Documente Academic
Documente Profesional
Documente Cultură
Sample History
Încărcat de
isprikitik3Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Sample History
Încărcat de
isprikitik3Drepturi de autor:
Formate disponibile
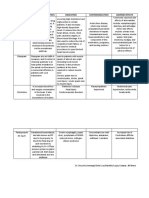
7/18/18
Patient was seen and assessed with the following vital signs: BP=110/70, CR=72, RR=20, Temp= 36.5,
O2sat=100%. Patient was unconscious with a GCS score of 8 (E2V1M5). Physical Examination revealed
bilateral rhonchi upon auscultation of the chest. Diet includes Glucorna 5 scoops in 1 glass of water every
4 hours with 30cc pre and post flushing and IVF of PNSS x 60cc/hour. Medications included Polymixin B
150 mg TIV q12, Noripenem 500mg TIV q8, Amlodipine + Indapamide 10/1.5 mg/tab, 1 tablet OD,
Rosuvastatin 10 mg/tab, 1 tablet OD at night, Lactiracetam 100 mg/mL, 10 mL every 12 hours, Duavent
½ +2cc NSS every 6 hours, NAC 600 mg/tab, 1 tab BID, Hexetidine swab q6, Theophylline 125 mg/tab BID,
Nebivolol 5mg/tab, 1 tablet OD, CaCO3 tab, OD, Conzace tab, 1 tablet OD, Paracetamol 500 mg/tab, 1
tablet every 4 hours PRN, Diazepam 5 mg TIV PRN, Insulin glargine 20 units SQ OD. Patient was seen by
ENT-OHNS, and Neuro services and was advised to continue present medications and management.
Patient was also seen by the pulmo service in which they modified the MV setup to FiO2= 30%, PEEP= 14,
VT= 350 mL BVR= 14. Additional procedures advised by the pulmo service included suctioning of
secretions as well as to watch out for Hypotension and desaturation.
7/19/18
Patient was seen and assessed with the following vital signs: BP=100/60, CR=88, RR=20, Temp= 36.5,
O2sat=98%. Patient had no febrile episodes as well as desaturation and hypotension. On evaluation,
patient was unconscious with a GCS score of 10 (E4V1M5). Pertinent findings on physical examination
revealed 3mm pupillary light reflex, bilateral rhonchi upon auscultation of the chest and +2 deep tendon
reflexes. Diet includes Glucorna 5 scoops in 1 glass of water every 4 hours with 30cc pre and post flushing.
CBG monitoring in the morning was requested as part of diagnostics. Medications included Polymixin B
150 mg TIV q12, Noripenem 500mg TIV q8, Amlodipine + Indapamide 10/1.5 mg/tab, 1 tablet OD,
Rosuvastatin 10 mg/tab, 1 tablet OD at night, Lactiracetam 100 mg/mL, 10 mL every 12 hours, Duavent
½ +2cc NSS every 6 hours, NAC 600 mg/tab, 1 tab BID, Hexetidine swab q6, Theophylline 125 mg/tab BID,
Nebivolol 5mg/tab, 1 tablet OD, CaCO3 tab, OD, Conzace tab, 1 tablet OD, Paracetamol 500 mg/tab, 1
tablet every 4 hours PRN, Diazepam 5 mg TIV PRN, Insulin glargine 20 units SQ OD. Patient was seen by
ENT-OHNS service and was advised to continue present medications and management. Additional
instructions include suctioning of secretions as well as to watch out for Hypotension, fever and
desaturation
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Antidepressant ChartDocument7 paginiAntidepressant Chartinher1tance100% (4)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Evaluation - For External Trainings 06222017Document1 paginăEvaluation - For External Trainings 06222017isprikitik3Încă nu există evaluări
- Biochemistry 1.6 - ABO Blood Typing and Crossmatching (A1 Group 6)Document68 paginiBiochemistry 1.6 - ABO Blood Typing and Crossmatching (A1 Group 6)isprikitik3Încă nu există evaluări
- Ao Final ProgramDocument16 paginiAo Final Programisprikitik3Încă nu există evaluări
- Drugs Mechanism of Action Indication Contraindication Adverse EffectsDocument2 paginiDrugs Mechanism of Action Indication Contraindication Adverse Effectsisprikitik3Încă nu există evaluări
- God's Creation: Christianity Is An Abrahamic, Monotheistic Religion Based On The Life and OralDocument2 paginiGod's Creation: Christianity Is An Abrahamic, Monotheistic Religion Based On The Life and Oralisprikitik3Încă nu există evaluări
- Individual Reflections Format (CPH)Document2 paginiIndividual Reflections Format (CPH)isprikitik3Încă nu există evaluări
- Recommendation LetterDocument1 paginăRecommendation Letterisprikitik3Încă nu există evaluări
- Crown Lengthening of ToothDocument4 paginiCrown Lengthening of Toothisprikitik3Încă nu există evaluări
- Clinical Chemistry (Lecture) - PrelimsDocument12 paginiClinical Chemistry (Lecture) - Prelimsisprikitik3100% (1)
- Request LetterDocument1 paginăRequest Letterisprikitik3Încă nu există evaluări
- Must Knows IDocument38 paginiMust Knows Iisprikitik3Încă nu există evaluări
- Carbohydrates 2Document37 paginiCarbohydrates 2isprikitik3Încă nu există evaluări
- ImmunityDocument70 paginiImmunityisprikitik30% (2)
- MycologyDocument3 paginiMycologyisprikitik3Încă nu există evaluări
- Must Knows IIDocument3 paginiMust Knows IIisprikitik3Încă nu există evaluări
- NPPA1Document3 paginiNPPA1haryroyÎncă nu există evaluări
- List HargaDocument40 paginiList HargaReza PahleviÎncă nu există evaluări
- Zimbabue Standard Guidelines Essential Medicines PDFDocument622 paginiZimbabue Standard Guidelines Essential Medicines PDFportosinÎncă nu există evaluări
- ORNIDAZOLEDocument9 paginiORNIDAZOLEroopendramauryaÎncă nu există evaluări
- Validation of Ultraviolet Spectrophotometry Method PDFDocument7 paginiValidation of Ultraviolet Spectrophotometry Method PDFArie NrcÎncă nu există evaluări
- Official: Á1079.1Ñ Storage and Transportation of Investigational Drug ProductsDocument4 paginiOfficial: Á1079.1Ñ Storage and Transportation of Investigational Drug ProductsDilawar BakhtÎncă nu există evaluări
- Appendix 1 Acceptable Intakes Established N Nitrosamines enDocument4 paginiAppendix 1 Acceptable Intakes Established N Nitrosamines enManikanthakumar TulaÎncă nu există evaluări
- Template Continued On Page 2Document3 paginiTemplate Continued On Page 2JaneÎncă nu există evaluări
- Core and CupDocument9 paginiCore and CupVikas JhawatÎncă nu există evaluări
- Soluvit N PIDocument3 paginiSoluvit N PIsigitÎncă nu există evaluări
- Medical PrecriptionDocument4 paginiMedical PrecriptionDimas Ajie PrasetyoÎncă nu există evaluări
- Drugs For TuberculosisDocument3 paginiDrugs For TuberculosisJeanneRoseBlancaflorÎncă nu există evaluări
- Psyc Un 2460Document11 paginiPsyc Un 2460Robyn AnÎncă nu există evaluări
- Chapter 35. Headache, Self-Assessment QuestionsDocument5 paginiChapter 35. Headache, Self-Assessment Questionstsegaab yosephÎncă nu există evaluări
- LearnEnglish Listening B1 at The ChemistDocument4 paginiLearnEnglish Listening B1 at The Chemistნინი მახარაძეÎncă nu există evaluări
- 04 - Extravascular Administration (Oral)Document41 pagini04 - Extravascular Administration (Oral)Prasanna PappuÎncă nu există evaluări
- NL H 2302 001 ParDocument9 paginiNL H 2302 001 Parshannon prijadiÎncă nu există evaluări
- Ascorbic Acid Tablets 500mg Label LeafletDocument4 paginiAscorbic Acid Tablets 500mg Label LeafletmostofarubalÎncă nu există evaluări
- Nclex Drug ReviewDocument2 paginiNclex Drug ReviewdoneshiaÎncă nu există evaluări
- Co AmoxiclavDocument1 paginăCo AmoxiclavMuhammad ArsalanÎncă nu există evaluări
- Unit 1: Introduction: Intended Learning OutcomesDocument7 paginiUnit 1: Introduction: Intended Learning Outcomesalibel caballeroÎncă nu există evaluări
- 2.BMD Study Guide Final 6.4.2023Document42 pagini2.BMD Study Guide Final 6.4.2023Phyo Wai KyawÎncă nu există evaluări
- Us 47524704r4r4rDocument8 paginiUs 47524704r4r4rResti Darojatin HalimaÎncă nu există evaluări
- Advanced Marketing Strategy: ZantacDocument6 paginiAdvanced Marketing Strategy: ZantacAALOK SINGLAÎncă nu există evaluări
- DILADocument1.369 paginiDILALilly Hoo LeeÎncă nu există evaluări
- Draft PDFDocument166 paginiDraft PDFashwaq000111Încă nu există evaluări
- Pharmacological Effects and Safety Monitoring of Anabolic Androgenic Steroid Use: Differing Perceptions Between Users and Healthcare ProfessionalsDocument10 paginiPharmacological Effects and Safety Monitoring of Anabolic Androgenic Steroid Use: Differing Perceptions Between Users and Healthcare ProfessionalsJames AertsÎncă nu există evaluări
- Invitro Toxicity Assay MethodsDocument11 paginiInvitro Toxicity Assay MethodsShubham RastogiÎncă nu există evaluări
- Instructions To Author-REACH2020Document2 paginiInstructions To Author-REACH2020pharma xlÎncă nu există evaluări