Documente Academic
Documente Profesional
Documente Cultură
Retinal Detachment: Jama Patient Page
Încărcat de
Kemal TaufikTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Retinal Detachment: Jama Patient Page
Încărcat de
Kemal TaufikDrepturi de autor:
Formate disponibile
JAMA PATIENT PAGE The Journal of the American Medical Association
EYE DISEASES
Retinal Detachment
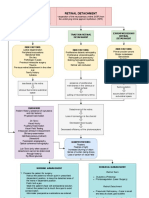
Anatomy of an eye with retinal detachment
T he retina is a light-sensitive, transparent tissue
located in the back of the eye. Light is focused
on the retina by the cornea and the lens. The
retina then converts the image into neural impulses
and sends them to the brain via the optic nerve
Cornea
CROSS SECTION
Retinal tear
Retina (detached)
Posterior
(the nerve connecting the eye to the brain). vitreous detachment
Iris
Retinal detachment is the separation of the retina Optic disc
from the tissues underneath it. It is important to
distinguish retinal detachment from posterior Pupil VITREOUS
Indirect
vitreous detachment (in which the jelly in the eye ophthalmoscope
Optic
peels away from the retina), which is a natural aging Lens nerve Lens
process that occurs in many people. Every year, about
Retinal
1 to 2 people per 10 000 develop retinal detachment. vessel
Retinal detachment is a medical emergency. The
April 4, 2012, issue of JAMA includes an article about
Retinal tears
the risk of retinal detachment from a type of antibiotic.
This Patient Page is based on one previously published
in the November 25, 2009, issue of JAMA.
RISK FACTORS
Nearsightedness is an important risk factor for retinal detachment: 67%
Area of retinal
of people who develop retinal detachment are nearsighted. Other risk detachment
factors include retinal detachment in the other eye, cataract surgery, (“billowing”)
a family history of retinal detachment, uncontrolled diabetes, and blunt
trauma to the eye.
Ophthalmoscope view
SYMPTOMS
Symptoms of posterior vitreous detachment may include sudden onset of floaters,
bright flashes of light, and blurred vision. A small percentage of people with posterior
vitreous detachment may develop a retinal tear (the vitreous jelly rips the retina during FOR MORE INFORMATION
the process of posterior vitreous detachment), which can progress to a retinal • National Eye Institute
detachment if it is not treated. An increasing area of grayness in one eye (“curtain of http://www.nei.nih.gov/health
darkness”) can mean that a retinal tear has progressed to a detached retina. Patients /retinaldetach/index.asp
with symptoms of posterior vitreous detachment or retinal detachment should • American Academy
immediately consult an ophthalmologist (physician specializing in diseases of the eye). of Ophthalmology
The goal is to prevent detachment of the macula (central region of the retina) because http://one.aao.org
this is the portion of the retina responsible for fine, detailed central vision.
INFORM YOURSELF
TREATMENT To find this and previous JAMA
The chances of recovering vision are greater when the retina is repaired before the Patient Pages, go to the Patient
macula is detached. Most people with retinal detachment need surgery to repair it, Page link on JAMA’s website at
either immediately or after a short time. There are several types of surgery used www.jama.com. Many are
depending on the severity and type of detachment. Patients with tears or small available in English and Spanish.
detachments can often be treated in the office with laser surgery, gas bubble injection, Sources: National Institutes of Health, American
or a freeze treatment called cryopexy. Patients with more severe retinal detachment Academy of Ophthalmology
need to go to the operating room, where different types of surgery can be performed
to reattach the retina. Once the retina is reattached, vision often improves or stabilizes.
A person’s ability to read with the affected eye after surgery depends on whether the
macula was detached, how long it was detached, the severity of the retinal
detachment, and the type of treatment performed.
Huan J. Chang, MD, MPH, Writer The JAMA Patient Page is a public service of JAMA. The information and recommenda-
tions appearing on this page are appropriate in most instances, but they are not a substi-
tute for medical diagnosis. For specific information concerning your personal medical
Cassio Lynm, MA, Illustrator condition, JAMA suggests that you consult your physician. This page may be photocopied
noncommercially by physicians and other health care professionals to share with patients.
Robert M. Golub, MD, Editor To purchase bulk reprints, call 312/464-0776.
©2012 American Medical Association. All rights reserved. JAMA, April 4, 2012—Vol 307, No. 13 1447
Downloaded From: http://jama.jamanetwork.com/ by a University of Sussex Library User on 08/07/2015
S-ar putea să vă placă și
- Management of Retinal Detachment: A Guide For Non-OphthalmologistsDocument6 paginiManagement of Retinal Detachment: A Guide For Non-OphthalmologistsadriantiariÎncă nu există evaluări
- Retinal DetachmentDocument3 paginiRetinal DetachmentzeejayÎncă nu există evaluări
- Retinal Detachment: PathogenesisDocument8 paginiRetinal Detachment: PathogenesisRashellya RasyidaÎncă nu există evaluări
- Retinal Detachment: The FoundationDocument2 paginiRetinal Detachment: The FoundationNeneng LukmanÎncă nu există evaluări
- Retinal Detachment Nava Joanna D.Document10 paginiRetinal Detachment Nava Joanna D.JoanneNBondocÎncă nu există evaluări
- Emergency Management: Retinal DetachmentDocument1 paginăEmergency Management: Retinal DetachmentSitti HazrinaÎncă nu există evaluări
- Retinal Detachments and The Current Trends of TreatmentDocument10 paginiRetinal Detachments and The Current Trends of Treatmentapi-235387260Încă nu există evaluări
- Retinal Detachment: Traction Retinal Detachment Rhegmatogenous Detachment Exudative/Serous Retinal DetachmentDocument3 paginiRetinal Detachment: Traction Retinal Detachment Rhegmatogenous Detachment Exudative/Serous Retinal DetachmentJordz Placi100% (1)
- Corneal Dystrophies: Retinal DetachmentDocument5 paginiCorneal Dystrophies: Retinal DetachmentCake ManÎncă nu există evaluări
- 2014FeltgenDABenglish PDFDocument14 pagini2014FeltgenDABenglish PDFNurul ArdaniÎncă nu există evaluări
- 2014FeltgenDABenglish PDFDocument14 pagini2014FeltgenDABenglish PDFNurul ArdaniÎncă nu există evaluări
- Blurring of Vision Ii: Retinal Vascular Disorders: Dr. Jose BondocDocument15 paginiBlurring of Vision Ii: Retinal Vascular Disorders: Dr. Jose BondocRea Dominique CabanillaÎncă nu există evaluări
- Corneal Dystrophies: Retinal DetachmentDocument6 paginiCorneal Dystrophies: Retinal DetachmentMarissa AsimÎncă nu există evaluări
- PatientEdSeries RetDetachDocument1 paginăPatientEdSeries RetDetachvijaykadam_ndaÎncă nu există evaluări
- Detection of Ocular Cataracts With Convolutional Neural NetworksDocument10 paginiDetection of Ocular Cataracts With Convolutional Neural NetworksAlejandro PerdomoÎncă nu există evaluări
- Oph SBR Case-QuizDocument4 paginiOph SBR Case-QuizRix tanÎncă nu există evaluări
- 1retinal DetachmentDocument5 pagini1retinal Detachmentsunny_jr_Încă nu există evaluări
- Retinal DetachmentDocument14 paginiRetinal DetachmentPui_Yee_Siow_6303Încă nu există evaluări
- (OPTHA) Lec 5 - RetinaDocument5 pagini(OPTHA) Lec 5 - RetinaPatricia ManaliliÎncă nu există evaluări
- Retinal Detachment: Case Report Operating RoomDocument35 paginiRetinal Detachment: Case Report Operating RoomCarlo Joseph Intal Llacer50% (2)
- Retinal Detachment SlideDocument54 paginiRetinal Detachment SlideHerin NataliaÎncă nu există evaluări
- Mata Tenang Visus Turun MendadakDocument74 paginiMata Tenang Visus Turun MendadakYeni AnggrainiÎncă nu există evaluări
- Retinal Detachment: Case Report Operating RoomDocument30 paginiRetinal Detachment: Case Report Operating RoomCarlo Joseph Intal LlacerÎncă nu există evaluări
- Retinal DetachmentDocument2 paginiRetinal DetachmentGusti Zidni FahmiÎncă nu există evaluări
- Das 2018 J. Phys. Conf. Ser. 1000 012053 PDFDocument11 paginiDas 2018 J. Phys. Conf. Ser. 1000 012053 PDFCHARANÎncă nu există evaluări
- Referat Ablatio Retina Viviiiy-1Document20 paginiReferat Ablatio Retina Viviiiy-1Vivi YolandhaÎncă nu există evaluări
- (Ophtha) Ocular Emergenices - Dr. VillalvaDocument6 pagini(Ophtha) Ocular Emergenices - Dr. VillalvaPatricia ManaliliÎncă nu există evaluări
- Diabetic Eye Disease Macular DegenerationDocument13 paginiDiabetic Eye Disease Macular DegenerationFadzilah NurraysaÎncă nu există evaluări
- Retinal DetachmentDocument10 paginiRetinal DetachmentSilpi HamidiyahÎncă nu există evaluări
- Retinal Detachment: Practice EssentialsDocument6 paginiRetinal Detachment: Practice EssentialsDeasy Arindi PutriÎncă nu există evaluări
- Management of Corneal Abrasions: STEPHEN A. WILSON, M.D., and ALLEN LAST, M.D., University of Pittsburgh Medical CenterDocument6 paginiManagement of Corneal Abrasions: STEPHEN A. WILSON, M.D., and ALLEN LAST, M.D., University of Pittsburgh Medical CenterGokull ShautriÎncă nu există evaluări
- Retinal DetachmentDocument8 paginiRetinal DetachmentJohanLazuardiÎncă nu există evaluări
- Eye Disorders: Presented by Carmelita Ramos, RNDocument65 paginiEye Disorders: Presented by Carmelita Ramos, RNJayme_Galang_7078100% (1)
- MDBooklet 2017-04 WEBDocument22 paginiMDBooklet 2017-04 WEBholly theressaÎncă nu există evaluări
- Carole-NUR220-EAQ Vision Disorders and ProblemsDocument14 paginiCarole-NUR220-EAQ Vision Disorders and ProblemsCarole EmenikeÎncă nu există evaluări
- Retinal Diseases 230210 210855Document108 paginiRetinal Diseases 230210 210855RgdÎncă nu există evaluări
- CataractDocument24 paginiCataractNeela Kandan100% (1)
- Bionic EyeDocument6 paginiBionic EyeAsfia_Samreen_29630% (1)
- Retinal DetachmentDocument31 paginiRetinal DetachmentEko KunaryagiÎncă nu există evaluări
- Low Vision: Assessment and Educational Needs: A Guide to Teachers and ParentsDe la EverandLow Vision: Assessment and Educational Needs: A Guide to Teachers and ParentsÎncă nu există evaluări
- December 2018 Ophthalmic PearlsDocument2 paginiDecember 2018 Ophthalmic PearlsFathirÎncă nu există evaluări
- HHS Public AccessDocument21 paginiHHS Public AccessAnonymous h0DxuJTÎncă nu există evaluări
- The Swollen Optic Nerve: An Approach To Diagnosis and ManagementDocument8 paginiThe Swollen Optic Nerve: An Approach To Diagnosis and Managementyalocim666Încă nu există evaluări
- A Case Presentation of CataractDocument16 paginiA Case Presentation of CataractDoneva Lyn Medina100% (1)
- Anatomy and Function of The Eye: Henry J. KaplanDocument7 paginiAnatomy and Function of The Eye: Henry J. KaplanCucută Alexandru-DanielÎncă nu există evaluări
- B06 Posterior SegmentDocument22 paginiB06 Posterior SegmentMigs MedinaÎncă nu există evaluări
- Dryeye 060718 NEJM PDFDocument12 paginiDryeye 060718 NEJM PDFGusti FerriÎncă nu există evaluări
- Retinal DetachmentDocument16 paginiRetinal DetachmentCandice Lim Swee LingÎncă nu există evaluări
- Vitreous Gel Eye Retinal Detachment OphthalmologistDocument12 paginiVitreous Gel Eye Retinal Detachment OphthalmologistLesTrechSaÎncă nu există evaluări
- Retinal DetachmentDocument14 paginiRetinal DetachmentChikita Artia Sari100% (1)
- Retinal DetachmentDocument21 paginiRetinal Detachmentณัช เกษมÎncă nu există evaluări
- Corneal Cross-Linking: Treatment for Cornea DiseaseDe la EverandCorneal Cross-Linking: Treatment for Cornea DiseaseÎncă nu există evaluări
- Introduction To Eye Problems in Indonesia: Gitalisa Andayani Department of Ophthalmology, FKUI Jakarta 2008Document45 paginiIntroduction To Eye Problems in Indonesia: Gitalisa Andayani Department of Ophthalmology, FKUI Jakarta 2008Firah MagfirahÎncă nu există evaluări
- Terminology: Nuclear Sclerotic CataractsDocument4 paginiTerminology: Nuclear Sclerotic CataractsBenjamin NgÎncă nu există evaluări
- Cataract PPT FinalDocument37 paginiCataract PPT FinalSibi John91% (22)
- Racgp Floaters and Flashes OpthalmologyDocument3 paginiRacgp Floaters and Flashes OpthalmologyBeaulah HunidzariraÎncă nu există evaluări
- Retinal Detachment and HomoeopathyDocument7 paginiRetinal Detachment and HomoeopathyDr. Rajneesh Kumar Sharma MD HomÎncă nu există evaluări
- Retinal DetachmentDocument6 paginiRetinal DetachmentNader Smadi100% (3)
- Cataracts by Idris HarunaniDocument2 paginiCataracts by Idris Harunanix2tnnwjhtvÎncă nu există evaluări
- Retinal DetachmentDocument3 paginiRetinal DetachmentRownald Lakandula PanuncialÎncă nu există evaluări
- DR - Erlyn EATING DISORDERS (2011)Document35 paginiDR - Erlyn EATING DISORDERS (2011)Nur faidahÎncă nu există evaluări
- Sertifikat Webinar 25 Juli 2020 NutritionDocument2 paginiSertifikat Webinar 25 Juli 2020 NutritionKemal TaufikÎncă nu există evaluări
- Primary Open-Angle Glaucoma: Review ArticleDocument12 paginiPrimary Open-Angle Glaucoma: Review ArticleKemal TaufikÎncă nu există evaluări
- #Galaxytheme #Galaxytheme #Galaxytheme #GalaxythemeDocument3 pagini#Galaxytheme #Galaxytheme #Galaxytheme #GalaxythemeKemal TaufikÎncă nu există evaluări
- Management of The Fetus in Transverse LieDocument6 paginiManagement of The Fetus in Transverse LieKemal TaufikÎncă nu există evaluări
- #Galaxytheme #Galaxytheme #Galaxytheme #GalaxythemeDocument3 pagini#Galaxytheme #Galaxytheme #Galaxytheme #GalaxythemeKemal TaufikÎncă nu există evaluări
- Skorin20020628 PDFDocument3 paginiSkorin20020628 PDFdigimon666Încă nu există evaluări
- 14 PDFDocument13 pagini14 PDFKemal TaufikÎncă nu există evaluări
- Lembar Diskusi EkgDocument3 paginiLembar Diskusi EkgKemal TaufikÎncă nu există evaluări
- Primary Retinal Detachment: Clinical PracticeDocument9 paginiPrimary Retinal Detachment: Clinical PracticeKemal TaufikÎncă nu există evaluări
- Cases Journal: Rhegmatogenous Retinal Detachment After A Lower Extremity Dog Bite: A Case ReportDocument6 paginiCases Journal: Rhegmatogenous Retinal Detachment After A Lower Extremity Dog Bite: A Case ReportKemal TaufikÎncă nu există evaluări
- Fluid Managment in Patient With TraumaDocument9 paginiFluid Managment in Patient With TraumaKemal TaufikÎncă nu există evaluări
- Antihistamin PDFDocument7 paginiAntihistamin PDFKarina Mega W100% (1)
- Pinkeye ST YesDocument3 paginiPinkeye ST YesKemal TaufikÎncă nu există evaluări
- Tugas Translate Coass RevDocument13 paginiTugas Translate Coass RevKemal TaufikÎncă nu există evaluări
- Os Laserasi Palpebra Superior Full ThicknessDocument30 paginiOs Laserasi Palpebra Superior Full ThicknessKemal TaufikÎncă nu există evaluări
- Ophthalmology PDFDocument28 paginiOphthalmology PDFKukuh Rizwido PrasetyoÎncă nu există evaluări
- Pathophysiology of Heart Disease, Lilly, 5th Edition, 2011Document1 paginăPathophysiology of Heart Disease, Lilly, 5th Edition, 2011Kemal TaufikÎncă nu există evaluări
- TandaDocument1 paginăTandaKemal TaufikÎncă nu există evaluări
- 6 Art:10.1186/s12886-015-0134-8Document9 pagini6 Art:10.1186/s12886-015-0134-8Kemal TaufikÎncă nu există evaluări
- CTEVDocument10 paginiCTEVKemal TaufikÎncă nu există evaluări
- Adhesive Capsulitis of The ShoulderDocument7 paginiAdhesive Capsulitis of The ShoulderKemal TaufikÎncă nu există evaluări
- High Mechanical Strain of Primary IntervertebralDocument27 paginiHigh Mechanical Strain of Primary IntervertebralKemal TaufikÎncă nu există evaluări
- 8 Emedicine MedscapeDocument17 pagini8 Emedicine MedscapeKemal Taufik100% (1)
- v2 Molusco Contagioso em Criancas Tratamentos ComparativosDocument4 paginiv2 Molusco Contagioso em Criancas Tratamentos ComparativosKemal TaufikÎncă nu există evaluări
- Molluscum Contagiosum and WartsDocument8 paginiMolluscum Contagiosum and WartscefalalgiaÎncă nu există evaluări
- Varicella GuidelineDocument6 paginiVaricella GuidelineMonika Margareta Maria ElviraÎncă nu există evaluări
- Oxygen AdministrationDocument29 paginiOxygen AdministrationKemal TaufikÎncă nu există evaluări
- Molluscum Contagiosum 2014 FinalDocument20 paginiMolluscum Contagiosum 2014 FinalKemal TaufikÎncă nu există evaluări
- Vaccination BOON or BANEDocument5 paginiVaccination BOON or BANERushil BhandariÎncă nu există evaluări
- Students Sleep During Classes: The Amount of Time VariesDocument7 paginiStudents Sleep During Classes: The Amount of Time Variesjason_aaÎncă nu există evaluări
- Unit - 1 Concepts and Definitions 1.1 Disaster (I)Document25 paginiUnit - 1 Concepts and Definitions 1.1 Disaster (I)RISHITHA LELLAÎncă nu există evaluări
- AcupunctureDocument10 paginiAcupunctureAngel Iulian Popescu0% (2)
- General Practitioner Sample Resume WWW - Careerfaqs.com - AuDocument3 paginiGeneral Practitioner Sample Resume WWW - Careerfaqs.com - AuSubhash RitwalÎncă nu există evaluări
- Adani Targets Debt Cuts, Income Boost Coastal Shipping To Get Infra Status, Says SonowalDocument20 paginiAdani Targets Debt Cuts, Income Boost Coastal Shipping To Get Infra Status, Says SonowalboxorÎncă nu există evaluări
- Leptospirosis PDFDocument48 paginiLeptospirosis PDFTuan HaikalÎncă nu există evaluări
- Pharmaceuticals Manufacturing - What Do We Know About The Occupational Health and Safety Hazards For Women Working in The Industry PDFDocument61 paginiPharmaceuticals Manufacturing - What Do We Know About The Occupational Health and Safety Hazards For Women Working in The Industry PDFCostas JacovidesÎncă nu există evaluări
- Diana Barnett Course Critique n5327 RDocument4 paginiDiana Barnett Course Critique n5327 Rapi-308950624Încă nu există evaluări
- Addressing The Gaps in Nutritional Care Before and During PregnancyDocument12 paginiAddressing The Gaps in Nutritional Care Before and During PregnancyBushra KainaatÎncă nu există evaluări
- Health 8 - 1st Grading ExamDocument3 paginiHealth 8 - 1st Grading Exammaria luzÎncă nu există evaluări
- APA Citations For Nursing TextbooksDocument1 paginăAPA Citations For Nursing Textbooksbbianca199075% (4)
- SuctioningDocument6 paginiSuctioningCriselda Ultado100% (2)
- GENDER Reseach 100%3Document46 paginiGENDER Reseach 100%3Mesud GemechuÎncă nu există evaluări
- Overcoming Obesogenic Environments: A Qualitative Study Exploring Mechanisms of Healthy EatersDocument10 paginiOvercoming Obesogenic Environments: A Qualitative Study Exploring Mechanisms of Healthy EatersCristina Saldias PorrasÎncă nu există evaluări
- Tcharestresumefinal 1009Document2 paginiTcharestresumefinal 1009tcharestÎncă nu există evaluări
- Personality Disorders PDFDocument35 paginiPersonality Disorders PDFABHINAVÎncă nu există evaluări
- ProQual Fees Schedule June 2021Document19 paginiProQual Fees Schedule June 2021Sohail SÎncă nu există evaluări
- 2018 MUSE Inspire Conference - Show and Tell SessionsDocument13 pagini2018 MUSE Inspire Conference - Show and Tell SessionsMichele LambertÎncă nu există evaluări
- ESI ER CompleteDocument45 paginiESI ER Completetammy2121Încă nu există evaluări
- Typology of Nursing Problems in Family Nursing PracticeDocument4 paginiTypology of Nursing Problems in Family Nursing PracticeLeah Abdul KabibÎncă nu există evaluări
- 50 Item Psychiatric Nursing Exam IDocument11 pagini50 Item Psychiatric Nursing Exam Iɹǝʍdןnos98% (40)
- Correlation Between Body Mass Index and Heart Rate in Males and Females of Different Age GroupDocument7 paginiCorrelation Between Body Mass Index and Heart Rate in Males and Females of Different Age GroupAdriel Jian NaldoÎncă nu există evaluări
- Fatima's CommissionDocument7 paginiFatima's CommissionSachie Daniela CheungÎncă nu există evaluări
- Inguinal Hernias: BMJ (Online) March 2008Document5 paginiInguinal Hernias: BMJ (Online) March 2008Karl PinedaÎncă nu există evaluări
- Research Chapter 1 V Final Autosaved 2 1Document57 paginiResearch Chapter 1 V Final Autosaved 2 1Mirate JessÎncă nu există evaluări
- Lab Report 15438869 20231127064225Document1 paginăLab Report 15438869 20231127064225carilloabhe21Încă nu există evaluări
- CSP Whiplash GuidelineDocument199 paginiCSP Whiplash GuidelineyaasarloneÎncă nu există evaluări
- A Combined Patient and Provider Intervention For Management of Osteoarthritis in VeteransDocument13 paginiA Combined Patient and Provider Intervention For Management of Osteoarthritis in VeteransHarshoi KrishannaÎncă nu există evaluări
- Medical Surgical Nursing 3 BulletsDocument4 paginiMedical Surgical Nursing 3 BulletsQueen ElizabethÎncă nu există evaluări