Documente Academic
Documente Profesional
Documente Cultură
65 - 43 Pregnancy Related Hypertension
Încărcat de
JackyHarianto0 evaluări0% au considerat acest document util (0 voturi)
4 vizualizări40 paginidasda
Titlu original
65_43 Pregnancy Related Hypertension
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentdasda
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
4 vizualizări40 pagini65 - 43 Pregnancy Related Hypertension
Încărcat de
JackyHariantodasda
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF sau citiți online pe Scribd
Sunteți pe pagina 1din 40
Chapter 43
PREGNANCY-RELATED HYPERTENSION
James M. Roberts, MD
© CLASSIFICATION AND DEFINITIONS
The hypertensive disorders of pregnancy challenge the
medical and obstetric skills of the health care team. Decisions
ws 0 the possible use and appropriate choice of pharmaco-
logic agents require not only an understanding of the patho-
physiology of the hypertensive disorders and a recognition of
the pharmacokinetic changes occurring during pregnancy but
also an appreciation of the possible fetal effects of such ther-
apeutic agents. Obstetric management demands meticulous
maternal observation and use of tests of fetal-placental fune-
tion and fetal maturity in order to weigh maternal risks and
the risks to the infant of intrauterine versus extra
existence.
‘The management of elevated blood pressure (BP) and the
impact of the disorder on the mother and fetus depend on
whether hypertension antedated the pregnancy or appeared as
the marker of pregaancy-specific vasospastic syndrome. An.
attempt to distinguish between the two has led to several
systems of nomenclature and classification. The hypertensive
disorders of pregnancy were for many years
mregnancy, a verm that originally included even hyperemesis
gravidarum and acute yellow atrophy of the liver. This term
reflected the opinion that these disorders had, as a common
etiology, circulating toxins, Failure to identify these toxins did
riot lead to a revision of this terminology, a circumstance
which is indicative of the continuing confusion that has
plagued the taxonomy of these disorders, This archaic rermi-
nology, which neither describes the disorders nor clarifies t
etiology, has rightly been abandoned.
(One of the difficulties in interpreting studies of the hyper-
tensive disorders of pregnancy is the inconsistency of termi-
nology (Rippman, 1969). Several systems of nomenclature are
in use around the world. The system prepared by the National
Institutes of Health (NIH) working group on hypertension in
pregnancy (Gifford et al., 2000a) although as imperfect as all
such systems, has the advantage of clarity and is available in
published form to investigators throughout the world. This
classification is as follows
led toxemias of
& Chronic hypertension
m Preeclampsia-eclampsia
Preeclampsia superimposed upon chronic hypertension
1 Gestational hypertension
The various classifications are explained in the following
discussion,
Chronic Hypertension
Chronic hypertension is defined as hypertension that is
present and observable prior to pregnancy or that is diagnosed
before the 20th week of gestation. Hypertension is defined as a
blood pressure greater than 140/90 mm Hg. Hypertension for
which a diagnosis is confirmed for the first time during preg
nancy, and which persists beyond the 84th day postpartum, is
also classified as chronic hypertension,
Preeclampsia and Eclampsia
The diagnosis of preeclampsia is determined by increased
blood pressure accompanied by proteinuria... Diagnostic blood
pressure increases are either a systolic blood pressure of greater
than of equal to 140 mm Hy or a diastolic blood pressure of
seater than or equal to 90 mm Hg, Diastolic blood pressure is
determined as Krotkoff V (disappearance of sounds), Ie is ec
ommended that gestational blood pressure elevation be
defined on the basis of at least two determinations. The repeat
blood pressure should be performed in a manner that will
reduce the likelihood of artifact and/or patient anxiety
(Gifford et al., 2000b), Absent from the diagnostic criteria ts
the former inclusion of an increment of 30 man Hg systolic or
15 mm Hg diastolic blood pressure, even when absolute values
are below 140/90 mm Hg. This definition was excluded
because the only available evidence shows that women in this
group are not likely to suffer increased adverse outcomes
(North et al,, 1999; Zhang et al., 2001). Nonetheless, women
who have a rise of 30 mm He systolic or 15 mm Hg diastolic
blood pressure warrant close observation, especially if pro-
teinuria and hyperuricemia (uric acid [UA] greater than or
equal t0 6 mg/dL) are also present (Gifford et al., 2000).
Proteinuria is defined as the urinary excretion of 03
protein or greater in a 24-hour specimen. This will usually
correlate with 30 myjdL ("I+ dipstick”) or greater in a random:
urine determination. Because of the discrepancy between
random protein determinations and 24-hour urine protein in
preeclampsia (which can be either higher or lower) (Abuelo,
1992; Kua et al, 1992; Meyer et al., 1994), itis recommended
that the diagnosis be hased on a 24-hour urine specimen if
at all possible of, if this is not feasible, it should be based
fon a timed collection corrected for creatinine excretion
Gifford et al., 2000b).
Preeclampsia occurs as a spectrum but is arbitrarily divided
into mild and severe forms. This terminology is useful for
clescriprive purposes but does not indicate specific diseases, not
859
860 43/Pregnancy-Related Hypertension
should it indicate arbitrary cutoff points for therapy. The diag:
nosis of severe preeclampsia is confirmed when the following
ctiteria are present:
Systolic blood pressure of 160 mm Hg or greater, or diastolic
pressure of 110 mm Hg or greater
2, Proteinuria of 2 g or more in 24 hours (2- or 3-plus on qual-
itative examination)
3. Increased serum creatinine (greater than 1.2 mgldL. unless
known to be previously elevated)
Persistent headache or cerebral or visual disturbances
. Persistent epigastric pair
Platelet count ess then 100,000/mm: and/or evidence of
microangiopathic hemolytic anemia (with increased lactic
acid dehydeogenase)
oat
Eclampsia is the occurrence of seizures in a proeclampric
patient that cannot be attributed to other causes,
Edlema occurs in too many normal pregnant women to be
discriminant and has been abandoned as a marker in
preeclampsia by the National High Blood Pressure Education,
Program (NHBPEP) and by other classification schemes
(Brown et al, 2001; Helewa et al., 1997; Practice, 2002).
Preeclampsia Superimposed
on Chronic Hypertension
There is ample evidence that preeclampsia can occur in
women who ate already hypertensive and that the prognosis
for mother and fetus is much worse for these women than with,
either condition alone. Distinguishing superimposed
preeclampsia from worsening chronic hypertension tests the
skills of the clinician. For clinical management, the principles
of high sensitivity and unavoidable overdiagnosis are appropri-
ate. The suspicion of superimposed preeclampsia mandates
close observation, with delivery indicared by the overall assess-
‘ment of maternal-fetal well being rather than by any fixed end-
point. The diagnosis of superimposed preeclampsia is highly
likely with the following findings:
1. In women with hypertension and no proteinuria early in
Pregnancy (prior to 20 weeks’ gestation) and new-onset
proteinuria, defined as the urinary excretion of 0.3 g protein
‘or more in a 24-hour specimen
2. In women with hypertension and proteinuria prior to
20 weeks’ gestation:
a. A sudden increase in proteinuria—urinary excretion of
0.3 g protein or more in a 24-hour specimen, or ewo
dlipstick-test results of 2+ (100 mg/dL), with the values
recorded at least 4 hours apart, with no evidence of
urinary tract infection
b. A sudden increase in blood pressure in a woman whose
blood pressure has previously heen well controlled
«. Thrombocytopenia (platelet count lower
100,000/mm:)
An inctease in ALT or AST to abnormal levels (Gifford
cet al., 2000b)
than
Gestational Hypertension
The woman who has blood pressure elevation detected for
the first time during pregnancy, without proteinuria, is
classified as having gestational hypertension. This nonspecific
term includes women with preeclampsia syndrome who have
not yet manifested proteinuria as well as women who do not
have the syndrome. The hypertension may be accompanied by
other signs of the syndrome, which will influence manage-
ment. The final differentiation chat the woman does not have
preeclampsia syndrome is made only postpartum. If preeclamp-
sia has not developed and blood pressure has returned to
normal by 12 weeks postpartum, the diagnosis of mansient
hypertension of pregnancy can be assigned. If blood pressure ele
vation persists, the woman is diagnosed as having chronic
hypertension. Note that the diagnosis of gestational hypetten-
sion is used during pregnancy only until a more specific din
‘nosis can be assigned postpartum (Gifford et al, 2000b).
Problems with Classification
The degree of blood pressure elevation that constitutes ges-
tational hypertension is controversial. Because average blood
pressure in women in their teens to 208 is 120/60 mim Hy, the
stanclatd definition of hypertension—blood pressure greater
than 140/90 mm Hg—is judged by some investigators to be too
high (Vartran, 1966). This has resulted in the suggestion in the
NHBPEP report that women with increased BP greater than
30 mm Hg systolic or 25 mm He diastolic be observed closely
even if absolute blood pressure has not exceeded 140/90.
There are also problems inherent in the use of blood pres-
sures measured in early pregnancy to diagnose chronte hyper
tension. Blood pressure usually decreases early in pregnat
reaching its nadir at about the stage of pregnancy at which
women usually present for obstetric care (Fig. 43-1). The
decrease averages 7 mm Hyg for diastolic and systolic readings.
In some women, obviously, blood pressure decreases more tha
7 mm Het in others, the early decline and subsequent return of
blood pressure to prepregnant levels in late gestation are
sufficient for a diagnosis of preeclampsia. Women who have
hypertension prior to pregnancy actually experience a greater
decrease in blood pressure in early pregnancy than do nor-
motensive women (Chesley and Annitto, 1947) and thus are
sm Hg
125
Systoe
PARAG
nsf.
10
75|
Diastolic
16 20 24 28 3296 a0
Gestational age (weeks)
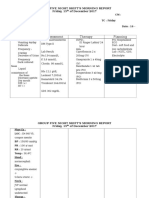
FIGURE 43-1 Mean blood pressure by gastational age in
{8000 Caucasian women 25-24 years of age who delivered singleton
term infants. (From Christianson &, Page EW. Stucies on blood
pressure during pregnancy: Influence at party and age. Am J Obstet
Gynecol 126:509, 1876. Courtesy of the American College of
Obstetricians and Gynecologists)
Mig TABLE 42-1. RENAL BIOPSY FINDINGS IN PATIENTS.
43/Pregnancy-Related Hypertension 61
WITH CLINICAL DIAGNOSIS OF PREECLAMPSIA
Biopsy Findings
Primigravidas (N= 62)
‘Multigravidas (N = 152)
Glomeruloendotheliosis 70%
Normal histologic appearance 5
Chronic renal disease (chronic GTN, chranic pyelonephritis) 255
Asteriolar nephrosclerosis °
GN, gostatenal wophebiastie neoplasia,
1% 4436 (with or without nephrosclerosis)
3% 533%
5% 21%
12%
Mociod rom McCartney CP; Pathological anatomy of acuta hypertension of oregrancy. Coulton 30Supph7, 1064, by permission ofthe Aenican Heart
Associaton Ine
even more likely to be misdiagnosed as preeclamptic according,
co blood pressure criteria.
‘Also, the diagnosis of chronic hypertension based on the
failure of blood pressure to return to normal by 84 days post-
partum can be in error. In a long-range prospective study by
Chesley (1956), many women who remained hypertensive
6 weeks postpartum were normotensive at long-term follow-
up. Even the proteinuria and hypertension are nonspecific
signs, and their presence in pregnancy could be due to condi-
tions other than preeclampsia
Renal biopsy specimens from women with a diagnosis of
preeclampsia (blood pressure increase and proteinuria) demon:
strate these diagnostic difficulties (Table 43-1) (McCartney,
1964). Of 62 women with a diagnosis of preeclampsia in their
fist pregnancies, 70% had a glomerular lesion believed to be
characteristic of the disorder; 24%, however, had evidence of
chronic renal disease that had not been suspected previously
Renal biopsy specimens of multiparous women with a clinical
diagnosis of superimposed preeclampsia also demonstrates the
difficulty in diagnosis. Of 152 subjects, only 3% had the char-
acteristic glomerular lesion, but 43% had evidence of preexist-
ing renal or vascular disease.
Preeclampsia has a clinical spectrum ranging from mild to
severe forms and then potentially to eclampsia. Affected
patients do not “catch” eclampsia or the severe forms of
preeclampsia bur rather progress through this spectrum, In
most cases, progression is slow, and the disorder may never
proceed beyond mild preeclampsia. In others, the disease can
progress more rapidly, changing from mild to severe over days
to weeks. In the most serious cases, progression can be fulmi-
nant, with mild preeclampsia evolving to severe preeclampsia
or eclampsia over hours to days
In a series of eclampric women analyzed by Chesley (1978),
25% had evidence of only mild preeclampsia in the days pre-
ceding convulsions. Thus, for purposes of clinical manage-
ment, we must accept the fact that we ate overdiagnosing the
condition because, as discussed lates, a major goal in managing
preeclampsia is the prevention of the serious complications of
preeclampsia and eclampsia, primarily through timing of deli
cry [vis also evident, however, that studies of preeclampsia w'
be confounded by inclusion of women who have been given a
diagnosis of preeclampsia but who actually have another car-”
diovascular or renal disorder.
HELLP
It is quite evident that the pathophysiological changes of
preeclampsia can_be present in the absence of hypertension
and proteinuria. This should not be surprising, as these diag-
nostic criteria are of historical rather than pathophysiological
relevance. Hypertension and proteinuria were the first signs
recognized as predicating preeclampsia (Chesley, 1978)
Understanding this historical evolution presents a challenge to
clinicians and dictates a high index of suspicion in managing
pregnant women with signs and symptoms that could be
explained by reduced organ perfusion. One clear setting in
which this occurs is the HELLP syndrome; the acronym stands
for Hemolysis, Elevated liver enzymes, and Low Platelets. This
seties of findings defines a reasonably consistent syndrome that
has now been studied for over twenty years (Weinstein, 1982),
Although for management purposes it is appropriate to con-
sider HELLP as a variant of preeclampsia, there are differences
in several features of preeclampsia and HELLP that suggest
they could be different entities. Women with HELLP tend to
be older and are more likely to be Caucasian and multiparous
than preeclamptic women; in many cases, they are not hyper
tensive (Egerman and Sibai, 1999). From a pathophysiological
perspective, changes in the renin-angiotensin system charac-
teristic of preeclampsia are not present in HELLP (Bussen
et al., 1998). Nonetheless, the progression of the disease and
its termination with delivery argue for an observation and
management strategy similar to that for preeclampsia. The
serendipitous observation that women who had received
“antepartum steroids appeared ro evidence improvement in the
HELLP syndrome (Magan et al., 1993) stimulated several ret~
rospective and observational studies (Magan and Marcin,
1995; Martin et al., 1997; O'Brien et al., 2000; O'Brien et al.,
2002; Tompkins and Thiagarajah, 1999; Yalcin et al. 1998).
These studies and a small randomized controlled trial (Magan
er al., 1994) suggest improvement in laboratory findings as well
as prolongation of pregnancy. The determination of appropri-
ate dosing and whether the benefit of therapy exceeds risks
await larger, randomized controlled trials.
@ PREECLAMPSIA AND ECLAMPSIA
In spite of che difficulty of making a clinical diagnosis of
preeclampsia, there is no question thac a disorder exists that is
unique to pregnancy, characterized by poor perfusion of many
vital organs (including the fetoplacental unit), and completely
reversible with the termination of pregnancy, Pathologic,
pathophysiologic, and prognostic findings clearly indicate
that this condition, preeclampsia, is not merely an unmasking
of preexisting, underlying hypertension. Although this fact
hhas been well documented for many years, problems still
arise owing to approaches in the management of preeclampsia
that are based solely on principles useful in- managing
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Morning Report 11 April 2019 (Autosaved)Document11 paginiMorning Report 11 April 2019 (Autosaved)JackyHariantoÎncă nu există evaluări
- Ni Hms 855012Document16 paginiNi Hms 855012JackyHariantoÎncă nu există evaluări
- Morning Report 10 April 2019Document22 paginiMorning Report 10 April 2019JackyHariantoÎncă nu există evaluări
- Morning Report: 3 April 2019 Kepaniteraan Ilmu Bedah Fakultas Kedokteran UKI Periode 25 Februari 2019-4 Mei 2019Document12 paginiMorning Report: 3 April 2019 Kepaniteraan Ilmu Bedah Fakultas Kedokteran UKI Periode 25 Februari 2019-4 Mei 2019JackyHariantoÎncă nu există evaluări
- Jadwal PosDocument1 paginăJadwal PosJackyHariantoÎncă nu există evaluări
- Jadwal PosDocument1 paginăJadwal PosJackyHariantoÎncă nu există evaluări
- Morning Report 2 April 2019 (Autosaved)Document15 paginiMorning Report 2 April 2019 (Autosaved)JackyHariantoÎncă nu există evaluări
- 59 - 42 Thromboembolic DiseaseDocument13 pagini59 - 42 Thromboembolic DiseaseJackyHariantoÎncă nu există evaluări
- SHOCK by DR Robert SP AnDocument22 paginiSHOCK by DR Robert SP AnOchabianconeriÎncă nu există evaluări
- Tugas Dr. HendrivanDocument1 paginăTugas Dr. HendrivanJackyHariantoÎncă nu există evaluări
- Ophthalmology Record: Dr. Gilbert W. Simanjuntak, SP.M (K)Document6 paginiOphthalmology Record: Dr. Gilbert W. Simanjuntak, SP.M (K)JackyHariantoÎncă nu există evaluări
- 63 - 45 Intensive Care Monitoring of The Critically Ill Pregnant PatientDocument27 pagini63 - 45 Intensive Care Monitoring of The Critically Ill Pregnant PatientJackyHariantoÎncă nu există evaluări
- 01 DermatotherapyDocument23 pagini01 DermatotherapyMomogi Foreverhappy100% (1)
- Early Warning SignDocument3 paginiEarly Warning SignJackyHariantoÎncă nu există evaluări
- Penjelasan BagusDocument10 paginiPenjelasan BagusJackyHariantoÎncă nu există evaluări
- Ibu Albine Tanggal 15 Desember Morning ReportDocument4 paginiIbu Albine Tanggal 15 Desember Morning ReportJackyHariantoÎncă nu există evaluări
- Ibu Syafrima Tanggal 20 Desember Morning ReportDocument4 paginiIbu Syafrima Tanggal 20 Desember Morning ReportJackyHariantoÎncă nu există evaluări
- TN Rahtomo Tanggal 14 Januari Morning Report (TIM JAGA 5)Document4 paginiTN Rahtomo Tanggal 14 Januari Morning Report (TIM JAGA 5)JackyHariantoÎncă nu există evaluări
- TN S Hutagaol 19 Januari Morning Report (TIM JAGA 5)Document4 paginiTN S Hutagaol 19 Januari Morning Report (TIM JAGA 5)JackyHariantoÎncă nu există evaluări
- Ibu Syafrima Tanggal 20 Desember Morning ReportDocument4 paginiIbu Syafrima Tanggal 20 Desember Morning ReportJackyHariantoÎncă nu există evaluări
- TN Abdul Wahid Tanggal 25 Desember Morning ReportDocument4 paginiTN Abdul Wahid Tanggal 25 Desember Morning ReportJackyHariantoÎncă nu există evaluări
- Ibu Sri Endang Tanggal 4 Januari Morning ReportDocument4 paginiIbu Sri Endang Tanggal 4 Januari Morning ReportJackyHariantoÎncă nu există evaluări
- TN Abdul Wahid Tanggal 25 Desember Morning ReportDocument4 paginiTN Abdul Wahid Tanggal 25 Desember Morning ReportJackyHariantoÎncă nu există evaluări
- Urinary Tract Infection (UTI)Document38 paginiUrinary Tract Infection (UTI)Trixie Anne GamotinÎncă nu există evaluări
- Engkau BesarDocument1 paginăEngkau BesarJackyHariantoÎncă nu există evaluări
- Get AttachmentDocument3 paginiGet AttachmentJackyHariantoÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)