Documente Academic
Documente Profesional
Documente Cultură
Antimicrobial Selection, Administration and Dosage: Continuing Education - Voortgesette Opleiding
Încărcat de
YaserAbbasiTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Antimicrobial Selection, Administration and Dosage: Continuing Education - Voortgesette Opleiding
Încărcat de
YaserAbbasiDrepturi de autor:
Formate disponibile
Continuing education — Voortgesette opleiding
Antimicrobial selection, administration and dosage
a
J Desmond Baggot
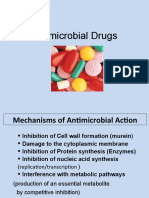
following general mechanisms:
ABSTRACT (i) Selective inhibition of bacterial cell
Various types of information contribute to the selection of an antimicrobial agent. Initial wall synthesis (penicillins, cephalo-
requirements are diagnosis of the site and nature of the infection, assessment of the severity sporins, bacitracin, vancomycin).
of the infectious process and medical condition of the diseased animal; these are embodied Following attachment to receptors
in clinical experience. Additional considerations include identification of the causative (penicillin-binding proteins), beta-
pathogenic microorganism, knowledge of its susceptibility to antimicrobial agents (micro- lactam antibiotics inhibit transpepti-
biological considerations) and of the pharmacokinetic properties of the drug of choice and
dation enzymes and thereby block the
alternative drugs, and their potential toxicity (pharmacological considerations) in the
final stage of peptidoglycan synthesis.
animal species. Select an antimicrobial drug and dosage form appropriate for use in the
This action is followed by inactivation
particular animal species. Usual dosage regimens may be applied, except in the presence of
renal or hepatic impairment, when either modified dosage or a drug belonging to another of an inhibitor of autolytic enzymes in
class should be used. The duration of therapy is determined by monitoring the response the bacterial cell wall. Bacitracin and
both by clinical assessment and bacterial culture. A favourable clinical response is the vancomycin inhibit early stages of
ultimate criterion of successful therapy. peptidoglycan synthesis.
(ii) Inhibition of cell membrane function
Key words: animal therapy, antimicrobial selection, dosage.
by disrupting functional integrity of
Baggot J D Antimicrobial selection, administration and dosage. Journal of the South African the bacterial (polymyxins) or fungal
Veterinary Association (1998) 69(4): 174–185 (En.). Preclinical Veterinary Studies, University
(antifungal azoles and polyenes) cyto-
of Zimbabwe, PO Box MP 167, Mount Pleasant, Harare, Zimbabwe.
plasmic membrane. Antifungal azoles
(e.g. ketoconazole, miconazole, fluco-
nazole) act by inhibiting the bio-
INTRODUCTION class generally have the same mechanism synthesis of fungal membrane lipids,
For the treatment of a bacterial infec- of action, a broadly similar spectrum of especially ergosterol. Polyenes (e.g.
tion, the antimicrobial agent selected antimicrobial activity (Table 1) and amphotericin B, natamycin) require
must have activity against the causative reasonably similar disposition (i.e. extent ergosterol as a receptor in the fungal
pathogenic microorganism and must of distribution and elimination processes) cell membrane in order to exert their
attain effective concentrations at the site (Table 2). Individual drugs within a class effect; this sterol is absent from the
of infection. The ultimate criterion of differ quantitatively in antimicrobial bacterial cell membrane. Polyene anti-
successful therapy is a favourable clinical activity and, when mainly eliminated by biotics and the synthetic antifungal
response to the treatment. Such a response hepatic metabolism, in the rate of elimina- azoles act on fungi, whereas the
depends on the interrelations between tion (usually expressed as half-life). polymyxins act on gram-negative
the causative pathogenic microorganism Bioavailability, which refers to the rate bacteria.
the antimicrobial drug selected and and extent of absorption, and the with- (iii) Inhibition of protein synthesis
dosage used, and the animal receiving drawal period, vary with the dosage form through an action on certain subunits
treatment. Inadequacy of host defense of a drug and may differ between animal of microbial ribosomes (aminoglyco-
mechanisms, particularly in neonatal species. Selective tissue binding (e.g. sides, tetracyclines, chloramphenicol
foals and in immuno -compromised aminoglycosides) is a cause for concern in and its derivatives, macrolides and
animals, could contribute to a discrep- terms of the pathological lesion that may lincosamides). Each class of anti-
ancy between the expected and actual be produced in the particular tissue and microbial agent attaches to a different
response to antimicrobial therapy. In the persistence of drug residues (a long receptor site, apart from macrolides
these animals, it is preferable to use withdrawal period is required). and lincosamides, which bind to the
antimicrobial agents, alone or combined, same site on the 50S subunit of the
that produce a bactericidal effect. MECHANISMS OF ACTION microbial ribosome.
Antimicrobial action usually depends (iv) Inhibition of nucleic acid synthesis.
ANTIMICROBIAL CLASSIFICATION on the inhibition of biochemical events Fluoroquinolones block the action of
Antimicrobial agents are classified on that exist in or are essential to the bacterial DNA gyrase; rifampin binds strongly
the basis of molecular structure, which pathogen but not the host animal. Unfor- to DNA-dependent RNA polymerase;
determines their chemical nature and tunately, the action of antimicrobial metronidazole, following chemical
related physico-chemical properties agents is not selective for pathogenic reduction of the nitro group of the
(pKa/pH-dependent degree of ionisation, microorganisms and the balance between molecule within anaerobic bacteria or
lipid solubility). The drugs within each the commensal flora can be seriously sensitive protozoal cells, produces a
disturbed, particularly in the colon of bactericidal effect by reacting with
horses (doxycycline, macrolides and various intracellular macromolecules.
a
Preclinical Veterinary Studies, University of Zimbabwe, lincosamides). (v) Inhibition of folic acid synthesis in
PO Box MP 167, Mount Pleasant, Harare, Zimbabwe.
The actions of antimicrobial agents can susceptible microorganisms and ulti-
Received: March 1998. Accepted: October 1998. be adequately distinguished by the mately the synthesis of nucleic acids.
174 0038-2809 Jl S.Afr.vet.Ass. (1998) 69(4): 174–185
Table 1: Spectrum of antimicrobial activity (semi-quantitative).
a
Antimicrobial class Usual effect Gram-positive Gram-negative Anaerobic bacteria Other microorganisms
Penicillinsb C
Penicillin G +++ (+) +(+) –
Aminobenzyl-penicillin ++ +(+) + –
Carboxy-penicillin + +(+) + –
Isoxazolyl-penicillin ++ – – –
Cephalosporinsc C
1st generation ++ + + –
2nd generation + ++ ++(cefoxitin) –
3rd generation + ++(+) +(ceftizoxime) –
Aminoglycosides C (+) +++ – (Mycoplasma spp.)
Fluoroquinolones C +(+) +++ – Mycoplasma spp.
Chlamydia spp.
Trimethoprim/sulphonamide C ++ ++ + Chlamydia spp.
Protozoa: Toxoplasma spp.
Tetracyclines S ++ ++ + Mycoplasma spp.
Chlamydia spp.
Rickettsia spp.
Protozoa: Theileria spp., Eperythrozoon spp., Anaplasma spp.
Chloramphenicol S ++ +(+) ++ (Mycoplasma spp.)
(Chlamydia spp.)
Rickettsia spp.
Macrolides S ++ (+) (+) Mycoplasma spp.
(Tylosin)
Lincosamides S ++ – ++(clindamycin) (Mycoplasma spp.)
Rifampin C ++ –/(+) +(+) Chlamydia spp.
Rickettsia spp.
Metronidazole C – – +++ –
Protozoa: Trichomonas foetus, Giardia lamblia, Histomonas meleagridis
Sulphonamides S + (+) + Chlamydia spp.
a
C = bactericidal; S = bacteriostatic.
b
Penicillins
Penicillin G: phenoxymethyl penicillin (penicillin V) – acid-stable.
Aminobenzyl penicillins: ampicillin, amoxillin and pro-drugs.
Carboxypenicillins: ticarcillin, carbenicillin – anti-pseudomonal (P. aeruginosa).
Isoxazolyl penicillins: cloxacillin, oxacillin, nafcillin, methicillin – relatively resistant to staphylococcal beta-lactamase; acid-stable.
c
Cephalosporins
1st generation: cefadroxil, cephalexin (both oral); cefazolin, cephalothin (both parenteral).
2nd generation: cefuroxime (oral); cefoxitin (IV).
3rd generation: cefixime (oral).
Cefotaxime, ceftizoxime, cefoperazone, ceftriaxone, ceftazidime (all IV).
By competing with para-aminobenzoic Knowledge of the mechanisms of action antimicrobial agent are clearly distin-
acid (PABA) for the enzyme dihydropte- of antimicrobial agents is required for guishable and due to different mecha-
roate synthetase, sulphonamides prevent understanding resistance acquired nisms, although lack of a favourable
the incorporation of PABA into dihydro- through chromosomal mutation and clinical response (therapeutic failure) is
folate, while trimethoprim, by selectively selection, and forms the basis of selecting the invariable outcome.
inhibiting dihydrofolate reductase, antimicrobials for concur rent use,
prevents the reduction of dihydrofolate either as combination preparations or Inherent resistance
to tetrahydrofolate (folic acid). Animal separately. Inherent resistance largely limits the
cells, unlike bacteria, utilise exogenous spectrum of activity of an antimicrobial
sources of folic acid. Pyrimethamine ANTIMICROBIAL RESISTANCE agent, while acquired resistance invari-
inhibits protozoal dihydrofolate reduc- There are many different mechanisms ably decreases the quantitative suscepti-
tase, but is less selective for the microbial whereby microorganisms might exhibit bility of pathogenic microorganisms.
enzyme and therefore more toxic than resistance to antimicrobial dr ugs. In order to reach receptors (penicil-
trimethoprim to mammalian species. Inherent and acquired resistance to an lin-binding proteins), beta-lactam
0038-2809 Tydskr.S.Afr.vet.Ver. (1998) 69(4): 174–185 175
Table 2: Extent of distribution and processes of elimination of antimicrobial agents.
a
Antimicrobial agent Extent of distribution (comment) Elimination process(es)
Beta-lactams Limited – low intracellular concentrations E (r), except nafcillin, cefoperazone and
ceftriaxone, E(r+h)
Aminoglycosides Limited – mainly ECF (selective binding to renal cortex; inner ear) E(r)
Fluoroquinolones Wide (developing cartilage) M(h) + E(r+h)
Trimethoprim Wide M(h) + E(r)
Sulphonamides Moderate M(H) + E(r), except sulfisoxazole, E(r) + M(h)
Tetracyclines Wide (sites of ossification; developing teeth) E(r+h), except doxycycline, E(f)
Chloramphenicolb Wide M(h) + E(r)
Metronidazoleb Wide M(h) + E(r)
Erythromycinb Wide – high intracellular concentration M(h) + E(h)
Clindamycin Wide M(h) + E(r)
Rifampinc Wide – high intracellular concentration, including phagocytes M(h) + E(h+r)
a
E(r) = excretion (renal); M(h) = metabolism (hepatic); E(r+h) = excretion (renal and hepatic in bile); E(f) = excretion (in faeces).
b
Inhibits hepatic microsomal enzymes.
c
Induces hepatic microsomal enzymes.
antibiotics must penetrate the outer The inherent resistance of aerobic bacte- adenylation, acetylation or phosphory-
layers of the bacterial cell envelope. ria to metronidazole may be attributed to lation. This type of resistance is usually
Inherent resistance of many gram- the absence of an anaerobic environment plasmid-mediated. Plasmids code for the
n e ga ti ve b a c te r i a t o p e n i ci l l i n G for activation (chemical reduction of the enzyme acetyltransferase that inactivates
(benzylpenicillin) is due to low bacterial nitro group) of the drug to take place. chloramphenicol. Florfenicol, an ana-
permeability, lack of penicillin-binding logue of thiamphenicol, is less susceptible
proteins and/or a wide variety of Acquired resistance than chloramphenicol to inactivation by
beta-lactamase enzymes. Gram-negative The potential for genetic exchange bacterial acetyltransferase. Defective
bacteria have an outer phospholipid between bacteria, combined with their active transport of tetracyclines across
membrane that may hinder passage of short generation time, can rapidly lead to the inner cytoplasmic membrane of
beta-lactam antibiotics. Some (such as resistant bacterial populations. Acquired, microorganisms that have acquired resis-
ampicillin and amoxicillin) pass through genetically based resistance may be due tance may be plasmid-mediated. Since
pore molecules in this outer barrier more to chromosomal mutation (altered struc- the plasmid genes that code for tetracy-
readily than penicillin G. Owing to their tural target or metabolic pathway essen- cline resistance are closely associated with
higher capacity to penetrate cell mem- tial for antimicrobial action) or, more those for chloramphenicol and amino-
branes, 3rd-generation cephalosporins importantly, the acquisition, by bacterial glycosides (especially streptomycin),
(except cefoperazone) have activity conjugation, of resistance (R) plasmids16. multiple drug resistance may result.
against an expanded range of gram- Resistance plasmids (transferable genetic Multiple drug-resistance plasmids, which
negative aerobic bacteria and reach infec- material) may be present in bacteria commonly occur in Enterobacteriaceae
tion sites in the central nervous system. as extrachromosomal circular DNA such as Salmonella, E. coli and Proteus, will
Streptococci have a natural permeability molecules that replicate independently be maintained in a population by the use
barrier to aminoglycosides. Their pene- of, but synchronously with, chromosomal of any antibiotic to which resistance is
trative capacity can be enhanced by the DNA. Plasmid genes for antimicrobial encoded by the plasmid genes.
simultaneous presence of a cell wall- resistance often control the formation of The spread of multiple drug resistance
active drug, such as a penicillin. bacterial enzymes that are capable of has serious implications on account of its
Most gram-negative aerobic bacteria, either inactivating antimicrobial agents persistence. Plasmid-mediated resistance
with the notable exception of Brucella or decreasing bacterial membrane to lincosamides and macrolides is the
spp., are relatively impermeable and permeability to antimicrobials11. result of methylation of the shared recep-
therefore inherently resistant to rifampin; Plasmid-mediated resistance to penicil- tor site on the 50S subunit of the bacterial
the site of action of rifampin is intra- lins and cephalosporins (beta-lactam ribosome. Plasmid-transferable resis-
cellular. Microbial susceptibility to antibiotics) is due to the formation of tance has recently been reported for
tetracyclines depends on the attainment beta-lactamase enzymes by S. aureus or fluoroquinolones13.
of high intracellular drug concentrations. enteric gram-negative rods. Some Chromosomal mutants are commonly
Individual tetracyclines differ in lipid beta-lactamases can be firmly bound by resistant by virtue of a change in a struc-
solubility. A distinction must be made compounds such as clavulanic acid (com- tural receptor for an antimicrobial agent.
between microorganisms that have low bined with amoxycillin or ticarcillin) and Resistance to beta-lactam antibiotics
capacity for penetration by tetracyclines sulbactam (combined with ampicillin) (penicillins and cephalosporins) may be
(inherently resistant) and those that and can thus be prevented from attacking attributed to the loss (or alteration) of
acquire resistance through defective hydrolysable penicillins. Gram-positive penicillin-binding proteins. Chromo-
active transport of these drugs across the bacteria, apart from staphylococci, gener- somal resistance to aminoglycosides
inner cytoplasmic membrane. Since ally lack the ability to acquire R plasmids. (including amikacin) is associated with
mycoplasmas are bounded by a triple- Gram-negative bacteria that are resis- the deletion (or alteration) of a specific
layered ‘unit membrane’ and lack a rigid t a n t t o a m i n o g l y c o s i d es p r o d u c e receptor (protein) on the 30S ribosomal
cell wall, these microorganisms are inher- enzymes that inactivate dr ugs in subunit. Resistance to fluoroquinolones
ently resistant to beta-lactam antibiotics. this class, apart from amikacin, by (especially in coagulase-positive staphy-
176 0038-2809 Jl S.Afr.vet.Ass. (1998) 69(4): 174–185
Table 3: Empirical antimicrobial drug selection based on knowledge of pathogenic microorganism.
Microorganism Drug of choice Alternatives
Gram-positive aerobic bacteria
Streptococcus spp. Penicillin G 1st-generation cephalosporin: trimethoprim/sulphonamide
Staphylococcus, non-penicillinase-producing Penicillin G 1st-generation cephalosporin
Staphylococcus, penicillinase-producing Isoxazolyl penicillins 1st-generation cephalosporin; fluoroquinolone;
amoxycillin/clavulanate
Staphylococcus, methicillin-resistant Fluoroquinolone Trimethoprim/sulphonamide
Bacillus spp. Penicillin G Erythromycin
Erysipelothrix rhusiopathiae Penicillin G Erythromycin
Corynebacterium spp. Penicillin G Erythromycin
Listeria monocytogenes Aminobenzyl-penicillin Chloramphenicol; trimethoprim/sulphonamide
Nocardia spp. Trimethoprim/sulphonamide Minocycline (± sulphonamide)
Mycobacterium tuberculosis Rifampin + isoniazid Streptomycin
Gram-negative aerobic bacteria
Coliforms (E. coli, Klebsiella spp., Proteus spp.,
enterobacter spp.) Gentamicin (or amikacin) Fluoroquinolone; 3rd-generation cephalosporin
Salmonella spp. Trimethoprim/sulphonamide Fluoroquinolone; aminobenzyl-penicillin
Pasteurella multocida Aminobenzyl-penicillin Aminoglycoside; fluoroquinolone
Actinobacillus spp. Trimethoprim/sulphonamide Fluoroquinolone; amoxycillin/clavulanate; tetracycline
Leptospira spp. Aminobenzyl-penicillin Erythromycin; streptomycin
Helicobacter spp. Erythromycin Fluoroquinolone
Bordetella bronchiseptica Tetracycline Trimethoprim/sulphonamide; chloramphenicol; gentamicin
Pseudomonas aeruginosa Gentamicin ± ticarcillin (or carbenicillin) Ciprofloxacin; 3rd-generation cephalosporin
Moraxella bovis Oxytetracycline Cephalothin; chloramphenicol; aminoglycoside
Anaerobic bacteria
Clostridium spp. Penicillin G 1st-generation cephalosporin; (clindamycin)
Actinomyces spp. Penicillin G Erythromycin; trimethoprim/sulphonamide
Fusobacterium spp Metronidazole Penicillin G; clindamycin; 1st-generation cephalosporin
Bacterioides spp. (other than B. fragilis) Metronidazole Penicillin G; clindamycin; cefoxitin
Bacterioides fragilis Metronidazole or clindamycin Chloramphenicol; ampicillin/sulbactam; cefoxitin
Other microorganisms
Mycoplasma spp. Tylosin or tiamulin Fluoroquinolone; tetracycline
Chlamydia spp. Tetracycline Trimethoprim/sulphonamide
Rickettsia spp. Tetracycline Chloramphenicol
lococci and Pseudomonas spp.) may be due use of antimicrobials does not induce tetracyclines have the same basic
to mutation of the target enzyme, DNA resistance but rather provides an intense structure, cross-resistance between
gyrase. The rapid development of high- selection pressure that, by destroying tetracyclines is to be expected. Although
level resistance to rifampin, associated the susceptible bacteria in the host l i n c o s a mi d es a n d ma c r o l i d e s a r e
with its use as the sole antimicrobial animal, allows the resistant bacteria to structurally unrelated, they share the
agent, results from chromosomal muta- proliferate9. The gravity of this adverse same receptor-binding site, have the
tion of bacterial RNA polymerase. In situation lies in the fact that, once devel- same mechanism of plasmid-mediated
sulphonamide-resistant mutants the oped, multi-resistant organisms can resistance, and cross-resistance between
affinity of dihydropteroate synthetase for persist in the individual or exposed drugs in these 2 classes is common.
p-aminobenzoic acid may exceed that for animal population and in the environ- Because of its unique action (inhibition of
sulphonamide, which is a reversal of the ment. The control of antimicrobial resis- RNA polymerase), cross-resistance
situation in sulphonamide-sensitive tance, in so far as is possible, depends on between rifampin and other anti-
m ic ro o r g a n i s m s . A t l e a s t s o m e the judicious selection and appropriate microbial agents does not occur.
sulphonamide-resistant bacteria can, like use of antimicrobial agents.
mammalian cells, utilise preformed folic APPROACH TO THERAPY
acid for nucleic acid synthesis. Cross-resistance Having diagnosed the presence of a
Microorganisms that are resistant to a bacterial infection, appropriate speci-
Significance of transferable drug certain antimicrobial agent may also be mens should be properly collected to
resistance resistant to other antimicrobials with the identify the causative pathogenic micro-
Acquired resistance to several antibiot- same mechanism of action or share the organism(s) and, when considered
ics is of particular concern in Enterobac- same receptor-binding site. Cross- necessary, to determine its susceptibility.
teriaceae and is increasingly found in resistance mainly applies to antimicrobial Perform immediate examination of the
non-enteric gram-negative bacterial agents that are closely related structur- specimen, including (whenever feasible)
pathogens, as well as in the commensal ally, i.e. are within the same class (e.g. a Gram-stained direct smear. The value of
flora. A causal relationship has been aminoglycosides, fluoroquinolones, immediate examination of clinical
shown between the use of antimicrobials lincosamides, sulphonamides, chloram- specimens in the initial selection of
and the development of resistance. The phenicol and its derivatives). Since all an antimicrobial agent cannot be
0038-2809 Tydskr.S.Afr.vet.Ver. (1998) 69(4): 174–185 177
Table 4: Suggested guideline for the interpretation of MIC (µg/m ) of various antimicrobial agents based on
bacterial isolates of equine origin, apart from fluoroquinolones which relate to isolates of canine origin.
Antimicrobial agent Susceptible Moderately susceptible Resistant
Penicillin G ≤0.125 0.25–16 >16
Ampicillin ≤1 2–16 >16
Amoxycillin ≤1 2–16 >16
Gentamicin ≤2 4–8 >8
Amikacin ≤4 8–16 >16
Fluoroquinolonesa ≤1 2–4 >4
Erythromycin ≤0.5 1–4 >4
Tetracycline ≤1 2–4 >4
Chloramphenicol ≤4 8–16 >16
Trimethoprim/sulfamethoxazole ≤0.5/10 1/20–2.5/50 >3/75
a
Quantitative susceptibility of bacterial pathogens varies between individual fluoroquinolones, e.g. the minimum inhibitory concentration
of ennofloxacin for the majority of susceptible E. coli strains isolated from calves is 0.25 µg/m .
Table 5: Usual dosage for antimicrobial preparations used in dogs and cats.
Drug preparation Route of administration Dosing rate
Dose (mg/kg) Interval (h)
Penicillin G, sodium IV,IM,SC 20 000–40 000 IU/kg 4–6
Penicillin G, procaine IM, SC 25 000 IU/kg 24
Penicillin V, calcium PO 10–20 8
Ampicillin sodium IV, IM, SC 10–20 8
Ampicillin PO 25 8
Hetacillin or pivampicillin PO 20–30 8
Amoxycillin trihydrate PO 12.5–25 8–12
Amoxycillin trihydrate/clavulanate, potassium PO 12.5–25 8–12
Cloxacillin sodium PO 25–35 8
Cefadroxil PO 20–30 8–12
Cephalexin monohydrate PO 20–30 8–12
Cefazolin sodium IV 10–20 8
Gentamicin sulphate IM/SC 3–5 8–12 (dogs)
(12–24 cats)
Amikacin sulphate IM/SC 6–10 8–12
Enrofloxacin PO 5–10 12
Marbofloxacin PO 2–4 24
Trimethoprim/sulphadiazine PO 5/25 12
Trimethoprim/sulphamethoxazole PO 5/25 12
Tetracycline hydrochloride PO 20 8
Oxytetracycline hydrochloride PO 20 12
Oxytetracycline dihydrate PO 40 12
Doxycycline hydrochloride PO 5 12
Chloramphenicol PO 25 8 (dogs)
12 (cats)
Chloramphenicol palmitate PO 25 8 (dogs)
Metronidazole PO 10–20 8–12
Erythromycin PO 10–20 8–12
Erythromycin estolate PO 10–20 8–12
Clindamycin hydrochloride PO 5–10 8–12
Sulfisoxazole PO 50 8
Sulfasalazine PO 25 8 (dogs)
Ketoconazole PO 5–10 12–24
Griseofulvin (micronised) PO 25–50 12–24
overemphasised. Initial (empirical) treatment drug for initial therapy is largely based on
Blood culture is a valuable, although not Since there will be some delay in obtain- clinical experience, the nature (and site)
invariably certain, technique for making a ing laboratory results, antimicrobial of the infectious disease process and
microbiological diagnosis of septicaemia therapy should be initiated on an epidemiological pattern in the herd or
in neonatal foals. informed empirical basis. The choice of geographical region, but should be
178 0038-2809 Jl S.Afr.vet.Ass. (1998) 69(4): 174–185
supported by the findings of specimen should be understood that the method 90 % of isolates tested, compared over
examination. A suggested choice of drug relates antimicrobial drug concentrations different time periods (e.g. on an annual
for initial therapy, based on knowledge achieved in the serum of human beings basis), would reveal the pattern of resis-
(although tentative at this stage) of the given usual dosages to the susceptibility tance to a drug.
pathogenic microorganism, is presented pattern of populations of fast-growing
in Table 3. While the drug of choice pre- aerobic bacteria15. The MIC of an organ- Maintenance therapy
sented in this table is generally applicable, ism can be extrapolated from inhibitory The choice of drug for maintenance
selection of the antimicrobial agent must zone diameters, and these MIC values therapy rests with the clinician and is
be related to the site of the infection, the have been used to define breakpoints to based on the severity, site and nature of
animal species and the readily available describe bacteria as susceptible or resis- the infection, knowledge of the suscepti-
dosage forms. tant. The disk-diffusion method provides bility of the causative pathogenic micro-
Provide supportive measures that a qualitative or, at best, semi-quantitative organism and the pharmacokinetic
would complement antimicrobial effec- indication of susceptibility, since some properties of the drug in the animal
tiveness and assist recovery of the animal antimicrobials become concentrated species, and on clinical experience.
from the infection. In neonatal animals, while others penetrate poorly into certain Consideration must be given to the toxic
care must be taken to avoid a too-rapid body fluids and tissues; furthermore, the potential of the antimicrobial agent of
rate of intravenous fluid administration. disposition of many antimicrobial agents choice, the dosage forms that would
Fever may serve a useful purpose in infec- differs between human beings and be suitable for administration to the
tious diseases and the change in body animal species. Owing to the aforemen- individual animal, the ease of repeated
temperature may be used to assess the tioned limitations of the disk-diffusion administration (which often determines
progress of the infection. In the presence method, it is necessary to determine owner compliance), and the overall cost
of an infectious disease, the only indica- quantitative susceptibility, using the of the likely course of therapy. Due
tion for an antipyretic drug, e.g. aspirin or broth dilution method (which measures account should be taken of the value,
paracetamol (acetaminophen) in dogs but MIC), of pathogenic microorganisms of according to the owner, of the animal in
not in cats, or dipyrone or sodium salicy- frequently unpredictable susceptibility. making the final choice of antimicrobial
late administered intravenously to They include coagulase-positive staphy- agent and the dosage form.
horses, is to decrease body temperature to lococci (S. aureus and S. intermedius) and Apply the usual dosage regimen for the
below a dangerous level, 41 °C (105.8 °F). enteric microorganisms (E. coli, Klebsiella, drug preparation (dosage form) selected,
Concurrent therapy with a non-steroidal, Proteus and Salmonella spp.). The determi- or apply a dosage regimen tailored to the
anti-inflammatory drug and an amino- nation of quantitative susceptibility could individual animal and based on the
glycoside antibiotic increases the risk of be considered essential for bacteria that quantitative susceptibility (MIC) of the
nephrotoxicity. If the infection is sus- have developed multiple drug resistance. causative pathogenic microorganism.
pected to be contagious, isolate the Quantitative susceptibility varies The latter approach to dosage (specific
diseased and in-contact animals. between bacterial genera and species, as therapy) assumes greater importance in
When an appreciable quantity of pus or well as between strains of a particular the treatment of severe systemic infec-
a foreign body is present, the appropriate species. Moreover, individual drugs tions (such as septicaemia).
surgical intervention is indicated. within a class differ quantitatively in Advise the owner regarding supportive
antimicrobial activity. Tetracyclines measures that should be provided and, in
Bacterial culture and susceptibility might constitute an exception, in that the case of food-producing animals, the
testing differences in clinical efficacy between specified withdrawal period for the drug
After the pathogenic microorganism tetracyclines are largely attributable to preparation selected. The withdrawal
has been isolated by bacterial culture features of bioavailability, distribution period for a drug may vary with the
(performed under various incubation and excretion. Suggested interpretative preparation (dosage form) as well as
conditions) and identified, the decision guidelines for MIC breakpoint values are between food-producing animal species.
can be made as to whether susceptibility presented (Table 4). The choice of It is stated on the label (and package
testing (particularly the determination antimicrobial agent for systemic therapy insert) of authorised drug preparations.
of minimum inhibitory concentration, is almost invariably limited to drugs to
MIC) is necessary. The susceptibility of which the bacterial pathogen is suscepti- DRUG ADMINISTRATION AND
certain commonly isolated bacteria is ble. For treatment of canine urinary tract DOSAGE
generally predictable. For example, infections, the range of antimicrobial The route of administration of an
beta-haemolytic Streptococci isolated agents can be extended to include antimicrobial drug depends on the site
from horses are susceptible to penicillin drugs to which the bacterial pathogen is and severity of the infection as well as on
G, as are anaerobes, except Bacterioides moderately susceptible provided urinary the animal species, but is often governed
spp. In mixed infections and abscesses, concentrations exceeding 4 times the MIC by the dosage forms that are available. It is
the presence of anaerobic bacteria should could be maintained during therapy. because bacterial susceptibility (MIC)
always be considered. The fostering of a Knowledge of the susceptibility of a can be determined in vitro and drug
close working relationship with the clini- pathogenic microorganism is most useful disposition processes are quantifiable (in
cal microbiology laboratory is important for selecting the antimicrobial agent of pharmacokinetic terms) that dosing rates
with regard to the relevance of the tech- choice and can be applied in tailoring for antimicrobial drugs can be calculated.
niques performed to the clinical situation dosage of the drug for an individual However, various formulations may
and the interpretation of the laboratory animal but, even though in vitro suscepti- differ significantly from a standard
results. bility (particularly MIC) generally corre- (reference) formulation in bioavailability
Concerning susceptibility testing, the lates well with clinical efficacy, it cannot of the drug substance (active moiety).
disk (agar)-diffusion method is satisfac- be relied upon to predict response to Only drug preparations that are bio-
tory only when a microorganism is either therapy. Accumulated data on MIC90, equivalent in the target species would be
very susceptible or very resistant. It which is the MIC breakpoint value for expected to have similar clinical efficacy.
0038-2809 Tydskr.S.Afr.vet.Ver. (1998) 69(4): 174–185 179
Table 6: Influence of food on the oral bioavailability of antimicrobial agents in tion from the former injection site could
dogs and cats.
be attributed to wider spread of the
parenteral preparation (aqueous suspen-
sion or non-aqueous solution) providing
a
Antimicrobial class/preparation Effect on oral bioavailability
greater access to a larger absorptive
Most penicillins, apart from ↓ surface area and possibly to higher blood
amoxycillin and – flow to tissues in this region. At least a
ampicillin pro-drugs – portion of the volume injected is more
Cephalosporins ↓ likely to be deposited between muscles
Fluoroquinolones – (intermuscular), which would facilitate
Trimethoprim/sulphonamide ↓ spread of the preparation along fascial
Most tetracycline, apart from ↓ planes, in the neck than in the buttock.
doxycycline ↑ Even though the usual dosage interval for
Chloramphenicol – oxytetracycline dihydrate (a long-acting
Chloramphenicol palmitate ↑ (cats) parenteral formulation) is 48 h, the intra-
Metronidazole ↑ (dogs) muscular injection of 2 doses (20 mg/kg,
Erythromycin base ↓
72 h apart) can be recommended for the
Erythromycin stearate ↓
treatment of infectious bovine kerato-
Erythromycin estolate ↑
conjunctivitis, caused by Moraxella bovis6.
Erythromycin ethylsuccinate ↑
Erythromycin enteric-coated formulations –
Antimicrobial agents are administered to
Clarithromycin – pigs either in the feed or drinking water,
Nitrofurantoin ↑ (dogs) or by intramuscular injection, provided
Ketoconazole ↑ injection site damage is not produced
Griseofulvin (micronised) ↑ (Table 8). Parenteral preparations should
be formulated in a manner such that their
a
Oral bioavailability of an antimicrobial agent may vary with formulation of the oral dosage form. intramuscular injection does not cause
tissue damage with persistence of drug
residues at the injection site. Ante-
Selected features of the plasma concen- tetracyclines, erythromycin base or mortem methods for evaluating the
tration-time profiles are used for stearate). The oral bioavailability of some extent of tissue irritation and rate of
bioequivalence assessment of formula- antimicrobial agents (e.g. amoxycillin, resolution at the injection site include the
tions of an antimicrobial agent12. fluoroquinolones) is indifferent to the use of ultrasonography2 and determina-
Oral administration is used, particularly time of feeding relative to dosing. tion of the kinetics of plasma creatine
in dogs and cats, in the treatment of mild Many of the antimicrobial agents that kinase (CK) activity1,19.
and moderate infections or when a pro- are given orally to dogs are administered The systemic availability of antimicro-
longed duration of therapy is anticipated by intramuscular injection, depending on bial agents administered orally (pastes) or
(Table 5). The oral bioavailability of many the availability of parenteral prepara- by nasogastric tube (aqueous suspen-
antimicrobial agents is affected by the tions, to ruminant animals (Table 7). The sions) to horses is significantly decreased
temporal relationship between feeding systemic availability (extent of absorp- by feeding before dosing. Food should be
and dosing (Table 6). Depending on this tion) of an antimicrobial agent from a withheld for up to 2 h after drug adminis-
relationship, food should either be given parenteral formulation injected intra- tration. Metronidazole, which is most
1 h before dosing (e.g. with doxycycline, muscularly is generally higher when the useful for the treatment of anaerobic
erythromycin estolate, ketoconazole) or site of injection is the lateral neck com- infections (e.g. pleuropneumonia, liver
be withheld for up to 2 h after dosing (e.g. pared with the buttock (M. semiten- abscesses, peritonitis), is an exception in
with most penicillins, cephalosporins, dineus)14,17. Better antimicrobial absorp- that the drug is well absorbed from the
Table 7: Usual dosage regimens for antimicrobial preparations used in cattle, sheep and goats.
Drug preparation Route of administration Dosing rate
Dose (mg/kg) Interval (h)
Penicillin G, sodium IV, IM 25 000 IU/kg 6–8
Penicillin G, procaine IM 25 000 IU/kg 24
Ampicillin sodium IV, IM 10–20 8
Ampicillin/sulbactam IM 10 8–12
Amoxycillin trihydrate IM 10 12
Trimethoprim/sulphonamide IM 4/20 12
Enrofloxacin IM 2.5–5 12
Oxytetracycline hydrochloride IV, IM 10 12
Oxytetracycline dihydrate (long-acting) IM 20 48
Erythromycin lactobionate IV, IM 5 8–12
Lincomycin hydrochloride IM 10 12
Tylosin IM 20 12
Sulphamethazine (10 % oral solution) PO 50 12
180 0038-2809 Jl S.Afr.vet.Ass. (1998) 69(4): 174–185
Fig. 1: Mean plasma penicillin concentration time curves after 20 000 IU procaine penicillin G/kg was administered to five animals (4 horses,
1 pony) at five different sites (after Firth et al. 19865).
Table 8: Usual dosage regimens for antimicrobial preparations used in pigs.
Drug preparation Route of administration Dose Interval Feed Water
(mg/kg) (h) (g/US ton) (mg/ )
Ampicillin sodium IM 10–20 8 – –
Penicillin G, procaine IM 20 000 – 40 000 IU/kg 24 – –
Amoxycillin trihydrate/clavulanate potassium PO 10–15 12 – –
Streptomycin sulphate IM 10 8 – –
Kanamycin sulphate IM 10 8 – –
Gentamicin sulphate IM 2–4 8 – 12.5
Apramycin sulphate PO 10–20 12 150 100
Neomycin sulphate PO 10 8 140 100
Enrofloxacin IM 2.5–5.0 12 – –
Trimethoprim/sulphonamide IM 4/20 12 – –
Sulphamethazine (10 % oral solution) PO 50 12 – 80–120
Oxytetracycline hydrochloride IM 10 12 200–800 –
Oxytetracycline dihydrate (long-acting) IM 20 48 – –
Lincomycin hydrochloride IM 10 12 100–200 30
Tylosin IM 20–30 12 100 80
Tiamulin IM 10–15 24 200 60
Virginiamycin – – – 100 –
Bacitracin – – – 250 –
Monensina – – – 100 –
a
NB: concurrent use of monensin and tiamulin must be avoided, otherwise toxicity will very likely occur.
gastrointestinal tract (systemic availabil- occupies a unique position in the treat- administration to horses but care must be
ity, 60–90 %) of fasted and fed horses. The ment of equine bacterial infections. This taken to avoid inadvertent intravenous
addition of an antimicrobial agent to the long-acting parenteral dosage form administration. The intramuscular injec-
feed (as a powder) is an unreliable (aqueous suspension) of penicillin G pro- tion of procaine penicillin G in the neck
method of dosing horses. Usual dosage vides effective plasma concentrations of region (M. serratus ventralis cervicis)
regimens for antimicrobial preparations the antibiotic for at least 12 h, owing to produces a higher peak plasma concen-
that may be used in horses are presented slow absorption from the intramuscular tration and higher systemic availability of
in Table 9. Parenteral (IV or IM) therapy injection site, and has high activity penicillin G than injection of the
with conventional (immediate-release) against commonly isolated equine bacte- long-acting product at other locations5
dosage forms is required in the treatment rial pathogens. It is the only long-acting (Fig. 1). The prime site for intramuscular
of severe infections. Procaine penicillin G antimicrobial preparation suitable for injection in the neck of the horse appears
0038-2809 Tydskr.S.Afr.vet.Ver. (1998) 69(4): 174–185 181
Table 9: Usual dosage regimens for antimicrobial preparations used in horses.
Drug preparation Route of administration Dosing rate
Dose (mg/kg) Interval (h)
Penicillin G, sodium IV, IM 15 000 – 30 000 IU/kg 6
Penicillin G, procaine IM 25 000 IU/kg 12
Ampicillin sodium IV, IM 10–20 8
Ticarcillin sodium/clavulanate potassium IV (slowly) 50 8
Cefadroxil PO 25 8
Cephalexin monohydrate PO 25 8
Cefazolin sodium IV 10–20 8
Gentamicin sulphate IM 2–4 8–12
Amikacin sulphate IM 4–8 8–12
Trimethoprim/sulphadiazine PO 5/25 12
Chloramphenicol palmitate PO 50 8
Chloramphenicol sodium succinate IV, IM 25 6
Metronidazole PO 20 12
Oxytetracycline hydrochloride IV (slowly) 3 12
Rifampin PO 5 12
Erythromycin estolate PO 20–25 8(foals)
Ketoconazole PO 10 12–24
Table 10: Suggested dosage regimens for antimicrobial preparations that may be used in reptilesa.
Drug preparation Species Route of administration Dosing rate
Dose (mg/kg) Interval (h)
Ampicillin sodium Tortoise IM 50 12
Carbenicillin Snakes IM 400 24
Tortoise IM 400 48
Gentamicin sulphate Alligator IM 1.75 72–96
Snakes IM 2.5 72
Tortoise IM 2.5 48
Amikacin sulphate Alligator IM 2.5 96
Snakes IM 5.0 72
Tortoise IM 5.0 48
Enrofloxacin Hermann’s tortoise IM 10.0 24
Gopher tortoise IM 5.0 24
Ciprofloxacin Snakes PO 2.5 48–72
Trimethoprim/sulphadiazine All species IM 5/25 First 2 doses 24 h
apart: thereafter 48
Tylosin All species IM 10 24
Ketoconazole Tortoise PO 15–30 24
a
Source: Jacobson (1993: adated from Table 29.4)10.
to be at the level of the 5th cervical verte- intramuscular injection should be the at 10 °C; 33 h at 24 °C), cattle (2.5 h), horse
bra, ventral to the funicular part of the anterior half of the body; most reptilian (3.6 h), dog (5.6 h) and human being
ligamentum nuchae but dorsal to the species have a well-developed renal (9.9 h). Oxytetracycline is slowly elimi-
brachiocephalic muscle3. The location of portal system. This also applies to birds. nated by glomerular filtration because the
the intramuscular injection site does not Fish, in common with reptiles, are drug undergoes enterohepatic circula-
affect the bioavailability (refers to rate and poikilothermic (cold-blooded) animals tion. The half-life of oxytetracycline is
extent of absorption) of gentamicin and ambient temperature may have a 89.5 h in rainbow trout (Salmo gairdneri)
(50 mg/ml solution), nor does gentamicin pronounced influence on the rate of drug at 12 °C and 80.3 h in African catfish
bioavailability differ following intramus- elimination, particularly when bio- (Clarias gariepinus) at 25 °C8, compared
cular or subcutaneous injection7,20. transformation is the principal process of with half-lives in the range 3.4–9.6 h in
Owing to the slow elimination (long elimination. The half-life of trimetho- domestic animals. In fish and reptiles, the
half-life) of antimicrobial agents in prim, administered intravenously as elimination of antimicrobial agents
reptiles, dosage intervals are substantially trimethoprim/sulphadiazine combina- increases with increase in ambient
longer in reptilian compared with tion, differs widely between carp temperature. When developing drug
mammalian species10 (Table 10). In order (Cyprinus carpio L) and mammalian products for use in farmed fish (food-
to avoid significantly decreased systemic species: carp (40.7 h at 10 °C; 20 h at 24 °C), producing animals), studies of the
availability of drugs that are eliminated cattle (1.25 h), horse (3.2 h), dog (4.6 h) and relationship between pharmacokinetics
by renal excretion (e.g. beta-lactam and human being (10.6 h). Sulphadiazine of the drugs and ambient (water) temper-
aminoglycoside antibiotics), the site of half-life similarly differs widely: carp (47 h ature should be performed.
182 0038-2809 Jl S.Afr.vet.Ass. (1998) 69(4): 174–185
Table 11: Activity of concurrently used antimicrobial drugs.
Antimicrobial agents Activity
Combination preparations
Trimethoprim/sulphonamide Synergistic: bactericidal against susceptible microorganisms
Ampicillin/sulbactam Enhanced (broader) activity of the penicillin
Amoxyllin/clavulanate Enhanced (broader) activity of the penicillin
Ticarcillin/clavulanate Enhanced (broader) activity of the penicillin
Administered separately
Ampicillin (or amoxycillin) – gentamicin May be synergistic, depending on the microorganism
Ticarcillin (or carbenicillin) – gentamicin Synergistic against some strains of: Pseudomonas, Proteus, Enterobacter, Klebsiella spp.
Erythromycin – rifampin Synergistic; Rhodococcus equi
Isoniazid – rifampin Prevents emergence of resistant strains Mycobacterium tuberculosis
Doxycycline – rifampin Brucella melitensis (human beings)
Minocycline – rifampin (or streptomycin) Brucella canis (dogs)
Oxytetracycline – rifampin (or streptomycin) Brucella abortus (horses)
Clindamycin (or metronidazolea) – gentamicin Additive; mixed gram-negative + anaerobic infections
Lincomycin – spectinomycin Additive; bacterial respiratory infections in cattle
a
Use metronidazole in horses.
ANTIMICROBIAL COMBINATIONS drug to prevent the rapid emergence of inhibitory concentrations following
The mechanisms of action as well as the strains resistant to rifampin. In mixed exposure of susceptible bacteria to drug
susceptibility of microorganisms underlie infections with anaerobic involvement, concentrations above the minimum
the type of interaction that may occur the concurrent use of clindamycin (or, in inhibitory concentration (MIC).
(generally additive, but may be synergis- horses, metronidazole) and gentamicin is Aminoglycosides inhibit ribosomal
tic or antagonistic) when antimicrobial the treatment of choice. protein synthesis in susceptible bacteria
agents of different classes are used con- Unless specifically indicated, which by inducing misreading of the genetic
currently (either as combination prepara- implies synergistic action and/or the code on the messenger RNA template
tions or administered separately). prevention of acquired resistance, or (30S ribosomal subunit). Fluoroquino-
Useful combination preparations there is circumstantial evidence to sup- lones block nucleic acid synthesis in
include trimethoprim/sulphonamide port the clinical effectiveness of anti- susceptible bacteria by selectively inhibit-
that, through synergistic action, produces microbial combinations, the concurrent ing DNA gyrase, an intracellular enzyme.
a bactericidal effect (at least in vitro), use of antimicrobial drugs should be Both classes of antimicrobial agent
amoxycillin/clavulanate and ticarcillin/ avoided. When 2 antimicrobial agents are produce a concentration-dependent
clavulanate (Table 11). The concurrent used concurrently, not as a combination bactericidal effect.
use of ampicillin (or amoxycillin) and preparation, they must be administered The clinical effectiveness of amino-
gentamicin is likely to provide synergistic independently at usual dosing rates. glycosides and fluoroquinolones is
action at least against streptococci (have a influenced both by the height of the peak
natural permeability barrier to amino- RELATIONSHIP BETWEEN PLASMA plasma concentration relative to the
glycosides), while ticarcillin (or carbeni- CONCENTRATION AND CLINICAL minimum inhibitory concentration
cillin) and gentamicin used concurrently EFFECTIVENESS (Cmax:MIC ratio) and the area under the
act synergistically against some strains of Penicillins and cephalosporins act by plasma concentration-time curve that is
Pseudomonas, Proteus, Enterobacter and causing selective inhibition of bacterial above the MIC during the dosage interval
Klebsiella spp. (i.e. gram-negative rods). cell wall synthesis; they interfere with the (AUIC = AUC/MIC). The former is rela-
Note that penicillins and gentamicin final stage of peptidoglycan synthesis. tively more important for fluoroquino-
should not be mixed in vitro, since activity Beta-lactam antibiotics produce a lones; maximum activity is achieved
of t h e a m i n o g l y c o s i d e w o u l d be time-dependent bactericidal effect on when peak plasma concentration is in the
decreased (owing to chemical interac- susceptible bacteria. The overall effective- range 5–10 times the MIC. The clinical
tion). The concurrent use of a bacterio- ness of therapy with penicillins (and effectiveness of the aminoglycosides is
static drug and a bactericidal drug, cephalosporins) is largely influenced by mainly determined by the area under the
especially a beta-lactam antibiotic, the aggregate time, though not necessar- inhibitory plasma concentration-time
ge n e r a l l y r e s u l ts i n a nt a g o n i s m . ily continuous, during which effective curve (AUIC). The area under the inhibi-
Chloramphenicol and a fluoroquinolone plasma concentrations (> MIC for patho- tory concentration curve indicates the
are antagonistic. However, erythromycin genic microorganism) are maintained; degree of exposure of a microorganism to
and rifampin act synergistically against peak height determines the rate of the drug. Aminoglycosides and fluoro-
Rhodococcus equi, while tetracycline and penicillin penetration into the site of quinolones induce a post-antibiotic
rifampin (or streptomycin) used concur- infection. The clinical effectiveness of sub-MIC effect on some species of
rently provide enhanced clinical efficacy discontinuous dosage regimens for gram-negative aerobic bacteria. On
against Brucella spp. in human beings, penicillins could be attributed to the account of its variable duration, generally
horses and dogs. While rifampin is post-antibiotic sub-MIC effect they exert from 1–6 h, the post-antibiotic effect is not
particularly useful against macrophage- on gram-positive bacteria. The post- taken into account when calculating
associated (intracellular) susceptible antibiotic sub-MIC effect (PASME) refers dosage regimens. For the treatment of
microorganisms, it should always be used to a temporally limited suppression of systemic bacterial infections caused by
concurrently with another antimicrobial bacterial growth that occurs at sub- susceptible microorganisms, the usual
0038-2809 Tydskr.S.Afr.vet.Ver. (1998) 69(4): 174–185 183
dosage intervals are 8–12 h for amino- therapy is largely governed by the should be based on monitoring the
glycosides, injected IM or SC, and 12 h for responsiveness of host defense mecha- response both by clinical assessment of
fluoroquinolones (with the exception of nisms. This applies particularly to drugs the animal and bacterial culture of
marbofloxacin, 24 h), administered orally, that produce a bacteriostatic effect. The p r o p er l y c o l l ec t ed s p ec i m e n s . B y
in dogs. Some authors contend, from both concentration attained by an anti- adopting the approach outlined in this
a safety and clinical efficacy standpoint, microbial agent at the site of infection paper, the success of antimicrobial
that the dosage interval for amino- may be influenced by disease-induced therapy will likely be increased and the
glycosides could be 24 h18,21. Since amino- changes in the disposition of the drug as indiscriminate use of antimicrobial agents
glycosides are potentially ototoxic and well as by local changes associated with will be reduced. Moreover, the animal
nephrotoxic and can accumulate, due to tissue inflammation or abscess formation. owner will become increasingly aware of
their prolonged terminal elimination, the Disease states that may alter the disposi- the fact that there is far more to
monitoring of trough serum/plasma tion of drugs include fever, dehydration, antimicrobial therapy than the adminis-
concentrations (Cmin), which should not hypoalbuminaemia (associated with tration of an empirically selected
be allowed to exceed 2 µg/m , is important chronic liver disease) and uraemia antimicrobial preparation and will
particularly in the presence of renal (chronic renal failure). The bactericidal ultimately appreciate the longterm bene-
impairment. activity of aminoglycosides and fluoro- fits and cost-effectiveness of the scientific
It is highly desirable for bactericidal quinolones (apart from difloxacin) approach.
drugs (e.g. beta-lactam antibiotics, against gram-negative aerobic bacteria is
aminoglycosides, fluoroquinolones) and greater in an alkaline than in an acidic REFERENCES
1. Aktas M, Lefebvre H P, Toutain P L, Braun J
essential for bacteriostatic drugs (e.g. environment. In the presence of impaired P 1995 Disposition of creatine kinase
tetracyclines, chloramphenicol and its renal function, which may be detected by activity in dog plasma following intrave-
derivatives, macrolides and lincosa- urinalysis (proteinuria and the presence nous and intramuscular injection of skeletal
mides) to maintain plasma concentra- of casts), dosage regimens for amino- muscle homogenates. Journal of Veterinary
Pharmacology and Therapeutics 18: 1–6
tions above the minimum effective glycosides should be adjusted (preferably
2. Banting A L, Baggot J D 1996 Comparison of
concentrations for the duration of by increasing the dosage interval in the pharmacokinetics and local tolerance of
therapy. The terms bactericidal and accordance with the decrease in glomeru- three injectable oxytetracycline formula-
bacteriostatic are relative, not absolute. lar filtration rate) in order to avoid drug tions in pigs. Journal of Veterinary Pharmacol-
accumulation with attendant toxic effects ogy and Therapeutics 19: 50–55
3. Boyd J S 1987 Selection of sites for intramus-
DURATION OF THERAPY (acute tubular necrosis and cochlear
cular injections in the neck of the horse. The
Antimicrobial therapy must be main- damage in dogs or vestibular damage in Veterinary Record 121: 197–200
tained for an adequate duration, which is cats). An indication of the extent of a 4. Finco D R, Brown S A, Vaden S L, Ferguson
based on monitoring the response both decrease in the glomerular filtration rate D C 1995 Relationship between plasma
by clinical assessment (resolution of fever, (GFR) may be obtained by measuring creatinine concentration and glomerular
filtration rate in dogs. Journal of Veterinary
leukocytosis and other signs of inflamma- endogenous creatinine clearance. In dogs Pharmacology and Therapeutics 18: 418–421
tion) and bacterial culture. Definitive with decreased renal function (GFR < 5. Firth E C, Nouws J F M, Driessens F,
diagnosis at an early stage of infection 3 m /min/kg; in normal dogs, GFR = 4.07 Schmaetz P, Peperkamp K, Klein W R 1986
and the application of specific therapy, ± 0.52 m /min/kg), the reciprocal of serum Effect of the injection site on the pharmaco-
based on knowledge of the causative creatinine concentration provides a clini- kinetics of procaine penicillin G in horses.
American Journal of Veterinary Research 47:
pathogenic microorganism and its cally useful estimation of the glomerular 2380–2384
susceptibility, will decrease the overall filtration rate4 that could serve as a guide 6. George L W, Smith J A 1985 Treatment of
duration of treatment and minimise for dosage interval adjustment of amino- Moraxella bovis infections in calves using a
residual sequelae. Therapy with an glycoside antibiotics. The monitoring of long acting oxytetracycline formulation.
aminoglycoside should not be extended trough serum/plasma concentrations of Journal of Veterinary Pharmacology and
Therapeutics 8: 55–61
beyond the duration required to treat the an aminoglycoside is highly desirable in 7. Gilman J M, Davis L E, Neff-Davis C A,
infection. The speed of clinical response is animals with severe infections or renal Koritz G D, Baker G J 1987 Plasma concen-
generally inversely related to the length impairment and is essential in animals tration of gentamicin after intramuscular or
of time the infection was present before with changing renal function. subcutaneous administration to horses.
initiating therapy. After an infectious disease has been Journal of Veterinary Pharmacology and Thera-
peutics 10: 101–103
There are certain infections that, owing diagnosed in an animal, the decision has 8. Grondel J L, Nouws J F M, Schutte A R,
to the relative inaccessibility of the caus- to be made as to whether an antimicrobial Driessens F 1989 Comparative pharmaco-
ative microorganisms to antimicrobial agent should be administered. When the kinetics of oxytetracycline in rainbow trout
agents, invariably require a prolonged answer is positive, and following proper (Salmo gairdneri) and African catfish (Clarias
duration (3–5 weeks, rather than 5–8 collection of appropriate specimens, the gariepinus). Journal of Veterinary Pharmacol-
ogy and Therapeutics 12: 157–162
days) of therapy. They include prostatitis, treatment should be promptly initiated 9. Hinton M 1986 The ecology of Escherichia
osteomyelitis and skin infections in dogs, with an antimicrobial selected on an coli in animals including man with particu-
and Rhodococcus equi pneumonia in foals informed empirical basis. The microbio- lar reference to drug resistance. The Veteri-
(6–16 weeks of age). In the treatment of logical and clinical chemistry results from nary Record 119: 420–426
10. Jacobson E R 1993 Antimicrobial drug use in
these infections, preference should be the samples submitted for analysis, in
reptiles. In Prescott J F, Baggot J D (eds)
given to the use of orally-effective conjunction with the response of the Antimicrobial therapy in veterinary medicine
antimicrobial agents. animal to the initial treatment, provide (2nd edn). Iowa State University Press,
the requisite information for selecting the Ames, Iowa: 542–552
VARIABLES THAT INFLUENCE antimicrobial agent to use for the continu- 11. Jacoby G A, Archer G L 1991 New mecha-
nisms of bacterial resistance to antimicro-
CLINICAL RESPONSE ation of treatment. The usual dosage
bial agents. New England Journal of Medicine
Even when the antimicrobial drug of regimen for the particular antimicrobial 324: 601–612
choice is administered at the recom- preparation selected can generally be 12. Martinez M N, Berson M R 1998 Bio-
mended dosing rate, the outcome of applied, while the duration of treatment availability/bioequivalence assessments. In
184 0038-2809 Jl S.Afr.vet.Ass. (1998) 69(4): 174–185
Hardee G E, Baggot J D (eds) Development Iowa State University Press, Ames, Iowa non-invasive and quantitative method
and formulation of veterinary dosage forms 17. Rutgers L J E, Van Miert A S J P A M, Nouws for the study of tissue injury caused by
(2nd edn). Marcel Dekker, New York: J F M, Van Ginneken C A M 1980 Effect of intramuscular injection of drugs in horses.
429–467 the injection site on the bioavailability of Journal of Veterinary Pharmacology and Thera-
13. Martinez-Martinez L, Pascual A, Jacoby G A amoxycillin trihydrate in dairy cows. Jour- peutics 18: 226–235
1998 Quinolone resistance from a transfer- nal of Veterinary Pharmacology and Therapeu- 20. Wilson R C, Duran S H, Horton C R, Wright
able plasmid. Lancet 351: 797–799 tics 3: 125–132 L C 1989 Bioavailability of gentamicin in
14. Nouws J F M, Vree T B 1983 Effect of 18. Swan G E, Guthrie A J, Mulders M S G, dogs after intramuscular or subcutaneous
injection site on the bioavailability of an Killeen V M, Nurton J P, Short, C R, Van den injections. American Journal of Veterinary
oxytetracycline formulation in ruminant Berg J S 1995 Single and multiple dose Research 50: 1748–1750
calves. The Veterinary Quarterly 5: 165–170 pharmacokinetics of gentamicin adminis- 21. Zhanel G G 1993 Once daily aminoglyco-
15. Prescott J F, Baggot J D 1985 Antimicrobial tered intravenously and intramuscularly in side dosing: the result of research on
susceptibility testing and antimicrobial adult conditioned Thoroughbred mares. antimicrobial pharmacodynamics. Ameri-
drug dosage. Journal of the American Veteri- Journal of the South African Veterinary Associa- can Journal of Pharmaceutical Education 56:
nary Medical Association 187: 363–368 tion 66: 151–156 156–167
16. Prescott J F, Baggot J D 1993 Antimicrobial 19. Toutain P L, Lassourd V, Costes G, Alvinerie
therapy in veterinary medicine (2nd edn). M, Bret L, Lefebvre H P, Braun J P 1995 A
Note added in proof
Foals treated with erythromycin and rifampin for Rhodococcus equi infection (pneumonia) could serve as a potential reservoir of Clostridium
difficile and excrete the microorganism, resistant to both antimicrobial agents, in the faeces. It would appear that erythromycin is the offending drug; it
may promote the growth of C. difficile in the intestine of the foal, and a variable fraction of the oral dose, seemingly irrespective of the dosage form, is
excreted in the faeces (Baverud et al. 1998 Clostridium difficile associated with acute colitis in mares when their foals are treated with erythromycin
and rifampin for Rhodococcus equi pneumonia. Equine Veterinary Journal 30: 482–488). Coprophagic behaviour of mares housed with
erythromycin-treated foals would lead to ingestion of the resistant microorganism and the antibiotic, which could severely disrupt the commensal flora
of the large intestine, resulting in acute colitis in the mares. The available evidence suggests that this scenario is nosocomial infection.
Obituary
Henri Pieter Albert de Boom — 16 October 1914 – 30 August 1998
Just after midnight on Sunday morning, 30 August, 1st-year student at Onderstepoort, where he qualified
veterinary science’s best-loved and respected teacher in 1936. Until then his career literally ran parallel to that
passed on. He is survived by his children Marcella, of another well-known colleague, Prof. Mike de Lange.
Carin and Jannie and 8 grandchildren. He lost his wife,
Sarie, in 1991. During the last years he fought valiantly
against deafness and increasing blindness due to a
retinal injury sustained in a serious motor accident
during the 1980s.
From January 1937 until his retirement in 1974, 37
years later, Boompie was attached to Onderstepoort,
initially as a research officer, later as a temporary
lecturer in the Department of Anatomy, Faculty of
Veterinary Science, until lecturing posts were changed
from part-time to full-time. In October 1955 he
succeeded Prof. Cecil Jackson as professor and head of
the Department of Anatomy.
His very earliest memory, he said, was an unforgetta-
ble day when, as a toddler, he sat on the steps in front of
his parents' home in Pretoria. His mother brought him
something to drink and, as he turned towards her, he
tumbled head over heels down the steps. He recalled
that it was like a vivid slow-motion movie as he stood on
his head and observed how fascinating the upside-
down world appeared. This conscious sense of wonder
about everything remained with him throughout his
life.
Born in Pretoria, he started and completed his
schooling at ‘Oosteindschool’. He was head boy when
he matriculated in 1931. The next year, he enrolled as a
Continued on p. 186
0038-2809 Tydskr.S.Afr.vet.Ver. (1998) 69(4): 174–185 185
S-ar putea să vă placă și
- AntibioticDocument84 paginiAntibioticDr. Kalavati PrajapatiÎncă nu există evaluări
- Antibiotics 1Document64 paginiAntibiotics 1Justin Ancog100% (1)
- Poultry Nutrition and FeedingDocument16 paginiPoultry Nutrition and FeedingYaserAbbasiÎncă nu există evaluări
- Poultry Nutrition and FeedingDocument16 paginiPoultry Nutrition and FeedingYaserAbbasiÎncă nu există evaluări
- Veterinary Drug Formulary2014 English PDFDocument19 paginiVeterinary Drug Formulary2014 English PDFSamuel LamÎncă nu există evaluări
- Diagnostic Microbiology and Laboratory MethodsDocument70 paginiDiagnostic Microbiology and Laboratory MethodsArulmany SelliahÎncă nu există evaluări
- Antimicrobial Therapy in Veterinary MedicineDe la EverandAntimicrobial Therapy in Veterinary MedicineSteeve GiguèreEvaluare: 4 din 5 stele4/5 (1)
- Bovine Disease Diagnostic ManualDocument40 paginiBovine Disease Diagnostic ManualYaserAbbasi100% (1)
- A Guidebook To Plant Screening - Phytochemical and BiologicalDocument19 paginiA Guidebook To Plant Screening - Phytochemical and BiologicalBere García50% (2)
- MBR 2019 - Pharmacology HandoutsDocument125 paginiMBR 2019 - Pharmacology HandoutsRgm UyÎncă nu există evaluări
- Antibiotics: Uses ActionDocument11 paginiAntibiotics: Uses Actionammar amerÎncă nu există evaluări
- The Role of PPRA in Antibiotic Prescription in ICUDocument34 paginiThe Role of PPRA in Antibiotic Prescription in ICUriko_synergy88Încă nu există evaluări
- L P 6 Antibiotics - LAB - Fina - 2022Document33 paginiL P 6 Antibiotics - LAB - Fina - 2022Zakria Al-HadadÎncă nu există evaluări
- Classification of Antibiotics: Antimicrobial Agents Antibiotics or AntimicrobialsDocument5 paginiClassification of Antibiotics: Antimicrobial Agents Antibiotics or AntimicrobialsDimple CosÎncă nu există evaluări
- ANTIMICROBIALSDocument1 paginăANTIMICROBIALSoperation KDNAÎncă nu există evaluări
- Sas Hes032 7Document7 paginiSas Hes032 7Jose Melmar Autida AutenticoÎncă nu există evaluări
- Sas 7 Hes032Document7 paginiSas 7 Hes032Shine Samm EstoseÎncă nu există evaluări
- Introduction and Overview Antibiotics and Chemotherapeutic Agents Micro 260 Chapter 12 NotesDocument8 paginiIntroduction and Overview Antibiotics and Chemotherapeutic Agents Micro 260 Chapter 12 NotesNEHA DIXITÎncă nu există evaluări
- S1473309905700517 - 1 s2.0 S1473309905700517 MainDocument10 paginiS1473309905700517 - 1 s2.0 S1473309905700517 MainwardaninurindahÎncă nu există evaluări
- Antibiotic Therapy: What Factors Influence Antibiotic Choice in Critically Ill Patients?Document5 paginiAntibiotic Therapy: What Factors Influence Antibiotic Choice in Critically Ill Patients?Felipe González RodríguezÎncă nu există evaluări
- Small Animal SurgeryDocument7 paginiSmall Animal Surgeryhonovezaann.a.campita.ctucvmÎncă nu există evaluări
- Best Practice & Research Clinical Gastroenterology: Maria Meneghini, Oriol Bestard, Josep Maria GrinyoDocument7 paginiBest Practice & Research Clinical Gastroenterology: Maria Meneghini, Oriol Bestard, Josep Maria GrinyoRohaniÎncă nu există evaluări
- Antimicrobial AgentsDocument4 paginiAntimicrobial AgentsKristine ManioÎncă nu există evaluări
- L2 - Antimicrobial AgentsDocument12 paginiL2 - Antimicrobial AgentstheresmachÎncă nu există evaluări
- Chapter 9 Surgical Infections and Antibiotic SelectionDocument42 paginiChapter 9 Surgical Infections and Antibiotic SelectionSteven Mark MananguÎncă nu există evaluări
- Disease Control by MorgsDocument11 paginiDisease Control by Morgseucharia.ezeumehÎncă nu există evaluări
- Fuller AbxDocument78 paginiFuller AbxKe XuÎncă nu există evaluări
- Antimicrobials 2018Document24 paginiAntimicrobials 2018Harsha MaheshwariÎncă nu există evaluări
- Chapter 5CDocument2 paginiChapter 5Cngoc.nguyenlamÎncă nu există evaluări
- Antibacterial Drugs: Principles of Antibacterial ChemotherapyDocument11 paginiAntibacterial Drugs: Principles of Antibacterial Chemotherapymanideep mungiÎncă nu există evaluări
- Fmicb 09 02066Document16 paginiFmicb 09 02066Renata CalixtoÎncă nu există evaluări
- Mechanisms of The Post-Antibiotic Effects Induced by Rifampicin and Gentamicin in Escherichia ColiDocument5 paginiMechanisms of The Post-Antibiotic Effects Induced by Rifampicin and Gentamicin in Escherichia ColiNoel Saúl Argüello SánchezÎncă nu există evaluări
- Tài Liệu Về Các Kháng Sinh 2Document15 paginiTài Liệu Về Các Kháng Sinh 2tuannguyen010700Încă nu există evaluări
- Fomnya Et AlDocument13 paginiFomnya Et AlJesse IshayaÎncă nu există evaluări
- Targeting Virulence A New Paradigm ForDocument8 paginiTargeting Virulence A New Paradigm ForSILVIANO PEREZ PEREZÎncă nu există evaluări
- Antimicrobial Susceptibility Testing & Antimicrobial AgentsDocument18 paginiAntimicrobial Susceptibility Testing & Antimicrobial AgentsMayra FlorÎncă nu există evaluări
- Antimikroba Pada Infeksi BedahDocument39 paginiAntimikroba Pada Infeksi BedahDenise JohnsonÎncă nu există evaluări
- Antimicrobial Pharmacology 9Document164 paginiAntimicrobial Pharmacology 9elias adugnaÎncă nu există evaluări
- Pharmacology MidtermDocument37 paginiPharmacology Midtermnaomie manaliliÎncă nu există evaluări
- Pharmacology MidtermDocument27 paginiPharmacology Midtermnaomie manaliliÎncă nu există evaluări
- AntibioticsDocument49 paginiAntibioticsShriefElghazalyÎncă nu există evaluări
- Antimicrobial Chemotherapy Part 2Document27 paginiAntimicrobial Chemotherapy Part 2Samara ZahidÎncă nu există evaluări
- Chapter-9 Antibiotic and Emergence of Resistance - 2Document28 paginiChapter-9 Antibiotic and Emergence of Resistance - 2Hillani TadesseÎncă nu există evaluări
- Serologic Tests Part 3Document2 paginiSerologic Tests Part 3Joshua TrinidadÎncă nu există evaluări
- Cơ Chế Kháng Thuốc Gram (+) 2Document9 paginiCơ Chế Kháng Thuốc Gram (+) 2Quỳnh Nguyễn Thị NhưÎncă nu există evaluări
- 2 Chemotherapy-BSN-PUDocument5 pagini2 Chemotherapy-BSN-PUNim DCÎncă nu există evaluări
- Principles To ChemotherapyDocument32 paginiPrinciples To ChemotherapyWezzyÎncă nu există evaluări
- 1.antibiotic Drugs (L1&L2)Document24 pagini1.antibiotic Drugs (L1&L2)Asem AlhazmiÎncă nu există evaluări
- Antibiotics: Sana Husain & Rabia Mukaty FY-C3Document8 paginiAntibiotics: Sana Husain & Rabia Mukaty FY-C3sanÎncă nu există evaluări
- Khameneh 2019Document28 paginiKhameneh 2019Monyet...Încă nu există evaluări
- CHAPTER 9 Micro Lec TranseesDocument4 paginiCHAPTER 9 Micro Lec TranseesDylan HimoÎncă nu există evaluări
- Antibiotics: Biotechnology IIDocument11 paginiAntibiotics: Biotechnology IINareshÎncă nu există evaluări
- Pharma 14 To 23Document298 paginiPharma 14 To 23Loai Mohammed IssaÎncă nu există evaluări
- Group 9 - Bacteriology Reporting (Written Report)Document6 paginiGroup 9 - Bacteriology Reporting (Written Report)DENISE MARA�AÎncă nu există evaluări
- Differentiated Extracts From Freshwater and Terrestrial Mollusks Inhibit Virulence Factor Production in CryptococcusDocument17 paginiDifferentiated Extracts From Freshwater and Terrestrial Mollusks Inhibit Virulence Factor Production in Cryptococcussooho32Încă nu există evaluări
- Module 4 AntimicrobialsDocument23 paginiModule 4 AntimicrobialsROJANE LAMENTACÎncă nu există evaluări
- Pelvic Inflammatory Disease - 5Document5 paginiPelvic Inflammatory Disease - 5fatqur28Încă nu există evaluări
- Prudent Used of AntibioticsDocument9 paginiPrudent Used of AntibioticsBintari AnindhitaÎncă nu există evaluări
- Pharmacokinetics and Pharmacodynamics of Antibacterial Agents PDFDocument29 paginiPharmacokinetics and Pharmacodynamics of Antibacterial Agents PDFarmitadewiÎncă nu există evaluări
- Day 2 General Microbiology 12-1-2021Document150 paginiDay 2 General Microbiology 12-1-2021ShriefElghazalyÎncă nu există evaluări
- MLS206 Antibiotics 2020 PDFDocument19 paginiMLS206 Antibiotics 2020 PDFdrtsotlhe mogolegwaÎncă nu există evaluări
- Ch12 Part1Document15 paginiCh12 Part1lasanders601Încă nu există evaluări
- Antimicrobial TherapyDocument18 paginiAntimicrobial TherapyekasukmawatyÎncă nu există evaluări
- Chemotherapy - General IntroductionDocument15 paginiChemotherapy - General Introductionwolverine12309Încă nu există evaluări
- Introduction To Chemotherapy PDFDocument15 paginiIntroduction To Chemotherapy PDFAbdulla Hil KafiÎncă nu există evaluări
- Antimicrobial ActionDocument26 paginiAntimicrobial ActionAnne CabreraÎncă nu există evaluări
- Medicinal Plants: Microbial Interactions, Molecular Techniques and Therapeutic TrendsDe la EverandMedicinal Plants: Microbial Interactions, Molecular Techniques and Therapeutic TrendsÎncă nu există evaluări
- Common Parasitic Diseases of CamelDocument2 paginiCommon Parasitic Diseases of CamelYaserAbbasiÎncă nu există evaluări
- 114 PDFDocument3 pagini114 PDFAhmad AssariÎncă nu există evaluări
- Drug Dosages Used - in Avian Medicine - App1 PDFDocument6 paginiDrug Dosages Used - in Avian Medicine - App1 PDFYaserAbbasiÎncă nu există evaluări
- Drug Dosages Used - in Avian Medicine - App1 PDFDocument6 paginiDrug Dosages Used - in Avian Medicine - App1 PDFYaserAbbasiÎncă nu există evaluări
- Surgical Problems of The Penis and Prepuce of Bulls Part IDocument4 paginiSurgical Problems of The Penis and Prepuce of Bulls Part IYaserAbbasiÎncă nu există evaluări
- Guinea Pigs PDFDocument1 paginăGuinea Pigs PDFYaserAbbasiÎncă nu există evaluări
- Feedlot Fattening of Sheep & Goats PDFDocument50 paginiFeedlot Fattening of Sheep & Goats PDFYaserAbbasiÎncă nu există evaluări
- Porcellus. The Guinea Pig Neither Comes From Guinea, Nor Is It A Pig. It Is Currently Considered ADocument7 paginiPorcellus. The Guinea Pig Neither Comes From Guinea, Nor Is It A Pig. It Is Currently Considered AYaserAbbasiÎncă nu există evaluări
- Trace Element Nutrition SheepDocument6 paginiTrace Element Nutrition SheepYaserAbbasiÎncă nu există evaluări
- Update On Antibiotic Therapy in The Horse PDFDocument3 paginiUpdate On Antibiotic Therapy in The Horse PDFYaserAbbasiÎncă nu există evaluări
- Ewe Fertility For Better Returns: Sheep BRP Manual 11Document24 paginiEwe Fertility For Better Returns: Sheep BRP Manual 11YaserAbbasiÎncă nu există evaluări
- Antimicrobial Use in Mare Re PDFDocument12 paginiAntimicrobial Use in Mare Re PDFYaserAbbasiÎncă nu există evaluări
- Mohamed Zain Eldein - Examination of Large RuminantDocument33 paginiMohamed Zain Eldein - Examination of Large RuminantYaserAbbasiÎncă nu există evaluări
- Bovine Disease AtlasDocument164 paginiBovine Disease AtlasYaserAbbasiÎncă nu există evaluări
- Lander's Veterinary ToxicologyDocument337 paginiLander's Veterinary ToxicologyYaserAbbasiÎncă nu există evaluări
- Ostrich Feeding and NutritionDocument8 paginiOstrich Feeding and NutritionYaserAbbasiÎncă nu există evaluări
- Equipment For Sheep ProductionDocument10 paginiEquipment For Sheep ProductionYaserAbbasiÎncă nu există evaluări
- Injectable Anesthesia and Analgesia of Birds 5-Aug PDFDocument15 paginiInjectable Anesthesia and Analgesia of Birds 5-Aug PDFYaserAbbasiÎncă nu există evaluări
- Ostrich NutritionDocument10 paginiOstrich NutritionYaserAbbasiÎncă nu există evaluări
- Sap245entire PDFDocument105 paginiSap245entire PDFYaserAbbasiÎncă nu există evaluări
- Handbook Control of Parasites of Sheep Dec2010Document56 paginiHandbook Control of Parasites of Sheep Dec2010ZandarPalimirÎncă nu există evaluări
- Surgery in Pet BirdsDocument14 paginiSurgery in Pet BirdsYaserAbbasiÎncă nu există evaluări
- Worm Control in Dogs and CatsDocument28 paginiWorm Control in Dogs and CatsYaserAbbasiÎncă nu există evaluări
- Management of Reproduction of SheepDocument4 paginiManagement of Reproduction of SheepYaserAbbasiÎncă nu există evaluări
- Small Animal OphthalmologyDocument8 paginiSmall Animal OphthalmologyYaserAbbasi100% (1)
- Enteritis and Colitis in HorsesDocument44 paginiEnteritis and Colitis in HorsesANDRE LEONARD FARFAN SUAREZÎncă nu există evaluări
- Uji Daya Hambat Ekstrak Etanol Rimpang Temu Giring (Curcuma Hey Neana Val.) Terhadap PertumbuhanDocument7 paginiUji Daya Hambat Ekstrak Etanol Rimpang Temu Giring (Curcuma Hey Neana Val.) Terhadap PertumbuhanMarina Silitonga94Încă nu există evaluări
- OctenidineDocument24 paginiOctenidinerima nurmayasariÎncă nu există evaluări
- Schiff Bases: A Short Review of Their Antimicrobial ActivitiesDocument8 paginiSchiff Bases: A Short Review of Their Antimicrobial ActivitiesDebdeep MondalÎncă nu există evaluări
- Antimicrobial and Wound Healing Activity7002672051305248058 PDFDocument150 paginiAntimicrobial and Wound Healing Activity7002672051305248058 PDFpaneisanÎncă nu există evaluări
- Bauhinia Purpurea ArticleDocument6 paginiBauhinia Purpurea Articlesakhi dewaniÎncă nu există evaluări
- Rosemary AntibacterialDocument5 paginiRosemary AntibacterialNurul Izzah Wahidul AzamÎncă nu există evaluări
- Chemical Composition, Antibacterial and Antifungal Activities of Ruta Graveolens L. Volatile OilsDocument11 paginiChemical Composition, Antibacterial and Antifungal Activities of Ruta Graveolens L. Volatile OilsRadwan AjoÎncă nu există evaluări
- TDS Troycare BD55Document5 paginiTDS Troycare BD55Sabun B-KlinÎncă nu există evaluări
- Parmetol A 26 ZTM P Ic e enDocument2 paginiParmetol A 26 ZTM P Ic e enalthea badayosÎncă nu există evaluări
- 4 Antibacterial Activity of Ethanolic Extract of Hibiscus Rosa Sinensis Flower Against Staphylococcus Epidermidis and Staphylococcus SaprophyticusDocument12 pagini4 Antibacterial Activity of Ethanolic Extract of Hibiscus Rosa Sinensis Flower Against Staphylococcus Epidermidis and Staphylococcus Saprophyticusrayven casugayÎncă nu există evaluări
- Inhibition of Cell Wall SynthesisDocument6 paginiInhibition of Cell Wall SynthesisDuaa ShamiehÎncă nu există evaluări
- Antimicrobial Activity of Medicinal Plants Thesis PDFDocument6 paginiAntimicrobial Activity of Medicinal Plants Thesis PDFjennifercruzwashington100% (1)
- Comparative Study of Bell Pepper On TheDocument3 paginiComparative Study of Bell Pepper On TheAngelica Mae DanaoÎncă nu există evaluări
- CXG 077eDocument28 paginiCXG 077equality control pt dusÎncă nu există evaluări
- DeclomycineDocument14 paginiDeclomycineRamanasarmaÎncă nu există evaluări
- Xue2016 PDFDocument34 paginiXue2016 PDFThamiris MartinyÎncă nu există evaluări
- Hygiene 02 00009Document11 paginiHygiene 02 00009Antimikrop MikrobiyolojiÎncă nu există evaluări
- HumboldtiaMS ReviewDocument7 paginiHumboldtiaMS ReviewKrishnaraj M VÎncă nu există evaluări
- WHO NetDocument50 paginiWHO Nettummalapalli venkateswara raoÎncă nu există evaluări
- Chapter 3 Bio461 (Revised)Document61 paginiChapter 3 Bio461 (Revised)Muhammad Arief AimanÎncă nu există evaluări
- Natural Products From Polar OrganismsDocument20 paginiNatural Products From Polar OrganismsRDVVÎncă nu există evaluări
- Limsuwan BiofilmDocument8 paginiLimsuwan BiofilmJi Hyun SeoÎncă nu există evaluări
- Conclusions and RecommendationsDocument4 paginiConclusions and RecommendationsNAPOLEONÎncă nu există evaluări
- Synergistic Antibacterial Activity of Salvia Officinalis and Cichorium Intybus Extracts and AntibioticsDocument7 paginiSynergistic Antibacterial Activity of Salvia Officinalis and Cichorium Intybus Extracts and AntibioticsSAHID IQBALÎncă nu există evaluări
- Antibacterial and Cytotoxicity Studies of Gossypol Isolated From Fruits of Thespesia Populnea (L.) Sol. Ex Correa - A Remedy For Skin DiseasesDocument10 paginiAntibacterial and Cytotoxicity Studies of Gossypol Isolated From Fruits of Thespesia Populnea (L.) Sol. Ex Correa - A Remedy For Skin DiseasesIJAR JOURNALÎncă nu există evaluări
- Articulo Cientifico Derivado Del FenilpropanoDocument23 paginiArticulo Cientifico Derivado Del FenilpropanoKaren GonzalezÎncă nu există evaluări