Documente Academic
Documente Profesional
Documente Cultură
HHS Public Access
Încărcat de
Mahlina Nur LailiTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
HHS Public Access
Încărcat de
Mahlina Nur LailiDrepturi de autor:
Formate disponibile
HHS Public Access
Author manuscript
Am J Obstet Gynecol. Author manuscript; available in PMC 2016 March 01.
Author Manuscript
Published in final edited form as:
Am J Obstet Gynecol. 2015 March ; 212(3): 375.e1–375.e11. doi:10.1016/j.ajog.2014.09.020.
The effect of a very short interpregnancy interval and pregnancy
outcomes following a previous pregnancy loss
Luchin F. WONG, M.D.1,2, Karen C. SCHLIEP, Ph.D.3, Robert M. SILVER, M.D.1,2, Sunni L.
MUMFORD, Ph.D.3, Neil J. PERKINS, Ph.D.3, Aijun YE, Ph.D.3, Noya GALAI, Ph.D.7, Jean
WACTAWSKI-WENDE, Ph.D.4, Anne M. LYNCH, M.D.5, Janet M. TOWNSEND, M.D.6, David
FARAGGI, Ph.D.7, and Enrique F. SCHISTERMAN, Ph.D.3
Author Manuscript
1Department of Obstetrics and Gynecology, University of Utah, Salt Lake City, UT, United States
2Department of Maternal-Fetal Medicine, Intermountain Healthcare, Salt Lake City, UT, United
States
3Epidemiology Branch, Division of Intramural Population Health Research, Eunice Kennedy
Shriver National Institute of Child Health and Human Development, Bethesda, MD, United States
4Department of Epidemiology and Environmental Health, University at Buffalo, Buffalo, NY,
United States
5Department of Obstetrics and Gynecology, University of Colorado, Denver, CO, United States
6Department of Family, Community and Rural Health, Commonwealth Medical College, Scranton,
PA, United States
Author Manuscript
7Department of Statistics, University of Haifa, Haifa, Israel
Abstract
Objective—We sought to assess the relationship between a short interpregnancy interval (IPI)
following a pregnancy loss and subsequent live birth and pregnancy outcomes.
Study Design—A secondary analysis of women enrolled in the Effects of Aspirin in Gestation
and Reproduction trial with an hCG-positive pregnancy test and whose last reproductive outcome
was a loss were included in this analysis (n=677). IPI was defined as the time between last
pregnancy loss and last menstrual period of the current pregnancy and categorized by 3-month
intervals. Pregnancy outcomes include live birth, pregnancy loss, and any pregnancy
Author Manuscript
© 2014 Elsevier Inc. All rights reserved.
Corresponding author: Luchin F. Wong, University of Utah Department of Obstetrics and Gynecology, 30 North Medical Drive, Suite
2B200, Salt Lake City, UT 84132, 347-563-8330 (mobile) / 801-581-8425 (office) / 801-585-2594 (fax), luchin.wong@hsc.utah.edu.
Disclosure: The authors report no conflict of interest.
Presentation: This paper was presented in part as a poster at the Society for Maternal-Fetal Medicine 34th Annual Meeting, Hilton
New Orleans Riverside, New Orleans, Louisiana, USA, February 3–8, 2014 (final abstract ID# 412)
Reprints will not be available.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our
customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of
the resulting proof before it is published in its final citable form. Please note that during the production process errors may be
discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
WONG et al. Page 2
complications. These were compared between IPI groups using multivariate relative risk
Author Manuscript
estimation by Poisson regression.
Results—Demographic characteristics were similar between IPI groups. The mean gestational
age of prior pregnancy loss was 8.6 ± 2.8 weeks. The overall live birth rate was 76.5%, with
similar live birth rates between those with IPI ≤ 3 months as compared to IPI > 3 months,
aRR=1.07 (95% CI 0.98–1.16). Rates were also similar for peri-implantation loss (aRR=0.95; 95%
CI 0.51–1.80), clinically confirmed loss, (aRR=0.75; 95% CI 0.51–1.10), and any pregnancy
complication (aRR=0.88; 95% CI 0.71–1.09) for those with IPI ≤ 3 months as compared to IPI > 3
months.
Conclusion—Live birth rates and adverse pregnancy outcomes, including pregnancy loss, were
not associated with a very short IPI after a prior pregnancy loss. The traditional recommendation
to wait at least 3 months after a pregnancy loss before attempting a new pregnancy may not be
warranted.
Author Manuscript
Keywords
interpregnancy interval; miscarriage; pregnancy loss; pregnancy outcomes; spontaneous abortion
Introduction
Pregnancy loss is the most frequent complication of early pregnancy (most commonly
occurring prior to 10 weeks gestation) and affects approximately 12–15% of clinically
recognized pregnancies.1,2 After a pregnancy loss, couples often seek counseling on how
long they should wait before attempting to conceive. The length of delay is of particular
concern for women who may be sub-fertile or who are over 35 years of age.
Author Manuscript
Most studies addressing interpregnancy interval (IPI) concentrate on the interval between
live births and subsequent pregnancies. There is considerable evidence that an IPI less than
18 months after a term or preterm delivery is associated with an increased risk for poor
maternal and perinatal outcome.3–6 However, there is significant controversy as to what the
optimal timing is for the next pregnancy following a pregnancy loss.
It is common practice for obstetricians to recommend waiting at least 3 months before
attempting a new pregnancy after an early pregnancy loss,7 while the World Health
Organization (WHO) recommends a minimum IPI of at least 6 months after a spontaneous
or elective abortion.8,9 However, there are few data to support these recommendations and
contemporary studies demonstrate an inverse relationship between the rate of live birth and
increasing IPI.10–13 Furthermore, published studies consist mostly of retrospective studies
Author Manuscript
without uniformity in documentation of gestational age and outcomes, and the majority do
not address very short IPI (less than 3 months).9–12 Thus, our primary objective was to
assess the relationship between the interval between pregnancy loss and subsequent live
birth in a large cohort of women, recruited from multiple clinical centers in the United
States, who were actively trying to conceive following a pregnancy loss. Our secondary
objective was explore the relationship between IPI and subsequent pregnancy complications
Am J Obstet Gynecol. Author manuscript; available in PMC 2016 March 01.
WONG et al. Page 3
including peri-implantation and clinical loss, preterm birth, preeclampsia, and gestational
Author Manuscript
diabetes.
Materials and Methods
This study is a secondary data analysis of women enrolled in the Effects of Aspirin in
Gestation and Reproduction (EAGeR) trial. The EAGeR trial, a block-randomized, multi-
center, double-blinded, placebo-controlled trial of preconception low-dose aspirin or
placebo, enrolled 1228 women, aged 18–40, with a history of one to two pregnancy losses.
Details of the study design and protocol have been published previously.14 Women were
stratified by eligibility criteria. The “original” eligibility stratum, included women actively
trying to conceive with a history of only one prior pregnancy loss at <20 weeks’ gestation
during the past year, up to one prior live birth, up to one elective termination/ectopic
pregnancy, regular menstrual cycles of 21–42 days in length during the preceding 12
Author Manuscript
months, no history of diagnosed or treated infertility and aged 18 to 40 years. Women in the
“expanded” stratum included women who had one or two pregnancy losses, including those
at >20 weeks’ gestation, with pregnancy losses occurring more than one year prior to
enrollment, and with up to two prior live births. All other criteria were identical between the
two strata. Of note, 14 women withdrew immediately following randomization and were
excluded from further analysis because they contributed no observed follow-up time.
The trial was conducted at four clinical sites in the United States with recruitment between
2007 and 2011. Women were followed for up to six menstrual cycles while trying to
conceive and through delivery if they became pregnant. The study was approved by the
Institutional Review Board (IRB) at each site, with each site serving as the IRB designated
by the National Institutes of Health under a reliance agreement. All participants gave written
Author Manuscript
informed consent prior to randomization.
Medical records were obtained documenting at least one of the up to two prior pregnancy
losses with hCG, ultrasound, and/or histology. Each woman underwent an extensive
questionnaire at baseline regarding her medical and obstetric history. Medical records were
abstracted by trained study personnel. The majority of women (n=653, 96.5%) had a
medically documented date of last loss. For the remaining 24 women (3.5%), we relied on
their self-reported date of last loss. Similarly, the majority of women (n=589, 87.0%) had a
medically documented gestational age of last loss, with an additional 86 women having a
self-reported gestational age of loss.
Data for this study assessing interpregnancy interval and pregnancy outcomes were limited
to women whose last reproductive outcome was a pregnancy loss (n=1074/1214, 88.5%) and
Author Manuscript
subsequently became pregnant (n=677/1214, 55.8%). Pregnancy was ascertained by a urine
pregnancy test (clinic and/or home with the majority [89%] having both) and confirmed by a
6–7 week ultrasound. IPI was defined as the time between previous loss and the last
menstrual period of the confirmed pregnancy. IPI was categorized by 3-month intervals (0 to
3 months, > 3 to 6 months, > 6 to 9 months, > 9 to 12 months, and > 12 months).
Am J Obstet Gynecol. Author manuscript; available in PMC 2016 March 01.
WONG et al. Page 4
The primary outcome was live birth. Secondary outcomes included pregnancy loss, types of
Author Manuscript
pregnancy loss,15 and obstetric complications (preeclampsia, gestational diabetes, and
preterm birth < 37 weeks). Peri-implantation loss was defined as a pregnancy loss before 5
weeks with no gestational sac visible on ultrasound. Pre-embryonic loss was defined as a
pregnancy loss at 5 0/7 to 5 6/7 weeks with visible gestational sac and/or yolk sac, but no
visible embryo on ultrasound. Embryonic loss was defined as a pregnancy loss at 6 0/7 to 9
6/7 weeks of an embryo with crown rump length (CRL) < 10mm and no visible cardiac
activity on ultrasound. Fetal loss was defined as a pregnancy loss at 10 0/7- 19 6/7 weeks
with documented fetal cardiac activity at or beyond 10 weeks (CRL ≥ 30mm) or passage of
conceptus with CRL measuring at least 30mm. Stillbirth was defined as a pregnancy loss of
a fetus at ≥ 20 weeks gestation without signs of life at the time of delivery. Clinically
confirmed loss was defined as any stillbirth, preembryonic, embryonic, fetal loss, or other
(including ectopic pregnancy). Preeclampsia was defined as having a systolic pressure ≥ 140
Author Manuscript
mmHg and/or diastolic pressure ≥ 90 mmHg that does not antedate the pregnancy and
presents after 20 weeks gestation on ≥ 2 occasions at least 4 hours apart and proteinuria ≥
0.3 grams in a 24-hour urine specimen or 1+ on dipstick.16 Preterm birth was defined as any
delivery prior to 37 weeks (including spontaneous and medically indicated preterm births).
Participant demographic, lifestyle, and reproductive history characteristics between IPI
intervals were compared using chi-squared or where appropriate Fisher’s exact test for
categorical variables, and ANOVA for continuous variables. Multivariable Poisson
regression with robust error variance (to correctly estimate the standard error) was used to
assess the relative risk (RR) of live birth, peri-implantation loss, clinical loss, or pregnancy
complication by IPI category (0–3, > 6–9, > 9–12, and > 12 versus reference of > 3–6
months; and ≤ 3 months versus reference of > 3 months).17,18 Models adjusted for potential
confounders that were selected a priori and included factors known to be associated with IPI
Author Manuscript
and pregnancy or live birth success, and not on the causal pathway. Final models were
adjusted for maternal age, race, BMI, eligibility stratum, and gestational age of last loss. We
compared results to models that additionally adjusted for self-reported months trying to
achieve most recent pregnancy to adjust for potential undiagnosed and untreated subfertility.
We conducted several sensitivity analyses including additionally adjusting for treatment
group (e.g., aspirin or placebo), intercourse frequency in the prior 12 months, and additional
demographic, lifestyle or reproductive history characteristics. As much of the literature
makes comparisons between an IPI of ≤ 6 months versus a longer IPI, we also estimated the
relative risks for live birth, pregnancy loss, and any pregnancy complication for women with
an IPI ≤ 6 months versus > 6 months along with assessing differences in very short IPI (0–1,
> 1–2, and > 2–3 months).
Author Manuscript
Results
Of the 677 women who became pregnant and whose last reproductive outcome was a
pregnancy loss, 2.7% of women became pregnant within the first month, 33.2% became
pregnant within 3 months and 65.7% became pregnant within 6 months. The median IPI was
4.3 months (inter-quartile range [IQR]: 2.6–7.4 months) and the median time from most
recent pregnancy loss to study entry was 13.8 weeks (IQR: 7.4–31.0 weeks). There were no
Am J Obstet Gynecol. Author manuscript; available in PMC 2016 March 01.
WONG et al. Page 5
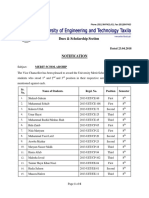
significant differences among IPI categories for demographic and lifestyle characteristics
Author Manuscript
(Table 1).
All women had a previous pregnancy loss prior to 19 weeks, with a mean gestational age of
loss at 8.6 ± 2.8 weeks (range 2–19 weeks). Thirty-five women (5.2%) had a previous
pregnancy loss between 14 and 19 weeks. Reproductive histories stratified by IPI group are
shown in Table 1. Rates of dilation and curettage in the previous pregnancy were similar for
the different IPI groups. The number of previous pregnancy losses was similar among IPI ≤
3 months versus > 3 months as well as individual 3 month IPI groups. Groups differed
slightly regarding prior live births with relatively fewer nulliparous women with an IPI < 3
months.
The overall live birth rate in our cohort was 76.5% (518/677). Live birth rates for IPI ≤ 3
months versus > 3 months were 80.4% (181/225) and 74.6% (337/452), respectively (Table
Author Manuscript
2). After adjustment for age, race, BMI, eligibility criteria, gestational age of previous loss,
and months tried to conceive for most recent pregnancy, there was no significant difference
in rate of achieving a live birth for IPI ≤ 3 months as compared to > 3 months, aRR=1.07
(95% CI, 0.98–1.16) (illustrated in Figure 1). A finer breakdown of IPI categories by 3-
month intervals demonstrated highest live birth rates for the 0–3 month IPI (80.4%) with the
lowest occurring in the > 12 month IPI group (65.0%). However, there were no statistically
significant differences in live birth rates between 0–3, > 6–9, > 9–12, and > 12 month IPI
groups compared to the reference of > 3–6 months. Live birth rates remained similar when
the 0–3 month IPI group was further broken down by one month intervals, with 83.3%,
85.9% and 76.2% achieving a live birth for 0–1 month, > 1–2 month, and > 2–3 month IPI
groups respectively.
Author Manuscript
The average gestational age of a pregnancy loss that occurred during the trial was 9.9 ± 4.1
wks (Table 3). The most common type of loss was embryonic (53.4%) followed by pre-
embryonic (27.1%), fetal (6.8%), and stillbirths (3.0%). These were similar for the different
IPI groups compared to the reference of > 3–6 months, with the exception of a greater risk
for peri-implantation failure among women with an IPI > 12 versus > 3–6 month IPI
(aRR=3.70, [95% CI: 1.49–9.19]) after adjusting for age, race, BMI, eligibility criteria,
gestational age of prior loss, and months tried to conceive for most recent pregnancy (Table
4). The risk of a clinically confirmed loss, however, remained similar between the different
3-month IPI groups.
For this study of EAGeR women whose last outcome was a pregnancy loss, 9.0% had
preeclampsia, 3.1% had gestational diabetes, and 8.1% had preterm birth among those
achieving a live birth. The unadjusted and adjusted risks for preeclampsia, gestational
Author Manuscript
diabetes, and preterm birth did not differ for IPI ≤ 3 months as compared to IPI > 3 months
nor across 3-month IPI groups (data not shown). Similarly, the risk for any pregnancy
complication was similar across 3-month IPI groups.
Inclusion of either treatment group (e.g., aspirin or placebo) or the intercourse frequency in
the prior 12 months did not appreciably alter the effect measures (Supplementary Tables 1
and 2) nor did adjustment for additional demographic, lifestyle or reproductive history
Am J Obstet Gynecol. Author manuscript; available in PMC 2016 March 01.
WONG et al. Page 6
characteristics. For women with an IPI ≤ 6 months versus > 6 months, we found similar
Author Manuscript
relative risks for live birth, pregnancy loss, and any pregnancy complication (Figure 2).
Comment
Women conceiving within 3 months of their last pregnancy loss had similar live birth rates
and rates of obstetric complications as those who conceived ≥ 3 months from their last
pregnancy loss. This study is unique in that it includes women with very short IPIs of less
than 3 months with the added strength that participants were enrolled preconceptionally and
followed closely while trying to conceive.
Current guidelines from the WHO recommend a minimum IPI of at least 6 months after a
spontaneous or elective abortion.8 This recommendation is based on one retrospective study
of 258,108 Latin American women who had a previous abortion (spontaneous and
Author Manuscript
induced).9 They reported greater rates of adverse obstetric outcomes (including low birth
weight <2500g, preterm delivery <37, and premature rupture of membranes) for those with a
post-abortion IPI of 0–2 and 3–5 months as compared to women with a post-abortion IPI of
18–23 months. While this is the largest study of its kind, findings from this study should be
interpreted with caution given that no distinction was made between spontaneous and
induced abortion. This was done in part because of the stigma and illegality associated with
induced abortion.9 Furthermore, because of the illegality of induced abortion in Latin
America, it may be assumed that safe abortions were not available to these women at the
time of the study.
Subsequent contemporary studies on women with one or more spontaneous abortions
suggest reproductive outcomes are best for an IPI less than 6 months, with an inverse
relationship between live birth rate and increasing IPI.10–13 Love et al reported decreasing
Author Manuscript
live birth rates of 85.2%, 77.8%, and 73.3% with increasing IPI of <6 months, 12–18
months, and > 24 months respectively among Scottish women who had a spontaneous
abortion in their first pregnancy.10 These results are consistent with a recent prospective
study of 4,619 Egyptian women with a history of spontaneous abortion in their first
pregnancy.13 El Behery and colleagues noted that women who conceived within 6 months
were twice as likely to have a live birth as compared to those who conceived over 12 months
after their first spontaneous abortion.13
Although these studies provide evidence that reproductive outcomes, particularly live birth
rates, are better for an IPI less than 6 months after a spontaneous abortion, they do not focus
on whether an interval of at least 3 months is necessary to optimize outcomes. Only one
study in an industrialized country has reported pregnancy outcomes for IPI ≤ 3 months.11
Author Manuscript
This was a limited secondary analysis of retrospectively collected data for 325 Israeli
women, finding no significant differences in pregnancy loss rates for IPI ≤ 3 months as
compared to IPI 3–6 months and > 6 months.11
Women with a longer IPI in our study tended to have lower (though non-significant) rates of
live births and increased peri-implantation losses, a pattern also reported in other
studies.10,12 Unlike these studies, the women with a longer IPI within our study were not
significantly older, nor were they more likely to be smokers, or alcohol consumers.
Am J Obstet Gynecol. Author manuscript; available in PMC 2016 March 01.
WONG et al. Page 7
However, we found that these women were more likely to be nulliparous. It is possible that
Author Manuscript
women with a longer IPI are more likely to have an unidentified underlying condition
causing delayed conception and adverse pregnancy outcomes such as infertility or sub-
fertility.
Because much of the literature makes comparisons between an IPI of ≤ 6 months versus a
longer IPI, we also estimated the relative risks for live birth, pregnancy loss, and any
pregnancy complication for women with an IPI ≤ 6 months versus > 6 months and found no
significant difference. However, these results should be interpreted with some qualifications,
since our cohort consisted of women actively trying to achieve pregnancy (only 34.3% of
our cohort had an IPI > 6 months) while other studies primarily investigated IPIs of longer
duration and used different IPI for their reference groups.
There are few studies examining adverse perinatal outcomes and IPI after a prior pregnancy
Author Manuscript
loss. El Behery et al identified a lower rate of preeclampsia and preterm birth < 36 weeks for
women with IPI less than 6 months as compared to women with IPI greater than 12
months.13 Love and colleagues noted a higher risk for PTB < 36 weeks among those with
IPI greater than 24 months as compared to shorter IPI.10 While our study did not identify an
association between varying IPI intervals and preterm birth or preeclampsia, we were
limited in the numbers of obstetric complications to make definitive conclusions regarding
these outcomes.
Our study had several limitations. First, as a secondary analysis, the trial was not primarily
designed and powered to examine live birth incidence and adverse pregnancy outcomes
associated with IPI. Second, not all women were enrolled in the study immediately after
their pregnancy loss. Accordingly we lack some data regarding whether women were trying
Author Manuscript
to conceive and on sub-clinical pregnancy loss in the months between their last loss and
enrollment in the EAGeR trial. This bias, however, was likely reduced by the fact that the
median delay between the most recent pregnancy loss and study entry was 11.9 weeks.
Furthermore, including the duration couples tried to conceive for the most recent pregnancy
as a marker of potential undiagnosed subfertility within our multivariate models did not alter
our findings. Results also remained robust even after additional consideration of intercourse
frequency within the year prior to study enrollment and the time interval from last
pregnancy loss to time the couple began to attempt conception. Nevertheless, a future study
that is designed and powered to assess differences in pregnancy outcomes by IPI, enrolling
and prospectively following women right after their loss through pregnancy outcome, is
recommended.
There were also numerous strengths of the study. Most importantly, all participants were
Author Manuscript
actively trying to conceive and were closely monitored for evidence of early pregnancy loss
using home and clinic pregnancy tests and early first trimester sonogram. Such studies are
difficult to conduct and as a consequence have been rare. Second, the timing and details of
prior losses were carefully and objectively documented. Third, the study was prospective,
allowing for early and accurate gestational dating, as well as characterization of the type of
pregnancy loss. Finally, there were a large number of participants with a range of IPIs
including over 200 women who became pregnant less than 3 months after a pregnancy loss.
Am J Obstet Gynecol. Author manuscript; available in PMC 2016 March 01.
WONG et al. Page 8
Traditional recommendations are to delay conception for 3 months following early
Author Manuscript
pregnancy loss.7 These recommendations stem from theoretical concerns regarding
normalization of hormone levels rather than clear scientific evidence. Pregnancy loss is an
emotionally distressing event and attempting to conceive again is often the only thing that
makes couples who have experienced a loss feel better.19 In addition, some women have
medical reasons to avoid delays in becoming pregnant such as advanced maternal age,
optimal windows with regard to chronic medical problems, or infertility. Our study suggests
that IPI ≤ 3 months is not associated with a lower rate of live birth, and appears to be
comparable to those with an IPI > 3 months. Similarly, longer IPI after a prior loss does not
appear to be associated with decreased rates of pregnancy loss, preterm birth, or
preeclampsia. Thus, reevaluation of the traditional recommendation for women with a prior
pregnancy loss to wait at least 3 months before attempting conception after a prior loss is
warranted.
Author Manuscript
Supplementary Material
Refer to Web version on PubMed Central for supplementary material.
Acknowledgments
Sources of Financial Support: This research was supported by the Intramural Research Program of the Eunice
Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health,
Bethesda, Maryland (Contract Nos. HHSN267200603423, HHSN267200603424, HHSN267200603426).
References
1. Rai R, Regan L. Recurrent miscarriage. Lancet. 2006; 368:601–611. [PubMed: 16905025]
2. Wilcox AJ, Weinberg CR, O’Connor JF, et al. Incidence of early loss of pregnancy. N Engl J Med.
Author Manuscript
1988; 319:189. [PubMed: 3393170]
3. Zhu BP, Rolfs RT, Nangle BE, Horan JM. Effect of the interval between pregnancies on perinatal
outcomes. N Engl J Med. 1999; 340:589. [PubMed: 10029642]
4. Fuentes-Afflick E, Hessol NA. Interpregnancy interval and the risk of premature infants. Obstet
Gynecol. 2000; 95:383–90. [PubMed: 10711549]
5. Zhu BP, Haines KM, Le T, McGrath-Miller K, Boulton ML. Effect of the interval between
pregnancies on perinatal outcomes among white and black women. Am J Obstet Gynecol. 2001;
185:1403–10. [PubMed: 11744916]
6. Conde-Agudelo A, Rosas-Bermudez A, Kafury-Goeta AC. Birth spacing and risk of adverse
perinatal outcomes – a metaanalysis. JAMA. 2006; 295:1809–23. [PubMed: 16622143]
7. Katz, VL. Spontaneous and recurrent abortion: etiology, diagnosis, treatment. In: Katz, VL., editor.
Comprehensive Gynecology. 5. Philadelphia, PA: Elsevier Inc; 2007. p. 381
8. World Health Organization. [Accessed May 22, 2014] Report of a WHO technical consultation on
birth spacing. 2005. http://www.who.int/maternal_child_adolescent/documents/birth_spacing.pdf
Author Manuscript
9. Conde-Agudelo A, Belizan JM, Breman R, Brockman SC, Rosas-Bermudez A. Effect of the
interpregnancy interval after an abortion on maternal and perinatal health in Latin America. Int J
Gynaecol Obstet. 2005; 89(Suppl 1):S34–40. [PubMed: 15820366]
10. Love ER, Bhattacharya S, Smith NC, Bhattacharya S. Effect of interpregnancy interval on
outcomes of pregnancy after miscarriage: retrospective analysis of hospital episode statistics in
Scotland. BMJ. 2010; 341:c3967. [PubMed: 20688842]
11. Bentolila Y, Ratzon R, Shoham-Vardi I, Serjienko R, Mazor M, Bashiri A. Effect of
interpregnancy interval on outcomes of pregnancy after recurrent pregnancy loss. J Matern Fetal
Neonatal Med. 2013; 26:1459–64. [PubMed: 23488821]
Am J Obstet Gynecol. Author manuscript; available in PMC 2016 March 01.
WONG et al. Page 9
12. DaVanzo J, Hale L, Rahman M. How long after a miscarriage should women wait before
becoming pregnant again? Multivariate analysis of cohort data from Matlab, Bangladesh. BMJ
Author Manuscript
Open. 2012; 2 pii: e001591.
13. El Behery MM, Siam S, Seksaka MA, Ibrahim ZM. Reproductive performance in the next
pregnancy for nulliparous women with history of first trimester spontaneous abortion. Arch
Gynecol Obstet. 2013; 288:939–44. [PubMed: 23564054]
14. Schisterman EF, Silver RM, Perkins NJ, et al. A randomised trial to evaluate the effects of low-
dose aspirin in gestation and reproduction: design and baseline characteristics. Paediatr Perinat
Epidemiol. 2013; 27:598–609. [PubMed: 24118062]
15. Silver RM, Branch DW, Goldenberg R, Iams JD, Klebanoff MA. Nomenclature for pregnancy
outcomes: time for a change. Obstet Gynecol. 2011; 118:1402–8. [PubMed: 22105271]
16. American College of Obstetricians and Gynecologists. Hypertension in pregnancy: Report of the
American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy.
Obstet Gynecol. 2013; 122:1122–31. [PubMed: 24150027]
17. Zou G. A Modified Poisson Regression Approach to Prospective Studies with Binary Data. Am J
Epidemiol. 2004; 159:702–6. [PubMed: 15033648]
Author Manuscript
18. Spiegelman D. und Hertzmark, Easy SAS Calculations for Risk or Prevalence Ratios and
Differences. E Am J Epidemiol. 2005; 162:199–205.
19. Cuisinier M, Janssen H, De Graauw C, Bakker S, Hoogduin C. Pregnancy following miscarriage:
course of grief and some determining factors. J Psychosom Obstet Gynecol. 1996; 17:168–74.
Author Manuscript
Author Manuscript
Am J Obstet Gynecol. Author manuscript; available in PMC 2016 March 01.
WONG et al. Page 10
Author Manuscript
Author Manuscript
Figure 1. Pregnancy outcomes for women with an interpregnancy interval ≤ 3 months versus > 3
months
1 Adjusted for age, race, BMI, eligibility criteria, gestational age of prior loss, and months
tried to conceive for most recent pregnancy.
Author Manuscript
Author Manuscript
Am J Obstet Gynecol. Author manuscript; available in PMC 2016 March 01.
WONG et al. Page 11
Author Manuscript
Author Manuscript
Figure 2. Pregnancy outcomes for women with an interpregnancy interval ≤ 6 months versus > 6
months
1 Adjusted for age, race, BMI, eligibility criteria, gestational age of prior loss, and months
tried to conceive for most recent pregnancy.
Author Manuscript
Author Manuscript
Am J Obstet Gynecol. Author manuscript; available in PMC 2016 March 01.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript
Table 1
Demographic, lifestyle, and reproductive history by interpregnancy interval
Interpregnancy interval
Characteristics
WONG et al.
Total n=677 0–3mo (n = 225) 3–6mo (n = 220) 6–9mo (n = 118) 9–12mo (n = 37) >12 mo (n = 77) P-value
33.2% 32.5% 17.4% 5.5% 11.4%
Demographics & Lifestyle
Age (mean ± SD) 28.6 ± 4.6 28.5 ± 4.4 28.9 ± 4.8 28.4 ± 4.6 28.8 ± 5.0 28.5 ± 4.6 0.84
BMI (mean ± SD) 25.4 ± 6.1 25.1 ± 5.8 25 ± 6.3 25.9 ± 5.7 25.6 ± 6.3 26.6 ± 7.0 0.30
Race (n [%]) 0.21
White 657 (97.0) 218 (96.9) 216 (98.2) 116 (98.3) 35 (94.6) 72 (93.5)
Non-White 20 (3.0) 7 (3.1) 4 (1.8) 2 (1.7) 2 (5.4) 5 (6.5)
Education (n [%]) 0.12
> High School 607 (90.0) 201 (89.3) 204 (92.7) 107 (90.7) 31 (83.8) 64 (83.1)
≤ High School 70 (10.3) 24 (10.7) 16 (7.3) 11 (9.3) 6 (16.2) 13 (16.9)
LDA Treatment (n [%]) 351 (51.9) 118 (52.4) 114 (51.8) 56 (47.5) 19 (51.4) 44 (57.1) 0.77
Smoking in past year (n [%]) 0.81
Never 604 (89.8) 206 (92.4) 193 (88.1) 106 (90.6) 33 (89.2) 66 (85.7)
Sometimes (<6 times/week) 48 (7.1) 13 (5.8) 18 (8.2) 7 (6) 3 (8.1) 7 (9.1)
Daily 21 (3.1) 4 (1.8) 8 (3.7) 4 (3.4) 1 (2.7) 4 (5.2)
Alcohol consumption in past year (n [%]) 0.35
Never 454 (67.8) 160 (71.4) 139 (64.1) 82 (70.1) 21 (58.3) 52 (68.4)
Sometimes 199 (29.7) 62 (27.7) 69 (31.8) 31 (26.5) 14 (38.9) 23 (30.3)
Often 17 (2.5) 2 (0.9) 9 (4.2) 4 (3.4) 1 (2.8) 1 (1.3)
Physical Activity (n [%]) 1.00
Am J Obstet Gynecol. Author manuscript; available in PMC 2016 March 01.
Low 171 (25.3) 60 (26.7) 53 (24.1) 31 (26.3) 10 (27.0) 17 (22.1)
Moderate 287 (42.4) 94 (41.8) 93 (42.3) 50 (42.4) 15 (40.5) 35 (45.5)
High 219 (32.4) 71 (31.6) 74 (33.6) 37 (31.4) 12 (32.4) 25 (32.5)
Reproductive History
Previous Live Births (n [%]) 0.01
0 304 (44.9) 82 (36.4) 93 (42.3) 63 (53.4) 22 (59.5) 44 (57.1)
1 260 (38.4) 104 (46.2) 84 (38.2) 40 (33.9) 10 (27.0) 22 (28.6)
2 113 (16.7) 39 (17.3) 43 (19.6) 15 (12.7) 5 (13.5) 11 (14.3)
Page 12
Author Manuscript Author Manuscript Author Manuscript Author Manuscript
Interpregnancy interval
Characteristics Total n=677 0–3mo (n = 225) 3–6mo (n = 220) 6–9mo (n = 118) 9–12mo (n = 37) >12 mo (n = 77) P-value
33.2% 32.5% 17.4% 5.5% 11.4%
Number of Previous Pregnancy Losses (n [%]) 0.72
1 436 (64.4) 147 (65.3) 144 (65.5) 74 (62.7) 26 (70.3) 45 (58.4)
WONG et al.
2 241 (35.6) 78 (34.7) 76 (34.6) 44 (37.3) 11 (29.7) 32 (41.6)
Gestational agea of previous loss (n[%]) 0.05
< 8 weeks 293 (43.4) 101 (45.1) 92 (41.8) 44 (37.3) 17 (46.0) 39 (51.3)
8–13 weeks 347 (51.4) 118 (52.7) 112 (50.9) 67 (56.8) 20 (54.1) 30 (39.5)
14–19 weeks 35 (5.2) 5 (2.2) 16 (7.3) 7 (5.9) 0 (0.0) 7 (9.2)
Gestational age of prior lossb 8.6 ± 2.8 8.3 ± 2.5 8.7 ± 3 9.2 ± 3 8.1 ± 2.4 8.2 ± 3.1 0.07
D & C performed on prior loss (n [%]) 230 (34.0) 77 (34.2) 75 (34.1) 44 (37.3) 13 (35.1) 21 (27.3) 0.71
Eligibility criteria (n [%]) <0.001
Original 344 (50.8) 118 (52.4) 119 (54.1) 67 (56.8) 22 (59.5) 18 (23.4)
Expanded 333 (49.2) 107 (47.6) 101 (45.9) 51 (43.2) 15 (40.5) 59 (76.6)
Months trying for most recent pregnancy (mean ± SD) 4.3 ± 4.9 3.6 ± 4.6 3.9 ± 3.9 4.4 ± 4.2 5.8 ± 6 6.8 ± 7.3 <0.001
Ever tried for more than 12 months to become pregnant (n [%]) 31 (4.7) 7 (3.1) 7 (3.2) 6 (5.1) 2 (5.7) 9 (12.2) 0.01
Intercourse in the past 12 months (n [%]) 0.44
3–6 times/week or more 226 (34.0) 78 (35.3) 74 (34.4) 35 (29.9) 11 (30.6) 28 (36.8)
1–2 times/week 329 (49.5) 106 (48) 109 (50.7) 62 (53) 22 (61.1) 30 (39.5)
2–3 times/month or less 110 (16.5) 37 (16.7) 32 (14.9) 20 (17.1) 3 (8.3) 18 (23.7)
Analyses performed via chi-square or Fisher’s exact test for categorical variables and analysis of variance or Kruskel-Walis for continuous variables. Study population includes women with one to two
previous pregnancy losses enrolled in the EAGeR trial (2007–2011), whose last reproductive outcome was a pregnancy loss and subsequently became pregnant (n=677).
a
n=675; 589 documented (continuous) and 86 self-report (categorical <8 weeks, 8–13 weeks, and 14–19 weeks).
Am J Obstet Gynecol. Author manuscript; available in PMC 2016 March 01.
b
n=589 with documented loss recorded continuously (self-report assessed categorically <8 weeks, 8–13 weeks, and 14–19 weeks).
Page 13
Author Manuscript Author Manuscript Author Manuscript Author Manuscript
Table 2
Incidence of achieving live birth according to interpregnancy interval (n=677 women)
Relative Risk (95% Confidence Interval)
WONG et al.
Interpregnancy interval Live Birth/Total n (%) Model 1 P-valuea Model 2 P-valueb
0–3 mo 181/225 (80.4) 1.1 (1–1.2) 0.32 1.0 (0.9–1.2) 0.37
3–6mo 168/220 (76.4) REF na REF na
6–9mo 91/118 (77.1) 1.0 (0.9–1.1) 0.86 1.0 (0.9–1.1) 0.86
9–12mo 28/37 (75.7) 1.0 (0.8–1.2) 0.95 1.0 (0.8–1.2) 0.95
>12mo 50/77 (64.9) 0.9 (0.7–1.0) 0.09 0.9 (0.7–1.1) 0.09
≤ 3 months vs. >3 months 181/225 (80.4) vs. 337/452 (74.6) 1.1 (1.0–1.2) 0.09 1.1 (1.0–1.2) 0.15
Analyses performed via multivariate relative risk (RR) estimation by Poisson regression with robust error variance. Study population includes women with one to two previous pregnancy losses enrolled in
the EAGeR trial (2007–2011), whose last reproductive outcome was a pregnancy loss and subsequently became pregnant (n=677).
a
Model 1: Adjusted for age, race, BMI, eligibility criteria, and gestational age of prior loss.
b
Model 2: Adjusted for age, race, BMI, eligibility criteria, gestational age of prior loss, and months tried to conceive for most recent pregnancy.
Am J Obstet Gynecol. Author manuscript; available in PMC 2016 March 01.
Page 14
Author Manuscript Author Manuscript Author Manuscript Author Manuscript
Table 3
Secondary obstetric outcomes according to interpregnancy interval (n=677 women)
Interpregnancy interval
Characteristics
WONG et al.
Total n=677 0–3mo (n = 225) 3–6mo (n = 220) 6–9mo (n = 118) 9–12mo (n = 37) >12 mo (n = 77) P-value
33.2% 32.5% 17.4% 5.5% 11.4%
Preterm birtha 42 (8.1) 12 (6.6) 15 (8.9) 8 (8.8) 4 (14.3) 3 (6.0) 0.65
Peri-implantation Loss (n [%]) 41 (6.0) 13 (5.8) 9 (4.1) 8 (6.8) 1 (2.7) 10 (13.0) 0.06
Clinical Loss (n [%]) 118 (17.4) 31 (13.8) 43 (19.6) 19 (16.1) 8 (21.6) 17 (22.1) 0.34
Clinical Loss Type (n [%])b 0.53
Embryonic 71 (53.4) 18 (58.1) 22 (51.2) 10 (52.6) 6 (75.0) 9 (52.9)
Pre-Embryonic 36 (27.1) 11 (35.5) 9 (20.9) 7 (36.8) 1 (12.5) 3 (17.7)
Fetal Loss 9 (6.8) 1 (3.2) 5 (11.6) 0 (0.0) 1 (12.5) 1 (5.9)
Stillbirth 4 (3.0) 1 (3.2) 2 (4.7) 0 (0.0) 0 (0.0) 1 (5.9)
Otherc 13 (9.8) 0 (0.0) 5 (11.6) 2 (10.5) 0 (0.0) 3 (17.7)
Gestational Age of Loss 9.9 ± 4.1 10.1 ± 5.5 10.1 ± 4.1 8.2 ± 1.7 11.9 ± 2.9 9.9 ± 3.7 0.26
Pre-eclampsia d 58 (9.0) 19 (8.8) 20 (9.4) 8 (7.2) 6 (16.7) 5 (7.3) 0.51
Gestational Diabetesd 20 (3.1) 6 (2.8) 9 (4.2) 2 (1.8) 1 (2.8) 2 (2.9) 0.81
Analyses performed via chi-square or Fisher’s exact test as appropriate for categorical variables and analysis of variance for continuous variables.
a
Among the live births (n=518)
b
Among those with a clinical loss (n=118)
c
Other included ectopic (n=8), very early (n=3), or unknown (n=2)
Am J Obstet Gynecol. Author manuscript; available in PMC 2016 March 01.
d
n=645
Page 15
Author Manuscript Author Manuscript Author Manuscript Author Manuscript
Table 4
Incidence of secondary obstetric outcomes according to interpregnancy interval (n=677 women)
Relative Risk (95% Confidence Interval)
WONG et al.
Interpregnancy interval Outcome/Total n (%) Model 1 P-valuea Model 2 P-valueb
0–3mo 13/225 (5.8) 1.4 (0.6–3.1) 0.44 1.6 (0.7–3.6) 0.30
3–6mo 9/220 (4.1) REF na REF na
Peri-implantation Loss 6–9mo 8/118 (6.8) 1.7 (0.7–4.2) 0.26 1.9 (0.7–4.9) 0.18
9–12mo 1/37 (2.7) 0.6 (0.1–4.7) 0.67 0.7 (0.1–4.4) 0.68
>12mo 10/77 (13.0) 3.5 (1.5–8.3) 0.01 3.7 (1.5–9.2) 0.01
Peri-implantation Loss ≤ 3 months vs. >3 months 13/225 (5.7) vs. 28/452 (6.2) 0.9 (0.5–1.7) 0.71 1.0 (0.5–1.8) 0.88
0–3mo 31/225 (13.8) 0.7 (0.5–1.1) 0.13 0.7 (0.5–1.1) 0.13
3–6mo 43/220 (19.6) REF na REF na
Clinical Loss 6–9mo 19/118 (16.1) 0.8 (0.5–1.3) 0.41 0.8 (0.5–1.3) 0.35
9–12mo 8/37 (21.6) 1.1 (0.6–2.1) 0.75 1.1 (0.6–2.1) 0.77
>12mo 17/77 (22.1) 1.1 (0.6–1.8) 0.80 1.0 (0.6–1.7) 0.91
Clinical Loss ≤ 3 months vs. >3 months 31/225 (13.8) vs. 87/452 (19.3) 0.7 (0.5–1.1) 0.12 0.8 (0.5–1.1) 0.14
0–3mo 77/225 (34.2) 0.9 (0.7–1.1) 0.22 1.0 (0.9–1.2) 0.37
3–6mo 88/220 (40.0) REF na REF na
Pregnancy Complicationc 6–9mo 44/118 (37.3) 0.9 (0.7–1.2) 0.61 1.0 (0.9–1.1) 0.89
9–12mo 17/37 (46.0) 1.1 (0.8–1.6) 0.55 1.0 (0.8–1.2) 0.94
>12mo 36/77 (46.8) 1.1 (0.8–1.5) 0.40 0.9 (0.7–1.1) 0.15
Am J Obstet Gynecol. Author manuscript; available in PMC 2016 March 01.
Pregnancy Complicationc ≤ 3 months vs. >3 months 77/225 (34.2) vs. 185/452 (40.9) 0.8 (0.7–1.0) 0.12 0.9 (0.7–1.1) 0.24
Analyses performed via multivariate relative risk (RR) estimation by Poisson regression with robust error variance.
a
Model 1: Adjusted for age, race, BMI, eligibility criteria, and gestational age of prior loss.
b
Model 2: Adjusted for age, race, BMI, eligibility criteria, gestational age of prior loss, and months tried to conceive for most recent pregnancy.
c
Pregnancy complication includes peri-implantation loss, clinical loss, preeclampsia, gestational diabetes, or preterm birth.
Page 16
S-ar putea să vă placă și
- Training Material Operasional Mitsubishi UNEJDocument35 paginiTraining Material Operasional Mitsubishi UNEJkhamid surajabÎncă nu există evaluări
- Chord ProgressionDocument6 paginiChord ProgressiongernÎncă nu există evaluări
- Harmonizing A MelodyDocument6 paginiHarmonizing A MelodyJane100% (1)
- Fill in The BlanksDocument38 paginiFill in The Blanksamit48897Încă nu există evaluări
- Recurrent Implantation Failure-Update Overview OnDocument19 paginiRecurrent Implantation Failure-Update Overview Onn2763288100% (1)
- Pregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsDe la EverandPregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsÎncă nu există evaluări
- FS2 Learning Experience 1Document11 paginiFS2 Learning Experience 1Jona May BastidaÎncă nu există evaluări
- Application Performance Management Advanced For Saas Flyer PDFDocument7 paginiApplication Performance Management Advanced For Saas Flyer PDFIrshad KhanÎncă nu există evaluări
- Cerclage For Women With Twin Pregnancies: A Systematic Review and MetaanalysisDocument16 paginiCerclage For Women With Twin Pregnancies: A Systematic Review and MetaanalysisSaira MendozaÎncă nu există evaluări
- Interpregnancy Interval After Pregnancy Loss Associated with Lowest Risk of Repeat MiscarriageDocument13 paginiInterpregnancy Interval After Pregnancy Loss Associated with Lowest Risk of Repeat Miscarriageyuliana khairiÎncă nu există evaluări
- Proforma Synopsis For Registration of SubjectDocument15 paginiProforma Synopsis For Registration of SubjectTamilArasiÎncă nu există evaluări
- Journal Reading: Influence of Interpregnancy Interval On Uterine RuptureDocument9 paginiJournal Reading: Influence of Interpregnancy Interval On Uterine RuptureIlham ErtandriÎncă nu există evaluări
- Articulo Peruano PDFDocument10 paginiArticulo Peruano PDFStephanyChavezFeriaÎncă nu există evaluări
- Efectele Pe Termen Lung Ale Alaptatului OMSDocument74 paginiEfectele Pe Termen Lung Ale Alaptatului OMSbobocraiÎncă nu există evaluări
- Paper Cervical LenghtDocument30 paginiPaper Cervical LenghtDanTe D' WinchesterÎncă nu există evaluări
- Defining Failed Induction of Labor: Maternal and Perinatal Outcomes by Latent Phase DurationDocument16 paginiDefining Failed Induction of Labor: Maternal and Perinatal Outcomes by Latent Phase DurationAhmad NazharÎncă nu există evaluări
- Postplacental or Delayed Levonorgestrel Intrauterine Device Insertion and Breastfeeding DurationDocument13 paginiPostplacental or Delayed Levonorgestrel Intrauterine Device Insertion and Breastfeeding DurationdeadanandaÎncă nu există evaluări
- Spontaneous Preterm Birth Prevention in Multiple PregnancyDocument7 paginiSpontaneous Preterm Birth Prevention in Multiple PregnancyElias Melo JrÎncă nu există evaluări
- Jurnal Placenta PreviaDocument9 paginiJurnal Placenta Previasheva25Încă nu există evaluări
- Art:10.1186/1471 2393 14 337 PDFDocument10 paginiArt:10.1186/1471 2393 14 337 PDF<_>Încă nu există evaluări
- Laborinduction: Areviewof Currentmethods: Mildred M. RamirezDocument11 paginiLaborinduction: Areviewof Currentmethods: Mildred M. RamirezRolando DiazÎncă nu există evaluări
- To Ignore or Not To Ignore Placental Calcifications On Prenatal Ultrasound: A Systematic Review and Meta-AnalysisDocument22 paginiTo Ignore or Not To Ignore Placental Calcifications On Prenatal Ultrasound: A Systematic Review and Meta-AnalysisMaulida HalimahÎncă nu există evaluări
- Debate GUIDE PDFDocument8 paginiDebate GUIDE PDFBlesse PateñoÎncă nu există evaluări
- Pregnancy Following Miscarriage What Is The Optimum Interpregnancy IntervalDocument3 paginiPregnancy Following Miscarriage What Is The Optimum Interpregnancy IntervallcmurilloÎncă nu există evaluări
- Care in Pregnancies Subsequent To Stillbirthor Perinatal DeatDocument12 paginiCare in Pregnancies Subsequent To Stillbirthor Perinatal DeatgalalÎncă nu există evaluări
- D'Souza-2019-Maternal Body Mass Index and PregDocument17 paginiD'Souza-2019-Maternal Body Mass Index and PregMARIATUL QIFTIYAHÎncă nu există evaluări
- Jurnal OG 4Document11 paginiJurnal OG 4Reka AmeliaÎncă nu există evaluări
- 1OudGvy8RaUCS I6Ynenp qqBDDAJMOPoDocument13 pagini1OudGvy8RaUCS I6Ynenp qqBDDAJMOPoJan Rey G. PelagioÎncă nu există evaluări
- BMJ f6398Document13 paginiBMJ f6398Luis Gerardo Pérez CastroÎncă nu există evaluări
- Sibai PDFDocument2 paginiSibai PDFAdriana PajueloÎncă nu există evaluări
- The Natural History of The Normal First Stage Of.6 PDFDocument6 paginiThe Natural History of The Normal First Stage Of.6 PDFreioctabianoÎncă nu există evaluări
- Antenatal Corticosteroids Beyond 34 Weeks Gestation: What Do We Do Now?Document8 paginiAntenatal Corticosteroids Beyond 34 Weeks Gestation: What Do We Do Now?XIMENAGILDAÎncă nu există evaluări
- Merced 2019Document14 paginiMerced 2019Vanessa CarinoÎncă nu există evaluări
- Guidelines On 8 Key Evidence Based Practices During Labour - 353Document35 paginiGuidelines On 8 Key Evidence Based Practices During Labour - 353National Child Health Resource Centre (NCHRC)Încă nu există evaluări
- Association Between Maternal Sleep Practices and Late Stillbirth - Findings From A Stillbirth Case-Control StudyDocument9 paginiAssociation Between Maternal Sleep Practices and Late Stillbirth - Findings From A Stillbirth Case-Control StudyWinniaTanelyÎncă nu există evaluări
- postpartum lit review nealeDocument9 paginipostpartum lit review nealeapi-726948535Încă nu există evaluări
- Pi Is 0002937810000815 JournallDocument12 paginiPi Is 0002937810000815 JournallRaisa AriesthaÎncă nu există evaluări
- Postpartum Hormonal Contraception in Breastfeeding Women: ReviewDocument6 paginiPostpartum Hormonal Contraception in Breastfeeding Women: ReviewmarialecifuentesbÎncă nu există evaluări
- Chouinard2019 PDFDocument8 paginiChouinard2019 PDFanggunÎncă nu există evaluări
- Caesarean Birth and Risk of Subsequent Preterm Birth: A Retrospective Cohort StudyDocument9 paginiCaesarean Birth and Risk of Subsequent Preterm Birth: A Retrospective Cohort Studyluis albenis mendoza guerraÎncă nu există evaluări
- Optimal Birth Spacing: What Can We Measure and What Do We Want To Know?Document3 paginiOptimal Birth Spacing: What Can We Measure and What Do We Want To Know?rizmahÎncă nu există evaluări
- Management Options For Early Incomplete MiscarriageDocument6 paginiManagement Options For Early Incomplete MiscarriagenikeratnakemalaÎncă nu există evaluări
- Clinico-Epidemiological Profile and Evidence Based Management of Recurrent Miscarriages in A Tertiary Care CentreDocument15 paginiClinico-Epidemiological Profile and Evidence Based Management of Recurrent Miscarriages in A Tertiary Care CentreIJAR JOURNALÎncă nu există evaluări
- Ojog 2018041214473648Document10 paginiOjog 2018041214473648RiniÎncă nu există evaluări
- ijwh-5-501Document7 paginiijwh-5-501MarianaafiatiÎncă nu există evaluări
- App Acog 2012Document10 paginiApp Acog 2012jimedureyÎncă nu există evaluări
- Spontaneous AbortionDocument17 paginiSpontaneous Abortionanon_985338331Încă nu există evaluări
- 2018 Article 414Document18 pagini2018 Article 414Haribabu ArumugamÎncă nu există evaluări
- Cervical EncerclageDocument25 paginiCervical EncerclageKartheek VarmaÎncă nu există evaluări
- Minor AilmentsDocument14 paginiMinor AilmentsGazala100% (1)
- Cervical Stitch (Cerclage) For Preventing Pregnancy Loss: Individual Patient Data Meta-AnalysisDocument17 paginiCervical Stitch (Cerclage) For Preventing Pregnancy Loss: Individual Patient Data Meta-AnalysisNi Wayan Ana PsÎncă nu există evaluări
- Javon WitherspoonDocument6 paginiJavon Witherspoonapi-445367279Încă nu există evaluări
- Antipsikotik Pregnancy 3Document9 paginiAntipsikotik Pregnancy 3ThalÎncă nu există evaluări
- Antenatal Betamethasone For Women at RiskDocument10 paginiAntenatal Betamethasone For Women at RiskThapakorn JalearnyingÎncă nu există evaluări
- The NeoUpdates - DecDocument7 paginiThe NeoUpdates - DecDr Satish MishraÎncă nu există evaluări
- Newspaper Clipping Service: PregnancyDocument2 paginiNewspaper Clipping Service: PregnancyNational Child Health Resource Centre (NCHRC)Încă nu există evaluări
- Anemia-1Document15 paginiAnemia-1Intan Wahyu CahyaniÎncă nu există evaluări
- Systematic Review Placenta Calcification and Fetal OutcomeDocument22 paginiSystematic Review Placenta Calcification and Fetal OutcomeRizka AdiÎncă nu există evaluări
- Short-Term Effects of BreastfeedingDocument54 paginiShort-Term Effects of BreastfeedingAnonymous Zk4Go4facOÎncă nu există evaluări
- Cervical Effacement Associated with Faster Labor Progression in Nulliparous WomenDocument12 paginiCervical Effacement Associated with Faster Labor Progression in Nulliparous WomenM Iqbal EffendiÎncă nu există evaluări
- Pneumonia and Pregnancy Outcomes: A Nationwide Population-Based StudyDocument7 paginiPneumonia and Pregnancy Outcomes: A Nationwide Population-Based StudyAdrin Mahmuddin HarahapÎncă nu există evaluări
- Impact of Oligohydramnios On Maternal and PerinataDocument6 paginiImpact of Oligohydramnios On Maternal and PerinataDiana SchlittlerÎncă nu există evaluări
- V615br MarhattaDocument4 paginiV615br MarhattaMarogi Al AnsorianiÎncă nu există evaluări
- Maternal and Perinatal Outcomes After Elective Labor Induction at 39 Weeks in Uncomplicated Singleton Pregnancies - A Meta-Analysis-sotiriadis2018Document27 paginiMaternal and Perinatal Outcomes After Elective Labor Induction at 39 Weeks in Uncomplicated Singleton Pregnancies - A Meta-Analysis-sotiriadis2018trongnguyen2232000Încă nu există evaluări
- Sankar Et Al-2015 MortalitiyDocument11 paginiSankar Et Al-2015 MortalitiyMirella Mir CamposÎncă nu există evaluări
- CDC 84627 DS1Document15 paginiCDC 84627 DS1Thu HoaiÎncă nu există evaluări
- OswegoDocument6 paginiOswegoMahlina Nur LailiÎncă nu există evaluări
- Weight-for-length BOYS growth chart z-scoresDocument1 paginăWeight-for-length BOYS growth chart z-scoresMahlina Nur LailiÎncă nu există evaluări
- Journal Pone 0022115 PDFDocument10 paginiJournal Pone 0022115 PDFMahlina Nur LailiÎncă nu există evaluări
- 2065 1378 1 PB PDFDocument11 pagini2065 1378 1 PB PDFDwi Fitri WÎncă nu există evaluări
- Impact of Advanced Maternal AgeDocument7 paginiImpact of Advanced Maternal AgeEgyed Fülöp AndreaÎncă nu există evaluări
- Sha Char 2014Document5 paginiSha Char 2014Mahlina Nur LailiÎncă nu există evaluări
- Pregnancy Hypertension Incidence by Age, Parity, RaceDocument8 paginiPregnancy Hypertension Incidence by Age, Parity, RaceMahlina Nur LailiÎncă nu există evaluări
- Anemia Pregnancy OutcomeDocument10 paginiAnemia Pregnancy OutcomeRaissa Metasari TantoÎncă nu există evaluări
- Ijpho 5 211Document8 paginiIjpho 5 211Mahlina Nur LailiÎncă nu există evaluări
- Prediction of Preeclampsia by A Combination of Body Mass Index (BMI), Mean Arterial Pressure (MAP), and Roll Over Test (ROT)Document4 paginiPrediction of Preeclampsia by A Combination of Body Mass Index (BMI), Mean Arterial Pressure (MAP), and Roll Over Test (ROT)Mahlina Nur LailiÎncă nu există evaluări
- Coo 2017Document14 paginiCoo 2017Mahlina Nur LailiÎncă nu există evaluări
- Folate Depletion Hypothesis Explains Adverse Pregnancy Outcomes After Short Interpregnancy IntervalsDocument4 paginiFolate Depletion Hypothesis Explains Adverse Pregnancy Outcomes After Short Interpregnancy IntervalsMahlina Nur LailiÎncă nu există evaluări
- Sha Char 2014Document5 paginiSha Char 2014Mahlina Nur LailiÎncă nu există evaluări
- Ann Am Raju 2016Document5 paginiAnn Am Raju 2016Mahlina Nur LailiÎncă nu există evaluări
- S0007114515001166a PDFDocument8 paginiS0007114515001166a PDFMahlina Nur LailiÎncă nu există evaluări
- Shachar2014 PDFDocument1 paginăShachar2014 PDFMahlina Nur LailiÎncă nu există evaluări
- Bab Ii PDFDocument16 paginiBab Ii PDFfaisalfachrurarifinÎncă nu există evaluări
- Tanduumba 2015Document6 paginiTanduumba 2015Mahlina Nur LailiÎncă nu există evaluări
- Hanley 2017Document8 paginiHanley 2017Mahlina Nur LailiÎncă nu există evaluări
- Ijpho 5 211Document8 paginiIjpho 5 211Mahlina Nur LailiÎncă nu există evaluări
- SaudiMedJ 36 146Document4 paginiSaudiMedJ 36 146Mahlina Nur LailiÎncă nu există evaluări
- 80 (11) 871 1 PDFDocument5 pagini80 (11) 871 1 PDFMahlina Nur LailiÎncă nu există evaluări
- Shachar2014 PDFDocument1 paginăShachar2014 PDFMahlina Nur LailiÎncă nu există evaluări
- jvc_kd-av7000_kd-av7001_kd-av7005_kd-av7008_kv-mav7001_kv-mav7002-ma101-Document159 paginijvc_kd-av7000_kd-av7001_kd-av7005_kd-av7008_kv-mav7001_kv-mav7002-ma101-strelectronicsÎncă nu există evaluări
- Social Responsibility and Ethics in Marketing: Anupreet Kaur MokhaDocument7 paginiSocial Responsibility and Ethics in Marketing: Anupreet Kaur MokhaVlog With BongÎncă nu există evaluări
- Spelling Errors Worksheet 4 - EditableDocument2 paginiSpelling Errors Worksheet 4 - EditableSGillespieÎncă nu există evaluări
- Research Methods LessonDocument26 paginiResearch Methods LessonCarole Janne EndoyÎncă nu există evaluări
- Unit 9Document3 paginiUnit 9Janna Rick100% (1)
- Legend of The Galactic Heroes, Vol. 10 Sunset by Yoshiki Tanaka (Tanaka, Yoshiki)Document245 paginiLegend of The Galactic Heroes, Vol. 10 Sunset by Yoshiki Tanaka (Tanaka, Yoshiki)StafarneÎncă nu există evaluări
- Emergency Order Ratification With AmendmentsDocument4 paginiEmergency Order Ratification With AmendmentsWestSeattleBlogÎncă nu există evaluări
- Arcmap and PythonDocument29 paginiArcmap and PythonMiguel AngelÎncă nu există evaluări
- MES - Project Orientation For Night Study - V4Document41 paginiMES - Project Orientation For Night Study - V4Andi YusmarÎncă nu există evaluări
- Karnataka PUC Board (KSEEB) Chemistry Class 12 Question Paper 2017Document14 paginiKarnataka PUC Board (KSEEB) Chemistry Class 12 Question Paper 2017lohith. sÎncă nu există evaluări
- Bhikkhuni Patimokkha Fourth Edition - Pali and English - UTBSI Ordination Bodhgaya Nov 2022 (E-Book Version)Document154 paginiBhikkhuni Patimokkha Fourth Edition - Pali and English - UTBSI Ordination Bodhgaya Nov 2022 (E-Book Version)Ven. Tathālokā TherīÎncă nu există evaluări
- Dues & Scholarship Section: NotificationDocument6 paginiDues & Scholarship Section: NotificationMUNEEB WAHEEDÎncă nu există evaluări
- UA-Series EN F2005E-3.0 0302Document25 paginiUA-Series EN F2005E-3.0 0302PrimanedyÎncă nu există evaluări
- Platform Tests Forj Udging Quality of MilkDocument10 paginiPlatform Tests Forj Udging Quality of MilkAbubaker IbrahimÎncă nu există evaluări
- Jurnal Manajemen IndonesiaDocument20 paginiJurnal Manajemen IndonesiaThoriq MÎncă nu există evaluări
- Interpersonal Communication LPDocument3 paginiInterpersonal Communication LPprincesslove.taduraÎncă nu există evaluări
- 100 Bedded Hospital at Jadcherla: Load CalculationsDocument3 pagini100 Bedded Hospital at Jadcherla: Load Calculationskiran raghukiranÎncă nu există evaluări
- City Government of San Juan: Business Permits and License OfficeDocument3 paginiCity Government of San Juan: Business Permits and License Officeaihr.campÎncă nu există evaluări
- Sadhu or ShaitaanDocument3 paginiSadhu or ShaitaanVipul RathodÎncă nu există evaluări
- Lucid Motors Stock Prediction 2022, 2023, 2024, 2025, 2030Document8 paginiLucid Motors Stock Prediction 2022, 2023, 2024, 2025, 2030Sahil DadashovÎncă nu există evaluări
- PAASCU Lesson PlanDocument2 paginiPAASCU Lesson PlanAnonymous On831wJKlsÎncă nu există evaluări
- Das MarterkapitalDocument22 paginiDas MarterkapitalMatthew Shen GoodmanÎncă nu există evaluări
- Alphabet Bean BagsDocument3 paginiAlphabet Bean Bagsapi-347621730Încă nu există evaluări
- CERTIFICATE - Guest Speaker and ParentsDocument4 paginiCERTIFICATE - Guest Speaker and ParentsSheryll Eliezer S.PantanosaÎncă nu există evaluări