Documente Academic
Documente Profesional
Documente Cultură
US-Guided Perisciatic Infiltration Relieves Piriformis Syndrome
Încărcat de
ardiTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
US-Guided Perisciatic Infiltration Relieves Piriformis Syndrome
Încărcat de
ardiDrepturi de autor:
Formate disponibile
Eur Radiol (2008) 18: 616–620
DOI 10.1007/s00330-007-0799-3 MUSCULO SKELETAL
Manuel Reus
Juan de Dios Berná
Piriformis syndrome: a simple technique
Victoria Vázquez
Ma Victoria Redondo
for US-guided infiltration of the perisciatic
José Alonso nerve. Preliminary results
Received: 24 June 2007
Abstract The piriformis syndrome is factorily in ten patients. Although the
Revised: 18 September 2007 an uncommon cause of sciatica, but- series in the study is limited, the
Accepted: 4 October 2007 tock or thigh pain. Because of the deep procedure for US-guided infiltration
Published online: 31 October 2007 location of the muscle and sciatic of the perisciatic nerve is a quick,
# European Society of Radiology 2007 nerve, infiltration has traditionally simple, economical and effective
been guided by electromyography, technique and can be considered an
fluoroscopy, computed tomography or alternative in the percutaneous treat-
M. Reus (*) . J. de Dios Berná . magnetic resonance imaging. The aim ment of the piriformis syndrome.
V. Vázquez . M. V. Redondo . J. Alonso of the present study is to describe a
Department of Radiology, University simple technique for ultrasound Keywords Sciatica . Piriformis
Hospital Virgen de la Arrixaca, (US)-guided perisciatic infiltration of syndrome . Ultrasound .
30120 El Palmar, Murcia, Spain corticosteroids and anaesthetic using Ultrasound-guided .
e-mail: mreus@um.es
Tel.: +34-968-369498 the inferior gluteal artery as a land- Myofascial syndrome . Pelvic pain
Fax: +34-968-369498 mark. This technique was used satis-
Introduction of muscle electromyography and CT in many hospitals.
Recently [8], ultrasound-guided infiltration of the piriformis
The piriformis syndrome (PS) is an uncommon cause of muscle has been described using bone references.
sciatica, buttock or thigh pain. The pain normally increases The purpose of our study is to describe a technique based
on muscle contraction, palpation or after prolonged sitting. on US-guide perisciatic infiltration of steroid and local
It is usually caused by alterations in the piriformis muscle anaesthetic. The inferior gluteal artery is used as a
such as hypertrophy, inflammation or anatomical varia- landmark to localise and identify the sciatic nerve, when
tions, which lead to trapping of the sciatic nerve [1–3]. PS it passes below the piriformis muscle.
is an infrequent and often wrongly diagnosed syndrome,
due to its rarity, lack of specific clinical symptoms, and
definitive diagnostic tests [2]. In cases in which medical Materials and methods
treatment [stretching exercises, massages, heat, ultrasound
(US), non-steroid anti-inflammatories and myorelaxant Patients
medication] for PS is not effective, the piriformis muscle is
injected with local anaesthesia and steroids or botulinum Between June 2005 and January 2007, ten patients (eight
toxin [1, 4, 5]. Some authors [6] also inject diluted local females and two males; age range: 19–60 years; mean age:
anaesthetic and steroids into the perisciatic region. The 45 years) diagnosed with unilateral PS (seven right and three
traditional procedure consists of blind injection into the left) were referred from the Traumatology and Rheumatology
area of maximum pain. Techniques such as electromyog- Departments to our Ultrasonography Unit for treatment with
raphy or computed tomography (CT) are currently used to US-guided percutaneous perisciatic injection of triamcinolone
identify the piriformis muscle, and a nerve stimulator to acetonide diluted with local anaesthetic.
identify the sciatic nerve [1, 5, 7]. A limitation for further The diagnosis of PS was established from the following:
development of these techniques is due to the unavailability clinical history, physical exploration, EMG findings and by
617
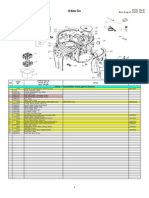
Technique
The procedure in all cases was carried out by an ultrasono-
grapher with expertise in infiltrations of the musculoskeletal
system (MR) using an EnVisor device (Royal Philips,
Eindhoven, Netherlands) equipped with a 7- to 12-MHz
multifrequency transducer. The inferior gluteal artery is used
as a landmark to identify the sciatic nerve, which is located just
beside it and lateral to the exit of the greater sciatic notch
(Fig. 1).
The perisciatic infiltration technique involves the fol-
lowing steps:
1. Location of the inferior gluteal artery.
With the patient in the prone position, the transducer is
placed over the pathological gluteal region at the level
of the supero-internal quadrant, the inferior gluteal
artery is located by transverse sections with colour
power Doppler, and the sciatic nerve is observed lateral
to the artery as an ovoid structure with hyperechogenic
points inside similar to a honeycomb (Fig. 2).
2. Location of the puncture site.
Longitudinal US sections are taken on the inferior
gluteal artery, and once situated on the longitudinal
axis of the inferior gluteal artery we move the
Fig. 1 Diagram of the posterior aspect of the pelvis showing the transducer laterally a little to clearly identify the sciatic
relationship between the piriformis muscle (arrowhead) and the nerve as a fibrillar hyperechogenic structure below the
inferior gluteal artery (arrow) and sciatic nerve (curved arrow).
Trajectory below the piriformis muscle of the inferior gluteal artery piriformis muscle (Fig. 3). Once the position of the
(dotted lines) and sciatic nerve (dashed lines) sciatic nerve is confirmed, the skin is marked with a
permanent marker pen (Fig. 4).
3. Perisciatic infiltration.
excluding other causes of sciatic pain. PS was suggested by Under conditions of rigorous asepsis, the transducer is
pain on palpation of the sciatic notch and reproduction of inserted into a sterile bag, and a sterile gel applied to
pain with manoeuvres that stretch or contract the piriformis the area of interest. We then perform percutaneous
muscle over the sciatic nerve (Frieberg, Beatty and Pace perisciatic injection of 1 ml of triamcinolone acetonide
manoeuvres) [9, 10]. (1 ml = 40 mg of triamcinolone acetonide, Bristol-
The patients were given detailed information on the Myers Squibb) diluted in 1 ml of 2% mepivacaine
procedure and informed written consent was obtained from using a 3.5-inch 22-gauge spinal needle (B/Braum)
all of them. The present study was approved by our under US guidance. The direction of the needle is
Hospital’s Ethics and Research Commission. controlled by longitudinal sections of the sciatic nerve.
Fig. 2 a Transverse colour
Doppler sonography in the
supero-internal quadrant of the
left buttock showing the inferior
gluteal artery (arrow) and vein
(curved arrow) and laterally the
sciatic nerve (arrowheads). b
Schematic illustration of a
showing the transducer place-
ment on the skin of the left
buttock
618
Results
All the patients in this study received US-guided perisciatic
infiltration satisfactorily. The average time of the procedure
was 8 min (range: 5–10 min). Three patients felt a slight
weakness in the lower limb after perisciatic injection, which
disappeared spontaneously a few hours later. No local or
general complications were observed after injection.
The symptoms in eight (80%) of the patients in this study
diminished progressively after the first week. The two
remaining cases (20%) required a further infiltration at
2 weeks because the pain had not remitted. The symptoms
disappeared in all the patients 2 months after perisciatic
infiltration.
Discussion
Fig. 3 Longitudinal sonography revealing the sciatic nerve as a The piriformis muscle originates from the anterior part of the
fibrillar hyperechogenic structure (arrows) sacrum, exits the pelvis through the greater sciatic foramen
and inserts distally on the upper border of the great tro-
chanter; it is innervated by branches from S1 and S2 [12, 13].
PS is a form of myofascial pain syndrome caused by
The free-hand technique [11] was used for injection. contracture of the piriformis muscle and characterised by
With this method, one hand holds the transducer whilst the pain in the buttocks, hip and posterior part of the thigh.
free hand pushes the needle towards the perisciatic region These symptoms are aggravated by prolonged hip flexion,
(Fig. 5), as perpendicular as possible to the US beam to adduction and internal rotation. PS and the lumbar facet
identify the route of the needle (Fig. 6). This technique syndrome can occasionally coincide [5]. About 5–8% of all
allows changes in needle direction during puncture. patients with low back pain and cases of sciatica may be
All the patients were followed up weekly for the first two caused by PS [1, 7, 12–14]. The diagnosis of PS is an
months by the specialists involved (traumatologists and exclusion diagnosis. All diagnostic techniques must rule out
rheumatologists). pathology of the spine, hip and sacroiliac joints [13, 14].
Fig. 4 Photograph of the pa-
tient’s right buttock with the
course of the sciatic nerve traced
on the skin to its exit through
the greater sciatic foramen. The
buttock is divided into four
quadrants (black lines)
619
Fig. 5 Photograph of the pa-
tient’s left buttock shows the
free-hand technique. One hand
holds the transducer while the
other one moves the 22-gauge
spinal needle until the perisciatic
region located below the
piriformis muscle. The crest of
ilium situation is drawn on the
skin as a curved black line
PS should be included in the differential diagnoses of
low-back pain and sciatica, specially when there is no
pathology in the lumbar spine or in the hip joints. This
syndrome is usually mistaken for a herniated disc. Spinal
stenosis, trochanteric bursitis, sacroiliac joint pathology,
pelvis tumor and endometriosis, should be considered in
the differential diagnoses. These conditions can often be
eliminated by means of a detailed medical history and a
thorough physical examination. [1, 13, 14]. CT and mag-
netic resonance imaging (MRI) can be useful in some
patients, in order to make a correct diagnosis [1, 2].
Traditional treatment for this myofascial syndrome
includes stretching exercises, massages, heat, US, non-
steroid anti-inflammatories and myorelaxant medication.
Conservative treatment is sufficient in many cases. Patients
who do not respond to a conservative therapy are
candidates for local infiltration of anaesthetics and steroids
[1]. Some authors suggest that the injection be given in
the muscular stomach, whilst others prefer injecting in
the medial aspect of the muscle or in the side [1, 14].
Botulinum toxin has also proved efficient for treating PS
and to have a longer-lasting effect [15]. In a randomised
study, Graboskiet al. [16] compared botulinum toxin injec-
tion with a local anaesthetic in the treatment of myofascial
pain syndrome and found no statistically significant dif-
ferences between either. The results of the study together
with the high cost of botulinum toxin advise against using
it as a first line of treatment.
Hypertrophy and inflammation of the piriformis muscle,
leading to sciatic nerve compression, irritation, and swell-
ing, are thought to be the causes of the radiating leg pain in
Fig. 6 Grey-scale longitudinal sonography revealing the echogenic piriformis syndrome. Perisciatic injection of steroid and
course of the needle (arrowheads), through the piriformis muscle local anaesthetic at the site of nerve compression was
with the tip located posterior and nearby to the sciatic nerve (arrow) shown to reduce nerve swelling, reduce ectopic discharge,
620
and facilitate the recovery of nerve conduction following colour power Doppler; we can also direct the needle
nerve injury. In our study, we have chosen the perisciatic towards the periphery of the sciatic nerve and control the
nerve infiltration based on other authors’ studies [6]. The advance of the needle at all times. Moreover, as there is no
perisciatic and the piriformis muscle infiltrations are two ionizing radiation exposure the procedure can be used in
techniques useful to treat the PS, although, at the moment, pregnant women. Smith et al. [8] also uses US to guide
there are no conclusive studies about the advantages of injection, but unlike us used bone structures as landmarks
both techniques. It would be necessary to make a pro- and the injection was given inside the piriformis muscle.
spective randomised study to compare these techniques. Surgery may be indicated in cases that resist medical
Hanania and Kitain [6] recommends using lower con- treatment or when there is an anatomical alteration in the
centrations of local anaesthetics to prevent motor block in piriformis muscle. Proposed surgical treatment consists of
the sciatic nerve. Motor block associated with injection of a reducing the volume of the muscle, dissecting it or excising
high concentration of local anaesthetic was minimal in our it [1, 18].
study. In conclusion, although our study is limited to a few
Various authors have used electromyography, fluoros- patients, we believe that the use of US to guide perisciatic
copy, CT or MRI [5, 17] as a guide for infiltration of the injection, and using the inferior gluteal artery as a
piriformis muscle. However, the US-guided perisciatic landmark, is a quick, simple, economical and effective
infiltration technique described in this study in quick, technique. We consider this procedure to be an interesting
simple, efficient and well tolerated by patients. The inferior option in the percutaneous treatment of PS.
gluteal artery used as a landmark is easily identifiable with
References
1. Benzon HT, Katz JA, Benzon HA, 7. Fanucci E, Masala S, Sodani G et al 14. Rodrigue T, Hardy R (2001) Diagnosis
Iqbal MS (2003) Piriforme síndrome. (2001) CT-guided injection of botulinic and treatment of piriformis syndrome.
Anatomic consderations, a new injec- toxin for percutaneous therapy of Nerosurg Clin N Am 12:311–319
tion technique, and a review of the piriformis muscle síndrome with pre- 15. Porta M (2000) A comparative trial of
literature. Anesthesiolgy 98:1442–1448 liminary MRI results about denervative botulinum toxin type A and methyl-
2. Lee EY, Margherita AJ, Gierada DS, process. Eur Radiol 11:2543–2548 prednisolone for the treatment of
Narra VR (2004) MRI of piriforme 8. Smith J, Hurdle MF, Locketz AJ, myofascial pain syndrome and pain
síndrome. Am J Roentgenol 183:63–64 Winiewski SJ (2006) Ultrasound- from chronic muscle spasm. Pain
3. Parziale JR, Hudgins TH, Fishman LM guided piriformis injection: technique 85:101–105
(1996) The piriformis síndrome. Am J description and verification. Arch Phys 16. Graboski CL, Gray DS, Burnham RS
Orthop 25:819–823 Med Rehabil 87:1664–1667 (2005) Botulinum toxin a vesus
4. Hong CZ, Hsueh TC (1996) Difference 9. Beatty RA (1994)The piriformis mus- bupivacaine trigger point injections for
in pain relief after trigger point injec- cle syndrome: a simple diagnostic ma- the treatment of myofascial pain
tions in myofascial pain patients with neuver. Neurosurgery 34:512–514 syndrome: a randomised double blind
and without fibromyalgia. Arch Phys 10. Durrani Z, Winnie AP (1991) crossover study. Pain 118:170–175
Med Rehabil 77:1161–1166 Piriformis muscle syndrome: an under- 17. Filler AG, Haynes J, Sheldon E et al
5. Fishman SM, Caneris OA, Bandman diagnosed cause of sciatica. J Pain (2005) Sciatica of nondisc origin and
TB, Audette JF, Borsook D (1998) Symptom Manage 6:374–379 piriformis syndrome: diagnosis by
Injetions of the piriformis muscle by 11. Otto R, Deyhle P (1980) Guided magnetic resonance neurography and
fluoroscopic and electromyographic puncture under real-time sonographic interventional magnetic resonance im-
guindance. Reg Anesth Pain Med control. Radiology 134:784–785 aging with outcome study of resulting
23:554–559 12. Lang AM (2004) Botulinum toxin typo treatment. J Neurosurg Spine 2:99–115
6. Hanania M, Kitain E (1998) Perisciatic B in piriformis syndrome. Am J Phys 18. Benson ER, Schutzer SF (1999) Port-
injection of steroid for the treatment of Med Rehabil 83:198–202 traumatic piriformis syndrome: diag-
sciatica due to piriformis syndrome. 13. Papadopoulos EC, Khan SN (2004) nosis and results of operative treatment.
Reg Anesth Pain Med 23:223–228 Piriformis syndrome and low back J Bone Joint Surg Am 81:941–949
pain: a new classification and review of
the literature. Orthop Clin N Am
35:65–71
S-ar putea să vă placă și
- General Anesthesia For C-SectionDocument4 paginiGeneral Anesthesia For C-SectionardiÎncă nu există evaluări
- An Algorithmic Approach To Low Back PainDocument8 paginiAn Algorithmic Approach To Low Back PainardiÎncă nu există evaluări
- Clinical Presentation of LastDocument7 paginiClinical Presentation of LastardiÎncă nu există evaluări
- Checklist For Local Anesthetic Toxicity Treatment 1-18-12Document2 paginiChecklist For Local Anesthetic Toxicity Treatment 1-18-12Akilesh RamasamyÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (72)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- 11 - Effective Pages: Beechcraft CorporationDocument80 pagini11 - Effective Pages: Beechcraft CorporationCarlos Andres Oviedo OsorioÎncă nu există evaluări
- Scheda Tecnica-Golf GTEDocument1 paginăScheda Tecnica-Golf GTEBlogo MotoriÎncă nu există evaluări
- English ESP Mapeh Filipino Aral. Pan. Math Mtb/Mle English ESP Mapeh Filipino Aral. Pan. Math Mtb/MleDocument2 paginiEnglish ESP Mapeh Filipino Aral. Pan. Math Mtb/Mle English ESP Mapeh Filipino Aral. Pan. Math Mtb/MleJackielou Biala-Guba Mosada RebualosÎncă nu există evaluări
- Adidas Suns CatalogDocument59 paginiAdidas Suns Catalogstumap8441Încă nu există evaluări
- Running With CeruttyDocument32 paginiRunning With Ceruttyviveksharma666100% (1)
- EVOBET88 Situs Judi Slot Online Gacor Dan Agen Judi Bola PDFDocument1 paginăEVOBET88 Situs Judi Slot Online Gacor Dan Agen Judi Bola PDFArrafi FahrezaÎncă nu există evaluări
- DC-3 - Recovery Software Guide - V06 04 00 5465 - ECD117-1Document20 paginiDC-3 - Recovery Software Guide - V06 04 00 5465 - ECD117-1ДмитрийÎncă nu există evaluări
- IELTS-Reading-Writing-7-8-Not Edititing VersionDocument134 paginiIELTS-Reading-Writing-7-8-Not Edititing VersionMd. Anwar HossainÎncă nu există evaluări
- Planeta ComicDocument31 paginiPlaneta ComicDavid ZxsÎncă nu există evaluări
- Today MagDocument35 paginiToday MagSofía BerrotaránÎncă nu există evaluări
- Saeco Odea GoDocument8 paginiSaeco Odea GotomitadanielÎncă nu există evaluări
- PriceList 201120Document1 paginăPriceList 201120KorRhinoÎncă nu există evaluări
- WWI 32nd Infantry DivisionDocument77 paginiWWI 32nd Infantry DivisionCAP History LibraryÎncă nu există evaluări
- Manteniment R290 R190 PDFDocument13 paginiManteniment R290 R190 PDFJoan Pladeveya SelvasÎncă nu există evaluări
- Oaklawn Park: Daily Racing FormDocument40 paginiOaklawn Park: Daily Racing FormReille VanderÎncă nu există evaluări
- La Espada Del Tiempo Rick RiordanDocument320 paginiLa Espada Del Tiempo Rick RiordanRafael VargasÎncă nu există evaluări
- Catalogo COMFORSIL SiliconasDocument51 paginiCatalogo COMFORSIL SiliconasTalquipen DbzapÎncă nu există evaluări
- Electrical Resistant Heavy Duty Safety Shoes With MidsoleDocument3 paginiElectrical Resistant Heavy Duty Safety Shoes With MidsoleEunice GayetaÎncă nu există evaluări
- Runner - World - UK - 2014 (GTRG) PDFDocument116 paginiRunner - World - UK - 2014 (GTRG) PDFhocusÎncă nu există evaluări
- FC Steaua BucureștiDocument27 paginiFC Steaua BucureștiRikky2403xÎncă nu există evaluări
- Exercies For Lower BackDocument2 paginiExercies For Lower BackAnkush RatanpalÎncă nu există evaluări
- 100 ESL Board Games PreviewDocument10 pagini100 ESL Board Games PreviewAmrah AmrahovÎncă nu există evaluări
- F 1 C 1Document2 paginiF 1 C 1Abel Gonzalez100% (7)
- AerobicsDocument8 paginiAerobicsIvan Dennis SalupanÎncă nu există evaluări
- Construction and Working:: Porter GovernorDocument5 paginiConstruction and Working:: Porter Governoraverify53Încă nu există evaluări
- Falls From LaddersDocument3 paginiFalls From Laddersao185029Încă nu există evaluări
- Wonderwall Chord Progression Song LyricsDocument2 paginiWonderwall Chord Progression Song LyricsJames WatsonÎncă nu există evaluări
- 2022 Hawaii Hall of HonorDocument1 pagină2022 Hawaii Hall of HonorHonolulu Star-AdvertiserÎncă nu există evaluări
- Short Story CinderellaDocument2 paginiShort Story CinderellaInbar Surya Seru0% (1)
- Season3 PKL DATA FOR DATA ANALYTICSDocument3 paginiSeason3 PKL DATA FOR DATA ANALYTICSBhagya SreeÎncă nu există evaluări