Documente Academic
Documente Profesional
Documente Cultură
Acl Immature Patient
Încărcat de
ariearifinDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Acl Immature Patient
Încărcat de
ariearifinDrepturi de autor:
Formate disponibile
Review Article
Anterior Cruciate Ligament
Injuries in the Skeletally Immature
Athlete: Diagnosis and
Management
Abstract
Jeremy S. Frank, MD Intrasubstance anterior cruciate ligament (ACL) injuries in children
Peter L. Gambacorta, DO and adolescents were once considered rare occurrences, with tibial
eminence avulsion fractures generally regarded as the pediatric
ACL injury equivalent. However, with increased single-sport focus,
less free play, and year-round training at younger ages,
intrasubstance ACL injuries in children and adolescents are being
diagnosed with increased frequency. As in the adult, a knee devoid
of ligamentous stability predisposes the pediatric patient to
meniscal and chondral injuries and early degenerative changes.
Management of ACL injuries in skeletally immature patients
includes physeal-sparing, partial transphyseal, and complete
transphyseal ACL reconstruction. Complications include iatrogenic
growth disturbance resulting from physeal violation.
I n the past 20 years, sports injuries
in pediatric and adolescent athletes
have dramatically increased.1 Ap-
the pediatric equivalent of the ACL tear
in adults. The incidence of midsub-
stance tears in pediatric patients has
proximately 38 million young ath- grown considerably, especially in sports
From the Division of Pediatric letes participate in organized sports that involve cutting, pivoting, and col-
Orthopaedics and Spinal annually in the United States.2 Of lision.
Deformities, Joe DiMaggio
Children’s Hospital, Hollywood, FL these, nearly 2 million high school In a recent study of high school
(Dr. Frank) and the Division of students and almost twice as many athletes, female soccer players were
Sports Medicine, Women and athletes aged <14 years are treated found to have the highest rate of
Children’s Hospital of Buffalo, East for a sports-related injury each year. ACL injury, with an incidence of
Amherst, NY (Dr. Gambacorta).
This new epidemic of sports-related 14.08 per 100,000 exposures; male
Neither of the following authors nor injuries can be partially attributed to football players had the second high-
any immediate family member has
received anything of value from or
the dramatic surge in the number of est rate, with 13.87 injuries per
has stock or stock options held in a participants since the passage of Title 100,000 exposures.3 Stanitski et al4
commercial company or institution IX, along with increased emphasis noted that 47% of preadolescent and
related directly or indirectly to the on year-round competition, single- 65% of adolescent athletes present-
subject of this article: Dr. Frank and
Dr. Gambacorta.
sport concentration, and more in- ing with an acute hemarthrosis of the
tense training. knee were ultimately diagnosed with
J Am Acad Orthop Surg 2013;21:
Injuries to the anterior cruciate liga- acute ACL rupture.
78-87
ment (ACL) were once thought to be a Management of ACL injuries in
http://dx.doi.org/10.5435/ rare phenomenon in pediatric athletes. the skeletally immature athlete is
JAAOS-21-02-78
Midsubstance tears were believed to challenging. In adults, the traditional
Copyright 2013 by the American occur only in adults, and the tibial em- arthroscopically assisted placement
Academy of Orthopaedic Surgeons.
inence fracture was considered to be of osseous tunnels for ACL recon-
78 Journal of the American Academy of Orthopaedic Surgeons
Jeremy S. Frank, MD, and Peter L. Gambacorta, DO
Figure 1 contact versus noncontact), and re- ducing the sense of instability; how-
sulting symptoms are critical pieces ever, it may not be well tolerated fol-
of information. For the young child, lowing acute injury.
most of these questions are directed
toward the parent or guardian, but it
is important to engage the child, as Imaging
well, to develop rapport. Any history
Imaging of the injured knee is essen-
of swelling or effusion in the knee re-
tial in devising a treatment plan. Ini-
quires further investigation. The pre-
tial AP, lateral, notch, and sunrise ra-
senting signs and symptoms of an
diographs of the injured knee are
ACL tear in pediatric patients are
helpful in assessing osseous struc-
similar to those experienced by
tures and skeletal maturity. MRI is
adults. The athlete may experience a
indicated to evaluate for partial ver-
pop at the time of injury. Nearly half
sus complete ACL injuries, define as-
of all ACL injuries are associated
sociated ligamentous pathology, and
with a hemarthrosis, which ensues
assess for suspected meniscal de-
between 6 and 12 hours after the in-
rangement. MRI is not absolutely
jury.3 Up to 70% of these injuries oc-
indicated for the patient with a de-
Sagittal T2-weighted magnetic cur through a noncontact mechan-
resonance image of a Tanner stage finitively positive and asymmetric
ism, and instability may recur if the
2 patient with a complete anterior Lachman and pivot shift examina-
young athlete continues to play on a
cruciate ligament rupture (arrow). tion, no additional ligamentous lax-
ruptured ACL.5
ity, and full knee ROM. With proper
sequencing, MRI has 95% sensitivity
struction is highly effective in pre-
for detecting ACL tears in pediatric
venting instability. This technique is Physical Examination patients6 (Figure 1).
usually avoided in younger patients
with significant growth remaining Proper physical evaluation is para-
because drilling across the growth mount in diagnosing pediatric knee Maturity Assessment
plate carries a potential risk of injuries. Performance of the physical
growth disturbance and angular de- examination can be a challenge be- Surgical management is guided by
formity. Historically, the approach cause pediatric patients are often the patient’s skeletal, physiologic,
for managing ACL tear in a young anxious and guarded. Examination and chronologic maturity. Chrono-
patient consisted of activity modifi- of the uninjured knee can be helpful logic age serves as a rough estimate;
cation and bracing until the onset of for demonstrating clinical maneuvers the skeletal and physiologic age may
skeletally maturity, at which point a and determining normal joint laxity. be quite different. The Tanner stag-
traditional transphyseal ACL recon- Visualization and gentle palpation ing system is best utilized to classify
struction could safely be performed. are used to detect any underlying ef- a patient’s physiologic maturity (Ta-
However, nonsurgical management fusion. Palpatory evaluation of the ble 1). Assessment of secondary sex
commonly leads to recurrent insta- knee should include the distal femo- characteristics and questions con-
bility, resulting in secondary injuries ral and proximal tibial physes, me- cerning menarche are useful in deter-
to the surrounding articular cartilage dial and lateral joint lines, patella, mining physiologic age. Skeletal ma-
and menisci. Several physeal-sparing patellar retinaculum, and tibial tu- turity can be determined by a variety
ACL reconstruction techniques have bercle apophysis. When normal of methods. Our preference is to ob-
been developed to stabilize the knee tain a PA radiograph of the left hand
range of motion (ROM) is compro-
and minimize the risk of physeal dis-
mised, a concomitant injury to the and wrist for comparison with the
ruption.
meniscus and/or cartilage should be Greulich and Pyle atlas.
considered. The collateral ligaments Child athletes who are being con-
History should be evaluated at zero degrees sidered for ACL reconstruction can
and 30°. A proper Lachman test is be classified as either prepubescent
A focused history is required before critical to assess anterior tibial trans- or pubescent. The prepubescent pa-
proceeding to physical examination. lation and end point firmness. The tient has physiologic findings consis-
Chronicity, mechanism of injury (ie, pivot shift test is beneficial in repro- tent with Tanner stages 1 and 2 and
February 2013, Vol 21, No 2 79
Anterior Cruciate Ligament Injuries in the Skeletally Immature Athlete: Diagnosis and Management
Table 1
Tanner Stages of Physiologic Maturity
Stage 1 Stage 2 Stage 3 Stage 4 Stage 5
Boys
Growth 5–6 cm/y 5–6 cm/y 7–8 cm/y 10 cm/y None
Testes, penis Testes: <4 mL or Testes: 4 mL or 2.5– Testes: 12 mL or 3.6 cm; Testes: 4.1–4.5 cm; Testes fully mature in
<2.5 cm 3.5 cm; penis usu- enlargement, lengthen- increased size and shape and size
ally not yet en- ing of penis breadth of penis
larged
Pubic hair None Sparse, at base of Pubic hair over pubis; Adult-like, but over a Fully mature in type
penis darker, coarser, and smaller area and quantity, extend-
more curled ing to the thighs
Girls
Growth 5–6 cm/y 7–8 cm/y 8 cm/y 7 cm/y None
Breasts No development Buds Elevation and areolar Areolae and papillae Mature
enlargement form secondary
mound
Pubic hair None Sparse, on labia; On mons pubis; darker, Adult-like, but over a Fully mature in type
slightly pigmented coarser, and more smaller area and quantity, extend-
curled ing to the thighs
a bone age of <12 years in boys and negative initially even when 75% of plete ACL injuries has been less suc-
<11 years in girls. The pubescent pa- the ligament is torn.8 MRI in the cessful. The high noncompliance rate
tient has physiologic findings consis- oblique coronal plane is useful in is associated with secondary damage
tent with Tanner stages 3 and 4 and quantifying the percentage of intact of the menisci and/or articular carti-
a bone age of 13 to 16 years in boys fibers. lage, and a large percentage of pa-
and 12 to 14 years in girls. To date, Kocher et al7 have per- tients eventually require surgical
formed the only study on partial reconstruction.9,10 In a recent system-
ACL tears in the adolescent patient. atic literature review, Vavken and
Nonsurgical Management
The study included 45 patients aged Murray9 compared 47 studies that
Historically, nonsurgical treatment op- <18 years. The diagnosis was made reported the clinical outcomes of sur-
tions for skeletally immature patients using physical examination, MRI, gical and nonsurgical management
with ACL tears consisted of activity and arthroscopic evidence consistent of skeletally immature patients with
modification, functional bracing, and with partial tear of the ACL. At a complete ACL tears (minimum
physical rehabilitation. The rationale minimum 2-year follow-up, 31% of follow-up, 6 months). The authors
for this approach was to allow the pa- patients underwent subsequent ACL concluded that in the skeletally im-
tient to mature skeletally before per- reconstruction. Risk factors associ- mature patient with a complete ACL
forming transphyseal ACL reconstruc- ated with failed nonsurgical manage- rupture, surgical intervention pro-
tion, thereby minimizing the risk of ment included tears involving >50% duces superior clinical outcomes
physeal violation and potential growth of the midsubstance ligament width, with regard to future stability and
deformity. This nonsurgical approach tears predominantly involving the secondary injury prevention. More-
is best used in the highly compliant, posterolateral bundle, a mildly posi- over, the specific procedure chosen
low-demand patient who has no addi- tive pivot shift test, and older chron- for surgical stabilization appears to
tional intra-articular pathologies or ologic and skeletal age. The authors have less clinical impact than does
who has a partial ACL tear. Partial of that study concluded that partial the selection of surgical treatment in
tears have been found to occur in 61% ACL tears in children and adoles- itself. In a cohort study, Lawrence
of adolescents with ACL injuries.7 cents aged ≤14 years with near nor- et al10 found that delaying manage-
Diagnosis of a partial tear based on mal Lachman and pivot shift tests ment of a complete ACL injury with
physical examination alone is diffi- may be managed nonsurgically. subjective knee instability for >12
cult. Instability maneuvers (eg, Lach- Conservative management of skele- weeks correlated with a significant
man test, pivot shift test) may be tally immature patients with com- increase in the amount of irreparable
80 Journal of the American Academy of Orthopaedic Surgeons
Jeremy S. Frank, MD, and Peter L. Gambacorta, DO
medial meniscal tears and lateral veyed members of the Herodicus So- produces a zone of physeal injury
compartment chondral injuries. ciety regarding growth disturbance that appears to increase the risk of
after skeletally immature ACL recon- abnormal growth in the distal femo-
struction and noted 15 additional ral physis postoperatively.
Surgical Management cases of growth disturbance. Those Yoo et al21 reviewed the postopera-
authors concluded that associated tive magnetic resonance images of 43
Historical Review risk factors for growth disturbance skeletally immature patients who un-
Traditional surgical techniques for included fixation hardware across derwent transphyseal ACL recon-
adult ACL reconstruction include the the physis, large tunnels (≥12 mm), struction (mean age, 14.8 years;
creation of transphyseal tunnels fol- lateral extra-articular tenodesis, dis- range, 12.4 to 16.5 years). The aver-
lowed by graft tensioning and fixa- section in proximity to the perichon-
age bone tunnel–to–growth plate
tion. In the skeletally immature pa- drial ring of LaCroix, and suturing
cross-sectional area ratio was <3%.
tient, conventional tunnel placement near the tibial tubercle.
Five patients developed MRI-
and graft tensioning risks iatrogenic More recent clinical studies have
documented focal physeal disruption
growth disturbance caused by phys- examined the use of MRI to charac-
without a perceived clinical growth
eal violation. Multiple animal11-13 terize physeal injury after transphys-
disturbance (11.6%). The authors of
and human clinical series14-16 have eal ACL reconstruction in skeletally
the study noted that, although trans-
documented such growth distur- immature patients. Kercher et al19 re-
physeal reconstruction of the ACL
bances. More recent animal studies viewed 31 patients aged 10 to 15 years
may not be a benign procedure in
have investigated the effect of small with MRI and custom three-dimen-
younger children with substantial
tunnels and soft-tissue grafts on sional modeling following transphyseal
growth potential, they were able to
physeal bar formation and subse- ACL reconstruction. The authors con-
safely perform this procedure in ado-
quent growth arrest.17-20 cluded that, with 8-mm tunnels, <3%
lescents with limited growth remain-
Stadelmaier et al17 compared phys- of the cross-sectional area of the physis
ing in this series.
eal defects with and without the use was violated. Moreover, using a custom
of soft-tissue interposition grafts in computerized model of the physis, they
Surgical Techniques
eight skeletally immature dogs. The documented that tunnel diameter was
authors concluded that the presence potentially more offensive to the physis The great majority of ACL tears in
of soft-tissue grafts in the transphys- than was drill angle. skeletally immature athletes occur in
eal tunnels prevented physeal bar Anatomic positioning of the femo- adolescents with limited growth re-
formation. These results have been ral tunnel with the use of single- or maining. Treatment traditionally in-
verified in subsequent animal stud- double-bundle techniques is becom- cludes transphyseal ACL reconstruc-
ies, which also noted that transphys- ing the standard in adult ACL recon- tion with minimal risk of growth
eal tunnels that occupy <5% of the struction. The anatomic placement disturbance.9 Surgical management
physeal cross-sectional area do not of the femoral tunnel is drilled at a of these injuries in the preadolescent
appear to cause growth distur- more oblique angle that, if per- patient is the subject of much debate,
bance.18 However, when >7% to 9% formed in a skeletally immature pa- given the substantial growth remain-
of the cross-sectional area of the tient, places the lateral physis at an ing, the poor prognosis of nonsurgi-
physis is violated, growth distur- increased risk of injury. Shea et al20 cal management, and the conse-
bance is possible even in the presence used a computer-aided three-dimen- quences of potential growth arrest.
of a soft-tissue graft.18 sional model to incorporate the drill-
Clinical reports of growth distur- ing of an anatomic double-bundle Graft Selection
bance are rare. Lipscomb and Ander- ACL femoral tunnel in 10 pediatric There has been considerable contro-
son14 reported one case of growth knees using a variety of drill-hole di- versy regarding the use of autograft
disturbance following transphyseal ameters. They demonstrated that, by versus allograft tissue in ACL recon-
hamstring ACL reconstruction out of using this technique, the average struction. In a recent study, the Mul-
a total of 24 patients aged 12 to 15 physeal volume removed—as a per- ticenter Orthopaedic Outcomes Net-
years. Koman and Sanders15 published centage of the total physeal vol- work patient database was analyzed
a case report on one 14-year-old boy ume—was between 3.7% and 6.5%. to evaluate graft choice and the risks
who experienced growth disturbance The authors concluded that ana- associated with failure and graft rup-
following transphyseal hamstring ACL tomic double-bundle drill-hole place- ture.22 Patients between ages 10 and
reconstruction. Kocher et al16 sur- ment during ACL reconstruction 19 years were found to have the
February 2013, Vol 21, No 2 81
Anterior Cruciate Ligament Injuries in the Skeletally Immature Athlete: Diagnosis and Management
Figure 2 with the use of a bioactive and bio- 1976.30 Although it was initially
compatible scaffold in the form of a thought to be a temporizing proce-
clot that could be placed in the dure until adult-type reconstruction
wound site to enhance cellular prolif- could be performed after skeletal
eration and biosynthesis at the torn maturity, the data of Kocher et al30
ACL edges.27 Human clinical studies demonstrated a low revision rate
are necessary prior to implementing (4.5%) and clinical laxity rate as
widespread clinical applications. well as a high rate of functional sta-
A variety of physeal-sparing tech- bility and return to prior levels of
niques has been reported. In 2003, sport (Figures 3 and 4).
Guzzanti et al28 reported the results
Three distinct physeal-sparing
of a new technique described to
techniques have been described, all
manage five Tanner stage 1 ACL
with excellent clinical results and no
tears (mean chronologic age, 11.15
reported evidence of growth distur-
years; mean bone age, 10.9 years). In
bance. Kennedy et al31 performed a
this technique, the hamstring ten-
biomechanical evaluation of each
dons were kept intact at their distal
attachment, passed through a trans- technique to determine which most
epiphyseal tibial tunnel, looped over closely restored native knee kinemat-
a staple at the femoral ACL origin, ics. In a controlled laboratory set-
Illustration of the physeal-sparing ting, six cadaver knees were sub-
all-intraepiphyseal anterior cruciate brought back through the tibial tun-
ligament reconstruction as nel, and sutured onto themselves. jected to static AP, varus, and
described by Anderson.29 The authors reported no functional internal rotation forces at zero de-
instability, 1.8 mm of graft laxity, grees, 15°, 30°, 45°, 60°, and 90° of
and no cases of growth disturbance. knee flexion. Displacement and rota-
highest percentage of graft failures Anderson29 described an all-intra- tion of the tibia with respect to the
regardless of graft type. Moreover, epiphyseal technique in patients with femur were measured in the intact
the odds of graft rupture were four a mean age of 13.3 years, in which knee after ACL disruption and after
times higher with allograft recon- autograft hamstring tendon was ACL reconstruction using all-
struction than with autograft recon- passed through the distal femoral epiphyseal, transtibial over-the-top,
struction. epiphysis and fixed with an En- and iliotibial band physeal-sparing
doButton (Smith & Nephew) over techniques. The authors concluded
Physeal-sparing Techniques the lateral femoral condyle. The re- that, although all physeal-sparing re-
As previously noted, current evi- maining portion of the graft was construction techniques restored
dence suggests that surgical stabiliza- then passed through an all- some stability to the knee, the iliotib-
tion is the preferred management for epiphyseal tibial tunnel and fixed ial band reconstruction best restored
ACL rupture in skeletally immature with a post distal to the proximal AP stability and rotation control;
patients, with physeal-sparing tech- tibial physis. The author reported no however, it appeared to slightly over-
niques used in preadolescent patients functional instability, no evidence of constrain the knee to rotational
and transphyseal techniques used in growth disturbance or limb-length forces at some flexion angles.
adolescent patients.9 Both techniques discrepancy, and 1.5 mm of clinical
carry a beneficial safety profile and laxity at 2- to 8-year follow-up (Fig- Partial Transphyseal
minimal risk of growth disturbance. ure 2). Finally, Kocher et al30 de- Technique
Poor results have been reported fol- scribed a physeal-sparing combined The partial transphyseal technique is
lowing early extra-articular reconstruc- intra- and extra-articular reconstruc- a hybrid of physeal-sparing recon-
tion in preadolescent patients.23-26 tion technique in 44 prepubescent struction and traditional transphys-
Similar reports of ACL repair during patients using autogenous iliotibial eal procedures performed in adults.
that time noted considerable clinical band graft (mean chronologic age, Traditionally, hamstring or bone–pa-
laxity and functional instability.24 10.3 years). This procedure is a mod- tellar tendon–bone grafts are used.
More recent studies investigating ification of the combined intra- and Either the distal femoral or the prox-
ACL repair in large animal models extra-articular reconstruction de- imal tibial physis is left undisturbed,
have indicated promising results scribed by MacIntosh and Darby in thereby minimizing the risk of
82 Journal of the American Academy of Orthopaedic Surgeons
Jeremy S. Frank, MD, and Peter L. Gambacorta, DO
Figure 3
A, Intraoperative photograph demonstrating harvest of the iliotibial band with proximal detachment. The distal insertion
onto the Gerdy tubercle is preserved. B, Intraoperative photograph after iliotibial band harvest and whipstitch suture
placement into the proximal portion. The distal attachment to the Gerdy tubercle is intact.
growth arrest. Smaller bone tunnels oral side. At a follow-up of 58 formed on adolescents with little to
(6 to 8 mm) and more vertical tun- months, 38% of patients had >3 mm no growth remaining. Some authors
nels are used to limit to <5% the of clinical laxity, and 13% reported advocate its use in even younger,
overall cross-sectional area of physis poor results. No clinically significant more skeletally immature patients.34
that is interrupted. limb-length discrepancies were Earlier work by Lipscomb and An-
Lipscomb and Anderson14 detailed noted. derson14 and Matava and Siegel35
their experience with partial trans- Lo et al33 described five skeletally touted the success of complete trans-
physeal reconstruction techniques immature patients (mean age, 12.9 physeal ACL reconstruction using
using transtibial physeal drilling only years; range, 8 to 14 years) who un- autograft hamstring tendons. Lip-
and autogenous semitendinosus and derwent partial transphyseal recon- scomb and Anderson14 reported one
gracilis tendons in 24 skeletally im- case of limb-length discrepancy,
struction using transtibial physeal
mature patients (mean age, 13 years; which measured 2 cm. More re-
drilling only and soft-tissue au-
range, 11 to 15 years). At an average cently, other authors have reported
tografts. At a mean 7.4-year follow-
35-month follow-up, 20 of 24 pa- success with complete transphyseal
up, no patient had >3 mm of clinical
tients had returned to similar activity reconstruction using autograft mate-
laxity, one patient reported a poor
and sporting levels. Clinical laxity of rial. McCarroll et al36 reported 92%
result, and no evidence of limb-
1.8 mm was noted, and one patient return to sport with no growth dis-
suffered a 2-cm limb-length discrep- length discrepancy was noted. turbances in 60 patients treated with
ancy. autograft bone–patellar tendon–bone
Andrews et al32 reported on eight Complete Transphyseal reconstruction. Aronowitz et al37 re-
patients with open physes who un- Reconstruction ported similar postoperative out-
derwent partial transphyseal ACL re- Complete transphyseal reconstruc- comes in 19 patients aged 11 to 15
construction using either fascia lata tion strongly resembles adult-type years who were treated with Achilles
or Achilles allograft (mean age, 13.5 ACL reconstruction, with some dif- allograft.
years; range, 10 to 15 years). Tibial ferences, including smaller, more ver- In 2007, Kocher et al38 reported on
tunnels were drilled through the tical tunnels; no hardware or bone their results of 61 knees in 59 skele-
proximal tibial physis, and the graft blocks at the level of the closing tally immature pubescent adolescents
material was secured in the over-the- physis; and metaphyseal fixation. (Tanner stage 3) (mean chronologic
top position and affixed on the fem- This procedure is typically per- age, 14.7 years) who were managed
February 2013, Vol 21, No 2 83
Anterior Cruciate Ligament Injuries in the Skeletally Immature Athlete: Diagnosis and Management
Figure 4 noted, and there were no growth ab-
normalities. Liddle et al40 noted simi-
lar results using a similar technique
in 17 patients with a mean age of
12.1 years (range, 9.5 to 14 years).
In this study, one patient had 5° val-
gus deformity compared with the
contralateral limb at a mean 44-
month follow-up.
Postoperative
Management
Proper rehabilitation after ACL re-
construction in the skeletally imma-
ture patient is paramount to ensure
an excellent outcome and a success-
ful and timely return to sports. Child
and adolescent athletes can pose a
challenge to traditional physical ther-
apists who specialize in working
with adult patients. Thus, it is impor-
tant to work with a therapist who
has experience with young patients
and who can make therapy sessions
both engaging and beneficial. Activ-
ity restrictions and compliance with
Illustration of physeal-sparing combined extra- and intra-articular anterior graduated activity levels are critical
cruciate ligament reconstruction using autogenous iliotibial band. A, The to successful outcomes. Compliance
iliotibial band is harvested free proximally and left attached distally to the can be problematic in this age group,
Gerdy tubercle. B, The graft is brought through the knee in the over-the-top
position. C, The graft is brought through the notch and under the
and patients must be carefully moni-
intermeniscal ligament anteriorly. D, The final intra- and extra-articular tored at school and home by teach-
reconstruction construct after the graft is sutured to the lateral femoral ers, parents, and caretakers.
condyle and proximal tibia.
Wright and Fetzer41 published a
systematic review of 12 randomized
with a transphyseal reconstruction immature pubescent patient, with a controlled trials on bracing after
technique involving autogenous qua- low revision rate and minimal risk of ACL reconstruction (predominantly
drupled hamstrings tendon and growth disturbance (Figure 5). in adults) and reported that there
metaphyseal fixation. Two patients Two recent studies tout the success was no conclusive evidence that use
(3%) underwent revision ACL recon- of complete transphyseal ACL recon- of a brace had any effect on pain,
struction because of late graft failure. struction. Cohen et al39 performed ROM, graft stability, or protection
No cases of angular deformities were complete transphyseal ACL recon- from subsequent injury. However,
noted radiographically, and no limb- structions on 26 skeletally immature these authors strongly encouraged
length discrepancy was noted clini- patients with autogenous hamstring bracing following ACL reconstruc-
cally. The authors concluded that tendons using metaphyseal fixation tion in children and adolescents,
transphyseal reconstruction of the away from both the distal femoral whose risk taking and behavior are
ACL with use of autogenous quadru- and proximal tibial physis (mean markedly more haphazard than that
pled hamstring tendons and meta- age, 13.3 years; range, 11 to 15 of adult patients. The duration and
physeal fixation provides excellent years). At a mean follow-up of 45 type of bracing method used is at the
functional outcome in the skeletally months, good clinical outcomes were surgeon’s discretion because there
84 Journal of the American Academy of Orthopaedic Surgeons
Jeremy S. Frank, MD, and Peter L. Gambacorta, DO
Figure 5 are no true evidence-based guide-
lines.
Authors’ Recommended
Management
A recent systematic review clearly
demonstrated the benefit and safety
profile of ACL reconstruction in the
skeletally immature patient.9 Our
current treatment algorithm is predi-
cated on the patient’s skeletal, chron-
ologic, and physiologic age, as well
as on the extent of the ACL tear
(Figure 6).
Patients with partial tears involv-
ing <50% of the entire ACL diame-
ter are treated nonsurgically with ac-
tivity modification, physical therapy,
and bracing. The patient with a clini-
cally stable knee on examination and
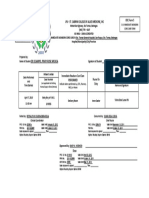
AP (A) and lateral (B) radiographs demonstrating complete transphyseal stress maneuvers typically can return
autogenous quadrupled hamstring anterior cruciate ligament reconstruction in
a 13-year-old patient (Tanner stage 3). Tunnels are placed more vertically to sport approximately 3 to 6
with metaphyseal fixation (arrows). months following the initial injury.
Complete ACL ruptures are man-
Figure 6
Authors’ preferred treatment algorithm for anterior cruciate ligament (ACL) reconstruction in the skeletally immature
patient. All ages referenced are bone ages.
February 2013, Vol 21, No 2 85
Anterior Cruciate Ligament Injuries in the Skeletally Immature Athlete: Diagnosis and Management
aged surgically even in the very with increased single-sport concen- 3. Comstock RD, Collins CL, McIlvain
NM: Summary Report: National High
young patient. In prepubescent pa- tration, year-round participation, School Sports-related Injury Surveillance
tients (ie, Tanner stages 1 and 2) and less time spent in free play. It is Study. 2009-2010 School Year. Available
(bone age: boys, ≤12 years; girls, ≤11 the role of pediatric sports medicine at: http://www.nationwidechildrens.org/
Document/Get/103353. Accessed
years), we prefer a physeal-sparing providers to properly diagnose and November 9, 2012.
combined intra- and extra-articular manage these injuries. Nonsurgical 4. Stanitski CL, Harvell JC, Fu F:
reconstruction using autogenous ilio- management, including activity mod- Observations on acute knee hemarthrosis
tibial band. Adolescent patients with in children and adolescents. J Pediatr
ification, bracing, and physical ther- Orthop 1993;13(4):506-510.
growth remaining (ie, Tanner stages apy, is best used for patients with
5. McNair PJ, Marshall RN, Matheson JA:
3 or 4) (bone age: boys, 13 to 16 partial tears involving <50% of the Important features associated with acute
years; girls, 12 to 14 years) are ACL diameter. In patients with com- anterior cruciate ligament injury. N Z
treated with complete transphyseal Med J 1990;103(901):537-539.
plete ruptures, chronologic, physio-
reconstruction using autogenous logic, and skeletal maturity must be 6. Lee K, Siegel MJ, Lau DM, Hildebolt
quadrupled hamstring tendons with CF, Matava MJ: Anterior cruciate
assessed to appropriately address the ligament tears: MR imaging-based
smaller, more vertical tunnels and injury. Treatment options are predi- diagnosis in a pediatric population.
metaphyseal fixation. In older ado- Radiology 1999;213(3):697-704.
cated on assessment of the patient’s
lescent patients with closing physes maturity and include physeal- 7. Kocher MS, Micheli LJ, Zurakowski D,
(ie, Tanner stage 5) (bone age: males, Luke A: Partial tears of the anterior
sparing, partial and complete trans- cruciate ligament in children and
>16 years; females, >14 years), we physeal, and adult-type anatomic adolescents. Am J Sports Med 2002;
prefer to perform an anatomic adult- 30(5):697-703.
ACL reconstruction. Postoperative
type ACL reconstruction with autog- management includes weight-bearing 8. Hole RL, Lintner DM, Kamaric E,
enous quadrupled hamstring or Moseley JB: Increased tibial translation
and activity modifications, bracing, after partial sectioning of the anterior
bone–patellar tendon graft and inter- and a progressive physical therapy cruciate ligament: The posterolateral
ference screw or aperture fixation. protocol emphasizing ROM, closed-
bundle. Am J Sports Med 1996;24(4):
556-560.
Patients are placed in a ROM chain strengthening, and a gradual
brace for 6 weeks postoperatively. 9. Vavken P, Murray MM: Treating
and measured return to sport-specific anterior cruciate ligament tears in
Patients treated with iliotibial band maneuvers. Surgical complications skeletally immature patients.
ACL reconstruction are restricted to Arthroscopy 2011;27(5):704-716.
are rare.
toe-touch weight bearing for 6 10. Lawrence JT, Argawal N, Ganley TJ:
weeks, whereas patients treated with Degeneration of the knee joint in
skeletally immature patients with a
a transphyseal technique are re- References diagnosis of an anterior cruciate
stricted to toe-touch weight bearing ligament tear: Is there harm in delay of
treatment? Am J Sports Med 2011;
for only 2 weeks. Progressive reha- Evidence-based Medicine: Levels of 39(12):2582-2587.
bilitation consisting of ROM, closed- evidence are described in the table of
11. Guzzanti V, Falciglia F, Gigante A,
chain quadriceps and hamstring contents. In this article, reference 10 Fabbriciani C: The effect of intra-
strengthening, patellar mobilization, is a level III study. References 9, 19, articular ACL reconstruction on the
growth plates of rabbits. J Bone Joint
and modalities are used for the first 21, and 39 are level IV studies. Surg Br 1994;76(6):960-963.
3 months postoperatively. Initiation References printed in bold type are 12. Houle JB, Letts M, Yang J: Effects of a
of straight-line jogging and plyomet- those published within the past 5 tensioned tendon graft in a bone tunnel
rics begins at 3 months after recon- years. across the rabbit physis. Clin Orthop
Relat Res 2001;(391):275-281.
struction. A full return to cutting and
1. National Federation of State High 13. Edwards TB, Greene CC, Baratta RV,
pivoting activities and sports is al- School Associations: High school sports Zieske A, Willis RB: The effect of
lowed at approximately 6 months participation increases for 20th placing a tensioned graft across open
consecutive year. Available at: http://
postoperatively. An ACL brace is ad- growth plates: A gross and histologic
www.nfhs.org/content.aspx?id=3505& analysis. J Bone Joint Surg Am 2001;
vised during sports activities for the terms=high+school+sports+participation 83(5):725-734.
first 2 years postoperatively. +increases+for+20th+consecutive+year.
Published September 15, 2009. Accessed 14. Lipscomb AB, Anderson AF: Tears of the
November 7, 2012. anterior cruciate ligament in adolescents.
J Bone Joint Surg Am 1986;68(1):19-28.
2. Safe Kids USA: Sport and recreation
Summary safety fact sheet. Available at: http:// 15. Koman JD, Sanders JO: Valgus
www.safekids.org/our-work/research/ deformity after reconstruction of the
fact-sheets/sport-and-recreation-safety- anterior cruciate ligament in a skeletally
ACL ruptures in skeletally immature fact-sheet.html. Revised November 1, immature patient: A case report. J Bone
patients are becoming more common 2011. Accessed November 7, 2012. Joint Surg Am 1999;81(5):711-715.
86 Journal of the American Academy of Orthopaedic Surgeons
Jeremy S. Frank, MD, and Peter L. Gambacorta, DO
16. Kocher MS, Saxon HS, Hovis WD, Am J Sports Med 1988;16(1):44-47. The outcome of operatively treated
Hawkins RJ: Management and anterior cruciate ligament disruptions in
complications of anterior cruciate 24. Engebretsen L, Svenningsen S, Benum P: the skeletally immature child.
ligament injuries in skeletally immature Poor results of anterior cruciate ligament Arthroscopy 1997;13(5):627-634.
patients: Survey of the Herodicus Society repair in adolescence. Acta Orthop
Scand 1988;59(6):684-686. 34. Redler LH, Brafman RT, Trentacosta N,
and The ACL Study Group. J Pediatr Ahmad CS: Anterior cruciate ligament
Orthop 2002;22(4):452-457. 25. Lazzarone C, Crova M, Brach Del Prever reconstruction in skeletally immature
17. Stadelmaier DM, Arnoczky SP, Dodds J, E, Comba D: Extraarticular reconstruc- patients with transphyseal tunnels.
tion in the treatment of chronic lesions Arthroscopy 2012;28(11):1710-1717.
Ross H: The effect of drilling and soft
tissue grafting across open growth plates: of the anterior cruciate ligament. Ital J
35. Matava MJ, Siegel MG: Arthroscopic
A histologic study. Am J Sports Med Orthop Traumatol 1990;16(4):459-465.
reconstruction of the ACL with
1995;23(4):431-435. 26. Nakhostine M, Bollen SR, Cross MJ: semitendinosus-gracilis autograft in
Reconstruction of mid-substance skeletally immature adolescent patients.
18. Janarv PM, Wikström B, Hirsch G: The Am J Knee Surg 1997;10(2):60-69.
influence of transphyseal drilling and anterior cruciate rupture in adolescents
tendon grafting on bone growth: An with open physes. J Pediatr Orthop 36. McCarroll JR, Shelbourne KD, Porter
experimental study in the rabbit. 1995;15(3):286-287. DA, Rettig AC, Murray S: Patellar
J Pediatr Orthop 1998;18(2):149-154. 27. Vavken P, Murray MM: The potential tendon graft reconstruction for
for primary repair of the ACL. Sports midsubstance anterior cruciate ligament
19. Kercher J, Xerogeanes J, Tannenbaum A, rupture in junior high school athletes: An
Al-Hakim R, Black JC, Zhao J: Anterior Med Arthrosc 2011;19(1):44-49.
algorithm for management. Am J Sports
cruciate ligament reconstruction in the 28. Guzzanti V, Falciglia F, Stanitski CL: Med 1994;22(4):478-484.
skeletally immature: An anatomical Physeal-sparing intraarticular anterior
study utilizing 3-dimensional magnetic cruciate ligament reconstruction in 37. Aronowitz ER, Ganley TJ, Goode JR,
resonance imaging reconstructions. preadolescents. Am J Sports Med 2003; Gregg JR, Meyer JS: Anterior cruciate
J Pediatr Orthop 2009;29(2):124-129. 31(6):949-953. ligament reconstruction in adolescents
with open physes. Am J Sports Med
20. Shea KG, Grimm NL, Belzer JS: 29. Anderson AF: Transepiphyseal 2000;28(2):168-175.
Volumetric injury of the distal femoral replacement of the anterior cruciate
physis during double-bundle ACL ligament in skeletally immature patients: 38. Kocher MS, Smith JT, Zoric BJ, Lee B,
reconstruction in children: A three- A preliminary report. J Bone Joint Surg Micheli LJ: Transphyseal anterior
dimensional study with use of magnetic Am 2003;85(7):1255-1263. cruciate ligament reconstruction in
resonance imaging. J Bone Joint Surg Am skeletally immature pubescent
2011;93(11):1033-1038. 30. Kocher MS, Garg S, Micheli LJ: Physeal adolescents. J Bone Joint Surg Am 2007;
sparing reconstruction of the anterior 89(12):2632-2639.
21. Yoo WJ, Kocher MS, Micheli LJ: cruciate ligament in skeletally immature
Growth plate disturbance after prepubescent children and adolescents. 39. Cohen M, Ferretti M, Quarteiro M,
transphyseal reconstruction of the J Bone Joint Surg Am 2005;87(11):2371- et al: Transphyseal anterior cruciate
anterior cruciate ligament in skeletally 2379. ligament reconstruction in patients with
immature adolescent patients: An MR open physes. Arthroscopy 2009;25(8):
imaging study. J Pediatr Orthop 2011; 31. Kennedy A, Coughlin DG, Metzger MF, 831-838.
31(6):691-696. et al: Biomechanical evaluation of
pediatric anterior cruciate ligament 40. Liddle AD, Imbuldeniya AM, Hunt DM:
22. Kaeding CC, Aros B, Pedroza A, et al: reconstruction techniques. Am J Sports Transphyseal reconstruction of the
Allograft versus autograft anterior Med 2011;39(5):964-971. anterior cruciate ligament in
cruciate ligament reconstruction: prepubescent children. J Bone Joint Surg
Predictors of failure from a MOON 32. Andrews M, Noyes FR, Barber-Westin Br 2008;90(10):1317-1322.
prospective longitudinal cohort. Sports SD: Anterior cruciate ligament allograft
Health 2011;3(1):73-81. reconstruction in the skeletally immature 41. Wright RW, Fetzer GB: Bracing after
athlete. Am J Sports Med 1994;22(1):48- ACL reconstruction: A systematic review.
23. McCarroll JR, Rettig AC, Shelbourne 54. Clin Orthop Relat Res 2007;455:162-
KD: Anterior cruciate ligament injuries 168.
in the young athlete with open physes. 33. Lo IK, Kirkley A, Fowler PJ, Miniaci A:
February 2013, Vol 21, No 2 87
S-ar putea să vă placă și
- Ankle ArthrodesisDocument10 paginiAnkle ArthrodesisariearifinÎncă nu există evaluări
- Animal Models of Osteoporosis - Necessity and LimitationsDocument16 paginiAnimal Models of Osteoporosis - Necessity and LimitationsariearifinÎncă nu există evaluări
- Peripheral Nervous System (PNS)Document16 paginiPeripheral Nervous System (PNS)ariearifinÎncă nu există evaluări
- The Surgical Treatment of Morton's NeuromaDocument15 paginiThe Surgical Treatment of Morton's NeuromaariearifinÎncă nu există evaluări
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- United States Court of Appeals, Eleventh CircuitDocument10 paginiUnited States Court of Appeals, Eleventh CircuitScribd Government DocsÎncă nu există evaluări
- 04 CIN and Cervical Cancer UNEDITEDDocument120 pagini04 CIN and Cervical Cancer UNEDITEDRalph JuicoÎncă nu există evaluări
- EPDSScoringGuide March2015 PDFDocument1 paginăEPDSScoringGuide March2015 PDFantivenomÎncă nu există evaluări
- Incomplete AbortionDocument2 paginiIncomplete AbortionKEn PilapilÎncă nu există evaluări
- Algoritma MFTIDocument1 paginăAlgoritma MFTITjoema AsriÎncă nu există evaluări
- PSDIRFDocument3 paginiPSDIRFRandy FauskeÎncă nu există evaluări
- Femur Fractures in Children - Case PresentationDocument22 paginiFemur Fractures in Children - Case PresentationChristian MicallefÎncă nu există evaluări
- Renal QuizDocument2 paginiRenal Quizgladz25Încă nu există evaluări
- Or JournalDocument2 paginiOr JournalNathaniel PulidoÎncă nu există evaluări
- EFL Pregnancy SheetDocument5 paginiEFL Pregnancy Sheetcharm000Încă nu există evaluări
- Abnormal LaborDocument20 paginiAbnormal Laborأ.م.د. إنعام فيصل محمدÎncă nu există evaluări
- En - Program 3Document15 paginiEn - Program 3Dr.ThiriÎncă nu există evaluări
- Nurse Deployment Program Journal FebruaryDocument3 paginiNurse Deployment Program Journal FebruaryMenchie Vivas-Alot100% (1)
- Acupuncture Imaging 31 40 PDFDocument10 paginiAcupuncture Imaging 31 40 PDFmamun31Încă nu există evaluări
- Theories of Labor Ons-EtDocument19 paginiTheories of Labor Ons-EtHeron BayaninÎncă nu există evaluări
- HCIA Study Guide 2023Document22 paginiHCIA Study Guide 2023consultasluisfloresdrÎncă nu există evaluări
- Med Sci PostDocument122 paginiMed Sci PostTyeana CampbellÎncă nu există evaluări
- The Grand MultiparaDocument5 paginiThe Grand MultiparaIndhumathiÎncă nu există evaluări
- De Ocampo, Pinky Rose Mojica: Lpu - St. Cabrini College of Allied Medicine, Inc ODC Form 5Document1 paginăDe Ocampo, Pinky Rose Mojica: Lpu - St. Cabrini College of Allied Medicine, Inc ODC Form 5Pinky TenshiÎncă nu există evaluări
- 4 Male and Female Reproductive Organs PPTDocument71 pagini4 Male and Female Reproductive Organs PPTDanica Marie Sibay100% (1)
- Tog 12709Document7 paginiTog 12709saeed hasan saeed100% (1)
- Jurnal Bedah 11Document20 paginiJurnal Bedah 11Andhyka Brillian KharismaÎncă nu există evaluări
- Primum Press Kit 2012Document13 paginiPrimum Press Kit 2012Karina EngraffÎncă nu există evaluări
- Structural and Dynamic Bases of Hand Surgery by Eduardo Zancolli 1969Document1 paginăStructural and Dynamic Bases of Hand Surgery by Eduardo Zancolli 1969khox0% (1)
- Summative Test HealthDocument2 paginiSummative Test HealthRheu-Ven N. IlustrisimoÎncă nu există evaluări
- Hemorrhoids: What Are Hemorroids?Document2 paginiHemorrhoids: What Are Hemorroids?Igor DemićÎncă nu există evaluări
- Bone RegenerationDocument360 paginiBone RegenerationMarc Balsells100% (1)
- Delegation DelegationDocument4 paginiDelegation Delegationapi-299331913Încă nu există evaluări
- Concomitant Squint: Noor Asmah MD Azmi Optometrist HsahDocument56 paginiConcomitant Squint: Noor Asmah MD Azmi Optometrist HsahAnonymous l2Fve4PpD33% (3)