Documente Academic
Documente Profesional
Documente Cultură
2009 - Intermittent Short Course Therapy For Pediatric Tuberculosis PDF
Încărcat de
Tammy Utami DewiTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
2009 - Intermittent Short Course Therapy For Pediatric Tuberculosis PDF
Încărcat de
Tammy Utami DewiDrepturi de autor:
Formate disponibile
SHORT COMMUNICATION
Intermittent Short Course Therapy for Pediatric Tuberculosis
CK INDUMATHI, K KUMAR PRASANNA, CHITRA DINAKAR, ANITA SHET AND S LEWIN
From the Department of Pediatrics, St John’s Medical College Hospital, Bangalore, India.
Correspondence to: We conducted this study to assess the efficacy of intermittent short course therapy
in all forms of pediatric tuberculosis using a coordinated approach with Revised
Dr Indumathi CK,
National Tuberculosis Control Programme (RNTCP). Sixty-five children were
Assistant Professor, Department of treated using RNTCP protocols with some modifications, such as dose
Pediatrics, St John’s Medical adjustments or prolongation of treatment in selected children. Overall response
College Hospital, Sarjapur Road, rate was 95% (pulmonary 94% and extra pulmonary 97%). There was one case
Bangalore 560 034, India. with possible relapse. With dynamic inputs from both the treating pediatrician and
ckindumathi@gmail. com personnel from Directly Observed Treatment – Short-course (DOTS) centers, we
Received: February 5, 2009; could successfully implement RNTCP protocols in childhood tuberculosis.
Initial review: March 12, 2009; Key words: Childhood tuberculosis, Intermittent therapy, RNTCP.
Accepted: July 27, 2009.
Published online: 2009 October 14. PII: S097475590900078-2
R
evised National Tuberculosis Control pulmonary and serious extra pulmonary tuberculosis
Programme (RNTCP) recommends in children using a coordinated approach with DOTS
intermittent short course chemotherapy centers.
(ISSC) under Directly Observed Treat-
METHODS
ment-Short course (DOTS) strategy and the Indian
Academy of Pediatrics endorses the same for all This prospective study conducted between January
forms of childhood tuberculosis(1). Though there 2005 and July 2008 enrolled children diagnosed at
are reports of efficacy of ISSC in children with the pediatric department, St. John’s Medical College
pulmonary tuberculosis (PTB) and other non-serious Hospital with tuberculosis of all forms, except those
forms(2-7), there are limited published data on its co-infected with HIV. They were diagnosed,
efficacy in serious extra pulmonary tuberculosis classified and treated using RNTCP protocol(1). All
(EPTB)(8-10). Regarding the efficacy of ISSC in children with PTB, intracranial tuberculoma,
tubercular meningitis (TBM), the published abdominal, disseminated and lymph node
evidence is almost non-existent in children, and tuberculosis were started on ISCC (thrice weekly) at
scarce in adults(11). This lack of published evidence the outset. Children with TBM received daily
limits the utilization of RNTCP in childhood treatment for first 2 weeks followed by ISCC. All
tuberculosis(1). Concerns regarding inadequate children were referred to DOTS centers for drugs
dosages with available pediatric patient-wise boxes and also followed up at the study center by a
in some weight bands(12), and lack of trained pediatrician once in 2 weeks in intensive phase, once
personnel at DOTS centers to determine treatment a month in continuation phase and once in 2 months
endpoints in children, especially in sputum negative after completion of treatment. The pediatrician also
PTB and EPTB, contribute to low referral of communicated regularly with the DOTS centers
pediatric tuberculosis patients to DOTS centers(1). ensuring dosage appropriateness. Doses were
This study evaluated the efficacy of ISCC in both calculated according to bodyweight at baseline and
INDIAN PEDIATRICS 93 VOLUME 47__JANUARY 17, 2010
INDUMATHI, et al. INTERMITTENT SHORT COURSE THERAPY FOR TUBERCULOSIS
adjusted for gain in weight. Dosages were as follows. 97% in extra-pulmonary TB). There were 2 failures
INH 10-15 mg/kg rifampicin 10 mg/kg pyrazinamide among PTB. Additionally, two children required
30-35 mg/kg ethambutol 30 mg/kg and streptomycin extension of treatment to 9 months. All six children
15 mg/kg. Loose drugs available at DOTS centers with sputum positive for AFB became negative at the
were used initially followed by pediatric patient- end of intensive phase. Radiological response was
wise boxes once they became available. ‘Top-up’ noted in 90% of children.
doses were prescribed when available pediatric
combinations were found to be under dosed. Of the 14 cases with neurotuberculosis, seven
Adherence to top up doses was ensured by using a had meningitis (2 in stage 3 and 5 in stage 2), six had
family member as the DOTS provider. Treatment tuberculoma, and one had spinal arachnoiditis.
was extended to 9 months in PTB if there were slow Twelve (86 %) children had complete cure without
clinical and radiological responses (<2/3rd clearance sequelae, one (7%) had clinical cure with motor
at 6 months) not amounting to treatment failure. This deficit and one (7%) had clinical failure due to poor
individualized treatment was again achieved by adherence. There was no mortality. All cases of
coordination between pediatrician and DOTS disseminated, abdominal and lymph node TB
officers. Ethical clearance for the study was obtained responded with a 100% cure rate (Table I).
by the Departmental ethical committee and parental Of 65 children initiated on ISCC, 1 with PTB
consent was obtained. died; 1 with failed therapy for meningitis was lost to
RESULTS follow up; and, 4 were lost to follow up after
successful completion and response to ISCC. The
A total of 65 children with tuberculosis (34 remaining 59 children were followed up post
pulmonary and 31 extra-pulmonary) were analyzed. treatment for a mean period of 9.4 months (SD 8.5
Mean age was 7.6 years (range 5 months to 17 years) mo), of which 40% were followed for 1 year or more.
with a male to female ratio of 0.8:1. Acid fast bacilli One child with meningitis had suspected relapse
(AFB) positivity was documented in 9 (12%) cases after 6 months. Clinical hepatitis was not
(sputum - 6, lymph node - 1, breast tissue-1, lung encountered in any child. Sixty children were found
tissue-1). 68% of cases were treated as RNTCP to be adherent to treatment, having received more
category 1, 6.7% as category 2, and 25.3% as than 95% of doses.
category 3.
Eight children were given ‘top-up’ doses; 2
Treatment outcome is tabulated in Table I. The children in 6-10 Kg weight band, and 3 each in 11-16
overall cure rate was 95% (94% in pulmonary and Kg and 17-25 Kg weight bands. Two children with
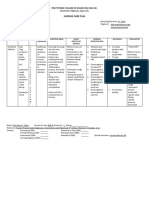
TABLE I TREATMENT OUTCOME IN CHILDHOOD TUBERCULOSIS
Type of tuberculosis Number Cured Failure Mean (range) duration Relapse
of follow up (mo)
Pulmonary 34 32 2 10.2 (0-37) 0
Extra pulmonary 31 30 1 8.5 (0-27) 1
Neurological 14 13 1 11.9 (0.27) 1
Lymphadenitis 7 7 0 7.7 (0-24) 0
Abdominal 4 4 0 3.7 (0-12) 0
Disseminated 3 3 0 8 (6-12) 0
Pericardial 1 1 0 1 0
Breast 1 1 0 6 0
Pleural effusion 1 1 0 22 0
INDIAN PEDIATRICS 94 VOLUME 47__JANUARY 17, 2010
INDUMATHI, et al. INTERMITTENT SHORT COURSE THERAPY FOR TUBERCULOSIS
WHAT THIS STUDY ADDS
• Intermittent short course chemotherapy is effective in childhood tuberculosis including serious forms of extra-
pulmonary tuberculosis.
PTB and one with EPTB required prolongation of Contributors: ICK: concept, planning and conduct of the
treatment to 9 months. study. ICK, PKK: drafting and data collection. CD, AS and
SL: critical revision of the manuscript.
DISCUSSION Funding: None.
This study revealed an overall response of 95%, Competing interests: None stated.
which is comparable to 90-100% response reported REFERENCES
with daily therapy(2,4,5). The 94% cure rate of PTB
1. Chauhan LS, Arora VK. Management of pediatric
is again comparable to response reported with daily
tuberculosis under the Revised National
therapy(2,4). Extension of treatment beyond 6 Tuberculosis Control Program (RNTCP) – The
months was required in 3 (4.6%) children compared consensus statement. Indian Pediatr 2004; 41: 901-
with 15% in another report(13). Residual 905.
radiological lesions were found in 13% of patients
2. Kumar L, Dhand R, Singhi PD, Rao LN, Katariya
on par with another study(4). Cure rates of 86% in
S. A randomized trial of fully intermittent vs daily
neurotuberculosis is encouraging, though this could followed by intermittent short course chemotherapy
not be compared with other studies with daily for childhood tuberculosis. Pediatr Infect Dis J
therapy(14,15), in view of very small numbers. 1990; 19: 802-806.
Further studies with a larger number of patients with
3. Hong Kong Chest Service, British Medical
neurotuberculosis are needed to validate these
Research Council. Controlled trial of four thrice-
conclusions. No child developed hepatitis compared weekly regimens and daily regimen all given for six
to 2.2-5% reported with daily therapy(3,13). More months for pulmonary tuberculosis. Lancet 1981;
than 95% adherence achieved has an important 8213: 171-174.
implication in preventing MDRTB. The main
4. Varudkar BL. Short-course chemotherapy for
limitation of our study was the absence of a control
tuberculosis in children. Indian J Pediatr 1985; 52:
group. 593-597.
Though RNTCP guidelines for diagnosis and 5. Te Water Naude JM, Donald PR, Hussey GD,
categorization could be implemented in the existing Kibel MA, Louw A, Perkins DR, et al. Twice
form, we had to modify the dosage schedules in few weekly vs daily chemotherapy for childhood
children. Under-dosage was a problem in children at tuberculosis. Pediatr Infect Dis 2000; 19: 405-410.
the upper end of weight bands across the ranges of 6- 6. Göçmen A, Ozçelic U, Kiper N, Toppare M, Kaya
10 Kg, 11-16 Kg and 17-25 Kg. We feel that this is an S, Cengizlier R, et al. Short course intermittent
important limitation in RNTCP that needs to be chemotherapy in childhood tuberculosis. Infection
addressed. We recommend to include a revision of 1993; 21: 324-327.
the weight bands to narrower ranges and provision 7. Jawahar MS, Rajaram K, Sivasubramanian S,
for increasing dosage with weight gain during Paramasivan CN, Chandracekar K, Kamaludeen
therapy, in addition to having trained personnel at MN, et al. Treatment of lymph node tuberculosis- a
DOTS centers to determine treatment endpoints for randomized clinical trial of two 6-month regimens.
children. Trop Med Int Health 2005; 10: 1090-1098.
8. Arora VK, Gupta R. Directly observed treatment
ACKNOWLEDGMENTS
for tuberculosis. Indian J Pediatr 2003; 70: 885-
We sincerely thank personnel of DOTS centers for 889.
the cooperation. 9. Anadol D, Kiper N, Gocmen A, Ozcelik U.
INDIAN PEDIATRICS 95 VOLUME 47__JANUARY 17, 2010
INDUMATHI, et al. INTERMITTENT SHORT COURSE THERAPY FOR TUBERCULOSIS
Intermittent chemotherapy for miliary tuberculosis 13. Kabra SK, Lodha R, Seth V. Category based
in children. Turk J Pediatr 1999; 41: 53-59. treatment of tuberculosis in children. Indian Pediatr
2004; 41: 927-937.
10. Rajeswari R, Sivasubramanian S, Balambal R,
Parthasarathy R, Ranjar R, Santha T, et al. A 14. Jacobs RF, Sunacorn P, Chotpttayasunonah
controlled clinical trial of short-course TC, Pope S, Kelleher K. Intensive short
chemotherapy for tuberculoma of the brain. Tuber course chemotherapy for tuberculous
Lung Dis 1995; 76: 311-317. meningitis. Pediatr Infect Dis J 1992; 11:
11. Venugopal K. Therapeutic efficacy of fully 194-198.
intermittent regimen for neuro TB-A field study in
15. Van Loenhout-Rooyackers JH, Keyser A, Laheij
South India. Pulmon 2006; 8; 89-92.
JF, Varbeek ALM, Van der meer JWM.
12. Lodha R, Menon PR, Kabra SK. Concerns on the Tuberculous meningitis: is a 6-month treatment
dosing of antitubercular drugs for children in regimen sufficient? Int J Tuberc Lung Dis 2001; 5:
RNTCP. Indian Pediatr 2008; 45: 852-854. 1028-1035.
INDIAN PEDIATRICS 96 VOLUME 47__JANUARY 17, 2010
S-ar putea să vă placă și
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Dilated CardiomyopathyDocument23 paginiDilated CardiomyopathyYanna Habib-MangotaraÎncă nu există evaluări
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- ECG Study GuideDocument7 paginiECG Study GuideannaÎncă nu există evaluări
- DefibrillationDocument9 paginiDefibrillationJara Maris Moreno BudionganÎncă nu există evaluări
- Mark Klimek Review DelegationDocument6 paginiMark Klimek Review DelegationKarima Jones100% (1)
- c22 Microbiology Tortora TestbankDocument16 paginic22 Microbiology Tortora Testbankwhitewave25Încă nu există evaluări
- The History of TuberculosisDocument9 paginiThe History of Tuberculosispimpaliukas1100% (1)
- Homeopathy Cases by KadwaDocument179 paginiHomeopathy Cases by Kadwaabckadwa100% (3)
- Endocrine NCLEX PN Pract & ANS Questions IIDocument13 paginiEndocrine NCLEX PN Pract & ANS Questions IIYA HOÎncă nu există evaluări
- MCQ-Chronic Obstructive Pulmonary DiseaseDocument3 paginiMCQ-Chronic Obstructive Pulmonary DiseaseMittulÎncă nu există evaluări
- Benign Breast DiseasesDocument35 paginiBenign Breast DiseasesBhim Nath KharelÎncă nu există evaluări
- 2016 - Health Profile of Paediatric Tuberculosis Patients On Directly Observed Treatment Short Course TherapyDocument4 pagini2016 - Health Profile of Paediatric Tuberculosis Patients On Directly Observed Treatment Short Course TherapyTammy Utami DewiÎncă nu există evaluări
- TB Treatment in ChildrenDocument11 paginiTB Treatment in ChildrenRathinasamy KrishnanÎncă nu există evaluări
- 2004 - Category Based Treatment of Tuberculosis in ChildrenDocument4 pagini2004 - Category Based Treatment of Tuberculosis in ChildrenTammy Utami DewiÎncă nu există evaluări
- Elevated Transaminases Are Common in Children On Prophylactic Treatment For TuberculosisDocument6 paginiElevated Transaminases Are Common in Children On Prophylactic Treatment For TuberculosisTammy Utami DewiÎncă nu există evaluări
- 2000 - WHO DOTS and Multidrug Resistant Tuberculosis Are Any Modifications RequiredDocument23 pagini2000 - WHO DOTS and Multidrug Resistant Tuberculosis Are Any Modifications RequiredTammy Utami DewiÎncă nu există evaluări
- TB Treatment in ChildrenDocument11 paginiTB Treatment in ChildrenRathinasamy KrishnanÎncă nu există evaluări
- DOTS and Multidrug-Resistant Tuberculosis: Are Any Medication Required?Document14 paginiDOTS and Multidrug-Resistant Tuberculosis: Are Any Medication Required?Tammy Utami DewiÎncă nu există evaluări
- DOTS and Multidrug-Resistant Tuberculosis: Are Any Medication Required?Document14 paginiDOTS and Multidrug-Resistant Tuberculosis: Are Any Medication Required?Tammy Utami DewiÎncă nu există evaluări
- DOTS and Multidrug-Resistant Tuberculosis: Are Any Medication Required?Document14 paginiDOTS and Multidrug-Resistant Tuberculosis: Are Any Medication Required?Tammy Utami DewiÎncă nu există evaluări
- End TB Brochure PDFDocument20 paginiEnd TB Brochure PDFTammy Utami DewiÎncă nu există evaluări
- DOTSDocument3 paginiDOTSTammy Utami DewiÎncă nu există evaluări
- 2001 - Diagnosis of Pediatric Tuberculosis Using The Indonesian National Concencus For Pediatric TuberculosisDocument5 pagini2001 - Diagnosis of Pediatric Tuberculosis Using The Indonesian National Concencus For Pediatric TuberculosisTammy Utami DewiÎncă nu există evaluări
- 2003 TB IndiaDocument67 pagini2003 TB IndiaTammy Utami DewiÎncă nu există evaluări
- 2014 WHO Child TB Training Toolkit WebDocument58 pagini2014 WHO Child TB Training Toolkit WebTammy Utami DewiÎncă nu există evaluări
- Elevated Transaminases Are Common in Children On Prophylactic Treatment For TuberculosisDocument6 paginiElevated Transaminases Are Common in Children On Prophylactic Treatment For TuberculosisTammy Utami DewiÎncă nu există evaluări
- 2009 - Intermittent Short Course Therapy For Pediatric Tuberculosis PDFDocument4 pagini2009 - Intermittent Short Course Therapy For Pediatric Tuberculosis PDFTammy Utami DewiÎncă nu există evaluări
- Diagnosis of Pediatric Tuberculosis Using The IndonesianDocument6 paginiDiagnosis of Pediatric Tuberculosis Using The IndonesianBella SalsabilaÎncă nu există evaluări
- 2009 - Intermittent Short Course Therapy For Pediatric TuberculosisDocument5 pagini2009 - Intermittent Short Course Therapy For Pediatric TuberculosisTammy Utami DewiÎncă nu există evaluări
- Child TB Training Toolkit WebDocument47 paginiChild TB Training Toolkit WebAsena TuiketeiÎncă nu există evaluări
- WHO HTM TB 2016.06 EngDocument16 paginiWHO HTM TB 2016.06 EngTammy Utami DewiÎncă nu există evaluări
- 2014 - Tuberculosis in Childhood A Systematic Review of National and International GuidelinesDocument10 pagini2014 - Tuberculosis in Childhood A Systematic Review of National and International GuidelinesTammy Utami DewiÎncă nu există evaluări
- 2009 - Intermittent Short Course Therapy For Pediatric Tuberculosis PDFDocument4 pagini2009 - Intermittent Short Course Therapy For Pediatric Tuberculosis PDFTammy Utami DewiÎncă nu există evaluări
- 2010 - Consensus Statement On Childhood TuberculosisDocument15 pagini2010 - Consensus Statement On Childhood TuberculosisTammy Utami DewiÎncă nu există evaluări
- GorjussAmi - EnGDocument10 paginiGorjussAmi - EnGTammy Utami DewiÎncă nu există evaluări
- End TB Brochure PDFDocument20 paginiEnd TB Brochure PDFTammy Utami DewiÎncă nu există evaluări
- 2013 - To Xray or Not To Xray Screening Asymptomatic Children For Pulmonary TB A Retrospective AuditDocument5 pagini2013 - To Xray or Not To Xray Screening Asymptomatic Children For Pulmonary TB A Retrospective AuditTammy Utami DewiÎncă nu există evaluări
- Blood PressureDocument60 paginiBlood PressureEnerolisa ParedesÎncă nu există evaluări
- Prevalence of High Blood Pressure and Association With Obesity in Spanish Schoolchildren Aged 4-6 Years OldDocument11 paginiPrevalence of High Blood Pressure and Association With Obesity in Spanish Schoolchildren Aged 4-6 Years OldMateus CarvalhoÎncă nu există evaluări
- Garssen, 2004 - Physical Training and Fatigue, Fitness, and Quality of Life in Guillain-Barre Syndrome and CIDPDocument3 paginiGarssen, 2004 - Physical Training and Fatigue, Fitness, and Quality of Life in Guillain-Barre Syndrome and CIDPkarinaÎncă nu există evaluări
- SN Erra Fazira Jururawat Terlatih U29 Jabatan Kecemasan, HAT Wilayah Kota KinabaluDocument14 paginiSN Erra Fazira Jururawat Terlatih U29 Jabatan Kecemasan, HAT Wilayah Kota Kinabaluyein yenÎncă nu există evaluări
- Tetanus: Guerrero, Djameica Danielle RDocument16 paginiTetanus: Guerrero, Djameica Danielle RDjameica GuerreroÎncă nu există evaluări
- ASCITES (Water Belly)Document5 paginiASCITES (Water Belly)Santosh BhandariÎncă nu există evaluări
- ConjunctivitisDocument9 paginiConjunctivitisSaranya DeviÎncă nu există evaluări
- NCP PryllDocument6 paginiNCP PryllpjcolitaÎncă nu există evaluări
- Horrific US Medical Experiments Come To LightDocument2 paginiHorrific US Medical Experiments Come To Lighthalojumper63Încă nu există evaluări
- Topical Oxygen Wound TherapyDocument9 paginiTopical Oxygen Wound TherapyTony LeeÎncă nu există evaluări
- 0199975744Document305 pagini0199975744nicoletaelenaÎncă nu există evaluări
- Evaluation of Macrocytic AnemiasDocument8 paginiEvaluation of Macrocytic Anemiasmy accountÎncă nu există evaluări
- C-Reactive Protein in Serum by NephelometryDocument12 paginiC-Reactive Protein in Serum by NephelometryTrajceÎncă nu există evaluări
- Drug Study FINALDocument32 paginiDrug Study FINALhomeworkping1Încă nu există evaluări
- Adhd InfographicDocument1 paginăAdhd Infographicapi-666361680Încă nu există evaluări
- ParalysisDocument4 paginiParalysissakuraleeshaoranÎncă nu există evaluări
- Journal Reading RPL EditDocument30 paginiJournal Reading RPL EditAnonymous l6Q1ROq2Încă nu există evaluări
- Implanted Venous Access Device (IVAD) - "Dome" or "Port"Document12 paginiImplanted Venous Access Device (IVAD) - "Dome" or "Port"JunkÎncă nu există evaluări
- Dr. Khairiyadi, M.Kes., Sp.A Departemen Ilmu Kesehatan Anak RSUD Ulin BanjarmasinDocument78 paginiDr. Khairiyadi, M.Kes., Sp.A Departemen Ilmu Kesehatan Anak RSUD Ulin BanjarmasinEldhaÎncă nu există evaluări
- ICD 9 Diagnosis CodesDocument41 paginiICD 9 Diagnosis CodesEvy Liesniawati0% (1)
- JH CERILLES STATE COLLEGE - Post TestDocument7 paginiJH CERILLES STATE COLLEGE - Post TestCrystal Ann TadiamonÎncă nu există evaluări
- Agust 2020Document29 paginiAgust 2020Danny YanuarÎncă nu există evaluări
- PONR - Comprehensive Nursing Health History and Physical ExaminationDocument21 paginiPONR - Comprehensive Nursing Health History and Physical ExaminationDRJC100% (1)