Documente Academic
Documente Profesional
Documente Cultură
Set
Încărcat de
Suci Asnatasia RamadhiniTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Set
Încărcat de
Suci Asnatasia RamadhiniDrepturi de autor:
Formate disponibile
The Clinical Nurse Leader as Risk Anticipator:
Optimizing the Completion and Accuracy of the Code Blue Recorder Sheet
Cathy Morano, RN BSN
Abstract Specific Aim Code Blue Recorder Revised Code Blue Sheet
Sheet Completion
A small community hospital in northern California
Evaluation Tool Post
implemented a practice improvement project in critical care
units to optimize best practices surrounding a “code blue”
The Critical Care Unit will optimize the completion and
and Accuracy
event. In-Hospital Cardiac Arrest (IHCA) is a high-risk
process of care that requires tremendous resources to deliver
accuracy of the code blue recorder sheet documentation
to 90% by July 31, 2017.
Jan 2017 to June 2017 Training
an efficient, safe, and cost-effective service. The code blue
recorder sheet summarizes the whole patient care event; this JAN FEB MAR APRIL MAY JUNE
necessitates careful documentation. As a risk anticipator, the
unit clinical nurse leader identified suboptimal variation in Kotter’s 8 Step Change CODE BLUE FOCUSED AREAS:
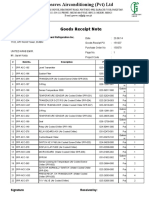
Was the code outside ICU?
2017
n=6
17%
2017
n=0
0%
2017
n=8
12%
2017 n=
4
100%
2017
n= 6
0%
2017
n= 8
50%
documentation after a microsystem assessment. This led to a
practice change project and targeted educational Model If code is outside ICU, did patient
survived?
Is the patient under Hospitalist
100% N/A 100% N/A N/A Yes
67% N/A 66% 100% 100% 100%
intervention for code blue recorders. Fifteen staff members care?
were identified from every shift to cover all IHCA events. Recorder Sheet completed? 17% N/A 38% 17% 67% 50%
Cardiac:
Baseline data indicated that the completion and accuracy of Type of the Code: Cardiac or 83% -
Cardiac N/A
75% -
Cardiac
50% Cardiac:
Cardiac: 75%
Respiratory:
Respiratory? Respiratory: 100%
the code blue documentation were critically low. A literature 17% - Resp 25% - Resp
50%
25%
Was CPR in progress upon arrival
review revealed best practices with an evidenced-based of the team?
100% N/A 100% 100% 100% 100%
educational approach including thorough assessment and Did patient survive? 67% N/A 66% 75% 50% 90%
responsiveness to staff learning needs and preparedness, Was the patient discharged alive? 0% N/A 66% 75% 0% 80%
Was there an RRT called prior to
enhancing knowledge and building confidence to impact the code?
0% N/A 0% 25% 0% 0%
patient care outcomes. Results of the educational intervention Was ACLS algorithm followed
40% N/A 88% 75% 67% 50%
appropriately?
demonstrated significant improvements in team member Was the Critique form
50% N/A 50% 0% 33% 30%
confidence in the skills specific to their role and completed?
Was this case referred for Risk
20% N/A 33% N/A 50% 0%
responsibilities. Completion and accuracy data indicated that review?
Was this a reportable event? 0% N/A 0% 0% 0% 0%
the rate improved from the baseline of 17% to 67% over the
two-month period of training. Clearly, in high acuity and high-
risk events such as IHCA, unit leaders need to carefully define
Selected References
the division of labor, role clarity, staff learning needs to
Results
implement, and maintain best practices in code blue
documentation.
Keywords: in-hospital cardiac arrest, focused training,
Power Point Carpico, B. & Jenkins, P. (2011). Resuscitation review to improve nursing performance
Presentation
during cardiac arrest. Journal for Nurses in Staff Development, 27(1). 7-12
recorder, documentation doi:10.1097/NND.0b013e 3182061ca7
Chan, P. S., Krein, S. L., Tang, F., Iwashyna, T. J., Harrod, M., Kennedy, M., …Nallamothu,
B. K. (2016). Resuscitation practices associated with survival after in-hospital cardiac arrest.
Journal of American Medical Association Cardiology, 1(2), 189-197. doi:
Global Aim Statement Why do we need a Code Team?
•Efficient and
safe
How to be an effective member?
•Be organized
•Proficient with knowledge
10.1001/jamacardio.2016.0073
Clarke, S., Apesoa-Verano, E.C., & Barton, J. (2016). Code blue: methodology for a qualitative
study of teamwork during simulated cardiac arrest. British Medical Journal, 6:e009259
and skills doi:10.1136/bmjopen-2015-009259
•Saves lives
•Able to apply standardized Prince, C. R., Hines, E. J., Chyou, P. H., & Heegeman. (2014). Finding the key to a better code:
•Reverse process code team restructure to improve performance and outcomes. Clinical Medicine
clinical death •Effective communication Research, 12(1-2), 47-57. doi: 10.3121/cmr.2014.1201
We aim to improve the completion and accuracy of the •Limit disability •Practice to maintain skills Resuscitation Central Documentation. (2017). Hospital Code Documentation: Why Document a
documentation for all in-hospital cardiac arrest (IHCA) •Clear identification of team Patient’s Resuscitation Event? Retrieved from
member roles and
events. The process begins when Code Blue is announced responsibilities
http://www.resuscitationcentral.com/documentation/hospital-code-data/
via overhead pager indicating the location of the patient The Recorder
identified as having respiratory, cardiac or both (also known •Document the entire resuscitation The benefits of a complete code blue
as cardiopulmonary) arrest. The process ends after the code process
recorder sheet:
blue recorder sheet and critique form is completed. By
working on this process, the educational intervention in
•Knowledgeable of the ACLS algorithm
•Reminds the Team Leader of the time,
name and dose of last medication
•Data help determine performance
improvement priorities
Acknowledgements
conjunction with the revised code blue recorder sheet administered •Data collected are used to monitor the
•Document cardiac rhythm and code stability of existing processes
contents will lead into the improvement of the assigned summary strips •Data will help determine if AHA guidelines Special thanks:
team member as the Code Blue Recorder to complete the •Document airway management are being followed To my supportive husband, Gary Morano
recorder sheet completely and accurately according to the •Complete Vital signs documentation •It provides information that can guide To my preceptor, mentor, & Director, Viki Ardito
•Document start and end time of the continuing care for the patient
sequence of the IHCA event, in compliance with American To our supportive professor & coach, Dr. Cathy Coleman
event •It helps to answer questions the family may
Heart Association (AHA) standard guidelines. •Indicates patient disposition have about the event, reducing the risk for
•Obtains Team Leader signature litigation
•Completes the critique form
S-ar putea să vă placă și
- Travel Itinerary: G3DW6YDocument6 paginiTravel Itinerary: G3DW6YSuci Asnatasia RamadhiniÎncă nu există evaluări
- Sap LipidDocument3 paginiSap LipidSuci Asnatasia RamadhiniÎncă nu există evaluări
- Follow UpDocument1 paginăFollow UpSuci Asnatasia RamadhiniÎncă nu există evaluări
- Diagnosis WordDocument2 paginiDiagnosis WordSuci Asnatasia RamadhiniÎncă nu există evaluări
- Tugas Evidence Based Medicine Nama: Suci Asnatasia - Ramadhini No. Mahasiswa: 1102009276 1. Treatment / Terapi - 1. PertanyaanDocument2 paginiTugas Evidence Based Medicine Nama: Suci Asnatasia - Ramadhini No. Mahasiswa: 1102009276 1. Treatment / Terapi - 1. PertanyaanSuci Asnatasia RamadhiniÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Empowerment Series Social Work With Groups Comprehensive Practice and Self Care 10Th Edition Charles Zastrow Full ChapterDocument67 paginiEmpowerment Series Social Work With Groups Comprehensive Practice and Self Care 10Th Edition Charles Zastrow Full Chapterruby.levi441100% (5)
- Lecture 5Document20 paginiLecture 5Paylaşım KanalıÎncă nu există evaluări
- Auto CadDocument67 paginiAuto CadkltowerÎncă nu există evaluări
- CoolonDocument2 paginiCoolonAnySikaÎncă nu există evaluări
- Bombas KMPDocument42 paginiBombas KMPReagrinca Ventas80% (5)
- 19 71 Hydrologic Engineering Methods For Water Resources DevelopmentDocument654 pagini19 71 Hydrologic Engineering Methods For Water Resources DevelopmentMartha LetchingerÎncă nu există evaluări
- Chapter 3 - Methods of Circuit Analysis and Circuit TheoremsDocument125 paginiChapter 3 - Methods of Circuit Analysis and Circuit TheoremsNaim NizamÎncă nu există evaluări
- Goods Receipt Note: Johnson Controls Air Conditioning and Refrigeration Inc. (YORK) DateDocument4 paginiGoods Receipt Note: Johnson Controls Air Conditioning and Refrigeration Inc. (YORK) DateSaad PathanÎncă nu există evaluări
- Bilateral Transfer of LearningDocument18 paginiBilateral Transfer of Learningts2200419Încă nu există evaluări
- Practicewith Argument Athletesas ActivistsDocument30 paginiPracticewith Argument Athletesas ActivistsRob BrantÎncă nu există evaluări
- ALTS150-12P Datasheet1Document2 paginiALTS150-12P Datasheet1mamloveÎncă nu există evaluări
- GE Uno Downlight Backlit BLDocument2 paginiGE Uno Downlight Backlit BLChen KengloonÎncă nu există evaluări
- S25580 MSDS Corn Starch FisherchiDocument6 paginiS25580 MSDS Corn Starch FisherchiProcurement ProlineÎncă nu există evaluări
- Cambridge: Global EnglishDocument34 paginiCambridge: Global EnglishLinh Nguyễn Thùy100% (1)
- Topic 3 Intellectual RevolutionDocument20 paginiTopic 3 Intellectual RevolutionOlive April TampipiÎncă nu există evaluări
- Gates Crimp Data and Dies Manual BandasDocument138 paginiGates Crimp Data and Dies Manual BandasTOQUES00Încă nu există evaluări
- FPGA Implementation For Humidity and Temperature Remote Sensing SystemDocument5 paginiFPGA Implementation For Humidity and Temperature Remote Sensing SystemteekamÎncă nu există evaluări
- With You: Full-Line CatalogDocument68 paginiWith You: Full-Line CatalogCOMIÎncă nu există evaluări
- Centrifugal Pumps: Turbo Machines Amit Pathania Roll No:09309 Mechanical EngineeringDocument4 paginiCentrifugal Pumps: Turbo Machines Amit Pathania Roll No:09309 Mechanical EngineeringAmit PathaniaÎncă nu există evaluări
- 1988 Mazda 323 Workshop Manual V1.0 (Turbo Only)Document880 pagini1988 Mazda 323 Workshop Manual V1.0 (Turbo Only)Mike Marquez100% (2)
- Evidence MODULE 1 Evidence DefinitionDocument8 paginiEvidence MODULE 1 Evidence Definitiondave BarretoÎncă nu există evaluări
- Slup 230Document24 paginiSlup 230Jelena TodorovicÎncă nu există evaluări
- Tekla SoakwayDocument2 paginiTekla SoakwayBalaji Naik100% (1)
- HCH - 15 04 004Document5 paginiHCH - 15 04 004NarvaxisÎncă nu există evaluări
- Reviewer in PE&H 1st Quarter 18-19Document7 paginiReviewer in PE&H 1st Quarter 18-19rhex minasÎncă nu există evaluări
- Filling The Propylene Gap On Purpose TechnologiesDocument12 paginiFilling The Propylene Gap On Purpose Technologiesvajidqc100% (1)
- Customer Service Metrics CalculatorDocument28 paginiCustomer Service Metrics CalculatorSelma Regita MahardiniÎncă nu există evaluări
- Kat-A 4102 Rotovalve Edition3!12!02-2013 enDocument4 paginiKat-A 4102 Rotovalve Edition3!12!02-2013 enWalter PiracocaÎncă nu există evaluări
- OB Case Study Care by Volvo UK 2020Document1 paginăOB Case Study Care by Volvo UK 2020Anima AgarwalÎncă nu există evaluări
- Pamphlet 89 Chlorine Scrubbing SystemsDocument36 paginiPamphlet 89 Chlorine Scrubbing Systemshfguavita100% (4)