Documente Academic
Documente Profesional
Documente Cultură
THE Florida State University College OF Medicine: Complete History Checklist Clinical Skills Course MS1-3
Încărcat de
mj CanilangTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
THE Florida State University College OF Medicine: Complete History Checklist Clinical Skills Course MS1-3
Încărcat de
mj CanilangDrepturi de autor:
Formate disponibile
Complete History Checklist
THE FLORIDA STATE UNIVERSITY
COLLEGE OF MEDICINE
COMPLETE HISTORY CHECKLIST
Clinical Skills Course MS1-3
This behaviorally explicit checklist provides query examples for the novice to learn a comprehensive medical history
encompassing history of present illness, functional history, past medical history, social history and family history.
Color coding allows recognition of 4 geriatrics principles of care applied across the lifespan. Subsequently, learners
apply clinical reasoning to selectively use these history components for two common patient encounters: problem
oriented examinations (new, undiagnosed concerns) and chronic illness management.
DISCLAIMER FOR STUDENTS: please be aware that this document does not include all the questions that you must ask to receive full
credit for an OSCE exam. In addition, the questions provided are not the only way or best way to ask the information but rather are provided
to help clarify areas of confusion such as the difference between onset and setting/context or how to ask about sexual activity.
Remember to start with open-ended general questions then move to more focused information when indicated. For example: As an adult,
what medical conditions have you been told you have? Specifically, has anyone ever told you that you have high blood pressure? What about
diabetes? …
Avoid multi-part questions. Ex. Do you have diabetes, hypertension, or heart problems? This should be 3 separate questions.
Avoid leading questions. Ex. You don’t have diabetes do you?
Use summarization to help you gather your thoughts, identify missing data, and confirm accuracy of information. The standardized patients
(SPs) are anticipating moments of silence during which you will “check-off” your mental checklist and feel confident that you have completed
gathering the data.
Sample questions used to elicit information
General Medical Etiquette, Communication, Identifying Information
Hello my name is Lisa Jones; I’m a first year medical student. 1. Introduction (first and last name, full title with year of medical
training e.g. 1st year medical student)
I’m going to take a moment to wash my hands before I shake yours. 2. Demonstrate attention to clean technique throughout the
encounter, wash hands before patient contact, rewash as
needed
I’m working with your doctor today and as a student I will be sharing 3. Explain purpose of encounter, student role (take info to doctor,
all of your information with the doctor and s/he will work with you to doctor decides care plan with you) and identify all patient
plan your care. agenda items within first 1-2 minutes of interview
What brings you to the doctor’s today? Was there something else
you wanted to speak with the doctor about today? (keep asking
something else until answer is no)
I’m going to start your evaluation by discussing your history (and
performing ___exam)
SOFTEN (nonverbal: smile, open body language, forward lean, 4. Utilize non-verbal SOFTEN skills and PEARLS statements
touch, eye contact, nod); PEARLS statements (verbal: partnership,
empathy, apology, respect, legitimization, support)
5. Communicate clearly throughout encounter: avoid jargon or
explain medical terminology after use; questions and
explanations clear, concise and organized
6. Use both open-ended and close-ended questions during
interview
Let me summarize what I just heard, please correct me if anything is 7. Use summarization to facilitate verification, clarification, or
wrong or incomplete. elaboration of information. Invite patient to correct information.
What is your name? How old are you? 8. Obtain and record patient name, age (inquiry), gender
(Must use formal address, ex. Ms. Smith) (observation). Must address patient formally (ex. Ms. Smith)
9. Attend to patient comfort, dignity, and privacy throughout exam
10. Physically offer/assist patient in/out of exam room
11. When present, obtain name and relationship of accompanying
people
12. Throughout visit acknowledge/ validate presence of
accompanying people (e.g. occasional eye contact, nod,
verbal communication)
13. When appropriate offer/ arrange to interview patient in private
Colors represent Principles of Care integration themes:
Pink =communication skills Green =functional ability Blue =social setting Yellow =therapeutic review
Copyright 2011, Florida State University College of Medicine/ Lisa Granville, MD. This work was supported by a grant from the Donald W. Reynolds Foundation.
All rights reserved. For information about using this form, contact Lisa Granville, MD at lisa.granville@med.fsu.edu.
Complete History Checklist
THE FLORIDA STATE UNIVERSITY
COLLEGE OF MEDICINE
when accompanied by others
Chief Concern
Capture ‘verbatim’ patient response to “Why are you here today?” 14. Primary concern (chief concern)
History of Present Illness
Could you show me (or tell me specifically) where you are feeling 15. Bodily location
this (insert symptom, ex. leg pain)? Does it seem to go anywhere AND radiation
else?
How would you describe this (insert symptom)? 16. Quality
For non-pain: Tell me about how severe this symptom is. 17. Quantity/severity
For pain: On a scale of 0 – 10, with 0=no pain and 10=worst pain
you can imagine; how would you rate your pain?
Onset: When did this problem start? 18. Timing (onset, duration, frequency, progression over time)
Duration: How long does an episode last?
Frequency: How often do you get this in a day (or week)?
Progression: Since it started, has it been getting better or worse? In
what way is it changing?
What were you doing when this problem first started? 19. Setting/context at onset
What makes the problem worse? 20. Aggravating factors
(keep asking something else until answer is nothing else)
What makes the problem better? 21. Relieving factors
(keep asking something else until answer is nothing else)
Do you have any other symptoms? Please describe them. Do you 22. Associated symptoms / pertinent negatives
think these other symptoms may be related to your (insert chief
symptom)? Note: should query specific symptoms that may be
associated, ex. if stomach pain ask about nausea, diarrhea;
if a cough should ask if it is productive, description of sputum,
presence of fever
Have you ever had anything like this before? 23. Ever had similar symptoms
24. When appropriate, why this problem/concern is being presented
today/now
What do you think is causing this? 25. Ideas, hypotheses/theories about cause(s) of
(keep asking something else until answer is nothing else) symptoms/condition
What worries you about this? 26. Worries/fears about cause(s)/implications of
(keep asking something else until answer is nothing else) symptoms/condition
How is this (insert chief symptom) affecting you? 27. Impact of symptoms/condition on one or more of the following:
How does it interfere with your daily activities? Your relationships daily functioning, relationships, or self-concept
with others? Your thoughts about yourself?
Baseline Functional History: Make a transition statement: I have just gathered information about your (symptom); I’m now going to ask you
some different questions that relate to general information, outside of the (symptom).
IADLs: How is your ability to do things around the house and 28. Baseline functional ability: ADLs, IADLs
nearby? Do you have any difficulty driving? Cooking? Using your
medications?
ADLs: How is your ability for personal care, do you have any
difficulty bathing? Dressing? Grooming?
AADLs: How are you doing with your work, are you having any 29. When appropriate, elicit information about AADLs
problems there? Any problems with your recreation?
Past Medical History: Make a transition statement: Now I’m going to ask you about your medical conditions and health
In general, how would you rate your health? 30. General state of health
If necessary provide scale: If I were to give you the following options:
excellent, very good, good, fair, or poor how would you rate your
health?
As an adult, what medical conditions have you been told you have? 31. Significant medical diseases/ conditions as an adult
Has anyone ever told you that you have high blood pressure? What
about diabetes? What about…
Colors represent Principles of Care integration themes:
Pink =communication skills Green =functional ability Blue =social setting Yellow =therapeutic review
Copyright 2011, Florida State University College of Medicine/ Lisa Granville, MD. This work was supported by a grant from the Donald W. Reynolds Foundation.
All rights reserved. For information about using this form, contact Lisa Granville, MD at lisa.granville@med.fsu.edu.
Complete History Checklist
THE FLORIDA STATE UNIVERSITY
COLLEGE OF MEDICINE
What mental health conditions have you been told you have? (keep 32. Significant psychiatric diseases/conditions
asking something else until answer is no)
What medications do you use? What do you use that for? What is 33. Prescription medications including dosage, frequency,
the dose? How many times a day do you take it? Do you think it is indication, effectiveness, side-effects, adherence for each
working (or effective)? Please explain. Do you think you are having
any side effects? If yes, tell me about it. How often do you forget to
take your medicine? When you feel better, do you sometimes stop
taking your medicine?
(keep asking any other medications until answer is no)
What over the counter medications do you use? What do you use 34. Non-prescription drugs: over the counter medications, vitamins,
that for? What is the dose? How many times a day do you take it? supplements, home/folk remedies
Do you think it is working (or effective)? Please explain. Do you think
you are having any side effects? If yes, tell me about it.
AND
What vitamins/supplements or home remedies do you use? Why do
you use that? Do you know the dose? How many times a day do you
take it? Do you think it is working (or effective)? Please explain. Do
you think you are having any side effects? If yes, tell me about the
side effects.
(keep asking any other therapies until answer is no)
Besides medication, what do you use for your medical condition (or 35. Non-medication approaches including “dosage”, frequency,
to promote health)? Why do you use that? How much do you use? indication, effectiveness, side-effects for each
How often do you use it? Do you think it is working (or effective)? Do
you think you are having any side effects?
(keep asking something else until answer is no; note the “dosage”
question may need modification depending on the therapeutic
approach; examples of approaches include acupressure, meditation,
prayer)
Are you allergic to anything? What happens when you are exposed 36. Allergies AND reactions
to _____?
Have you ever been hospitalized? What was it for? When was that? 37. Hospitalizations
(keep asking something else until answer is no)
Have you ever had surgery? What was it for? When was that? (keep 38. Surgeries
asking something else until answer is no)
Have you ever had an accident or injury that needed medical care? 39. Accidents/injuries
What happened?
Have you ever had a blood transfusion? When was that? 40. Blood transfusions
What illnesses did you have as a child? Did you have the chicken 41. Significant childhood illnesses
pox? Measles?
How old were you when you started your periods? Do you have any 42. Menstrual history (age of onset, current problems, menopause)
problems currently? Are you still having your periods? Do you think AND pregnancy (number, outcomes)
you have started menopause?
How many times have you been pregnant? Tell me what happened
with each of those pregnancies.
Over the past 2 weeks have you often been bothered by feeling 43. Over the past 2 weeks have you often been bothered by (2
down, depressed, or hopeless? items): 1. feeling down, depressed, or hopeless; 2. loss of
Over the past 2 weeks have you often been bothered by little or no interest/pleasure in doing things
pleasure in doing things?
Do you regularly have your blood pressure checked? How often do 44. Elicit information (action, frequency, results) about at least 3
you do that? What were the results? preventive/screening practices
Do you regularly have your vision checked? How often? What were For women: pap smears and mammograms
the results? For 50+:colon cancer screening with fecal occult blood testing
Note a woman over age 50 would have at least 7 items queried: 3 and endoscopy
general practice; PAP smears and mammograms; fecal occult blood
test and endoscopy (Have you had your stool tested for blood? How
often do you get that done? What were the results?; Have you had a
colonoscopy or sigmoidoscopy where a lighted tube is placed up
Colors represent Principles of Care integration themes:
Pink =communication skills Green =functional ability Blue =social setting Yellow =therapeutic review
Copyright 2011, Florida State University College of Medicine/ Lisa Granville, MD. This work was supported by a grant from the Donald W. Reynolds Foundation.
All rights reserved. For information about using this form, contact Lisa Granville, MD at lisa.granville@med.fsu.edu.
Complete History Checklist
THE FLORIDA STATE UNIVERSITY
COLLEGE OF MEDICINE
your bottom and the doctor looks at the lining of the intestines? How
often? What were the results?
Have you had a tetanus shot in the last 10 years? When? 45. Current immunization status: tetanus, hepatitis B, influenza; For
Have you had the 3 shots for hepatitis B? When? diabetic / geriatric Pneumovax
Do you get the influenza vaccine once a year? When was the last
one?
Family History: Make a transition statement: Now I’m going to ask you about your family’s health
Has anyone in your family had (insert chief symptom, or query 46. Blood relatives having similar illness/ condition
problems with relevant system)?
Tell me about your parents. How old are they? How would you 47. Age (now or at time of death) and health status of immediate
describe their health? OR How old was s/he when s/he died? What family members
did s/he die from?
Tell me about any brothers or sisters you have. How old are each of
them? How would you describe each person’s health?
Continue with spouse and children
Do any medical conditions run in your family? 48. Diseases that run in family
Let me ask you about some specific conditions that are very
common; has anyone in your family been told they have high blood
pressure? What about heart disease? Etc.
Personal and Social History: Make a transition statement Now I’m going to ask you about your personal background
How far did you go in school? OR What is the highest level of school 49. Education level
you have completed? Preferred language
What languages do you speak? Which language do you prefer?
Are you married? 50. Marital status
Who do you live with? (ask anyone else until answer is no one else) Living situation (household members and environment)
What type of home do you have? (Offer single family home,
apartment, etc. if clarification needed)
What do you do for a living? What other jobs have you had? 51. Current and former occupations
Have you ever been in the military? What branch? How long? Associated hazards/risks
Do you feel any of your jobs have had hazards or risks to your Military service
health? Which jobs and what were the health hazards?
Do you have any financial concerns about your home? Food? Do 52. Adequate financial resources: food, shelter, medical care
you have any financial concerns about your health care?
Do you use any tobacco products? What type? How much? How 53. Tobacco use—current and past use— quantify
often? How long have you been using this?
If no current use: Have you ever used tobacco products? How much,
etc?
Alternative = begin with past info: Have you used tobacco products
in the past? Are you using tobacco products currently? What type?
How much? How often? How long have you been using this?
How much alcohol do you drink? What type? How much? How 54. Alcohol use—current and past use— quantify
often? How long have you been using this?
If No current use: Have you used alcohol in the past? How much, etc
Alternative = begin with past info
Do you use any other recreational drugs? What type? How much? 55. Recreational drug use—current and past use— quantify
How often? How long have you been using this?
If No current use: Have you used drugs in the past? How much, etc
Alternative = begin with past info
Have you been sexually active in the past? 56. Sexual activity—current and past—in the future, follow-up by
Are you currently sexually active? identifying gender of sexual partners, sexual activities/practices,
satisfaction with current
Tell me about your diet. 57. Dietary practices
Do you follow a special diet? If yes: What is it?
What do you do for leisure or to relax? 58. Leisure activities/hobbies
(keep asking something else until all items gathered)
What do you do for physical activity or exercise? 59. Physical activity/exercise
Colors represent Principles of Care integration themes:
Pink =communication skills Green =functional ability Blue =social setting Yellow =therapeutic review
Copyright 2011, Florida State University College of Medicine/ Lisa Granville, MD. This work was supported by a grant from the Donald W. Reynolds Foundation.
All rights reserved. For information about using this form, contact Lisa Granville, MD at lisa.granville@med.fsu.edu.
Complete History Checklist
THE FLORIDA STATE UNIVERSITY
COLLEGE OF MEDICINE
How often? For how long do you do that (quantify each activity)?
Do you feel safe in your relationships? Has anyone physically hurt 60. Safe in relationships; may use HITS domestic violence query–
you? Insulted you? Threatened you with bodily harm? Screamed at physically hurt, insulted, threatened with bodily harm,
you? screamed at
Do you have someone who can help you if you are physically ill or 61. Support system for illness and/or emotional upset
emotionally upset? Who would that be?
How does religion or spirituality influence your health care? 62. Influence of religious beliefs/spirituality
How often do you wear a seat belt? 63. Safety practices—including use of seat belts, smoke detectors,
How often do you use sun screen? sun screens/sun protection, presence of weapons in house,
Do you have any weapons in the house? What type? Do you keep weapon safety
these locked up or out of children’s reach?
Do you have a living will (a written statement about your healthcare 64. Advance care plan, presence of 2 items: living will AND health
wishes)? Have you designated someone to make healthcare care surrogate
decisions for you if you are unable to do so?
Oral Presentation: Ask patient to leave the room and then present findings
Subjective: Chief Concern
65. Report chief concern, verbatim sentence(s)
Objective: General Observations Presentation
Report observation compared to stated age 66. Report comparison of the patient’s estimated age (based on
observations) with stated age
State gender 67. Report apparent gender
Report at least 2 descriptors (ex. well developed, moderately obese) 68. Report body habitus: include physical appearance and body
build.
State consciousness level 69. Report level of consciousness (ex. alert, lethargic, stuporous, or
comatose)
Report at least 1 descriptor 70. Report demeanor (ex. pleasant, irritable, confused, or
combative)
Report at least 1 descriptor 71. Report apparent health status (ex. appears acutely ill, in pain,
or in acute distress (physical or emotional); if the patient has
been seen previously, does the patient appear as he/she
usually appears)
Report at least 1 descriptor 72. Report notable characteristics
Report at least 1 descriptor 73. Report grooming / clothing
Report at least 1 descriptor 74. Report eye contact
Report at least 1 descriptor 75. Report level of cooperation
Report at least 1 descriptor 76. Report abnormal movement or mannerisms (ex. lack of
expression, tremors, hand wringing)
Sample report:
Identifying Information
The patient, Mr. Albert, is a 40 year old man.
Subjective Information
The patient’s chief concern was “I have a pain in my knee that won’t go away.”
Objective Information
General Observations
Mr. Albert is a 40 year old man who appears younger than his stated age. He is well developed, obese; alert; pleasant; in no acute
distress; and when looking for notable characteristics, no tattoos, piercings or scars were noted. He is well groomed and his clothes are
appropriate for age, gender, season and occasion. He makes good eye contact without staring. He was cooperative throughout the
exam and exhibited no abnormal movements such as tremors or hand wringing. That concludes my presentation for this patient.
Colors represent Principles of Care integration themes:
Pink =communication skills Green =functional ability Blue =social setting Yellow =therapeutic review
Copyright 2011, Florida State University College of Medicine/ Lisa Granville, MD. This work was supported by a grant from the Donald W. Reynolds Foundation.
All rights reserved. For information about using this form, contact Lisa Granville, MD at lisa.granville@med.fsu.edu.
S-ar putea să vă placă și
- Older Adult Health Promotion ProjectDocument6 paginiOlder Adult Health Promotion Projectapi-404271262Încă nu există evaluări
- HealthDocument6 paginiHealthapi-422930884Încă nu există evaluări
- Ethics and The Covid-19 Pandemic Everyday Challenges Uams LGG No NarrationDocument42 paginiEthics and The Covid-19 Pandemic Everyday Challenges Uams LGG No Narrationapi-136237609Încă nu există evaluări
- Jonathan Onigama n360 Capstone Paper WorkDocument16 paginiJonathan Onigama n360 Capstone Paper Workapi-302664277Încă nu există evaluări
- Sbar Template RN To PDFDocument2 paginiSbar Template RN To PDFMichael StefanoÎncă nu există evaluări
- Ostomy CareDocument3 paginiOstomy CareKit ChanÎncă nu există evaluări
- Nur320-Plan of CareDocument4 paginiNur320-Plan of Careapi-559074394100% (1)
- Heart Disease Research Paper Final DraftDocument13 paginiHeart Disease Research Paper Final Draftapi-301442453Încă nu există evaluări
- My Nursing Philosophy - Mai Nomura FinalDocument9 paginiMy Nursing Philosophy - Mai Nomura Finalmai_nomura_2Încă nu există evaluări
- Nursing Diagnosis Using NANDADocument9 paginiNursing Diagnosis Using NANDAynottrip0% (1)
- Liver CirrhosisDocument14 paginiLiver CirrhosisCharissa Magistrado De LeonÎncă nu există evaluări
- O'Connor v. Donaldson, 422 U.S. 563 (1975)Document21 paginiO'Connor v. Donaldson, 422 U.S. 563 (1975)Scribd Government DocsÎncă nu există evaluări
- Form Ama PDFDocument1 paginăForm Ama PDFLOVI KRISSADIÎncă nu există evaluări
- NANDA DefinitionDocument3 paginiNANDA DefinitionDeology JuaninoÎncă nu există evaluări
- Process Recording Template 1Document5 paginiProcess Recording Template 1api-584340241Încă nu există evaluări
- Ma Cristy L. Exconde, MD, FPOGSDocument62 paginiMa Cristy L. Exconde, MD, FPOGSCAROL ANN PATITICO100% (1)
- New Patient Health History IMDocument3 paginiNew Patient Health History IMj kim100% (1)
- Dementia Symptoms and CareDocument32 paginiDementia Symptoms and CareKiran Mini Ravi100% (1)
- Admission Nursing AssessmentDocument20 paginiAdmission Nursing AssessmentKhaskheli NusratÎncă nu există evaluări
- Therapeutic Communication - Doc 12345Document8 paginiTherapeutic Communication - Doc 12345KBSÎncă nu există evaluări
- Teaching Plan For Patient With CopdDocument2 paginiTeaching Plan For Patient With Copdapi-3530442990% (1)
- Blood Pressure Chart - Norm..Document6 paginiBlood Pressure Chart - Norm..roshukkÎncă nu există evaluări
- Life and DeathDocument23 paginiLife and DeathJea Joel MendozaÎncă nu există evaluări
- AdvocacyassignmentintropagefinalDocument3 paginiAdvocacyassignmentintropagefinalapi-290938460Încă nu există evaluări
- Laryngeal MassDocument36 paginiLaryngeal MassJayson de GuzmanÎncă nu există evaluări
- ReferralDocument2 paginiReferralJowi Tsidkenu Pili CruzÎncă nu există evaluări
- NLN Vision Statement Achieving DiversityDocument16 paginiNLN Vision Statement Achieving DiversitySarmad SultanÎncă nu există evaluări
- Malaybalay City, Bukidnon: Bukidnon State University College of NursingDocument3 paginiMalaybalay City, Bukidnon: Bukidnon State University College of NursingJune Bars100% (1)
- Ncmb317 Lecture: BSN 3Rd Year 2Nd Semester Prelim 2023: Bachelor of Science in Nursing 3YBDocument62 paginiNcmb317 Lecture: BSN 3Rd Year 2Nd Semester Prelim 2023: Bachelor of Science in Nursing 3YB2 - GUEVARRA, KYLE JOSHUA M.Încă nu există evaluări
- Challenges in NursingDocument4 paginiChallenges in NursingAnju PandeyÎncă nu există evaluări
- Physical Examination Form: Medications AllergiesDocument4 paginiPhysical Examination Form: Medications AllergiesIris Ann PhillipsÎncă nu există evaluări
- Interaction Process Analysis IpaDocument6 paginiInteraction Process Analysis Ipaapi-392699632Încă nu există evaluări
- Nurs 3020 Final EvalDocument9 paginiNurs 3020 Final Evalapi-312968341Încă nu există evaluări
- Health Teaching Plan: EffectsDocument2 paginiHealth Teaching Plan: EffectsRheal P EsmailÎncă nu există evaluări
- Ethics Essay Professional MisconductDocument7 paginiEthics Essay Professional Misconductapi-283071924Încă nu există evaluări
- Fall Lecture 2018 PDFDocument51 paginiFall Lecture 2018 PDFBong SinonÎncă nu există evaluări
- Patient-Reported Physical Activity Questionnaires A Systematic Review of Content and FormatDocument18 paginiPatient-Reported Physical Activity Questionnaires A Systematic Review of Content and FormatHanif FakhruddinÎncă nu există evaluări
- Sample Letter of Medical NecessityDocument2 paginiSample Letter of Medical NecessityMin SoeÎncă nu există evaluări
- CH11. Substance-Related Disorders PDFDocument44 paginiCH11. Substance-Related Disorders PDFAngie morenoÎncă nu există evaluări
- Pdfill PDF Editor With Free Writer and Tools: Physical AssessmentDocument20 paginiPdfill PDF Editor With Free Writer and Tools: Physical Assessmentgheen215100% (1)
- Informed Consent and PracticeDocument10 paginiInformed Consent and PracticeAnonymous GpgioaDAbÎncă nu există evaluări
- Principle of JUSTICEDocument41 paginiPrinciple of JUSTICEEvelyn Lacson100% (1)
- Final Draft For CapstoneDocument15 paginiFinal Draft For Capstoneapi-282022477Încă nu există evaluări
- Windshield SurveyDocument11 paginiWindshield Surveyapi-240927368Încă nu există evaluări
- Community Health Paper IIDocument19 paginiCommunity Health Paper IIapi-444056287Încă nu există evaluări
- Week 4 ReflectionDocument1 paginăWeek 4 ReflectionSara NielsenÎncă nu există evaluări
- Nur 4142 Personal Philosophy of Nursing PaperDocument9 paginiNur 4142 Personal Philosophy of Nursing Paperapi-337559523Încă nu există evaluări
- Health PromotionDocument5 paginiHealth Promotionapi-433917537Încă nu există evaluări
- APOLONIO, JC - Duty Ethics - Emmanuel KantDocument2 paginiAPOLONIO, JC - Duty Ethics - Emmanuel KantJustin ApolonioÎncă nu există evaluări
- INTERVIEWDocument3 paginiINTERVIEWLuis DetriniadÎncă nu există evaluări
- Bathing On Adult or Pediatric ClientDocument25 paginiBathing On Adult or Pediatric Clientkto12Încă nu există evaluări
- NursingCare PlanDocument8 paginiNursingCare PlanSunSearra Kennedy RuffinÎncă nu există evaluări
- Final EvaluationDocument10 paginiFinal Evaluationapi-338285420Încă nu există evaluări
- Patient Care CompetencyDocument4 paginiPatient Care CompetencyEmer Joy T. ValeÎncă nu există evaluări
- Learning Plans EportfolioDocument2 paginiLearning Plans Eportfolioapi-345810410Încă nu există evaluări
- Name of StudentDocument20 paginiName of StudentHassan KhanÎncă nu există evaluări
- Roleplay Physical AssessmentDocument7 paginiRoleplay Physical AssessmentSinta Dewi Pap100% (1)
- Mental Health Testu3Document5 paginiMental Health Testu3clarheenaÎncă nu există evaluări
- ETOH Case StudyDocument5 paginiETOH Case StudyCharme Jean RaygonÎncă nu există evaluări
- Cancer-Related Symptoms & Supportive Care: Medical Cannabis: Unlocking the Potential for Top Conditions, #5De la EverandCancer-Related Symptoms & Supportive Care: Medical Cannabis: Unlocking the Potential for Top Conditions, #5Încă nu există evaluări
- Pharmacology MCQDocument1 paginăPharmacology MCQmj CanilangÎncă nu există evaluări
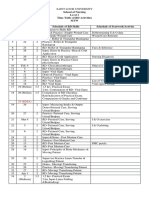
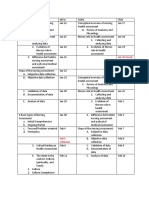
- Grading System For NCM 103 - 103A - Funda SL and RDDocument2 paginiGrading System For NCM 103 - 103A - Funda SL and RDmj CanilangÎncă nu există evaluări
- Prelim Exam PharmaDocument2 paginiPrelim Exam Pharmamj CanilangÎncă nu există evaluări
- WHO Core Nurse Educator CompetenciesDocument1 paginăWHO Core Nurse Educator Competenciesmj CanilangÎncă nu există evaluări
- Chapter 46 Chest AssessmentDocument12 paginiChapter 46 Chest Assessmentmj CanilangÎncă nu există evaluări
- Funda RLE RD Time TableDocument4 paginiFunda RLE RD Time Tablemj CanilangÎncă nu există evaluări
- Soliman SchedDocument1 paginăSoliman Schedmj CanilangÎncă nu există evaluări
- Wifi HackingDocument3 paginiWifi Hackingmj CanilangÎncă nu există evaluări
- Alignment Matrix For PLOs Health AssessmentDocument4 paginiAlignment Matrix For PLOs Health Assessmentmj CanilangÎncă nu există evaluări
- School of Nursing Level 1 Time Table of RD Activities MTW Day Dates Hrs. Schedule of RD Skills Schedule of Seatwork/ActivityDocument4 paginiSchool of Nursing Level 1 Time Table of RD Activities MTW Day Dates Hrs. Schedule of RD Skills Schedule of Seatwork/Activitymj CanilangÎncă nu există evaluări
- Time Monday Tuesday Wednesday Thursday Friday SaturdayDocument1 paginăTime Monday Tuesday Wednesday Thursday Friday Saturdaymj CanilangÎncă nu există evaluări
- Time Monday Tuesday Wednesday Thursday Friday SaturdayDocument1 paginăTime Monday Tuesday Wednesday Thursday Friday Saturdaymj CanilangÎncă nu există evaluări
- PA Lec SchedDocument5 paginiPA Lec Schedmj CanilangÎncă nu există evaluări
- Grading System For NCM 100 - Skills Lectute and RDDocument2 paginiGrading System For NCM 100 - Skills Lectute and RDmj CanilangÎncă nu există evaluări
- Schedule For Faculty Use - DHDocument1 paginăSchedule For Faculty Use - DHmj CanilangÎncă nu există evaluări
- Grading System For NCM 100 - Skills Lectute and RDDocument2 paginiGrading System For NCM 100 - Skills Lectute and RDmj CanilangÎncă nu există evaluări
- Teaching Problem Solving in Large Introductory Classes: The View From PhysicsDocument48 paginiTeaching Problem Solving in Large Introductory Classes: The View From PhysicsAlvaro H GalvisÎncă nu există evaluări
- Wound CareDocument3 paginiWound Caremj CanilangÎncă nu există evaluări
- Laxatives PpsDocument22 paginiLaxatives Ppschan_dar100% (1)
- Anti-Asthmatic Potential of Dried Draco SpilopterusDocument6 paginiAnti-Asthmatic Potential of Dried Draco SpilopterusNxxxÎncă nu există evaluări
- Pelvic Osteotomies in The Child and Young Adult Hip: Indications and Surgical TechniqueDocument8 paginiPelvic Osteotomies in The Child and Young Adult Hip: Indications and Surgical TechniqueLeonardo Guerrero CardozoÎncă nu există evaluări
- Pa Dance's ReadingsDocument6 paginiPa Dance's Readingsdancenong35Încă nu există evaluări
- Cirrhosis Patient Education 2014Document3 paginiCirrhosis Patient Education 2014Robert G. Gish, MDÎncă nu există evaluări
- Methods of Speech Therapy Treatment For Stable Dysarthria A ReviewDocument14 paginiMethods of Speech Therapy Treatment For Stable Dysarthria A ReviewDavid Trujillo BEatoÎncă nu există evaluări
- MJDF Mcqs - Mixed - PDFDocument19 paginiMJDF Mcqs - Mixed - PDFAyesha Awan0% (3)
- Prevention of Access Recirculation During Hemodialysis TreatmentDocument26 paginiPrevention of Access Recirculation During Hemodialysis TreatmentIrma HermaliaÎncă nu există evaluări
- Anand-Paris Sewer SystemDocument25 paginiAnand-Paris Sewer Systemanand saurabh100% (1)
- Biomed IncDocument48 paginiBiomed IncriddhiÎncă nu există evaluări
- Setting Cleaning Validation Acceptance Limits For Topical FormulationsDocument8 paginiSetting Cleaning Validation Acceptance Limits For Topical Formulationsvijayns_250355172Încă nu există evaluări
- Ok Ok Notes PediaDocument14 paginiOk Ok Notes PediaChristian PasicolanÎncă nu există evaluări
- Common Ocular EmergenciesDocument33 paginiCommon Ocular EmergenciesMaimoona AimanÎncă nu există evaluări
- Course No.: BIOF216 Course Title: Water, Sanitation and Solid Waste ManagementDocument6 paginiCourse No.: BIOF216 Course Title: Water, Sanitation and Solid Waste ManagementJeswin EldhoÎncă nu există evaluări
- Acute Lymphocytic LeukemiaDocument2 paginiAcute Lymphocytic LeukemiaAlleah Salbo KepusÎncă nu există evaluări
- Drug Study - CaDocument3 paginiDrug Study - Casaint_ronald8Încă nu există evaluări
- Sore TroatDocument2 paginiSore TroatD'Say P'alaranÎncă nu există evaluări
- Profile - Plant-Strong Healthy Living - Rip Esselstyn at TedxfremontDocument7 paginiProfile - Plant-Strong Healthy Living - Rip Esselstyn at Tedxfremontapi-273526330Încă nu există evaluări
- Cord Presentation and ProlapseDocument15 paginiCord Presentation and ProlapsechandanÎncă nu există evaluări
- Denali Individual Dental All Other States - AETNADocument10 paginiDenali Individual Dental All Other States - AETNAJohn BerkowitzÎncă nu există evaluări
- Ebook Chemical Engineering Journal Vol 155 Issues 1-2 2009 ISSN.1386-8947Document19 paginiEbook Chemical Engineering Journal Vol 155 Issues 1-2 2009 ISSN.1386-8947ariyasti100% (1)
- 4ps of InnovationDocument5 pagini4ps of InnovationAdrianProud100% (2)
- Standards of Psychiatric-Mental Health Nursing PracticeDocument4 paginiStandards of Psychiatric-Mental Health Nursing PracticeAnna Sofia ReyesÎncă nu există evaluări
- Gary Null Robert Houston Penthouse Magazine 1979 - Great Cancer FraudDocument9 paginiGary Null Robert Houston Penthouse Magazine 1979 - Great Cancer FraudAnonymous AWVQB8ccJÎncă nu există evaluări
- Lopez 2021Document9 paginiLopez 2021toaldoÎncă nu există evaluări
- Assessment - and - Management - of - Patients - With - Diabetes - Mellitus (1) FINALDocument80 paginiAssessment - and - Management - of - Patients - With - Diabetes - Mellitus (1) FINALAMIT MODWALÎncă nu există evaluări
- Ssssihms PG Department Manual - Ortho DeptDocument55 paginiSsssihms PG Department Manual - Ortho DeptshanmukhaÎncă nu există evaluări
- Aplastic Anemia Pa Tho PhysiologyDocument3 paginiAplastic Anemia Pa Tho Physiologyneil052275% (4)
- Who's Who in NLPDocument10 paginiWho's Who in NLPjan_modaaltjeÎncă nu există evaluări
- Next Generation of MBBR TechnologyDocument48 paginiNext Generation of MBBR TechnologyLouay Mansour100% (1)