Fibrillation: Original ArticleGavin WinkelÎncă nu există evaluări
- Hypertension Testing GuidelinesDocument129 paginiHypertension Testing GuidelinesChunlei WangÎncă nu există evaluări
- Reversibledementias: Milta O. LittleDocument26 paginiReversibledementias: Milta O. LittleLUCAS IGNACIO SANCHEZÎncă nu există evaluări
- Practice ECGStripsDocument300 paginiPractice ECGStripsrobby zayendraÎncă nu există evaluări
- Chapter 036Document3 paginiChapter 036marinor467Încă nu există evaluări
- Health Care Provider Satisfaction With A New Electronic Progress Note Format - SOAP Vs APSO FormatDocument3 paginiHealth Care Provider Satisfaction With A New Electronic Progress Note Format - SOAP Vs APSO FormatPrem KumarÎncă nu există evaluări
- Peripocedural Anticoagulation LPDocument11 paginiPeripocedural Anticoagulation LPlauraalvisÎncă nu există evaluări
- Lets Talk About Risk Factors For Stroke UCM - 309713 PDFDocument2 paginiLets Talk About Risk Factors For Stroke UCM - 309713 PDFHifza LuthfianiÎncă nu există evaluări