Documente Academic
Documente Profesional
Documente Cultură
Koda Kimble Fartddder 9th
Încărcat de
simon bagasTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Koda Kimble Fartddder 9th
Încărcat de
simon bagasDrepturi de autor:
Formate disponibile
22-14 PULMONARY DISORDERS
Studies comparing responses to SABAs administered by
Metered-Dose Inhaler
nebulization versus IPPB have shown no significant advan-
(MDI) tages for the IPPB method of administration.5 Furthermore,
dose-response studies that compared nebulization with IPPB
and pressurized metered-dose aerosols in stable chronic asthma
patients have shown no advantage among these methods of
administration when equivalent doses are administered.5,25,26
Each method delivers approximately 10% of the beginning
dose to the patient’s airways.27 Trials comparing metered-dose
aerosols of short-acting inhaled β 2 -agonists with the nebuliza-
tion of those same drugs in acute asthma also have shown no
significant advantage for the nebulization method of adminis-
tration when the metered-dose aerosolized administration was
carefully supervised by experienced personnel and a spacer
device was used. 28,29 However, in some younger acutely ill
children, it is difficult (even with supervision) to administer an
effective SABA with a metered-dose canister. Because many
patients and clinicians perceive that nebulizers provide more
Open Nebulizer intensive therapy, it often is important psychologically to give
at least the first dose of a SABA via a nebulizer. Thereafter,
it is more cost-effective to use the therapeutically equivalent
MDI plus spacer.30
The dose ratio for SABAs delivered by MDI plus spacer
versus nebulizer has varied in the literature. For children with
mild acute asthma, 2 puffs of albuterol MDI attached to a
spacer were not different from 6 to 10 puffs of albuterol or via
nebulizer 0.15 mg/kg.31 In one double-blind trial in children
with a severe exacerbation, investigators used a dose ratio of 1:5
(i.e., albuterol MDI-spacer 1 mg [10 puffs]: nebulized albuterol
5 mg).32 Nebulization of albuterol with compressed air or,
preferably, oxygen was the preferred method of administration
Closed Nebulizer for Q.C. initially.
DOSING
7. Starting 20 minutes after the first albuterol dose, two more
doses of 2.5 mg of albuterol were administered by nebulizer Q 20
minutes over the next 40 minutes. After three treatments, Q.C.’s
breath sounds became increasingly clear. She was no longer in
distress and could speak in complete sentences. Her PEF was now
70% of predicted, her SaO2 was 97% on room air, and discharge to
home was planned. Were the dose and dosing interval of albuterol
appropriate for Q.C.?
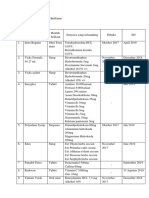
FIGURE 22-10 Metered-dose inhaler and nebulizer.
Schuh et al.33 demonstrated that a higher-dose albuterol reg-
imen (0.15 mg/kg vs. 0.05 mg/kg every 20 minutes) produced
Nebulized significantly greater improvement with no greater incidence of
Medication
Solution adverse effects. Schuh et al.34 subsequently reported greater ef-
Jet Orifice Baffle ficacy of albuterol in a dose of 0.3 mg/kg (up to 10 mg) hourly
over a dose of 0.15 mg/kg (up to 5 mg) hourly in children. The
Mainstream larger dose was tolerated as well as the 0.15 mg/kg dose.
Gas Flow Patient
Therefore, Q.C.’s albuterol regimen of 2.5 mg (0.13 mg/kg)
nebulized every 20 minutes for 40 minutes subsequent to her
first dose of aerosolized albuterol could have been even more
Capillary aggressive but was appropriate. Figure 22-12 and Table 22-5
Tube list the doses for inhaled β -agonists for acute asthma as well
as doses of other medications.1
COMPARISON OF SHORT-ACTING INHALED β2 -AGONISTS
Medication Solution
8. Would another SABA have been more effective in the initial
FIGURE 22-11 Air jet nebulizer. therapy of Q.C.?
S-ar putea să vă placă și
- VALIDASI 1 (Aris DKK) A. Baku Konsentrasi (PPM) AUCDocument8 paginiVALIDASI 1 (Aris DKK) A. Baku Konsentrasi (PPM) AUCsimon bagasÎncă nu există evaluări
- VALIDASI 1 (Aris DKK) A. Baku Konsentrasi (PPM) AUCDocument8 paginiVALIDASI 1 (Aris DKK) A. Baku Konsentrasi (PPM) AUCsimon bagasÎncă nu există evaluări
- RDGerroranalDocument7 paginiRDGerroranalsjjbioÎncă nu există evaluări
- QwertyuiscscsopDocument1 paginăQwertyuiscscsopsimon bagasÎncă nu există evaluări
- Farmakokinetik Soal JawabanDocument1 paginăFarmakokinetik Soal Jawabansimon bagasÎncă nu există evaluări
- NoDocument1 paginăNosimon bagasÎncă nu există evaluări
- ReadmeDocument1 paginăReadmesimon bagasÎncă nu există evaluări
- EscgvyDocument1 paginăEscgvysimon bagasÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (120)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Aetiology of Canine Infectious Respiratory Disease Complex and Prevalence of Its Pathogens in EuropeDocument23 paginiAetiology of Canine Infectious Respiratory Disease Complex and Prevalence of Its Pathogens in EuropeNadia AbarcaÎncă nu există evaluări
- A Guide To The Pathology and Inspection of Poultry: H Thompson R Irvine D J Taylor W SteeleDocument92 paginiA Guide To The Pathology and Inspection of Poultry: H Thompson R Irvine D J Taylor W SteeleorigatÎncă nu există evaluări
- MalariaDocument21 paginiMalariayusak tapakedingÎncă nu există evaluări
- Growth Hormone DisordersDocument1 paginăGrowth Hormone DisordersVishalÎncă nu există evaluări
- Communication Skills For Medicine Lloyd PDFDocument2 paginiCommunication Skills For Medicine Lloyd PDFLester10% (10)
- Childrens Colour Trail TestDocument5 paginiChildrens Colour Trail Testsreetama chowdhuryÎncă nu există evaluări
- Comparison of Vildagliptin-Metformin and Glimepiride-Metformin Treatments in Type 2 Diabetic PatientsDocument7 paginiComparison of Vildagliptin-Metformin and Glimepiride-Metformin Treatments in Type 2 Diabetic PatientsGregory VeintimillaÎncă nu există evaluări
- Passenger/Traveler Details: Undertaking and Acknowledgement Form Related To COVID-19 Health MeasuresDocument1 paginăPassenger/Traveler Details: Undertaking and Acknowledgement Form Related To COVID-19 Health MeasuresLabli BicÎncă nu există evaluări
- Drug Safety Priorities 2021: Center For Drug Evaluation and ResearchDocument52 paginiDrug Safety Priorities 2021: Center For Drug Evaluation and ResearchSamaa Al TabbahÎncă nu există evaluări
- Detailed Study On Infertility Its Causes and TreatmentDocument2 paginiDetailed Study On Infertility Its Causes and TreatmentBibhuti bhusan MondalÎncă nu există evaluări
- Verrucous CarcinomaDocument12 paginiVerrucous Carcinomaanatomimanusia100% (1)
- Automated DatabasesDocument14 paginiAutomated DatabasesAnilkumar Sagi100% (4)
- Diagnosis Management Hepatic Encephalopathy Diagnosis Dan Penatalaksanaan Ensefalopati HepatikDocument21 paginiDiagnosis Management Hepatic Encephalopathy Diagnosis Dan Penatalaksanaan Ensefalopati HepatikKadek Rudita YasaÎncă nu există evaluări
- Ano Rectal ExaminationDocument12 paginiAno Rectal ExaminationSnehal SinghÎncă nu există evaluări
- 01f2 - ICD vs. DSM - APA PDFDocument1 pagină01f2 - ICD vs. DSM - APA PDFfuturistzgÎncă nu există evaluări
- Potassium Chloride GuidelinesDocument25 paginiPotassium Chloride GuidelinesYasser Gebril86% (7)
- Low VisionDocument7 paginiLow VisionUme HabibaÎncă nu există evaluări
- Annual Report 2010Document72 paginiAnnual Report 2010Yan-Lin Jubi LeeÎncă nu există evaluări
- Suture Size: SmallestDocument2 paginiSuture Size: SmallestGeraldine BirowaÎncă nu există evaluări
- Plan Design Review GuideDocument37 paginiPlan Design Review GuideclrhoadesÎncă nu există evaluări
- Sujok Global MagazineDocument52 paginiSujok Global MagazineNidhi ShahÎncă nu există evaluări
- 5.3 - Structured Communication Using The SBAR ToolDocument15 pagini5.3 - Structured Communication Using The SBAR ToolJehad AlturkÎncă nu există evaluări
- PedoDocument2 paginiPedoHenyo AkoÎncă nu există evaluări
- Clinical Case Studies 2013 Bunaciu 179 98Document21 paginiClinical Case Studies 2013 Bunaciu 179 98adri90Încă nu există evaluări
- Discharge Planning ProjectDocument5 paginiDischarge Planning Projectapi-325271731Încă nu există evaluări
- WEF Scaling Smart Solutions With AI in Health Unlocking Impact On High Potential Use CasesDocument37 paginiWEF Scaling Smart Solutions With AI in Health Unlocking Impact On High Potential Use Casesdaniela cabedoÎncă nu există evaluări
- AHA Scientific StatementDocument42 paginiAHA Scientific StatementepraetorianÎncă nu există evaluări
- Anesthesia in The FutureDocument11 paginiAnesthesia in The FuturesayednourÎncă nu există evaluări
- Mariana Katkout, Health Psychology 7501PSYSCI (AP1) A Defense of The Biopsychosocial Model vs. The Biomedical ModelDocument13 paginiMariana Katkout, Health Psychology 7501PSYSCI (AP1) A Defense of The Biopsychosocial Model vs. The Biomedical ModelMariana KatkoutÎncă nu există evaluări
- Burn Lecture NotesDocument5 paginiBurn Lecture NotesJerlyn Lopez100% (1)