Documente Academic
Documente Profesional
Documente Cultură
Ciclooxigenasa 1y2 PDF
Încărcat de
YariCárdenasTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Ciclooxigenasa 1y2 PDF
Încărcat de
YariCárdenasDrepturi de autor:
Formate disponibile
CLINICAL STUDIES
Cyclooxygenase-1 and Cyclooxygenase-2
Selectivity of Widely Used Nonsteroidal
Anti-Inflammatory Drugs
Byron Cryer, MD, Mark Feldman, MD
PURPOSE: Both isoforms of cyclo-oxygenase, COX-1 and RESULTS: Inhibitory potency and selectivity of NSAIDs for
COX-2, are inhibited to varying degrees by all of the available COX-1 and COX-2 activity in blood varied greatly. Some
nonsteroidal anti-inflammatory drugs (NSAIDs). Because inhi- NSAIDs (eg, flurbiprofen, ketoprofen) were COX-1 selective,
bition of COX-1 by NSAIDs is linked to gastrointestinal ulcer some (eg, ibuprofen, naproxen) were essentially nonselective,
formation, those drugs that selectively inhibit COX-2 may have while others (eg, diclofenac, mefenamic acid) were COX-2 se-
less gastrointestinal toxicity. We measured the extent to which lective. Inhibitory effects of NSAIDs on gastric prostaglandin E2
NSAIDs and other anti-inflammatory or analgesic drugs inhibit synthesis correlated with COX-1 inhibitory potency in blood (P
COX-1 and COX-2 in humans. ,0.001) and with COX-1 selectivity (P ,0.01), but not with
SUBJECTS AND METHODS: Aliquots of whole blood from COX-2 inhibitory potency. Even COX-2 “selective” NSAIDs
16 healthy volunteers were incubated ex vivo with 25 antiin- still had sufficient COX-1 activity to cause potent inhibitory
flammatory or analgesic drugs at six concentrations ranging effects on gastric prostaglandin E2 synthesis at concentrations
from 0 (control) to 100 mM (n 5 5 for each). Blood was assayed achieved in vivo.
for serum-generated thromboxane B2 synthesis (COX-1 assay) CONCLUSION: No currently marketed NSAID, even those
and for lipopolysaccharide-stimulated prostaglandin E2 synthe- that are COX-2 selective, spare gastric COX activity at therapeu-
sis (COX-2 assay). In addition, gastric biopsies from the same tic concentrations. Thus, all NSAIDs should be used cautiously
volunteers were incubated with each drug ex vivo and mucosal until safer agents are developed. Am J Med. 1998;104:
prostaglandin E2 synthesis measured. 413– 421. q1998 by Excerpta Medica, Inc.
N
onsteroidal anti-inflammatory drugs (NSAIDs) most tissues throughout the body, including the gastro-
inhibit cyclooxygenase (COX), the rate-limiting intestinal mucosa. COX-2 is expressed at low levels in
enzyme for synthesis of prostaglandins. Al- most cells, including the normal human stomach and in-
though inhibition of COX may underlie the beneficial testine (10,11). Unlike COX-1, however, expression of
anti-inflammatory, analgesic, and antipyretic effects of COX-2 can be up-regulated at inflammatory sites by cy-
NSAIDs, simultaneous COX inhibition in the gastroin- tokines and bacterial products such as lipopolysaccha-
testinal mucosa often results in gastric and intestinal ul- ride. Thus, a NSAID that inhibits COX-2 while sparing
cers, which may have serious consequences. Indeed, all COX-1 has the potential to be anti-inflammatory yet
COX-inhibiting NSAIDs currently available by prescrip- nontoxic to the gastrointestinal tract.
tion in the United States carry a warning about life- Although currently available NSAIDs inhibit both
threatening gastrointestinal ulcers. COX-1 and COX-2, many appear to inhibit one isoform
The recent discovery that there are two COX isoforms, to a greater extent than the other (12–19). Most data on
COX-1 and COX-2, that are variably expressed in differ- functional differences in COX isoform inhibition (selec-
ent tissues raised the possibility that the therapeutic effect tivity) of NSAIDs have come from studies in animals or in
of NSAIDs could be separated from their toxic gastroin- isolated cells. No studies have compared the effects of
testinal effects (1–9). COX-1 is expressed constitutively in various NSAIDs on the human gastrointestinal mucosa.
In this study, we investigated the COX-selectivity of
several NSAIDs in healthy men and women. First, we
From the Department of Medicine, Dallas Department of Veterans Af-
fairs Medical Center and University of Texas Southwestern Medical measured the effects of the drugs in whole blood, using
School, Dallas, Texas. assays that specifically detect COX-1 or COX-2 inhibi-
Supported by a Merit Review Grant from the Department of Veterans tion. Second, we studied the effects of the same drugs in
Affairs and Southland Financial Corporation Distinguished Chair in
Geriatrics. the stomach by measuring ex vivo rates of prostaglandin
Requests for reprints should be addressed to Byron Cryer, MD, Gas- synthesis in human gastric mucosal biopsies exposed to
troenterology (111B1), Dallas VA Medical Center, 4500 S. Lancaster these agents. Finally, we compared inhibitory effects of
Rd., Dallas, Texas 75216.
Manuscript submitted October 2, 1997 and accepted in revised form the drugs on COX-1 and COX-2 in blood with their abil-
February 25, 1998. ity to inhibit prostaglandin synthesis in the stomach.
q1998 by Excerpta Medica, Inc. 0002-9343/98/$19.00 413
All rights reserved. PII S0002-9343(98)00091-6
NSAID Effects on COX-1 and COX-2/Cryer and Feldman
Table 1. Drugs Tested interval between study days 1 and 10, no medications
Non-aspirin NSAIDs were dispensed or allowed.
•Diclofenac (Voltaren) We studied 25 anti-inflammatory, analgesic, and other
•Etodolac (Lodine) drugs of interest (Table 1). Most were NSAIDs, including
•Fenoprofen (Nalfon) 6-methoxy napthalene acetic acid (6-MNA), the active
•Flurbiprofen (Ansaid) metabolite of nabumetone. (Sulindac sulfide, the active
•Ibuprofen (Motrin) metabolite of sulindac was not available.) Other drugs
•Indomethacin (Indocin) included four nonacetylated salicylates, the corticoste-
•Ketoprofen (Orudis) roid dexamethasone, acetaminophen, and two experi-
•Ketorolac (Toradol) mental anti-inflammatory agents (NS-398 and nimesu-
•Mefenamic Acid (Ponstel) lide). We purchased from the manufacturer powdered
•Naproxen (Naprosyn) formulations of 22 of the drugs, specifically ibuprofen,
•Oxaprosin (Daypro) ketorolac, 6-methoxy napthalene acetic acid, nimesulide,
•Piroxicam (Feldene) NS-398, and valeryl salicylate (from Cayman Chemical
•Tolmetin (Tolectin) Co., Ann Arbor, Michigan); and acetylsalicylic acid (as-
Pro-drug NSAIDs pirin), acetaminophen, dexamethasone, diclofenac,
•Sulindac (Clinoril)
etodolac, fenoprofen, flurbiprofen, indomethacin, keto-
•Nabumetone (Relafen)
profen, mefenamic acid, naproxen, nabumetone, piroxi-
Metabolite
cam, tolmetin, salicylic acid, and sulindac (from Sigma
•6-MNA (metabolite of nabumetone)
Acetylated salicylate
Chemical Co., St. Louis, Missouri). Powdered formula-
•Aspirin tions of bismuth subsalicylate (Proctor and Gamble, Cin-
Non-acetylated Salicylates cinnati, Ohio), oxaprosin (G.D. Searle Pharmaceuticals,
•Salicylic acid Chicago, Illinois), and salsalate (3M Pharmaceuticals, St.
•Salsalate (Disalcid) Paul, Minnesota) were donated by the manufacturer.
•Valeryl salicylate For each drug, stock solutions were made by mixing
•Bismuth subsalicylate (Pepto-Bismol) powdered drug with dimethyl sulfoxide (Sigma Chemical
Analgesic Co., St. Louis, Missouri). Then, six concentrations of
•Acetaminophen (Tylenol) drug (100, 10, 1, 0.1, 0.01 and 0 mM) were prepared by
Steroid mixing the appropriate amount of stock solution either
•Dexamethasone (Decadron) with 10 mM phosphate buffer saline (Sigma Chemical
Investigational Co., St. Louis, Missouri) for COX-1 and COX-2 whole
•NS-398 blood assays or with 150 mM Tris Buffer (Trizma Hydro-
•Nimesulide chloride; Sigma Chemical Co., St. Louis, Missouri) for
gastric mucosal COX assays. New solutions were made on
each study day just prior to obtaining whole blood or
gastric mucosal biopsies.
MATERIALS AND METHODS
COX-1 whole blood assay. The measurement of throm-
Prior to enrollment of study subjects, this study was ap- boxane B2 synthesis from platelets following blood coag-
proved by the Human Studies Subcommittee of the Dal- ulation is a specific test for COX-1 activity (18,19). Plate-
las Department of Veterans Affairs Medical Center. lets constitutively express COX-1. In response to endog-
We enrolled 16 nonsmoking healthy volunteers (6 men enous thrombin formation (ie, clot formation) platelet
and 10 nonpregnant women) between the ages of 23 and COX-1 is maximally stimulated to produce thromboxane
46 years. None had a history of peptic ulcer, gastrointes- A2, which is converted to thromboxane B2. Thrombox-
tinal surgery (except for appendectomy), NSAID use in ane B2 production reaches a plateau 1 hour after coagu-
the past 2 weeks, chronic upper gastrointestinal symp- lation.
toms, or use of histamine H2-receptor antagonists, pro- On each study day, siliconized glass tubes were orga-
ton pump inhibitors, misoprostol, or sucralfate. Each nized into four sets of six tubes so that each subject’s
subject was seronegative for Helicobacter pylori infection blood sample would be exposed to the same four drugs as
(FlexSure Hp; SmithKline Diagnostics, Inc. San Jose, Cal- his or her gastric mucosal biopsies. After venipuncture,
ifornia). Subjects were scheduled for visits on study days 1 4-mL aliquots of whole blood were immediately trans-
and 10. At both visits, health and medication histories ferred to tubes preloaded with freshly made study drug
were confirmed, venous blood was obtained for COX-1 solution so that final drug concentrations in each set of 6
and COX-2 whole blood assays, after which each subject tubes were 100, 10, 1, 0.1, 0.01, and 0 mM. All tubes were
underwent endoscopy with mucosal biopsy. During the briefly and gently vortexed to distribute drug thoroughly
414 May 1998 THE AMERICAN JOURNAL OF MEDICINEt Volume 104
NSAID Effects on COX-1 and COX-2/Cryer and Feldman
and then allowed to clot, initially for 45 minutes at 378C curvature of the gastric body. Each gastric mucosal biopsy
and then for 2 additional hours at room temperature. At was immediately placed in a study drug incubation solu-
the end of the 2-hour 45-minute incubation period, in- tion.
domethacin was added to the tube at a final concentra-
Gastric mucosal prostaglandin E2 ex vivo synthesis
tion of 30 mM, to terminate thromboxane B2 synthesis.
assay. The ability of the gastric mucosa to generate pros-
This was followed by centrifugation at 2,000g for 10 min-
taglandins (prostaglandin synthesis rate) estimates total
utes at room temperature. One mL serum from each tube
gastric COX activity (COX-1 plus any COX-2). To mea-
was then stored at 2708C until thromboxane B2 was mea-
sure ex vivo prostaglandin synthesis rates, gastric muco-
sured by radioimmunoassay, as previously described
sal biopsies were immediately placed in 1.5 mL polypro-
(18). Mean (6 SD) baseline thromboxane B2 synthesis in
pylene microcentrifuge tubes (Fisher Scientific, Pitts-
whole blood at 2 hours 45 minutes was 236.0 6 105.4
burgh, Pennsylvania) that contained 1 mL study drug
ng/mL.
incubation solution. The 24 biopsies from each endo-
COX-2 whole blood assay. The measurement of pros- scopic session were allocated to four different drugs at six
taglandin E2 production from monocytes and macro- concentrations per drug as directed by a previously deter-
phages in whole blood following stimulation with lipo- mined drug allocation schedule. This schedule was de-
polysaccharide is a specific test for COX-2 activity. Twen- signed so that gastric mucosal prostaglandin synthesis
ty-four hours after incubation of whole blood with was assessed five times for each of the six concentrations
lipopolysaccharide, 95% to 99% of COX activity is of every drug, and so that each time a drug concentration
COX-2 (18,19). Thus, prostaglandin E2 measured 24 was tested (n 5 5), the incubated gastric mucosal biopsy
hours after lipopolysaccharide stimulation should almost would be from a different study subject.
exclusively reflect COX-2 activity. Ex vivo gastric mucosal prostaglandin synthesis was
First, 1.5 mL polypropylene microcentrifuge tubes performed by a modification of a method previously de-
(Fisher Scientific, Pittsburgh, Pennsylvania) were pre- scribed by our laboratory (20). Briefly, incubation tubes
loaded with the same drugs and concentrations used for containing biopsies were weighed, and mucosal biopsy
that subject’s COX-1 and gastric mucosal assays. Next, weight was determined after subtraction of the original
whole blood was collected by venipuncture into heparin- tube weight. Each mucosal biopsy was then finely minced
ized vacuum tubes, pooled, and aliquoted into 24, with scissors for 15 seconds, allowed to incubate after
500-mL samples so that the same final six drug concen- mincing for 3 minutes, and then briefly centrifuged at
trations would be achieved as with the other assays. Lipo- 14,000g for 15 seconds to pellet tissue. Since endoscopic
polysaccharide (50 mg E Coli serotype (127:B8; Sigma biopsies were placed in solution at varying times, original
Chemical Co., St. Louis, Missouri) was added to each incubation solutions were then discarded by aspiration
tube, briefly vortexed, and then incubated for 24 hours at and replaced with 1 mL identical fresh solutions at timed
378C for induction of COX-2. Tubes were then centri- intervals. Next, biopsies were briskly vortexed for 3 min-
fuged at 12,000g for 5 minutes, and 100 mL of the result- utes (to generate and liberate prostaglandins). After 15
ing plasma was mixed with 400 ml of methanol for extrac- seconds of centrifugation, indomethacin (1025 M) was
tion of prostaglandins and precipitation of proteins. Su- added to the supernatant to stop further prostaglandin
pernatants were then stored at 2708C until they were synthesis. Supernatants were then stored at 2708C until
assayed for prostaglandin E2 by radioimmunoassay using ready for measurement of prostaglandin E2 by radioim-
a kit (Prostaglandin E2 [I125], Biotrak radioimmunoassay munoassay (21). Prostaglandin synthesis is expressed as
system; Amersham Life Sciences, Arlington Heights, Illi- nanograms of prostaglandin E2 synthesized per gram-
nois). Mean (6 SD) lipopolysaccharide-stimulated pros- minute of tissue incubation. Mean (6 SD) gastric muco-
taglandin E2 synthesis in whole blood at 24 hours was sal prostaglandin E2 synthesis at baseline was 190.2 6
127.8 6 105.5 ng/mL. 318.7 ng/g-min.
Endoscopy and gastric mucosal biopsy. Each subject, Calculation of drug IC50. For each study drug, a dose-
after an overnight fast, received topical pharyngeal anes- response curve was constructed by plotting the six drug
thesia with tetracaine hydrochloride (Pontocaine; concentrations (x axis, logarithmic scale) against mean
Winthrop Pharmaceuticals, New York, New York), fol- percent inhibition for each group of five subjects (y axis)
lowed by light sedation with intravenous midazolam of thromboxane B2 (for blood COX-1 assay), lipopoly-
(Versed; Roche Laboratories, Nutley, New Jersey). Using saccharide-induced prostaglandin E2 (for blood COX-2
an Olympus endoscope (Olympus Corporation, New assay), or gastric prostaglandin E2 (for gastric mucosal
York, New York), the gastroduodenal mucosa was visu- COX assay). Next, the concentration of study drug that
ally inspected. No subject had any gastroduodenal ero- inhibited mean COX activity by 50% (IC50) was calcu-
sion or ulcer at either endoscopy. Following mucosal in- lated by computer-assisted extrapolation. Specifically, a
spection, 24 mucosal biopsies were taken from the greater computer-generated curve of concentration versus mean
May 1998 THE AMERICAN JOURNAL OF MEDICINEt Volume 104 415
NSAID Effects on COX-1 and COX-2/Cryer and Feldman
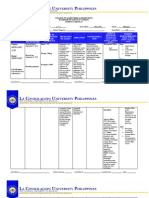
Table 2. Concentration of Drug (IC50) that Inhibited 50% of two of the drugs (salicylic acid and salsalate) inhibited
Cyclooxygenase (COX) Activity in Blood and in Gastric Mu- COX-1 at the concentrations tested in this study. Keto-
cosa (mM) profen had the lowest IC50 (0.11 mM) and was thus the
COX-1 COX-2 Gastric most potent COX-1 inhibitor in blood. The range in po-
in Blood in Blood Mucosa tency of COX-1 inhibition varied at least 1,000-fold
Drug (Rank) (Rank) (Rank) among the 25 drugs.
Ketoprofen 0.11 (1) 0.88 (8) 0.08 (2) All 25 drugs tested also inhibited COX-2 activity in
Indomethacin 0.21 (2) 0.37 (7) 0.85 (11) blood (Table 2), with potency varying approximately
Diclofenac 0.26 (3) 0.01 (1) 0.23 (4) 4,000-fold. The NSAID, diclofenac, had the most potent
Ketorolac 0.27 (4) 0.18 (6) 0.33 (6) COX-2 inhibitory effect in blood (IC50 5 0.01 mM), even
Flurbiprofen 0.41 (5) 4.23 (13) 0.23 (5) more potent than dexamethasone. Some NSAIDs (eg,
Tolmetin 1.08 (6) 2.25 (11) 3.50 (16) fenoprofen, naproxen, oxaprosin and 6-MNA, the active
Mefenamic acid 1.94 (7) 0.16 (4) 0.70 (10) metabolite of nabumetone) were less potent COX-2 in-
Piroxicam 2.68 (8) 2.11 (10) 0.87 (12) hibitors in blood than acetaminophen. Aspirin and acet-
Fenoprofen 2.73 (9) 14.03 (17) 0.17 (3) aminophen had similar effects on COX-2 in blood (Table
Aspirin 4.45 (10) 13.88 (16) 0.03 (1)
2), contrasting with aspirin’s nearly 10-fold greater po-
Ibuprofen 5.90 (11) 9.90 (14) 0.70 (9)
Nimesulide 10.48 (12) 0.18 (5) 1.49 (13)
tency on COX-1 (Table 2).
Oxaprosin 14.58 (13) 36.67 (23) 2.62 (14) COX selectivity in blood. Rankings of the 25 drugs in
Etodolac 19.58 (14) 2.47 (12) 3.20 (15) Table 3 reflect their relative selectivity for inhibition of
NS-398 21.93 (15) 0.92 (9) 100.00 (18) COX-1 or COX-2 in blood. A ratio of COX-2 IC50 to
6-MNA 31.01 (16) 19.84 (19) 0.48 (7)
Naproxen 32.01 (17) 28.19 (22) 0.52 (8)
Valeryl 32.64 (18) 0.04 (2) .100.00 (21) Table 3. Ratio of Concentration of Drug (IC50) that Inhibited
salicylate 50% of Cyclooxygenase-1 (COX-1) Activity to the IC50 for
Nabumetone 33.57 (19) 20.83 (20) 20.09 (17) COX-2 Activity in Blood
Sulindac 41.26 (20) 24.94 (21) .100.00 (19) Rank Drug Ratio*
Acetaminophen 42.23 (21) 10.69 (15) .100.00 (23)
Dexamethasone 59.95 (22) 0.13 (3) .100.00 (25) 1 Flurbiprofen 10.27
Bismuth 75.24 (23) 37.50 (24) .100.00 (22) 2 Ketoprofen 8.16
subsalicylate 3 Fenoprofen 5.14
Salicylic acid .100.00 (24) 14.08 (18) .100.00 (20) 4 Aspirin 3.12
Salsalate .100.00 (25) 39.90 (25) .100.00 (24) 5 Oxaprosin 2.52
6 Tolmetin 2.09
6-MNA 5 6-methoxy napthalene acetic acid. 7 Indomethacin 1.78
8 Ibuprofen 1.69
percent inhibition (for each group of five subjects) was 9 Naproxen 0.88
constructed for each drug. Using the formula for the 10 Piroxicam 0.79
slope of the line between the two drug doses that brack- 11 Ketorolac 0.68
12 6-MNA 0.64
eted (above and below) 50% inhibition, the IC50 was cal-
13 Nabumetone 0.62
culated. For some study drugs, COX activity was inhib- 14 Sulindac 0.61
ited by less than 50% at the maximal concentration tested 15 Bismuth subsalicylate 0.50
(100 mM). In such instances the IC50 is reported as greater 16 Salsalate 0.29†
than 100 mM. 17 Acetominophen 0.25
18 Salicylic acid 0.13†
Statistical Analysis 19 Etodolac 0.12
To determine correlations between drug IC50s in whole 20 Mefenamic acid 0.08
blood assays and gastric mucosal assays, Spearman’s 21 Diclofenac 0.05
rank-correlation coefficient and Pearson’s coefficient of 22 NS-398 0.042
correlation were used (22). P values less than 0.05 were 23 Nimesulide 0.017
considered statistically significant. 24 Dexamethasone 0.002
25 Valeryl salicylate 0.001
* Ratios .1 indicate that a drug is more COX-1 selective; ratios ,1
RESULTS indicate that a drug is more COX-2 selective.
†
Since the actual IC50 for COX-1 in blood was .100 mM, a value of
For the 25 study drugs, IC50s for inhibition in the COX-1 100 mM was used in the calculation of this ratio. Therefore, these ratios
exclusive whole blood assay (platelet-generated serum represent a maximum possible ratio of IC50 COX-2/IC50 COX-1 in
thromboxane B2 synthesis) are ranked in Table 2. All but blood.
416 May 1998 THE AMERICAN JOURNAL OF MEDICINEt Volume 104
NSAID Effects on COX-1 and COX-2/Cryer and Feldman
Figure 1. Correlation of gastric IC50 with COX-1 IC50 in blood for the 25 drugs. Rank order correlation was 0.79 (P ,0.001) and
Pearson correlation coefficient was 0.75 (P ,0.001). Drugs with an IC50 in gastric mucosa or blood .100 mM are arbitrarily plotted
at 100 mM in this and subsequent figures. ASA 5 acetysalicylic acid (aspirin); MNA 5 methoxy napthalene acetic acid.
COX-1 IC50 close to 1.0 indicates nearly equal selectivity. COX effects in gastric mucosa. Potency on gastric mu-
Selectivity among the 25 drugs varied approximately cosal COX inhibition varied by at least 300-fold among
10,000-fold. A few NSAIDs were COX-2 selective in the 25 drugs (Table 2). Aspirin was the most potent gas-
blood, particularly diclofenac (IC50 ratio 5 0.05, indicat- tric COX inhibitor. The four non-acetylated salicylates
ing 20-fold selectivity for COX-2), mefenamic acid (12.5- (valeryl salicylate, salicylic acid, salicylsalicylic acid, and
fold), and etodolac (8.5-fold). The two experimental bismuth subsalicylate), acetaminophen, and dexametha-
NSAIDs, nimesulide (59-fold) and NS-398 (24-fold), sone had no measurable effects on COX activity in the
were particularly COX-2 selective. Dexamethasone and stomach. As shown in Figure 1, the IC50 for gastric mu-
the experimental compound valeryl salicylate were the cosal COX correlated significantly correlated with the
most COX-2 selective agents tested. IC50 for COX-1 in blood (P ,0.001). As illustrated in
Figure 2. Correlation of gastric IC50 with ratio of COX-2 IC50/COX-1 IC50 in blood for the 25 drugs. Rank order correlation was
20.59 (P ,0.01) and Pearson correlation coefficient was 20.54 (P ,0.01). ASA 5 acetysalicylic acid (aspirin); MNA 5 methoxy
napthalene acetic acid.
May 1998 THE AMERICAN JOURNAL OF MEDICINEt Volume 104 417
NSAID Effects on COX-1 and COX-2/Cryer and Feldman
Figure 3. Correlation of gastric IC50 with COX-2 IC50 in blood for the 25 drugs. Rank order correlation was 0.26 and Pearson
correlation coefficient was 0.27 (both P 5 0.19). ASA 5 acetysalicylic acid (aspirin); MNA 5 methoxy napthalene acetic acid.
Figure 2, the IC50 for gastric COX also correlated with the sponsible for catalyzing the synthesis of mucosal-protec-
degree of COX-1 selectivity in blood (P ,0.01). In con- tive prostaglandins from their precursor, arachidonic
trast, the IC50 for gastric mucosal COX inhibition did not acid (4,6,21). NSAIDs that are specific or very highly se-
correlate with the IC50 for COX-2 in blood (Figure 3). lective inhibitors of COX-2 might have few gastrointesti-
nal side effects because mucosal synthesis of prostaglan-
dins would be preserved. Of the currently available
DISCUSSION
NSAIDs that we examined, diclofenac was the most po-
We have conducted a comprehensive analysis of the tent and the most selective inhibitor of COX-2 in whole
COX-1 versus COX-2 effects of NSAIDs in healthy vol- blood. Even though diclofenac was 20 times more selec-
unteers. Our results regarding COX-selectivity can be tive for COX-2 than for COX-1, this drug still had suffi-
compared with those of previous reports using nonhu- cient COX-1 inhibitory activity in the stomach to be a
man cells (14,16). We found that two agents, indometh- potent inhibitor of gastric mucosal prostaglandin synthe-
acin and piroxicam, that were quite COX-1 selective for sis. Dexamethasone, on the other hand, one tenth as po-
murine COX, were essentially nonselective for COX in tent as diclofenac as a COX-2 inhibitor, was 25 times
human blood (Table 3). Likewise, 6-MNA was sevenfold more selective than diclofenac for COX-2 inhibition in
selective for murine COX-2, but only onefold to twofold blood. Moreover, this corticosteroid had essentially no
for human COX-2. Using bovine endothelial cells gastric mucosal COX inhibition at concentrations up to
(COX-1) and murine macrophages stimulated by lipo- 100 mM, perhaps explaining why corticosteroid medica-
polysaccharide (COX-2), Mitchell et al (16) analyzed the tions given without NSAIDs are not a risk factor for gas-
selectivity of five of the NSAIDs that we examined. They troduodenal ulcers (23). The observation that a highly
found aspirin (166-fold), indomethacin (60-fold), and selective and potent COX-2 inhibitor such as dexameth-
ibuprofen (15-fold) to be quite COX-1 selective, while asone had no demonstrable effect on gastric COX sup-
these drugs were only twofold to threefold COX-1 selec- ports previous observations (10,11) that there is very little
tive in human blood (16). Naproxen was COX nonselec- COX-2 activity within the human stomach. The correla-
tive in both Mitchell’s study and in ours. Diclofenac was tion we found between COX-1 potency of NSAIDs in
also nonselective in the previous study, while we found blood and the gastric mucosa also reinforces the concept
diclofenac to be 20-fold COX-2 selective in human blood. that the healthy stomach mainly, if not exclusively, ex-
Differences in COX selectivity among these various stud- presses COX-1.
ies are probably related to species differences in the COX In addition to the potency and selectivity of a drug for
proteins. COX-1 or COX-2, the administered dose is another im-
The healthy gastrointestinal mucosa in humans pre- portant feature that must be taken into consideration
dominantly expresses COX-1, with very little COX-2 ex- when assessing overall potential gastrointestinal mucosal
pression (10,11). Gastrointestinal mucosal COX-1 is re- effects. To evaluate whether the drug concentrations used
418 May 1998 THE AMERICAN JOURNAL OF MEDICINEt Volume 104
NSAID Effects on COX-1 and COX-2/Cryer and Feldman
Table 4. Serum Nonsteroidal Antiinflammatory Drug (NSAID) Concentrations at Usual Thera-
peutic Dosage
Mean Serum IC50 for Gastric
Normal Dose Concentration COX Inhibition
NSAID (mg/day) (mM) (mM)* Reference
Aspirin (high dose) 1200–5200 111.0† 0.03 (25)
(low dose) 81–325 4.9–18.6† 0.03 ‡
Diclofenac 150–200 6.1† 0.23 (26)
Etodolac 600–1200 83.5 3.20 (24)
Fenoprofen 800–3200 89.5 0.17 (24)
Flurbiprofen 200–300 53.2 0.23 (27)
Ibuprofen (high dose) 1200–3200 111.0† 0.70 (28)
(low dose) 800–1200 38.8† 0.70 (28)
Indomethacin 75–200 1.4 0.85 (25)
Ketoprofen 100–300 9.4 0.08 (24)
Ketorolac 10–40 8.0† 0.33 (24)
Mefenamic acid 500 82.9 0.70 (24)
Naproxen 500–1000 1.3 0.52 (29)
Nimesulide 100–200 14.6 1.49 (30)
Oxaprosin 1200 681.9 2.62 (24)
Piroxicam 20 16.6 0.87 (24)
Tolmetin 1200–1800 126.9 3.50 (24)
Sulindac sulfide§ 300–400\ 14.6 not tested (31)
6-MNA¶ 1000–2000\ 155.4 0.48 (32,33)
* From Table 5.
†
Single-dose serum concentration.
‡
Cryer and Feldman, unpublished information.
§
Active metabolite of sulindac (prodrug).
\
Dosed as prodrug.
¶
Active metabolite of probumetone (prodrug).
6-MNA 5 6-methoxy napthalene acetic acid
in these experiments and the calculated IC50s were com- humans administered these two drugs at doses that pro-
parable with the usual serum concentrations seen with duced identical serum salicylate concentrations, aspirin
therapeutic dosing, we compiled pharmacokinetic data markedly reduced gastroduodenal mucosal prostaglan-
for NSAIDs from a review of the available literature (Ta- din content, while the effects of salsalate were indistin-
ble 4) (24 –33). For every drug for which data could be guishable from placebo (37).
compared, their expected therapeutic serum concentra- COX inhibition by aspirin via acetylation appears to
tions was well above their IC50 for gastric COX inhibition. play less of a role in COX-2 inhibition than in COX-1
For example, the peak concentration of diclofenac in inhibition, since valeryl salicylate (pentanoyl rather than
blood after a single oral dose is 6.1 mM, more than 25 acetyl substitution) was a very potent and selective inhib-
times higher than the IC50 in gastric mucosa. Although it itor of COX-2, while aspirin only modestly inhibited
is not known to what extent, and for how long, gastric COX-2 in blood. Interestingly, aspirin acetylates active
COX must be blocked to increase the risk of ulcer forma- serine sites in both COX-1 and COX-2 (34 –36). In the
tion, all of the NSAIDs that we studied appear capable of case of COX-1, aspirin acetylation reduces COX activity
producing gastrointestinal mucosal prostaglandin deple- by preventing arachidonate binding to the COX active
tion at customary doses. site (34,35). With COX-2, however, acetylation does not
Aspirin irreversibly acetylates COX at a serine moiety block substrate binding (36).
near the active site of the enzyme (34 –36). In the systems Two prodrug NSAIDs were evaluated in our study, su-
we tested, aspirin’s ability to acetylate COX allowed it to lindac and nabumetone. Only after absorption are these
be a modestly potent inhibitor of COX-1 in blood and the prodrugs converted to active metabolites that have anti-
most potent gastric COX inhibitor, while the nonacety- inflammatory activity. Shortly after absorption, sulindac
lated salicylates had relatively few effects in either COX-1 is reversibly reduced to sulindac sulfide, its active metab-
system. These ex vivo comparisons of the effects of sal- olite (31). Sulindac sulfide is systemically distributed and
salate (salicylsalicylic acid) and aspirin in the human inhibits COX throughout the body, including the stom-
stomach confirm our previous in vivo observations. In ach. Sulindac sulfide has been reported to be 500 times
May 1998 THE AMERICAN JOURNAL OF MEDICINEt Volume 104 419
NSAID Effects on COX-1 and COX-2/Cryer and Feldman
more potent than sulindac as a COX inhibitor (25); un- are COX-2 selective, have these gastrointestinal-sparing
fortunately, sulindac sulfide was not available to us at the features. NSAIDs should, therefore, continue to be used
time of the study. When sulindac was introduced, it was cautiously until safer agents are developed.
stated to have a low incidence of gastrointestinal side ef-
fects (38). With longer periods of clinical experience,
however, gastrointestinal complications with sulindac ACKNOWLEDGMENTS
have been similar to those of other NSAIDs (39). The authors wish to thank Kristi Rushin, Libby McAllister, and
Nabumetone is a prodrug that is converted to its active Mary Walker for expert technical assistance, Vicky Robertson
metabolite 6-MNA (32,33) after absorption. When for help with manuscript preparation, and Dr. Stuart Spechler
6-MNA and nabumetone were compared in the current for thoughtful comments regarding the manuscript. Part of this
study, they were equally potent as inhibitors of COX-1 work was presented at the Annual Meeting of the American
and COX-2 in blood, and both were only minimally Gastroenterological Association in Washington, DC, in May,
1997.
COX-2 selective. This probably occurred because nabu-
metone is rapidly converted to 6-MNA in blood (32).
However, this conversion may not occur in the gastric
mucosa, since 6-MNA was 40 times more potent a gastric REFERENCES
1. Xie W, Chipman JG, Robertson DL, et al. Expression of a mitogen-
COX inhibitor than nabumetone. Thus, the 6-MNA me-
responsive gene encoding prostaglandin synthase is regulated by
tabolite of nabumetone may lead to gastrointestinal mu- mRNA splicing. Proc Natl Acad Sci. 1991;88:2692–2696.
cosal prostaglandin depletion and predispose to ulcer 2. Kujubu DA, Fletcher BS, Varnum BC, et al. TIS10, a phorbol ester
formation. Chronic nabumetone administration in hu- tumor promoter-inducible mRNA from Swiss 3T3 cells, encodes a
mans is associated with gastrointestinal ulceration (24), novel prostaglandin synthase/cyclooxygenase homologue. J Biol
but the incidence may be somewhat lower than with Chem. 1991;266:12866 –12872.
3. Picot D, Loll PJ, Garavito RM. The x-ray crystal structure of the
other NSAIDs (40). membrane protein prostaglandin H2 synthase-1. Nature. 1994;367:
Because of the limitations that are inherent in the esti- 243–249.
mation of IC50s through extrapolation, relative ranking 4. DeWitt DL, Meade EA, Smith WL. Prostaglandin H synthase isoen-
of drugs’ COX effects may not be as precise as suggested zyme selectivity: the potential for safer nonsteroidal antiinflamma-
tory drugs. Am J Med. 1993;95:40S– 46S.
by our listings. For example, a minor change in the ex-
5. Meade EA, Smith WL, DeWitt DL. Expression of the murine pros-
trapolated estimates of COX-1 inhibitory IC50s for di- taglandin H synthase-1 and prostaglandin H synthase-2 isozymes
clofenac and ketorolac could result in a switching of their in COX-1 cells. J Lipid Mediators. 1993;6:119 –129.
positions in the rank list. The COX effects of our study 6. Williams CS, Dubois RN. Prostaglandin endoperoxide synthase:
drugs should be viewed as relative ranges of selectivity or why two isoforms? Am J Physiol. 1996;270:G393– 400.
7. Morita I, Schindler M, Reginaler MK, et al. Different intracellular
potency rather than absolute rankings. Another limita-
locations for prostaglandin endoperoxide H synthase-1 and -2.
tion is that COX responses to NSAIDs in our ex vivo J Biol Chem. 1995;270:10902–10908.
biopsy specimens may differ from in vivo responses. Fi- 8. Morham SG, Langenbach R, Loftin CD, et al. Prostaglandin syn-
nally, it is possible that COX isoform distribution or COX thase-2 gene disruption causes severe renal pathology in the mouse.
responses to NSAIDs in healthy subjects may differ from Cell. 1995;83:473– 482.
9. Hempel SL, Monick MM, Hunninghake GW. Lipopolysaccharide
those in nonhealthy patients such as those with peptic
induces prostaglandin H synthase-2 protein and mRNA in human
ulcer disease or other inflammatory conditions, or who alveolar macrophages and blood monocytes. J Clin Invest. 1994;93:
are taking other medications. 391–396.
Newer drugs that may be more COX-2 selective than 10. Kargman S, Charleson S, Cartwright M, et al. Characterization of
currently available drugs are in various stages of research prostaglandin G/H synthase 1 and 2 in rat, dog, monkey, and hu-
man gastrointestinal tracts. Gastroenterology. 1996;111:445– 454.
and development (41,42). Such agents may prove to be
11. Ristimaki A, Honkanen N, Jankala H, et al. Expression of cycloox-
effective anti-inflammatory agents that spare the gastro- ygenase-2 in human gastric carcinoma. Cancer Res. 1997;57:1276 –
intestinal tract from injury. However, as seen from the 1280.
comparisons in the current study, even a high degree of 12. Chan C, Boyce S, Brideau C, et al. Pharmacology of a selective
COX-2 selectivity does not guarantee freedom from gas- cyclooxygenase-2 inhibitor, L-745,337: a novel nonsteroidal anti-
inflammatory agent with an ulcerogenic sparing effect in rat and
tric COX inhibition. Gastric mucosal COX inhibition is
nonhuman primate stomach. J Pharmacol Exp Ther. 1995;274:
affected by a combination of COX selectivity, COX po- 1531–1537.
tency, and drug pharmacokinetics. The ideal NSAID 13. Langenbach R, Morham SG, Tiano HF, et al. Prostaglandin syn-
should be prescribed in doses that are high enough to be thase 1 gene disruption in mice reduces arachidonic acid-induced
anti-inflammatory, antipyretic, or analgesic, but not so inflammation and indomethacin-induced gastric ulceration. Cell.
high that they result in serum and gastrointestinal muco- 1995;83:483– 492.
14. Meade EA, Smith WL, DeWitt DL. Differential inhibition of pros-
sal concentrations that substantially reduce gastrointesti- taglandin endoperoxide synthase (cyclooxygenase) isozymes by as-
nal mucosal COX-1 activity and prostaglandin synthesis. pirin and other non-steroidal anti-inflammatory drugs. J Biol
None of the currently marketed NSAIDs, even those that Chem. 1993;268:6610 – 6614.
420 May 1998 THE AMERICAN JOURNAL OF MEDICINEt Volume 104
NSAID Effects on COX-1 and COX-2/Cryer and Feldman
15. Glaser K, Sung M, O’Neil K. Etodolac selectively inhibits human properties and therapeutic efficacy in rheumatic disorders. Drugs.
prostaglandin G/H synthase 2 (prostaglandin HS-2) versus human 1971;2:416 – 446.
prostaglandin HS-1. Eur J Pharm. 1995;281:107–11. 29. Hundal O, Rugstad HE, Husby G. Naproxen free plasma concen-
16. Mitchell JA, Akarasereenont P, Thiemermann C, et al. Selectivity of trations and unbound fractions in patients with osteoarthritis: re-
nonsteroidal antiinflammatory drugs as inhibitors of constitutive lation to age, sex, efficacy, and adverse events. Therapeut Drug Mon-
and inducible cyclooxygenase. Proc Natl Acad Sci. 1994;90:11693– itor. 1991;13:478 – 484.
11697. 30. Olive G, Rey E. Effect of age and disease on the pharmacokinetics of
17. Laneuville O, Breuer DK, DeWitt DL, et al. Differential inhibition nimesulide. Drugs. 1993;46:73–78.
of human prostaglandin endoperoxide H synthase-1 and -2 by non- 31. Duggan DE, Hare LE, Ditzler CA. The disposition of sulindac. Clin
steroidal anti-inflammatory drugs. J Pharmacol Exp Ther. 1994;271: Pharmacol Ther. 1977;21:326 –335.
927–934. 32. Friedel HA, Todd PA. Nabumetone: a preliminary review of its
18. Patrignani P, Panara MR, Greco A, et al. Biochemical and pharma- pharmacodynamics and pharmacokinetic properties, and thera-
cological characterization of the cyclooxygenase activity of human peutic efficacy in rheumatic diseases. Drugs. 1988;35:504 –524.
blood prostaglandin endoperoxide synthases. J Pharmacol Exp 33. McMahon FG, Vargas R, Ryan JR, Fitts DA. Nabumetone kinetics
Ther. 1994;271:1705–1712. in the young and elderly. Am J Med. 1987;83:92–95.
19. Brideau C, Kargman S, Liu S, Dallob AL. A human whole blood 34. DeWitt DL, El-Harith A, Kraemer SA, et al. The aspirin and heme-
assay for clinical evaluation of biochemical efficacy of cyclooxygen- binding sites of ovine and murine prostaglandin endoperoxide syn-
ase inhibitors. Inflamm Res. 1996;45:68 –74. thases. J Biol Chem. 1990;265:5192–5198.
20. Lee M, Feldman M. Nonessential role of leukotrienes as mediators 35. Shimokawa T, Smith WL. Prostaglandin endoperoxide synthase.
of acute gastric mucosal injury induced by aspirin in rats. Dig Dis The aspirin acetylation regastrointestinalon. J Biol Chem. 1992;267:
Sci. 1992;37:1282–1287. 12387–12392.
21. Redfern JS, Lee E, Feldman M. Effect of indomethacin on gastric 36. Lecomte M, Laneuville O, Ji C, et al. Acetylation of human prosta-
mucosal prostaglandins in humans. Correlation with mucosal glandin endoperoxide synthase-2 (cyclooxygenase-2) by aspirin.
damage. Gastroenterology. 1987;92:969 –977. J Biol Chem. 1994;269:13207–13215.
22. Colton T. Statistics in Medicine. Boston, Mass: Little, Brown and 37. Cryer B, Goldschmiedt M, Redfern JS, Feldman M. Comparison of
Co.; 1974. salsalate and aspirin on mucosal injury and gastroduodenal muco-
23. Piper RM, Ray WA, Daugherty JR, Griffin MR. Corticosteroid use sal prostaglandins. Gastroenterology. 1990;99:1616 –1621.
and peptic ulcer disease: role of nonsteroidal anti-inflammatory 38. Graham DY, Smith JL, Holmes GI, Davies RO. Nonsteroidal anti-
drugs. Ann Intern Med. 1991;114:735–740. inflammatory effect of sulindac sulfoxide and sulfide on gastric mu-
24. Physicians’ Desk Reference. 51st ed. Montvale, NJ: Medical Econom- cosa. Clin Pharmacol Ther. 1985;38:65–70.
ics Co. 1997. 39. Henry D, Lim LL, Garcia-Rodriguez LA, et al. Variability in risk of
25. Insel PA. Analgesic-antipyretics and antiinflammatory agents: gastrointestinal complications with individual non-steroidal anti-
drugs employed in the treatment of rheumatoid arthritis and gout. inflammatory drugs: results of a collaborative meta-analysis. BMJ.
In: Gillman AG, Rall TW, Nies AS, Taylor P, eds. Goodman and 1996;312:1563–1566.
Gillman’s: The Pharmacological Basis of Therapeutics. 8th ed. New 40. Willkens RF. An overview of the long-term safety experience of
York: Pergamon Press; 1990:638 – 681. nabumetone. Drugs. 1990;40:34 –37.
26. Crook PR, Willis JV, Kendall MJ, et al. The pharmacokinetics of 41. Lanza F, Simon T, Quan H, et al. Selective inhibition of cyclooxy-
diclofenac sodium in patients with active rheumatoid disease. Eur genase-2 (COX-2) with MK-0966 (250 mg q.d.) is associated with
J Clin Pharmacol. 1982;21:331–334. less gastroduodenal damage than aspirin (ASA) 650 mg q.i.d. or
27. Small RE, Cox SR, Adams WJ. Influence of H2 receptor antagonists ibuprofen (IBU) 800 mg t.i.d. Gastroenterology. 1997;112:A194.
on the disposition of flurbiprofen enantiomers. J Clin Pharmacol. 42. Lanza FL, Rack MF, Callison DA, et al. A pilot endoscopic study of
1990;30:660 – 664. the gastroduodenal effects of SC-5835, a novel COX-2-selective in-
28. Davies EF, Avery GS. Ibuprofen: a review of its pharmacological hibitor. Gastroenterology. 1997;112:A194.
May 1998 THE AMERICAN JOURNAL OF MEDICINEt Volume 104 421
S-ar putea să vă placă și
- Comparative Pathophysiology and Toxicology of CyclooxygenasesDe la EverandComparative Pathophysiology and Toxicology of CyclooxygenasesÎncă nu există evaluări
- Clinical Pharmacology of Non Steroidal A20151118 17879 2qewjq WithDocument14 paginiClinical Pharmacology of Non Steroidal A20151118 17879 2qewjq WithAli KareemÎncă nu există evaluări
- Non-Steroidal Anti-Inflammatory Drugs ComparisonDocument10 paginiNon-Steroidal Anti-Inflammatory Drugs ComparisonMuchammad Karunia FadillahÎncă nu există evaluări
- The Special Case of Diclofenac: Gwenaëlle VEYRAC, Enliven: Pharmacovigilance and Drug SafetyDocument4 paginiThe Special Case of Diclofenac: Gwenaëlle VEYRAC, Enliven: Pharmacovigilance and Drug Safetyfriska masyitahÎncă nu există evaluări
- Selective Cox-2 Inhibitor: Visha.M.GDocument6 paginiSelective Cox-2 Inhibitor: Visha.M.GinventionjournalsÎncă nu există evaluări
- NSAIDsDocument2 paginiNSAIDsOm Prakash MishraÎncă nu există evaluări
- Drugs Used in OrthodonticsDocument143 paginiDrugs Used in OrthodonticsSweta SaravananÎncă nu există evaluări
- Pharmacology of ParecoxibDocument8 paginiPharmacology of ParecoxibLee June LyngÎncă nu există evaluări
- Anti Inflamasi (Nonsteroid)Document29 paginiAnti Inflamasi (Nonsteroid)Hariati KemelasariÎncă nu există evaluări
- Batlouni Introduação PDFDocument8 paginiBatlouni Introduação PDFEryclisNunesÎncă nu există evaluări
- Anti Inflammatory DrugsDocument82 paginiAnti Inflammatory DrugsShardendu MishraÎncă nu există evaluări
- Kharkov National Medical University Department of Pharmacology Lecture on Anti-inflammatory DrugsDocument82 paginiKharkov National Medical University Department of Pharmacology Lecture on Anti-inflammatory DrugsHerry HendrayadiÎncă nu există evaluări
- Indomethacin 392Document17 paginiIndomethacin 392Mahadie Hasan JahadÎncă nu există evaluări
- Piroxicamarticle PDFDocument7 paginiPiroxicamarticle PDFPriska FebiolaÎncă nu există evaluări
- Piroxicamarticle PDFDocument7 paginiPiroxicamarticle PDFPriska FebiolaÎncă nu există evaluări
- Piroxicam Article: Journal of Pharmacy Research April 2018Document7 paginiPiroxicam Article: Journal of Pharmacy Research April 2018Ulfah RahmanÎncă nu există evaluări
- Nonsteroidal Anti-Inflammatory Drugs in Animals - Pharmacology - MSD Veterinary ManualDocument12 paginiNonsteroidal Anti-Inflammatory Drugs in Animals - Pharmacology - MSD Veterinary ManualFairuz Nanda MarhabanazÎncă nu există evaluări
- NSAIDS ComparisonDocument60 paginiNSAIDS ComparisonsillymajorÎncă nu există evaluări
- Olanzapine-Induced Renal Damages and Metabolic Side Effects: The Protective Effects of ThymoquinoneDocument6 paginiOlanzapine-Induced Renal Damages and Metabolic Side Effects: The Protective Effects of ThymoquinonezainÎncă nu există evaluări
- 2019 NSAIDs and ParacetamolDocument53 pagini2019 NSAIDs and Paracetamolgowod86101Încă nu există evaluări
- PainoxiaDocument66 paginiPainoxiaOmar WahbiÎncă nu există evaluări
- NSAIDsDocument45 paginiNSAIDsAnamta AshfaqÎncă nu există evaluări
- Febuxostat (Uloric) - A Xanthine Oxidase Inhibitor - Aug 1, 2023Document24 paginiFebuxostat (Uloric) - A Xanthine Oxidase Inhibitor - Aug 1, 2023Ramdas BorhadeÎncă nu există evaluări
- 1 s2.0 S0753332222006424 MainDocument11 pagini1 s2.0 S0753332222006424 Mainlarissa dias freitasÎncă nu există evaluări
- NSAIDSDocument12 paginiNSAIDSNikita ShokurÎncă nu există evaluări
- Anti-Inflammatory Drugs Class Notes 2023Document82 paginiAnti-Inflammatory Drugs Class Notes 2023Jacob MasikaÎncă nu există evaluări
- DSG PKDocument14 paginiDSG PKJagdish ChanderÎncă nu există evaluări
- Presentation Nadi and DanyDocument7 paginiPresentation Nadi and DanyFadel AhdabÎncă nu există evaluări
- Antiinflammatorydrugs: Beatriz Monteiro,, Paulo V. SteagallDocument19 paginiAntiinflammatorydrugs: Beatriz Monteiro,, Paulo V. SteagallYohan Oropeza VergaraÎncă nu există evaluări
- Nardostachys jatamansi shows antioxidant effects against stressDocument6 paginiNardostachys jatamansi shows antioxidant effects against stressAmanda HoffmannÎncă nu există evaluări
- 2018 IJRPS Acetaminophen1Document7 pagini2018 IJRPS Acetaminophen1dvckpjuÎncă nu există evaluări
- NSAIDsDocument27 paginiNSAIDsshatz_014Încă nu există evaluări
- Antiinflammatory and Anti Diabetic ResultsDocument14 paginiAntiinflammatory and Anti Diabetic ResultsTota wa YassoÎncă nu există evaluări
- OtcDocument37 paginiOtcJoanne Ferrer100% (1)
- Xanthorrhizol Has A Potential To Attenuate The High Dose Cisplatin-Induced Nephrotoxicity in MiceDocument6 paginiXanthorrhizol Has A Potential To Attenuate The High Dose Cisplatin-Induced Nephrotoxicity in MiceFajri RifaldiÎncă nu există evaluări
- Nsid 1Document12 paginiNsid 1Afni Panggar BesiÎncă nu există evaluări
- NsaidDocument23 paginiNsaidArtika Tika ArtikaÎncă nu există evaluări
- Analgesic and Nsaids: Dr. Budhi Setiawan, M.Kes PharmacologyDocument24 paginiAnalgesic and Nsaids: Dr. Budhi Setiawan, M.Kes PharmacologyErwin BawonoÎncă nu există evaluări
- 10 Nonopioid Analgesics PDFDocument6 pagini10 Nonopioid Analgesics PDFRohit NaiduÎncă nu există evaluări
- Asam Salisilat Dalam UrinDocument6 paginiAsam Salisilat Dalam UrinChrisantusSuryaÎncă nu există evaluări
- Steroidal Anti - Inflammatory Drugs: NsaidsDocument96 paginiSteroidal Anti - Inflammatory Drugs: NsaidsDR AbidÎncă nu există evaluări
- Sedative EffectsDocument4 paginiSedative EffectsluispastenÎncă nu există evaluări
- NSAIDsDocument54 paginiNSAIDsAlaaÎncă nu există evaluări
- 4 5999270362695600886Document20 pagini4 5999270362695600886123Încă nu există evaluări
- Quercetin PankreasDocument7 paginiQuercetin PankreasAlmas TÎncă nu există evaluări
- COX-1 and COX-2 Inhibitory Activity in Extracts Prepared From Eucomis Species, With Further Reference To Extracts From E. Autumnalis AutumnalisDocument6 paginiCOX-1 and COX-2 Inhibitory Activity in Extracts Prepared From Eucomis Species, With Further Reference To Extracts From E. Autumnalis AutumnalisFatima RiveraÎncă nu există evaluări
- Final CPD PAIN MANAGEMENT LECTURE Edit 2Document57 paginiFinal CPD PAIN MANAGEMENT LECTURE Edit 2auliaÎncă nu există evaluări
- Study of Osteoarthritis Treatment With Anti-InflammatoryDocument11 paginiStudy of Osteoarthritis Treatment With Anti-InflammatoryDezha DetiroÎncă nu există evaluări
- Evolution of Nonsteroidal Anti-Inflammatory Drugs (Nsaids) : Cyclooxygenase (Cox) Inhibition and BeyondDocument30 paginiEvolution of Nonsteroidal Anti-Inflammatory Drugs (Nsaids) : Cyclooxygenase (Cox) Inhibition and BeyondnesakusumaÎncă nu există evaluări
- Iaft10i2p188 PDFDocument5 paginiIaft10i2p188 PDFVirgo Eri SendiÎncă nu există evaluări
- FlurbiprofenDocument18 paginiFlurbiprofenUmar ZulfiqarÎncă nu există evaluări
- Nonsteroidal Antiinflammatorydrugsfor Acuteandchronicpain: Timothy J. Atkinson,, Jeffrey FudinDocument13 paginiNonsteroidal Antiinflammatorydrugsfor Acuteandchronicpain: Timothy J. Atkinson,, Jeffrey FudinMaBe MejíaÎncă nu există evaluări
- Katzung & Trevor's Pharmacology Examination & Board Review-Pages-303-311Document9 paginiKatzung & Trevor's Pharmacology Examination & Board Review-Pages-303-311Princess Alyssa H. PasajolÎncă nu există evaluări
- Estudio 2Document5 paginiEstudio 2Gabriel GarridoÎncă nu există evaluări
- NSAID Mechanism and UsesDocument11 paginiNSAID Mechanism and UsesSuranjan GhoshÎncă nu există evaluări
- 18 Applied PharmacologyDocument88 pagini18 Applied Pharmacologyrajkamal kÎncă nu există evaluări
- Effects of Omega-3 Co-Administered With Therapeutic Dose of Lornoxicam On Male Rats' LiverDocument6 paginiEffects of Omega-3 Co-Administered With Therapeutic Dose of Lornoxicam On Male Rats' Livernhan phamÎncă nu există evaluări
- Non-Steroidal Anti Inflammatory Drugs (NSAIDS)Document5 paginiNon-Steroidal Anti Inflammatory Drugs (NSAIDS)Pardhasaradhi PantaÎncă nu există evaluări
- Anti Inflammatory Agents: Tishk International UniversityDocument13 paginiAnti Inflammatory Agents: Tishk International Universityhappy babyÎncă nu există evaluări
- Non Steroidal Anti Inflammatory DrugDocument21 paginiNon Steroidal Anti Inflammatory DrugRanganath NagarajÎncă nu există evaluări
- La Mitosis y Su Regulación Lectura 2Document14 paginiLa Mitosis y Su Regulación Lectura 2lililaÎncă nu există evaluări
- Adverse Cardiovascular Effects of Rofecoxib: CorrespondenceDocument3 paginiAdverse Cardiovascular Effects of Rofecoxib: CorrespondenceYariCárdenasÎncă nu există evaluări
- Drayna 2005Document23 paginiDrayna 2005YariCárdenasÎncă nu există evaluări
- Andropause: Current Concepts: Keywords: Androgen Deficiency in Ageing Male, Late Onset Hypogonadism, TestosteroneDocument14 paginiAndropause: Current Concepts: Keywords: Androgen Deficiency in Ageing Male, Late Onset Hypogonadism, TestosteroneYariCárdenasÎncă nu există evaluări
- Baron2008 002 PDFDocument9 paginiBaron2008 002 PDFYariCárdenasÎncă nu există evaluări
- Coxibs and Heart Disease: What We Have Learned and What Else We Need To KnowDocument14 paginiCoxibs and Heart Disease: What We Have Learned and What Else We Need To KnowYariCárdenasÎncă nu există evaluări
- Sistema Renina-AngiotensinaDocument10 paginiSistema Renina-AngiotensinaYariCárdenasÎncă nu există evaluări
- Sistema Renina-AngiotensinaDocument10 paginiSistema Renina-AngiotensinaYariCárdenasÎncă nu există evaluări
- Case 27: What Is The Response of The Kidney To Metabolic Acidosis?Document10 paginiCase 27: What Is The Response of The Kidney To Metabolic Acidosis?YariCárdenasÎncă nu există evaluări
- Cardiovascular Events Associated With Rofecoxib in A Colorectal Adenoma Chemoprevention TrialDocument11 paginiCardiovascular Events Associated With Rofecoxib in A Colorectal Adenoma Chemoprevention TrialYariCárdenasÎncă nu există evaluări
- Physiology and Pathophysiology of Cyclooxygenase-2 and Prostaglandin E2 in The KidneyDocument7 paginiPhysiology and Pathophysiology of Cyclooxygenase-2 and Prostaglandin E2 in The KidneyYariCárdenasÎncă nu există evaluări
- Coxibs and Heart Disease: What We Have Learned and What Else We Need To KnowDocument14 paginiCoxibs and Heart Disease: What We Have Learned and What Else We Need To KnowYariCárdenasÎncă nu există evaluări
- Bombardier2000 002 PDFDocument9 paginiBombardier2000 002 PDFYariCárdenasÎncă nu există evaluări
- COX-2 Expression in Atherosclerosis - The Good, The Bad or The UglyDocument12 paginiCOX-2 Expression in Atherosclerosis - The Good, The Bad or The UglyYariCárdenasÎncă nu există evaluări
- Ciclooxigenasa 1y 2 PDFDocument9 paginiCiclooxigenasa 1y 2 PDFYariCárdenasÎncă nu există evaluări
- Bombardier2000 002Document9 paginiBombardier2000 002YariCárdenasÎncă nu există evaluări
- Rofecoxib Case PDFDocument4 paginiRofecoxib Case PDFYariCárdenasÎncă nu există evaluări
- Cardiovascular Events Associated With Rofecoxib: Fi Nal Analysis of The Approve TrialDocument9 paginiCardiovascular Events Associated With Rofecoxib: Fi Nal Analysis of The Approve TrialYariCárdenasÎncă nu există evaluări
- Harrisons Principles of Internal Medicine, 19th EditionDocument22 paginiHarrisons Principles of Internal Medicine, 19th EditionTALBIYAH SABDAH RIZAN TAUPIQ -Încă nu există evaluări
- NSAID's QuestionsDocument3 paginiNSAID's QuestionsManikanta Guptha100% (2)
- Prostaglandins & COX Pathway OverviewDocument34 paginiProstaglandins & COX Pathway Overviewmirza_baig_46Încă nu există evaluări
- Draft Update Review Artikel Farmakologi Bawang Dayak 040423Document29 paginiDraft Update Review Artikel Farmakologi Bawang Dayak 040423Zuliar PermanaÎncă nu există evaluări
- Basics of Pharmacoeconomics and Outcomes ResearchDocument48 paginiBasics of Pharmacoeconomics and Outcomes ResearchArvind NagÎncă nu există evaluări
- Plants 11 00247 v2Document39 paginiPlants 11 00247 v2MOHAMMAD OVAISÎncă nu există evaluări
- Bursitis TrocanterDocument18 paginiBursitis TrocanterAngie Paola RodriguezÎncă nu există evaluări
- J.T (Mefenamic) Drug StudyDocument3 paginiJ.T (Mefenamic) Drug StudyAngelica Marie MacaslingÎncă nu există evaluări
- Kwatra 2017Document12 paginiKwatra 2017Daniel OctavianusÎncă nu există evaluări
- Antibiotics & Analgesics in Dentistry: Dr. Hala Helmi A. HazzaaDocument69 paginiAntibiotics & Analgesics in Dentistry: Dr. Hala Helmi A. HazzaaPuchka IndurÎncă nu există evaluări
- Common OPD DrugsDocument22 paginiCommon OPD DrugsAira Jhamaica DimacaleÎncă nu există evaluări
- Nimesulide Particle SizeDocument11 paginiNimesulide Particle Sizerodrigue yanÎncă nu există evaluări
- InflammatoryDocument20 paginiInflammatoryAS RifathÎncă nu există evaluări
- IJPAR - 14 - 613 - 55-66 Venkat Subba Reddy PDFDocument12 paginiIJPAR - 14 - 613 - 55-66 Venkat Subba Reddy PDFSriram NagarajanÎncă nu există evaluări
- Common Drugs With Effective Off-Label UsesDocument10 paginiCommon Drugs With Effective Off-Label Usesredwan_rnÎncă nu există evaluări
- 9 The Post Anesthesia Care UnitDocument77 pagini9 The Post Anesthesia Care Unitsanjivdas100% (1)
- Dolo 650 MG (Paracetamol) : Uses, Side Effects, DosageDocument3 paginiDolo 650 MG (Paracetamol) : Uses, Side Effects, DosageRaluca Elena Raluca ElenaÎncă nu există evaluări
- Acute Kidney Injury in Pregnancy and The Use of Non-Steroidal Anti-In Ammatory Drugs PDFDocument9 paginiAcute Kidney Injury in Pregnancy and The Use of Non-Steroidal Anti-In Ammatory Drugs PDFSai Khin Aung TintÎncă nu există evaluări
- Update Open Inguinal Hernia Repair PDFDocument86 paginiUpdate Open Inguinal Hernia Repair PDFBenny GunawanÎncă nu există evaluări
- Understanding The Pain and Its Management: Dr. Mohammad Shoaib D/o Ilaj-bit-Tadbeer, F/o Unani Medicine, A.M.U., AligarhDocument28 paginiUnderstanding The Pain and Its Management: Dr. Mohammad Shoaib D/o Ilaj-bit-Tadbeer, F/o Unani Medicine, A.M.U., AligarhDr SadiyaÎncă nu există evaluări
- Coxib 2Document4 paginiCoxib 2ras emil sazuraÎncă nu există evaluări
- Non-Steroidal Anti Inflammatory Drugs (NSAIDS)Document5 paginiNon-Steroidal Anti Inflammatory Drugs (NSAIDS)Pardhasaradhi PantaÎncă nu există evaluări
- Nonsteroidal Antiinflammatorydrugsfor Acuteandchronicpain: Timothy J. Atkinson,, Jeffrey FudinDocument13 paginiNonsteroidal Antiinflammatorydrugsfor Acuteandchronicpain: Timothy J. Atkinson,, Jeffrey FudinMaBe MejíaÎncă nu există evaluări
- NabumetoneDocument3 paginiNabumetoneJihaÎncă nu există evaluări
- Pharmacology in The Musculoskeletal System: Anwen S Williams and Rhian GoodfellowDocument6 paginiPharmacology in The Musculoskeletal System: Anwen S Williams and Rhian GoodfellowQuiropraxiayequilibrioÎncă nu există evaluări
- Practice Paper For MD1 2021 - AnswersDocument10 paginiPractice Paper For MD1 2021 - AnswersAlex TaylorÎncă nu există evaluări
- Biology WS AnswersDocument17 paginiBiology WS AnswersKazeÎncă nu există evaluări
- Biochemistry of InflamationDocument45 paginiBiochemistry of Inflamationmichot feleguÎncă nu există evaluări
- FeverDocument0 paginiFeverRegina SeptianiÎncă nu există evaluări
- Moore 2013Document11 paginiMoore 2013JulioRoblesZanelliÎncă nu există evaluări