Documente Academic
Documente Profesional
Documente Cultură
OK + Poi160044
Încărcat de
Nofiyanty NicolasTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
OK + Poi160044
Încărcat de
Nofiyanty NicolasDrepturi de autor:
Formate disponibile
Research
JAMA Pediatrics | Original Investigation
Kidney Outcomes 5 Years After Pediatric Cardiac Surgery
The TRIBE-AKI Study
Jason H. Greenberg, MD, MHS; Michael Zappitelli, MD, MSc; Prasad Devarajan, MD;
Heather R. Thiessen-Philbrook, MMath; Catherine Krawczeski, MD; Simon Li, MD, MPH;
Amit X. Garg, MD; Steve Coca, DO, MS; Chirag R. Parikh, MD, PhD; for the TRIBE-AKI Consortium
Supplemental content
IMPORTANCE Acute kidney injury (AKI) after pediatric cardiac surgery is associated with high
short-term morbidity and mortality; however, the long-term kidney outcomes are unclear.
OBJECTIVE To assess long-term kidney outcomes after pediatric cardiac surgery and to
determine if perioperative AKI is associated with worse long-term kidney outcomes.
DESIGN, SETTING, AND PARTICIPANTS This prospective multicenter cohort study recruited
children between ages 1 month to 18 years who underwent cardiopulmonary bypass for
cardiac surgery and survived hospitalization from 3 North American pediatric centers
between July 2007 and December 2009. Children were followed up with telephone calls
and an in-person visit at 5 years after their surgery.
EXPOSURES Acute kidney injury defined as a postoperative serum creatinine rise from
preoperative baseline by 50% or 0.3 mg/dL or more during hospitalization for cardiac
surgery.
MAIN OUTCOMES AND MEASURES Hypertension (blood pressure ⱖ95th percentile for height,
age, sex, or self-reported hypertension), microalbuminuria (urine albumin to creatinine ratio
>30 mg/g), and chronic kidney disease (serum creatinine estimated glomerular filtration rate
[eGFR] <90 mL/min/1.73 m2 or microalbuminuria).
RESULTS Overall, 131 children (median [interquartile range] age, 7.7 [5.9-9.9] years)
participated in the 5-year in-person follow-up visit; 68 children (52%) were male. Fifty-seven
of 131 children (44%) had postoperative AKI. At follow-up, 22 children (17%) had hypertension
(10 times higher than the published general pediatric population prevalence), while 9 (8%),
13 (13%), and 1 (1%) had microalbuminuria, an eGFR less than 90 mL/min/1.73 m2, and an eGFR
less than 60 mL/min/1.73 m2, respectively. Twenty-one children (18%) had chronic kidney
disease. Only 5 children (4%) had been seen by a nephrologist during follow-up. There was no
significant difference in renal outcomes between children with and without postoperative AKI.
CONCLUSIONS AND RELEVANCE Chronic kidney disease and hypertension are common 5 years
after pediatric cardiac surgery. Perioperative AKI is not associated with these complications.
Longer follow-up is needed to ascertain resolution or worsening of chronic kidney disease
and hypertension.
Author Affiliations: Author
affiliations are listed at the end of this
article.
Group Information: The
Translational Research Investigating
Biomarker Endpoints in Acute Kidney
Injury (TRIBE-AKI) Consortium
investigators are listed at the end of
this article.
Corresponding Author: Chirag
Parikh, MD, PhD, Yale Program of
Applied Translational Research,
60 Temple St, 6th Floor, Ste 6C,
JAMA Pediatr. 2016;170(11):1071-1078. doi:10.1001/jamapediatrics.2016.1532 New Haven, CT 06510
Published online September 12, 2016. (chirag.parikh@yale.edu).
(Reprinted) 1071
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/peds/935842/ by a Sam Ratulangi University Hospital User on 04/03/2017
Research Original Investigation Kidney Outcomes 5 Years After Pediatric Cardiac Surgery
P
ediatric acute kidney injury (AKI) is a significant health
concern because it is associated with inpatient mortal- Key Points
ity and length of hospital stay.1,2 Acute kidney injury is
Question What are the 5-year kidney outcomes after pediatric
estimated to occur in 25% to 60% of children undergoing car- cardiac surgery and is perioperative acute kidney injury a risk
diac surgery.3,4 The mechanism of AKI after cardiac surgery factor for worse outcomes?
is multifactorial, including systemic inflammatory response
Findings Hypertension and chronic kidney disease were common
to cardiopulmonary bypass, renal ischemia, oxidative stress,
5 years after cardiac surgery. Acute kidney injury was not a risk
microemboli, and reperfusion injury.5 factor for worse outcomes.
It is currently unknown whether an episode of AKI in any
Meaning These findings will provide data to begin making
pediatric population is associated with permanent renal dam-
recommendations for renal follow-up after cardiac surgery
age and progressive decline in kidney function. Previous stud-
in children.
ies in children have reported on long-term outcomes in pa-
tients with AKI without any suitable controls.6 Therefore, the
relative risk of long-term outcomes after pediatric AKI re- Study Visits
mains unknown. There is a robust association between AKI and Once the participant was recruited into this long-term fol-
chronic kidney disease (CKD) in adults.7 Recent evidence from low-up study, he or she was followed up annually by tele-
a large prospective cohort study in adults also supports the as- phone until a 5-year in-person visit. The telephone calls con-
sociation of AKI with a long-term risk of hypertension.8 This sisted of detailed questionnaires focused on interim medical
potential association of AKI with hypertension and CKD in history, hospitalizations, diagnosis of hypertension, dialysis
children is crucial to elucidate because they are important and requirement, medical visits for a kidney problem, current medi-
potentially treatable cardiovascular risk factors. Moreover, cur- cations, and interim laboratory testing. Five-year in-person vis-
rent AKI guidelines in children do not provide recommenda- its were performed by a research nurse at the hospital clinic
tions for long-term follow-up, primarily due to a lack of stud- or at the participant’s home (per family preference). Height,
ies with reliable evidence. weight, and blood pressure were measured, and blood and
The long-term risk of renal complications is increasingly urine were collected at the time of the visits scheduled by par-
important as the outcomes of children after cardiac surgery ticipant availability. Height was measured with a SECA stadi-
have improved dramatically and more children are surviving ometer (SECA) and weight was measured with a Precision
to adulthood.9,10 An excess burden of renal disease has been Health Scale (A&D Engineering). Percentiles and z scores of
reported in adults with congenital heart disease but has not height, weight, and body mass index (BMI; calculated as weight
been elucidated in children.11,12 The goal of the present study in kilograms divided by height in meters squared) were cal-
was to assess long-term renal outcomes after cardiac surgery culated using Centers for Disease Control and Prevention
and determine if perioperative AKI is associated with these growth charts.15 Blood pressures were measured with an ap-
outcomes. propriate-size cuff using the Omron HEM-711AC home blood
pressure monitor (Omron Healthcare, Inc). The blood pres-
sure monitor was standardized and annually calibrated at each
of the participating institutions. The average of 3 blood pres-
Methods sure measurements at each visit were used to calculate the
Study Cohort blood pressure percentile. If the average blood pressure was
This is a prospective longitudinal cohort study of children with greater than the 95th percentile, the blood pressure was re-
congenital cardiac defects who were enrolled between July measured manually. Blood pressure percentiles were calcu-
2007 and December 2009. Children who were 1 month to 18 lated as per The Fourth Report on the Diagnosis, Evaluation,
years old undergoing cardiac surgery with cardiopulmonary and Treatment of High Blood Pressure in Children and
bypass at Cincinnati Children’s Hospital, Montreal Children’s Adolescents.15 During the visit, other details on the medical
Hospital, and Yale New Haven Children’s Hospital, were en- history, interim hospital admissions, medication history, and
rolled in the Translational Research Investigating Biomarker laboratory testing since cardiac surgery were also collected. Dis-
Endpoints in AKI (TRIBE-AKI) study.3,13,14 Children were ex- charge summaries from hospital admissions and other medi-
cluded if they had a history of renal transplantation or dialy- cal records were obtained for each hospitalization from the re-
sis. Details around patient recruitment before the cardiac sur- spective medical institutions. Full details of the analyte
gery were published previously.3,13,14 Before discharge from the measurements, including sample collection and processing,
cardiac surgery hospitalization, children were invited to par- are included in the eMethods in the Supplement.
ticipate in follow-up studies along with permission for future
contact. At a median of 3 years after discharge from the index Data From the Index Cardiac Surgery Admission
hospitalization, the children who consented to future con- The following detailed index cardiac surgery admission infor-
tact were invited to participate in the current study. In- mation was available in all participants from our prior in-
formed consent was obtained from all parents or legal guard- hospital study: preoperative characteristics, operative de-
ians, along with assent, when appropriate, from children. This tails, and postoperative complications using the definitions of
study was approved by the institutional review board of each the Society of Thoracic Surgeons.16 We used the risk adjust-
participating institution. ment for congenital heart surgery-1 (RACHS-1) consensus-
1072 JAMA Pediatrics November 2016 Volume 170, Number 11 (Reprinted) jamapediatrics.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/peds/935842/ by a Sam Ratulangi University Hospital User on 04/03/2017
Kidney Outcomes 5 Years After Pediatric Cardiac Surgery Original Investigation Research
based scoring system to categorize the complexity of surgery.16
Figure 1. TRIBE-AKI Study Population
Higher scores signify more complex surgeries. This method of
risk stratification is a widely accepted tool for the evaluation
311 Patients enrolled in
of differences in outcomes of surgery for congenital heart dis- perioperative cohort
ease. Acute kidney injury was defined as the development of
at least stage I AKI, defined by Acute Kidney Injury Network 6 In-hospital deaths
(AKIN)17 as at least a 50% or more increase or a 0.3 mg/dL (to
convert mg/dL to μmol/L, multiply by 88.4) or more increase 305 Patients survived
from baseline serum creatinine during hospitalization after car- index hospitalization
diac surgery. We also analyzed the outcome of stage II AKI, de- 105 Patients declined future
contact
fined as receiving acute dialysis during the hospital stay or a
200 Patients eligible
doubling in serum creatinine from baseline. We measured uri- for consent
nary biomarkers of tubular injury (neutrophil gelatinase– 4 Deaths after discharge
associated lipocalin [NGAL], interleukin 18 [IL-18], kidney in- 49 Patients declined consent
16 Patients lost to follow-up
jury molecule 1 [KIM-1], and liver fatty acid–binding protein
131 Patients completed
[L-FABP]) on the preoperative and first postoperative day and a 5-year in-person
assessed the relationship of these biomarkers with 5-year visit
renal outcomes. Details of the in-hospital study have been
previously described.3,13,14 Translational Research Investigating Biomarker Endpoints in Acute Kidney
Injury (TRIBE-AKI) long-term follow-up cohort selection process.
Outcome Definitions
For participants up to age 18 years, hypertension was defined the outcomes of hypertension, microalbuminuria, and CKD.
as systolic or diastolic blood pressure greater than or equal to SAS version 9.4 (SAS Institute Inc) was used for analyses.
the 95th percentile for age, height, and sex.15 For participants
older than 18 years, hypertension was defined as systolic or
diastolic blood pressure greater than 140 mm Hg or greater
than 90 mm Hg, respectively.18 Prehypertension was defined
Results
as a systolic or diastolic blood pressure from the 90th to the Of the 311 children enrolled in the original TRIBE-AKI pediat-
95th percentile in children 18 years or younger. For patients ric cohort, 305 children survived the index hospitalization;
older than 18 years old, prehypertension was defined as sys- 105 children declined future contact, which left 200 children
tolic or diastolic blood pressure 120 mm Hg to 139 mm Hg or eligible for participation in the follow-up study. After various
80 mm Hg to 89 mm Hg, respectively. Additionally, partici- exclusions, 131 children, at a mean of 5.4 years after surgery,
pants were classified as having hypertension if they reported agreed to in-person follow-up (Figure 1). Baseline character-
a history of hypertension. Estimated glomerular filtration istics were not significantly different between children that par-
rate (eGFR) was calculated using the Chronic Kidney Disease ticipated in the long-term follow-up vs did not (eTable 1 in the
in Children study (CKiD) serum creatinine–based equation.19 Supplement). Patient baseline characteristics along with their
Additionally we calculated cystatin C–based eGFR and com- preoperative medications at the time of cardiac surgery by AKI
bined serum creatinine-cystatin C–based eGFR using the status are shown in Table 1. Several patients were taking medi-
CKiD-derived equations.19,20 Microalbuminuria was defined cations for optimization of hemodynamics that also lower
as urine albumin to creatinine ratio greater than 30 mg/g. blood pressure. Children with AKI had a younger median age
Chronic kidney disease was defined as an eGFR less than (P = .05). The median (interquartile range [IQR]) age of the co-
90 mL/min/1.73 m2 or microalbuminuria.21 hort at the 5-year follow-up was 7.7 (5.9-9.9) years, and 68 chil-
dren (52%) were male. Overall, 57 children (44%) had experi-
Statistical Analysis enced AKI after their index cardiac surgery. Median height and
Baseline characteristics of those who completed and did not weight z scores of the cohort were −0.56 and −0.14 at 5 years
complete follow-up visits were compared. Of the 131 partici- after cardiac surgery and did not significantly differ by AKI sta-
pants with follow-up visits, all had blood pressure measure- tus (Table 2). Median BMI z score was 0.36 and significantly
ments or responded to the questionnaire regarding hyperten- lower in children with AKI compared with children without
sion, 116 had urine samples taken, and 101 had blood samples AKI (P = .01).
taken. For each outcome, only those participants with non-
missing values were included in the analysis. Five-Year Renal Outcomes
Continuous variables were compared with 2-sample t test Glomerular Filtration Rate
or Wilcoxon rank sum test and dichotomous variables with the Blood samples were available on 101 of 131 children to assess
χ2 test or Fisher exact test. Five-year outcome prevalence con- eGFR. At follow-up, median (IQR) eGFR in children with and
fidence intervals were calculated with the Wilson score without AKI was not significantly different: 118 (105-132) mL/
method. We performed multivariate analyses to examine the min/1.73 m2 and 108 (93-121) mL/min/1.73 m2, respectively,
association between the baseline covariates of age, sex, race, using the serum creatinine–based CKiD equation (P = .09)
preoperative GFR, and postoperative serum creatinine rise with (Table 2). Estimated GFR less than 90 mL/min/1.73 m2 was
jamapediatrics.com (Reprinted) JAMA Pediatrics November 2016 Volume 170, Number 11 1073
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/peds/935842/ by a Sam Ratulangi University Hospital User on 04/03/2017
Research Original Investigation Kidney Outcomes 5 Years After Pediatric Cardiac Surgery
Table 1. Baseline and Postoperative Characteristics of Study Cohort by AKI Status
No. (%)
Overall AKI Group Non-AKI Group
Characteristic (n = 131) (n = 57) (n = 74) P Value
Preoperative/baseline
Age, median (IQR), mo 31.9 (6.0-58.6) 13 (5.8-48.7) 38 (7.4-68.9) .05
Male sex 68 (52) 32 (56) 36 (49) .39
Abbreviations: AKI, acute kidney
Nonwhite 20 (15) 10 (18) 10 (14) .52
injury; CRRT, continuous renal
Preoperative estimated SCr-GFR, 78 (93-110) 97 (78-126) 89 (81-101) .08 replacement therapy;
median (IQR) GFR, glomerular filtration rate;
Preoperative SCr-eGFR, mg/dL, 26 (20) 5 (9) 21 (29) .005 IQR, interquartile range; RACHS-1, risk
abnormal for agea adjustment for congenital heart
Preoperative urine albumin to creatinine 23.6 (10.9-75.5) 23.6 (11.9-88.5) 24.0 (10.5-72.1) .14 surgery; SCr, serum creatinine.
ratio, mg/g
b
SI conversion factor: To convert
Preoperative microalbuminuria 26 (20) 11 (19) 15 (20) .56 creatinine to micromoles per liter,
c
Preoperative CKD 48 (37) 16 (28) 32 (43) .07 multiply by 88.4.
a
RACHS-1 surgical category Defined as age-based GFR
1 7 (5) 0 7 (9) <.001 thresholds: 2 years or older, less
than 90 mL/min/1.73 m2; 1.5 to 2.0
2 66 (51) 26 (46) 40 (54) years, less than 76 mL/min/1.73 m2;
3 52 (40) 25 (45) 27 (36) 1 to 1.5 years, less than
4 5 (4) 5 (9) 0 74 mL/min/1.73 m2; younger than 1
year, less than 65 mL/min/1.73 m2;
Type of surgery 3 months to 8 months old, less than
Septal defect repair 44 (36) 18 (33) 26 (38) .41 58 mL/min/1.73 m2.
b
Inflow/outflow tract or valve procedure 23 (19) 8 (15) 15 (22) Preoperative microalbuminuria
defined by age-based albumin to
Combined procedure 56 (46) 28 (52) 28 (41)
creatinine ratio thresholds: older
Index hospitalization than 2 years, more than 30 mg/g;
Peak postoperative SCr rise from baseline, 0.2 (0.3-0.7) 0.7 (0.5-1) 0.2 (0, 0.3) <.001 6 months to 2 years, more than
mg/dL, median (IQR) 75 mg/g.
Renal replacement 3 (2) 3 (5) 0 .04 c
Preoperative CKD defined as eGFR
CRRT, No. (%) 1 (33) 1 (33) 0 less than than age-based thresholds
or microalbuminuria more than
Peritoneal dialysis, No. (%) 2 (67) 2 (67) 0
age-based thresholds.
identified in 13 children (13%), and an eGFR less than discharge from the index hospitalization. Children with CKD
60 mL/min/1.73 m2 in 1 child (1%). All 13 children with an 5 years after cardiac surgery had a lower preoperative eGFR
eGFR less than 90 mL/min/1.73 m 2 were in the non-AKI (median [IQR]. 83 [72-89] mL/min/1.73 m2) compared with
group. Table 3 displays eGFR results using other estimating patients without CKD (median [IQR], 96 [83-115] mL/min/
equations. Using a cystatin C–based eGFR equation, we 1.73 m2) (P = .02) (eTable 2 in the Supplement). The presence
identified 17 participants with AKI and 24 participants with- of any AKI or of stage II AKI or worse was not associated
out AKI with an eGFR between 60 mL/min/1.73 m 2 and with a higher prevalence of 5-year CKD (Table 2) (eTables 3
90 mL/min/1.73 m2. and 4 in the Supplement).
Albuminuria Hypertension
Urine samples were available for 116 of 131 children to mea- We determined hypertension status on the entire cohort of
sure albuminuria. At the 5-year follow-up visit, microalbu- 131 children through either blood pressure measurement (18
minuria was identified in 3 children (6%) with AKI and 6 chil- patients) or self-history (6 patients). Systolic hypertension was
dren (9%) without AKI (P = .54). The median (IQR) albumin to found in 5 children (9%) with AKI and 9 children (12%) with-
creatinine ratio in children with AKI was 5.92 (2.80-10.40) mg/g out AKI. Diastolic hypertension was found in 0 children with
and 4.88 (2.00-13.80) mg/g in children without AKI (P = .88). AKI and 4 children (5%) without AKI. There was no signifi-
There was no difference in proteinuria by dipstick in children cant difference in hypertension between children with and
with and without AKI (P = .49). without perioperative AKI. Additionally, baseline age, sex, race,
preoperative GFR, and postoperative serum creatinine in-
Chronic Kidney Disease crease were not associated with 5-year hypertension. Over-
Chronic kidney disease, defined as the composite of eGFR all, hypertension (systolic or diastolic) was identified in 17%
less than 90 mL/min/1.73 m2 or microalbuminuria, was pres- of children and prehypertension (systolic or diastolic) was iden-
ent in 21 children (18%), 3 children with AKI (6%), and 18 tified in an additional 9% of children (Table 2). Seven chil-
children without AKI (27%) (P = .01). Overall, 37 children dren were being treated for hypertension or kidney disease.
(30%) had an eGFR less than 90 mL/min/1.73 m2, microalbu- Only 5 children (4%) were being followed up by a pediatric ne-
minuria, or hypertension. No children required dialysis since phrologist. Figure 2 shows the prevalence of hypertension in
1074 JAMA Pediatrics November 2016 Volume 170, Number 11 (Reprinted) jamapediatrics.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/peds/935842/ by a Sam Ratulangi University Hospital User on 04/03/2017
Kidney Outcomes 5 Years After Pediatric Cardiac Surgery Original Investigation Research
Table 2. Five-Year Outcomes by AKI Status
Overall AKI Group Non-AKI Group
Characteristics (n = 131) (n = 57) (n = 74) P Value
Height z score, median (IQR) −0.56 (−1.6 to 0.5) −0.58 (−1.43 to −0.18) −0.52 (−1.74 to −0.74) .90
Weight z score, median (IQR) −0.14 (−1.01 to 0.61) −0.33 (−1.29 to 0.43) −0.08 (−0.73 to 0.74) .16
BMI z score, median (IQR) 0.36 (−0.45 to 1.05) 0.03 (−0.92 to 0.66) 0.49 (−0.14 to 1.14) <.001
Patients enrolled in school, No. (%) 117 (90) 48 (86) 69 (93) .16
Patients enrolled in special education, No. (%) 42 (36) 20 (42) 22 (32) .28
Any form of dialysis 0 0 0 NA
Nephrologist follow-up, No. (%) 5 (4) 2 (4) 3 (4) .86
Family history of renal disease, No. (%) 61 (47) 25 (44) 36 (49) .56
At least 1 hospital/ED readmission, No. (%) 32 (24) 12 (21) 20 (27) .43
GFRa
eGFR, median (IQR) 101 (112-126) 118 (105-132) 108 (93-121) .01
2
eGFR<90 mL/min/1.73 m , No. (%) 13 (13) 0 13 (22) <.001
eGFR<60 mL/min/1.73 m2, No. (%) 1 (1) 0 1 (2) .39
Albuminuria, No. (%)
Proteinuriab
Negative 109 (90) 44 (86) 65 (93)
Trace 5 (4) 3 (6) 2 (3) .49
Small 7 (6) 4 (8) 3 (4)
Large 0 0 0
Albumin to creatinine ratio, mg/g, median (IQR) 5.1 (2.39-12.13) 5.92 (2.76-10.43) 4.88 (1.96-13.78) .87
Microalbuminuriac 9 (8) 3 (6) 6 (9) .54
CKD,d No. (%) 21 (18) 3 (6) 18 (27) <.001
Hypertension
Systolic BP z score, median (IQR) 0.41 (−0.21 to 1.03) 0.45 (−0.31 to 1.01) 0.41 (−0.17 to 1.1) .62
Systolic pre-HTN, No. (%) 12 (9) 3 (5) 9 (12) .29
Systolic HTN, No. (%) 14 (11) 5 (9) 9 (12) .29
Diastolic BP z score, median (IQR) −0.01 (−0.27 to 0.35) −0.1 (−0.32 to 0.26) 0.03 (−0.25 to 0.46) .15
Diastolic pre-HTN, No. (%) 8 (6) 2 (4) 6 (8) .11
Diastolic HTN, No. (%) 4 (3) 0 4 (5) .11
Pre-HTN, No. (%) 12 (9) 3 (5) 9 (12) .29
HTN,e No. (%) 22 (17) 6 (11) 16 (22) .09
b
Abbreviations: AKI, acute kidney injury; BMI, body mass index (calculated as Proteinuria measured by urine dipstick.
weight in kilograms divided by height in meters squared); BP, blood pressure; c
Microalbuminuria defined as more than 30 mg/g.
CKD, chronic kidney disease; ED, emergency department; eGFR, estimated d
Chronic kidney disease defined as the composite of estimated GFR less than
GFR; GFR, glomerular filtration rate; HTN, hypertension; IQR, interquartile
90 mL/min/1.73 m2 or microalbuminuria.
range; NA, not available; SCr, serum creatinine.
e
Hypertension defined by BP or self-report.
SI conversion factor: To convert creatinine to micromoles per liter, multiply by
88.4.
a
Estimated GFR calculated with SCr–based Chronic Kidney Disease in Children
Study equation.19
Table 3. Comparing 5-Year Kidney Function Outcomes Using 3 Pediatric GFR Estimating Equations
AKI Group Non-AKI Group
Pediatric Estimating Equations eGFR eGFR <90 eGFR eGFR <90
Renal Measurement Name Equation Median (IQR) No. (%) Median (IQR) No. (%)
Creatinine CKiD19 0.413 × ht/Cr 118 (105-132) 0 108 (93-121) 13 (22)
Cystatin C CKiD20 70.69 × CysC−0.931 92 (87-99) 18 (42) 89 (83-101) 30 (52)
Creatinine and cystatin C CKiD19 41.6 (ht/Cr)0.599 × (1.8/CysC)0.317 101 (95-111) 2 (5) 96 (87-105) 20 (34)
Abbreviations: AKI, acute kidney injury; CKiD, Chronic Kidney Disease in Children Study; Cr, serum creatinine; CysC, cystatin C; eGFR, estimated glomerular filtration
rate (mL/min/1.73 m2); ht, height; IQR, interquartile range.
jamapediatrics.com (Reprinted) JAMA Pediatrics November 2016 Volume 170, Number 11 1075
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/peds/935842/ by a Sam Ratulangi University Hospital User on 04/03/2017
Research Original Investigation Kidney Outcomes 5 Years After Pediatric Cardiac Surgery
disease in our cohort. However, hypertension is not typical in
Figure 2. Hypertension Prevalence Among Pediatric Center Cohorts
Included in the TRIBE-AKI Study
this pediatric population. Long-term risk of hypertension
has been described previously after coarctation repair but
18 not after surgery in a diverse group of congenital cardiac
16 conditions.27,28 The hypertension identified in this cohort is
likely multifactorial and may have several underlying mecha-
14
Hypertension Prevalence, %
nisms such as an upregulated renin-angiotensin system in an
12 attempt to preserve renal perfusion, a disturbance of cardiac
10 receptors during surgery leading to enhanced sympathetic ac-
tivity, and the development of either clinical or subclinical
8
CKD.29,30 Chronic kidney disease in our patients may be caused
6
by chronic renal hypoperfusion and neurohormonal activa-
4 tion owing to congenital heart disease and/or the observed
2
hypertension.11 Despite the high prevalence of hypertension
and CKD after cardiac surgery, only 7 children were being
0
TRIBE-AKI Kaiser Northeast NHANES treated for hypertension or kidney disease. Treatment of hy-
Ohio
pertension and CKD in childhood is critical because these risk
Pediatric Cohorts
factors in children are associated with increased cardiovascu-
Comparison of hypertension prevalence in 4 pediatric cohorts from the
lar outcomes in adults.26,31 The impact of CKD and hyperten-
Translational Research Investigating Biomarker Endpoints in Acute Kidney sion is especially relevant in children with congenital heart dis-
Injury (TRIBE-AKI) pediatric cohort 5 years after cardiac surgery, the National ease because they are a high-risk population for long-term
Health and Nutrition Examination Survey (NHANES), the Kaiser Permanente
cardiac events.32,33
health care system, and a large urban medical system in Northeast Ohio
(eTable 3 in the Supplement). The NHANES, Kaiser, and Northeast Ohio Prior studies12 have performed cross-sectional analyses ex-
cohorts were identified through a literature review. amining CKD and hypertension in individuals with congeni-
tal heart disease. In a study of 9952 children and adults with
congenital heart disease and 29 837 matched controls, con-
3 other published pediatric cohorts demonstrating that genital heart disease conferred a 1.4-fold higher risk (95% CI,
the current cohort had substantially higher hypertension 1.3-1.5) of hypertension and a 3.4-fold higher risk (95% CI, 2.3-
prevalence.22-24 Detailed characteristics of these 3 cohorts are 5.1) of CKD.12 These findings are relevant to our research but
described in eTable 5 in the Supplement. not generalizable because only 25% of children with congen-
ital heart disease require cardiac surgery.34 Our research sug-
Perioperative Biomarker Results and 5-Year Risk gests that the excess burden of CKD and hypertension previ-
of Renal Outcomes ously identified in adults with congenital heart disease may
We examined the relationship between perioperative bio- indeed develop during childhood.
marker levels and 5-year outcomes. There was no association There are more than 20 studies in adults that have dem-
between preoperative urinary biomarkers of kidney injury onstrated an association of AKI with long-term outcomes such
(ie, albumin, NGAL, KIM-1, IL-18, L-FABP) and CKD or hyper- as CKD and more recently hypertension.8,35 This association
tension at the 5-year follow-up (eTables 6-8 in the Supple- has also been seen in AKI after cardiac bypass surgery in
ment). Additionally, none of the first postoperative (0-hour to adults.36 We have previously shown that pediatric AKI after
6-hour time point) urinary biomarkers were independently cardiac surgery affected short-term outcomes such as length
associated with 5-year CKD or hypertension. of hospital stay and length of ventilation.3 Thus, the present
study was hypothesized to demonstrate that pediatric AKI, like
adult AKI, would also affect long-term renal outcomes. Inter-
estingly, we found that children without AKI were more likely
Discussion to have CKD. We determined that these children with CKD also
The present study is the first prospective study that we know had an abnormal eGFR prior to cardiac surgery. One potential
of to evaluate long-term renal outcomes after cardiac surgery reason for our lack of association of AKI as a risk factor for long-
in children and its association with perioperative AKI. Though term outcomes could be the superior renal regenerative po-
the prevalence of hypertension and CKD was high at 5 years tential and greater renal reserve in children compared with
after cardiac surgery, we did not detect any increased risk of older adults with diminished nephron mass.37 Furthermore,
renal outcomes after exposure to AKI. children with AKI may develop glomerular hyperfiltration in
The hypertension prevalence in our study population was response to nephron loss, thereby increasing GFR.38
more than 10 times greater than the prevalence in the general Another possible explanation for the lack of an AKI out-
pediatric population.25 This is especially significant and re- come association is that our duration of follow-up was inad-
markable because our cohort was much younger than those equate. Children may need to be followed up for a longer pe-
reported elsewhere22-24,26 and would therefore be expected to riod of time before there is sufficient nephron loss to cause
display a lower prevalence of hypertension. A potential expla- changes in serum creatinine concentration. This is because
nation could be the presence of underlying congenital heart serum creatinine starts to rise only after as much as 50% of
1076 JAMA Pediatrics November 2016 Volume 170, Number 11 (Reprinted) jamapediatrics.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/peds/935842/ by a Sam Ratulangi University Hospital User on 04/03/2017
Kidney Outcomes 5 Years After Pediatric Cardiac Surgery Original Investigation Research
kidney function has been lost.39 A recent study by Cooper et who declined to participate in the long-term follow-up. The
al40 studied 51 children who underwent cardiopulmonary by- exclusion of a large number of children may have produced
pass (33 children with AKI and 18 without) for a mean dura- imprecise results, although the baseline characteristics did
tion of 7 years. Seven years after cardiopulmonary bypass, there not differ between participating and nonparticipating chil-
was no difference in eGFR between children with AKI or with- dren. Finally, we were unable to obtain blood and urine from
out. However, at long-term follow-up, patients in the AKI group some children in this cohort owing to child refusal, parent
demonstrated significantly increased levels of the estab- refusal, or technical factors while collecting biospecimens.
lished tubule injury biomarkers IL-18, KIM-1, and L-FABP when
compared with the age-matched AKI-negative group. This
study suggests the ongoing evolution of subtle subclinical kid-
ney injury and supports the need for long-term follow-up into
Conclusions
and throughout adulthood. Nonetheless, adult studies have We found a high prevalence of hypertension and CKD 5 years
shown that AKI is a risk factor for CKD with a smaller length after pediatric cardiac surgery, but this risk was not associ-
of follow-up.41,42 Furthermore, CKD comorbidities may be an ated with AKI exposure. Despite many children having hyper-
important cofactor and play a vital role in the risk for long- tension and CKD, the majority were not being followed up or
term outcomes after AKI. Comorbidities, such as coronary ar- treated for these medical problems. Approximately 10 000 in-
tery disease, diabetes, smoking, and hypertension, are highly fants with congenital heart disease undergo cardiac surgery
prevalent in adults, whereas children are generally free of these each year in the United States, and our results bear signifi-
comorbidities. cant implications for the early detection and prevention of
The strengths of this study include its prospective design hypertension and CKD in this vulnerable population. These
and 5-year long-term follow-up. This is also the first prospec- findings will provide data needed to begin making recom-
tive study, to our knowledge, to assess long-term outcomes af- mendations for renal follow-up after pediatric cardiac sur-
ter AKI in children and include a representative control group gery. Future studies could consider using ambulatory blood
of patients without AKI. Additionally, no children were lost to pressure monitoring and echocardiogram to more accurately
follow-up after enrollment in the long-term study. The limi- characterize hypertension risk and cardiac function after car-
tations include our sample size, which may have been inad- diac surgery in general, and after cardiac surgery-associated
equate. In addition, we had a substantial number of patients AKI in particular.
ARTICLE INFORMATION Thiessen-Philbrook, Krawczeski, Li, Garg, Coca, the study; collection, management, analysis, and
Accepted for Publication: May 16, 2016. Parikh. interpretation of the data; preparation, review, or
Drafting of the manuscript: Greenberg, Zappitelli, approval of the manuscript; and decision to submit
Published Online: September 12, 2016. Devarajan, Parikh. the manuscript for publication.
doi:10.1001/jamapediatrics.2016.1532 Critical revision of the manuscript for important Group Information: Prasad Devarajan, MD; Charles
Author Affiliations: Section of Nephrology, intellectual content: Greenberg, Zappitelli, Edelstein, MD, PhD; Amit Garg, MD, PhD; Kathleen
Department of Pediatrics, Yale University School of Devarajan, Thiessen-Philbrook, Krawczeski, Li, F. Kerr, PhD; Jay Koyner, MD; Cary Passik, MD; Uptal
Medicine, New Haven, Connecticut (Greenberg); Garg, Coca, Parikh. Dinesh Patel, MD; Michael Shlipak, MD; Michael
Program of Applied Translational Research, Yale Statistical analysis: Zappitelli, Thiessen-Philbrook. Zappitelli, MD, MSc.
University School of Medicine, New Haven, Obtained funding: Zappitelli, Devarajan, Parikh.
Connecticut (Greenberg, Thiessen-Philbrook, Coca, Administrative, technical, or material support: Additional Contributions: We thank Gagan Verma,
Parikh); Division of Pediatric Nephrology, Greenberg, Krawczeski, Parikh. MPH, Program of Applied Translational Research,
Department of Pediatrics, McGill University Health Study supervision: Greenberg, Devarajan, Yale University School of Medicine, for his
Centre, Montreal, Quebec, Canada (Zappitelli); Krawczeski, Parikh. assistance with statistical analyses and data
Nephrology and Hypertension, Cincinnati Children's processing. Prof Verma was not compensated for
Conflict of Interest Disclosures: Dr Devarajan his contributions.
Hospital Medical Center, Cincinnati, Ohio reported being a coinventor on the neutrophil
(Devarajan); Division of Cardiology, Department of gelatinase–associated lipocalin patent. No other
Pediatrics, Stanford University School of Medicine, REFERENCES
conflicts were reported.
Stanford, California (Krawczeski); Division of Critical 1. Sutherland SM, Ji J, Sheikhi FH, et al. AKI in
Care, Department of Pediatrics, Maria Fareri Funding/Support: This study was supported by hospitalized children: epidemiology and clinical
Children’s Hospital, Valhalla, New York (Li); Division the National Institutes of Health (NIH) (grant associations in a national cohort. Clin J Am Soc
of Nephrology, Department of Medicine, Western R01HL085757 to Dr Parikh) to fund the TRIBE-AKI Nephrol. 2013;8(10):1661-1669.
University, London, Ontario, Canada (Garg); Section Consortium to study novel biomarkers of acute
kidney injury in cardiac surgery. Dr Greenberg is 2. Devarajan P. Pediatric acute kidney injury:
of Nephrology, Department of Internal Medicine, different from acute renal failure but how and why.
Mount Sinai School of Medicine, New York, New funded by the T32DK007276-35 training grant to
the Yale University School of Medicine Section of Curr Pediatr Rep. 2013;1(1):34-40.
York (Coca); Section of Nephrology, Department
of Internal Medicine, Yale University School of Nephrology. Dr Devarajan is supported by the NIH 3. Li S, Krawczeski CD, Zappitelli M, et al; TRIBE-AKI
Medicine, New Haven, Connecticut (Parikh); VA (grant P50DK096418). Dr Garg is supported by Consortium. Incidence, risk factors, and outcomes
Medical Center, West Haven, Connecticut (Parikh). Western University’s Dr Adam Linton Chair in of acute kidney injury after pediatric cardiac
Kidney Health Analytics. Dr Parikh is supported by surgery: a prospective multicenter study. Crit Care
Author Contributions: Drs Thiessen-Philbrook and the NIH (grant K24DK090203) and the O'Brien Med. 2011;39(6):1493-1499.
Parikh had full access to all of the data in the study Center (grant P30 DK079310-07). Dr Parikh is also
and take responsibility for the integrity of the data 4. Morgan CJ, Zappitelli M, Robertson CM, et al;
a member of the NIH-sponsored Assess, Serial Western Canadian Complex Pediatric Therapies
and the accuracy of the data analysis. Evaluation, and Subsequent Sequelae in Acute
Study concept and design: Zappitelli, Devarajan, Follow-Up Group. Risk factors for and outcomes
Kidney Injury Consortium (U01DK082185). of acute kidney injury in neonates undergoing
Krawczeski, Li, Coca, Parikh.
Acquisition, analysis, or interpretation of data: Role of the Funder/Sponsor: The funders/ complex cardiac surgery. J Pediatr. 2013;162(1):
Greenberg, Zappitelli, Devarajan, sponsors had no role in the design and conduct of 120-7.e1.
jamapediatrics.com (Reprinted) JAMA Pediatrics November 2016 Volume 170, Number 11 1077
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/peds/935842/ by a Sam Ratulangi University Hospital User on 04/03/2017
Research Original Investigation Kidney Outcomes 5 Years After Pediatric Cardiac Surgery
5. Kwiatkowski DM, Krawczeski CD. Acute kidney 17. Mehta RL, Kellum JA, Shah SV, et al; Acute 29. Wallach R, Karp RB, Reves JG, Oparil S,
injury after cardiovascular surgery in children. In: Kidney Injury Network. Acute Kidney Injury Smith LR, James TN. Pathogenesis of paroxysmal
Thakar CV, Parikh CR, eds. Perioperative Kidney Injury. Network: report of an initiative to improve hypertension developing during and after coronary
New York: Springer; 2015:99-110. outcomes in acute kidney injury. Crit Care. 2007;11 bypass surgery: a study of hemodynamic and
6. Greenberg JH, Coca S, Parikh CR. Long-term risk (2):R31. humoral factors. Am J Cardiol. 1980;46(4):
of chronic kidney disease and mortality in children 18. James PA, Oparil S, Carter BL, et al. 2014 559-565.
after acute kidney injury: a systematic review. BMC evidence-based guideline for the management of 30. Cooper TJ, Clutton-Brock TH, Jones SN,
Nephrol. 2014;15:184. high blood pressure in adults: report from the panel Tinker J, Treasure T. Factors relating to the
7. Chawla LS, Eggers PW, Star RA, Kimmel PL. members appointed to the Eighth Joint National development of hypertension after
Acute kidney injury and chronic kidney disease as Committee (JNC 8). JAMA. 2014;311(5):507-520. cardiopulmonary bypass. Br Heart J. 1985;54(1):
interconnected syndromes. N Engl J Med. 2014;371 19. Schwartz GJ, Muñoz A, Schneider MF, et al. 91-95.
(1):58-66. New equations to estimate GFR in children with 31. Oh J, Wunsch R, Turzer M, et al. Advanced
8. Hsu CY, Hsu RK, Yang J, Ordonez JD, Zheng S, CKD. J Am Soc Nephrol. 2009;20(3):629-637. coronary and carotid arteriopathy in young adults
Go AS. Elevated BP after AKI. J Am Soc Nephrol. 20. Schwartz GJ, Schneider MF, Maier PS, et al. with childhood-onset chronic renal failure. Circulation.
2016;27(3):914-923. Improved equations estimating GFR in children 2002;106(1):100-105.
9. Mackie AS, Ionescu-Ittu R, Therrien J, Pilote L, with chronic kidney disease using an 32. Bolger AP, Coats AJ, Gatzoulis MA. Congenital
Abrahamowicz M, Marelli AJ. Children and adults immunonephelometric determination of cystatin C. heart disease: the original heart failure syndrome.
with congenital heart disease lost to follow-up: who Kidney Int. 2012;82(4):445-453. Eur Heart J. 2003;24(10):970-976.
and when? Circulation. 2009;120(4):302-309. 21. International Society of Nephrology. Kidney 33. Rodriguez FH III, Marelli AJ. The epidemiology
10. Williams RG, Pearson GD, Barst RJ, et al; Disease Improving Global Outcomes: KDIGO 2012 of heart failure in adults with congenital heart
National Heart, Lung, and Blood Institute Working Clinical Practice Guideline for the Evaluation and disease. Heart Fail Clin. 2014;10(1):1-7.
Group on research in adult congenital heart disease. Management of Chronic Kidney Disease. Kidney Int 34. Oster ME, Lee KA, Honein MA,
Report of the National Heart, Lung, and Blood Supplements. http://www.kdigo.org/clinical_practice Riehle-Colarusso T, Shin M, Correa A. Temporal
Institute Working Group on research in adult _guidelines/pdf/CKD/KDIGO_2012_CKD_GL.pdf. trends in survival among infants with critical
congenital heart disease. J Am Coll Cardiol. 2006; Accessed August 9, 2016. congenital heart defects. Pediatrics. 2013;131(5):
47(4):701-707. 22. Xi B, Zhang T, Zhang M, et al. Trends in e1502-e1508.
11. Dimopoulos K, Diller GP, Koltsida E, et al. elevated blood pressure among US Children and 35. Coca SG, Singanamala S, Parikh CR. Chronic
Prevalence, predictors, and prognostic value of adolescents: 1999-2012. Am J Hypertens. 2016;29 kidney disease after acute kidney injury:
renal dysfunction in adults with congenital heart (2):217-225. a systematic review and meta-analysis. Kidney Int.
disease. Circulation. 2008;117(18):2320-2328. 23. Lo JC, Sinaiko A, Chandra M, et al. 2012;81(5):442-448.
12. Billett J, Cowie MR, Gatzoulis MA, Vonder Muhll Prehypertension and hypertension in 36. Lim CC, Tan CS, Chia CM, et al. Long-term risk
IF, Majeed A. Comorbidity, healthcare utilisation community-based pediatric practice. Pediatrics. of progressive chronic kidney disease in patients
and process of care measures in patients with 2013;131(2):e415-e424. with severe acute kidney injury requiring dialysis
congenital heart disease in the UK: cross-sectional, 24. Hansen ML, Gunn PW, Kaelber DC. after coronary artery bypass surgery. Cardiorenal
population-based study with case-control analysis. Underdiagnosis of hypertension in children and Med. 2015;5(3):157-163.
Heart. 2008;94(9):1194-1199. adolescents. JAMA. 2007;298(8):874-879. 37. Goldstein SL. Renal recovery at different ages.
13. Parikh CR, Thiessen-Philbrook H, Garg AX, et al; 25. Kit BK, Kuklina E, Carroll MD, Ostchega Y, Nephron Clin Pract. 2014;127(1-4):21-24.
TRIBE-AKI Consortium. Performance of kidney Freedman DS, Ogden CL. Prevalence of and trends 38. Brenner BM, Lawler EV, Mackenzie HS.
injury molecule-1 and liver fatty acid-binding protein in dyslipidemia and blood pressure among US The hyperfiltration theory: a paradigm shift in
and combined biomarkers of AKI after cardiac children and adolescents, 1999-2012. JAMA Pediatr. nephrology. Kidney Int. 1996;49(6):1774-1777.
surgery. Clin J Am Soc Nephrol. 2013;8(7):1079-1088. 2015;169(3):272-279.
39. Zappitelli M. Epidemiology and diagnosis of
14. Parikh CR, Coca SG, Thiessen-Philbrook H, et al; 26. Theodore RF, Broadbent J, Nagin D, et al. acute kidney injury. Semin Nephrol. 2008;28(5):
TRIBE-AKI Consortium. Postoperative biomarkers Childhood to early-midlife systolic blood pressure 436-446.
predict acute kidney injury and poor outcomes trajectories: early-life predictors, effect modifiers,
after adult cardiac surgery. J Am Soc Nephrol. 2011; and adult cardiovascular outcomes. Hypertension. 40. Cooper DS, Claes D, Goldstein SL, et al.
22(9):1748-1757. 2015;66(6):1108-1115. Follow-Up Renal Assessment of Injury Long-Term
After Acute Kidney Injury (FRAIL-AKI). Clin J Am Soc
15. National High Blood Pressure Education 27. Bocelli A, Favilli S, Pollini I, et al. Prevalence and Nephrol. 2016;11(1):21-29.
Program Working Group on High Blood Pressure in long-term predictors of left ventricular
Children and Adolescents. The fourth report on the hypertrophy, late hypertension, and hypertensive 41. Lo LJ, Go AS, Chertow GM, et al.
diagnosis, evaluation, and treatment of high blood response to exercise after successful aortic Dialysis-requiring acute renal failure increases the
pressure in children and adolescents. Pediatrics. coarctation repair. Pediatr Cardiol. 2013;34(3): risk of progressive chronic kidney disease. Kidney Int.
2004;114(2)(suppl 4th report):555-576. 620-629. 2009;76(8):893-899.
16. Jenkins KJ, Gauvreau K, Newburger JW, Spray 28. Clarkson PM, Nicholson MR, Barratt-Boyes BG, 42. James MT, Ghali WA, Tonelli M, et al. Acute
TL, Moller JH, Iezzoni LI. Consensus-based method Neutze JM, Whitlock RM. Results after repair of kidney injury following coronary angiography is
for risk adjustment for surgery for congenital heart coarctation of the aorta beyond infancy: a 10 to 28 associated with a long-term decline in kidney
disease. J Thorac Cardiovasc Surg. 2002;123(1): year follow-up with particular reference to late function. Kidney Int. 2010;78(8):803-809.
110-118. systemic hypertension. Am J Cardiol. 1983;51(9):
1481-1488.
1078 JAMA Pediatrics November 2016 Volume 170, Number 11 (Reprinted) jamapediatrics.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/peds/935842/ by a Sam Ratulangi University Hospital User on 04/03/2017
S-ar putea să vă placă și
- Advanced Practice Nursing Procedures 2º PDFDocument561 paginiAdvanced Practice Nursing Procedures 2º PDFKey Guilbert100% (6)
- Sciatica Relief GuideDocument15 paginiSciatica Relief GuideElliott Nunez100% (2)
- CataractDocument52 paginiCataracttammycristobalmd100% (4)
- Sush Unity Corrected EMERGENCY1700Document76 paginiSush Unity Corrected EMERGENCY1700Dr-Jahanzaib GondalÎncă nu există evaluări
- Fdar GammyDocument2 paginiFdar GammyAndrea Sibayan SorianoÎncă nu există evaluări
- Hemodialysis - Different AspectsDocument321 paginiHemodialysis - Different AspectsIndera VyasÎncă nu există evaluări
- Mission Indradhanush: Submitted By-Jayesh Agrawal Mba-Rural Development Semester-IstDocument20 paginiMission Indradhanush: Submitted By-Jayesh Agrawal Mba-Rural Development Semester-IstJayeshAgrawalÎncă nu există evaluări
- Internship Report Pharma CompanyDocument19 paginiInternship Report Pharma CompanyMuhammad Haider Ali100% (1)
- Unit Plan (3) Child Health NursingDocument5 paginiUnit Plan (3) Child Health Nursinggill priyaÎncă nu există evaluări
- International RseaechDocument9 paginiInternational RseaechVillooardÎncă nu există evaluări
- NIRS Renale Chir CardiaqueDocument17 paginiNIRS Renale Chir Cardiaquebouregaa.radia11Încă nu există evaluări
- Awaken StudyDocument9 paginiAwaken StudyManju KumariÎncă nu există evaluări
- Ayuno y SedaciónDocument8 paginiAyuno y SedaciónXerexÎncă nu există evaluări
- Ischemic Cerebrovascular Accident and Its Secondary Renal ImpairmentDocument5 paginiIschemic Cerebrovascular Accident and Its Secondary Renal ImpairmentAditya Angela AdamÎncă nu există evaluări
- Giovannetti (2019) - Cognition and Cerebral Infarction in Older Adults After Surgical Aortic Valve ReplacementDocument8 paginiGiovannetti (2019) - Cognition and Cerebral Infarction in Older Adults After Surgical Aortic Valve ReplacementVanessaÎncă nu există evaluări
- New England Journal Medicine: The ofDocument12 paginiNew England Journal Medicine: The ofBill BerilÎncă nu există evaluări
- Acute Kidney Injury and Risk of Death After.27 PDFDocument8 paginiAcute Kidney Injury and Risk of Death After.27 PDFtasya claudiaÎncă nu există evaluări
- 2018 NEJM Outcomes After Angiography With Sodium Bicarbonate and AcetylcysteineDocument12 pagini2018 NEJM Outcomes After Angiography With Sodium Bicarbonate and AcetylcysteineFlorin BranisteÎncă nu există evaluări
- Trial of Decompressive Craniectomy For Traumatic Intracranial HypertensionDocument12 paginiTrial of Decompressive Craniectomy For Traumatic Intracranial HypertensionV AÎncă nu există evaluări
- ECG in Low Risk PatientsDocument8 paginiECG in Low Risk PatientsSondang JasmineÎncă nu există evaluări
- 2004 JACC A Simple Risk Score For Prediction of Contrast Induced NephropathyDocument9 pagini2004 JACC A Simple Risk Score For Prediction of Contrast Induced NephropathyFlorin BranisteÎncă nu există evaluări
- Jamainternal Hsu 2020 Oi 200074 1606936160.50628Document8 paginiJamainternal Hsu 2020 Oi 200074 1606936160.50628Kezia AngelinaÎncă nu există evaluări
- Outcomes After Angiography With Sodium Bicarbonate and AcetylcysteineDocument12 paginiOutcomes After Angiography With Sodium Bicarbonate and AcetylcysteineIrmagian PaleonÎncă nu există evaluări
- Cardiac Interventions in Neonates WiDocument11 paginiCardiac Interventions in Neonates WiimÎncă nu există evaluări
- 10 1001@jama 2019 15686Document10 pagini10 1001@jama 2019 15686bruno mañonÎncă nu există evaluări
- WJN 4 148Document13 paginiWJN 4 148Rafela Agatha ChristyÎncă nu există evaluări
- Biomarcadores en AKIDocument14 paginiBiomarcadores en AKIhemer hadyn calderon alvitesÎncă nu există evaluări
- ACO Peripro 2016Document10 paginiACO Peripro 2016Philippe Bocanegra FernándezÎncă nu există evaluări
- Use of Intravenous Iodinated Contrast Media in PatDocument10 paginiUse of Intravenous Iodinated Contrast Media in PatOrlin ZlatarskiÎncă nu există evaluări
- Acknowledgments: Competency in Medical KnowledgeDocument1 paginăAcknowledgments: Competency in Medical KnowledgeTaniaÎncă nu există evaluări
- Lee, Et Al. 2018 - JACCDocument8 paginiLee, Et Al. 2018 - JACCCARLOS SANTIAGO PEREZ RODRIGUEZÎncă nu există evaluări
- Jurnal Clinical L OutcomeDocument14 paginiJurnal Clinical L OutcomeaesunnitheticÎncă nu există evaluări
- Guidelines For The Conduct of Clinical Trials ForDocument17 paginiGuidelines For The Conduct of Clinical Trials ForTùng KimÎncă nu există evaluări
- UOCTDocument8 paginiUOCTUlquiorra SchifferÎncă nu există evaluări
- Determinants Influencing Length of Icu Stay in Renal Transplant Recipients Undergoing General AnaesthesiaDocument8 paginiDeterminants Influencing Length of Icu Stay in Renal Transplant Recipients Undergoing General AnaesthesiaIJAR JOURNALÎncă nu există evaluări
- Jiang2018 2Document5 paginiJiang2018 2Anonymous Inj7eQÎncă nu există evaluări
- Cerebral Oximetry Monitoring To Maintain Normal Cerebral ExplainDocument11 paginiCerebral Oximetry Monitoring To Maintain Normal Cerebral ExplainDaniel EllerÎncă nu există evaluări
- Randomized Trial of Stents Versus Bypass Surgery For Left Main Coronary Artery DiseaseDocument9 paginiRandomized Trial of Stents Versus Bypass Surgery For Left Main Coronary Artery DiseaseTommy WidjayaÎncă nu există evaluări
- Adding Insult To Injury Journal CritiqueDocument1 paginăAdding Insult To Injury Journal Critiqueapi-357707616Încă nu există evaluări
- Study of Clinical Profile of Patient With Acute Kidney DiseaseDocument7 paginiStudy of Clinical Profile of Patient With Acute Kidney DiseaseIJAR JOURNALÎncă nu există evaluări
- Document Journal Review 4.09Document11 paginiDocument Journal Review 4.09Anonymous diwFs3MsWRÎncă nu există evaluări
- 1 s2.0 S1051227616301789 MainDocument7 pagini1 s2.0 S1051227616301789 MainResearch OfficeÎncă nu există evaluări
- Patient Safety During Sedation by Anesthesia ProfeDocument8 paginiPatient Safety During Sedation by Anesthesia ProfeIsmar MorenoÎncă nu există evaluări
- Diagnosis and Treatment of Acute Kidney Injury in PediatricsDocument13 paginiDiagnosis and Treatment of Acute Kidney Injury in PediatricsagungÎncă nu există evaluări
- Serum Electrolyte Levels and Outcomes in Patients Hospitalized With Hepatic EncephalopathyDocument7 paginiSerum Electrolyte Levels and Outcomes in Patients Hospitalized With Hepatic EncephalopathyhimayatullahÎncă nu există evaluări
- 10 1148@radiol 2019192094Document9 pagini10 1148@radiol 2019192094msaenz.medÎncă nu există evaluări
- Acute Kidney Injury After Cardiac Surgery Chew2018Document54 paginiAcute Kidney Injury After Cardiac Surgery Chew2018Oğuz KayıkçıÎncă nu există evaluări
- Sincope y TEP JAMA 2018Document7 paginiSincope y TEP JAMA 2018coniestivillÎncă nu există evaluări
- Fragasso2018 AKI TRRDocument14 paginiFragasso2018 AKI TRRLeydi johana Rodriguez alzateÎncă nu există evaluări
- Intravenous Fluid Therapy in The Adult Surgic 2016 International Journal ofDocument1 paginăIntravenous Fluid Therapy in The Adult Surgic 2016 International Journal ofoomculunÎncă nu există evaluări
- Outcome of Pediatric Cardiac Surgery and Predictors of Major Complication in A Developing CountryDocument7 paginiOutcome of Pediatric Cardiac Surgery and Predictors of Major Complication in A Developing CountryNensy AnggrainyÎncă nu există evaluări
- Article: Joel Neugarten, Sandipani Sandilya, Beenu Singh, and Ladan GolestanehDocument10 paginiArticle: Joel Neugarten, Sandipani Sandilya, Beenu Singh, and Ladan GolestanehThe Curious BenzÎncă nu există evaluări
- CRRT After Cardiac SurgeryDocument16 paginiCRRT After Cardiac SurgeryZainab MotiwalaÎncă nu există evaluări
- SPLIT Trial Young2015Document10 paginiSPLIT Trial Young2015Jessica HernandezÎncă nu există evaluări
- What's New in Spine Surgery: Specialty UpdateDocument11 paginiWhat's New in Spine Surgery: Specialty UpdatePoliceÎncă nu există evaluări
- 2021 Article 2564Document10 pagini2021 Article 2564Cinthya Añazco RomeroÎncă nu există evaluări
- FentonDocument6 paginiFentonjessicaesmrldaÎncă nu există evaluări
- 16 PDFDocument8 pagini16 PDFAkhileshÎncă nu există evaluări
- Accuracy of Non-Ultrasound Guided Thyroid Gland Fine Needle Aspiration With BiopsyDocument4 paginiAccuracy of Non-Ultrasound Guided Thyroid Gland Fine Needle Aspiration With BiopsyPeertechz Publications Inc.Încă nu există evaluări
- Indocyanine Green Fluorescence Angiography and The.17Document7 paginiIndocyanine Green Fluorescence Angiography and The.17Icaro DanielÎncă nu există evaluări
- (19330693 - Journal of Neurosurgery) Predictors of Primary Autograft Cranioplasty Survival and Resorption After CraniectomyDocument8 pagini(19330693 - Journal of Neurosurgery) Predictors of Primary Autograft Cranioplasty Survival and Resorption After CraniectomyfransiskalilieÎncă nu există evaluări
- Integrative Review 1Document17 paginiIntegrative Review 1api-442558242Încă nu există evaluări
- PeritDialInt 2012 Mishra 431 6Document7 paginiPeritDialInt 2012 Mishra 431 6Muhammad Halil GibranÎncă nu există evaluări
- Jurnal CardioDocument10 paginiJurnal CardiohengkileonardÎncă nu există evaluări
- PIIS1053077023003403Document12 paginiPIIS1053077023003403lxluizÎncă nu există evaluări
- Flat-Head Positioning Increases Cerebral Blood Flow in Anterior Circulation Acute Ischemic Stroke. A Cluster Randomized Phase Iib TrialDocument12 paginiFlat-Head Positioning Increases Cerebral Blood Flow in Anterior Circulation Acute Ischemic Stroke. A Cluster Randomized Phase Iib TrialSelvi PurnamasariÎncă nu există evaluări
- Art TaaDocument7 paginiArt TaaCristinaÎncă nu există evaluări
- Exercise in Dialysis - ZocalliDocument3 paginiExercise in Dialysis - ZocalliRaluca DumeaÎncă nu există evaluări
- Kidney Transplant Management: A Guide to Evaluation and ComorbiditiesDe la EverandKidney Transplant Management: A Guide to Evaluation and ComorbiditiesÎncă nu există evaluări
- Evaluation and Treatment of Neonatal Hyperbilirubinemia: IssuesDocument13 paginiEvaluation and Treatment of Neonatal Hyperbilirubinemia: IssuesNofiyanty NicolasÎncă nu există evaluări
- NIH Public Access: Author ManuscriptDocument10 paginiNIH Public Access: Author ManuscriptNofiyanty NicolasÎncă nu există evaluări
- Effects of Different Probiotic Strains of Lactobacillus and Acute Liver Injury ModelDocument8 paginiEffects of Different Probiotic Strains of Lactobacillus and Acute Liver Injury ModelNofiyanty NicolasÎncă nu există evaluări
- Seminars in Fetal & Neonatal Medicine: Tonse N.K. RajuDocument6 paginiSeminars in Fetal & Neonatal Medicine: Tonse N.K. RajuNofiyanty NicolasÎncă nu există evaluări
- 5.J Clin Pathol 2012 Salinas 928 33Document7 pagini5.J Clin Pathol 2012 Salinas 928 33Nofiyanty NicolasÎncă nu există evaluări
- 1n2 OrganicSD-drshakyaDocument26 pagini1n2 OrganicSD-drshakyaUMESH KANDELÎncă nu există evaluări
- Eblr Formal Paper KropkoDocument10 paginiEblr Formal Paper Kropkoapi-586815209Încă nu există evaluări
- 1.3 Describe Factors That May Impact Upon The Development of The Baby During: Pre-ConceptionDocument2 pagini1.3 Describe Factors That May Impact Upon The Development of The Baby During: Pre-Conceptionjoel TorresÎncă nu există evaluări
- Glucocorticoids in Systemic Lupus Erythematosus. Ten Questions and Some IssuesDocument13 paginiGlucocorticoids in Systemic Lupus Erythematosus. Ten Questions and Some IssuesSundas EjazÎncă nu există evaluări
- Benning Vanessa - Resume-2Document1 paginăBenning Vanessa - Resume-2api-489132887Încă nu există evaluări
- Dental EssayDocument3 paginiDental Essayvaleriana calaniÎncă nu există evaluări
- Thoracic Radiofrequency AblationDocument2 paginiThoracic Radiofrequency AblationIevgen DanylchukÎncă nu există evaluări
- Surgery Songbook CompressedDocument69 paginiSurgery Songbook CompressedBrandon HayashiÎncă nu există evaluări
- Vaccine Card - 20231120 - 175739 - 0000Document2 paginiVaccine Card - 20231120 - 175739 - 0000MarilynÎncă nu există evaluări
- Globus: A Feeling of A Lump in The ThroatDocument3 paginiGlobus: A Feeling of A Lump in The ThroatAlia MohamadÎncă nu există evaluări
- Rules and Guidelines For Mortality and Morbidity CodingDocument5 paginiRules and Guidelines For Mortality and Morbidity Codingzulfikar100% (2)
- Institute of Nursing: Far Eastern UniversityDocument3 paginiInstitute of Nursing: Far Eastern UniversityaleccespirituÎncă nu există evaluări
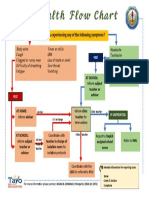
- Health Flow ChartDocument1 paginăHealth Flow ChartAlex Cainoy JrÎncă nu există evaluări
- Plan Your DrillDocument4 paginiPlan Your DrillStan BTOB,BTS,TXTÎncă nu există evaluări
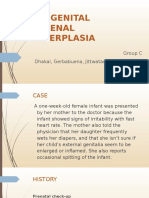
- Congenital Adrenal HyperplasiaDocument30 paginiCongenital Adrenal HyperplasiaIrene Jordan100% (1)
- Cycle BeadsDocument2 paginiCycle Beadsgihan200100% (2)
- A Case Study On MalariaDocument10 paginiA Case Study On MalariaAnant KumarÎncă nu există evaluări
- Leaflet - ProsoganDocument7 paginiLeaflet - ProsoganurmymelodyÎncă nu există evaluări
- Case 1 - Pneumonia (Final)Document4 paginiCase 1 - Pneumonia (Final)Joegie ArioÎncă nu există evaluări
- Nursing Seminar 1 SAS Session 2Document9 paginiNursing Seminar 1 SAS Session 2ZiaÎncă nu există evaluări
- Drug StudyDocument4 paginiDrug StudyDanica de LunaÎncă nu există evaluări