Documente Academic
Documente Profesional
Documente Cultură
Cardio Vascular Mortality
Încărcat de
asdsadDrepturi de autor
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Cardio Vascular Mortality
Încărcat de
asdsadDrepturi de autor:
Articles
Cardiovascular mortality, all-cause mortality, and diabetes
incidence after lifestyle intervention for people with
impaired glucose tolerance in the Da Qing Diabetes
Prevention Study: a 23-year follow-up study
Guangwei Li, Ping Zhang, Jinping Wang, Yali An, Qiuhong Gong, Edward W Gregg, Wenying Yang, Bo Zhang, Ying Shuai, Jing Hong,
Michael M Engelgau, Hui Li, Gojka Roglic, Yinghua Hu, Peter H Bennett
Summary
Lancet Diabetes Endocrinol Background Lifestyle interventions among people with impaired glucose tolerance reduce the incidence of diabetes,
2014; 2: 474–80 but their effect on all-cause and cardiovascular disease mortality is unclear. We assessed the long-term effect of
Published Online lifestyle intervention on long-term outcomes among adults with impaired glucose tolerance who participated in the
April 3, 2014
Da Qing Diabetes Prevention Study.
http://dx.doi.org/10.1016/
S2213-8587(14)70057-9
See Comment page 441 Methods The study was a cluster randomised trial in which 33 clinics in Da Qing, China—serving 577 adults with
Department of Endocrinology,
impaired glucose tolerance—were randomised (1:1:1:1) to a control group or lifestyle intervention groups (diet or
China-Japan Friendship exercise or both). Patients were enrolled in 1986 and the intervention phase lasted for 6 years. In 2009, we followed up
Hospital, Beijing, China participants to assess the primary outcomes of cardiovascular mortality, all-cause mortality, and incidence of diabetes
(Prof G Li MD, W Yang MD, in the intention-to-treat population.
B Zhang MD,
Y Shuai BD, J Hong MD);
Center of Endocrinology Findings Of the 577 patients, 439 were assigned to the intervention group and 138 were assigned to the control group
and Cardiovascular Disease, (one refused baseline examination). 542 (94%) of 576 participants had complete data for mortality and 568 (99%)
National Center of Cardiology contributed data to the analysis. 174 participants died during the 23 years of follow-up (121 in the intervention group vs 53
& Fuwai Hospital, Beijing,
China (G Li, Y An MD,
in the control group). Cumulative incidence of cardiovascular disease mortality was 11·9% (95% CI 8·8–15·0) in the
Q Gong MD); Division of intervention group versus 19·6% (12·9–26·3) in the control group (hazard ratio [HR] 0·59, 95% CI 0·36–0·96; p=0·033).
Diabetes Translation All-cause mortality was 28·1% (95% CI 23·9–32·4) versus 38·4% (30·3–46·5; HR 0·71, 95% CI 0·51–0·99; p=0·049).
(P Zhang PhD, E W Gregg PhD),
Incidence of diabetes was 72·6% (68·4–76·8) versus 89·9% (84·9–94·9; HR 0·55, 95% CI 0·40–0·76; p=0·001).
Center for Global Health
(M M Engelgau MD), Centers for
Disease Control and Interpretation A 6-year lifestyle intervention programme for Chinese people with impaired glucose tolerance can
Prevention, Atlanta, GA, USA; reduce incidence of cardiovascular and all-cause mortality and diabetes. These findings emphasise the long-term
Department of Cardiology,
clinical benefits of lifestyle intervention for patients with impaired glucose tolerance and provide further justification
Da Qing First Hospital, Da Qing,
China (J Wang MD, H Li MD, for adoption of lifestyle interventions as public health measures to control the consequences of diabetes.
Y Hu MD); Department of
Management of Funding Centers for Disease Control and Prevention, WHO, the China-Japan Friendship Hospital, Da Qing First Hospital.
Noncommunicable Diseases,
World Health Organization,
Geneva, Switzerland Introduction implications. We assessed such effects in people who
(G Roglic MD); and Phoenix Lifestyle interventions for people with impaired glucose participated in the Da Qing Diabetes Prevention Study
Epidemiology and Clinical tolerance can delay or prevent the development of over a 23-year period.
Research Branch, National
diabetes and lead to improvements for other
Institute of Diabetes and
Digestive and Kidney Diseases, cardiovascular risk factors.1–11 However, whether these Methods
Phoenix, AZ, USA changes reduce the incidence of long-term complications, Study design and participants
(P H Bennett FRCP) and the excess cardiovascular disease and all-cause The design of the Da Qing Diabetes Prevention Study and
Correspondence to: mortality that accompany diabetes is uncertain.12,13 In our the 20-year follow-up study have been reported pre-
Prof Guangwei Li, Department
previous analysis7 of 20-year follow-up data from the viously.1,7,14 In 1986, 33 primary care clinics in Da Qing,
of Endocrinology, 167 Beilishi
Road, Xicheng District, Beijing, Da Qing Diabetes Prevention Study, we reported a China serving 577 people with impaired glucose tolerance
100037, China statistically insignificant 17% reduction in cardiovascular were enrolled into a cluster randomised trial. All patients
guangwei_li@medmail.com.cn disease mortality and a significantly lower incidence of treated at the clinics were eligible if they had impaired
Or severe diabetic retinopathy that seems to have been glucose tolerance in 1985. We did a 20-year follow-up
Dr Ping Zhang, Division of mediated primarily by delaying the onset of diabetes.14 study up to the end of 20067 and here report results after
Diabetes Translation, Centers for Because cardiovascular disease is the major cause of an additional 3 years. The institutional review boards of
Disease Control and Prevention,
4770 Buford HWY, NE, F-75
excess mortality in people with impaired glucose WHO and the China-Japan Friendship Hospital approved
Atlanta, GA 30341, USA tolerance, more definitive information about the effect of the protocol. All study participants, or their proxies who
pzhang@cdc.gov lifestyle intervention on cardiovascular disease and all- provided information about deceased participants, gave
cause mortality in such people has crucial public health written informed consent.
474 www.thelancet.com/diabetes-endocrinology Vol 2 June 2014
Downloaded for Anonymous User (n/a) at University of Queensland Library from ClinicalKey.com.au by Elsevier on September 24, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
Articles
Randomisation and masking any diabetes-related macrovascular or microvascular
Clinics were cluster randomised (1:1:1:1) to one of three complications. This report includes data for only the first
lifestyle interventions (25 clinics with a total of three because no new data for diabetes-related
439 people) or a control group (eight clinics with macrovascular and microvascular complications were
138 people). Of the 25 intervention clinics, nine collected at the 23-year follow-up.
(148 participants) were assigned to a diet only
intervention, nine clinics (155 participants) to an Statistical analysis
exercise only intervention, and seven clinics Power calculations were done for the original 6-year
(136 participants) to a diet plus exercise intervention. intervention trial. For the present study we estimated
The diet intervention was designed to produce weight minimal detectable differences. With an α of 0·05, we
loss in those who were overweight or obese, and to estimated that there was an 80% chance of detecting a
reduce simple carbohydrate and alcohol intake in people 43% reduction in all-cause mortality and a 63% reduction
of normal weight. The exercise intervention was in cardiovascular disease mortality when comparing the
designed to increase the leisure time spent doing control group with the combined lifestyle intervention
physical activity. groups.
All participants (including those at clinics in the control The observational period for mortality was from date of
group) received examinations at baseline, 2 years, 4 years, randomisation to date of death, loss to follow-up, or Dec 31,
and 6 years after randomisation and at 20-year and 2009, whichever came first. For diabetes incidence, the
23-year follow-up. Participants in the control group observational period was from the date of randomisation
received standard medical care. The interventions were to the date of diagnosis, or Dec 31, 2009, whichever came
delivered for 6 years (1986–92), after which all participants first. As the incidence of diabetes at both the end of the
were informed of the results and asked to continue with 6-year intervention period and the 20-year follow-up period
usual medical care. was similar in each of the three intervention groups, we
Investigators who assessed the outcomes at follow-up combined the intervention groups a priori to increase the
were masked to treatment allocation. Patients and other
investigators were not masked. 577 patients enrolled in randomly assigned clinic
Procedures 1 refused baseline examination
We tried to follow up all the original study participants to
establish their vital status. For deceased participants, we
collected date and cause of death from death certificates, 438 in intervention group 138 in control group
reviews of medical records, and interviews with proxy
informants. We asked proxy informants about the date, 31 lost to 3 lost to
place, and circumstances of death along with information follow-up follow-up
about hospitals or physicians from whom the participant
had received care around the time of death. We obtained 407 assessed 135 assessed
medical records and death certificates and, together with
the informant interviews, they were reviewed and Figure 1: Trial profile
adjudicated independently by two doctors (JW and YA) to
establish the underlying cause of death. Disagreements
were resolved by a third senior physician (HL or YH). Intervention Control
group group
Causes of death were classified into two categories: (n=430) (n=138)
cardiovascular disease death (defined as death attributed
Sex
to coronary heart disease, stroke, or sudden death), and
Men 230 (53%) 79 (57%)
non-cardiovascular disease death (death from all other
Women 200 (47%) 59 (43%)
causes).
Age (years) 44·7 (9·3) 46·6 (9·3)
Diabetes was defined by 1985 WHO criteria with the
BMI (kg/m2) 25·7 (3·8) 26·2 (3·8)
results of oral glucose tolerance tests done every 2 years
Systolic blood pressure (mm Hg) 132·4 (23·5) 134·4 (23·4)
between 1986 and 1992, and at the 20-year and 23-year
Diastolic blood pressure (mm Hg) 87·3 (14·5) 88·5 (13·5)
follow-up examinations,15 or from a report of physician-
diagnosed diabetes with evidence in the medical record FPG (mmol/L) 5·6 (0·8) 5·5 (0·8)
of high glucose concentrations, or use of hypoglycaemic 2hPG (mmol/L) 9·0 (0·9) 9·0 (16·1)
drugs, as described previously.7 Current smoker (%) 165 (38%) 69 (50%)
Data are n (%) or mean (SD). FPG=fasting venous plasma glucose. 2hPG=venous
Outcomes plasma glucose concentration 2 h after intake of 75 g oral glucose.
The four primary outcomes were all-cause mortality,
Table 1: Baseline characteristics
cardiovascular disease mortality, diabetes incidence, and
www.thelancet.com/diabetes-endocrinology Vol 2 June 2014 475
Downloaded for Anonymous User (n/a) at University of Queensland Library from ClinicalKey.com.au by Elsevier on September 24, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
Articles
statistical power to detect a mortality difference attributable Results
to the intervention. Mortality and diabetes incidence were Of the original 577 study participants, one declined the
calculated as the number of events divided by total person- baseline examination, eight had only a baseline
years since randomisation. examination, and 20 participants were lost to follow-up
We assessed cumulative all-cause and cardiovascular during the 6-year intervention period, mainly because of
mortality with the Kaplan-Meier method. We fitted a job relocation. During the subsequent 17 years after the
Weibull proportional hazards model16 with the SAS intervention, only six participants were lost to follow-up.
NLMIXED procedure for the primary analysis. The time Thus, 542 participants (94%) had complete data for
to all-cause and cardiovascular disease death or date of mortality and 568 (99%) contributed data to the analysis
diagnosis of diabetes was treated as the dependent (figure 1). 563 participants (98%) had complete data for
variable. Treatment group was included as a fixed effect diabetes incidence. Table 1 shows the baseline
and clinic was included as a random effect. No other characteristics.
covariates were adjusted for because the original study 174 participants died during the 23 years of follow-up
was a cluster randomised trial. We estimated hazard (121 in the intervention group and 53 in the control
ratios (HRs) and 95% CIs from the NLMIXED model. group). The cumulative incidence of all-cause death was
Differences were considered statistically significant if 28·1% (95% CI 23·9–32·4) in the intervention group
p<0·05 in two-sided tests. All primary analyses were for and 38·4% (95% CI 30·3–46·5) in the control group,
the intention-to-treat population. with an HR (adjusted for cluster randomisation) of 0·71
Mortality of people with and without diabetes varies (95% CI 0·51–0·99; p=0·049; table 2, figure 2). Few
greatly by sex and age.17–19 Therefore, we did post-hoc patients died during the first 10 years of the study, but
secondary analyses to assess the effect of intervention on the rates rose progressively thereafter (table 2, figure 2).
the primary outcomes of all-cause mortality and 78 participants died as a result of cardiovascular disease;
cardiovascular disease mortality separately in women 51 in the intervention group versus 27 in the control
and men. Because of an imbalance in the age distribution group. Cumulative incidences were 11·9% (95% CI
and smoking rates between men and women in the 8·8–15·0) versus 19·6% (95% CI 12·9–26·3; HR 0·59,
intervention and control groups, we adjusted for these 95% CI 0·36–0·96; p=0·03; table 2, figure 2). Significant
differences—as well as for the effect of delay in onset of differences between groups in the incidence of
diabetes—in post-hoc multivariable analyses with the diabetes—present at the end of the 6-year intervention
SAS NLMIXED procedure. We did the statistical analyses period and at 20-year follow-up1,7—persisted, with a
with SAS (version 9.1). cumulative incidence of 72·6% (95% CI 68·4–76·8) in
the intervention group and 89·9% (95% CI 84·9–94·9)
Role of the funding source in the control group (HR 0·55, 95% CI 0·40–0·76;
Employees of the study sponsors were involved in the p=0·001; table 2, figure 2).
study design; collection, analysis, interpretation of the Secondary post-hoc analyses stratified by sex and age
data; and the writing of the report. The corresponding showed substantial differences between women and
authors had full access to all data in the study and had men for the effect of intervention on all-cause and
See Online for appendix the final responsibility for the decision to submit for cardiovascular disease mortality (table 3, appendix).
publication. Among women, the cumulative incidence of all-cause
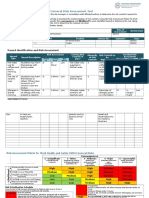
Intervention group Control group Hazard ratio p value
(n=430) (n=138) (95% CI)
All-cause mortality
Deaths 121 (28%) 53 (38%) ·· ··
Deaths per 1000 person-years (95% CI) 14·3 (11·8–16·9) 19·9 (14·5–25·2) ·· ··
Cumulative incidence (%; 95% CI) 28·1% (23·9–32·4) 38·4% (30·3–46·5) 0·71 (0·51–0·99) 0·049
Cardiovascular disease mortality
Deaths 51 (12%) 27 (20%) ·· ··
Deaths per 1000 person-years (95% CI) 6·0 (4·4–7·7) 10·1 (6·3–14·0) ·· ··
Cumulative incidence (%; 95% CI) 11·9% (8·8–15·0) 19·6% (12·9–26·3) 0·59 (0·36–0·96) 0·033
Diabetes incidence
Cases of diabetes 312 (73%) 124 (90%) ·· ··
Cases per 1000 person-years (95% CI) 73·2 (65·1–81·3) 122·9 (101·3–144·5) ·· ··
Cumulative incidence (%; 95% CI) 72·6% (68·4–76·8) 89·9% (84·9–94·9) 0·55 (0·40–0·76) 0·001
Data are n (%) unless stated otherwise. Hazard ratios adjusted by clinic.
Table 2: Effect of lifestyle intervention on all-cause mortality, cardiovascular disease mortality, and diabetes (1986–2009)
476 www.thelancet.com/diabetes-endocrinology Vol 2 June 2014
Downloaded for Anonymous User (n/a) at University of Queensland Library from ClinicalKey.com.au by Elsevier on September 24, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
Articles
mortality in the control group was almost double that in
the intervention group (table 3) and cardiovascular A
45 Control group
disease mortality showed a similar pattern (table 3). Intervention group
40
Conversely, for men, the intervention had no significant
Proportion of participants (%)
effect on either all-cause mortality or cardiovascular 35
disease mortality (table 3), although the reduction in 30
diabetes incidence was much the same in men and 25
women (table 3).
20
A greater proportion of men than women were smokers
(61% vs 16%) and mean age in the control group was 15
higher for men than for women (appendix). A higher 10
percentage of women were smokers in the control 5
HR 0·71, 95% CI (0·51–0·99)
compared with the intervention group (appendix). We 0
did a post-hoc multivariable analysis to test whether such 0 2 4 6 8 10 12 14 16 18 20 22 23
differences in baseline characteristics could account for Number at risk
the overall reduction of mortality and differences in the Control group 138 137 135 130 127 118 113 108 103 99 95 84 82
Intervention 438 426 412 395 384 373 364 355 338 321 305 290 286
effectiveness of the intervention between the sexes group
(appendix). However, after adjustment for age, sex,
smoking and the interaction between sex and B
25
intervention , the effect of lifestyle intervention remained
significant for both all-cause and cardiovascular disease
Proportion of participants (%)
20
mortality, suggesting that differences in baseline
characteristics did not account for the differences.
15
Because lifestyle intervention delays the onset of
diabetes and reduces the incidence of diabetes, we
10
assessed how mortality was affected by the time free
from diabetes, which was defined as the time between
randomisation and onset of diabetes (appendix). 5
Increased delay in the onset of diabetes was associated HR 0·59, 95% CI (0·36–0·96)
with significantly lower all-cause and cardiovascular 0
0 2 4 6 8 10 12 14 16 18 20 22 23
disease mortality. After inclusion of time to onset of
diabetes in the multivariable models the intervention Number at risk
Control group 138 137 135 130 127 118 113 108 103 99 95 84 82
variable was no longer statistically significant, suggesting Intervention 438 426 412 395 384 373 364 355 338 321 305 290 286
that the reduction in mortality associated with the group
intervention is mediated by its effect in delaying the C
onset of diabetes. 100
90
Discussion 80
This study is the first randomised clinical trial to show
Proportion of participants (%)
70
that lifestyle intervention in people with impaired
glucose tolerance reduces all-cause and cardiovascular 60
disease mortality (panel). These findings seem to mainly 50
be a result of lower mortality among women in the
40
intervention group. The Malmo study13 showed lower
mortality over a 12-year period in men with impaired 30
glucose tolerance treated with lifestyle intervention 20
compared with a group who received routine treatment,
10
but the study was not randomised. Other lifestyle HR 0·55, 95% CI (0·40–0·76)
studies—such as the Finnish Diabetes Prevention Study2 0
0 2 4 6 8 10 12 14 16 18 20 22 23
and the Diabetes Prevention Program3—consistently
showed that a lifestyle intervention could reduce the Follow-up (years)
Number at risk
incidence of diabetes and decrease other cardiovascular Control group 138 105 69 48 40 37 34 27 27 23 14 13 13
disease risk factors8,10,11,13 but have not reported a reduction Intervention 438 387 314 250 230 206 192 161 147 136 114 114 114
group
in the incidence of all-cause and cardiovascular disease
mortality. Moreover, in the Look AHEAD study,23 a Figure 2: Cumulative incidence of (A) all-cause mortality, (B) cardiovascular disease mortality, and (C)
lifestyle intervention designed to produce weight loss in diabetes incidence over the 23-year follow-up (1986–2009)
obese or overweight people with diabetes did not HR=hazard ratio.
www.thelancet.com/diabetes-endocrinology Vol 2 June 2014 477
Downloaded for Anonymous User (n/a) at University of Queensland Library from ClinicalKey.com.au by Elsevier on September 24, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
Articles
Women Men
Control group Intervention group Hazard ratio p value Control group Intervention group Hazard ratio p value
(n=59) (n=200) (95% CI)* (n=79) (n=230) (95% CI)*
All-cause mortality
Number of deaths 17 30 ·· ·· 36 91 ·· ··
Deaths per 1000 person-years (95% CI) 14·1 (7·4–20·8) 7·4 (4·7–10·0) ·· ·· 24·7 (16·6–32·7) 20·8 (16·6–25·1) ·· ··
Cumulative incidence (%; 95% CI) 28·8% (17·2–40·4) 15·0% (10·1–19·9) 0·46 (0·24–0·87) 0·02 45·6% (34·6–56·6) 39·6% (33·3–45·9) 0·97 (0·65–1·46) 0·9
Cardiovascular disease mortality
Number of deaths 10 12 ·· ·· 17 39 ·· ··
Deaths per 1000 person-years (95% CI) 8·3 (3·2–13·4) 3·0 (1·3–4·6) ·· ·· 11·6 (6·1–17·2) 8·9 (6·1–11·7) ·· ··
Cumulative incidence (%; 95% CI) 17·0 (7·4–26·6) 6·0 (2·7–9·3) 0·28 (0·11–0·71) 0·01 21·5 (12·5–30·5) 17·0 (12·2–21·8) 0·91 (0·50–1·65) 0·7
Diabetes incidence
Number with diabetes 55 148 ·· ·· 69 164 ·· ··
Cases per 1000 person-years (95% CI) 128·5 (94·5–162·5) 74·9 (62·8–86·9) ·· ·· 118·8 (90·7–146·8) 71·8 (60·8–82·8) ·· ··
Cumulative incidence (%; 95% CI) 93·2 (86·7–99·7) 74·0 (67·9–80·1) 0·55 (0·35–0·87) 0·006 87·3 (80·0–94·6) 71·3 (65·4–77·2) 0·56 (0·39–0·81) 0·004
*Adjusted for randomisation by clinic and age.
Table 3: Effect of lifestyle intervention on all-cause mortality, cardiovascular disease mortality, and diabetes in women and men (1986–2009)
study, a difference in cardiovascular disease mortality
Panel: Research in context between the intervention and control group started to
emerge 12 years after the study began, slowly increased
Systematic review
to a 17% difference by the 20-year follow-up,7 but became
Three systematic reviews20–22 of randomised controlled clinical trials have assessed the
statistically significant only after 23 years (figure 2).
effects of lifestyle intervention on prevention of type 2 diabetes for people with impaired
The reduction in mortality mainly occurred in women;
glucose tolerance. They show that dietary or physical activity interventions reduce the
the intervention seemed to have little effect in men,
incidence of diabetes, not only during the period of active intervention,20 but also for
despite similar reductions in the incidence of diabetes.
many years afterwards: for 13 years or more in the Finnish Diabetes Prevention study,11 at
The prevalence of smoking at baseline was much higher
least 10 years in the US Diabetes Prevention Program,8 and 20 years in the Da Qing
for men than for women, and epidemiological analysis of
Diabetes Prevention Study.7 Lifestyle interventions for people with impaired glucose
the whole study population showed that smoking
tolerance are also associated with amelioration of some cardiovascular risk factors such as
increased the risk of all-cause death by almost 50% (data
blood pressure and concentrations of HDL and LDL cholesterol, and triglycerides.10 The risk
not shown). Nevertheless, adjustment for imbalances in
of death for people with type 2 diabetes is about twice that of people of a similar age who
smoking and age did not account for the apparent sex
do not have diabetes. A key question is whether or not lifestyle intervention to prevent or
differences in mortality, nor did this adjustment eliminate
delay the onset of diabetes can lower this excess mortality risk in people with impaired
the overall beneficial effect of the intervention. Poorer
glucose tolerance. However, to date, no randomised clinical trials have reported a
compliance with lifestyle intervention by men than by
significant reduction for either cardiovascular disease mortality or all-cause mortality.21,22
women, or differences in unmeasured confounders,
Interpretation might also have contributed to more favourable outcomes
Our study shows that a 6-year period of lifestyle intervention in Chinese people with for women. We have been unable to establish any
impaired glucose tolerance reduced the incidence of diabetes over a protracted period, definitive reasons for differences in the effect of the
and was ultimately associated with a significant reduction in total and cardiovascular intervention on mortality between men and women.
disease mortality. This reduction in mortality seems to be partly mediated by a delay in Our study has several strengths. First, individuals with
onset of diabetes. These findings provide yet further justification to implement lifestyle impaired glucose tolerance were recruited by screening a
interventions for people with impaired glucose tolerance as clinical and public health well-defined population and most people who were
measures to control the long-term consequences of diabetes. screened were enrolled in the trial.1 Consequently, the
findings are probably generalisable to most people in
significantly reduce cardiovascular disease events or China with impaired glucose tolerance. Second,
cardiovascular disease mortality. A key difference randomisation by clinic rather than by the individual
between these studies and the Da Qing Diabetes minimises the likelihood of contamination between the
Prevention Study is the length of follow-up; in previous intervention and control groups. Our primary analyses
studies, the length of follow-up might have been were adjusted to control for the cluster randomisation.
insufficient to detect an effect of intervention on Third, follow-up for mortality is very high (94%), reducing
mortality. Although the association between duration of non-response bias. Of the 35 participants who were lost to
diabetes and mortality is well established, serious chronic follow-up, 29 were lost during the initial active
complications and excess mortality typically only occur intervention phase of the study mainly because of
after at least 10 years of having diabetes.24–28 In the present relocation for work and migration from Da Qing. Fourth,
478 www.thelancet.com/diabetes-endocrinology Vol 2 June 2014
Downloaded for Anonymous User (n/a) at University of Queensland Library from ClinicalKey.com.au by Elsevier on September 24, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
Articles
all participants received usual care from the primary care 5·1 million excess deaths and at least US$548 billion in
clinics in a single health-care system in Da Qing, which health-care expenditure in 2013.33 Our findings imply
was provided by the state-run oil company. This reduces that implementation of lifestyle intervention for people
the likelihood that variations in medical care could have with impaired glucose tolerance—especially women—
biased the results. Fifth, diabetes incidence, mortality, who are at high risk for diabetes in China, or elsewhere,
and causes of death were assessed systematically. would reduce the incidence of diabetes and associated
Diabetes was assessed by oral glucose tolerance test every health-care expenditure, eventually resulting in a lower
2 years during the 6-year intervention period and at the number of diabetes-related deaths.
20-year and 23-year follow-up examinations, and then Contributors
systematically measured, albeit by conventional clinical GL coordinated and designed the study, acquired funding, collected data,
methods, for the remainder of the follow-up period. did the statistical analysis, and wrote the report. PZ coordinated and
designed the study, acquired funding, did the statistical analysis, and
Finally, and perhaps most importantly, the follow-up wrote the report. JW and QG designed the study, collected data, and did
period lasted for 23 years, providing enough time for the the statistical analysis. YA collected data and did the statistical analysis.
development of the chronic complications of diabetes and EWG and MME designed the study, acquired funding, did the statistical
a sufficient number of deaths to enable us to detect analysis, and wrote the report. WY designed the study. BZ, YS, JH, and
HL collected data. GR designed the study and acquired funding. YH
differences in mortality between the control and designed the study and collected data. PHB designed the study, did the
intervention groups. statistical analysis, and wrote the report.
The study has some important limitations. First, Declaration of interests
because of the small size of the original trial, we combined We declare that we have no competing interests.
the three intervention groups to provide sufficient power. Acknowledgments
Second, different methods of follow-up were used during Supported by CDC/WHO Cooperative Agreement No. U58/
the 6 years of active intervention compared with the CCU424123-01-02 and the China-Japan Friendship Hospital. We thank
subsequent years. Nevertheless, the baseline and follow- the participants in the original Da Qing Diabetes Prevention Study and
their proxies who contributed to the follow-up study. We also thank
up assessments were systematic and identical in the Lingzhi Kong, China Ministry of Health, the leadership at the
control and intervention groups. Third, not all deaths China-Japan Friendship Hospital, Da Qing First Hospital, the Da Qing
were documented by death certificate. However, death City Health Bureau, and the Beijing and West Pacific Regional Office of
WHO for their general support. We thank Xilin Yang (Tianjin Medical
was ascertained from hospital records for more than 90%
University), Yang Yang (National Center of Cardiology and Fuwai
of those who died. This method has been used Hospital, China), and Ted Thompson (Centers for Disease Control and
successfully in other studies29,30 of mortality in low-income Prevention, USA) for statistical advice. Our special thanks go to the late
and middle-income countries. Fourth, the study was Prof Xiaoren Pan as this study would not have been possible without
his leadership in the design and implementation of the original
originally designed and powered to establish whether a
Da Qing Diabetes Prevention Study. The contents of this report are
lifestyle intervention could reduce the incidence of solely the responsibility of the authors and do not necessarily represent
diabetes over a 6-year period. Only later, after this the official positions of the Centers for Disease Control and Prevention,
hypothesis had been proven, was the follow-up phase the National Institute of Diabetes and Digestive and Kidney Diseases,
or WHO.
designed. Consequently, we lack systematic information
about changes in behaviour and cardiovascular risk References
1 Pan XR, Li GW, Hu YH, et al. Effects of diet and exercise in
factors such as smoking habits, blood pressure, serum preventing NIDDM in people with impaired glucose tolerance. The
cholesterol concentration, and drug use beyond the 6-year Da Qing IGT and Diabetes Study. Diabetes Care 1997; 20: 537–44.
active intervention phase. This shortcoming limits our 2 Tuomilehto J, Lindstrom J, Eriksson JG, et al. Prevention of type 2
diabetes mellitus by changes in lifestyle among subjects with
ability to investigate possible explanatory variables. impaired glucose tolerance. N Engl J Med 2001; 344: 1343–50.
However, the primary analyses based on the initial cluster 3 Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the
randomisation of participants are robust and only used incidence of type 2 diabetes with lifestyle intervention or
metformin. N Engl J Med 2002; 346: 393–403.
information for mortality outcomes that can be obtained
4 Ratner R, Goldberg R, Haffner S, et al. Impact of intensive lifestyle
reliably in retrospect from death certificates, medical and metformin therapy on cardiovascular disease risk factors in the
records, and informant interviews. diabetes prevention program. Diabetes Care 2005; 28: 888–94.
This study is the first to show that lifestyle intervention 5 Kosaka K, Noda M, Kuzuya T. Prevention of type 2 diabetes by
lifestyle intervention: a Japanese trial in IGT males.
in people with impaired glucose tolerance can both Diabetes Res Clin Pract 2005; 67: 152–62.
reduce the incidence of diabetes and decrease mortality, 6 Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD,
and so it has important implications for public health Vijay V. The Indian Diabetes Prevention Programme shows that
lifestyle modification and metformin prevent type 2 diabetes in
policy about diabetes prevention in China and worldwide. Asian Indian subjects with impaired glucose tolerance (IDPP-1).
In China, as elsewhere, the health and economic burdens Diabetologia 2006; 49: 289–97.
of diabetes are large and growing. In 2008, an estimated 7 Li G, Zhang P, Wang J, et al. The long-term effect of lifestyle
interventions to prevent diabetes in the China Da Qing Diabetes
92 million adults in China (9·7% of the adult population) Prevention Study: a 20-year follow-up study. Lancet 2008;
had diabetes and 148 million (15·5%) had prediabetes.31 371: 1783–89.
A more recent study reports an even larger estimate of 8 Knowler WC, Fowler SE, Hamman RF, et al. 10-year follow-up of
diabetes incidence and weight loss in the Diabetes Prevention
113·9 million (11·6% of adults) with diabetes in 2010.32 Program Outcomes Study. Lancet 2009; 374: 1677–86.
Worldwide, diabetes was estimated to be responsible for
www.thelancet.com/diabetes-endocrinology Vol 2 June 2014 479
Downloaded for Anonymous User (n/a) at University of Queensland Library from ClinicalKey.com.au by Elsevier on September 24, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
Articles
9 Saito T, Watanabe M, Nishida J, et al. Lifestyle modification and 20 Yamaoka K, Tango T. Efficacy of lifestyle education to prevent type 2
prevention of type 2 diabetes in overweight Japanese with impaired diabetes: a meta-analysis of randomized controlled trials.
fasting glucose levels: a randomized controlled trial. Diabetes Care 2005; 28: 2780–86.
Arch Intern Med 2011; 171: 1352–60. 21 Hopper I, Billah B, Skiba M, Krum H. Prevention of diabetes and
10 Orchard TJ, Temprosa M, Barrett-Connor E, et al. Long-term effects reduction in major cardiovascular events in studies of subjects with
of the Diabetes Prevention Program interventions on cardiovascular prediabetes: meta-analysis of randomised controlled clinical trials.
risk factors: a report from the DPP Outcomes Study. Diabet Med Eur J Cardiovasc Prev Rehabil 2011; 18: 813–23.
2013; 30: 46–55. 22 Yoon U, Kwok LL, Magkidis A. Efficacy of lifestyle interventions
11 Lindstrom J, Peltonen M, Eriksson JG, et al. Improved lifestyle and in reducing diabetes incidence in patients with impaired glucose
decreased diabetes risk over 13 years: long-term follow-up of the tolerance: a systematic review of randomized controlled trials.
randomised Finnish Diabetes Prevention Study (DPS). Diabetologia Metabolism 2013; 62: 303–14.
2013; 56: 284–93. 23 Wing RR, Reboussin D, Lewis CE. Intensive lifestyle intervention
12 Uusitupa M, Peltonen M, Lindstrom J, et al. Ten-year mortality and in type 2 diabetes. N Engl J Med 2013; 369: 2358–59.
cardiovascular morbidity in the Finnish Diabetes Prevention 24 Knowler WC, Sartor G, Melander A, Schersten B. Glucose tolerance
Study--secondary analysis of the randomized trial. PLoS One 2009; and mortality, including a substudy of tolbutamide treatment.
4: e5656. Diabetologia 1997; 40: 680–86.
13 Eriksson KF, Lindgarde F. No excess 12-year mortality in men 25 Kim NH, Pavkov ME, Looker HC, et al. Plasma glucose regulation
with impaired glucose tolerance who participated in the Malmo and mortality in pima Indians. Diabetes Care 2008; 31: 488–92.
Preventive Trial with diet and exercise. Diabetologia 1998; 26 Brun E, Nelson RG, Bennett PH, et al. Diabetes duration and
41: 1010–16. cause-specific mortality in the Verona Diabetes Study. Diabetes Care
14 Gong Q, Gregg EW, Wang J, et al. Long-term effects of a 2000; 23: 1119–23.
randomised trial of a 6-year lifestyle intervention in impaired 27 Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year
glucose tolerance on diabetes-related microvascular complications: follow-up of intensive glucose control in type 2 diabetes.
the China Da Qing Diabetes Prevention Outcome Study. N Engl J Med 2008; 359: 1577–89.
Diabetologia 2011; 54: 300–07.
28 Hu FB, Stampfer MJ, Solomon CG, et al. The impact of diabetes
15 WHO Study Group. Diabetes Mellitus. Report of a WHO Study mellitus on mortality from all causes and coronary heart disease in
Group. 727, 1–113; Geneva: World Health Organization, 1985. women: 20 years of follow-up. Arch Intern Med 2001; 161: 1717–23.
16 Collett D. Modeling survival data in medical research. London: 29 Gajalakshmi V, Peto R. Commentary: verbal autopsy procedure for
Chapman & Hall, 1994. adult deaths. Int J Epidemiol 2006; 35: 748–50.
17 Barnett KN, Ogston SA, McMurdo ME, Morris AD, Evans JM. 30 Yang G, Rao C, Ma J, et al. Validation of verbal autopsy procedures
A 12-year follow-up study of all-cause and cardiovascular mortality for adult deaths in China. Int J Epidemiol 2006; 35: 741–48.
among 10,532 people newly diagnosed with Type 2 diabetes in
31 Yang W, Lu J, Weng J, et al. Prevalence of diabetes among men and
Tayside, Scotland. Diabet Med 2010; 27: 1124–29.
women in China. N Engl J Med 2010; 362: 1090–101.
18 Seshasai SR, Kaptoge S, Thompson A, et al. Diabetes mellitus,
32 Xu Y, Wang L, He J, et al. Prevalence and control of diabetes in
fasting glucose, and risk of cause-specific death. N Engl J Med 2011;
Chinese adults. JAMA 2013; 310: 948–59.
364: 829–41.
33 International Diabetes Federation. Diabetes Atlas, 5th edn.
19 Sievers ML, Nelson RG, Knowler WC, Bennett PH. Impact of
Brussels: International Diabetes Federation, 2011.
NIDDM on mortality and causes of death in Pima Indians.
Diabetes Care 1992; 15: 1541–49.
480 www.thelancet.com/diabetes-endocrinology Vol 2 June 2014
Downloaded for Anonymous User (n/a) at University of Queensland Library from ClinicalKey.com.au by Elsevier on September 24, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (894)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Pangmalakasan NP1Document134 paginiPangmalakasan NP1MikEeAyanEsterasÎncă nu există evaluări
- Factors Influencing HIV Disclosure Among People Living With HIV/AIDS in Nigeria: A Systematic Review Using Narrative Synthesis and Meta-AnalysisDocument16 paginiFactors Influencing HIV Disclosure Among People Living With HIV/AIDS in Nigeria: A Systematic Review Using Narrative Synthesis and Meta-AnalysisTrisna SariÎncă nu există evaluări
- Case Study Obstetric PatientDocument19 paginiCase Study Obstetric PatientPrinz Lozano100% (1)
- LabCorp+Virology+Report+Quantitative+RNA CDocument5 paginiLabCorp+Virology+Report+Quantitative+RNA CSooah ParkÎncă nu există evaluări
- Training BrochureDocument60 paginiTraining BrochureAbdur RahmanÎncă nu există evaluări
- Sewage-Treatment Plant PDFDocument3 paginiSewage-Treatment Plant PDFBanhisikha Goswami OfficialÎncă nu există evaluări
- Negative AutopsyDocument21 paginiNegative Autopsydr rizwanÎncă nu există evaluări
- Toronto CA - Rest of The World Should Learn From Canada-Toronto CA (2023)Document3 paginiToronto CA - Rest of The World Should Learn From Canada-Toronto CA (2023)haroldpsbÎncă nu există evaluări
- Cancer Prevention & Screening GuideDocument56 paginiCancer Prevention & Screening Guidenoorulzaman84Încă nu există evaluări
- Paediatric tuberculosis assessment scoresDocument1 paginăPaediatric tuberculosis assessment scoresGalaleldin AliÎncă nu există evaluări
- PCOS Factors BacolodDocument3 paginiPCOS Factors BacolodPrincess Faniega SugatonÎncă nu există evaluări
- Risk Assessment Grandparents DayDocument5 paginiRisk Assessment Grandparents Dayapi-436147740Încă nu există evaluări
- The Role of Branding in PublicDocument16 paginiThe Role of Branding in PublicUsamah HussainÎncă nu există evaluări
- Epidemiological Tools: Fractions, Measures of Disease Frequency and Measures of AssociationDocument16 paginiEpidemiological Tools: Fractions, Measures of Disease Frequency and Measures of AssociationJerry Sifa0% (1)
- Should Minors Be Able To Purchase Birth Control Without Parental ConsentDocument4 paginiShould Minors Be Able To Purchase Birth Control Without Parental ConsentjohnÎncă nu există evaluări
- Hygiene PresentationDocument21 paginiHygiene Presentationproject_genomeÎncă nu există evaluări
- Soal Bhs Inggris 1 PerbaikanDocument7 paginiSoal Bhs Inggris 1 PerbaikanNurul LailiÎncă nu există evaluări
- Nutrients: On The Reporting of Odds Ratios and Risk RatiosDocument2 paginiNutrients: On The Reporting of Odds Ratios and Risk Ratiosfatihatus siyadaÎncă nu există evaluări
- CHE135 - Ch1 Intro To Hazard - MII - L1.1Document26 paginiCHE135 - Ch1 Intro To Hazard - MII - L1.1SyafiyatulMunawarahÎncă nu există evaluări
- Indiviual Rack: ProvidedDocument4 paginiIndiviual Rack: Providedkevin tomÎncă nu există evaluări
- Caring For Vulnerable Populations During A Pandemic: Literature ReviewDocument6 paginiCaring For Vulnerable Populations During A Pandemic: Literature ReviewMohamed AbdulqadirÎncă nu există evaluări
- SPH 596 Lecture 1 September 7 2018Document28 paginiSPH 596 Lecture 1 September 7 2018Kevin Rosen CÎncă nu există evaluări
- Imci Quiz 1Document2 paginiImci Quiz 1Neptali Cardinal100% (1)
- STD PreventionDocument12 paginiSTD Preventionapi-370125730Încă nu există evaluări
- 2019-20 Handbook CatalogDocument254 pagini2019-20 Handbook CatalogGH PractitionerÎncă nu există evaluări
- Hafiya Kezia - COVIDDocument2 paginiHafiya Kezia - COVIDHafiya KeziaÎncă nu există evaluări
- Water Sanitation and Hygiene UnderstandingDocument4 paginiWater Sanitation and Hygiene UnderstandingGreen Action Sustainable Technology GroupÎncă nu există evaluări
- FOOD SAFETY & GMP (Refresher Course) 2018Document156 paginiFOOD SAFETY & GMP (Refresher Course) 2018QA SpicemixÎncă nu există evaluări
- Part4 Evidence1 CozineDocument2 paginiPart4 Evidence1 Cozineapi-286143658Încă nu există evaluări
- Hospital Acquired Infections:: Yesterday, Today & TomorrowDocument87 paginiHospital Acquired Infections:: Yesterday, Today & TomorrowSharad BhallaÎncă nu există evaluări