Documente Academic
Documente Profesional
Documente Cultură
FOM Study Guide PREGNANCY AND MENOPAUSE
Încărcat de
yelloweverglowTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
FOM Study Guide PREGNANCY AND MENOPAUSE
Încărcat de
yelloweverglowDrepturi de autor:
Formate disponibile
PREGNANCY AND MENOPAUSE
2. Explain how and when ovulation occurs
in normal 28 day cycle in female, ovulation occurs 14 days after onset of menstruation
follicle swells rapidly -> stigma protrudes like nipple -> viscous fluid evaginate out (carries the ovum
surrounded w/ corona radiata)
surge of LH is necessary for ovulation
o 2 days before ovulation
rate of LH secretion (by AP gland) increases markedly
FSH also increases
o last few days before ovulation
FSH and LH act synergistically to cause rapid swelling of the follicle
LH convert granulosa and theca cells into progesterone secreting cells
o 1 day before ovulation
↓ estrogen secretion
Ovulation occurs in an environment of:
o rapid growth of the follicle
o ↓ estrogen secretion (after prolonged phase of excessive estrogen secretion)
o initiation of secretion of progesterone
INITIATION OF OVULATION:
o LH causes rapid secretion of follicular steroid hormones that contain progesterone
o 2 events needed for ovulation:
theca externa release proteolytic enzymes from lysosomes -> dissolution of follicular
capsular wall -> weakened wall -> further swelling of entire follicle and degeneration of
the stigma
rapid growth of new blood vessels into follicle wall and; prostaglandins are secreted into follicular tissues
o the 2 events cause plasma transudation into follicle ->follicle swelling and degeneration of stigma -> follicle rupture -> discharge of ovum
CORPUS LUTEUM
o After ovulation, secretory cells of the ovulating follicle develop into a corpus luteum
o secrete large quantities of progesterone and estrogen
o after 2 weeks, corpus luteum degenerates
↓ estrogen and progesterone
menstruation begins -> new ovarian cycle
3. Outline the major events and hormonal changes of each phase of the uterine cycle and correlate them with events of the ovarian cycle.
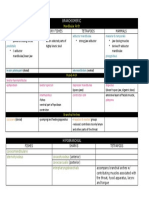
UTERINE CYCLE OVARIAN CYCLE
- menstrual cycle - describes the development and release of oocyte in the ovary and
- growth and differentiation controlled by estrogen and progesterone changes in follicles
- averages 28 days - average of 28 days
- preparation of endometrium for implantation of fertilized and shedding if
implantation has failed
[ 1st ] Proliferative Phase [ 1st ] Follicular Phase
• Aka follicular or estrogenic phase Gonadotropin releasing hormone (GnRH) from the hypothalamus stimulates
• Coincides with rapid growth of small group ovarian follicles the release of FSH and LH
Theca interna secretes estrogen Follicle stimulating hormone (FSH) from the pituitary
• Estrogen - regeneration of functional layer lost during menstruation o Stimulates the process of follicular growth of a small group of
• Cells of the basal ends of glands proliferate, migrate and form new epithelial primordial follicles each month
covering Growth of oocyte - FSH
• Spiral arteries lengthen as functional layer is reestablished primary follicle
• Endometrium is 2-3mm at the end of this phase vesicular/antral follicle
• Proliferative phase = 8 to 10 days o contains the secondary oocyte to be ovulated
o cumulus oophorus
o corona radiate
mature/ Pre- ovulatory/ Graafian follicle
o forms a bulge at ovary surface
atretic follicles – primary and antral follicles undergo atresia after dominant
follicle is ovulated
[ 2nd ] Secretory Phase (Luteal Phase) [2nd] Luteal Phase
Starts a result of progesterone secreted by corpus luteum Corpus luteum
Endometrium reaches its maximum thickness (5mm) during this phase o Formed by collapse and folding of the granulosa and thecal layers of
o Result of the accumulation of secretions and edema in the stroma the follicle’s wall
IF fertilization occurs, embryo attaches to the uterine epithelium o Formation under the influence of LH
o Endometrial thickness and secretory activity are optimal for embryonic o For extensive production of progesterone in addition to estrogens
implantation and nutrition o Granulosa lutein cells
o Progesterone inhibits strong contractions of the myometrium that Role in aromatase conversion of androstenedione into
might interfere with embryo implantation estradiol
Secretory phase = 14 days o Theca lutein cells
Previously theca interna
LH causes these cells to produce progesterone and
androstenedione
o Ovulatory LH causes corpus luteum to secrete progesterone (10 to 12
days) and estrogen
Without further LH stimulation and in the absence of
pregnancy, cells undergo apoptosis and regression of tissue
Decrease in progesterone levels: causes
menstruation
Decrease in estrogen levels: FSH release resumes
Stimulates another group of follicles to begin
new cycle
If pregnancy occurs:
o Trophoblast cells of implanted embryo produce human chorionic
gonadotropin ▪ hCG has similar activity to LH (Maintains corpus
luteum -> Maintains progesterone levels -> No menstruation)
[ 3rd ] Menstrual Phase
Caused by a decline in progesterone and estrogen levels
o Happens when fertilization does not occur and corpus luteum
degenerates
Drop in progesterone
o Causes muscle contraction in the spiral arteries = interrupts normal
blood flow
o Increased synthesis by arterial cells of prostaglandins = vasoconstriction
and local hypoxia
Hypoxic injury cause cells to release cytokines
o Increase permeability and immigration of leukocytes
o Release collagenase and matrix metalloproteinases (MMPs) that
degrade basement membranes and other ECM components
Basal layer of the endometrium is not affected
o Does not depend on progesterone-sensitive spiral arteries
Menses
o Major portion of the functional layer detach from the endometrium
and slough away
Endometrium is reduced to a thin layer ready to begin a new cycle after this
phase
Menstrual period = 3 to 4 days
4. Maternal physiologic changes and adaptation to pregnancy.
weight gain - Due to amniotic fluid, placenta and fetal membrane, Due to the action of progesterone leads to higher tidal
uterus, breasts, blood, fat accumulation volume
Metabolism o Enlarging uterus results in increased intra-abdominal pressure
o Increased metabolism due to hormonal changes and increased and elevation of diaphragm
muscle activity (because of weight bearing) o Resting ventilation increases by about 48%
o Basal metabolic rate (BMR) rises by the 4th month o More efficient exchange of gases
o The net effect of maternal fuel adaptations is to increase the Gastrointestinal changes
use of fat as fuel by the mother and conserve the glucose for o Decreased intestinal motility
the fetus action of progesterone
Cardiovascular changes Creates tendency to develop gallstones
o Increase in Cardiac Output o Constipation
Due to increase blood volume Due to compression of rectum
Also, higher levels of aldosterone and estrogen leads o Gastric reflux and heart burn
to higher fluid retention which causes the increase in Due to relaxation of Lower Esophageal Sphincter
blood volume (LES)
o Higher heart rate Changes in the skin
o Blood pressure lowers o Hyperpigmentation of nipple areolar complex, linea alba
o Higher RBC production (adaptation to hematoctrit) Due to increased MSH secretion
o Mild hypertrophy of the heart Facial melasma
o IVC compression (lower blood flow to RA) o Striae Gravidarum (Pregnancy stretch marks)
o Pelvic vein compression (backflow of blood leads to varicose Due to abdominal wall stretching Leads to pruritus
veins and ankle swelling) Kidney Function
o Heart is displaced and may lead to a larger cardiac shadow o Rate of urine formation is increased
Respiratory Adaptation Due to increased fluid intake and increased load of
o Increase in minute ventilation excretory products
o Higher respiratory rate (RR) o Renal tubules’ (re)absorptive capacity for Na, Cl and water is
o Lower arterial CO2 increased
Leads to respiratory alkalosis Due to increased production of salt and water
o Increased upper respiratory vascularization and capillary retaining hormones from the placenta and adrenal
engorgement cortex
o Relaxation of thoracic cage ligaments o Renal blood flow and glomerular filtration rate increase
Due to renal vasodilation and/or as compensation for
increased tubular reabsorption of Na and water
PREGNANCY
AMENORRHEA
For a female who has not undergone fertilization, the following occurs:
o Corpus luteum involutes
o No estrogen and progesterone that keep the endometrium
intact
o Shedding of endometrial lining; thus, menstruation occurs
For a female who has undergone fertilization, the following occurs:
o Formation of Zygote
o Implantation into endometrium as blastocyst
o Trophoblast secretes hCG (Mimics action of LH)
o Corpus luteum still secretes Estrogen and Progesterone
o prevents sloughing off of the endometrium
o No menstruation occurs
HORMONAL CHANGES DURING PREGNANCY
Human Chorionic Gonadotropin (hCG)
o Primary function: Prevents involution of the corpus luteum at the end of the monthly
female cycle, causing it to secrete larger quantities of its sex hormones
o hCG increase prevents sloughing off of the endometrium (secreted by the placenta and
the syncytial trophoblast cells)
o Increase is seen 8 to 9 days after ovulation and rises to reach a maximum at about 10 to
12 weeks of pregnancy
o Decreases back to a lower value by 16 to 20 weeks
Estrogens
o Secreted by the syncytial trophoblast cells of the placenta
o Towards the end of pregnancy, quantity increases to about 30 times the normal level
o Estrogen produced by placenta differs from that of the ovaries:
Not synthesized de novo ▪ Formed entirely from androgenic steroid compounds
o Causes enlargement of the mother’s uterus, breast ductal structure, and enlargement of the mother’s female external genitalia
Relaxes the pelvic ligaments for easier passage of the fetus
Progesterone
o During early pregnancy, secreted in moderate quantities by the corpus luteum
o Secreted in tremendous amounts in late pregnancy by the placenta
o Causes decidual cells to develop in the uterine endometrium (for nutrition of embryo)
o Decreases the contractility of the pregnant uterus (lowers risk for abortion)
o Helps develop the conceptus even before implantation occurs via increasing the secretions of the fallopian tubes and uterus (for nutrition)
o Helps estrogen prepare the mother’s breast for lactation
Human Chorionic Somatomammotropin
o Secreted by placenta during the 5th week of pregnancy (increases at this point)
o Increases progressively during the remainder of pregnancy
o Possible effects: breast development, lactation, formation of proteins similar to GH, decreased insulin sensitivity and decreased utilization of
glucose by mother
CHANGES IN REPRODUCTIVE ORGANS
Endometrium:
o hCG prevents involution of corpus luteum
o Prevents menstruation → Cause continuous endometrium growth and storage of nutrients rather than being shed in the menstruum
o Glands and blood vessels increase in size and number
o Vascular spaces fuse to become the placenta
Uterus
o Enlargement of the Uterus
o Enlargement is caused by:
Stretching and marked hypertrophy of muscle cells (production of new myocytes is limited)
Accumulation of fibrous and elastic tissue especially in the external muscle layer
Vagina
o Enlargement of the female external genitalia
o Vaginal walls change: ▪ Increase in mucosal thickness ▪ Loosening of connective tissue ▪ Smooth muscle hypertrophy
o Papillae of the vaginal epithelium undergo hypertrophy → Hobnailed appearance
o Pregnancy results in increased elastic fiber degradation and an increase in the proteins necessary for new elastic fiber synthesis → Vaginal wall
prolapse
Cervix
o This rearrangement includes the decrease in collagen and proteoglycan concentrations and increase in water content
o Uterine glands proliferate, doubling in number compared to the non-pregnant female
o Relax the pelvic ligaments of the mother → sacroiliac joints relatively limber + symphysis pubis becomes elastic → allow easier passage of the
fetus through the birth canal
MENOPAUSE
↑ FSH - No more negative feedback mechanism from the estrogen →
no
inhibition of FSH
↓ Estradiol - Follicle is no longer released → ovulation no longer occurs →
corpus luteum will no longer produce estrogen
Types of estrogen:
o E1: Estrone – predominant estrogen during menopause
o E2: Estradiol – predominant estrogen during reproductive
o age
o E3: Estriol – predominant estrogen during pregnancy
HORMONAL CHANGES AND EFFECTS ON REPRODUCTIVE ORGANS
Uterus
o Shrinks (becomes as small as the uterus during puberty due to reduced level of estrogen)
No longer enlarges in response to sexual stimulation as it once did
Sexual stimulation is still possible but takes longer – feelings of sexual excitation, orgasm, and fulfillment remain
Endometrium
o less thickening
Progesterone promotes the secretory changes in the uterine endometrium during the latter half of the monthly sexual cycle
Reduced production of progesterone (as in menopause) results to less thickening of the endometrium
Cervix
o Thinning out
Cervical glands and cells that line the endocervical canal make mucus in response to the female hormones produced during menstrual
cycle
Cessation of these hormones leads to less production of mucus by the glands which leads to thinning of the cervix
Vagina
o Dryness due to less lubrication from the decreased mucus secretion
o
SIGNS AND SYMPTOMS OF MENOPAUSE
Hot flushes
o Mechanism is still not understood
o Believed to be due to fluctuation of estrogen and progesterone which impacts the functioning of the hypothalamus (responsible for
controlling body temperature, appetite, sex hormones, and sleep)
o Not a trouble in the Philippines
Mood swings & irritability
o Sleep deprivation
o Horm
o onal imbalance
o Social factors (aging, children are away)
Vaginal dryness & itching
o Less lubrication leads to atrophy of cells and contributes to itching
o Desquamated cells lead to decreased lactic acid secretion producing an alkaline environment and reducing the protective moisture in the
vagina
Treatment is usually based on symptoms such as:
o Use of vaginal lubricants and creams
o Cool environment
o Low-dose antidepressants
o Hormonal replacement
Case: A female patient was diagnosed with PCOS and she was characterized to Describe the histological changes that happen during the proliferative and
have no ovulation and missed menses. There was also existence of secretory phases of the menstrual cycle
endometrial thickening. What is the most probable sex hormone (Estrogen or ANSWER: • Proliferative
Progesterone) absent from this patient? Begins during the first day of menstruation During this phase, the
ANSWER: endometrium is lined with simple
• A person with PCOS has high amounts of androgens Has male columnar cells Regeneration of functional layer lost during menstruation
characteristics (facial and body hair) Harder to get pregnant is acted upon by estrogen Stromal and epithelial cell proliferation
• Presence of aromatase converts androgens to estrogen ▪ Re-epithelialized after 4-7 days Endometrium thickens after a week and a
• Increase in estrogen prematurely inhibits anterior pituitary no secretion half
of FSH and LH ▪ Due to the increase in number of the stromal cells and the growth of the
• Lack of FSH and LH leads to no maturation of the follicles No ovulation endometrial glands and new blood vessels
occurs ▪ After this phase, the endometrium is 2-3 mm thick
• TH Note: Follicles will still grow and be filled up with fluid but when ovulation Spiral arteries lengthen as functional layer is
do not occur, the follicles simply remain as cysts. Multiple small fluid-filled reestablished
ovarian cysts and excess androgens present PCOS or POLYCYSTIC OVARIAN Endometrial glands secrete stringy mucus which
Syndrome guide the sperm towards the uterus • Secretory Starts when the
• Since no ovulation occurs, no corpus luteum is formed Corpus luteum is corpus luteum secretes progesterone estrogen Estrogen causes
responsible for the secretion of progesterone Leads to no progesterone slight additional cellular proliferation in the endometrium
formation Progesterone causes marked swelling and secretory development
• Endometrial thickening is still present since estrogen is the hormone of the endometrium Blood supply to the endometrium further
responsible for cell proliferation in the endometrium increases in proportion to the developing secretory activity
• Menstruation requires an increase in progesterone followed by its Progesterone stimulates epithelial cells of the uterine glands to
decrease No progesterone to begin with -> no menstruation secrete and accumulate glycogen ▪ Causes them to become
coiled Endometrium reaches 5 mm in thickness due to accumulation
of secretions and edema of the stroma
S-ar putea să vă placă și
- Hypoxia TypesDocument3 paginiHypoxia TypesyelloweverglowÎncă nu există evaluări
- Fom 4.1Document8 paginiFom 4.1yelloweverglowÎncă nu există evaluări
- Hepatobiliary Obstruction and Jaundice CausesDocument6 paginiHepatobiliary Obstruction and Jaundice CausesyelloweverglowÎncă nu există evaluări
- StickersDocument1 paginăStickersyelloweverglowÎncă nu există evaluări
- The Goldman Equation Explains Neuron Membrane PotentialDocument7 paginiThe Goldman Equation Explains Neuron Membrane PotentialyelloweverglowÎncă nu există evaluări
- Boys LyricsDocument2 paginiBoys LyricsyelloweverglowÎncă nu există evaluări
- Physio Formulas (Cardiovascualr)Document1 paginăPhysio Formulas (Cardiovascualr)yelloweverglowÎncă nu există evaluări
- CH 7 OutlineDocument6 paginiCH 7 OutlineyelloweverglowÎncă nu există evaluări
- Tests Chem LabDocument2 paginiTests Chem LabyelloweverglowÎncă nu există evaluări
- Set Me As A SealDocument4 paginiSet Me As A SealyelloweverglowÎncă nu există evaluări
- Carnavalito QuebradenoDocument2 paginiCarnavalito QuebradenoyelloweverglowÎncă nu există evaluări
- Theory Exp 7Document2 paginiTheory Exp 7yelloweverglowÎncă nu există evaluări
- CHAP 5 Connective TissueDocument15 paginiCHAP 5 Connective TissueyelloweverglowÎncă nu există evaluări
- Bacteria Chosen For BioinformaticsDocument2 paginiBacteria Chosen For BioinformaticsyelloweverglowÎncă nu există evaluări
- Bioinformatics CMB Lab IntroductionDocument7 paginiBioinformatics CMB Lab IntroductionyelloweverglowÎncă nu există evaluări
- TitcurveDocument1 paginăTitcurveyelloweverglowÎncă nu există evaluări
- Circu Table LecDocument3 paginiCircu Table LecyelloweverglowÎncă nu există evaluări
- UnfinishedDocument1 paginăUnfinishedyelloweverglowÎncă nu există evaluări
- Early DevelopmentDocument2 paginiEarly DevelopmentyelloweverglowÎncă nu există evaluări
- Endo 2Document2 paginiEndo 2yelloweverglowÎncă nu există evaluări
- Chordates Specimens (Comparative Anatomy Lab)Document46 paginiChordates Specimens (Comparative Anatomy Lab)yelloweverglowÎncă nu există evaluări
- Hong Kong Trip Proposal: MNL To HKG HKG To MNLDocument1 paginăHong Kong Trip Proposal: MNL To HKG HKG To MNLyelloweverglowÎncă nu există evaluări
- Muscular Table - KentDocument3 paginiMuscular Table - KentyelloweverglowÎncă nu există evaluări
- Endo 2Document2 paginiEndo 2yelloweverglowÎncă nu există evaluări
- Early DevelopmentDocument2 paginiEarly DevelopmentyelloweverglowÎncă nu există evaluări
- Cranial Muscles KardongDocument1 paginăCranial Muscles KardongyelloweverglowÎncă nu există evaluări
- Chapter 6-Adipose TissueDocument9 paginiChapter 6-Adipose TissueyelloweverglowÎncă nu există evaluări
- Pigeon DRU LabelDocument2 paginiPigeon DRU LabelyelloweverglowÎncă nu există evaluări
- Lit Quiz One TableDocument1 paginăLit Quiz One TableyelloweverglowÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Encouraging Human Croc & CoexistenceDocument52 paginiEncouraging Human Croc & CoexistenceAdmin Bataraza Fire Station PalawanÎncă nu există evaluări
- The Mechanism Isorhythmic: of Synchronization A-VDocument11 paginiThe Mechanism Isorhythmic: of Synchronization A-VSheila AdiwinataÎncă nu există evaluări
- Soal I KUNCIDocument4 paginiSoal I KUNCIAyie Sharma100% (1)
- Centrifugal PumpDocument36 paginiCentrifugal PumpshubhamÎncă nu există evaluări
- Corporate Agent License DetailsDocument980 paginiCorporate Agent License DetailsskpakaleÎncă nu există evaluări
- Perkins 1103,1104 Industrial Engine Opp and Main ManualDocument92 paginiPerkins 1103,1104 Industrial Engine Opp and Main ManualBiruk YifruÎncă nu există evaluări
- The Optic NerveDocument7 paginiThe Optic NerveEdwin DarmawanÎncă nu există evaluări
- The Historical Background To The Culture of Violence in Trinidad and Tobago - by Bridget Brereton (Issue 4 - 2010) in Journal of Caribbean Perspectives On Gender and FeminismDocument16 paginiThe Historical Background To The Culture of Violence in Trinidad and Tobago - by Bridget Brereton (Issue 4 - 2010) in Journal of Caribbean Perspectives On Gender and FeminismAbuAbdur-RazzaqAl-MisriÎncă nu există evaluări
- Material Safety Data Sheet: Section 1 - Chemical Product and Company IdentificationDocument6 paginiMaterial Safety Data Sheet: Section 1 - Chemical Product and Company IdentificationRahasia Tahu RahasiaÎncă nu există evaluări
- Bianca TimelineDocument4 paginiBianca TimelineNix RobertsÎncă nu există evaluări
- SMQ 3043 Linear ProgrammingDocument10 paginiSMQ 3043 Linear ProgrammingRAMLI BIN ABDUL NAJIDÎncă nu există evaluări
- Genetics and Probability Practice ProblemsDocument2 paginiGenetics and Probability Practice ProblemsMarcos Valdez Jr.0% (1)
- Physiological Understanding of Medovaha Srotas in The Current PerspectiveDocument3 paginiPhysiological Understanding of Medovaha Srotas in The Current PerspectiveAdvanced Research PublicationsÎncă nu există evaluări
- Food 8 - Part 2Document7 paginiFood 8 - Part 2Mónica MaiaÎncă nu există evaluări
- ICP5000DV BROCHURE SEPTEMBER 2020 Lo Resolution-2Document4 paginiICP5000DV BROCHURE SEPTEMBER 2020 Lo Resolution-2OriÎncă nu există evaluări
- Lits Menu SCBD 20 July 2022 Small 1Document39 paginiLits Menu SCBD 20 July 2022 Small 1Priambodo SulistyoÎncă nu există evaluări
- Personal Development: Quarter 1 - Module 1: Knowing and Understanding Oneself During Middle and Late AdolescenceDocument9 paginiPersonal Development: Quarter 1 - Module 1: Knowing and Understanding Oneself During Middle and Late AdolescenceALLAN SANTOSÎncă nu există evaluări
- Souldrama: A New Model For Putting The Twelve Steps Into ActionDocument3 paginiSouldrama: A New Model For Putting The Twelve Steps Into ActionedyyantoÎncă nu există evaluări
- (Steam Boiler Turnkey Installation Project 1.5TPH) (PO Order Number PTTPO09001)Document3 pagini(Steam Boiler Turnkey Installation Project 1.5TPH) (PO Order Number PTTPO09001)mohd sakirin roslanÎncă nu există evaluări
- Indra: Total SheetDocument633 paginiIndra: Total SheetPHAM PHI HUNGÎncă nu există evaluări
- Catalogo RWGDocument8 paginiCatalogo RWGFolpoÎncă nu există evaluări
- Akapulko ResearchDocument10 paginiAkapulko Researchmary_ramaÎncă nu există evaluări
- Community Directory (May 2023)Document32 paginiCommunity Directory (May 2023)The Livingston County NewsÎncă nu există evaluări
- CHCDIV001 Work With Diverse People: Student Questions Case Study/ Scenarios Observations Oral Questions OtherDocument14 paginiCHCDIV001 Work With Diverse People: Student Questions Case Study/ Scenarios Observations Oral Questions OtherHardeep kaur0% (1)
- CSHQ - Doc Somn Copii Si Prescolari Si ScolariDocument2 paginiCSHQ - Doc Somn Copii Si Prescolari Si ScolariMadalina PotoroacaÎncă nu există evaluări
- Rosen 48V 200AH LiFePo4 Battery-PowerwallDocument5 paginiRosen 48V 200AH LiFePo4 Battery-Powerwallgihan_maÎncă nu există evaluări
- Life Skills Curriculum - Secondary 1Document546 paginiLife Skills Curriculum - Secondary 1Jeff Zacker100% (2)
- Bac Blanc All Units - Docx Versión 1Document13 paginiBac Blanc All Units - Docx Versión 1markaz talebÎncă nu există evaluări
- TPP eDocument1 paginăTPP eOliva R. SeguraÎncă nu există evaluări
- Duterte's Drug War in the Philippines Leads to Extrajudicial KillingsDocument11 paginiDuterte's Drug War in the Philippines Leads to Extrajudicial KillingsJOEL D. BATERISNAÎncă nu există evaluări